Published online Jan 19, 2023. doi: 10.5498/wjp.v13.i1.15
Peer-review started: August 24, 2022
First decision: October 21, 2022
Revised: October 25, 2022
Accepted: November 30, 2022
Article in press: November 30, 2022
Published online: January 19, 2023
Processing time: 141 Days and 15.1 Hours
Recommendations for psychotherapy have evolved over the years, with cognitive behavioral therapy (CBT) taking precedence since its inception within clinical guidelines in the United Kingdom and United States. The use of CBT for severe mental illness is now more common globally.
To investigate the feasibility and acceptability of a culturally adapted, CBT-based, third-wave therapy manual using the Comprehend, Cope, and Connect approach with individuals from a diverse population presenting to primary and secondary healthcare services.
A pilot study was used to assess the feasibility and acceptability of the manualised intervention. Outcome measures were evaluated at baseline, post-intervention and 12 wk-follow up. 32 participants with mental health conditions aged 20-53 years were recruited. Assessments were completed at three time points, using Clinical Outcomes in Routine Evaluation (CORE), Hospital Anxiety and Depression Scale (HADS), Bradford Somatic Inventory and World Health Organization Disability Assessment Schedule 2.0 (WHODAS). The Patient Experience Ques-tionnaire was completed post-treatment.
Repeated measures of analysis of variance associated with HADS depression, F (2, 36) = 12.81, P < 0.001, partial η2 = 0.42 and HADS anxiety scores, F (2, 26) = 9.93, P < 0.001, partial η2 = 0.36; CORE total score and WHODAS both showed significant effect F (1.25, 18.72) = 14.98, P < 0.001, partial η2 = 0.5. and F (1.29, 14.18) = 6.73, P < 0.001, partial η2 = 0.38 respectively.
These results indicate the effectiveness and acceptability of the culturally adapted, CBT-based, third-wave therapy manual intervention among minoritized groups with moderate effect sizes. Satisfaction levels and acceptability were highly rated. The viability and cost-effectiveness of this approach should be explored further to support universal implementation across healthcare systems.
Core Tip: This study explores the relevance of a cultural cognitive behavioral therapy manual to manage mental health and wellbeing in primary and secondary care settings in the United Kingdom. Specificity and adaptability are key to demonstrating the relevance as well as the cost-effectiveness of mental health management approaches. Results show the effectiveness of the proposed intervention, with high levels of acceptability and participant satisfaction.
- Citation: Phiri P, Clarke I, Baxter L, Zeng YT, Shi JQ, Tang XY, Rathod S, Soomro MG, Delanerolle G, Naeem F. Evaluation of a culturally adapted cognitive behavior therapy-based, third-wave therapy manual. World J Psychiatry 2023; 13(1): 15-35
- URL: https://www.wjgnet.com/2220-3206/full/v13/i1/15.htm
- DOI: https://dx.doi.org/10.5498/wjp.v13.i1.15
Cognitive behavioral therapy (CBT) was developed by Beck et al[1] with the aim of reducing cognitive biases and dysfunctional behaviors in order to alleviate symptoms of psychopathology. CBT was developed in an ethnocentric environment however, recent research has enabled adaptations to be made to CBT in various aspects[2]. Changes to treatment goals, assigned homework, and types of coping mechanisms taught are some of the adjustments that have been made to this intervention to make it more applicable to different psychological conditions[3,4]. Currently, adaptations to CBT to ensure relevancy and accessibility to ethnic minority groups are also being implemented such as introducing family involvement, use of appropriate language terms, and developed understanding of psychopathology from a culture viewpoint[5,6]. Social constructs and determinants play a vital role in the psychotherapies developed, driven by varying cultural factors of those within developed country-based populations. This is often identified with dysfunctions such as inadequate health policies, transparency in healthcare access and accountability mechanisms, and democratic deficits of global governance systems due to persistent global political determinants of health that have a negative impact. As such, the inclination for cultural factors and sociological constructs to influence the delivery of evidence-based therapeutics would be a logical consensus.
Few CBT adaptations employ surface changes to the intervention, which involve general and practical adaptations, such as increased awareness of cultural issues, aligning therapy with public service messages, or translating materials[7-9]. Most studies used cognitive behavioral strategies and included a variety of ethnic minority samples[6,10-15]. These studies also found that culture-specific values related to interpersonal relationships, family, and spirituality could play a significant role when providing therapy to culturally diverse patients[6,12,13,16]. Specifically, treatments that carefully accommodated cultural values resulted in improved outcomes, especially when adaptions ensured that therapy was problem-focused and direct, supports arguments that culturally diverse individuals may struggle with open-ended and non-directive therapy[17-20].
The implementation of Improving Access to Psychological Therapies (IAPT) initiatives within the United Kingdom increased the development and delivery of psychology treatments for depression and anxiety to be jointly provided with primary care services[21]. IAPT services operate through a 5-stage model, which enable adequate adjustments to be made to ensure beneficial treatment outcomes[22]. Minority ethnic groups face difficulties with accessing mental health services and it is common for them to have unfavorable experiences[23]. Hence, IAPT implemented the BAME Service User Positive Practice Guide which outlines core elements needed in IAPT service provision in order for ethnic minority groups to receive equitable treatments and outcomes[24]. One change currently active within IAPT services is ability to self-referral, removing to obstacle of organizational discrimination for many groups[24]. This has seen an increase in recovery rates from 43.8% to 50% among Black and Asian populations between Quarter 4 2015/16 and Quarter 1 2021/22 data[25]. This being said, there is still a huge gap in culturally-accommodating interventions within IAPT service provision.
Interestingly, National Health Service (NHS) Digital reported that the service users of IAPT were primarily Caucasian patients (78.2%) while only 16.4% were from ethnic minority background[26]. This may indicate a lack of acceptability of IAPT treatments in their current form and it could be argued that the accessibility of IAPT services to diverse populations may still be limited. Although these initial findings have highlighted the need for adaptation of therapy for patients from diverse ethnic minority backgrounds, concerns around the adaptation of CBT for every ethnic group have been raised from a pragmatic perspective, due to limitations within scalability and sustainability[27]. In the past few years, there has been a huge shift towards personalised mental health care services, highlighting the need to consider the individual and any interplaying factors when implementing services[27,28]. Culture is an entity which has significant effects on the psychopathology and help-seeking behavious of individuals hence should be accounted for when implementing interventions[6]. It is common for interventions and assessment tools to be translated to endless languages[29,30], and adaptations in accordance to culture should be accepted on the same terms. This being said, the translatability of interventions to other languages raises socio-economical issues for healthcare systems and policymakers alike yet, not considering translatability could exacerbate health inequality concerns and the same goes for adaptations to cultures. For these reasons, the authors developed a therapy manual that uses a generic third-wave approach, taking into consideration the above factors as well as sensitive forms of therapy in recognition of cultural bias in psychological therapies[15,23,31-35]. CBT and Comprehend, Cope, and Connect (CCC) interventions can be adapted to treat various psychological illnesses but there is also scope for these treatments to be adjusted in accordance to culture[36]. CCC has been chosen due to its universal applicability to levels of processing as it does not require specific adaptation for different ethnicities[37], and indeed the current study included individuals from African, Caribbean, South Asian, and Chinese backgrounds among others. Many Western therapies were developed through an individualistic approach but CCC lends itself to involving family and significant others within the intervention, incorporating aspects of mindfulness, spirituality, and faith. Third-wave approaches to CBT moved the focus towards interpersonal impacts on psychopathology and treatments such as relationships, values, acceptance, and beliefs[38]. Acceptance of different faiths and beliefs are equally important to ensure clinically optimal, yet culturally sensitive diagnostic and treatment approaches are rendered to all patients. Previous literature reports on the increased efficacy of third wave treatments, such as mindfulness-based cognitive therapy or acceptance and commitment therapy, compared with standard interventions across all populations and this paper aims to add to current understandings[39-41].
CCC is a third-wave cognitive behavioral approach based on a collaboratively arrived at, emotion focused, strengths based and trauma informed formulation that leads naturally to the identification of vicious cycles. It is evident at this stage that breaking the cycles is necessary, and skills such as mindfulness, arousal management and emotion management, as well as behavior change are identified and encouraged[42]. The development of the culturally adapted CBT based third-wave CCC manual offers high replicability of this study and the potential for a larger sample and introduction of a control group for comparison. High feasibility for further research using this manualized therapy is also indicated by the good recovery and retention rates, as well as positive patient experience questionnaire (PEQ) scores, which significantly indicated high levels of satisfaction and experience.
An uncontrolled pilot study was conducted to explore the feasibility, acceptability, and effectiveness of culturally adapted, a third-wave based cognitive behavioral approach using CCC as a therapeutic intervention for patients with common mental disorders and emotional problems. The study was conducted within IAPT and secondary adult mental health services at an NHS Foundation Trust in the United Kingdom as CCC training has been implemented across both services.
The recruitment of participants was through Community Mental Health Team (CMHT) services and IAPT’s iTalk service at NHS Trust. The study was advertised through posters in CMHT and iTalk services. Recruiting participants for this study was difficult despite inclusion across both IAPT and CMHT services.
Potential participants could also contact the study therapist if they were interested in taking part. All potential participants were screened for eligibility before joining the study to ensure they met the inclusion criteria. Permission to approach potential participants was obtained from the treating clinicians. Participants who agreed to be approached were contacted and provided with an ethically approved participant information sheet. The researcher met participants in person to discuss the study in detail and obtain informed consent if interested in taking part. Participants were given a minimum of 48 h to decide if they would like to participate in the study. All participants who consented were informed that they could withdraw from the study at any time.
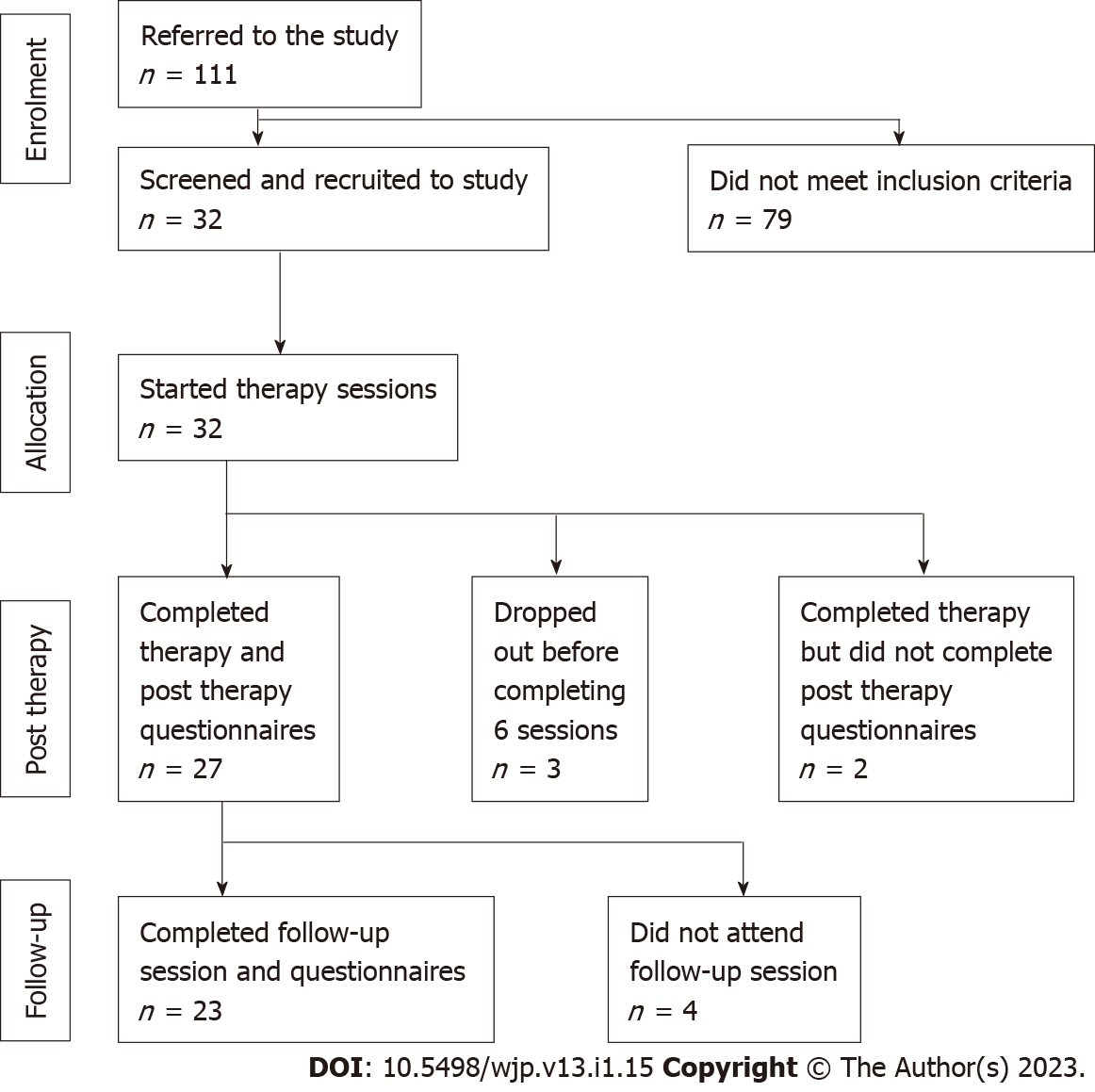
Participants with moderate to severe mental health problems were identified from IAPT services and secondary care services within the NHS Trust. Our target population was adult patients, aged 18 years and above, with moderate to severe mental illness as confirmed by specialist psychiatric services and documented in the electronic health records (F32: Depressive episode; F20: Schizophrenia; F41.1: Generalised anxiety disorder; F40.1: Social phobia; F43.1: Post-traumatic stress disorder; F42: Obsessive-compulsive disorder; F41.8: Mixed depression and anxiety). All patients from ethnic minority backgrounds were included following written informed consent. However, participants with an organic illness or a primary diagnosis of substance misuse and those experiencing acute psychotic symptoms were excluded from the study. Overall, 32 participants met the inclusion criteria and consented to take part in the study (Figure 1).
The study was approved by the Health Research Authority London-Camden & Kings Cross Research Ethics Committee, reference number: 16/LO/1899.
In terms of simultaneous interventions, CMHT patients were provided this intervention alongside standard treatment whilst IAPT patients were offered the adapted intervention. The CCC intervention was first evaluated within Acute Mental Health services[39-41] and developed for delivery in primary care IAPT services for complex cases[43]. Within primary care, the programme consisted of four individual sessions in which the collaborative emotion and trauma-focused formulation is agreed followed by a 12-wk group and skills-based interventions targeting emotion management and behaviour change (Tables 1 and 2). One or two review sessions concluded the programme. The CCC manual was culturally adapted by the authors using the cultural adaptation framework published elsewhere[23]. A full account of the intervention outlining the theory and applicability of CCC is published elsewhere[44]. Although this is aside from the focus of this study, research on acute services and CCC has also been published[43].
| Session no | Activity |
| 1-4 | Listening; introducing the states of mind; introducing mindfulness and/or breathing |
| Collaboratively creating the formulation diagram | |
| Negotiating goals for therapy based on what is needed to break the vicious circles | |
| Sharing the draft compassionate summing up letter and looking forward to what to work on through the group programme | |
| 5-12 | Goals based interventions aimed at breaking the cycles. Mindfulness is the core intervention, and the following are employed as indicated by the formulation |
| Arousal management, including relaxation breathing and lifestyle adjustment to reduce chronic stress | |
| Behavioural activation | |
| Emotion management includes facing, expressing and letting go of emotion self-compassion | |
| Aspects of self; mindfulness managed subpersonality work. Relationship management including assertiveness building a new relationship with the past | |
| Follow-up at 12 wk post-therapy |
| Intervention |
| Mindfulness is the core intervention; it informs the application of the others |
| Arousal management (relaxation breathing etc.) |
| Behavioral activation |
| Facing, expressing and letting go of emotion |
| Self-compassion |
| Positive anger work |
| Aspects of self (mindfulness managed subpersonality work) |
| Relationship management including assertiveness |
| Building a new relationship with the past |
The adaptation facilitated the inclusion of family members and careers to be involved in the therapy; allowed for the somatic conceptualisation of emotional issues and teaching stories Spirituality and religion, where relevant, are integral to all versions of CCC. The manual developed this aspect further to meet the needs of a diverse population. In many ethnic minority cultures, the family is the nucleus within households and communities, so incorporating this core value with ensure more efficacious treatment outcomes. Families are able to provide support within therapy sessions, at home with homework tasks, but also within the wider community promoting positive outcomes for the patient and acceptance of such interventions and services in the wider community[12,14]. Similarly, ethnic minority groups hold various spiritual and religious values which greatly impact understanding of psychopathology and influence help-seeking behaviors[6,45-48]. It is important to understand these elements as they greatly impact values and beliefs, and these are the concepts of wellness explored within therapy[37]. Culturally-adapted CCC used in the current study is an abridged version of standard CCC offered in IAPT therapy at the moment.
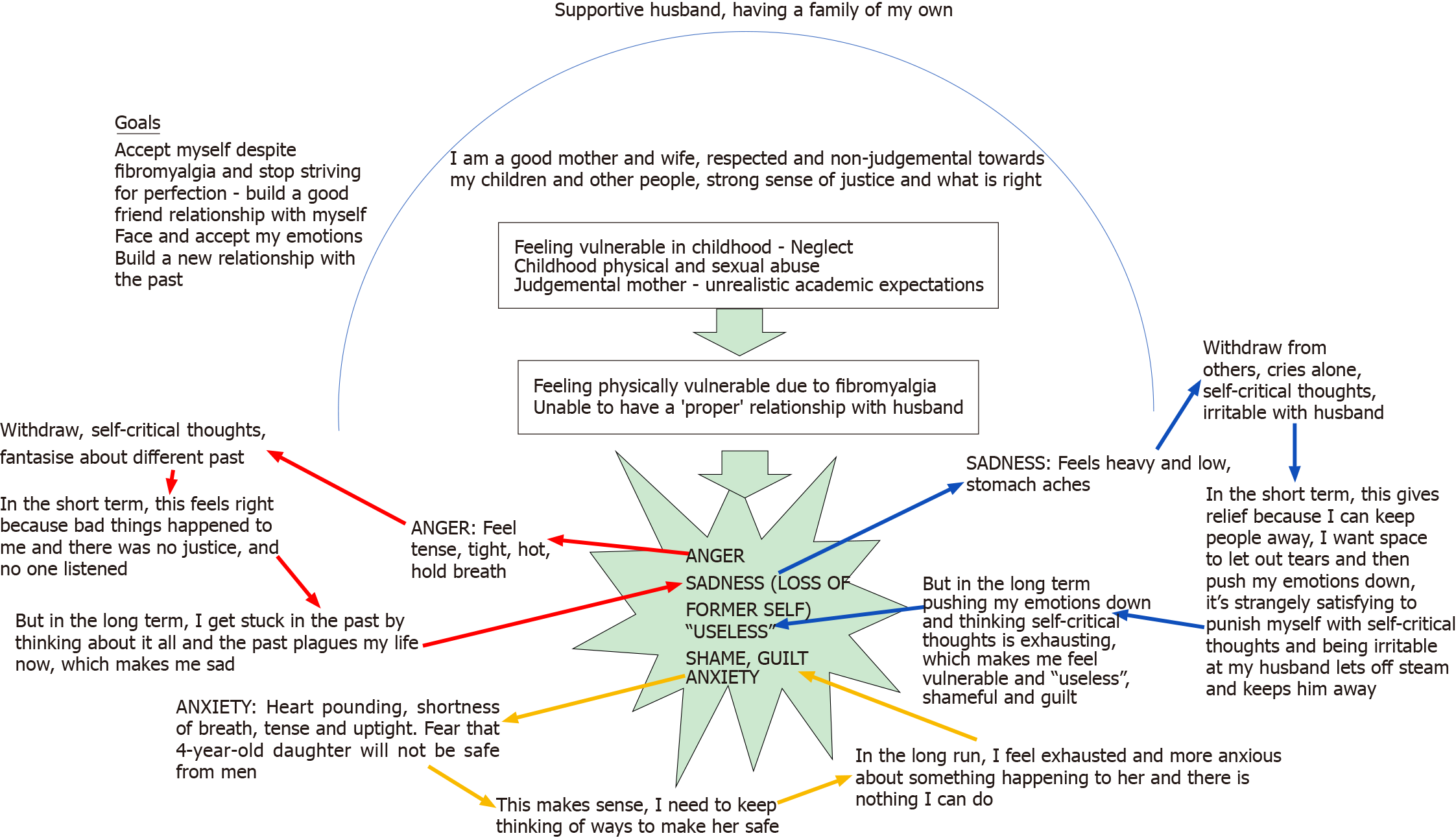
A collaborative and compassionate conceptualisation was completed within the first four sessions (Figure 2). The process starts with open-minded listening and starts with the individual’s internal state and how this has been affected by recent circumstances and past adversities. The impact of the past on the present is explained. Strengths, potential values, faith, or spiritual connections are identified before the vicious cycle, representing the current management of the internal state, are tracked. Finally, a compassionate letter summing up the formulation is shared, and the intervention phase of the therapy comprises new skills to break the vicious cycles.
Refining the manual was a key aim of the study in light of new learning arising from the challenges that emerged during therapy delivery. Adherence to the manual was monitored by an independent experienced clinician, where key cultural issues were identified and addressed accordingly. Adaptations followed the cultural adaptation framework already published elsewhere[6]. Some of the modifications included the following: (1) Allowing somatic conceptualisation of emotional challenges; (2) Managing faith issues where this impacts mental health; (3) Managing the balance between family and system expectations of the individual and their own needs; and (4) Cultural differences in attitudes to assertiveness and anger.
Use of clinical outcome measures varies across primary, secondary and tertiary services. The measures used in this study were not adapted to diverse communities. This is acknowledged in the discussion section under limitations. IAPT participants in the current study also completed standard IAPT measures as this was a service requirement. The study specific outcome measures are listed below:
Socio-demographic measures: A case report form was developed and used to collect this information from the participants. This included the following variables: Date of birth, gender, primary diagnosis, ethnicity, education, and employment history.
Hospital Anxiety and Depression scale: Hospital Anxiety and Depression Scale (HADS) is a 14-item self-report measure of anxiety and depression. It is scored on a 4-point Likert scale. It has good internal consistency[47,48] and good concurrent validity[49].This measure was designed for a nonclinical population but has recently been validated for a mental health population and the reliability estimates have shown that the Cronbach’s alpha for HADS (all items), HADS-Anxiety subscale (HADS-A) and HADS-Depression subscale (HADS-D) was 0.91, 0.90 and 0.80 respectively[45,47].
The Bradford Somatic Inventory: Bradford Somatic Inventory (BSI) is used to measure somatic symptoms. It has 45 items[50]. Scores above 21 indicate depression. It was developed from symptom reports by psychiatric patients in Pakistan and Britain with clinical diagnoses of common mental health problems. The BSI enquires about a wide range of somatic symptoms during the previous month, and if the subject has experienced a particular symptom, whether the symptom has occurred on more or less than 15 d during the month (scoring 2 or 1, respectively).
World Health Organization Disability Assessment Schedule 2.0: World Health Organization (WHO) Disability Assessment Schedule 2.0 (WHODAS) was developed by the WHO to measure disability due to physical and psychological problems and has been used extensively in research[51]. The scale covers 6 domains of functioning, including cognition, mobility, self-care, getting along, life activities, and participation. Responses are on a Likert scale of 0-4.
Clinical outcomes in Routine Evaluation: Clinical outcomes in Routine Evaluation (CORE) is a self-report questionnaire designed to be administered before and after therapy[52]. The participants were asked to respond to 34 questions about how they have been feeling over the last week, using a 5-point scale ranging from ‘not at all’ to ‘most or all of the time’. The 34 items of the measure cover four dimensions: (1) Subjective well-being; (2) Problems/symptoms; (3) Life functioning; and (4) Risk/harm. The responses are designed to be averaged by the practitioner to produce a mean score to indicate the level of current psychological global distress (from ‘healthy’ to ‘severe’).
PEQ: Participant therapy satisfaction will be measured using the post-treatment PEQ, an 11-item self-administrated questionnaire[53]. Items 1-10 ask respondents to indicate whether their needs were met using either a two-point scale (1 being yes and 2 being no) or a five-point scale (ranging from 0 = ‘not satisfied’ to 5 = ‘very satisfied with services’). Item 11 will capture qualitative data with any recommendations for improvement.
Frequency and descriptive commands were used to measure descriptive statistics, and an explore command was utilised to measure the normality of the data, using histograms and the Kolmorogov-Smirnov test. For each questionnaire score, an analysis of variance (ANOVA) and analysis of covariance (ANCOVA) were used. Factors used for the covariates included age, gender, diagnosis, psychiatric medication, living with someone or alone, ethnic group, having higher education or not having a partner or not, duration of mental illness, being under care of a CMHT or IAPT, history of the previous admission, use of additional services and employment status. However, because of the small sample size, these were individually entered into the analysis.
PEQ measured patient satisfaction with the intervention. It had an ordinal structure, with some items having three or more levels and others having only two levels. A correlation was carried out between PEQ and other outcome scales to investigate whether satisfaction with the intervention was related to other outcomes. Kendal’s Tau was calculated where PEQ items had three or more levels, and Sommer’s D was calculated where PEQ items had two levels. The statistical package IBM SPSS v20 was used to analyse the data.
Demographic data was collected and coded between 29th March 2017 and 4th September 2019. A total of 32 participants (n = 27) female were included in the final sample. Nine participants were from Back African, Black Caribbean and Black Other ethnic groups. Thirteen participants were from either Indian, Bangladeshi, Chinese or Other Asian groups. Ten participants were from Other/Mixed groups. Baseline demographic characteristics are detailed in Table 3. It is worth noting that most participants in this study presented with a high proportion of such complexity and history of trauma (Table 4).
| Characteristics | Total sample, (n = 32) |
| Gender (n, %) | |
| Male | 5 (16) |
| Female | 27 (84) |
| Age in years range (mean) | 20-53 (34.8) |
| Ethnicity (n, %) | |
| Black African | 2 (6) |
| Black Caribbean | 4 (12) |
| Black Other | 3 (9) |
| Indian | 7 (21) |
| Bangladeshi | 1 (3) |
| Chinese | 3 (9) |
| Other Asian | 2 (6) |
| Other/mixed | 10 (32) |
| Diagnosis (n, %) | |
| F32: Depressive episode | 12 (38) |
| F20: Schizophrenia | 1 (3) |
| F41.1: Generalised anxiety disorder | 9 (28) |
| F40.1: Social phobia | 2 (6) |
| F43.1: Post traumatic stress disorder | 2 (6) |
| F42: Obsessive compulsive disorder | 2 (6) |
| F41.8: Mixed depression and anxiety | 4 (13) |
| Setting (n, %) | |
| Community Mental Health Team | 6 (19) |
| Improving Access to Psychological Therapies | 26 (81) |
| Therapist delivering intervention (n, %) | |
| 1 | 2 (6) |
| 2 | 19 (60) |
| 3 | 9 (28) |
| 4 | 2 (6) |
| Number of sessions completed (n, %) | |
| 12 (maximum) | 19 (60) |
| 6-11 | 9 (28) |
| Under 6 | 2 (6) |
| Unrecorded | 2 (6) |
| Participant | Earlier life experiences (traumatic context) | Presenting problem and impact of past | Specific CCC coping, strategies in addition to mindfulness |
| 1 | Childhood abuse (by a close family member), age 4 yr, and neglect; judgmental mother - unrealistic academic expectations | Acquiring physical disability (fibromyalgia and chronic pain), triggers sadness, anger, shame and anxiety, and feeling useless | Building a new relationship with the past: Self compassion |
| 2 | Childhood abuse. Domestic violence from partners | Anger and cannot cope when feeling unsupported, let down in the present. Unassertiveness | Building a new relationship with the past: Self-compassion; positive; anger work |
| 3 | Over-looked academically as a girl; sense of injustice. Sexual abuse by older brother told not to tell (approx 7 years old) told mother, who blamed and chastised her for the act | Unacknowledged in current family leading to disproportionate depression and anger | Emotion management; selfcompassion |
| 4 | Punishing and neglectful mother. Anxious childhood | Inability to deal with emotions. Avoidant of relationships | Self-compassion; emotion management |
| 5 | Childhood trauma. Father nearly died in car crash when 9 years old. Family preoccupied with impact on sibling | Obsessional thoughts regarding harm to daughter. Avoidance | Arousal management; aspects of self1; self compassion |
| 6 | Extreme childhood fear engendered by tales of black magic | Post-natal fears for safety of son. High anxiety. Compensates with controlling pre-emptive and perfectionist behaviors | Arousal management; building a new relationship with the past; emotion management |
| 7 | Neglectful and chaotic childhood. Alcoholic father | Avoidance of emotion leading to constant activity and chronic stress. Alcohol | Arousal management; emotion management |
| 8 | Multiple deaths of family members coming close together | Obsessive health anxiety | Arousal management; self-compassion; relationship management2 |
| 9 | Shamed within family as teen for (culturally unacceptable) homosexuality. Physical and emotional abuse by mother. Father left when 3 years old | Envy, anger, relationship and career difficulties. Loneliness copes with perfectionist ideas but behavioral inactivity (fear of failure) | Emotion management; relationship management2 |
| 10 | Sister preferred. Sexual abuse by ex-partner. Experienced racism at work | Low self-esteem. Perfectionism leading to high stress | Positive anger work; aspects of self; relationship management |
| 11 | Childhood trauma - mother left. Sex abuse by a parent at 12 yr. Abusive childhood. Adult trauma - loss of daughter in a road traffic accident. Impact of road traffic accident - reduced memory, increased emotionality and impulse control | Flashbacks. Dissociation. Low self-esteem. Problems with emotions and relationships | Building a new relationship with the past; emotion management; relationship management2 |
| 12 | Childhood trauma - loving family, experienced war conflict while in Turkey during Kurdish and Turkish conflict - witnessed village members being tortured by soldiers. ‘Reported seeing ‘Jinns’, dead bodies and evil spirits’ - hallucinations? Adult trauma - illegal immigrant for 14 yr - experienced extreme anxiety and feeling under attack from others | Panic, hypervigilance, avoidance of crowds and exercise | Arousal management; emotion management |
| 13 | Mental, physical and sexual abuse | Avoidance of emotion. Avoidance of intimacy | Building a new relationship with the past; relationship management2; emotion management; aspects of self1 |
| 14 | Childhood sexual abuse by a parent between 5 to 12 yr. Experienced 13 yr of mental and physical abuse from husband | Emotionally overwhelmed. Withdrawal and unmotivated, or dysregulated anger | Arousal management; relationship management; self-compassion |
| 15 | Emotionally abusing and criticising childhood | Dissociation. Emotional overwhelm and relationship difficulties | Positive anger work; emotion management;self-compassion |
| 16 | Migration age 19 yr of age; hostile in-laws. Major health difficulties severely impact marriage | Suicidal and self-harm. Low mood | Arousal management; relationship management; self compassion2 |
| 17 | Unhappy childhood; migration distress. Breast cancer | Obsessive anger at neighbours leading to conflict | Arousal management positive anger work; emotion management |
| 18 | Diagnosed with Autism. Early childhood developmental problems | Social avoidance | Arousal management; behavioral activation; relationship management2 |
| 19 | Ran away from home age 11 yr. ‘Kicked out’ of family home at the age of 19 yr. Loss of young sibling and felt excluded | Suicidal. Avoidant of emotion | Building a new relationship with the past; self compassion; emotion management |
| 20 | Long exploitative and abusive marriage plus racial bullying at work | Stress, chronic hypertension. Relationship difficulties | Arousal management; emotion management; positive anger work; aspects of self1 |
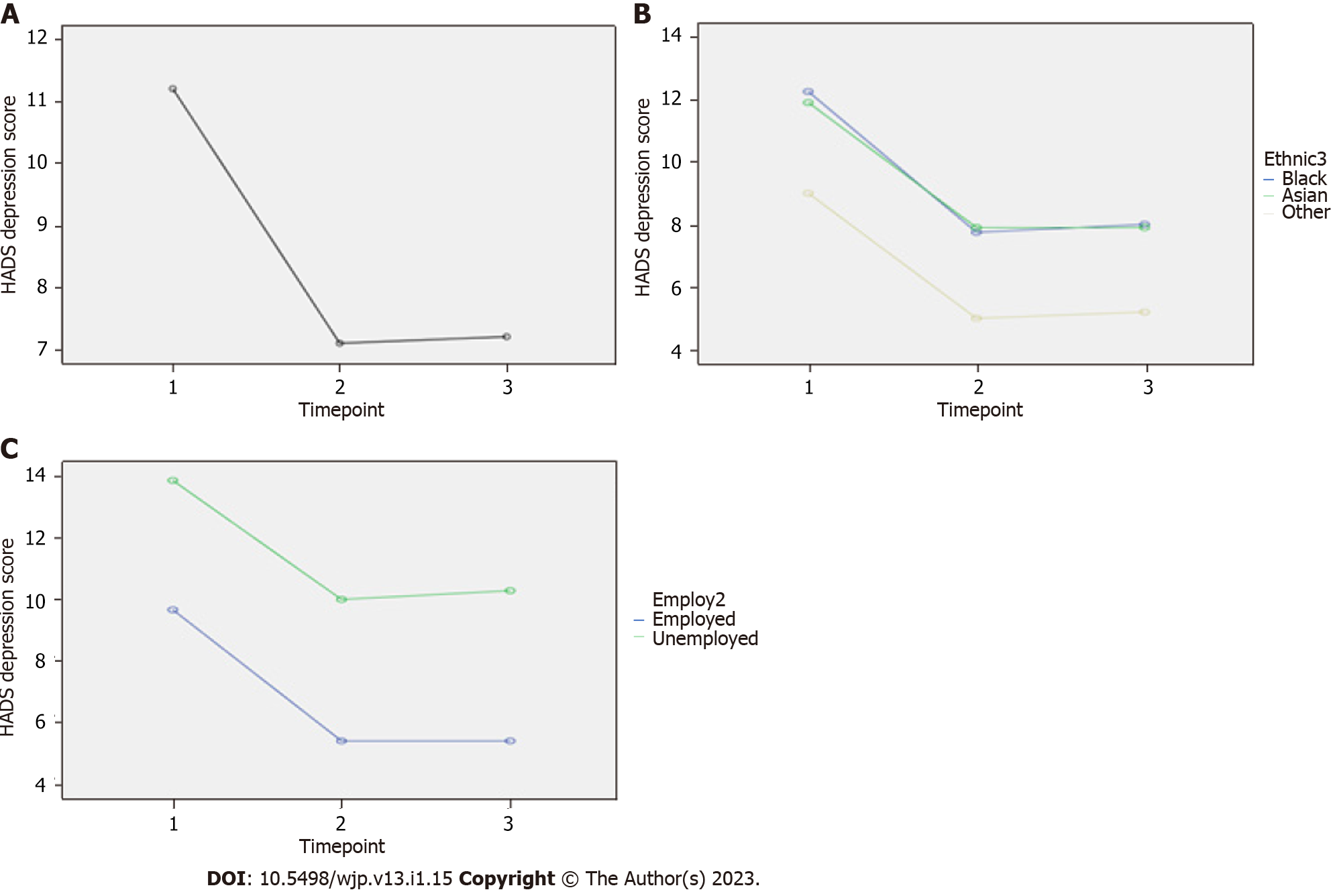
Change in HADS depression using repeated measures ANOVA: HADS depression score was significantly different when all three time points were compared simultaneously: F (2, 36) = 12.81, P < 0.001, partial eta squared = 0.42 (Figure 3A). However, Bonferroni-adjusted pairwise comparisons showed that HADS depression significantly reduced from baseline to post-treatment and baseline to follow-up, but there was no significant difference between posttreatment and follow-up (Table 5). This meant that there was a benefit at post-treatment and that the benefit was maintained at follow-up.
| Dependent variable | Independent variable | Degrees of freedom | F value | P value | Partial eta squared (variance explained; i.e., effect size) | Bonferroni adjusted pairwise comparisons | ||
| HADS depression | Timepoint (within subjects) | 2, 36 | 12.81 | < 0.001 | 0.42 | Baseline (mean 11.21 SD 4.28) vs post-treatment (mean 7.11, SD 3.99), P = 0.004 | Baseline vs follow-up (mean 7.21, SD 4.99), P = 0.001 | Post treatment vs follow-up, P = 1.0 |
| Employment (between subjects) | 1, 17 | 9.73 | 0.006 | 0.36 | Employed vs unemployed mean difference1 -4.55 (95%CI: -7.62 to -1.47); employed have lower mean score at all three time points | |||
| Employment X time point (within subjects) | 2, 34 | 0.06 | 0.94 | 0.004 | NA | NA | NA | |
| HADS Anxiety | Timepoint (within subjects) | 2, 36 | 9.93 | < 0.001 | 0.36 | Baseline (mean 14.53 SD 4.01) vs post-treatment (mean 11.05, SD 3.40), P = 0.003 | Baseline vs follow-up (mean 11.21, SD 4.05), P = 0.001 | Post treatment vs follow-up, P = 0.831 |
| WHO disability scale total | Timepoint (within subjects) | 1.29, 14.182 | 6.732 | 0.016 | 0.382 | Baseline (mean 66.58 SD 40.13) vs post-treatment (mean 44.42, SD 32.35), P = 0.034 | Baseline vs follow-up (mean 38.75, SD 26.499), P = 0.014 | Post treatment vs follow-up, P = 0.194 |
| Living alone (between subjects) | 1, 10 | 8.99 | 0.013 | 0.47 | Living alone vs with someone mean difference1 51.9 (95%CI: 13.33 to 90.47); living alone have higher score at all three timepoints | |||
| Living alone X timepoint (within subjects) | 1.21, 12.072 | 0.392 | 0.581 | 0.042 | NA | NA | NA | |
| Employment (between subjects) | 1, 10 | 8.68 | 0.015 | 0.47 | Employed vs unemployed mean difference1 -44.26 (95%CI: -77.62 to -10.79); employed have lower mean score at all three time points | |||
| Employment X Time point (within subjects) | 1.32, 13.182 | 2.992 | 0.1 | 0.232 | NA | NA | NA | |
| CORE total | Timepoint | 1.25, 18.722 | 14.982 | 0.001 | 0.52 | Baseline (mean 76.81, SD 23.26) vs post-treatment (mean 49.25, SD 27.00), P = 0.002 | Baseline vs follow-up (mean 52.19, SD 25.72), P < 0.001 | Post treatment vs follow-up, P = 0.404 |
| CORE total mean with risk | Timepoint | 1.25, 18.722 | 14.982 | 0.001 | 0.52 | Baseline (mean 2.26, SD 0.68) vs post-treatment (mean 1.45, SD 0.79), P = 0.002 | Baseline vs follow-up (mean 1.53, SD 0.76), P < 0.001 | Post treatment vs follow-up, P = 0.404 |
| CORE Total mean without risk | Timepoint | 1.24, 18.662 | 16.58 | < 0.001 | 0.532 | Baseline (mean 2.62, SD 0.71) vs post-treatment (mean 1, SD 0.87), P = 0.001 | Baseline vs follow-up (mean 1.77, SD 0.79), P < 0.001 | Post treatment vs follow-up, P = 0.523 |
| CORE risk mean | Timepoint | 2, 36 | 1.83 | 0.175 | 0.09 | Baseline (mean 0.48, SD 0.75) vs post-treatment (mean 0.26, SD 0.55), P = 0.109 | Baseline vs follow-up (mean 0.39, SD 0.77), P = 0.418 | Post treatment vs follow-up, P = 0.096 |
| CORE symptoms mean | Timepoint | 2, 32 | 91.10 | < 0.001 | 0.54 | Baseline (mean 2.81, SD 0.77) vs post-treatment (mean 1.76, SD 1.03), P < 0.001 | Baseline vs follow-up (mean 1.91, SD 0.89), P < 0.001 | Post treatment vs follow-up, P = 0.317 |
| CORE functioning mean | Timepoint | 1.25, 19.922 | 7.26 | 0.01 | 0.31 | Baseline (mean 2.25, SD 0.88) vs post-treatment (mean 1.61, SD 0.86), P = 0.016 | Baseline vs follow-up (mean 1.65, SD 0.83), P = 0.009 | Post treatment vs follow-up, P = 0.692 |
| CORE well being mean | Timepoint | 2, 36 | 20.41 | < 0.001 | 0.53 | Baseline (mean 2.82, SD 0.67) vs post-treatment (mean 1.68, SD 0.68), P < 0.001 | Baseline vs follow-up (mean 1.76, SD 0.87), P < 0.001 | Post treatment vs follow-up, P = 0.61 |
| BSI total | Timepoint | 2, 36 | 6.50 | 0.008 | 0.26 | Baseline (mean 22.11, SD 11.40) vs post-treatment (mean 19.05, SD 10.23), P < 0.066 | Baseline vs follow-up (mean 16.47, SD 11.10), P < 0.008 | Post treatment vs follow-up, P = 0.041 |
No difference between ethnic groups meant that the intervention showed similar effect in the groups (Figure 3B). However, the effect of employment status as a covariate on HADS depression was significant: F (1, 17) = 9.73, P = 0.006, eta squared = 0.36 (Figure 3C). Employed people showed lower HADS depression mean scores at all three time points. Interaction of employment with timepoint was not significant.
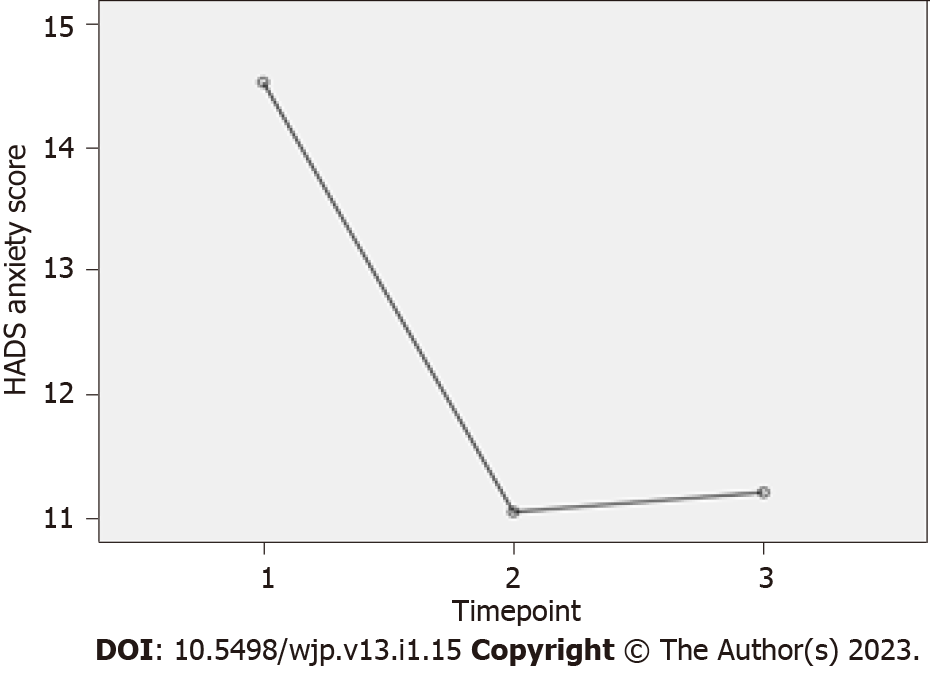
Change in HADS anxiety using repeated measures ANOVA: HADS anxiety score was significantly different when all three time points were compared simultaneously: F (2, 36) = 9.93, P < 0.001, partial eta squared = 0.36 (Figure 4). However, Bonferroni-adjusted pairwise comparisons showed that HADS anxiety significantly reduced from baseline to post-treatment and baseline to follow-up, but there was no significant difference between post-treatment and follow-up (Table 5). This meant that there was a benefit at post-treatment and that the benefit was maintained at follow-up.
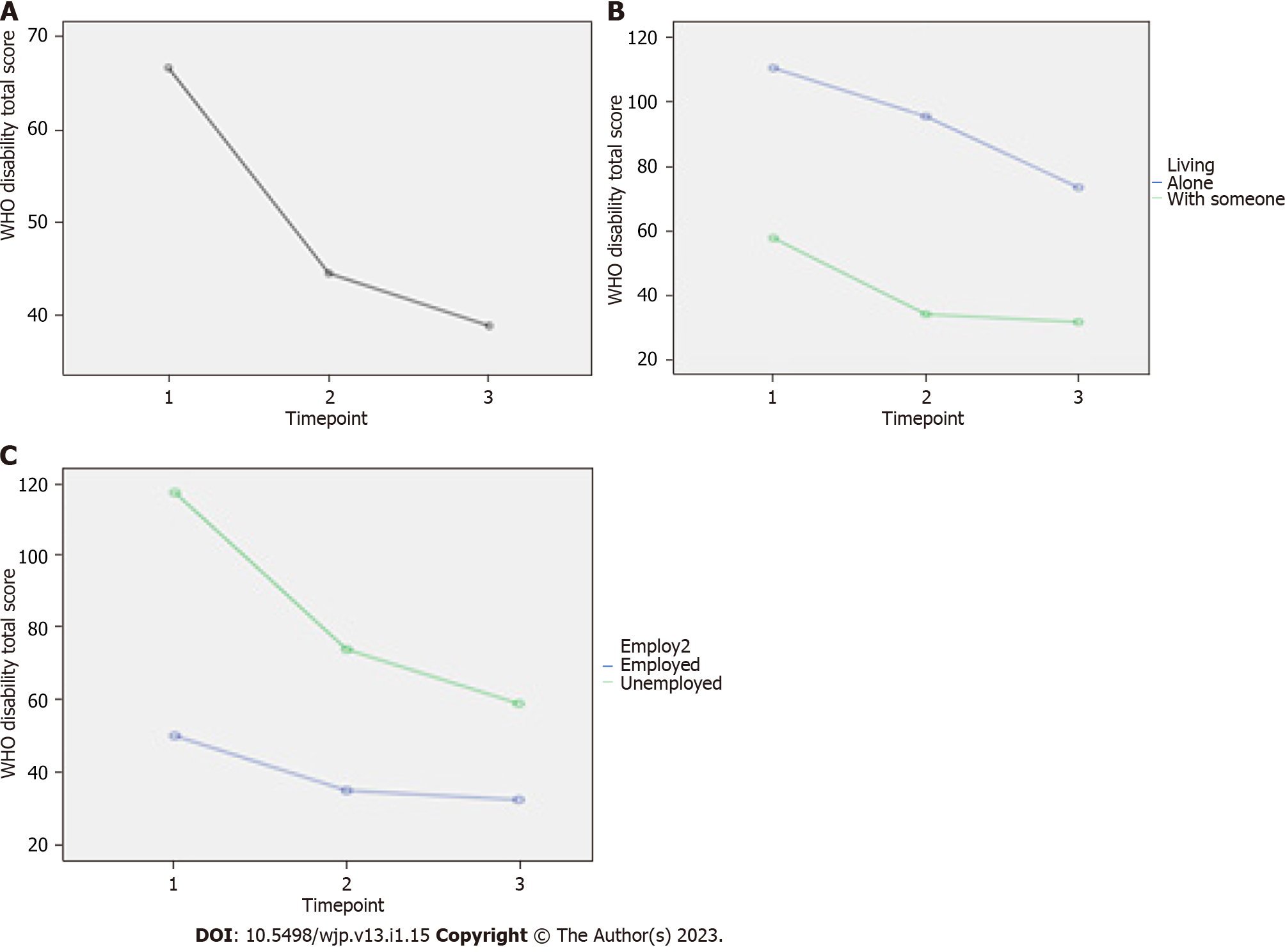
Change in WHO disability scale using repeated measures ANOVA: WHO disability scale was significantly different when all three time points were compared simultaneously: F (1.29, 14.18) = 6.73, P < 0.016, partial eta squared = 0.38 (Figure 5A). However, Bonferroni-adjusted pairwise comparisons showed that the WHO disability scale significantly reduced from baseline to post-treatment and baseline to follow-up, but there was no significant difference between post-treatment and follow-up (Table 5). This meant that there was a benefit at post-treatment and that the benefit was maintained at follow-up. However, the effect of living alone as covariate on WHO disability scale was significant: F (1, 10) = 8.99, P = 0.013, eta squared = 0.47 (Figure 5B). Those who were living alone had higher mean score at all three times. Interaction of living with timepoint was not significant. In addition, the effect of employment status as a covariate on WHO disability scale was significant, F (1, 10) = 8.68, P = 0.015, eta squared = 0.47 (Figure 5C). Employed people showed lower WHO disability scale mean score at all three time points. Interaction of employment with timepoint was not significant.
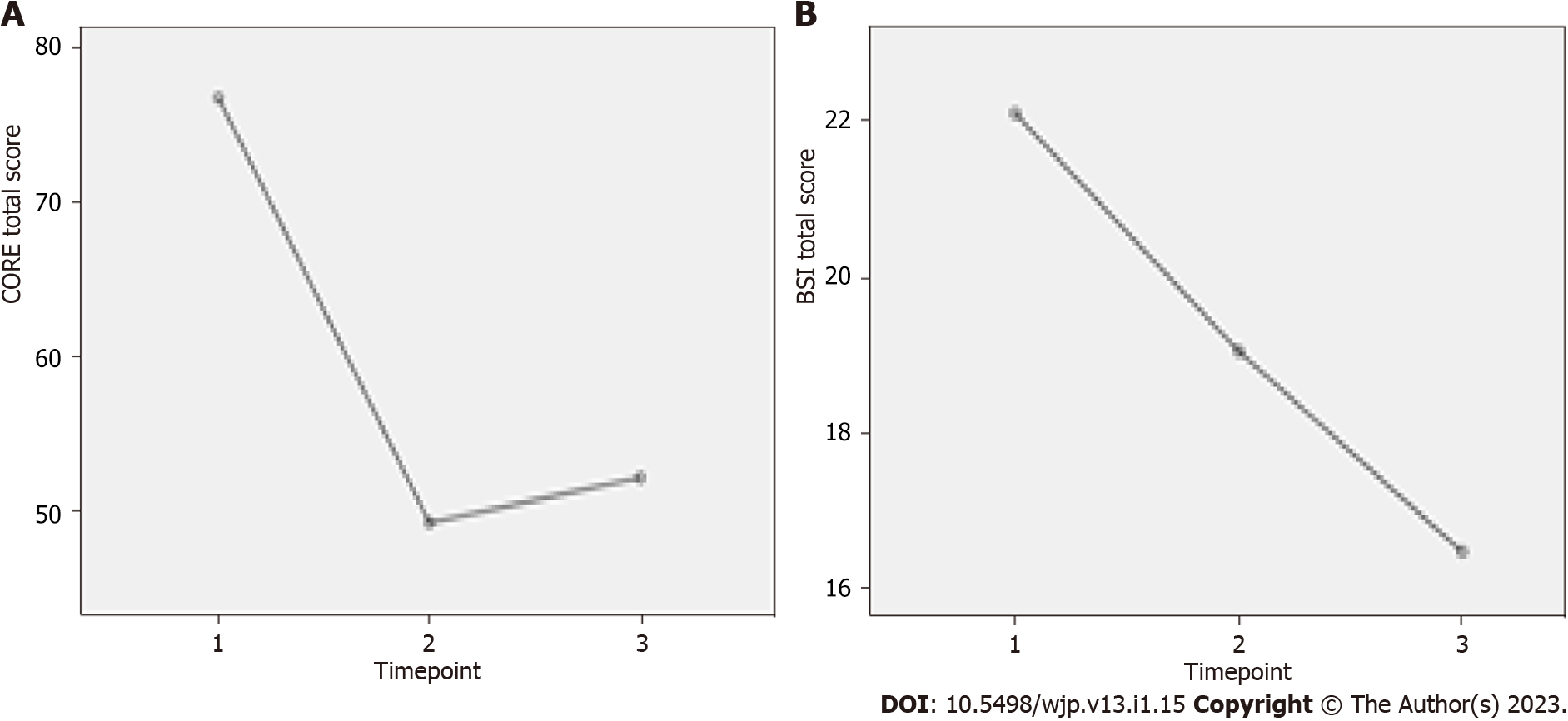
Change in CORE total score using repeated measures ANOVA: The CORE total score was significantly different when all three time points were compared simultaneously: F (1.25, 18.72) = 14.98, P = 0.001, partial eta squared = 0.5 (Figure 6A). However, Bonferroni-adjusted pairwise comparisons showed that CORE total score significantly reduced from baseline to post-treatment and baseline to follow-up, but there was no significant difference between post-treatment and follow-up (Table 5). This meant that there was a benefit at post-treatment and that the benefit was maintained at follow-up.
Change in CORE total mean to risk using repeated measures ANOVA: The CORE total mean with risk was significantly different when all three time points were compared simultaneously: F (1.25, 18.72) = 14.98, P = 0.001, partial eta squared = 0.5. However, Bonferroni-adjusted pairwise comparisons showed that the CORE total mean with risk significantly reduced from baseline to post-treatment and baseline to follow-up; but there was no significant difference between post-treatment and follow-up (Table 5). This meant that there was a benefit at post-treatment and that the benefit was maintained at follow-up.
The effect of the following covariates on the HADS, WHODAS, and CORE total mean with risk was not significant: Age, gender, diagnosis, psychiatric medication, living with someone or alone, ethnic group, having higher education or not, having a partner or not, duration of mental illness, being under care of CMHT or IAPT, history of previous admission, use of additional services and employment status. No difference between ethnic groups meant that the intervention showed similar effects in the groups.
Change in CORE total mean without risk using repeated measures ANOVA: The CORE total mean without risk was significantly different when all three time points were compared simultaneously: F (1.24, 18.66) = 16.58, P < 0.001, partial eta squared = 0.53. However, Bonferroni-adjusted pairwise comparisons showed that the CORE total mean without risk significantly reduced from baseline to post-treatment and baseline to follow-up; but there was no significant difference between post-treatment and follow-up (Table 5). This meant that there was a benefit at post-treatment and that the benefit was maintained at follow-up.
Change in CORE risk mean using repeated measures ANOVA: The CORE risk mean was not significantly different when all three time points were compared simultaneously: F (2, 36) = 11.83, P = 0.175, partial eta squared = 0.09. Furthermore, Bonferroni-adjusted pairwise comparisons showed that the CORE risk mean was not significantly different in any of the three-way comparisons (Table 5). This meant that this measurement did not change significantly between the three time points. Thus, no covariates were entered in this analysis.
Change in CORE symptoms mean using repeated measures ANOVA: The CORE symptom mean was significantly different when all three time points were compared simultaneously: F (2, 32) = 91.10, P < 0.001, partial eta squared = 0.54. However, Bonferroni-adjusted pairwise comparisons showed that the CORE symptom mean significantly reduced from baseline to post-treatment and baseline to follow-up; but there was no significant difference between post-treatment and follow-up (Table 5). This meant that there was a benefit at post-treatment and that the benefit was maintained at follow-up.
Changes in CORE functioning mean using repeated measures ANOVA: The CORE functioning mean was significantly different when all three time points were compared simultaneously: F (1.25, 91.92) = 7.26, P = 0.01, partial eta squared = 0.31. However, Bonferroni-adjusted pairwise comparisons showed that the CORE functioning mean significantly reduced from baseline to post-treatment and baseline to follow-up; but there was no significant difference between post-treatment and follow-up (Table 5). This meant that there was a benefit at post-treatment and that the benefit was maintained at follow-up.
Changes in CORE wellbeing mean using repeated measures ANOVA: CORE wellbeing mean was significantly different when all three time points were compared simultaneously, F (2, 36) = 20.41, P = 0.01, partial eta squared = 0.53. However, Bonferroni-adjusted pairwise comparisons showed that CORE wellbeing mean significantly reduced from baseline to post-treatment and baseline to follow-up; but there was no significant difference between post-treatment and follow-up (Table 5). This meant that there was a benefit at post-treatment and that the benefit was maintained at follow-up.
Change in BSI total using repeated measures ANOVA: The BSI total was significantly different when all three time points were compared simultaneously: F (2, 36) = 6.50, P = 0.008, partial eta squared = 0.26 (Figure 6B). However, Bonferroni-adjusted pairwise comparisons showed that the BSI total did not reduce significantly from baseline to post-treatment and but did so from baseline to follow-up; there was also a significant difference between post-treatment and follow-up (Table 5). This meant that there was no benefit at post-treatment but there was at follow-up.
Compared with ANOVA, ANCOVA further analysed the outcomes adjusted by certain covariates. This allowed us to examine the sensitivity of the findings in ANOVA towards certain covariates. If the significant results in ANOVA changed tremendously to unsignificant, the reliability of the results in ANOVA should be doubted. Such covariates could be influencing the outcomes in an undetected way and thereby contribute to the differences between groups. Therefore, we further analysed the significant model in ANOVA. After adding covariates, the P-value in ANOVA changed from less than 0.05 to larger than 0.05 in ANCOVA, thus these covariates were the key variables we should pay attention to. If the significant results in ANOVA remained significant in ANCOVA, i.e., no drastic changes in the P-value, it would consolidate our finding in ANOVA by evidencing the insensitivity of the result towards the covariate.
Change in HADS depression using mixed factorial ANCOVA: With Timepoint and Employment being factor, HADS depression score adjusted by gender was not significantly different when all three time points were compared simultaneously: F (2, 42) = 0.158, P = 0.855. Also, when adjusted by age, HADS depression score did not show significant difference across three time points: F (2.42) = 0.595, P = 0.556 (Table 6). This suggested part of the differences of HADS depression scores across three timepoints could be explained by gender. Bonferroni-adjusted pairwise comparisons had the similar results to those of ANOVA.
| Dependent variable | Covariate | Independent variable | Degrees of freedom | F value | P value | Bonferroni adjusted pairwise comparisons | ||
| HADS depression | Gender | Timepoint (within subjects) | 2, 42 | 0.158 | 0.855 | Baseline (mean 11.77 SD 0.78) vs post-treatment (mean 7.75, SD 0.73), P = 0.003 | Baseline vs follow-up (mean 7.55, SD 0.89), P < 0.001 | Post treatment vs follow-up, P = 1.0 |
| Employment (between subjects) | 1, 21 | 9.788 | 0.005 | Employed vs unemployed mean difference1 -3.96 (95%CI: -6.60 to -1.33); employed have lower mean score at all three time points | ||||
| Age | Timepoint (within subjects) | 2, 42 | 0.595 | 0.556 | Baseline (mean 11.85 SD 0.77) vs post-treatment (mean 7.78, SD 0.74), P = 0.002 | Baseline vs follow-up (mean 7.62, SD 0.89), P < 0.001 | Post treatment vs follow-up, P = 1.0 | |
| Employment (between subjects) | 1, 21 | 11.266 | 0.003 | Employed vs unemployed mean difference1 -4.33 (95% CI: -7.02 to -1.65); employed have lower mean score at all three time points | ||||
| HADS Anxiety | Gender | Timepoint (within subjects) | 2, 44 | 0.014 | 0.986 | Baseline (mean 14.54 SD 0.77) vs post-treatment (mean 10.33, SD 0.75), P < 0.001 | Baseline vs follow-up (mean 10.38, SD 0.86), P < 0.001 | Post treatment vs follow-up, P = 1.0 |
| WHO disability scale total | Gender | Timepoint (within subjects) | 1.24, 22.382 | 0.3542 | 0.7042 | Baseline (mean 85.32 SD 8.72) vs post-treatment (mean 65.83, SD 7.42), P = 0.143 | Baseline vs follow-up (mean 53.59, SD 8.26), P = 0.014 | Post treatment vs follow-up, P = 0.016 |
| Living alone (between subjects) | 1, 18 | 8.288 | 0.010 | Living alone vs with someone mean difference1 37.82 (95%CI: 10.22 to 65.42); living alone have higher score at all three timepoints | ||||
| Employment (between subjects) | 1, 18 | 10.674 | 0.004 | Employed vs unemployed mean difference1 -30.52 (95%CI: -50.14 to -10.89); employed have lower mean score at all three time points | ||||
| Age | Timepoint (within subjects) | 1.25, 22.412 | 3.6312 | 0.0622 | Baseline (mean 84.69 SD 8.62) vs post-treatment (mean 65.47, SD 6.89), P = 0.138 | Baseline vs follow-up (mean 53.30 SD 7.41), P = 0.011 | Post treatment vs follow-up, P = 0.013 | |
| Living alone (between subjects) | 1, 18 | 8.167 | 0.010 | Living alone vs with someone mean difference1 34.92 (95%CI: 9.25 to 60.59); living alone have higher score at all three timepoints | ||||
| Employment (between subjects) | 1, 18 | 14.555 | 0.001 | Employed vs unemployed mean difference1 -35.13 (95%CI: -54.47 to -15.78); employed have lower mean score at all three time points | ||||
| Higher Education | Timepoint (within subjects) | 1.22, 20.782 | 3.5062 | 0.0682 | Baseline (mean 84.60 SD 8.89) vs post-treatment (mean 65.38, SD 7.64), P = 0.165 | Baseline vs follow-up (mean 52.48, SD 8.31), P = 0.014 | Post treatment vs follow-up, P = 0.008 | |
| Living alone (between subjects) | 1, 17 | 7.318 | 0.015 | Living alone vs with someone mean difference1 36.75 (95%CI: 8.09 to 65.41); living alone have higher score at all three timepoints | ||||
| Employment (between subjects) | 1, 17 | 10.370 | 0.005 | Employed vs unemployed mean difference1 -31.02 (95%CI: -51.34 to -10.70); employed have lower mean score at all three time points | ||||
| CORE total | Gender | Timepoint | 1.47, 32.302 | 0.0282 | 0.9382 | Baseline (mean 73.88, SD 4.56) vs post-treatment (mean 47.42, SD 5.11), P < 0.001 | Baseline vs follow-up (mean 48.04, SD 5.25), P < 0.001 | Post treatment vs follow-up, P = 1.0 |
| Age | Timepoint | 1.47, 32.232 | 0.9752 | 0.3642 | Baseline (mean 73.88, SD 4.48) vs post-treatment (mean 47.42, SD 4.95), P < 0.001 | Baseline vs follow-up (mean 48.04, SD 5.15), P < 0.001 | Post treatment vs follow-up, P = 1.0 | |
| BSI total | Age | Timepoint | 2, 46 | 0.285 | 0.753 | Baseline (mean 22.64, SD 2.06) vs post-treatment (mean 18.60, SD 2.06), P = 0.041 | Baseline vs follow-up (mean 16.60, SD 2.09), P = 0.001 | Post treatment vs follow-up, P = 0.406 |
| Gender | Timepoint | 2, 46 | 1.027 | 0.366 | Baseline (mean 22.64, SD 2.03) vs post-treatment (mean 18.60, SD 2.09), P = 0.026 | Baseline vs follow-up (mean 16.60, SD 2.07), P = 0.001 | Post treatment vs follow-up, P = 0.411 | |
| Higher education | Timepoint | 2, 44 | 2.811 | 0.071 | Baseline (mean 22.58, SD 2.19) vs post-treatment (mean 18.21, SD 2.15), P = 0.028 | Baseline vs follow-up (mean 16.75, SD 2.11), P = 0.003 | Post treatment vs follow-up, P = 0.661 | |
| Marital status | Timepoint | 2, 46 | 3.146 | 0.052 | Baseline (mean 22.64, SD 2.05) vs post-treatment (mean 18.60, SD 2.08), P = 0.040 | Baseline vs follow-up (mean 16.60, SD 2.08), P = 0.002 | Post treatment vs follow-up, P = 0.434 | |
In addition to this, other covariates, such as psychiatric medication, living with someone or alone, having higher education or not, having a partner or not, duration of mental illness, being under care of a CMHT or IAPT, history of previous admission and use of additional services, didn’t change the results of the ANOVA analysis. Therefore, with factors living alone and employment, differences in questionnaire scores at three timepoints were not caused by these covariates.
Change in HADS anxiety using repeated measures ANCOVA: Results in ANOVA showed that HADS anxiety score was significantly different through three timepoints with a P-value less than 0.001 (Table 6). While HADS anxiety score adjusted by gender was not significantly different when all three time points were compared simultaneously: F (2, 44) = 0.014, P = 0.986 (Table 6). This suggested part of the difference of HADS anxiety score across three time points could be explained by gender. Bonferroni-adjusted pairwise comparison kept the similar results with those of ANOVA analysis.
Change in WHO disability scale using mixed factorial ANCOVA: Based on the results of ANOVA, model with factors employment and living alone had a P-value of 0.016 between three timepoints (Table 6). In ANCOVA analysis, with the same two factors, WHO disability scale adjusted by gender was not significantly different when all three time points were compared simultaneously: F (1.24, 22.38) = 0.354, P = 0.704 (Table 6). This meant that part of the difference of WHO disability scale across three time points could be explained by gender. With the same factors, using covariates age or higher education respectively resulted in a small increase in the P-value of time-point: From P = 0.016 (Table 5) to P = 0.062 and P = 0.068 (Table 6). It was evident from the results that the changes to the WHO disability scale between three time points was not easily explained by age or higher education. Bonferroni-adjusted pairwise comparison failed to show significant reduction of the WHO disability scale from baseline to post-treatment. However, our results showed a significant reduction of the WHO disability scale from baseline to follow-up and from post-treatment to follow-up.
Change in CORE total score using repeated measures ANCOVA: The CORE total score adjusted by gender and age respectively was not significantly different when all three time points were compared simultaneously: F (1.47, 32.30) = 0.028, P = 0.938 and F (1.47, 32.23), P = 0.364 (Table 6). After adding these two covariates respectively, the differences of scores between three timepoint were not that much, which suggested part of the difference of CORE total score across three time points could be explained by gender and age. Bonferroni-adjusted pairwise comparison result did not change.
Change in BSI total using repeated measures ANCOVA: The BSI total adjusted by age and gender respectively was not significantly different when all three time points were compared simultaneously: F (2, 46) = 0.285, P = 0.753 and F (2, 46), P = 0.366 (Table 6). As for the covariate higher education, it showed a small increase in the P-value of timepoint from ANOVA results to ANCOVA results: From P = 0.008 (Table 5) to P = 0.071 (Table 6). This suggested part of the difference of BSI total across three time points could be explained by age and gender. Bonferroni-adjusted pairwise comparison result was the same as ANOVA results.
BSI item 45 asked only at baseline ‘Have felt that you have been passing urine in the semen?’ A total n = 6 men answered “no”. BSI item 46 asked at all three time points, ‘Have you had difficulty getting a full erection?’ All n = 6 male respondents answered “no” at baseline, while post-treatment (n = 4) responded “no” and (n = 1) said “yes”, while 1 did not respond. At follow-up timepoint, (n = 4) responded “no” and (n = 2) did not respond.
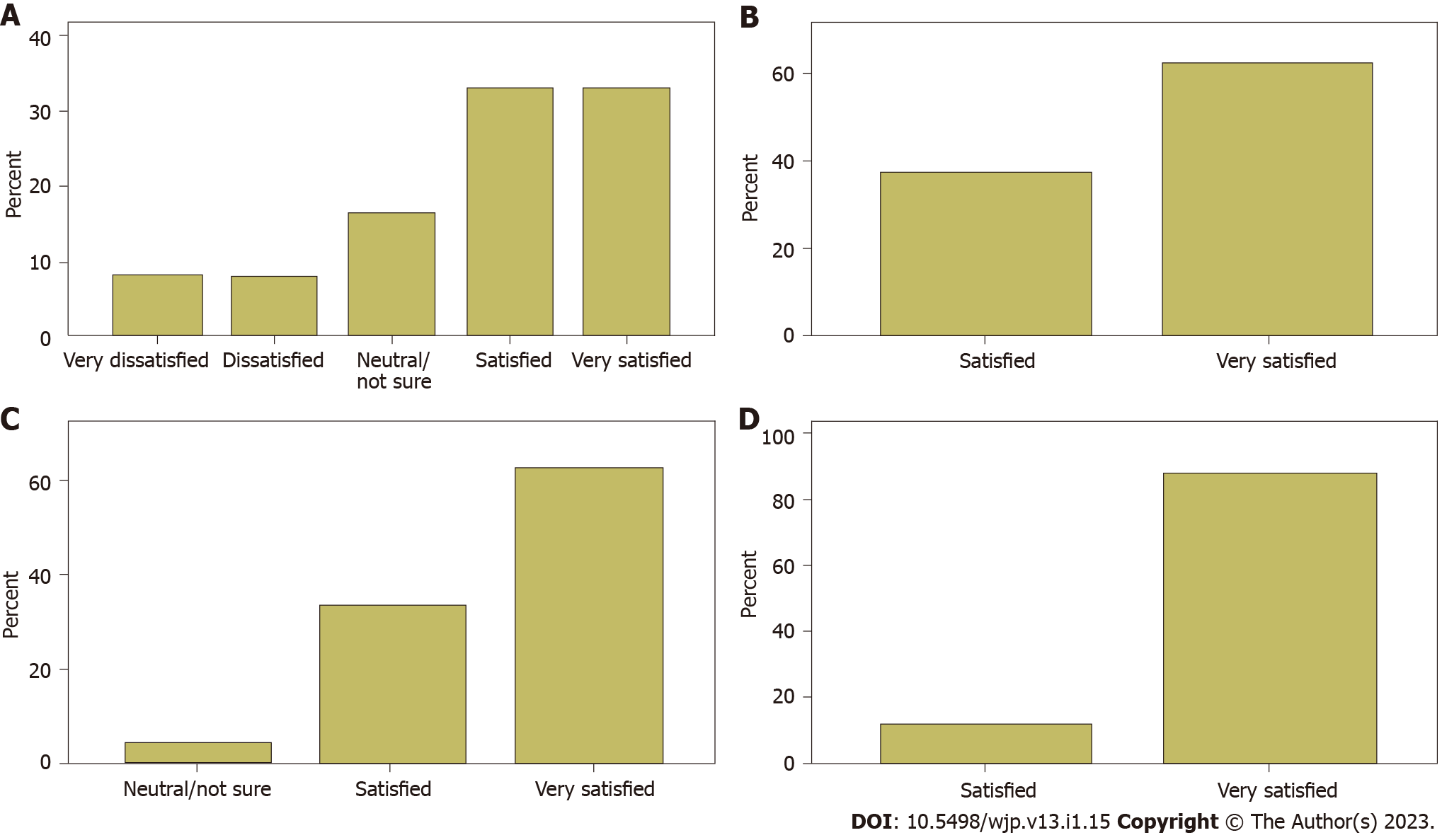
PEQ analysis involved descriptive data on each item relating to the patient experience and satisfaction of the intervention. Figures 7A-D display a graphical presentation of the PEQ items 1, 3, 5, and 10. A total of 24 out of 32 participants completed the questionnaire. There was a significant positive correlation between PEQ item 8 and CORE risk mean (Somers D = 0.5); between PEQ item 8 and HADS Depression (Somers D = 0.67); and between PEQ item 8 and CORE functioning mean (Somers D = 0.69). This meant that the people who had worse scores on risk, functioning, and depression were more engaged with the treatment. However, all other correlations were not significant. Therefore, overall, the experience of treatment was independent of the changes in the outcome scales.
Our feasibility study sought to explore how some of the cultural barriers could be addressed with a manual that adapts the CBT based, third-wave based, CCC therapy- for diverse ethnic minority groups. Of the 32 participants within our sample, 3 dropped out before completing a total of 6 sessions. Thus, there is a positive notion for acceptability and adherence to the intervention. Given the ethnic diversity within the study sample, our manual appears to have relevance to operate cross-culturally. Significant improvement on anxiety/depression (HADS, anxiety and depression, BSI, and CORE) and overall quality of life (WHODAS) is suggested within the study sample. Developing the manual in response to challenges posed by the therapy in supervision raised interesting issues that were resolved within the CCC framework. Therefore, the development of CBT approaches built around mindfulness, commonly referred to as the third-wave, promotes a reflective space between the individual’s thoughts and feelings, in contrast to the direct challenge, which makes it more acceptable to ethnic minority groups. CCC avoids much of the complexity of other therapies by drawing on its roots in cognitive science to target the universal human need to establish a tolerable internal state. Attempts to regain equilibrium where this state is not tolerable led to behaviors and experiences that are then labelled as symptoms.
In addition, difference in cultural attitudes where assertiveness and anger proved amenable to the controlled expression of emotion with a mindfulness approach, which is similar to previous research conducted[18,37]. This could also be an intervention that could aid managing family expectations’ to highly sensitive subject matter[6]. Issues that raised religious and cultural sensitivity, such as sexual abuse, required both validation of the individual’s experience and acceptance of the limitation of open acknowledgement by the wider group. The relational nature of the interacting cognitive subsystems-based model of the person opens the way to the discussion of religious and faith issues that sidestepped contentious dogmas. CCC enables deep reflection by accommodating cultural adjustments, it makes this process of therapy more applicable and relevant. At present, four studies on CCC have been published looking at acute psychology which is different to the intervention used in this study[43,54-56], while demonstrating the ability of the approach to engage a challenging population. Three more studies are in preparation. Research into CCC is sparse at the moment and this pilot study is preliminary research into the CCC intervention, hence currently lacks any research comparators. The findings of this study are largely in line with previous research on culturally adapted CBT. Previous research found that adaptations in core elements, such as family, therapy delivery, and religious/spiritual views, enabled for the most efficacious outcomes for ethnic minority groups[14,15].
The recognized role of childhood or adult trauma in the development of psychological stress needing clinical management and psychological input is fully incorporated into CCC. The participant characteristics highlight the spectrum of trauma and past adversity contributing to current mental health difficulties across a primary care sample not selected for trauma. In the United Kingdom, National Institute for Health and Care Excellence guidelines provide an important consideration for clinicians who have such patients. Therefore, it is essential that primary, secondary, and tertiary care health professionals are fully aware of such issues to ensure patients receive optimal short, medium, and long-term care that is detrimental to reducing distress and improving their quality of life. Similarly, emotional, and general wellbeing, should be considered as an undercurrent to this intervention that requires to be kept at proximity, when managing ongoing care for these patients. Equally, in the event, potential patients have underlying chronic long-term comorbidities, the correlational aspect should be considered at the time of introducing this intervention and measuring its outcome longitudinally.
The main limitation of this study was that it was an uncontrolled pilot study to assess the feasibility of the manualized intervention. Therefore, the sample size remained sizable to demonstrate an effect size. The sample used was skewed towards female participants (84.4%) and outcome measures were not adapted accordingly. Future studies should consider gender accountability. The emphasis was on learning from individual therapies with individuals who presented to an IAPT service and a CMHT with a wide range of problems and from diverse ethnicities. In relation to using both primary and secondary care samples, results have shown that both groups accepted in intervention and participant satisfaction was significant. As such, it represents the normal clinical practice in its complexity, making generalization more difficult. However, within these limitations, the results are promising and should merit a more extensive and definitive phase three randomized controlled interventions in the future.
In terms of future research, it would be ideal for a comprehensive randomized study design to be implemented. It would be insightful to include a much larger sample size with proportionate participant numbers from each ethnic group included. This would allow for stronger statistical outputs and more generalizable conclusions regarding the impact of this CaCBT-based third-wave therapy manual.
The culturally adapted CBT third-wave based manual intervention showed significant improvement in symptoms (HADS, anxiety and depression and CORE) and overall quality of life (WHODAS) from baseline to post-treatment. The study therapists reported that the adapted CCC formulation was simple, effective, and validated the patients’ experiences well. This study adds to the body of knowledge supporting cultural adaptations of evidence-based therapies for diverse and minoritized ethnic groups.
Currently, cognitive behavioral therapy (CBT) is one of the most common interventions implemented to treat symptoms of psychopathology of various illnesses. Standardised CBT manuals may not be completely relevant to all populations for several reasons including cultural and psychosocial variations.
Culturally adapted CBT could be beneficial to individuals of minority ethnic backgrounds as the contextual relevance may elevate the therapeutic benefit. Hence, this paper proposes a CaCBT-based third-wave therapy manual based on the Comprehend, Cope and Connect model.
This study aimed to test the feasibility, acceptability and adherence of the proposed intervention within ethnic minority participants who are currently engaged in Improving Access to Psychological Therapies’ iTalk and Community Mental Health Team services that are part of the United Kingdom’s National Health Service.
In order to test the intervention, an uncontrolled feasibility study was deployed with 32 participants. Various outcome measures were recorded at three time points (baselines, post-intervention, and 12-wk follow-up).
A repeated measures analysis of variance revealed significant improvements in symptoms across Hospital Anxiety and Depression Scale depression and anxiety scores as well as the Clinical Outcomes in Routine Evaluation total score and World Health Organization Disability Assessment Schedule 2.0 measures.
The results of this feasibility study reported that the CaCBT-based third-wave therapy was effective. Our results also showed significant adherence and acceptability among minority ethnic participants. Moderate effect sizes were reported with high participant satisfaction levels although a wider clinical trial will be required to fully assess the efficacy and effectiveness of the manual in the future.
It would be important to further explore a randomised controlled trial as well as its’ cost-effectiveness, overall benefit and scalability to a more diverse sample within the United Kingdom. This would aid in conducting wider global clinical trials to better understand the suitability of this adapted intervention.
The authors would like to thank all participants who contributed to the study. The authors would like to thank Matthew McNought and Carmen Caro Morente for their contributions as research therapists in the project and Sana Sajid and Joanna Pang for their administrative support.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Corresponding Author’s Membership in Professional Societies: Nursing and Midwifery Council (NMC), 98I1393; British Association for Behavioural and Cognitive Psychotherapies (BABCP), 060632.
Specialty type: Psychology
Country/Territory of origin: United Kingdom
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: El Sayed S, Egypt; Lee N, South Korea S-Editor: Wang JJ L-Editor: A P-Editor: Wang JJ
| 1. | Beck AT, Rush AJ, Shaw BF, Emery G. Cognitive Therapy of Depression. New York: Guilford Press, 1979. |
| 2. | Knapp P, Kieling C, Beck AT. What do psychotherapists do? Psychother Psychosom. 2015;84:377-378. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 10] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 3. | Chu BC, Harrison TL. Disorder-specific effects of CBT for anxious and depressed youth: a meta-analysis of candidate mediators of change. Clin Child Fam Psychol Rev. 2007;10:352-372. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 90] [Cited by in RCA: 72] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 4. | Gallagher MW, Long LJ, Richardson A, D'Souza J, Boswell JF, Farchione TJ, Barlow DH. Examining Hope as a Transdiagnostic Mechanism of Change Across Anxiety Disorders and CBT Treatment Protocols. Behav Ther. 2020;51:190-202. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 36] [Article Influence: 7.2] [Reference Citation Analysis (0)] |
| 5. | Bernal G, Bonilla J, Bellido C. Ecological validity and cultural sensitivity for outcome research: issues for the cultural adaptation and development of psychosocial treatments with Hispanics. J Abnorm Child Psychol. 1995;23:67-82. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 450] [Cited by in RCA: 480] [Article Influence: 16.0] [Reference Citation Analysis (0)] |
| 6. | Rathod S, Phiri P, Naeem F. An evidence-based framework to culturally adapt cognitive behaviour therapy. CBT. 2019;12:E10. [RCA] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 26] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 7. | Cavagnol RM, De NS. Repurposing english language CBT to Japanese language WBT using an international translation authoring program (iTAP). Performance Improvement. 2006;45:9-14. [DOI] [Full Text] |
| 8. | López SR, Grover KP, Holland D, Johnson MJ, Kain CD, Kanel K, Mellins C, Rhyne MC. Development of culturally sensitive psychotherapists. Professional Psychol Res Pract. 1989;20:369-376. [RCA] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 40] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 9. | Resnicow K, Soler R, Braithwaite RL, Ahluwalia JS, Butler J. Cultural sensitivity in substance use prevention: Bridging the gap between research and practice in community-based substance abuse prevention. J Commun Psychol. 2002;28. [DOI] [Full Text] |
| 10. | Arundell LL, Barnett P, Buckman JEJ, Saunders R, Pilling S. The effectiveness of adapted psychological interventions for people from ethnic minority groups: A systematic review and conceptual typology. Clin Psychol Rev. 2021;88:102063. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 47] [Cited by in RCA: 43] [Article Influence: 10.8] [Reference Citation Analysis (0)] |
| 11. | Chowdhary N, Jotheeswaran AT, Nadkarni A, Hollon SD, King M, Jordans MJ, Rahman A, Verdeli H, Araya R, Patel V. The methods and outcomes of cultural adaptations of psychological treatments for depressive disorders: a systematic review. Psychol Med. 2014;44:1131-1146. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 178] [Cited by in RCA: 180] [Article Influence: 16.4] [Reference Citation Analysis (0)] |
| 12. | Degnan A, Baker S, Edge D, Nottidge W, Noke M, Press CJ, Husain N, Rathod S, Drake RJ. The nature and efficacy of culturally-adapted psychosocial interventions for schizophrenia: a systematic review and meta-analysis. Psychol Med. 2018;48:714-727. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 43] [Cited by in RCA: 50] [Article Influence: 7.1] [Reference Citation Analysis (0)] |
| 13. | Hernández Hernández ME, Waller G, Hardy G. Cultural adaptations of cognitive behavioural therapy for Latin American patients: unexpected findings from a systematic review. CBT. 2020;13:e57. [RCA] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 14. | Naeem F, Farooq S, Kingdon D. Cognitive behavioral therapy (brief vs standard duration) for schizophrenia. Schizophr Bull. 2014;40:958-959. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 15. | Rathod S, Phiri P, Harris S, Underwood C, Thagadur M, Padmanabi U, Kingdon D. Cognitive behaviour therapy for psychosis can be adapted for minority ethnic groups: a randomised controlled trial. Schizophr Res. 2013;143:319-326. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 95] [Cited by in RCA: 67] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 16. | Tseng WS. Culture and Psychotherapy: Review and Practical Guidelines. Transcul Psychiatry. 1999;36:131-179. [DOI] [Full Text] |
| 17. | Barrera M, Castro FG. A Heuristic Framework for the Cultural Adaptation of Interventions. Clin Psychol Sci Practice. 2006;13:311-316. [RCA] [DOI] [Full Text] [Cited by in Crossref: 147] [Cited by in RCA: 163] [Article Influence: 8.6] [Reference Citation Analysis (0)] |
| 18. | Castro FG, Barrera M Jr, Martinez CR Jr. The cultural adaptation of prevention interventions: resolving tensions between fidelity and fit. Prev Sci. 2004;5:41-45. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 715] [Cited by in RCA: 633] [Article Influence: 30.1] [Reference Citation Analysis (0)] |
| 19. | Domenech-Rodríguez M, Wieling E. Developing culturally appropriate, evidence-based treatments for interventions with ethnic minority populations. In: Rastogi M, Wieling E. Voices of color: First-person accounts of ethnic minority therapists. United States: Sage Publications, 2005: 313-333. |
| 20. | Kalibatseva Z, Leong FT. A critical review of culturally sensitive treatments for depression: recommendations for intervention and research. Psychol Serv. 2014;11:433-450. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 33] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 21. | Clark DM. Realizing the Mass Public Benefit of Evidence-Based Psychological Therapies: The IAPT Program. Annu Rev Clin Psychol. 2018;14:159-183. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 214] [Cited by in RCA: 276] [Article Influence: 39.4] [Reference Citation Analysis (0)] |
| 22. | Clark DM. Implementing NICE guidelines for the psychological treatment of depression and anxiety disorders: the IAPT experience. Int Rev Psychiatry. 2011;23:318-327. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 452] [Cited by in RCA: 449] [Article Influence: 32.1] [Reference Citation Analysis (0)] |
| 23. | Rathod S, Phiri P, Naeem F, Halvorsrud K, Bhui K. The importance of cultural adaptation of psychological interventions: Learning from UK experiences of IAP and CBT services. 2020. [cited 10 August 2022]. Available from: https://legacy.synergicollaborativecentre.co.uk/wp-content/uploads/2020/12/The-importance-of-cultural-adaptation-IAPT-and-CBT.pdf. |
| 24. | Beck A, Naz S, Brooks M, Jankowska M, Brooks-Ucheaga M. Improving Access to Psychological Therapies (IAPT) BLACK, ASIAN AND MINORITY ETHNIC SERVICE USER POSITIVE PRACTICE GUIDE 2019-long version. [cited 10 August 2022]. Available from: https://www.researchgate.net/publication/362017500_Improving_Access_to_Psychological_Therapies_IAPT_BLACK_ASIAN_AND_MINORITY_ETHNIC_SERVICE_USER_POSITIVE_PRACTICE_GUIDE_2019-long_version. |
| 25. | NHS Digital. Psychological Therapies: reports on the use of IAPT services, England, May 2022 Final including a report on the IAPT Employment. [cited 12 August 2022]. Available from: https://digital.nhs.uk/data-and-information/publications/statistical/psychological-therapies-report-on-the-use-of-iapt-services/may-2022-final-including-a-report-on-the-iapt-employment-advisers-pilot. |
| 26. | NHS Digital. Psychological Therapies: reports on the use of IAPT services, England January 2019 final including reports on the IAPT pilots. [cited 10 August 2022]. Available from: https://digital.nhs.uk/data-and-information/publications/statistical/psychological-therapies-report-on-the-use-of-iapt-services/january-2019-final-including-reports-on-the-iapt-pilots. |
| 27. | Lloyd M. Practical care planning for personalised mental health care. London: Open University Press, 2012. |
| 28. | NHS England. Universal personalised care: implementing the comprehensive model. [cited 10 August 2022]. Available from: https://www.england.nhs.uk/publication/universal-personalised-care-implementing-the-comprehensive-model/. |
| 29. | Bornman J, Sevcik RA, Romski M, Pae HK. Successfully Translating Language and Culture when Adapting Assessment Measures: Translating Assessment Measures. JPPID. 2010;7:111-118. [RCA] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 32] [Article Influence: 2.1] [Reference Citation Analysis (1)] |
| 30. | Tannenbaum M, Har E. Beyond basic communication: The role of the mother tongue in cognitive-behavioral therapy (CBT). Int J Bilingual. 2020;24:881-892. [DOI] [Full Text] |
| 31. | Rathod S, Kingdon D, Phiri P, Gobbi M. Developing culturally sensitive cognitive behaviour therapy for psychosis for ethnic minority patients by exploration and incorporation of service users' and health professionals' views and opinions. Behav Cogn Psychother. 2010;38:511-533. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 123] [Cited by in RCA: 79] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 32. | Rathod S, Kingdon D, Pinninti N, Turkington D, Phiri P. Cultural Adaptation of CBT for Serious Mental Illness: A Guide for Training and Practice. New York: John Wiley & Sons, 2015. |
| 33. | Naeem F, Phiri P, Rathod S, Kingdon D. Using CBT with diverse patients: Working with South Asian Muslims. In: Mueller M, Kennerley H, McManus F, Westbrook D. Oxford Guide to Surviving as a CBT Therapist (Oxford Guides to Cognitive Behavioural Therapy) 1st edition. New York: Oxford University Press, 2010. |
| 34. | Naeem F, Phiri P, Nasar A, Gerada A, Munshi T, Ayub M, Rathod S. An evidence-based framework for cultural adaptation of Cognitive Behaviour Therapy: Process, methodology and foci of adaptation. World Cultural Psychiatry Res Review. 2016;11:61-67. |
| 35. | Phiri P, Clarke I, Baxter L, Elliot K, Rathod S, Naeem F. Culture Free CBT for Diverse Groups. Vienna: Intechopen Publishers, 2021. |
| 36. | Carona C. The philosophical assumptions across the ‘three waves’ of cognitive–behavioural therapy: how compatible are they? BJPsych Advances. 2022;1-5. [RCA] [DOI] [Full Text] [Cited by in RCA: 5] [Reference Citation Analysis (0)] |
| 37. | Clarke I. Meeting mental breakdown mindfully - how to help the Comprehend, Cope and Connect way. United States: Routledge, 2021. |
| 38. | Hayes SC, Hofmann SG. The third wave of cognitive behavioral therapy and the rise of process-based care. World Psychiatry. 2017;16:245-246. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 267] [Cited by in RCA: 300] [Article Influence: 37.5] [Reference Citation Analysis (0)] |
| 39. | Greenfield BL, Roos C, Hagler KJ, Stein E, Bowen S, Witkiewitz KA. Race/ethnicity and racial group composition moderate the effectiveness of mindfulness-based relapse prevention for substance use disorder. Addict Behav. 2018;81:96-103. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 25] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 40. | Griffiths C, Williamson H, Zucchelli F, Paraskeva N, Moss T. A Systematic Review of the Effectiveness of Acceptance and Commitment Therapy (ACT) for Body Image Dissatisfaction and Weight Self-Stigma in Adults. J Contemp Psychother. 2018;48:189-204. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 31] [Cited by in RCA: 47] [Article Influence: 6.7] [Reference Citation Analysis (0)] |
| 41. | Tickell A, Ball S, Bernard P, Kuyken W, Marx R, Pack S, Strauss C, Sweeney T, Crane C. The Effectiveness of Mindfulness-Based Cognitive Therapy (MBCT) in Real-World Healthcare Services. Mindfulness (N Y). 2020;11:279-290. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 40] [Cited by in RCA: 38] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 42. | Laungani P. Asian Perspectives in Counselling and Psychotherapy. United States: Routledge, 2004. |
| 43. | Bullock J, Whiteley C, Moakes K, Clarke I, Riches S. Single-session Comprehend, Cope, and Connect intervention in acute and crisis psychology: A feasibility and acceptability study. Clin Psychol Psychother. 2021;28:219-225. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 44. | Clarke I, Nicholls H. Third Wave CBT Integration for Individuals and Teams: Comprehend, Cope and Connect. United States: Routledge, 2018. |
| 45. | Naeem F, Phiri P, Rathod S, Ayub M. Cultural adaptation of cognitive–behavioural therapy. BJPsych Advances. 2019;25:387-395. [RCA] [DOI] [Full Text] [Cited by in Crossref: 65] [Cited by in RCA: 35] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 46. | Ruef AM, Litz BT, Schlenger WE. Hispanic ethnicity and risk for combat-related posttraumatic stress disorder. Cultur Divers Ethnic Minor Psychol. 2000;6:235-251. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 61] [Cited by in RCA: 58] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 47. | Zigmond AS, Snaith RP. The hospital anxiety and depression scale. Acta Psychiatr Scand. 1983;67:361-370. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28548] [Cited by in RCA: 31806] [Article Influence: 757.3] [Reference Citation Analysis (0)] |
| 48. | Allan R, Martin CR. Can the Hospital Anxiety and Depression Scale be used in patients with schizophrenia? J Eval Clin Pract. 2009;15:134-141. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 12] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 49. | Bjelland I, Dahl AA, Haug TT, Neckelmann D. The validity of the Hospital Anxiety and Depression Scale. An updated literature review. J Psychosom Res. 2002;52:69-77. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6329] [Cited by in RCA: 7233] [Article Influence: 314.5] [Reference Citation Analysis (0)] |
| 50. | Mumford DB, Bavington JT, Bhatnagar KS, Hussain Y, Mirza S, Naraghi MM. The Bradford Somatic Inventory. A multi-ethnic inventory of somatic symptoms reported by anxious and depressed patients in Britain and the Indo-Pakistan subcontinent. Br J Psychiatry. 1991;158:379-386. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 154] [Cited by in RCA: 139] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 51. | World Health Organization. WHO Disability Assessment Schedule II (WHODAS 2.0). [cited 2 August 2022]. Available from: https://www.who.int/standards/classifications/international-classification-of-functioning-disability-and-health/who-disability-assessment-schedule. |
| 52. | Evans C, Connell J, Barkham M, Margison F, McGrath G, Mellor-Clark J, Audin K. Towards a standardised brief outcome measure: psychometric properties and utility of the CORE-OM. Br J Psychiatry. 2002;180:51-60. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 532] [Cited by in RCA: 512] [Article Influence: 22.3] [Reference Citation Analysis (0)] |
| 53. | NHS. Improving Access to Psychological Therapies (IAPT) Outcomes Toolkit 2008/9. [cited 2 August 2022]. Available from: http://ipnosis.postle.net/PDFS/iapt-outcomes-toolkit-2008-november(2).pdf. |
| 54. | Durrant C, Clarke I, Tolland A, Wilson H. Designing a CBT Service for an Acute In-patient Setting: A pilot evaluation study. Clin Psychol Psychotherapy. 2007;14:117-125. [RCA] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 21] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 55. | Araci D, Clarke I. Investigating the efficacy of a whole team, psychologically informed, acute mental health service approach. J Ment Health. 2017;26:307-311. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 56. | Paterson C, Karatzias T, Harper S, Dougall N, Dickson A, Hutton P. A feasibility study of a cross-diagnostic, CBT-based psychological intervention for acute mental health inpatients: Results, challenges, and methodological implications. Br J Clin Psychol. 2019;58:211-230. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 6] [Article Influence: 0.9] [Reference Citation Analysis (0)] |