Published online Aug 19, 2022. doi: 10.5498/wjp.v12.i8.1076
Peer-review started: March 19, 2022
First decision: April 18, 2022
Revised: April 20, 2022
Accepted: July 6, 2022
Article in press: July 6, 2022
Published online: August 19, 2022
Processing time: 151 Days and 19.8 Hours
In the post-pandemic era, the emergence of sporadic cases of coronavirus disease 2019 (COVID-19) and the scale of the pandemic are unpredictable. Therefore, the impact of sporadic cases of COVID-19 and isolation measures on mental health and sleep in different groups of people need to be analyzed.
To clarify the severity of psychological problems and insomnia of staff and community residents around a hospital with sporadic cases of COVID-19, and their relationship with quarantine location and long-term changes.
A cross-sectional survey was conducted on community residents and medical staff. Many of these medical staff had been subjected to different places of quarantine. Community residents did not experience quarantine. Hospital anxiety and depression scale (HADS), acute stress disorder scale (ASDS) and insomnia severity index (ISI) were used to evaluate anxiety and depression, acute stress disorder symptoms, and the severity of insomnia. Additionally, we conducted a 1-year follow-up study on medical staff, with related scales measurement immediately after and one year after the 2-wk quarantine period.
We included 406 medical staff and 226 community residents. The total scores of ISI and subscale in HADS of community residents were significantly higher than that of medical staff. Further analysis of medical staff who experienced quarantine showed that 134 were quarantined in hotels, 70 in hospitals and 48 at home. Among all subjects, the proportions of HADS, ASDS and ISI scores above normal cutoff value were 51.94%, 19.17% and 31.11%, respectively. Multivariable logistic regression analysis found that subjects with higher total ASDS scores had a greater risk to develop anxiety and depression. The total ISI score for medical staff in hotel quarantine was significantly higher than those in home quarantine. Total 199 doctors and nurses who completed the 1-year follow-up study. Compared with baseline, HADS and ASDS scores decreased significantly one year after the end of quarantine, while ISI scores did not change significantly.
Sporadic COVID-19 cases had a greater psychological impact on residents in surrounding communities, mainly manifested as insomnia and depressive symptoms. Hotel quarantine aggravated the severity of insomnia in medical staff, whose symptoms lasted ≥ 1 year.
Core Tip: This is the first study to research the severity of psychological problems and insomnia of medical staff and community residents around a hospital with sporadic coronavirus disease 2019 (COVID-19) cases, along with long-term changes in the post-pandemic era. We found that sporadic COVID-19 cases had a greater impact on mental health and sleep for community residents, and hotel quarantine had a higher risk for insomnia in doctors and nurses. The insomnia symptoms of doctors and nurses could last for ≥ 1 year. Therefore, our results indicate psychological and sleep problems after sporadic COVID-19 might need long-term mental and psychological intervention, especially for insomnia in doctors and nurses.
- Citation: Li XJ, Guo TZ, Xie Y, Bao YP, Si JY, Li Z, Xiong YT, Li H, Li SX, Lu L, Wang XQ. Cross-sectional survey following a longitudinal study on mental health and insomnia of people with sporadic COVID-19 . World J Psychiatry 2022; 12(8): 1076-1087
- URL: https://www.wjgnet.com/2220-3206/full/v12/i8/1076.htm
- DOI: https://dx.doi.org/10.5498/wjp.v12.i8.1076
Coronavirus disease 2019 (COVID-19)[1] is caused by severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2)[2] and was declared a public health emergency of international concern by the World Health Organization (WHO). According to the WHO report[3] by December 31, 2021, there were > 2.8 billion cases and > 5.4 million deaths worldwide. The number of new cases reported globally currently exceeds 135 million per day. It can be seen that the global outbreak of COVID-19 is still very serious.
The impact of the COVID-19 pandemic on mental health is expected to be immense and likely to be long-lasting worldwide[4,5]. The current COVID-19 pandemic may have psychological implications for many reasons[5]. Some of these reasons, including physical distance, fear of infection, inadequate information, stigma, quarantine measures, contribute to the pandemic and government responses[4,6,7]. China has adopted class A infectious disease prevention and control measures[8], which are also included in the management of quarantine for infectious diseases. That is, quarantine is needed not only for confirmed COVID-19 and suspected cases but also those who are in close contact. Quarantine measures urgently adopted to control the COVID-19 pandemic might have had negative psychological and social effects[6], such as senses of insecurity, shame, and hostility. Quarantine for COVID-19 often aggravates the above-mentioned mental and psychological reactions, and may cause anxiety, depression and suicide[9], and acute stress disorder (ASD) may appear[10,11], characterized by separation, avoidance, re-experience, and high alertness. The onset occurs within a few minutes or hours after the stress, and the symptoms usually do not exceed 1 mo. The results of a large-sample data study in China and worldwide suggest that the incidence of ASD among the public during the COVID-19 pandemic was 21.2% and 34.9%[12,13]. The long-term psychological impact of COVID-19 requires attention to the occurrence of post-traumatic stress disorder (PTSD)[14,15], which is characterized by repeated invasive traumatic experiences, avoidance behaviors, increased alertness symptoms, and even suicidal behaviors or psychoactive substances abuse.
With vaccination, various countries have adopted active prevention and control measures for COVID-19[16,17]. At present, the spread of COVID-19 in some countries and regions is mainly in the form of sudden and unpredictable disease and all types of people can be affected[4,5,16,17]. Although general hospitals do not admit patients with COVID-19 in China[8,18], compared with other locations, they are more likely to find cases of COVID-19. Therefore, in the post-pandemic era, the impact of sporadic cases of COVID-19 and isolation measures on mental health and sleep in different groups of people needs to be analyzed. This study focused on the psychological effects on hospital staff and surrounding community populations who reported patients with COVID-19, and the long-term impact on mental health and sleep for medical staff in the hospital.
Subjects included in this study were divided into two groups: medical staff from the hospital where patients with COVID-19 were found, and residents from the community surrounding the hospital. Some of the medical staff had adopted different forms of quarantine according to the degree of close contact with COVID-19 patients. Those who were close contacts were isolated in a hotel (could not leave the room); those who were close contacts of close contacts (secondary close contacts) were isolated in the hospital in single quarters (could not leave the room); and those who were general contacts were quarantined at home (could not leave home). Different quarantine places have different restrictions on the range of activities of the individual, and they also have different risks of infection and may have different psychological effects on the individual. Community residents had not experienced isolation measures. Participants in the follow-up survey were doctors and nurses who completed the baseline survey and a 1-year after survey.
The hospital anxiety and depression scale (HADS)[19] is used to assess the anxiety and depression symptoms of medical staff in general hospitals. There are 14 items in total, divided into two parts: the anxiety subscale (HADS-A) and the depression subscale (HADS-D). A total score of 0–7 is classified as asymptomatic, 8–10 as marginal/suspicious, and 11–21 as abnormal.
The acute stress disorder scale (ASDS)[20,21] is a self-rating scale, compiled according to the diagnostic criteria of the fourth edition of the Manual of Diagnosis and Statistics of Mental Disorders, used to assess acute stress disorder (ASD) symptoms and predict PTSD. ASDS contains 19 items, including the characteristics of screening for ASD, and can identify individuals with acute trauma who need an in-depth assessment of the risk of PTSD. Generally, 56 points are selected as the cutoff value for predicting PTSD by ASDS: dissociative symptom score ≥ 9 points, and other symptom score ≥ 28 points, and the diagnostic sensitivity of ASD is 0.95, specificity is 0.83, positive predictive power is 0.80, negative predictive power is 0.96, and validity is 0.87.
The insomnia severity index (ISI)[22] is a simple tool for screening insomnia, including seven items to assess the severity of sleep symptoms, satisfaction with sleep patterns, impact of the degree of insomnia on daily functions, awareness of the impact of insomnia on the subjects, and level of depression caused by sleep disorders. Total score of 0–7 points = insomnia without clinical significance; 8–14 points = subclinical insomnia; 15–21 points = clinical insomnia (moderate); and 22–28 points = clinical insomnia (severe).
A general survey questionnaire was designed to collect demographic data (gender, age, occupation), quarantine information, and subjectively describe the psychological reactions.
A cross-sectional survey was conducted on July 2, 2020, immediately after the quarantine was lifted, with participants who worked in a hospital with sporadic cases of COVID-19, and the surrounding community residents. HADS, ASDS and ISI were used to evaluate the anxiety and depression, ASD symptoms, and severity of insomnia. The general survey questionnaire was used to collect demographic information, quarantine information and psychological reactions.
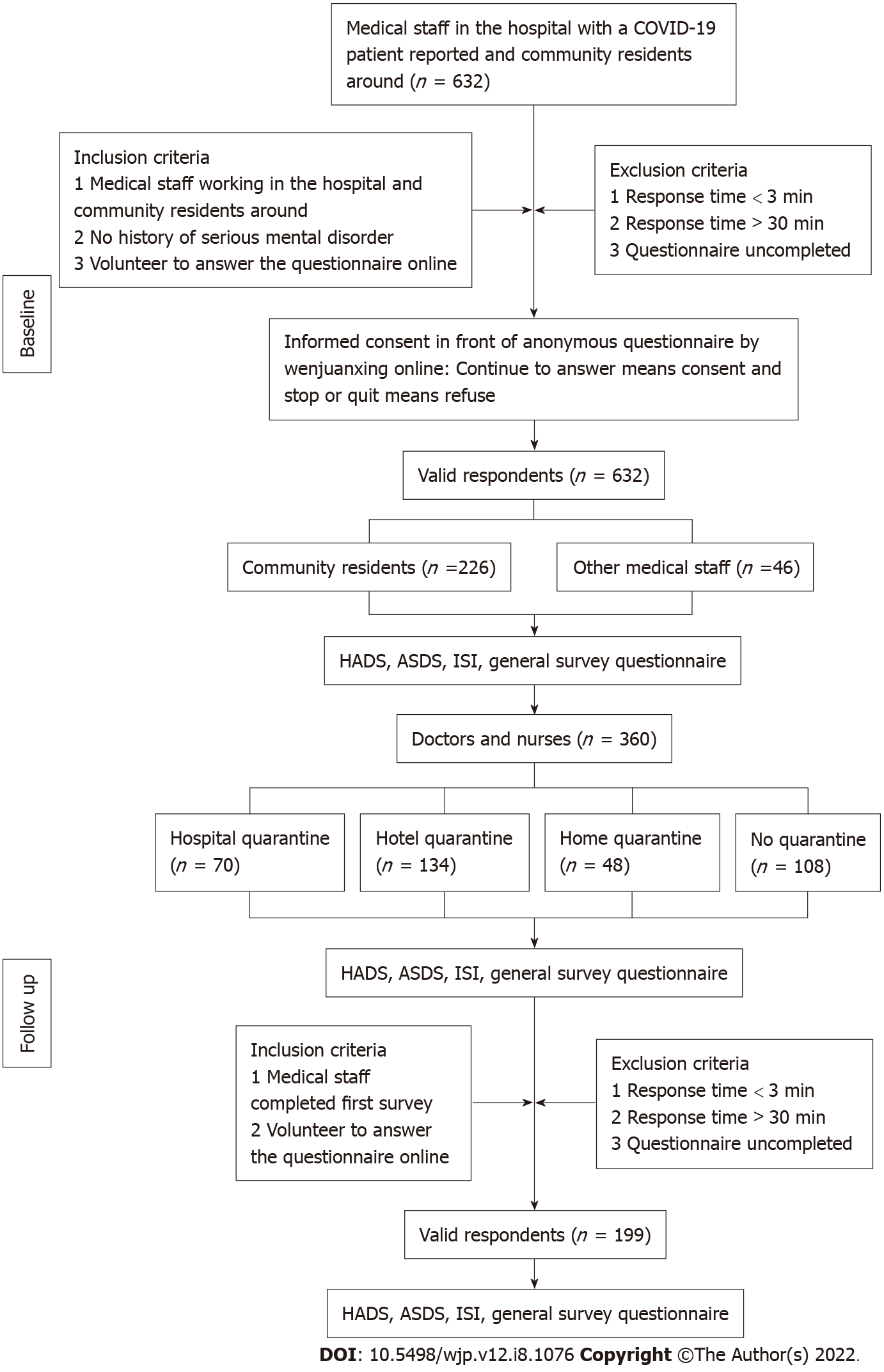
A follow-up longitudinal survey was conducted in May 2021, one year after quarantine, to clarify any changes in the psychological and insomnia symptoms of medical doctors and nurses (D&N group) that had a higher infection risk. The flow chart of the study is shown in Figure 1.
The Department of Psychological and Behavioral Medicine carried out a missionary style psychological crisis intervention to the entire population in the hospital during quarantine from June 18 to July 1, 2021. The research team provided targeted and layered psychological interventions for the medical staff, such as providing psychological crisis team contact information and providing psychological rescue support 24 h a day. The research team daily released audio, video and text content for relaxation, meditation and mindfulness therapy through a WeChat (a social media software) group in the hospital; provided contact information actively to the medical staff who were seeking help to carry out in-depth psychiatric evaluations; and provided psychological crisis intervention and treatment through remote diagnosis, treatment, or combined antianxiety and antidepressant medications when necessary. At the same time, the hospital immediately released pandemic prevention and control information and data updates until the end of quarantine. There were no new cases of COVID-19 reported throughout the quarantine.
The protocol was registered at clinicaltrials.gov with identification number NCT04978220.
We used independent t test, χ2 test, nonparametric Mann–Whitney U test, and Kruskal–Wallis test to compare the demographic characteristics at baseline, and scores of HADS, ASDS and ISI at baseline and at the end of 1-year follow up. The scores of the three scales were not all normally distributed and so are presented as medians with interquartile ranges. The ranked data, which were derived from the counts of each level for symptoms of depression, anxiety, stress and insomnia, were presented as numbers and percentages. To determine potential risk factors for symptoms of depression, anxiety, insomnia, and distress in participants, multivariable logistic regression analysis was performed to find the associations between risk factors and outcomes, and results presented as odds ratios (ORs) and 95%CIs.
Differences between medical staff and residents of surrounding community: Medical staff (n = 406), including doctors, nurses and other hospital staff, and residents of the surrounding community (n = 226) were recruited through questionnaires distributed online on their own will. The demographic data and scale scores were compared between medical staff and residents of the surrounding community (Table 1).
| Variable | Medical staff (n = 406) | Community residents (n = 226) | t/χ²/Z | P value |
| Age (yr), mean ± SD | 36.18 ± 8.83 | 41.54 ± 11.84 | 1.46 | 0.145 |
| Gender, n (%) | ||||
| Male | 70 (17.24) | 80 (35.40) | ||
| Female | 336 (82.76) | 146 (64.60) | 632 | 0.000 |
| Scale scores, median (range) | ||||
| HADS | 11 (4-35) | 12 (4-32) | -1.517 | 0.129 |
| HADS-A | 6 (2-18) | 7 (2-17) | -0.889 | 0.374 |
| HADS-D | 5 (1-20) | 5 (1-18) | -1.984 | 0.047 |
| ASDS | 28 (19-89) | 27 (19-76) | -0.439 | 0.66 |
| ISI | 4 (0-28) | 5 (0-28) | -2.05 | 0.040 |
The difference in total ISI scores between the two groups was significant (Z = 2.050, P = 0.040) and the severity of insomnia among medical staff was lower than that of residents in the surrounding community. Among the scores on the ISI scale (Mann–Whitney), the difference in daily function between the two groups was significant (Z = 3.332, P = 0.001).
There was no significant difference in the total HADS score between the two groups (Z = 1.517, P = 0.129). In HADS-D (Z = 1.984, P = 0.047), the score for the item of fidgeting (Z = 2.809, P = 0.005) was higher and the score for enjoyment of a good book/broadcast/program was lower (Z = 2.787, P = 0.005) in community residents than in medical staff. This meant that the depressive symptoms of community residents were significantly worse, and they showed more fidgeting and decreased ability to feel pleasure than the medical staff did. There was no significant difference in the HADS-A score between the two groups (Z = 0.889, P = 0.374).
There was no significant difference in the total ASDS score between the two groups (Z = 0.439, P = 0.660). However, the scores for each ASDS item in community residents showed a greater psychological impact on the subjective report (Z = 2.478, P = 0.013) and deeper fear of COVID-19 (Z = 2.821, P = 0.005) than the scores in medical staff.
Impact of different quarantine places on medical staff: To study the psychological and sleep effects of different quarantine places, we divided quarantined medical staff into the hospital group, hotel group, and home group according to the different quarantine measures. We did not find significant differences between each group for total HADS score (χ² = 0.319, P = 0.956), HADS-A score (χ² = 0.920, P = 0.821) and HADS-D score (χ² = 1.049, P = 0.789); total ASDS score (χ² = 0.528, P = 0.913); and total ISI score (χ² = 0.290, P = 0.407). Therefore, different quarantine places may have had no obvious influence on the anxiety and depression level, stress and insomnia in medical staff.
We further studied these quarantined doctors or nurses who had higher infection risk. There were 360 doctors or nurses. Among them, 252 experienced quarantine. These quarantined staff were divided into three subgroups according to the quarantine location: hospital single quarters (n = 70), hotel (n = 134) and home (n = 48). There was no significant difference in the HADS and ASDS scores (P > 0.05) among the three groups. There was a significant difference in total ISI scores between home and hotel quarantine (t = 0.691, P < 0.05), and the total ISI score for hotel quarantine was significantly higher than that of home quarantine (mean ± SE = 2.164 ± 0.960, 95%CI: 0.272–4.056, P = 0.025). For ISI items, severity of recent insomnia (e.g., in the past week) (χ² = 7.654, P = 0.022), difficulty in falling asleep (χ² = 6.793, P = 0.033), and difficulty staying asleep (χ² = 9.290, P = 0.010) were significantly higher in the hotel than home quarantine groups (Table 2).
| Variable | Groups based on quarantine site’s | χ² | P value | ||
| Hospital (n = 70) | Hotel (n = 134) | Home (n = 48) | |||
| ISI items | |||||
| Severity (1 + 2 + 3) | 1 (0, 9) | 2 (0, 12) | 1 (0, 9) | 7.654 | 0.022 |
| 1 Falling asleep | 0 (0, 3) | 0 (0, 4) | 0 (0, 4) | 6.793 | 0.033 |
| 2 Staying asleep | 0 (0, 3) | 0 (0, 4) | 0 (0, 3) | 9.29 | 0.010 |
| 3 Early awakening | 0 (0, 3) | 1 (0, 4) | 0 (0, 3) | 3.841 | 0.147 |
| 4 Satisfaction | 1 (0, 4) | 1 (0, 4) | 1 (0, 4) | 1.164 | 0.559 |
| 5 Interfere | 1 (0, 4) | 1 (0, 4) | 0.5 (0, 4) | 3.143 | 0.208 |
| 6 Noticeable | 1 (0, 4) | 1 (0, 4) | 0 (0, 3) | 4.293 | 0.117 |
| 7 Worried | 0 (0, 3) | 1 (0, 4) | 0 (0, 3) | 3.769 | 0.152 |
Subjective description of subjects: The main symptoms of the subjects were decreased interest, fear, anticipatory anxiety, akathisia, and decreased pleasure. According to response to the item “subjectively describe the content of psychological reactions” collected by the general survey questionnaire, the above-mentioned psychological reactions and symptoms were mainly due to the following reasons: (1) Worry about being infected; (2) Restricted activities in isolation, especially when being isolated, and worry about family members; (3) Worry about work; (4) Sudden notification of isolation, with no psychological preparation; (5) Worry about economic problems; and (6) Depressed mood for unstated reasons.
Risk factors for anxiety and depression in D&N group: Among medical staff, 187 with anxiety and depression were screened based on HADS score ≥ 11. Logistic regression analysis found that differences in age and total ASDS scores between subjects with anxiety and depression were significant (t = 2.858, P< 0.01 and t = 10.657, P < 0.01, respectively). Subjects with higher total ASDS scores (OR = 1.227, 95%CI: 1.17–1.29) had a greater risk of developing anxiety and depression, and young age (OR = 0.995, 95%CI: 0.93–0.99) was a protective factor.
Risk factors for insomnia in D&N group: Among medical staff, 112 subjects with insomnia were screened based on ISI score ≥ 8. Logistic regression analysis was performed to analyze the risk factors for insomnia during quarantine. The differences in total ASDS scores (t = 9.148, P < 0.01) and quarantine between those with and without insomnia (χ² = 7.895, P < 0.05) were significant. Subjects who experienced quarantine (OR = 2.799, 95%CI: 1.099–7.129) and subjects with higher total ASDS scores (OR = 1.195, 95%CI: 1.145–1.246) had a greater risk of insomnia.
To clarify the changes in psychological and insomnia symptoms of doctors or nurses who had a higher infection risk, we followed up them for one year. At baseline, 360 subjects (D&N group) completed the survey. The average age of the subjects was 35.79 ± 8.53 years, and 85.28% of them were women. One year later, 199 of 360 subjects, accounting for 55.28%, completed the whole study. There was no significant difference in age and gender for the subjects at the end point compared with baseline (Table 3).
| Variable | Baseline (n = 360) | Follow-up (n = 199) | t/χ²/Z | P value |
| Age (yr), mean ± SD | 35.79 ± 8.53 | 34.71 ± 7.80 | 1.46 | 0.145 |
| D&N group, n (%) | 360 (100) | 199 (100) | ||
| Gender, n (%) | ||||
| Male | 53 (14.72) | 22 (11.06) | ||
| Female | 307 (85.28) | 177 (88.94) | 1.483 | 0.223 |
| Scale scores, median (range) | ||||
| HADS | 11 (4-35) | 10 (0-33) | -3.923 | 0.000 |
| HADS-A | 6 (2-18) | 6 (0-19) | -4.469 | 0.000 |
| HADS-D | 4 (1-20) | 4 (0-16) | -3.286 | 0.001 |
| ASDS | 27.5 (19-89) | 26 (19-66) | -2.468 | 0.014 |
| ISI | 4 (0-28) | 5 (0-25) | -0.928 | 0.353 |
The percentages of those whose HADS, ASDS and ISI scores were above the cut-off value were 51.9%, 19.17% and 31.11%, respectively. After 1-year follow-up, the percentages for HADS and ASDS scores decreased, and ISI increased to 43.72%, 18.09%, and 32.16%, respectively, but the differences were not significant (χ² = 3.240, 0.097 and 0.065 respectively, P > 0.05).
Compared with baseline, the total HADS score was significantly lower (Z = 3.923, P < 0.01) after one year. The levels of anxiety and depression were both significantly lower than that at baseline (for HADS-A, Z = 4.469, P < 0.01; for HADS-D, Z = 3.286, P < 0.01). The total ASDS score also significantly decreased compared with that at baseline (Z = 2.468, P < 0.05), but the total ISI scores were not significantly different from those at baseline (Z = 0.928, P > 0.05) after one year (Table 3).
We further compared each item of the three scales between baseline and at the end of follow-up. The scores for items, such as “I enjoy the things I used to enjoy” (Z = 2.336, P < 0.05); “I get a sort of frightened feeling as if something awful is about to happen” (Z = 4.277, P <0.01); “I can sit at ease and feel relaxed” (Z = 12.771, P < 0.01); and “I can enjoy a good book or radio or TV program” (Z = 14.311, P < 0.01), in HADS were significantly reduced after one year. The scores for items, such as “Feeling frightened” (Z = 7.238, P < 0.01); “Sense of re-experiencing” (Z = 4.780, P < 0.01); and “Feeling more alert to danger” (Z = 2.173, P < 0.05), in ASDS were significantly reduced after one year. The scores for each item in ISI did not have a significant difference between baseline and the end of follow-up.
Our results showed that the psychological impact of COVID-19, such as depressive symptoms, on community residents was more obvious than that on medical staff. The main manifestations were restlessness and decreased ability to feel pleasure. The severity of insomnia in community residents was higher than that of medical staff. The main manifestations were impairment in daytime functions, such as daytime fatigue, ability to handle work and daily affairs, concentration, memory, and emotions. Because none of the community residents were quarantined, their depressive symptoms and the severity of insomnia were not directly related to quarantine. They might have been psychologically affected for the following reasons. They had been to the hospital for treatment, lived close to the hospital, or their family members were medical staff and they were worried that the medical staff may have been active in the community. Objectively speaking, the risk of COVID-19 infection among community residents who are not quarantined is less than that of medical staff. Therefore, although the difference in ASDS scores between the two groups was not significant, it could also explain the higher psychological reaction of community residents to acute stress.
The government has adopted various prevention and control measures to gradually return people’s life to normal[23]. However, the impact of sporadic COVID-9 cases[24] and the spread of variants[25] on people’s mental health and sleep in the post-pandemic era needs to be paid attention. In the post-pandemic era, government officials should also provide sufficient support, such as health education, open a psychological hotline for consultation, psychological and sleep evaluation, and any necessary treatment.
Among all subjects, we found higher levels of anxiety and depression among the doctors and nurses in the hospital, according to the HADS screening results, regardless of quarantine. The proportion of doctors and nurses reaching abnormal levels of anxiety and depression was 51.94%. This result is similar to that of the front-line healthcare workers in Wuhan[26]. It is also comparable to the internationally reported upper levels of anxiety and depression of medical staff (anxiety, 6.33%–50.9%; depression, 6.33%–50.9%)[11]. Although the screening tools used[27,28] differed from ours, subjective description of the psychological reactions also reflects that sporadic COVID-19 cases still have a negative impact on medical staff. It suggests that the situation needs to be evaluated in a timely manner and active countermeasures need to be taken.
This study showed that the different quarantine locations did not result in anxiety and depression, or acute stress symptoms in doctors and nurses who are in quarantine. Many studies have reported the negative emotions of medical staff caused by quarantine measures[9,29,30]. This may be because the pandemic prevention and control was at a stable stage when this study was carried out. The domestic pandemic prevention task is to control mainly sporadic and imported cases, and the prevention and control pressure is greatly reduced. At the same time, the mental state of the doctors and nurses in the hospital may also be one of the reasons. The experiences learned from the outbreak of the pandemic and confidence in domestic pandemic prevention[31] may also reduce the severity of symptoms such as anxiety, depression and acute stress.
We also found that higher total ASDS score were risk factors for anxious and depressive symptoms and young age was a protective factor; total ASDS scores and quarantine were risk factors for insomnia; and the different quarantine locations had a significant impact on the sleep of doctors and nurses. The severity of insomnia among doctors and nurses in those who were in hotel quarantine was greater than those who were in home quarantine. The main manifestation of insomnia was difficulty in falling asleep and in maintaining sleep. The unfamiliar and simple environment of the hotel did not bring comfort to the doctors and nurses who were experiencing emergencies, while in home quarantine, they could enjoy regular daily life in familiar places. In addition, those who were in home quarantine could directly seek emotional help or obtain support from the family. This is consistent with a study on the current status of social support for doctors and nurses under the COVID-19 pandemic[32], in which good family support enabled individuals to quickly adapt to changes in the environment when faced with emergencies in order to obtain positive emotional responses and social support.
After one year, the proportion of respondents who used HADS to screen for anxiety and depression decreased to 43.72%, and the total HADS score was also lower than that at baseline. However, the proportion of respondents with anxiety and depression was still higher than at baseline, although the symptoms were significantly reduced and the number of affected individuals had also decreased. There may have been a benefit from the reduction of COVID-19 infection risk, release from quarantine, return to work and family, and timely and effective mental and psychological intervention and treatment. However, it is necessary to pay attention to the long-term psychological effects of COVID-19 infection and the preventive measures on the hospital medical staff.
According to the results of ASDS assessment, we did not find any clear PTSD patients after 1-year follow-up. From the perspective of ASD, in the early stage of detection of COVID-19 infection cases, doctors and nurses showed typical symptoms: fear of COVID-19, anticipatory anxiety, and increased alertness[33]. Previous studies have reported that the general population[12] has similar stress symptoms and lower PTSD rate[14,34],which is in line with our findings. The time period from typical expression of acute stress symptoms after the discovery of sporadic COVID-19 to the improvement of related symptoms after 1-year follow-up showed a dynamic change in the psychological status of the medical staff in the hospital, and timely psychological crisis intervention was indispensable[35].
The insomnia symptoms of doctors and nurses had not improved along with improvement of their mental and psychological conditions after one year. This may be related to night shift work and the nature of work in the hospital. It suggests that concerns about the mental and psychological effects of the COVID-19 pandemic should be accompanied by concerns about insomnia symptoms among doctors and nurses because sleep status is inseparable from mental health[36].
This was a single-center study, and the subjective assessments of people might cause bias in the results. In the future, the multiple center study could be done in different places for comparison, and objective testing, such as polysomnography, could be used to obtain more objective insomnia parameters.
Sporadic cases of COVID-19 had a greater impact on residents in the surrounding community compared with hospital staff in the post-pandemic era, mainly manifested as insomnia and depression. The difference in quarantine location was an important factor affecting the severity of insomnia of doctors and nurses. Hotel quarantine aggravated the severity of insomnia of doctors and nurses. The early stage of sporadic COVID-19 cases appeared to have a significant impact on the mental health and sleep of doctors and nurses. Therefore, timely and effective psychological and behavioral intervention and treatment of insomnia symptoms, especially for those in hotel quarantine, is crucial. The long-term presence of insomnia symptoms in doctors and nurses should be paid high attention and be treated with positive intervention.
Coronavirus disease 2019 (COVID-19) is highly contagious and has a wide-ranging and serious impact on mental health. Although vaccination in some countries and regions has gradually restored people’s lives, the emergence of virus mutations and sporadic cases might persist in the long term and affect mental health and sleep.
There is a higher risk in general hospitals for COVID-19. The severity of psychological problems and insomnia of medical staff and community residents around a hospital with sporadic COVID-19 cases, and long-term changes in the post-pandemic period remain ambiguous. Additionally, the risk of COVID-19 and different quarantine locations among medical staff may affect doctors’ and nurses’ mental health and sleep. There have been few long-term follow-up studies about mental health and sleep in the post-pandemic era.
This study aimed to clarify the severity of psychological problems and insomnia of staff and community residents around a hospital with sporadic cases of COVID-19, and their relationship with quarantine location and long-term changes in the post-pandemic era.
Medical staff from the hospital where patients with COVID-19 were found, and residents from the community surrounding the hospital were included in the study. Rating scales were provided by wenjuanxing on the internet. SPSS version 18.0 was used to perform statistical analysis. The significance level was set at α = 0.05 and all tests were two-tailed.
In the cross-sectional study, 632 subjects were recruited, including 406 medical staff in the hospital that reported sporadic COVID-19 cases and 226 community residents in the surrounding area. The total insomnia severity index (ISI) scores and hospital anxiety and depression scale (HADS) scores were significantly higher in the community residents than in the medical staff. Among medical staff, there were 360 doctors and nurses and 252 of them were quarantined in different locations according to contact level with the patient. The total ISI score for medical staff in hotel quarantine was significantly higher than that in home quarantine. One year later, 199 doctors and nurses completed the follow-up study. The total HADS and acute stress disorder scale scores of doctors and nurses were decreased, but there was little change in ISI total score.
Our findings indicated that in the post-pandemic period, sporadic COVID-19 cases had a greater psychological impact on residents in the surrounding community than in hospital staff, and mainly manifested as insomnia and depressive symptoms. Doctors and nurses exposed to sporadic COVID-19 cases experienced anxiety and depression, stress, and insomnia in the early stage. Hotel quarantine means a higher risk of infection, and has a greater impact on doctors and nurses’ insomnia than home quarantine. One year later, the anxiety and depression of doctors and nurses significantly improved. However, the long-term mental and psychological problems should not be ignored, especially their insomnia symptoms.
Sporadic COVID-19 has a greater psychological effect on surrounding community residents than on hospital staff. Government officials should give them relevant support, such as health education. A psychological and sleep rating hotline for people living in surrounding communities and those quarantined in hotels should help. We suggest that effective measures should also be implemented to treat the long-term insomnia in doctors and nurses.
We would like to thank all the participants who were under investigation in the study. Many departments of Peking University International Hospital and Peking University Sixth Hospital gave sufficient management supports and wise advice during the study.
Provenance and peer review: Invited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Psychiatry
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): A
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Karnyoto AS, China; Nazari N, Iran S-Editor: Zhang H L-Editor: A P-Editor: Zhang H
| 1. | World Health Organization. Coronavirus disease (COVID-19) pandemic. Updates on the novel coronavirus 2019 outbreak up to August 7, 2021. [cited 8 August 2021]. Available from: https://www.who.int/emergencies/diseases/novel-coronavirus-2019. |
| 2. | Muralidar S, Ambi SV, Sekaran S, Krishnan UM. The emergence of COVID-19 as a global pandemic: Understanding the epidemiology, immune response and potential therapeutic targets of SARS-CoV-2. Biochimie. 2020;179:85-100. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 139] [Cited by in RCA: 167] [Article Influence: 33.4] [Reference Citation Analysis (0)] |
| 3. | World Health Organization. WHO Coronavirus (COVID-19) Dashboard. Updates on the novel coronavirus outbreak up to August 6, 2021. [cited 6 August 2021]. Available from: https://covid19.who.int/. |
| 4. | Bao Y, Sun Y, Meng S, Shi J, Lu L. 2019-nCoV epidemic: address mental health care to empower society. Lancet. 2020;395:e37-e38. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1076] [Cited by in RCA: 1009] [Article Influence: 201.8] [Reference Citation Analysis (0)] |
| 5. | Serafini G, Parmigiani B, Amerio A, Aguglia A, Sher L, Amore M. The psychological impact of COVID-19 on the mental health in the general population. QJM. 2020;. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 736] [Cited by in RCA: 618] [Article Influence: 123.6] [Reference Citation Analysis (1)] |
| 6. | Wang Y, Shi L, Que J, Lu Q, Liu L, Lu Z, Xu Y, Liu J, Sun Y, Meng S, Yuan K, Ran M, Lu L, Bao Y, Shi J. The impact of quarantine on mental health status among general population in China during the COVID-19 pandemic. Mol Psychiatry. 2021;26:4813-4822. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 129] [Cited by in RCA: 167] [Article Influence: 41.8] [Reference Citation Analysis (0)] |
| 7. | Al-Jabi SW. Current global research landscape on COVID-19 and depressive disorders: Bibliometric and visualization analysis. World J Psychiatry. 2021;11:253-264. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 24] [Cited by in RCA: 24] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 8. | NHCC (2020). "Bulletin 1 of National Health Commission of China (No. 1 of 2020)." Retrieved 20 Jan 2020. Available from: http://www.nhc.gov.cn/xcs/zhengcwj/202001/44a3b8245e8049d2837a4f27529cd386.shtml.9. |
| 9. | Brooks SK, Webster RK, Smith LE, Woodland L, Wessely S, Greenberg N, Rubin GJ. The psychological impact of quarantine and how to reduce it: rapid review of the evidence. Lancet. 2020;395:912-920. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9682] [Cited by in RCA: 8090] [Article Influence: 1618.0] [Reference Citation Analysis (1)] |
| 10. | Lin LY, Wang J, Ou-Yang XY, Miao Q, Chen R, Liang FX, Zhang YP, Tang Q, Wang T. The immediate impact of the 2019 novel coronavirus (COVID-19) outbreak on subjective sleep status. Sleep Med. 2021;77:348-354. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 110] [Cited by in RCA: 144] [Article Influence: 28.8] [Reference Citation Analysis (0)] |
| 11. | Xiong J, Lipsitz O, Nasri F, Lui LMW, Gill H, Phan L, Chen-Li D, Iacobucci M, Ho R, Majeed A, McIntyre RS. Impact of COVID-19 pandemic on mental health in the general population: A systematic review. J Affect Disord. 2020;277:55-64. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2424] [Cited by in RCA: 3008] [Article Influence: 601.6] [Reference Citation Analysis (0)] |
| 12. | Zheng YB, Shi L, Lu ZA, Que JY, Yuan K, Huang XL, Liu L, Wang YH, Lu QD, Wang Z, Yan W, Han Y, Sun XY, Bao YP, Shi J, Lu L. Mental Health Status of Late-Middle-Aged Adults in China During the Coronavirus Disease 2019 Pandemic. Front Public Health. 2021;9:643988. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 14] [Cited by in RCA: 25] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 13. | Ma Z, Zhao J, Li Y, Chen D, Wang T, Zhang Z, Chen Z, Yu Q, Jiang J, Fan F, Liu X. Mental health problems and correlates among 746 217 college students during the coronavirus disease 2019 outbreak in China. Epidemiol Psychiatr Sci. 2020;29:e181. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 269] [Cited by in RCA: 247] [Article Influence: 49.4] [Reference Citation Analysis (0)] |
| 14. | Sun L, Sun Z, Wu L, Zhu Z, Zhang F, Shang Z, Jia Y, Gu J, Zhou Y, Wang Y, Liu N, Liu W. Prevalence and risk factors for acute posttraumatic stress disorder during the COVID-19 outbreak. J Affect Disord. 2021;283:123-129. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 76] [Cited by in RCA: 94] [Article Influence: 23.5] [Reference Citation Analysis (0)] |
| 15. | Busch IM, Moretti F, Mazzi M, Wu AW, Rimondini M. What We Have Learned from Two Decades of Epidemics and Pandemics: A Systematic Review and Meta-Analysis of the Psychological Burden of Frontline Healthcare Workers. Psychother Psychosom. 2021;90:178-190. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 82] [Cited by in RCA: 124] [Article Influence: 31.0] [Reference Citation Analysis (0)] |
| 16. | Ma ZR, Idris S, Pan QW, Baloch Z. COVID-19 knowledge, risk perception, and information sources among Chinese population. World J Psychiatry. 2021;11:181-200. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 13] [Cited by in RCA: 11] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 17. | Pandey K, Thurman M, Johnson SD, Acharya A, Johnston M, Klug EA, Olwenyi OA, Rajaiah R, Byrareddy SN. Mental Health Issues During and After COVID-19 Vaccine Era. Brain Res Bull. 2021;176:161-173. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 75] [Cited by in RCA: 67] [Article Influence: 16.8] [Reference Citation Analysis (0)] |
| 18. | CNPC (2013). "Law of the People's Republic of China on Prevention and Control of Infectious Diseases." Bulletin of the Standing Committee of the National People's Congress of the People's Republic of China 4: 619-630. Available from: http://www.nhc.gov.cn/xcs/spbd/201308/b8438903163041b7bc9c071b07004220.shtml. |
| 19. | Smarr KL, Keefer AL. Measures of Depression and Depressive Symptoms. Arthritis Care Res (Hoboken). 2020;72 Suppl 10:608-629. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 35] [Article Influence: 7.0] [Reference Citation Analysis (0)] |
| 20. | Zhang C, Peng D, Lv L, Zhuo K, Yu K, Shen T, Xu Y, Wang Z. Individual Perceived Stress Mediates Psychological Distress in Medical Workers During COVID-19 Epidemic Outbreak in Wuhan. Neuropsychiatr Dis Treat. 2020;16:2529-2537. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 19] [Cited by in RCA: 17] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 21. | Bryant RA, Moulds ML, Guthrie RM. Acute Stress Disorder Scale: a self-report measure of acute stress disorder. Psychol Assess. 2000;12:61-68. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 269] [Cited by in RCA: 268] [Article Influence: 10.7] [Reference Citation Analysis (0)] |
| 22. | Morin CM, Belleville G, Bélanger L, Ivers H. The Insomnia Severity Index: psychometric indicators to detect insomnia cases and evaluate treatment response. Sleep. 2011;34:601-608. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1955] [Cited by in RCA: 3078] [Article Influence: 219.9] [Reference Citation Analysis (0)] |
| 23. | Eshun-Wilson I, Mody A, McKay V, Hlatshwayo M, Bradley C, Thompson V, Glidden DV, Geng EH. Public Preferences for Social Distancing Policy Measures to Mitigate the Spread of COVID-19 in Missouri. JAMA Netw Open. 2021;4:e2116113. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 10] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 24. | Nie A, Su X, Zhang S, Guan W, Li J. Psychological impact of COVID-19 outbreak on frontline nurses: A cross-sectional survey study. J Clin Nurs. 2020;29:4217-4226. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 115] [Cited by in RCA: 191] [Article Influence: 38.2] [Reference Citation Analysis (0)] |
| 25. | Luo M, Guo L, Yu M, Jiang W, Wang H. The psychological and mental impact of coronavirus disease 2019 (COVID-19) on medical staff and general public - A systematic review and meta-analysis. Psychiatry Res. 2020;291:113190. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 909] [Cited by in RCA: 957] [Article Influence: 191.4] [Reference Citation Analysis (0)] |
| 26. | Lai J, Ma S, Wang Y, Cai Z, Hu J, Wei N, Wu J, Du H, Chen T, Li R, Tan H, Kang L, Yao L, Huang M, Wang H, Wang G, Liu Z, Hu S. Factors Associated With Mental Health Outcomes Among Health Care Workers Exposed to Coronavirus Disease 2019. JAMA Netw Open. 2020;3:e203976. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5313] [Cited by in RCA: 4375] [Article Influence: 875.0] [Reference Citation Analysis (0)] |
| 27. | An Y, Yang Y, Wang A, Li Y, Zhang Q, Cheung T, Ungvari GS, Qin MZ, An FR, Xiang YT. Prevalence of depression and its impact on quality of life among frontline nurses in emergency departments during the COVID-19 outbreak. J Affect Disord. 2020;276:312-315. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 142] [Cited by in RCA: 182] [Article Influence: 36.4] [Reference Citation Analysis (0)] |
| 28. | Kahlon MK, Aksan N, Aubrey R, Clark N, Cowley-Morillo M, Jacobs EA, Mundhenk R, Sebastian KR, Tomlinson S. Effect of Layperson-Delivered, Empathy-Focused Program of Telephone Calls on Loneliness, Depression, and Anxiety Among Adults During the COVID-19 Pandemic: A Randomized Clinical Trial. JAMA Psychiatry. 2021;78:616-622. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 63] [Cited by in RCA: 111] [Article Influence: 27.8] [Reference Citation Analysis (0)] |
| 29. | Benke C, Autenrieth LK, Asselmann E, Pané-Farré CA. Lockdown, quarantine measures, and social distancing: Associations with depression, anxiety and distress at the beginning of the COVID-19 pandemic among adults from Germany. Psychiatry Res. 2020;293:113462. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 281] [Cited by in RCA: 351] [Article Influence: 70.2] [Reference Citation Analysis (0)] |
| 30. | Fernández RS, Crivelli L, Guimet NM, Allegri RF, Pedreira ME. Psychological distress associated with COVID-19 quarantine: Latent profile analysis, outcome prediction and mediation analysis. J Affect Disord. 2020;277:75-84. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 127] [Cited by in RCA: 148] [Article Influence: 29.6] [Reference Citation Analysis (0)] |
| 31. | Zhong BL, Luo W, Li HM, Zhang QQ, Liu XG, Li WT, Li Y. Knowledge, attitudes, and practices towards COVID-19 among Chinese residents during the rapid rise period of the COVID-19 outbreak: a quick online cross-sectional survey. Int J Biol Sci. 2020;16:1745-1752. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1814] [Cited by in RCA: 1364] [Article Influence: 272.8] [Reference Citation Analysis (0)] |
| 32. | Blake H, Bermingham F, Johnson G, Tabner A. Mitigating the Psychological Impact of COVID-19 on Healthcare Workers: A Digital Learning Package. Int J Environ Res Public Health. 2020;17. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 359] [Cited by in RCA: 316] [Article Influence: 63.2] [Reference Citation Analysis (0)] |
| 33. | Lin D, Friedman DB, Qiao S, Tam CC, Li X. Information uncertainty: a correlate for acute stress disorder during the COVID-19 outbreak in China. BMC Public Health. 2020;20:1867. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 25] [Cited by in RCA: 31] [Article Influence: 6.2] [Reference Citation Analysis (0)] |
| 34. | Tang W, Hu T, Hu B, Jin C, Wang G, Xie C, Chen S, Xu J. Prevalence and correlates of PTSD and depressive symptoms one month after the outbreak of the COVID-19 epidemic in a sample of home-quarantined Chinese university students. J Affect Disord. 2020;274:1-7. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 428] [Cited by in RCA: 473] [Article Influence: 94.6] [Reference Citation Analysis (0)] |
| 35. | Bäuerle A, Graf J, Jansen C, Musche V, Schweda A, Hetkamp M, Weismüller B, Dörrie N, Junne F, Teufel M, Skoda EM. E-mental health mindfulness-based and skills-based 'CoPE It' intervention to reduce psychological distress in times of COVID-19: study protocol for a bicentre longitudinal study. BMJ Open. 2020;10:e039646. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 29] [Cited by in RCA: 27] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 36. | Freeman D, Sheaves B, Goodwin GM, Yu LM, Nickless A, Harrison PJ, Emsley R, Luik AI, Foster RG, Wadekar V, Hinds C, Gumley A, Jones R, Lightman S, Jones S, Bentall R, Kinderman P, Rowse G, Brugha T, Blagrove M, Gregory AM, Fleming L, Walklet E, Glazebrook C, Davies EB, Hollis C, Haddock G, John B, Coulson M, Fowler D, Pugh K, Cape J, Moseley P, Brown G, Hughes C, Obonsawin M, Coker S, Watkins E, Schwannauer M, MacMahon K, Siriwardena AN, Espie CA. The effects of improving sleep on mental health (OASIS): a randomised controlled trial with mediation analysis. Lancet Psychiatry. 2017;4:749-758. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 350] [Cited by in RCA: 438] [Article Influence: 54.8] [Reference Citation Analysis (0)] |