Published online Nov 19, 2023. doi: 10.5498/wjp.v13.i11.893
Peer-review started: August 3, 2023
First decision: August 16, 2023
Revised: August 25, 2023
Accepted: September 22, 2023
Article in press: September 22, 2023
Published online: November 19, 2023
Processing time: 106 Days and 0.4 Hours
Alcohol addiction, or alcohol dependence, refers to a psychological state of strong craving for alcohol caused by drinking when both the drinking times and alcohol consumption reach a certain level. Alcohol addiction can cause irreversible damage, leading to mental illness or mental disorders, negative changes in their original personality, and a tendency to safety incidents such as committing suicide or violent attacks on others. Significant attention needs to be given to the mental health of alcohol addicts, which could reflect their abnormal personality traits. However, only a few papers on this issue have been reported in China.
To investigate the correlation between mental health and personality in patients with alcohol addiction.
In this single-center observational study, we selected 80 patients with alcohol addiction as the research subjects, according to the criteria of the K10 scale to evaluate the mental health of patients with alcohol addiction, and divided these patients into four groups based on the evaluation results: Good, average, relatively poor and bad. And then analyzed the correlation between mental health conditions and personality characteristics from these four groups of patients.
The average score of the K10 scale (Kessler 10 Simple Psychological Status Assessment Scale) in 80 patients with alcohol addiction was 25.45 points, the median score was 25 points, the highest score was 50 points, and the lowest score was 11 points. Pearson's analysis showed that the K10 score was positively correlated with the scores of these two subscales, such as the P-subscale and the N-subscale (P < 0.05). In contrast, the K10 score had no significant correlation with the scores from the E-subscale and the L-subscale (P > 0.05).
The mental health conditions of patients with alcohol addiction are positively correlated with their personality characteristics.
Core Tip: Alcohol addiction, as a special behavioral pattern, can cause serious mental and physical burdens, and therefore must be highly valued. This article aims to explore the correlation between the formation of alcohol addiction as a behavioral pattern and personality. By randomly grouping alcohol addicted patients and evaluating their mental health using the K10 scale, the results showed that the mental health status of alcohol addicted patients was positively correlated with their personality traits.
- Citation: Liu Y, Liu Y, Cheng J, Pang LJ, Zhang XL. Correlation analysis of mental health conditions and personality of patients with alcohol addiction. World J Psychiatry 2023; 13(11): 893-902
- URL: https://www.wjgnet.com/2220-3206/full/v13/i11/893.htm
- DOI: https://dx.doi.org/10.5498/wjp.v13.i11.893
Alcohol addiction, or alcohol dependence, refers to a psychological state of strong craving for alcohol caused by drinking when both the drinking times and alcohol consumption reach a certain level. Alcohol addicts may get to the point of failing to control their drinking behavior, and a series of physical tolerance or withdrawal symptoms will appear[1]. These reactions will manifest as the patient's compulsive craving for alcohol. After the cessation of drinking behavior, some physical withdrawal symptoms may occur, such as palpitations, trembling, and dyspnea, or psychological withdrawal symptoms, such as anxiety, depression, and delusions of victimization. The above symptoms could disappear with the resumption of the drinking behavior[2]. Alcohol addiction is a disease that is difficult to cure, with a high prevalence rate and a high rate of relapse. According to data from the World Health Organization in 2018[3], approximately 237 million men and 46 million women worldwide suffered from alcohol dependence syndrome. The data shows that, in 2018, the annual drinking volume per capita in Chinese was 7.14 L, the annual drinking volume per capita in Northern American countries was 9.71 L, the annual drinking volume per capita in Western Europe countries was 11.13 L, and the yearly drinking volume per capita in Australia was 10.47 L. The proportion of heavy drinkers among China adults was 22.6%. The proportion of heavy drinkers among North American adults was 25.7%; among Western European adults was 30.5%; and among Australian adults was 34.4%[3].
According to the World Health Organization, health is defined as the absence of disease or being free of infirmity and the balanced and normal state of physical, psychological, and social[4]. Mental health is one of the most important public health issues in the world all the time. Psychological health, like physical health, can also affect the life quality of individuals; this fact should be prompting people to pay more attention to mental illness as to physical diseases[5]. Alcohol addiction can cause irreversible damage to the physical status, psychological conditions, and social adaptations of patients who suffer from it. It results in mental illness or mental disorders, causing negative changes in their original personality characteristics[6] and leading to vicious public safety incidents such as committing suicide or launching violent attacks on others. It is important to pay attention to the mental health of people with alcohol addiction.
Personality is the organic unity of the dynamic internal organization and the corresponding behavior patterns formed by individuals in various interactions. It is a complex structural system, mainly including two aspects; the tendency of personality and the rational characteristics of personality, the former is the driving force of personality, and the latter refers to the differences that exist among individuals[7]. In addition to physical damage like alcoholic liver disease, long-term heavy drinking can disturb their social adaptation and potentiate negative personality changes[8]. Alcohol addiction is strongly associated with personality disorders[9,10]. Personality disorders are considered important factors in the pathogenesis, persistence, and outcome of alcohol dependence in patients with these pernicious features[11].
The mental health condition of individuals is closely related to their personality characteristics. The mental health of alcohol addicts may reflect their unique but abnormal personality traits. However, at present, few related research has been reported in China. Based on this, this study aimed to investigate the correlation between mental health status and personality characteristics in people suffering from alcohol addiction.
In this single-centered observational study, we selected 80 patients with alcohol addiction treated in our hospital from January 2022 to January 2023 as the research subjects. And the inclusion criteria were the following: (1) Patients clinically diagnosed with alcohol addiction[12]; (2) The patient being aware and consciously participating in the investigation; and (3) The patient able to fill out the questionnaire independently or with the help of an investigator. Exclusion Criteria: (1) Patients with other serious illnesses that may affect their psychological condition (such as disability, cancer, etc.); (2) Patients with severe mental disorders that could impact affect the accuracy of the study; and (3) Those who are unwilling to cooperate with the investigation standards. All proceedings were carried out per the Declaration of Helsinki.
The content of the questionnaire mainly included; (1) The basic personal information on alcohol addicts; their gender, age, marital status, education level, etc.; (2) The participants’ financial situation, including the self-assessment of the financial level, whether they are autonomous, and whether they were indebted; (3) Daily life behaviors of patients, whether smoking, suffering from a sleep disorder, maintaining a good frequency of daily exercise, etc.; (4) The number of years set to the establishment of the alcohol addiction; and (5) Other related psychological conditions, including whether they had close friends to talk to, whether they encountered major setbacks or unfortunate situations, etc.
The K10 scale[13], developed by Kessler and Mrocze of the University of Michigan, assesses patients' mental health and can screen for self-management scoring scales on the population's psychological status risk factors[14]. The scale is convenient to operate, owns the non-specific character in assessment, and has been widely used in the survey of mental health group in the United States, Canada, and other countries. The K10 scale contains ten items about anxiety, depression, and stress levels experienced in the last four weeks before the assessment. These are: (1) How often do you feel tired for no reason? (2) How often do you feel nervous? (3) How often do you feel nervous, and nothing else can calm you down? (4) How often do you feel hopeless about life? (5) How often do you feel uneasy and irritable? (6) How often do you feel restless and irritable so that it is difficult for you to calm down? (7) How often do you feel depressed? (8) How often do you feel strenuous when doing anything? (9) How often do you feel sad and nothing can interest you? and (10) How often do you you’re your existence as meaningless? To each question corresponds five response criteria and scored in this manner; 5 points for "all time," 4 for "most of the time," 3 for "sometimes," 2 for "occasionally present," and 1 for "almost nonexistent." The total score is calculated according to the respondent's responses, with a score ranging from 10 to 50 points, where a maximum of 50 points could indicate that the patient has serious psychological distress, and a minimum score of 10, indicates that the patient has no psychological distress. This study was designed according to previous assessment criteria, and the overall score was classified into four levels: 10-19 points at the first level, which represented good mental health; level 2, 20-25 points, representing average mental health; level 3 score of 26-29, which represented relatively poor mental health; a score of 30-50 on a fourth scale represented bad mental health. The evaluation items of the K10 scale mainly focused on the two routine measurements such as anxiety and depression, which ascertain the degree of anxiety, depression, and life stress of the respondent during the previous four weeks and contribute to analyzing the population's mental health.
Compiled by Eysenck in 1952, revised by Professor Gong Yaoxian in 1983, and formed a Chinese edition. The adult version of the questionnaire consists of four subscales, psychotropic (P), extrovert (E), neuroticism (N), and lie (L), with 88 questions[15]. Among them, psychopathic tendencies are reflected by the P dimension, introversion and extroversion are reflected by the introvert-E dimension, emotional stability is reflected by the N dimension, and the L tendency is used as an effectiveness scale. The P, E, N, and L scales include 23, 21, 24, and 20 items in the adult questionnaire, each of which only answers "yes" and "no," with 1 point per question. Among them, the introvert-E: A high score indicates that the person is extroverted, emotionally impulsive, adventurous, and good at interacting with people. A low score can indicate introversion, emotional stability, taciturn, indifference to people, quietness, introspection, and conformity. N: A high score would suggest depression, anxiety, preoccupation, emotional instability, and sometimes irrationality. Mental quality (P): High scores may indicate delayed reaction, being withdrawn and lazy, having no contact with anyone, being emotionally cold, poorly adaptable, eccentric and bizarre, and being incongruous with the environment. L: A high score indicates it is disguised and untrue. Disguise itself has a stable personality function related to various elements of other people. In this study, Cronbach's α of the P, E, N, and L subscales were 0.71, 0.78, 0.87, and 0.71, respectively.
SPSS22.0 statistical software was used to analyze and process data. Continuous variables were confirmed by the normality test and homogeneity test for variance, and it determined that they have the homogeneity of variance based on approximately normal distribution, expressed as mean ± SD, t-test, and ANOVA (analysis of variance). Categorical variables expressed as percentages, chi-square test, Fisher exact test or Mann-Whitney test, the correlation using Pearson correlation analysis, and taking the result of P < 0.05 to indicate that the difference was statistically significant.
Biostatistics statement: The statistical methods of this study were reviewed by the clinical research office from the corresponding author’s institution prior to the submission.
Eighty patients with alcohol addiction were included in this study, 67 male patients, 13 female patients, aged 20-65 years, and the duration of the addiction was 5-30 years. For other information (Table 1).
| Variable | Number of cases (n = 80) | Constitution ratio (%) |
| Age | ||
| < 50 | 47 | 58.75 |
| ≥ 50 | 33 | 41.25 |
| Female | 13 | 16.25 |
| Man | 67 | 83.75 |
| Level of education | ||
| Primary school and below | 25 | 31.25 |
| Junior high school and Senior high school | 49 | 61.25 |
| University and above | 6 | 7.50 |
| Marital status | ||
| Married | 51 | 63.75 |
| Unmarried | 9 | 11.25 |
| Divorced or widowed | 20 | 25.00 |
| Self-evaluation of economic abundance | ||
| Yes | 31 | 38.75 |
| No | 49 | 61.255 |
| Liabilities | ||
| Yes | 33 | 41.25 |
| No | 47 | 58.75 |
| Smoking | ||
| Yes | 53 | 66.25 |
| No | 27 | 33.75 |
| Sleep disorders | ||
| Yes | 46 | 57.50 |
| No | 34 | 42.50 |
| Daily exercise | ||
| Often | 20 | 25.00 |
| Sometimes | 31 | 38.75 |
| Never | 29 | 36.25 |
| The number of years set for getting ill | ||
| ≤ 5 | 24 | 30.00 |
| 6-10 | 34 | 42.50 |
| ≥ 11 | 22 | 27.50 |
| Close friends | ||
| Yes | 28 | 35.00 |
| No | 52 | 65.00 |
| Major setbacks or unfortunate situations | ||
| Yes | 57 | 71.25 |
| No | 23 | 28.75 |
The average K10 score of the 80 patients with alcohol addiction was 25.45, with a median score of 25, with the highest score being 50 and the lowest being 11. A score of K10 between 10 and 19 indicated that the patient's mental health was good (Grade 1, low risk of mental illness) in 17 people, accounting for 21.25%; A score of K10 on a score of 20-24 indicated that the patient's mental health status is average (Grade 2, low risk of mental illness), and there are 20 people in this group, accounting for 20.00%; A K10 score of 25-29 indicated that the patient's mental health is poor (Grade 3, higher risk of mental illness) in 32 people, accounting for 40.00%; A K10 score of 30-50 indicated that the patient's mental health is poor (Grade 4, high risk of mental illness) in 11 people, accounting for 13.75% (Table 2).
| K10 Score | Number of cases | Percentage (%) |
| 10-19 | 17 | 21.25 |
| 20-24 | 20 | 20.00 |
| 25-29 | 32 | 40.00 |
| 30-50 | 11 | 13.75 |
| Total | 80 | 100.00 |
The scores of the two subscales, including P-subscale and N-subscale in the 10-19 group, 20-24 group, 25-29 group, and 30-50 group of the K10 score, were statistically significant (P < 0.05). In contrast, the overall comparison of scores in E-subscale and L-subscale was not statistically significant (P > 0.05). Among them, the scores of the P-subscale were compared in the following groups, the 10-19 groups, and the 20-24 groups were smaller than the 25-29 groups and 30-50 groups, and the differences were statistically significant (P < 0.05). About the comparison in N-subscale scores, 10-19 groups < 20-24 groups < 25-29 groups, and 30-50 groups, and the differences were statistically significant (P < 0.05) (Table 3).
| K10 scores | P | E | N | L |
| 10-19 (n = 17) | 6.34 ± 1.01b,c | 7.51 ± 1.07 | 8.88 ± 2.72a,b,c | 15.55 ± 2.31 |
| 20-24 (n = 20) | 6.91 ± 1.40b,c | 7.77 ± 2.06 | 11.84 ± 2.81b,c | 15.18 ± 3.06 |
| 25-29 (n = 32) | 8.98 ± 1.86 | 8.25 ± 1.91 | 14.72 ± 4.24 | 14.81 ± 3.47 |
| 30-50 (n = 11) | 9.71 ± 1.67 | 8.42 ± 2.29 | 15.36 ± 2.11 | 15.61 ± 1.90 |
| F | 17.920 | 0.869 | 13.670 | 0.328 |
| P value | < 0.001 | 0.460 | < 0.001 | 0.804 |
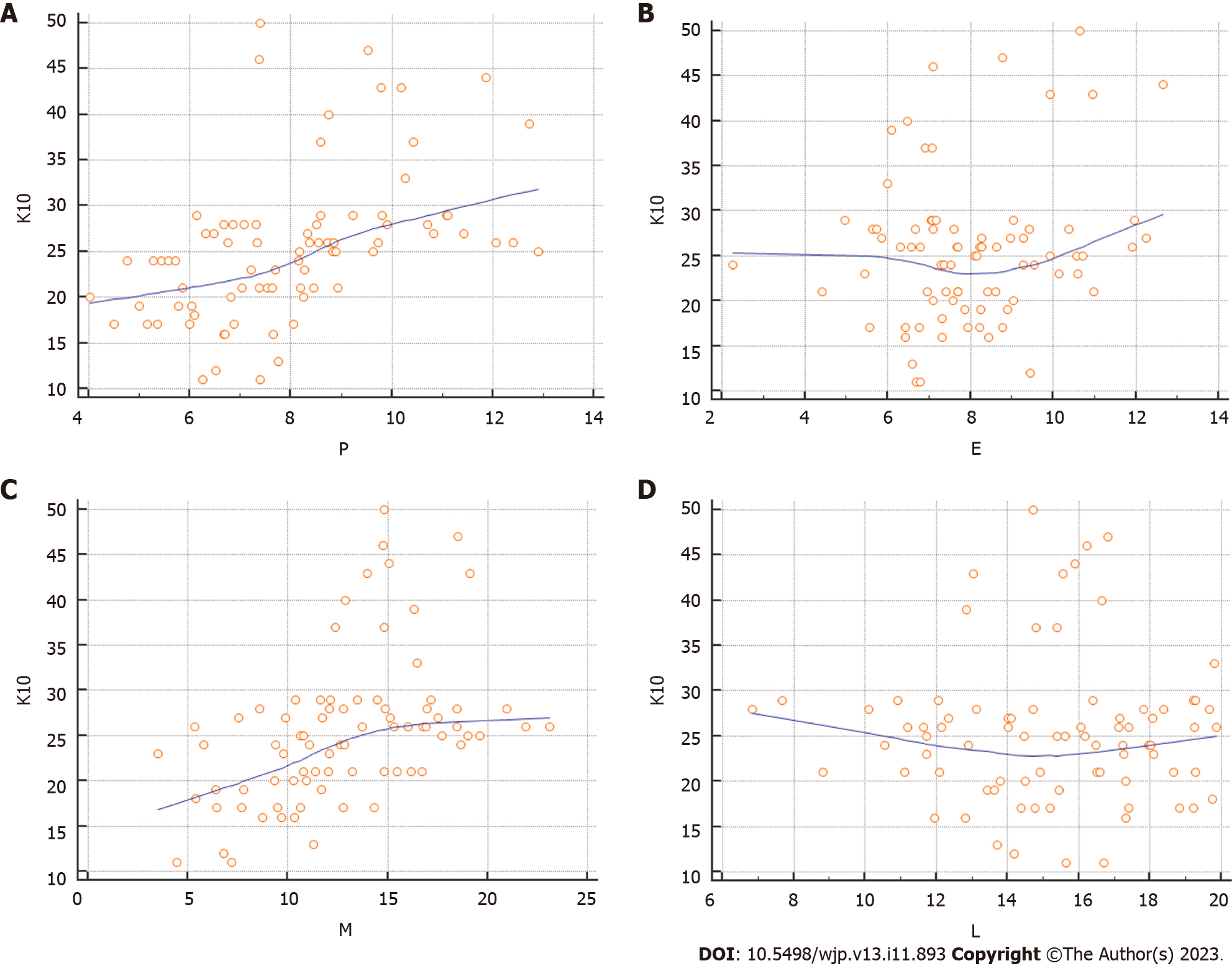
Pearson's analysis showed that the K10 score was positively correlated with the scores of the P-subscale, N-subscale, and other two subscales (P < 0.05). In contrast, the K10 score had no significant correlation with the scores of E-subscale and L-subscale (P > 0.05) (Table 4 and Figure 1).
| Item | r value | P value |
| P | 0.477 | < 0.001 |
| E | 0.201 | 0.074 |
| N | 0.454 | < 0.001 |
| L | -0.013 | 0.904 |
Alcohol dependence, namely alcohol addiction, is a chronic and recurrent encephalopathy characterized by compulsive, intense cravings for alcohol, loss of control over alcohol use, and negative emotions and physical discomfort that will emerge when alcohol is unavailable. Harmful use of alcohol is one of the largest risk factors for death, disease, and disability[15-18]. The Global Report on Alcohol Use and Health WHO in 2018 states that[3] in 2016, the global prevalence of alcohol use disorders (AUD) among people aged 15 and above reached 5.1%, and the prevalence of alcohol dependence in this age group reached 2.6%. The harmful use of alcohol caused approximately 3 million deaths worldwide in the same year, accounting for 5.6% of all deaths. According to the 2019 survey of Chinese groups of mental illnesses, the 12-month prevalence of AUD in China was 1.8%, and the lifetime prevalence was 4.4%, of which the 12-month prevalence of alcohol dependence was 0.7% and the lifetime prevalence was 1.3%[19]. Alcohol abuse can cause damage to multiple systems, including the nervous system, cardiovascular system, digestive system, respiratory system, etc. Long-term drinking can also cause the breakdown of family relationships, disturb normal work, and cause accidents after drinking that seriously endanger personal and social safety. Exploring the mechanisms of addiction in alcohol dependence, actively seeking new treatment options, and encouraging patients with alcohol dependent to receive professional treatment for alcohol withdrawal would be essential methods to reduce the harm due to alcohol abuse[20].
Addictive substances such as alcohol can activate the brain's reward system, and the reward hypothesis is a widely accepted neurobiological hypothesis of addiction[21]. The central nervous system can produce a rewarding effect on natural rewards, such as food, sex, etc., thereby maintaining the continuity of the species. Almost all addictive substances can stimulate the brain's reward circuit, making it faster and more intense than natural rewards, resulting in intense pleasure in the individual. Positron emission tomography studies have shown that drunken doses of alcohol can promote the release of dopamine and opioid peptides from the brain to the ventral striatum, and rapid and high amounts of dopamine in the midbrain limbic system are associated with the subjective feeling of "hi," which is the rewarding effect[22]. Individuals associate alcohol use with positive rewards, which is positive reinforcement. The neurotransmitters and neuromodulators involved in alcohol reward include not only dopamine but also the opioid peptides, γ-aminobutyric acid, glutamic acid, serotonin, acetylcholine, and endocannabinoids acting on the ventral tegmental area or nucleus accumbens[23,24].
Patients with alcohol addiction are given to addictive substances, which greatly affect their mental health and personality characteristics. Jung[25] used the California Personality Questionnaire to implement the longitudinal measurement on adolescents who initially did not have drinking problems. Comparing boys who later developed drinking problems with the control group without similar issues, it was found that male alcohol addicts exhibited more rebellion and extroversion than others before they started drinking. While among female subjects, heavy drinkers showed more pessimism, introversion, and dependence as adolescents than light drinkers[25]. Cloninger et al[26] followed 431 subjects longitudinally for 16 years using a Three-dimensional Personality Questionnaire, which played an important role in clarifying the relationship between personality characteristics and alcohol abuse[26]. Cloninger et al[26] evaluated the participants' personality characteristics at 11 by behavioral assessment; Participants were then assessed for alcohol addiction at 27. The results showed that high sensation seeking and low harm avoidance were risk traits for alcohol addiction and that participants with these two traits in childhood were 20 times more likely to experience alcohol addiction in adulthood than those without these two traits. The thesis of De la Rosa-Cáceres et al[27] in 2022 noted that medium-to-high-risk personality characteristics in participants correlated with the diagnostic criteria for alcohol addiction[27]. Labouvie and McGee[28] conducted longitudinal studies of subjects aged 12 to 21 years, reaffirming that personality predicts alcohol and substance abuse and that adolescents with early substance abuse scored with a low degree on fulfillment, cognitive structure, and avoidance of harm but scored with a high degree on relationships, independence, depression, impulsivity, and play[28]. Gmel et al[29] analyzed the questionnaire results in 5125 young men and pointed out that high impulsivity and sensory seeking are also risk factors for alcohol addiction.
The results of this study showed that the K10 score of patients with alcohol addiction was positively correlated with the scores of two subscales such as P-subscale and N-subscale (r = 0.477, 0.518, 0.454, P < 0.05), patients with higher K10 scores had higher scores in P-subscale and N-subscale. The personality characteristics of those with high scores on the P-subscale presented social withdrawal trait, with strange behaviors like apathy and poor control. Herein, they responded strongly to various stimuli. People with high scores on N-subscale often have overt nervousness, fear, terror, irritability, restlessness, anxiety, depression, and panic; when these people encounter abnormal psychosocial problems, they are more difficult to extricate themselves than ordinary people and will be worried, depressed, and hesitant.
Alcohol-dependent patients with higher scores on P-subscale on the eysenck personality questionnaire (EPQ) score tend to have personality characteristics such as isolation, isolation, bizarre behavior, apathy, poor control, and therefore strong responses to various stimuli[30-32]. The reason may be that individuals who are withdrawn and introverted when they encounter unsatisfactory and unpleasant life events in daily life are neither good at alleviating their bad emotions by confiding inward troubles and depression to others, nor can they self-regulate through healthy and effective coping, so it is easier to apply the simple, direct but self-anesthesia method of drinking because of “Quench a thirst with poison” to avoid the bad reality, which is the so-called "Drinking can relieve thousands of worries." It might achieve certain results in the short term. Although individuals can also realize that long-term drinking could harm their bodies due to poor self-control. When they reencounter unsolvable life problems, they will involuntarily apply the so-called "effective" method as before, that is, "drinking." Consequently, they enter a vicious circle, increasing the possibility of "alcohol dependence." In addition, if the individual's sensitivity is high and it is easy to have a strong rational response to various stimuli, especially in the trivial matters of life, then it will be easier for them to all day long bothered by life dissatisfaction, which increases the possibility of "drinking" as a bad coping style. Moreover, patients with alcohol dependence due to long-term drinking habits will undergo certain changes. They will no longer care about their family, life, and work, having no emotional expression on their families and friends, just immersed in the "anesthesia" of alcohol all day. The general social interaction cannot interest them. Naturally, they will be like outliers and indifferent to anything. The patient will also have "foraging" behavior; that is, the patient will take all possible ways to find alcohol and meet the purpose of their drinking in the process of the patient's "foraging" in juncture to the conventional way. It may also include unconventional methods such as "Proposing a toast," "Cheating others to drink," "Gifting alcohol as private bribery," "Stealing alcohol," etc. these strange behaviors usually do not appear in normal individuals and represent the embodiment of "Weird behaviors."
Patients with alcohol dependence with higher N scores in the EPQ questionnaire had more obvious personality characteristics such as nervousness, fear, fear, irritability, restlessness, anxiety, depression, panic, anxiety, anxiety, depression, depression, and indecision[32-34]. The reasons could be that when individuals with tense, fearful, and indecisive personalities deal with life events, they are prone to cause difficulties in dealing with them correctly and in time due to their personality defects. When faced with choices in life, they will also miss the best time of choice and decision because of their indecision, so they might often fall into self-regret and afterward complain. Although individuals have also tried to apply healthy coping methods for solving problems, because of their nervous, fearful, and hesitant personality. These healthy coping styles are difficult to succeed in, so individuals will easily apply bad coping methods such as "drinking" to solve their adverse reactions. For individuals, "drinking" can not only solve the current dilemma in the short term, but more importantly, it does not require too many personality characteristics and self-effort and successfully "avoids" the "negative influence" and "self-denial" brought about by their bad personality characteristics in the process of solving problems. Therefore, when individuals encounter similar life difficulties and other adverse conditions in the future, they will naturally use "drinking" to deal with it, which lays a certain foundation and conditions for forming later "alcohol dependence." In addition, if the individual's attitude to life is more negative, the individual is prone to be dissatisfied and disappointed with life and the future and will adopt more avoidance coping methods to deal with bad emotions and produce a sense of self "abandoned" by the world. At this time, the individual cannot solve his inner depression and resentment, and it is easy to use “drinking” to escape reality and self-anesthetize, and over time, the possibility of "alcohol dependence" will increase.
However, there were some limitations worth highlighting in this study. Firstly, the size of the sample studied was relatively smaller. And secondly, because this research was a single-center-based study, thus, the selection of these patients was limited to the scope of the patients in this hospital, which may have brought some biases in the interpretation of the results. Therefore, it appears necessary to design a larger, multi-center and multiethnic sample to further analyze and probe into the results of this study with an in-depth and sophisticated method.
Correlation analysis of the correlation between alcohol addiction behavior and personality traits, exploring the causes of this behavior pattern, and thus serving the clinical treatment of alcohol addiction.
Alcohol addiction behavior is related to the personality characteristics of patients, and psychotropic (P) and neuroticism (N) dimensions of personality can positively induce alcohol addiction behavior.
There is a positive correlation between the scores of mental health assessment and the scores of P and N dimensions in personality assessment.
Using the K10 Mental Health Assessment Scale, analyze the mental health status of alcohol addiction patients and its correlation with personality.
Based on existing research on the mental health of alcohol addiction, explore the correlation between the occurrence of alcohol addiction behavior and self-personality.
Based on the existing talent gap of clinical research nurses, the training scheme of nurses should be scientifically customized to promote the development of clinical trials.
Alcohol addiction, as a serious pattern of physical and mental harm, can lead to irreversible harm in severe cases. However, research reports on the causes of alcohol addiction behavior are not yet clear.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Psychiatry
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Eskandari F, Iran; Irrera N, Italy S-Editor: Fan JR L-Editor: A P-Editor: Wu RR
| 1. | Wang SC, Chen YC, Chen SJ, Lee CH, Cheng CM. Alcohol Addiction, Gut Microbiota, and Alcoholism Treatment: A Review. Int J Mol Sci. 2020;21. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 33] [Cited by in RCA: 74] [Article Influence: 14.8] [Reference Citation Analysis (0)] |
| 2. | Choi HY, Seo JS, Lee SK. [Assessment and Treatment of Alcohol Withdrawal Syndrome]. Korean J Gastroenterol. 2020;76:71-77. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 3. | Peacock A, Leung J, Larney S, Colledge S, Hickman M, Rehm J, Giovino GA, West R, Hall W, Griffiths P, Ali R, Gowing L, Marsden J, Ferrari AJ, Grebely J, Farrell M, Degenhardt L. Global statistics on alcohol, tobacco and illicit drug use: 2017 status report. Addiction. 2018;113:1905-1926. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 624] [Cited by in RCA: 660] [Article Influence: 94.3] [Reference Citation Analysis (0)] |
| 4. | Leonardi F. The Definition of Health: Towards New Perspectives. Int J Health Serv. 2018;48:735-748. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 60] [Article Influence: 8.6] [Reference Citation Analysis (0)] |
| 5. | Cuijpers P, Auerbach RP, Benjet C, Bruffaerts R, Ebert D, Karyotaki E, Kessler RC. The World Health Organization World Mental Health International College Student initiative: An overview. Int J Methods Psychiatr Res. 2019;28:e1761. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 57] [Cited by in RCA: 91] [Article Influence: 15.2] [Reference Citation Analysis (0)] |
| 6. | Kwako LE, Patterson J, Salloum IM, Trim RS. Alcohol Use Disorder and Co-Occurring Mental Health Conditions. Alcohol Res. 2019;40. [PubMed] |
| 7. | Mariotti EC, Waugh MH, McClain CM, Beevers LG, Clemence AJ, Lewis KC, Miller R, Mulay AL, Ridenour JM, Huprich SK, Pitman SR, Meehan KB. Assessing Self-Definition and Relatedness in Level of Personality Functioning. J Pers Disord. 2021;35:857-880. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 8. | Kovács I, Gál BI, Horváth Z, Demeter I, Rózsa S, Janka Z, Urbán R, Demetrovics Z, Andó B. Externalizing personality characteristics define clinically relevant subgroups of alcohol use disorder. PLoS One. 2022;17:e0265577. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 9. | Helle AC, Watts AL, Trull TJ, Sher KJ. Alcohol Use Disorder and Antisocial and Borderline Personality Disorders. Alcohol Res. 2019;40. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 14] [Cited by in RCA: 28] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 10. | Newton-Howes G, Foulds J. Personality Disorder and Alcohol Use Disorder: An Overview. Psychopathology. 2018;51:130-136. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 8] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 11. | Newton-Howes G, Foulds J. Personality disorder and treatment outcome in alcohol use disorder. Curr Opin Psychiatry. 2018;31:50-56. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 9] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 12. | Cohen SM, Alexander RS, Holt SR. The Spectrum of Alcohol Use: Epidemiology, Diagnosis, and Treatment. Med Clin North Am. 2022;106:43-60. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 19] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 13. | Mei XX, Wu XN, Wang HY, Wu JY, Wang XQ, Ye ZJ. Heterogeneity in Psychological Resilience and Mental Health among Newly Graduated Nursing Students: A Latent Profile and Generalized Additive Model Analysis. Psychol Res Behav Manag. 2022;15:597-606. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 13] [Cited by in RCA: 3] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 14. | Andrews G, Slade T. Interpreting scores on the Kessler Psychological Distress Scale (K10). Aust N Z J Public Health. 2001;25:494-497. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1181] [Cited by in RCA: 1311] [Article Influence: 54.6] [Reference Citation Analysis (0)] |
| 15. | García-Torres F, Castillo-Mayén R. Differences in Eysenck's Personality Dimensions between a Group of Breast Cancer Survivors and the General Population. Int J Environ Res Public Health. 2019;16. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 5] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 16. | Fuchs FD, Fuchs SC. The Effect of Alcohol on Blood Pressure and Hypertension. Curr Hypertens Rep. 2021;23:42. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 66] [Article Influence: 16.5] [Reference Citation Analysis (0)] |
| 17. | Becker U, Tolstrup J. [Alcohol-related morbidity and mortality]. Ugeskr Laeger. 2021;183. [PubMed] |
| 18. | Kposowa AJ, Breault K. Disability Status, Unemployment, and Alcohol-Related Liver Disease (ALD) Mortality: A Large Sample Individual Level Longitudinal Study. Subst Abuse Rehabil. 2021;12:81-88. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 9] [Reference Citation Analysis (0)] |
| 19. | Huang Y, Wang Y, Wang H, Liu Z, Yu X, Yan J, Yu Y, Kou C, Xu X, Lu J, Wang Z, He S, Xu Y, He Y, Li T, Guo W, Tian H, Xu G, Ma Y, Wang L, Yan Y, Wang B, Xiao S, Zhou L, Li L, Tan L, Zhang T, Ma C, Li Q, Ding H, Geng H, Jia F, Shi J, Wang S, Zhang N, Du X, Wu Y. Prevalence of mental disorders in China: a cross-sectional epidemiological study. Lancet Psychiatry. 2019;6:211-224. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1590] [Cited by in RCA: 1358] [Article Influence: 226.3] [Reference Citation Analysis (0)] |
| 20. | Di Sarno R, Brigida A, Caprio GG, Ciardiello D, Dallio M, Sangineto M, Fagoonee S, Abenavoli L, Luzza F, Gravina AG, De Magistris L, Federico A, Loguercio C. Critical review on the use and abuse of alcohol. When the dose makes the difference. Minerva Med. 2020;111:344-353. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 3] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 21. | Kramer J, Dick DM, King A, Ray LA, Sher KJ, Vena A, Vendruscolo LF, Acion L. Mechanisms of Alcohol Addiction: Bridging Human and Animal Studies. Alcohol Alcohol. 2020;55:603-607. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 18] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 22. | Radoman M, Crane NA, Gorka SM, Weafer J, Langenecker SA, de Wit H, Phan KL. Striatal activation to monetary reward is associated with alcohol reward sensitivity. Neuropsychopharmacology. 2021;46:343-350. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 19] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 23. | Bauer MR, McVey MM, Boehm SL 2nd. Drinking history dependent functionality of the dorsolateral striatum on gating alcohol and quinine-adulterated alcohol front-loading and binge drinking. Alcohol. 2022;105:43-51. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 6] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 24. | Molina-Martínez LM, Juárez J. Differential expression of μ-opioid receptors in the nucleus accumbens, amygdala and VTA depends on liking for alcohol, chronic alcohol intake and estradiol treatment. Behav Brain Res. 2020;378:112255. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 10] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 25. | Jung J. Psychology of alcohol and other drugs: A research perspective. Sage Publications: London, 2001: 603. |
| 26. | Cloninger CR, Sigvardsson S, Bohman M. Childhood personality predicts alcohol abuse in young adults. Alcohol Clin Exp Res. 1988;12:494-505. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 469] [Cited by in RCA: 399] [Article Influence: 10.8] [Reference Citation Analysis (0)] |
| 27. | De la Rosa-Cáceres A, Narvaez-Camargo M, Blanc-Molina A, Romero-Pérez N, Dacosta-Sánchez D, González-Ponce BM, Parrado-González A, Torres-Rosado L, Mancheño-Velasco C, Lozano-Rojas ÓM. Bridge Nodes between Personality Traits and Alcohol-Use Disorder Criteria: The Relevance of Externalizing Traits of Risk Taking, Callousness, and Irresponsibility. J Clin Med. 2022;11. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 28. | Labouvie EW, McGee CR. Relation of personality to alcohol and drug use in adolescence. J Consult Clin Psychol. 1986;54:289-293. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 94] [Cited by in RCA: 88] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 29. | Gmel G, Marmet S, Studer J, Wicki M. Are Changes in Personality Traits and Alcohol Use Associated? A Cohort Study Among Young Swiss Men. Front Psychiatry. 2020;11:591003. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 11] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 30. | La Grange L, Jones TD, Erb L, Reyes E. Alcohol consumption: biochemical and personality correlates in a college student population. Addict Behav. 1995;20:93-103. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 46] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 31. | Drummond DC, Phillips TS. Alcohol urges in alcohol-dependent drinkers: further validation of the Alcohol Urge Questionnaire in an untreated community clinical population. Addiction. 2002;97:1465-1472. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 49] [Cited by in RCA: 53] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 32. | Dash GF, Slutske WS, Martin NG, Statham DJ, Agrawal A, Lynskey MT. Big Five personality traits and alcohol, nicotine, cannabis, and gambling disorder comorbidity. Psychol Addict Behav. 2019;33:420-429. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 68] [Article Influence: 11.3] [Reference Citation Analysis (0)] |
| 33. | Martin KP, Benca-Bachman CE, Palmer RHC. Risk for alcohol use/misuse among entering college students: The role of personality and stress. Addict Behav Rep. 2021;13:100330. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 6] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 34. | Dean SF, Fede SJ, Diazgranados N, Momenan R. Addiction neurocircuitry and negative affect: A role for neuroticism in understanding amygdala connectivity and alcohol use disorder. Neurosci Lett. 2020;722:134773. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 11] [Article Influence: 2.2] [Reference Citation Analysis (0)] |