Published online Nov 19, 2023. doi: 10.5498/wjp.v13.i11.838
Peer-review started: July 18, 2023
First decision: August 4, 2023
Revised: August 28, 2023
Accepted: September 22, 2023
Article in press: September 22, 2023
Published online: November 19, 2023
Processing time: 122 Days and 0.6 Hours
The background of this study was analgesia in natural delivery. The combined spinal-epidural anesthesia has obvious analgesic effect on the parturients in natural labor, and combined spinal-epidural anesthesia has been widely used in anesthesia for various diseases.
To study the effects of combined spinal-epidural anesthesia on anxiety, labor analgesia, and motor blocks in parturients during natural delivery.
A total of 120 women who gave birth at Changning District Maternal and Child Health Hospital between December 2021 to December 2022 were included; a random number table approach was employed to divide the women into a control group and a joint group, with each group consisting of 60 women. The control group was given epidural anesthesia, while the joint group was given combined spinal-epidural anesthesia. The visual analog scale (VAS) was used to evaluate the degree of maternal pain. Comparisons were made between the two groups’ conditions of childbirth and the duration of labor. Apgar scores were used to evaluate the status of the newborns at birth; Self-rating Anxiety Scale (SAS) and General Self-Efficacy Scale (GSES) scores, umbilical artery blood gas analysis indices and stress indices were compared between the two groups; and the frequencies of motor block and postpartum complications were analyzed.
In comparison to the control group, in the joint group, the VAS scores for the first, second, and third stages of labor were lower (P < 0.05). The rates of conversion to cesarean section and postpartum blood loss in the joint group were lower than those in the control group (P < 0.05). No significant differences were observed in the Apgar score, the duration of the first stage of labor, or the total duration of labor between the two groups (P > 0.05). The second and third stages of labor in the joint group were shorter than those in the control group (P < 0.05). When compared to the control group, the postpartum SAS score of the joint group was lower, while the GSES score was greater (P < 0.05). Between the control group and the joint group, the differences observed in pH, arterial carbon dioxide partial pressure, arterial oxygen partial pressure, or arterial hydrogen ion concentration were not significant (P > 0.05). Nitric oxide, cortisol, and adrenaline levels were lower in the joint group than in the control group (P < 0.05). There were no substantial differences in Bromage grade or rate of complications between the two groups (P > 0.05).
For parturients during natural delivery, combined spinal-epidural anesthesia can reduce anxiety, provide labor analgesia, shorten labor time, and reduce postoperative stress levels but did not result in a motor block.
Core Tip: The pain of parturients in natural delivery is serious. Spinal anesthesia and epidural analgesia are widely used, but the analgesia effect is not good, and the nerve block effect of lumbar epidural anesthesia is better. The objective of this study was to compare the effects of combined epidural and lumbar anesthesia on labor analgesia and movement block.
- Citation: Cai L, Jiang JJ, Wang TT, Cao S. Effects of combined spinal-epidural anesthesia on anxiety, labor analgesia and motor blocks in women during natural delivery. World J Psychiatry 2023; 13(11): 838-847
- URL: https://www.wjgnet.com/2220-3206/full/v13/i11/838.htm
- DOI: https://dx.doi.org/10.5498/wjp.v13.i11.838
Labor is a complicated physiological and psychological process, and labor pain is a subjective feeling of the human body that lacks objective indicators. Currently, combined spinal-epidural anesthesia is widely used to relieve the pain of parturients during natural childbirth, which has less impact on contraction pain than other analgesic methods[1]. However, various research studies have shown that epidural anesthesia alone has a poor analgesic effect in parturients. Based on this fact, intraspinal anesthesia can be used to effectively enhance the analgesic effect[2]. Combined spinal-epidural anesthesia has a more rapid analgesic effect and better nerve block efficacy than epidural anesthesia[3]. Childbirth is a natural biological process as well as a complex period involving volatile emotions. Related research suggests that the intensity of labor pain is associated with individual pain thresholds as well as many other influencing factors[4]. Poor mood around the time of delivery can directly reduce a woman’s pain threshold, making her more sensitive to pain. In addition, severe pain during childbirth increases the fear, tension, and anxiety of parturients, forming a vicious cycle, which keeps them in a state of high stress and has adverse effects on delivery[5,6]. Therefore, reducing negative emotions in patients during childbirth is crucial for smooth deliveries. Based on the above, this study explored the effects of combined spinal-epidural anesthesia on anxiety levels, labor analgesia and motor blocks in women during natural delivery, with the view of selecting a better method of labor anesthesia and promoting smooth deliveries.
A total of 120 women who gave birth in Changning District Maternal and Child Health Hospital from December 2021 to December 2022 without signs of cesarean section were studied. By employing a random number table, they were separated into control and joint groups, each of which included 60 women. Table 1 demonstrates that no significant differences were present in the general data between the two groups (P > 0.05).
| Classification | Joint group (n = 60) | Control group (n = 60) | T value | P value |
| Age (yr) | 26.79 ± 3.18 | 27.03 ± 3.21 | 0.411 | 0.682 |
| Gestational age (wk) | 39.35 ± 0.24 | 39.28 ± 0.21 | 1.700 | 0.092 |
| Number of pregnancies | 1.84 ± 0.17 | 1.89 ± 0.21 | 1.433 | 0.154 |
| Parity | 1.59 ± 0.12 | 1.61 ± 0.15 | 0.806 | 0.422 |
| Estimated newborn body mass (kg) | 3.58 ± 0.53 | 3.65 ± 0.49 | 0.751 | 0.454 |
The inclusion criteria were as follows: (1) Women aged 23-34 years old; (2) Women with American Society of Anesthesiologists physical status grade I; (3) Primiparas; and (4) Women with a gestational age of 36-40 wk. The exclusion criteria were as follows: (1) Patients with a medical history of hematological diseases; (2) Patients with long-term use of anticoagulants or drugs that affect coagulation function; (3) Patients with contraindications for combined spinal-epidural anesthesia; and (4) Patients with pregnancy-induced hypertension and other obstetric complications.
The joint group was given combined spinal-epidural anesthesia. When the uterine orifice was opened to 2 cm, puncture was performed in the lumbar L2-3 space. After successful subarachnoid puncture, cerebrospinal fluid flow was continuous. A subarachnoid injection of 1 μg sufentanil (Yichang Humanwell Pharmaceutical Co., LTD., batch number: SFDA approval number H20054171) and 0.2 mg ropivacaine (Jiangsu Hengri Pharmaceutical Co., LTD., batch number: SFDA approval number H20060137) was given. Epidural catheterization was performed. After successful catheterization, 3 mL of 1.5% lidocaine (Shanghai Pujin Linzhou Pharmaceutical Co., LTD., batch number: SFDA approval number H41022244) was given as the experimental dose. After confirming correct placement in the epidural space, the epidural catheter was fixed with adhesive tape. Sufentanil (0.5 μg/mL) and +0.1% ropivacaine was combined with an epidural infusion pump. The first dose of the infusion pump was set at 10 mL, the patient-controlled analgesia dose was set at 9 mL, and the patient-controlled lockout time was 20 min. The infusion pump was turned on 1 h after anesthesia. Epidural anesthesia was given to the control group with the same specific method as that in the joint group.
The observation targets were as follows: (1) Labor pain: The degree of labor pain in each stage of labor was evaluated by employing the visual analog scale (VAS)[7]. The scores ranged from 0-10, and the severity of the pain increased with the score; (2) Childbirth-related conditions: The two groups’ rates of conversion to cesarean section, forceps-assisted delivery, and postpartum blood loss and newborn Apgar scores were compared. The Apgar score was utilized to evaluate the status of newborns[8]. The Apgar scores ranged from 0-10, with a score of 10 representing healthy newborns and a score < 7 indicating asphyxia; (3) Labor duration: Between the two groups, the first, second, and third stages of labor as well as the overall duration of labor were compared; (4) Emotion: The Self-Rating Anxiety Scale (SAS) was employed to evaluate the anxiety levels of patients[9]. The scores ranged from 20-80, and a score of > 50 indicated anxiety. The General Self-Efficacy Scale (GSES) was utilized to evaluate the patients’ self-efficacy[10], with scores ranging between 10 and 40 points. Higher scores suggested a stronger sense of self-efficacy; (5) Blood gas analysis indices of the umbilical artery: After delivery, 1 mL of umbilical artery blood was extracted with a heparin anticoagulant syringe. Then, the pH, partial pressure of oxygen (PO2), partial pressure of carbon dioxide (PCO2) and arterial hydrogen ion concentration (BE) of the maternal umbilical artery were detected by an ABL77 automatic blood gas analyzer (Radiometer, Denmark); (6) Stress index: Before and 3 d after delivery, 3 mL of maternal venous blood was drawn and subjected to centrifugation, serum cortisol (Cor) and adrenaline (ADR) levels were measured by ELISA, and serum nitric oxide (NO) levels were measured by the NO enzyme method; (7) Degree of motor block: The modified Bromage score was employed to evaluate the degree of motor block[11]. Level 0 indicated that there was no motor block, and the lower limbs could be raised; level 1 indicated the inability to lift the thigh; level 2 indicated difficulty in bending the knee; and level 3 indicated difficulty in bending the ankle; and (8) Complications: In both groups, the frequency of postoperative issues such as hypotension, nausea, and vomiting was measured.
SPSS 22.0 software was utilized to process the data. Counting data are reported as percentages, and differences between groups were compared by Fisher’s exact test or the χ2 test. Measurement data are reported as mean ± SD after the normality test, and the differences between groups were compared via t tests. Ranked data were analyzed by Z tests. P < 0.05 indicated a statistically significant difference.
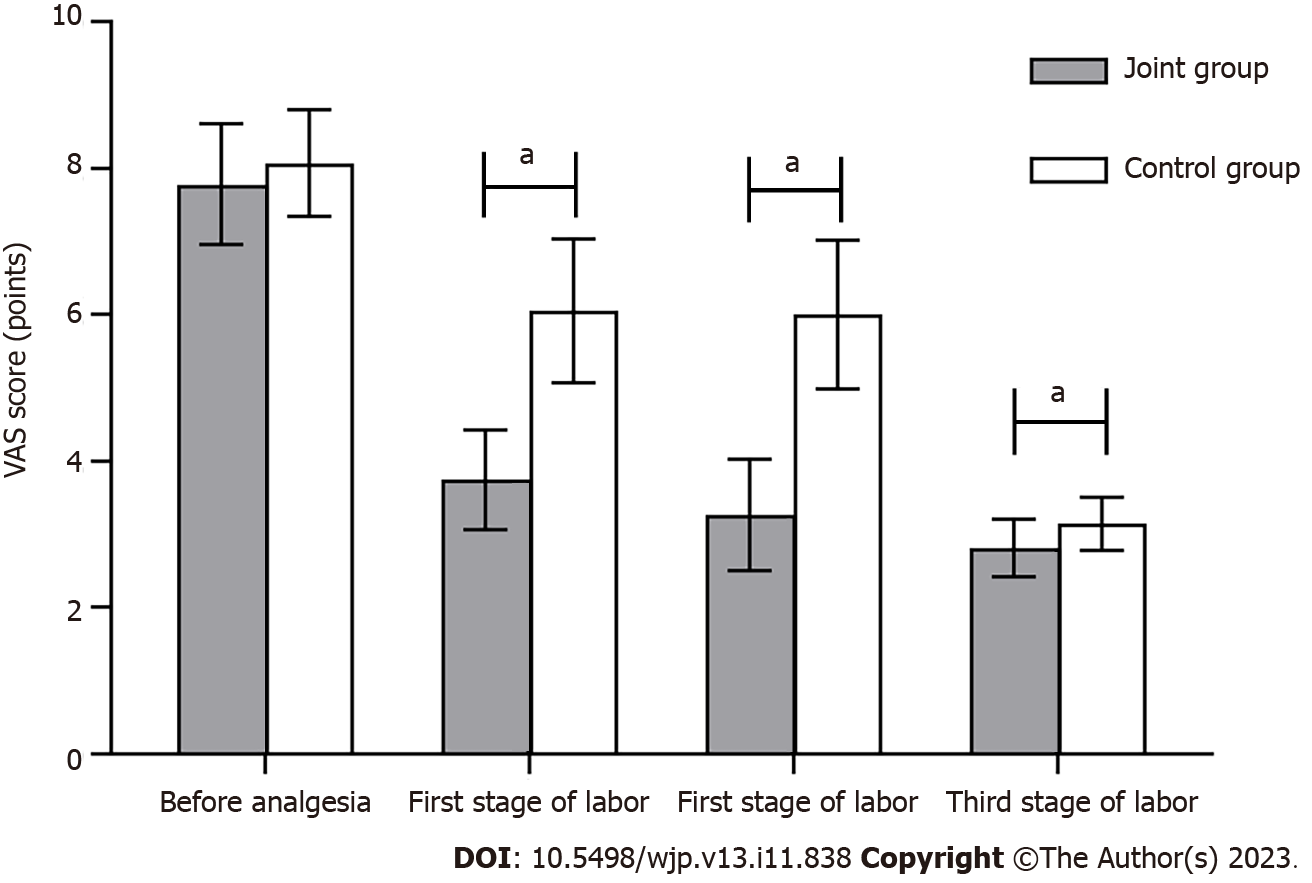
Comparison of labor pain between the two groups: Before anesthesia, no significant difference was observed in the VAS scores of the two groups (P > 0.05). In comparison to the control group, in the joint group, the VAS scores for the first, second, and third stages of labor were lower (P < 0.05) (Figure 1).
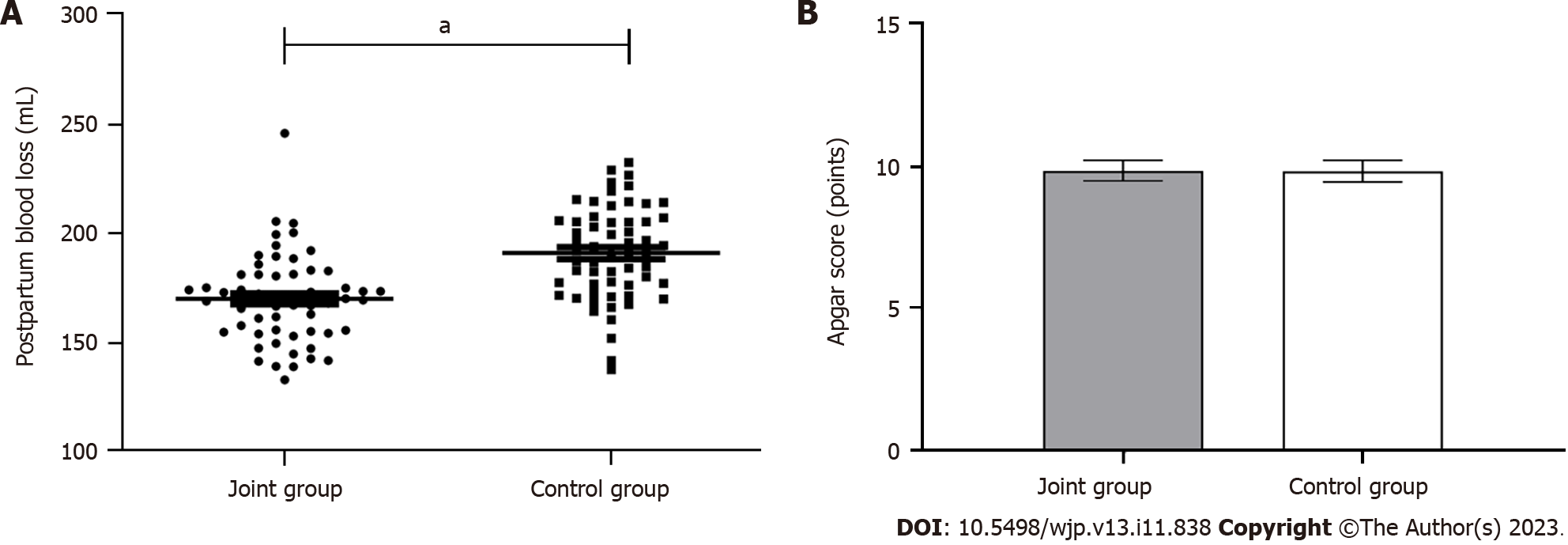
Comparing the childbirth-related conditions between the groups: The rates of conversion to cesarean section and postpartum blood loss were lower in the joint group than in the control group (P < 0.05); no significant differences were observed in the two groups’ Apgar scores (P > 0.05) (Table 2, Figure 2).
| Group | n | Rate of conversion to cesarean section | Rate of forceps-assisted delivery |
| Joint group | 60 | 0.00 (0) | 3.33 (2) |
| Control group | 60 | 8.33 (5) | 6.67 (4) |
| P value | < 0.05 | > 0.05 |
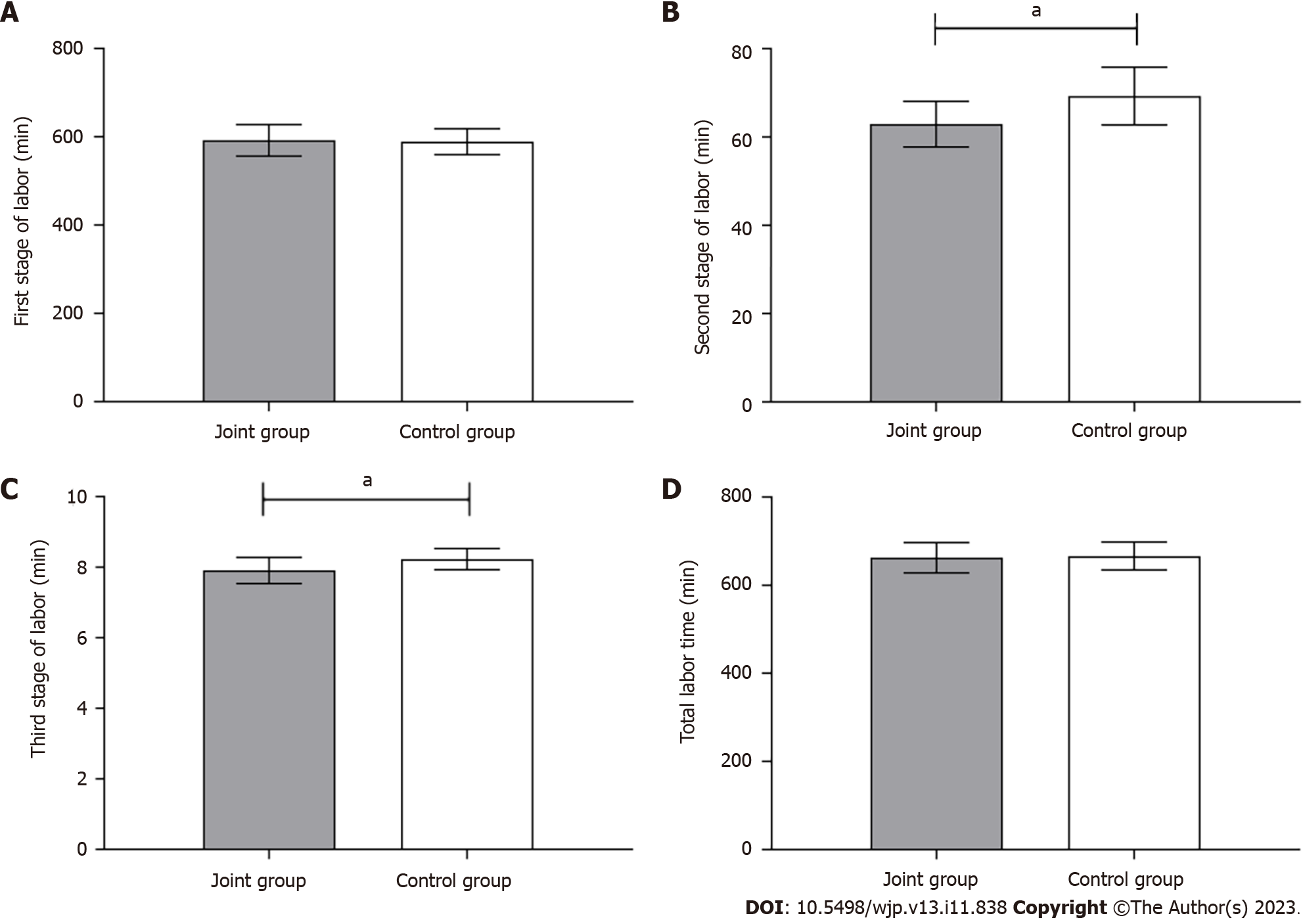
Comparison of labor duration between the two groups: The initial stage of labor and the overall duration of labor did not substantially differ between the two groups (P > 0.05); the joint group experienced slightly shorter second and third stages of labor in comparison to the control group (P < 0.05), as shown in Figure 3.
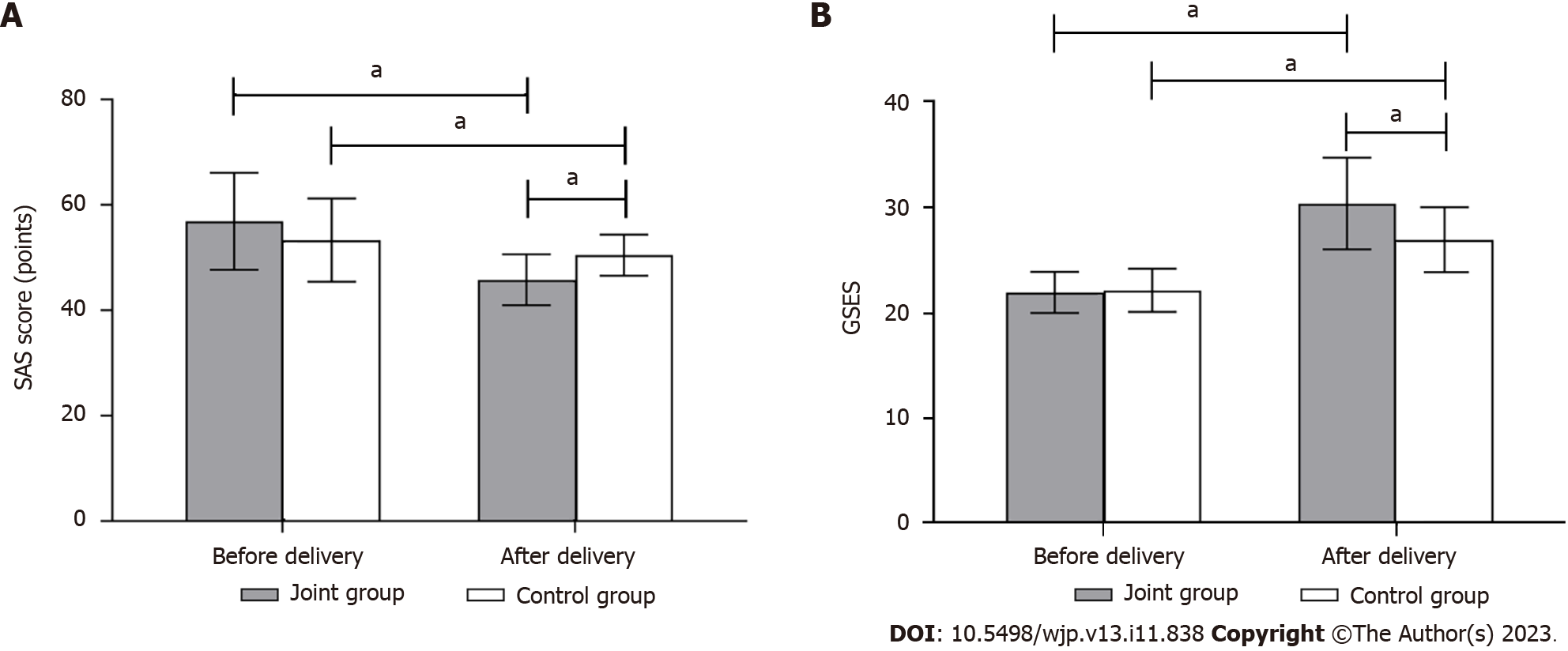
Comparison of anxiety and depression between the two groups: Prenatal SAS and GSES scores did not differ significantly between the groups (P > 0.05). The SAS scores of both groups were lower in the postpartum period than the prenatal period, and the SAS scores of the joint group were lower than those of the control group (P < 0.05). The GSES scores were higher in both groups in the postnatal period compared to the corresponding scores in the prenatal period, with the joint group having higher scores than the control group (P < 0.05) (Figure 4).
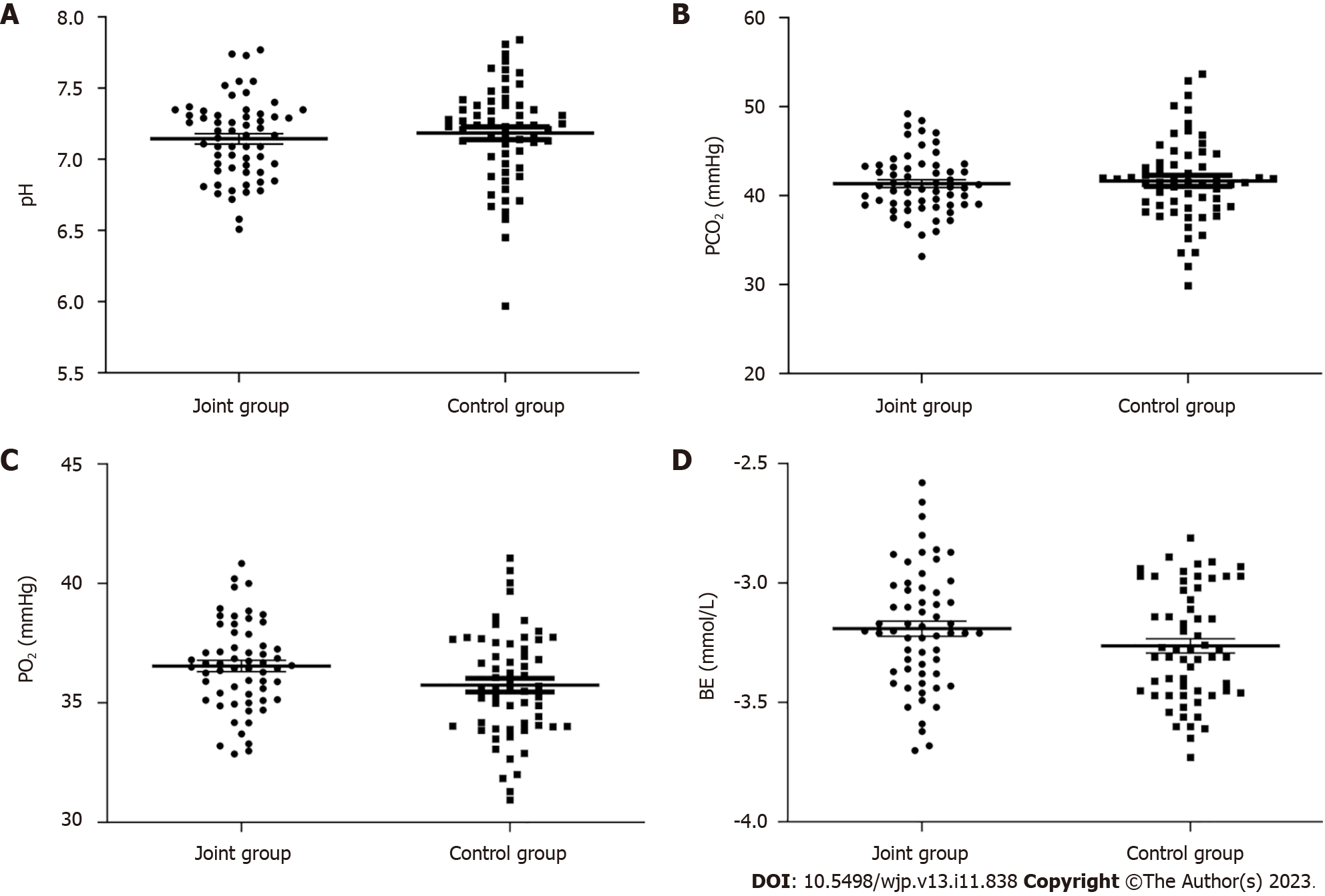
Comparison of blood gas analysis indices of the umbilical artery between the two groups: The changes observed in pH, PCO2, PO2, and BE between the control and joint groups were not significantly different (P > 0.05), as shown in Figure 5.
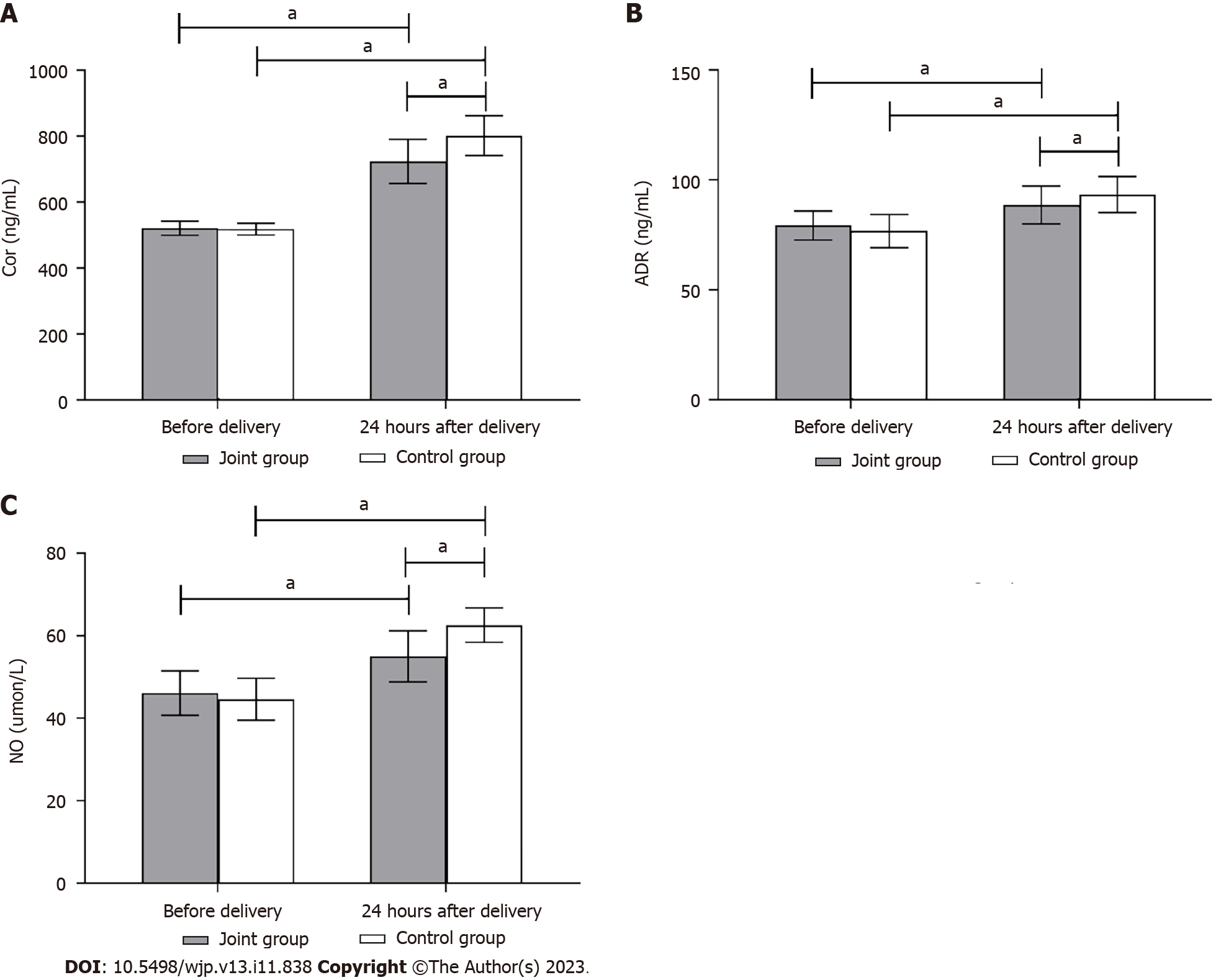
Comparison of stress indices between the two groups: No significant differences were observed in the prenatal Cor, ADR, and NO levels between the groups (P > 0.05). Following delivery, the levels of Cor, ADR, and NO increased in both groups compared to those before delivery. Additionally, the scores in the control group were elevated compared to those in the joint group (P < 0.05) (Figure 6).
Comparison of motor block effects between the two groups: The Bromage grade did not substantially differ between the two groups (P > 0.05) (Table 3). Comparison of complication rates between the two groups. The complication rates between the two groups did not differ significantly (P > 0.05) (Table 4).
| Group | n | Grade 0 | Grade 1 | Grade 2 | Grade 3 |
| Joint group | 60 | 52 | 7 | 1 | 0 |
| Control group | 60 | 46 | 9 | 4 | 1 |
| Z value | 2.277 | ||||
| P value | 0.131 | ||||
| Group | Joint group | Control group | χ2 | P value |
| n | 60 | 60 | ||
| Hypotension | 0 | 1 | ||
| Nausea and vomiting | 2 | 1 | ||
| Pruritus | 0 | 1 | ||
| Deceleration of fetal heart rate | 0 | 1 | ||
| Total incidence | 3.33 (2) | 6.67 (4) | 0.702 | 0.402 |
Labor pain refers to the pain caused by strong uterine contractions, pelvic floor muscle expansion, and contraction of uterine tissue. Relevant studies have pointed out that intense and sustained pain during natural labor can directly lead to the occurrence of postpartum depression[12]. Hence, it is important to explore a better method of pain relief during labor. Specifically, optimal pain relief during labor can make pain relief easy to control, which is conducive to the smooth progress of labor. Continuous epidural block has been widely used internationally, with exact analgesic effects, lasting effects, little influence on circulation, and no side effects or complications of general anesthesia, such as changes in consciousness, hypoxia, hypercapnia, or aspiration[13]. Previous studies have shown that combined spinal-epidural anesthesia can reduce the pain of women during natural childbirth[14]. Intravertebral analgesia is currently considered by most scholars to be the most effective labor analgesia method. This method can effectively reduce pain during uterine contraction, reduce the stress response during labor, and contribute to the stability of the internal environment of the parturient and the smooth recovery of the body in the postpartum period[15]. The current study revealed that the VAS scores during the first, second, and third stages of labor were lower in the joint group than in the control group, suggesting that combined spinal-epidural anesthesia could alleviate labor pain for women during natural labor, which was consistent with the above research results. However, it should be noted that although combined anesthesia reduces the degree of labor pain, the analgesic drugs used will still have varying degrees of impact on the mother and child, and analgesic drug use during labor can easily hide excessive contractions and can also lead to contraction inhibition. Hence, it is necessary to choose the appropriate delivery method according to the patient’s condition. Moreover, the outcomes of the present research demonstrated lower rates of conversion to cesarean section and postpartum blood loss in the joint group than in the control group, suggesting that combined anesthesia can promote the smooth progress of natural delivery. Because pain during labor can be alleviated, a series of physiological changes caused by labor pain can be relieved, and maternal fear and tension can be alleviated, which is conducive to the smooth progress of labor and indirectly reduces the rate of cesarean section[16].
Childbirth is a complex physiological and psychological process that is affected by mental, psychological, and environmental factors. Fear-tension-pain syndrome is common in parturient women. Due to a lack of understanding of the delivery process, an abnormal pregnancy history, existing mental and psychological disorders, and endocrine changes during childbirth, parturient women, especially primiparous parturient women, experience negative emotions such as fear, tension, anxiety, and depression, which are different from those in nonpregnancy[17]. According to literature reports, approximately 5% of the normal population has anxiety, and the incidence of prenatal anxiety can reach 8%-16.5%[18]. Childbirth self-efficacy refers to the belief or confidence that one can apply some techniques to manage and reduce pain during labor. According to some studies, the threshold of childbirth pain for women with poor mental health is reduced, and the psychological advantages generated by the participation of parturients in analgesia can eliminate the tension and anxiety caused by childbirth, increase their self-confidence, reduce the rates of dystocia and childbirth complications, and create favorable conditions for ensuring the safety of the mother and child during childbirth[19]. In the present study, it was found that the SAS score was decreased and the GSES score was increased in the postpartum period in the joint group, implying that the combined spinal-epidural anesthesia improved the sense of self-efficacy and reduced the degree of anxiety. Therefore, medical workers need consider parturients are a whole, determine their mental state in a timely manner, choose safe, rapid, effective, and appropriate analgesic methods, and implement individualized treatment for parturients to achieve ideal labor analgesia. For parturients with low anxiety and depression levels, psychotherapy can be used to comfort them by addressing doubts, relieving tension and loneliness and enhancing maternal confidence in giving birth. In addition, the durations of the second and third stages of labor in the joint group were slightly decreased compared to those in the control group, indicating that combined spinal-epidural anesthesia could reduce the duration of labor in women with natural delivery, which may be related to the reduction of labor pain and anxiety by combined anesthesia.
Umbilical cord blood gas is affected not only by the process of labor but also by placental function, umbilical cord factors, and maternal blood gas status. According to relevant reports, abnormal blood gas indices of cord blood are related to maternal emotions in addition to labor pain[20]. During childbirth, appropriate tension and anxiety can improve a mother’s ability to adapt to the environment, which can be accompanied by activation of the sympathetic nervous system. Increased catecholamines acting on α receptors constrict peripheral blood vessels, increase the heart rate, redistribute cardiac output, and ensure the supply of vital organs such as the heart and brain, making up for the shortage of the maternal supply and improving the fetus’s tolerance to hypoxia; however, excessive anxiety can affect umbilical cord blood hemodynamics, leading to fetal hypoxia[21,22]. Since the above research results showed that combined anesthesia can help to reduce patients’ anxiety, the author believes that this anesthesia method can improve umbilical artery blood gas indices. In the present research, no significant differences were seen in pH, PO2, PCO2, and BE between the joint group and the control group, indicating that combined spinal-epidural anesthesia and single epidural anesthesia had little impact on the umbilical artery blood gas indices in parturients who gave birth naturally, which is inconsistent with the relevant research results[23]. This might be due to the study’s small sample size; thus, the sample size should be increased for further analysis.
Experiencing high levels of tension, anxiety, and intense pain during labor can trigger a cascade of neuroendocrine reactions within the body. This can lead to elevated levels of catecholamines and adrenal corticosteroids in the bloodstream, resulting in increased oxygen consumption, heightened cardiac burden, uterine vasoconstriction, decreased blood flow, fetal distress, and potential uterine inertia. Pain can cause hyperventilation in parturients, which has adverse effects on their cardiovascular, endocrine, and psychological conditions and can increase the incidence of uterine inertia and uncoordinated uterine contraction. The current study demonstrated that Cor, ADR, and NO levels were comparatively lower in the joint group than in the control group, implying that the combination of lumbar and epidural anesthesia could reduce the postoperative stress level of the body, which was largely associated with the reduction in postoperative pain and improvement in negative emotions of the women in the combined anesthesia group. Related research demonstrates that the degree of motor block can be reduced by giving combined spinal-epidural anesthesia to women during natural childbirth[24]. Nevertheless, no significant differences were found in the Bromage grade or complication rate between the two groups, indicating that combined anesthesia and epidural block alone had little effect on motor block. The reason for this remains unknown, so further analysis should be conducted.
Combined spinal-epidural anesthesia for women during natural labor can reduce anxiety, ease pain, shorten the labor time, and reduce the postoperative stress level of the body, but did not result in a motor block. This study shows that, in addition to improving the method of anesthesia, prenatal education should also be carried out. By fully providing knowledge on labor and labor pain, prenatal education can help parturients understand how to judge labor pain, which is conducive to improving continuous muscle tension and enhancing the analgesic effect for painless labor.
The background of this study is that the rate of natural childbirth is increasing, the rate of cesarean section is decreasing, and anesthesia and analgesia in natural childbirth are getting more and more clinical attention. The significance of this study is to explore new methods of anesthesia and analgesia in natural childbirth.
The main topic of this study is anesthesia and analgesia for natural parturients, and it is necessary to explore more effective anesthesia and analgesia methods for natural parturients. The significance of this study is to confirm the effectiveness of combined spinal-epidural anesthesia in the analgesia of women in natural childbirth, and encourage clinical teams to continue to explore more effective analgesia methods for women in natural childbirth.
The purpose of this study was to compare the analgesic effect of different analgesic methods on women in natural childbirth, and to observe the analgesic advantage of combined spinal-epidural anesthesia on women in natural childbirth. It was found that the combined spinal-epidural anesthesia can effectively improve the labor pain, shorten the labor process, relieve the bad mood and reduce the postoperative stress of the parturients. To provide a new reference for the analgesia of parturients in clinical natural labor in the future.
In this study, the pregnant women were divided into two groups by randomized control method, and the general data, pain degree, newborn condition, self-efficacy, umbilical artery blood gas analysis index, stress index and movement blocker complications of the two groups were statistically analyzed by independent sample t test, paired sample t test and χ2 test.
Combined spinal-epidural anesthesia has a more significant effect on the improvement of labor pain in women with natural delivery, with significant improvements in labor pain, cesarean section rate, blood loss, adverse emotions, stress reaction and other aspects, providing a new analgesic method for women with natural delivery. Further large-scale studies are needed to verify the effectiveness of this method.
The bad mood of natural childbirth women can affect the pain threshold of women, making them more sensitive to pain, and pain strengthens the bad mood of women, affecting childbirth. Therefore, we should pay attention to the influence of analgesic methods on maternal bad mood. Combined spinal-epidural anesthesia has good analgesic effect on parturients in natural labor.
Natural childbirth women should not only consider the outcome of childbirth, but also pay attention to the personal state of the mother during childbirth. Future research aims to further explore the effects of analgesia on maternal adverse mood and stress response.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Psychiatry
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Papadakis S, Greece; Vaccaro M, Italy S-Editor: Wang JJ L-Editor: A P-Editor: Wu RR
| 1. | Buran G, Aksu H. Effect of Hypnobirthing Training on Fear, Pain, Satisfaction Related to Birth, and Birth Outcomes: A Randomized Controlled Trial. Clin Nurs Res. 2022;31:918-930. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 2. | Wu L, Zhao H, Zhang Z, Huang M, Wu S, Fang C, Wang R, Li S, Yi W, Zhou A. Combined spinal-epidural anesthesia with acupoint injection for labor anesthesia reduces IL-1β/IL-10 ratio in maternal peripheral blood, umbilical cord blood and improves the labor outcomes: A prospective randomized controlled trial. Clin Immunol. 2022;236:108935. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 6] [Reference Citation Analysis (0)] |
| 3. | Borrelli S, Evans K, Pallotti P, Evans C, Eldridge J, Spiby H. Mixed-methods systematic review: Childbearing women's views, experiences, and decision-making related to epidural analgesia in labour. J Adv Nurs. 2020;76:3273-3292. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 14] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 4. | Torkiyan H, Sedigh Mobarakabadi S, Heshmat R, Khajavi A, Ozgoli G. The effect of GB21 acupressure on pain intensity in the first stage of labor in primiparous women: A randomized controlled trial. Complement Ther Med. 2021;58:102683. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 10] [Reference Citation Analysis (0)] |
| 5. | Yan ZQ, Song BJ, Lv XJ, Zhu LJ, Liu ZY, Li G. [Observation on the Application of Epidural Block Analgesia in Obese Maternal Delivery through Dural Puncture]. Shandong Med J. 2021;61:48-51. [DOI] [Full Text] |
| 6. | Zhu Y, Xiong Y, Li HY, Chen Y, Lu KZ, Ning JL. [A randomized controlled study on the analgesic effect of ropivacaine infiltration anesthesia on perineal pain after natural childbirth under intraspinal analgesia]. J Third Military Med University. 2019;41:691-695. [DOI] [Full Text] |
| 7. | Langley GB, Sheppeard H. The visual analogue scale: its use in pain measurement. Rheumatol Int. 1985;5:145-148. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 278] [Cited by in RCA: 368] [Article Influence: 9.2] [Reference Citation Analysis (0)] |
| 8. | De Bernardo G, De Santis R, Giordano M, Sordino D, Buonocore G, Perrone S. [Predict respiratory distress syndrome by umbilical cord blood gas analysis in newborns with reassuring Apgar score]. Ital J Pediatr. 2020;46:20. [RCA] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 17] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 9. | Olatunji BO, Deacon BJ, Abramowitz JS, Tolin DF. Dimensionality of somatic complaints: factor structure and psychometric properties of the Self-Rating Anxiety Scale. J Anxiety Disord. 2006;20:543-561. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 107] [Cited by in RCA: 123] [Article Influence: 6.5] [Reference Citation Analysis (0)] |
| 10. | Luszczynska A, Scholz U, Schwarzer R. The general self-efficacy scale: multicultural validation studies. J Psychol. 2005;139:439-457. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 772] [Cited by in RCA: 821] [Article Influence: 43.2] [Reference Citation Analysis (0)] |
| 11. | Shi YN, Su JT, Mao HM. [Application of multimodal analgesia based on the concept of accelerated rehabilitation surgery in cesarean section]. Shandong Medical J. 2019;59:90-92. [DOI] [Full Text] |
| 12. | Tilahun S, Giru BW, Snshaw W, Moges N. Magnitude and associated factors of suicidal behavior among postpartum mothers attending public health centers of Addis Ababa, Ethiopia. BMC Psychiatry. 2022;22:465. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 13. | Blajic I, Zagar T, Semrl N, Umek N, Lucovnik M, Stopar Pintaric T. Analgesic efficacy of remifentanil patient-controlled analgesia versus combined spinal-epidural technique in multiparous women during labour. Ginekol Pol. 2021;92:797-803. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 12] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 14. | Sun X, Zhou Q, Zhou M, Cao R, Chen Z, Tang S, Huang S. The Effect of Epidural Nalbuphine Combined With Ropivacaine on Epidural Analgesia During Labor: A Multicenter, Randomized, Double-blind, Controlled Study. Clin J Pain. 2021;37:437-442. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 6] [Reference Citation Analysis (0)] |
| 15. | Wei CN, Chang XY, Dong JH, Zhou QH. Remifentanil for Carboprost-Induced Adverse Reactions During Cesarean Delivery Under Combined Spinal-Epidural Anesthesia. Front Pharmacol. 2020;11:980. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 16. | Wang Y, Xu M. Comparison of ropivacaine combined with sufentanil for epidural anesthesia and spinal-epidural anesthesia in labor analgesia. BMC Anesthesiol. 2020;20:1. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 19] [Cited by in RCA: 35] [Article Influence: 7.0] [Reference Citation Analysis (0)] |
| 17. | Gannon M, Short V, Becker M, Parikh S, McGuigan K, Hand D, Keith S, Abatemarco D. Doula engagement and maternal opioid use disorder (OUD): Experiences of women in OUD recovery during the perinatal period. Midwifery. 2022;106:103243. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 9] [Reference Citation Analysis (0)] |
| 18. | Ying H, Hong Z, Lin XF. [Survey on the Cognition and Needs of Pregnant Women for Labor Analgesia in a Third Class Comprehensive Hospital]. China Health Education. 2020;36:86-88. |
| 19. | Savory NA, Hannigan B, John RM, Sanders J, Garay SM. Prevalence and predictors of poor mental health among pregnant women in Wales using a cross-sectional survey. Midwifery. 2021;103:103103. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 9] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 20. | Yin XY, Bian XX, Liu AM. [The diagnostic significance of combined detection of fetal ultrasound hemodynamics and umbilical cord blood gas analysis for neonatal asphyxia]. Chongqing Med. 2019;48:1600-1602. [DOI] [Full Text] |
| 21. | Liu C, Liu Q, Li HY, Chen Q. [The application of combined spinal epidural anesthesia in cesarean section of PIH parturients and its effect on hemodynamics and hemorheology]. Shandong Medical J. 2019;59:79-81. [DOI] [Full Text] |
| 22. | Chen Y, Liu W, Gong X, Cheng Q. Comparison of Effects of General Anesthesia and Combined Spinal/Epidural Anesthesia for Cesarean Delivery on Umbilical Cord Blood Gas Values: A Double-Blind, Randomized, Controlled Study. Med Sci Monit. 2019;25:5272-5279. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 20] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 23. | Zhou JS, Luo D. [Determination of the 50%effective dose of sequential method for determining methoxamine with continued pumping and infusion to prevent hypotension during combined spinal epidural anesthesia]. J Chongqing Medical University. 2021;46:223-226. [DOI] [Full Text] |
| 24. | Chen XL, Liang YG, Weng DG. [The Application Research of Combined Spinal-Epidural Anesthesia and Continuous Epidural Anesthesia for Labor Analgesia of Normal Parturient]. J Fujian Medical University. 2021;55:343-345. [DOI] [Full Text] |