Published online Aug 19, 2022. doi: 10.5498/wjp.v12.i8.1004
Peer-review started: March 11, 2022
First decision: April 18, 2022
Revised: April 28, 2022
Accepted: July 25, 2022
Article in press: July 25, 2022
Published online: August 19, 2022
Processing time: 159 Days and 23.6 Hours
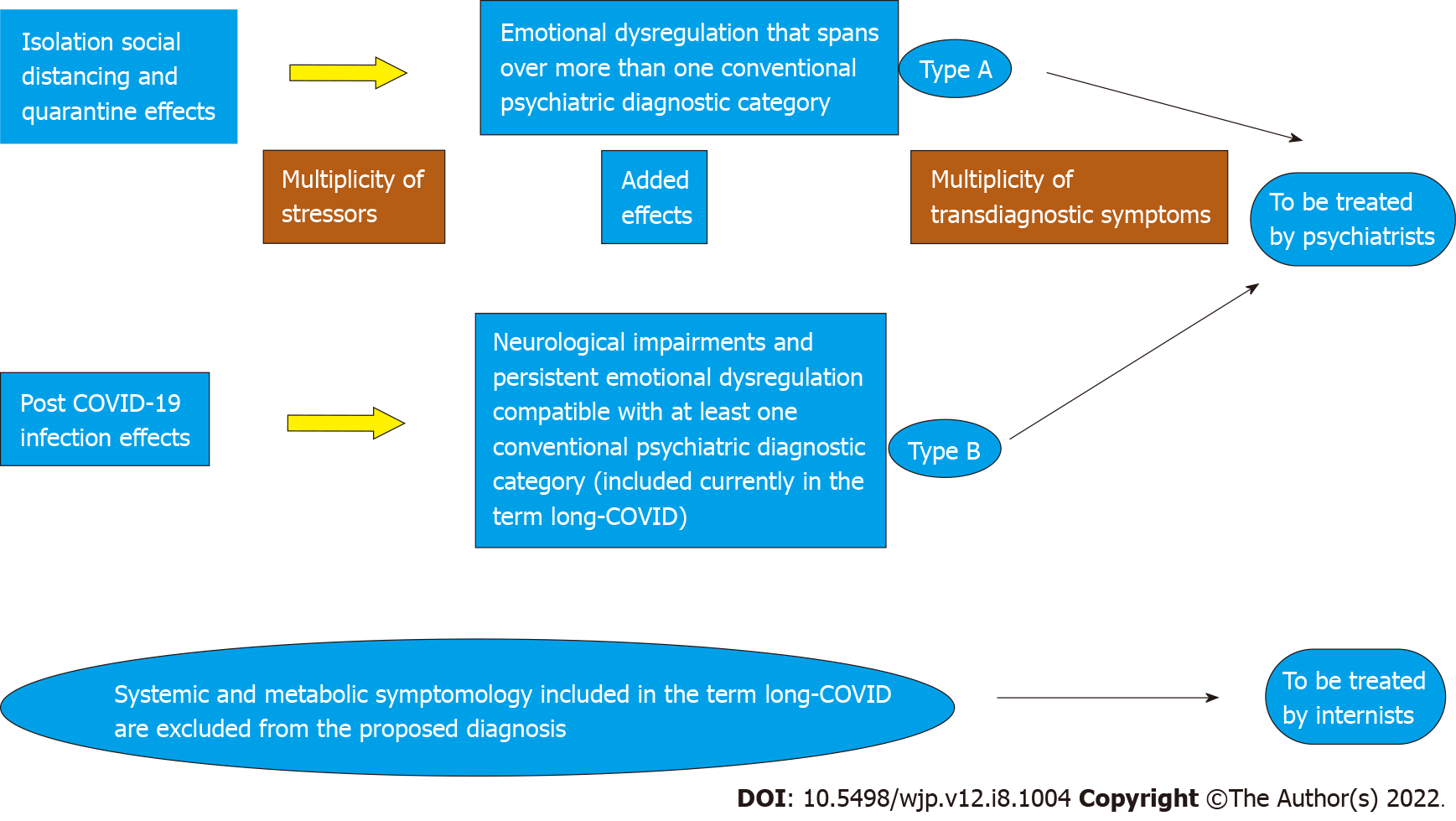
The clinical presentation that emerges from the extensive coronavirus disease 2019 (COVID-19) mental health literature suggests high correlations among many conventional psychiatric diagnoses. Arguments against the use of multiple comorbidities for a single patient have been published long before the pandemic. Concurrently, diagnostic recommendations for use of transdiagnostic considerations for improved treatment have been also published in recent years. In this review, we pose the question of whether a transdiagnostic mental health disease, including psychiatric and neuropsychiatric symptomology, has emerged since the onset of the pandemic. There are many attempts to identify a syndrome related to the pandemic, but none of the validated scales is able to capture the entire psychiatric and neuropsychiatric clinical presentation in infected and non-infected individuals. These scales also only marginally touch the issue of etiology and prevalence. We suggest a working hypothesis termed Complex Stress Reaction Syndrome (CSRS) representing a global psychiatric reaction to the pandemic situation in the general population (Type A) and a neuropsychiatric reaction in infected individuals (Type B) which relates to neurocognitive and psychiatric features which are part (excluding systemic and metabolic dysfunctions) of the syndrome termed in the literature as long COVID. We base our propositions on multidisciplinary scientific data regarding mental health during the global pandemic situation and the effects of viral infection reviewed from Google Scholar and PubMed between February 1, 2022 and March 10, 2022. Search in-clusion criteria were “mental health”, “COVID-19” and “Long COVID”, English language and human studies only. We suggest that this more comprehensive way of understanding COVID-19 complex mental health reactions may promote better prevention and treatment and serve to guide implementation of recommended administrative regulations that were recently published by the World Psychiatric Association. This review may serve as a call for an international investigation of our working hypothesis.
Core Tip: This Review asks a question shown in its title and hidden to date in the scientific literature on coronavirus disease 2019 (COVID-19) pandemic. It integrates the immense COVID-19 and long COVID literature on psychiatric and neuropsychiatric reactions to the pandemic in the general population. It also derives a working hypothesis on Type A and Type B of a hypothesized syndrome to be termed Complex Stress Reaction Syndrome. This working hypothesis is elaborated in the manuscript and supports the need to ask the transdiagnostic question in a timely manner based on a novel interdisciplinary and genuine integration of the relevant scientific literature.
- Citation: Goldstein Ferber S, Shoval G, Zalsman G, Weller A. Does COVID-19 related symptomatology indicate a transdiagnostic neuropsychiatric disorder? - Multidisciplinary implications. World J Psychiatry 2022; 12(8): 1004-1015
- URL: https://www.wjgnet.com/2220-3206/full/v12/i8/1004.htm
- DOI: https://dx.doi.org/10.5498/wjp.v12.i8.1004
Since the outbreak of the coronavirus disease 2019 (COVID-19) pandemic, increasing evidence revealed several psychiatric diagnoses suspected as being involved in the reaction of the general population to the pandemic and its related stressors. The majority of the studies investigated the comorbidity of depression and anxiety[1-4] and others added stress[5-9] and posttraumatic stress disorder (PTSD)[10-14]. However, many others found a significant incidence of other symptoms that are not clearly related to these comorbidities as outlined in the Diagnostic and Statistical Manual of Mental Disorders (DSM-5) and International Classification of Diseases (ICD-11): Latent infection phobia[15], OCD symptoms[16-19], somatization[20], health anxiety[19,21], internet gaming disorder[22,23], reports of repeated nightmares with virus-related narratives and intrusive thoughts, change in dream recall frequency[24], addictive social media use[25,26], thoughts of self-injury or suicide[27-31], emotional eating and binge eating[32], antisocial behavior, and substance abuse to relieve stress or boredom[33].
Thus, as the COVID-19 pandemic evolved, the psychiatric symptomatology reportedly progressed from single disorders to mixtures of diagnoses. These mixtures could be found even within the same patient, while a complex of symptoms derived from several diagnostic categories was found in many individuals[34-36]. This multiplicity of diagnoses is in accordance with the recent concern that multiple diagnoses are given to single patients and that the term “comorbidity” is excessively used, thus undermining treatment focus and prevention efforts[37].
A more accurate diagnosis could further reduce individual and organizational challenges, including, e.g., the risk for stigmatization[38]. It is of relevance also that the World Psychiatric Association produced an ethical protocol aimed at treatment of psychiatric patients during the COVID-19 era. This protocol is relevant for new patients and those with previous psychiatric diagnoses and for both infected and non-infected people[39]. However, how can we apply administrative regulations and provide and allocate appropriate treatment without an available accurate diagnosis? If changes are recommended, research efforts for a valid diagnosis are warranted.
In this review, we ask whether a new mental health disease has emerged since the onset of the pandemic, if its main characteristic is its transdiagnostic feature of symptomatology, and whether this new suspected syndrome may be related to the neuropsychiatric manifestation included in the general term “Long COVID”. This latter term contains neurological, psychiatric, and systemic symptoms in a manner which makes it difficult to differentiate for deriving appropriate treatment by different medical specialists.
An accurate diagnosis has always been the starting point for the development of appropriate psychotherapeutic and pharmacological treatments and for clinical trials examining their effectiveness. This developmental process within the professional field of psychiatry is expected to reach the identification of precise therapeutic components for further benefit of the diagnosed individuals. This potential for an accurate diagnosis may also emerge as the initial stage for the implementation of new institutional regulations for in- and out-patients with psychiatric reactions to the pandemic and with residual syndromes of the infection. It must be noted that accurate diagnosis has been only recently recognized as a professional need[40].
The psychiatric consequences of COVID-19 have been reported according to ICD or DSM illness codes in many studies to date. These studies have reported greater depression and anxiety levels compared to pre-pandemic prevalence of depressive- and anxiety-related syndromes[3,4]. Intolerance to uncertainty has been related to COVID-19 related anxieties due to the inherent uncertainty in the pandemic situation[41]. In addition, the literature reports on specific pandemic-related psychopathology. Several reports show that the severity of diverse symptoms across diagnostic categories are correlated during the pandemic and suggest that a link exists among these symptoms[17,42-45]. The reports of COVID-19 related symptoms evolved from single diagnostic categories to combinations of ICD-10 and DSM-5 diagnoses, often within a single patient, and altogether many individuals present a complex symptomatology across several diagnostic disorders[34-36]. The reports are worldwide and related to all ages, and includes even pregnant mothers[46].
Several tools have been suggested in the literature following investigation and validation for identifying a mental health disorder particular to the pandemic situation. Following research, construction, and validation of the COVID Stress Scales[47], Taylor et al[45] proposed COVID Stress Syndrome[45]. The main aspect of this syndrome is worry about the dangers of the pandemic with four additional concerns: (1) Worry regarding the impact of the pandemic on one’s personal socioeconomic situation; (2) Xenophobic worries regarding spread of the virus; (3) Nightmares or intrusive thoughts related to COVID-19; and (4) Compulsive checking and reassurance seeking. These researchers have also described a second set of beliefs, termed COVID-19 Disregard Syndrome. It is centered around the conviction that the viral threat is exaggerated. This belief is associated with disregard for social distancing, poor hand hygiene, and anti-vaccination attitude, also termed as “pandemic related adjustment”[33,48]. Persian[49], Turkish[50], and Singaporean versions[51] added to the overall vali-dation of the study in these cultures. Another transdiagnostic scale (containing 12 sub-scales) is the self-reported COVID-19 Pandemic Mental Health Questionnaire, which includes patterns of contamination anxiety, paranoid ideations, and several additional beliefs, behaviors, and sources of resilience[52]. The COV19-quality of life scale assesses quality of life regarding mental health[53]. The COVID-19 phobia scale measures “corona phobia”[15]. Multidimensional Assessment of COVID-19-Related Fears assess related concerns[54]. Another group has suggested two additional scales: The Coronavirus Anxiety Scale (CAS) and Fear of COVID-19 Scale[55-57]. This group demonstrated how the levels of anxiety and fear, measured by these scales, co-varied with gender, age, cohabitation status, educational levels, and the presence of positive cases or pandemic-related deaths. The CAS has been shown to have cross-cultural validity in 12 Latin American countries[58]. A different anxiety scale, validated in England, is the COVID-19 Anxiety Syndrome Scale[59]. In China, COVID-19 Related Psychological Distress has been assessed[60]. The COVID-19 Stressor Scale assesses stressor exposure and appraisal with demonstrated convergent and discriminant validity, from an online survey of a national sample (n = 437) in the United States[61]. Combined scales for anxiety, depression and stress also exist. However, neither of these versions distinguished patients diagnosed with depression and anxiety from each other or from other psychiatric conditions when studied during the COVID-19 quarantine period in Saudi Arabia[62]. A Chinese distress scale (used in a nationwide survey) is the COVID-19 Peritraumatic Distress Index[63]. Another approach to studying trauma in COVID-19 is to use the Impact of Event Scale with modifications for COVID-19[64].
The COVID-19 literature indicates high correlations among several symptoms in a manner that shows that the architecture of the pandemic-related mental health reactions spans over the conventional DSM-5/ICD-11 criteria[8,65]. A recent narrative review of the psychometric qualities of scales noted that the heterogeneous and insufficient description of methods used to assess the psychometric characteristics of these scales may limit their usefulness for clinical and research purposes[66]. A systematic review focusing on the quality of data collection addressing 37 relevant mental health cross-sectional surveys of the general public (average sample size = 5137) noted a high risk of selection bias[67].
Regarding etiology, there are limited data and research. Most of the studies assumed that the COVID situation is combined from different stressors but have not shown the personality structure covariance with a specific stressor or more than one stressor. Recently it had been mentioned that the investigation of stressors is a challenge because of the independence between different stressors when they impact the elicitation of a syndrome and because of their dependency on premorbid psychiatric conditions and earlier predispositions of personality traits[61,68]. Therefore, to date, we still do not know in a causative manner if the COVID-19 situation is a global source for a new psychiatric disorder or a transient stressful condition that should be dealt with from the level of personal coping perspective and coping accepted theories.
Another insufficiently studied issue is the mental health problems associated with the viral infection following recovery, often referred to as “long COVID”. The syndrome recognized as “long COVID” has been described with heterogeneous symptomatology, including psychiatric, neurological, and systemic symptoms[69-73]. These symptoms include loss of smell and/or taste, fatigue, cough, aching pain, “brain fog”, insomnia, shortness of breath, and tachycardia[74-78]. The prevalence of long COVID as found in modest and large samples is around 40% of recovering individuals with different manifestations and not necessarily with all symptoms in a patient[79]. A wide range of prevalence and of prevalence over time were reported for the different symptoms[74,80]. The syndrome has been recognized 12 wk to 6 mo following recovering from the acute COVID-19 infection[79,81].
The long COVID syndrome has been related to the identification of the COVID virus as a multi-organ infection with differential damages to each cell type in many organs[74,82,83]. The assumed underlying mechanisms are complex. They include dysregulation of mitochondria, which results in systemic decrease in metabolic activity and bioenergetics at the cellular level within the nervous system. The factors underlying brain fog may also produce additional pathogenic insults. It has been suggested that these pathological insults can progress to repetitive viral and bacterial propagation cycles[84]. The mental health symptoms have been suggested to be connected to increased susceptibility to infection due to a compromised immune system[84]. Others suggested a list of pathologies, i.e., production of inflammatory cytokines, cellular damage, and pro-coagulant state that underlie long-lasting COVID-19 symptomatology[85].
We suggest that mental health problems following recovery from COVID-19 infection result directly from damage to redox and antioxidative defenses of the cell, as well as the neural basis for the fatigue manifestation, which has been identified as the most common symptom included in the long COVID term[79,86-90]. This fatigue may be the basis for the cognitive impairment reported too. We note that the psychiatric components of long-COVID may be secondary effects of the immense fatigue and neurological symptom’s impact on emotional regulation and may not result from direct damage to neural cells. As there are conflicting results on the association of severity in the acute phase and the manifestation of long COVID syndrome, it is unclear whether there is one or more underlying mechanisms underlying this syndrome and whether there is a cascade of deteriorating effects of one or more cellular damages caused by the infection. There are only scarce research efforts to disentangle the long COVID syndrome from its psychiatric, neurological, and systemic components[28,82].
The pattern of findings appears mixed and inconsistent. While most studies reported more severe mental health disorders in infected compared to non-infected individuals, some studies did not reveal this pattern. Some representative findings from the majority of studies are as follows: (1) Prevalence of post-traumatic stress symptoms was more severe in COVID-19 survivors compared to healthy controls[91]; (2) Anxiety and depression were more prevalent in infected compared to non-infected people in a large Chinese sample[92]; (3) “Prevalence of stress, anxiety, depression, intrusion, hypervigilance, and avoidance among infected health care workers (HCWs) were significantly higher in comparison to non-infected HCWs”[93]; and (4) Suicidal ideation was more prevalent in infected vs non-infected individuals, in the United States[27]. Even months after recovery from the infection, depression, anxiety, and PTSD were prevalent[94]. In contrast, the prevalence of psychological distress among healthcare workers in Quebec was not associated with COVID infection status[95]. Furthermore, surprisingly, in a geriatric sample, the risk for depression symptoms was lower in infected (and recovering from COVID-19) individuals compared to non-infected controls[96]. A study using a different approach compared the transcriptome and data on immune factor transcription (from peripheral blood mononuclear cells) between infected patients and individuals with psychiatric disorders[97]. COVID-19 infected patients had a transcriptional profile prominently presenting inflammatory cytokine and interferon response genes, a profile fitting with a pro-inflammatory state. The authors also reported 39 dysregulated genes shared by COVID-19 and bipolar disorder, 22 shared with schizophrenia, and 19 with PTSD. The profile of the common genes is dominated by pro-inflammatory and cytokine factors. Finally, infected patients showed profiles of the peripheral (blood) immune system with considerable correspondence with those among the patients with the psychiatric conditions[97]. In a small sample of infected patients, a neuroradiological severity clinical index was correlated significantly with injury to the CNS (measures: Glial fibrillary acidic protein, total-tau, ubiquitin carboxyl-terminal hydrolase L1), and inflammation (C-reactive protein)[98]. A recent Cochrane review reported that stroke, paralysis, and altered mental status were the most frequent neurological disorders associated with COVID-19 infection[99]. The authors also suggested that COVID-19 could potentially induce new-onset of seizures, Guillain-Barre Syndrome, encephalitis, and other neurological disorders. Additionally, in a large sample of infected individuals, in 55% of the people at least one neurological symptom was observed; the prevalence was greater in people with high body mass index and older age[100]. In this study, headaches and loss of smell and taste were prevalent, while seizures and stroke were the least common neurological symptoms.
We conclude the following two risks based on this mixed clinical picture as it arises from the extensive COVID literature: (1) The COVID-19 situation is a multiple stressor condition posing risks to mental health in the general population; and (2) Being infected poses an additional neuropsychiatric risk, implying that the two risks should be investigated and dealt with from psychiatric and neuropsychiatric perspectives for better diagnosis and treatment.
COVID-19 has been shown to elicit transdiagnostic psychiatric symptomatology[65,101,102]. Beyond peripheral somatic effects, COVID-19 also affects the brain, as shown in neurocognitive impaired functions of recovering individuals. Therefore, we propose two sub-categories of this new perspective/syndrome. In principle, the two types are not mutually exclusive. Thus, we suggest including psychiatric and neuropsychiatric components in the newly suspected syndrome while excluding systemic and metabolic manifestations.
The first type is found in non-COVID-19 infected people, who present with psychopathology similar to that described above. We hypothesize that the etiology of this “Type A” follows exposure to pandemic stressors, including quarantine and social isolation, fear of infection, and both social and physical distancing. “Type B” is manifested in infected individuals. We suggest that it includes neurological and psychiatric characteristics which emerge from the resulting effects of the viral infection, e.g., coagulopathy-related strokes and cranial nerve injury[103], and sensory impairment[104,105]. It may be diagnosed as a part (excluding systemic and metabolic dysfunctions) of the heterogeneous syndrome, currently termed in the literature as long COVID.
It has been reported in a large sample (n = 84285) of COVID-19 infection survivors that those chronic neurocognitive impairments persisted, even when gender, age, racial-ethnic group, income, education level, and previously experienced medical conditions were considered. This study supported the authors’ conclusion that COVID-19-related symptoms are induced by the virus acting at multi-system levels, affecting the brain beyond the effects on other organs[106]. Bi-directional associations between psychiatric disorders and COVID-19 infection have been suggested, based on retrospective analysis of data from a large sample[107]. Specifically, survivors of COVID-19 infection presented an increased risk of psychiatric outcomes, and an existing psychiatric diagnosis was a risk factor for COVID-19 infection.
Thus, a clinical neurological evaluation is needed in addition to assessing psychopathology to provide a comprehensive clinical picture of COVID-19-related symptoms. The etiology of Type A is hypothesized to be linked to the multiplicity of COVID-19 situational stressors. The etiology of Type B is suggested to be mainly the consequence of the infection itself, including the neuropsychiatric effects of the virus. This approach may provide an overarching framework for future studies (see Figure 1).
In contrast to traditional diagnoses, mental disorders associated with COVID-19 are different as follows: (1) PTSD diagnosis includes exposure to a frightening stressor, resulting in nightmare and over-generalization to other situations. However, the COVID-19 reactions include extended exposure to complex stressors, diffused anxiety regarding infection and disease, without repeated nightmares, flashbacks or over-generalization as recently reported[47]; (2) Diagnosis of Adjustment Disorder rules out PTSD and bereavement, and it displays a short stressor to symptoms onset. In contrast, during COVID-19, several months may elapse before symptom onset; (3) Diagnosis of Acute Stress Disorder implies a simpler stressor and a specific symptom response. In contrast, the pandemic stressors and the pattern of response are complex, as detailed above; (4) Obsessional thoughts are ego-syntonic by definition. During the pandemic, fear of contamination and associated behaviors are justified by the objective situation (e.g., need for masks, extra hygienic guidelines, social distancing); the behaviors related to these guidelines are clearly not part defined by Obsessive Compulsive Disorder; (5) The criteria for defining Generalized Anxiety Disorder list excessive worrying (on diverse issues) and shifting back and forth among them. In contrast, COVID-19-related mental health reports include anxiety that is clearly related to the several pandemic-relevant stressors[47]; and (6) The diagnosis of Major Depression Disorder includes anhedonia, low affect, psychomotor agitation, unfitting guilt feelings, diminished drive and energy, trouble concentrating, and indecisiveness. Some of these symptoms, along with others, are to be found in COVID-19-related mental health reports. Future studies should address all these issues.
There is no agreement in the literature on the neuropsychiatric impacts of the pandemic on children, adolescents, and youth and especially on the prevalence of the post-infection syndrome termed long COVID[108-110]. According to available data, both psychiatric and neuropsychiatric effects are shown in young ages[110-112]. Regarding the elderly, a population with greater risk for infection and severe conditions, we suggest that premorbid psychiatric and neurological problems related to older ages may be involved in the older population’s reactions to the pandemic. Some reports support our transdiagnostic CSRS understanding, even in elderly[74,113].
Therefore, further studies are warranted to evaluate the applicability of our working hypothesis across the life span. As an elaboration of our working hypothesis, we suggest that on the axis between Type A and Type B of the proposed diagnosis, Type A may be more prevalent in younger ages, Type B may be more prevalent in older ages, and the variability in the incidence of Type A, Type B or both together may be greater during adulthood than in younger or older ages.
The clinical presentation of mental health symptomatology during the pandemic in infected and non-infected individuals implies many “comorbidities,” i.e., a transdiagnostic manifestation as arising from the literature. In the available diagnostic manuals, there are no transdiagnostic categories as yet, while the study of the mental health reactions to the pandemic shows such a pattern. Additionally, the suspected mental health disorder, as we suggest diagnosing it, implies the effect of multiplicity of co-occurring stressors, which result in a mixed clinical picture. Such a stress syndrome may be valid for post-pandemic days as well. Therefore, our outline for the suggested new diagnosis may be termed as CSRS, Type A, Type B. The validation of this hypothesis may relate the psychiatric and neuropsychiatric symptomatology to be treated by professional psychiatrists while other types of systemic and metabolic symptoms remain to be treated by internal medicine professionals (see Figure 1). This hypothesis has the potential to secure appropriate treatments for the suffering patients. This review may serve as a call for a meta-analysis and systematic reviews of the literature as well as for an international investigation of our working hypothesis.
The authors thank Megan Trow MA, for her considerable contribution to this manuscript.
Provenance and peer review: Invited article; Externally peer reviewed.
Peer-review model: Single blind
Corresponding Author’s Membership in Professional Societies: NIDCAP International, 054920673.
Specialty type: Psychiatry
Country/Territory of origin: Israel
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Radford-Smith DE, Australia; Seeman MV, Canada S-Editor: Wang JJ L-Editor: Filipodia P-Editor: Wang JJ
| 1. | Torrente F, Yoris A, Low D, Lopez P, Bekinschtein P, Vázquez GH, Manes F, Cetkovich M. Psychological symptoms, mental fatigue and behavioural adherence after 72 continuous days of strict lockdown during the COVID-19 pandemic in Argentina. BJPsych Open. 2022;8:e10. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 13] [Cited by in RCA: 7] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 2. | Boluarte-Carbajal A, Navarro-Flores A, Villarreal-Zegarra D. Explanatory Model of Perceived Stress in the General Population: A Cross-Sectional Study in Peru During the COVID-19 Context. Front Psychol. 2021;12:673945. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 15] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 3. | Hossain MM, Tasnim S, Sultana A, Faizah F, Mazumder H, Zou L, McKyer ELJ, Ahmed HU, Ma P. Epidemiology of mental health problems in COVID-19: a review. F1000Res. 2020;9:636. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 536] [Cited by in RCA: 558] [Article Influence: 111.6] [Reference Citation Analysis (0)] |
| 4. | Fiorillo A, Sampogna G, Giallonardo V, Del Vecchio V, Luciano M, Albert U, Carmassi C, Carrà G, Cirulli F, Dell'Osso B, Nanni MG, Pompili M, Sani G, Tortorella A, Volpe U. Effects of the lockdown on the mental health of the general population during the COVID-19 pandemic in Italy: Results from the COMET collaborative network. Eur Psychiatry. 2020;63:e87. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 208] [Cited by in RCA: 226] [Article Influence: 45.2] [Reference Citation Analysis (0)] |
| 5. | Pang NTP, James S, Giloi N, Rahim SSSA, Omar A, Jeffree MS, Hayati F, Lim MC, Kassim MAM, Ng JR. Relationships between Psychopathology, Psychological Process Variables, and Sociodemographic Variables and Comparison of Quarantined and Non-Quarantined Groups of Malaysian University Students in the COVID-19 Pandemic. Int J Environ Res Public Health. 2021;18. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 9] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 6. | Lopes AR, Nihei OK. Depression, anxiety and stress symptoms in Brazilian university students during the COVID-19 pandemic: Predictors and association with life satisfaction, psychological well-being and coping strategies. PLoS One. 2021;16:e0258493. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 28] [Cited by in RCA: 102] [Article Influence: 25.5] [Reference Citation Analysis (0)] |
| 7. | Ibar C, Fortuna F, Gonzalez D, Jamardo J, Jacobsen D, Pugliese L, Giraudo L, Ceres V, Mendoza C, Repetto EM, Reboredo G, Iglesias S, Azzara S, Berg G, Zopatti D, Fabre B. Evaluation of stress, burnout and hair cortisol levels in health workers at a University Hospital during COVID-19 pandemic. Psychoneuroendocrinology. 2021;128:105213. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 32] [Cited by in RCA: 48] [Article Influence: 12.0] [Reference Citation Analysis (0)] |
| 8. | Ma Z, Zhao J, Li Y, Chen D, Wang T, Zhang Z, Chen Z, Yu Q, Jiang J, Fan F, Liu X. Mental health problems and correlates among 746 217 college students during the coronavirus disease 2019 outbreak in China. Epidemiol Psychiatr Sci. 2020;29:e181. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 269] [Cited by in RCA: 245] [Article Influence: 49.0] [Reference Citation Analysis (0)] |
| 9. | Burke T, Berry A, Taylor LK, Stafford O, Murphy E, Shevlin M, McHugh L, Carr A. Increased Psychological Distress during COVID-19 and Quarantine in Ireland: A National Survey. J Clin Med. 2020;9. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 68] [Cited by in RCA: 52] [Article Influence: 10.4] [Reference Citation Analysis (0)] |
| 10. | Peng M, Song X, Liu L, Zhao W, Lai P, Bao G, Guo T, Zhang X. Comparison of Prevalence and Risk Factors of PTSS Between Chinese Patients With Depression and Non-depressed Controls During COVID-19 Outbreak. Front Psychiatry. 2021;12:719931. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 11. | Rossi R, Socci V, Talevi D, Niolu C, Pacitti F, Di Marco A, Rossi A, Siracusano A, Di Lorenzo G, Olff M. Trauma-spectrum symptoms among the Italian general population in the time of the COVID-19 outbreak. Eur J Psychotraumatol. 2021;12:1855888. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 20] [Cited by in RCA: 25] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 12. | Jiang W, Ren Z, Yu L, Tan Y, Shi C. A Network Analysis of Post-traumatic Stress Disorder Symptoms and Correlates During the COVID-19 Pandemic. Front Psychiatry. 2020;11:568037. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 19] [Cited by in RCA: 25] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 13. | Forte G, Favieri F, Tambelli R, Casagrande M. COVID-19 Pandemic in the Italian Population: Validation of a Post-Traumatic Stress Disorder Questionnaire and Prevalence of PTSD Symptomatology. Int J Environ Res Public Health. 2020;17. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 258] [Cited by in RCA: 234] [Article Influence: 46.8] [Reference Citation Analysis (0)] |
| 14. | Di Crosta A, Palumbo R, Marchetti D, Ceccato I, La Malva P, Maiella R, Cipi M, Roma P, Mammarella N, Verrocchio MC, Di Domenico A. Individual Differences, Economic Stability, and Fear of Contagion as Risk Factors for PTSD Symptoms in the COVID-19 Emergency. Front Psychol. 2020;11:567367. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 126] [Cited by in RCA: 110] [Article Influence: 22.0] [Reference Citation Analysis (0)] |
| 15. | Arpaci I, Karataş K, Baloğlu M. The development and initial tests for the psychometric properties of the COVID-19 Phobia Scale (C19P-S). Pers Individ Dif. 2020;164:110108. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 238] [Cited by in RCA: 149] [Article Influence: 29.8] [Reference Citation Analysis (0)] |
| 16. | Ji G, Wei W, Yue KC, Li H, Shi LJ, Ma JD, He CY, Zhou SS, Zhao Z, Lou T, Cheng J, Yang SC, Hu XZ. Effects of the COVID-19 Pandemic on Obsessive-Compulsive Symptoms Among University Students: Prospective Cohort Survey Study. J Med Internet Res. 2020;22:e21915. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 58] [Article Influence: 11.6] [Reference Citation Analysis (0)] |
| 17. | Abba-Aji A, Li D, Hrabok M, Shalaby R, Gusnowski A, Vuong W, Surood S, Nkire N, Li XM, Greenshaw AJ, Agyapong VIO. COVID-19 Pandemic and Mental Health: Prevalence and Correlates of New-Onset Obsessive-Compulsive Symptoms in a Canadian Province. Int J Environ Res Public Health. 2020;17. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 54] [Cited by in RCA: 78] [Article Influence: 15.6] [Reference Citation Analysis (1)] |
| 18. | Fontenelle LF, Albertella L, Brierley ME, Thompson EM, Destrée L, Chamberlain SR, Yücel M. Correlates of obsessive-compulsive and related disorders symptom severity during the COVID-19 pandemic. J Psychiatr Res. 2021;143:471-480. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 38] [Cited by in RCA: 33] [Article Influence: 8.3] [Reference Citation Analysis (0)] |
| 19. | Wheaton MG, Messner GR, Marks JB. Intolerance of uncertainty as a factor linking obsessive-compulsive symptoms, health anxiety and concerns about the spread of the novel coronavirus (COVID-19) in the United States. J Obsessive Compuls Relat Disord. 2021;28:100605. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 66] [Cited by in RCA: 61] [Article Influence: 15.3] [Reference Citation Analysis (0)] |
| 20. | Shangguan F, Zhou C, Qian W, Zhang C, Liu Z, Zhang XY. A Conditional Process Model to Explain Somatization During Coronavirus Disease 2019 Epidemic: The Interaction Among Resilience, Perceived Stress, and Sex. Front Psychol. 2021;12:633433. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 5] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 21. | Tyrer P. COVID-19 health anxiety. World Psychiatry. 2020;19:307-308. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 71] [Cited by in RCA: 65] [Article Influence: 13.0] [Reference Citation Analysis (0)] |
| 22. | Balhara YPS, Kattula D, Singh S, Chukkali S, Bhargava R. Impact of lockdown following COVID-19 on the gaming behavior of college students. Indian J Public Health. 2020;64:S172-S176. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 76] [Cited by in RCA: 85] [Article Influence: 17.0] [Reference Citation Analysis (0)] |
| 23. | Király O, Potenza MN, Stein DJ, King DL, Hodgins DC, Saunders JB, Griffiths MD, Gjoneska B, Billieux J, Brand M, Abbott MW, Chamberlain SR, Corazza O, Burkauskas J, Sales CMD, Montag C, Lochner C, Grünblatt E, Wegmann E, Martinotti G, Lee HK, Rumpf HJ, Castro-Calvo J, Rahimi-Movaghar A, Higuchi S, Menchon JM, Zohar J, Pellegrini L, Walitza S, Fineberg NA, Demetrovics Z. Preventing problematic internet use during the COVID-19 pandemic: Consensus guidance. Compr Psychiatry. 2020;100:152180. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 390] [Cited by in RCA: 355] [Article Influence: 71.0] [Reference Citation Analysis (0)] |
| 24. | Fränkl E, Scarpelli S, Nadorff MR, Bjorvatn B, Bolstad CJ, Chan NY, Chung F, Dauvilliers Y, Espie CA, Inoue Y, Leger D, Macêdo T, Matsui K, Merikanto I, Morin CM, Mota-Rolim S, Partinen M, Penzel T, Plazzi G, Sieminski M, Wing YK, De Gennaro L, Holzinger B. How our Dreams Changed During the COVID-19 Pandemic: Effects and Correlates of Dream Recall Frequency - a Multinational Study on 19,355 Adults. Nat Sci Sleep. 2021;13:1573-1591. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 33] [Cited by in RCA: 28] [Article Influence: 7.0] [Reference Citation Analysis (0)] |
| 25. | Gao J, Zheng P, Jia Y, Chen H, Mao Y, Chen S, Wang Y, Fu H, Dai J. Mental health problems and social media exposure during COVID-19 outbreak. PLoS One. 2020;15:e0231924. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1367] [Cited by in RCA: 1295] [Article Influence: 259.0] [Reference Citation Analysis (0)] |
| 26. | Brailovskaia J, Truskauskaite-Kuneviciene I, Margraf J, Kazlauskas E. Coronavirus (COVID-19) outbreak: Addictive social media use, depression, anxiety and stress in quarantine - an exploratory study in Germany and Lithuania. J Affect Disord Rep. 2021;5:100182. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 11] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 27. | DeVylder J, Zhou S, Oh H. Suicide attempts among college students hospitalized for COVID-19. J Affect Disord. 2021;294:241-244. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 11] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 28. | Donnelly SC. Post-COVID syndrome and suicide risk. QJM. 2021;114:81. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 29. | Zalsman G. Neurobiology of suicide in times of social isolation and loneliness. Eur Neuropsychopharmacol. 2020;40:1-3. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 11] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 30. | Zalsman G, Levy Y, Sommerfeld E, Segal A, Assa D, Ben-Dayan L, Valevski A, Mann JJ. Suicide-related calls to a national crisis chat hotline service during the COVID-19 pandemic and lockdown. J Psychiatr Res. 2021;139:193-196. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 16] [Cited by in RCA: 25] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 31. | Pirkis J, John A, Shin S, DelPozo-Banos M, Arya V, Analuisa-Aguilar P, Appleby L, Arensman E, Bantjes J, Baran A, Bertolote JM, Borges G, Brečić P, Caine E, Castelpietra G, Chang SS, Colchester D, Crompton D, Curkovic M, Deisenhammer EA, Du C, Dwyer J, Erlangsen A, Faust JS, Fortune S, Garrett A, George D, Gerstner R, Gilissen R, Gould M, Hawton K, Kanter J, Kapur N, Khan M, Kirtley OJ, Knipe D, Kolves K, Leske S, Marahatta K, Mittendorfer-Rutz E, Neznanov N, Niederkrotenthaler T, Nielsen E, Nordentoft M, Oberlerchner H, O'Connor RC, Pearson M, Phillips MR, Platt S, Plener PL, Psota G, Qin P, Radeloff D, Rados C, Reif A, Reif-Leonhard C, Rozanov V, Schlang C, Schneider B, Semenova N, Sinyor M, Townsend E, Ueda M, Vijayakumar L, Webb RT, Weerasinghe M, Zalsman G, Gunnell D, Spittal MJ. Suicide trends in the early months of the COVID-19 pandemic: an interrupted time-series analysis of preliminary data from 21 countries. Lancet Psychiatry. 2021;8:579-588. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 373] [Cited by in RCA: 434] [Article Influence: 108.5] [Reference Citation Analysis (0)] |
| 32. | López-Moreno M, López MTI, Miguel M, Garcés-Rimón M. Physical and Psychological Effects Related to Food Habits and Lifestyle Changes Derived from Covid-19 Home Confinement in the Spanish Population. Nutrients. 2020;12. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 144] [Cited by in RCA: 125] [Article Influence: 25.0] [Reference Citation Analysis (0)] |
| 33. | Taylor S, Paluszek MM, Rachor GS, McKay D, Asmundson GJG. Substance use and abuse, COVID-19-related distress, and disregard for social distancing: A network analysis. Addict Behav. 2021;114:106754. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 67] [Cited by in RCA: 137] [Article Influence: 34.3] [Reference Citation Analysis (0)] |
| 34. | Xiang YT, Yang Y, Li W, Zhang L, Zhang Q, Cheung T, Ng CH. Timely mental health care for the 2019 novel coronavirus outbreak is urgently needed. Lancet Psychiatry. 2020;7:228-229. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2288] [Cited by in RCA: 1882] [Article Influence: 376.4] [Reference Citation Analysis (0)] |
| 35. | Troyer EA, Kohn JN, Hong S. Are we facing a crashing wave of neuropsychiatric sequelae of COVID-19? Brain Behav Immun. 2020;87:34-39. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 665] [Cited by in RCA: 619] [Article Influence: 123.8] [Reference Citation Analysis (0)] |
| 36. | GBD 2017 Disease and Injury Incidence and Prevalence Collaborators. Global, regional, and national incidence, prevalence, and years lived with disability for 354 diseases and injuries for 195 countries and territories, 1990-2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. 2018;392:1789-1858. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9354] [Cited by in RCA: 8390] [Article Influence: 1198.6] [Reference Citation Analysis (4)] |
| 37. | Maj M. "Psychiatric comorbidity": an artefact of current diagnostic systems? Br J Psychiatry. 2005;186:182-184. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 170] [Cited by in RCA: 160] [Article Influence: 8.0] [Reference Citation Analysis (0)] |
| 38. | Kuzman MR, Curkovic M, Wasserman D. Principles of mental health care during the COVID-19 pandemic. Eur Psychiatry. 2020;63:e45. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 53] [Cited by in RCA: 59] [Article Influence: 11.8] [Reference Citation Analysis (0)] |
| 39. | Stewart DE, Appelbaum PS. COVID-19 and psychiatrists' responsibilities: a WPA position paper. World Psychiatry. 2020;19:406-407. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 96] [Cited by in RCA: 97] [Article Influence: 19.4] [Reference Citation Analysis (0)] |
| 40. | Trestman R, Waghray A. COVID 19: How the pandemic changed Psychiatry for good. Psychiatr Clin North Am. 2022;45:i. [RCA] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 41. | Goldstein Ferber S, Shoval G, Zalsman G, Mikulincer M, Weller A. Between Action and Emotional Survival During the COVID-19 era: Sensorimotor Pathways as Control Systems of Transdiagnostic Anxiety-Related Intolerance to Uncertainty. Front Psychiatry. 2021;12:680403. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 14] [Cited by in RCA: 7] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 42. | Attal JH, Lurie I, Neumark Y. A rapid assessment of migrant careworkers' psychosocial status during Israel's COVID-19 lockdown. Isr J Health Policy Res. 2020;9:61. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 15] [Cited by in RCA: 15] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 43. | Riello M, Purgato M, Bove C, MacTaggart D, Rusconi E. Prevalence of post-traumatic symptomatology and anxiety among residential nursing and care home workers following the first COVID-19 outbreak in Northern Italy. R Soc Open Sci. 2020;7:200880. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53] [Cited by in RCA: 52] [Article Influence: 10.4] [Reference Citation Analysis (0)] |
| 44. | Smith L, Jacob L, Yakkundi A, McDermott D, Armstrong NC, Barnett Y, López-Sánchez GF, Martin S, Butler L, Tully MA. Correlates of symptoms of anxiety and depression and mental wellbeing associated with COVID-19: a cross-sectional study of UK-based respondents. Psychiatry Res. 2020;291:113138. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 225] [Cited by in RCA: 241] [Article Influence: 48.2] [Reference Citation Analysis (0)] |
| 45. | Taylor S, Landry CA, Paluszek MM, Fergus TA, McKay D, Asmundson GJG. COVID stress syndrome: Concept, structure, and correlates. Depress Anxiety. 2020;37:706-714. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 345] [Cited by in RCA: 400] [Article Influence: 80.0] [Reference Citation Analysis (0)] |
| 46. | Vardi N, Zalsman G, Madjar N, Weizman A, Shoval G. COVID-19 pandemic: Impacts on mothers' and infants' mental health during pregnancy and shortly thereafter. Clin Child Psychol Psychiatry. 2022;27:82-88. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 12] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 47. | Taylor S, Landry CA, Paluszek MM, Fergus TA, McKay D, Asmundson GJG. Development and initial validation of the COVID Stress Scales. J Anxiety Disord. 2020;72:102232. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 547] [Cited by in RCA: 611] [Article Influence: 122.2] [Reference Citation Analysis (0)] |
| 48. | Taylor S, Landry CA, Paluszek MM, Rachor GS, Asmundson GJG. Worry, avoidance, and coping during the COVID-19 pandemic: A comprehensive network analysis. J Anxiety Disord. 2020;76:102327. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 93] [Cited by in RCA: 109] [Article Influence: 21.8] [Reference Citation Analysis (0)] |
| 49. | Khosravani V, Asmundson GJG, Taylor S, Sharifi Bastan F, Samimi Ardestani SM. The Persian COVID stress scales (Persian-CSS) and COVID-19-related stress reactions in patients with obsessive-compulsive and anxiety disorders. J Obsessive Compuls Relat Disord. 2021;28:100615. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 36] [Cited by in RCA: 50] [Article Influence: 12.5] [Reference Citation Analysis (0)] |
| 50. | Demirgöz Bal M, Dişsiz M, Bayri Bingöl F. Validity and Reliability of the Turkish Version of the COVID Stress Scale. J Korean Acad Nurs. 2021;51:525-536. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 6] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 51. | Ang CS, Das S/O A Sudha Ann Nancy AAELE. 'Dirty foreigners' are to blame for COVID-19: impacts of COVID stress syndrome on quality of life and gratitude among Singaporean adults. Curr Psychol. 2022;1-13. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 6] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 52. | Rek SV, Bühner M, Reinhard MA, Freeman D, Keeser D, Adorjan K, Falkai P, Padberg F. The COVID-19 Pandemic Mental Health Questionnaire (CoPaQ): psychometric evaluation and compliance with countermeasures in psychiatric inpatients and non-clinical individuals. BMC Psychiatry. 2021;21:426. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 13] [Cited by in RCA: 22] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 53. | Repišti S, Jovanović N, Kuzman MR, Medved S, Jerotić S, Ribić E, Majstorović T, Simoska SM, Novotni L, Milutinović M, Stoilkovska BB, Radojičić T, Ristić I, Zebić M, Pemovska T, Russo M. How to measure the impact of the COVID-19 pandemic on quality of life: COV19-QoL–the development, reliability and validity of a new scale. Glob Psychiatry. 2020;3:1-10. [DOI] [Full Text] |
| 54. | Schimmenti A, Starcevic V, Giardina A, Khazaal Y, Billieux J. Multidimensional Assessment of COVID-19-Related Fears (MAC-RF): A Theory-Based Instrument for the Assessment of Clinically Relevant Fears During Pandemics. Front Psychiatry. 2020;11:748. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 60] [Cited by in RCA: 60] [Article Influence: 12.0] [Reference Citation Analysis (0)] |
| 55. | Orrù G, Bertelloni D, Diolaiuti F, Conversano C, Ciacchini R, Gemignani A. A Psychometric Examination of the Coronavirus Anxiety Scale and the Fear of Coronavirus Disease 2019 Scale in the Italian Population. Front Psychol. 2021;12:669384. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 24] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 56. | Ahorsu DK, Lin CY, Imani V, Saffari M, Griffiths MD, Pakpour AH. The Fear of COVID-19 Scale: Development and Initial Validation. Int J Ment Health Addict. 2022;20:1537-1545. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2229] [Cited by in RCA: 1974] [Article Influence: 394.8] [Reference Citation Analysis (0)] |
| 57. | Lee SA. Coronavirus Anxiety Scale: A brief mental health screener for COVID-19 related anxiety. Death Stud. 2020;44:393-401. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 850] [Cited by in RCA: 796] [Article Influence: 159.2] [Reference Citation Analysis (0)] |
| 58. | Caycho-Rodríguez T, Valencia PD, Vilca LW, Carbajal-León C, Vivanco-Vidal A, Saroli-Araníbar D, Reyes-Bossio M, White M, Rojas-Jara C, Polanco-Carrasco R, Gallegos M, Cervigni M, Martino P, Palacios DA, Moreta-Herrera R, Samaniego-Pinho A, Lobos-Rivera ME, Figares AB, Puerta-Cortés DX, Corrales-Reyes IE, Calderón R, Tapia BP, Ferrari IF, Flores-Mendoza C. Cross-cultural validation of the new version of the Coronavirus Anxiety Scale in twelve Latin American countries. Curr Psychol. 2022;1-18. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 15] [Cited by in RCA: 11] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 59. | Nikčević AV, Spada MM. The COVID-19 anxiety syndrome scale: Development and psychometric properties. Psychiatry Res. 2020;292:113322. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 69] [Cited by in RCA: 95] [Article Influence: 19.0] [Reference Citation Analysis (1)] |
| 60. | Feng LS, Dong ZJ, Yan RY, Wu XQ, Zhang L, Ma J, Zeng Y. Psychological distress in the shadow of the COVID-19 pandemic: Preliminary development of an assessment scale. Psychiatry Res. 2020;291:113202. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 55] [Cited by in RCA: 53] [Article Influence: 10.6] [Reference Citation Analysis (0)] |
| 61. | Tambling RR, Russell BS, Park CL, Fendrich M, Hutchinson M, Horton AL, Tomkunas AJ. Measuring Cumulative Stressfulness: Psychometric Properties of the COVID-19 Stressors Scale. Health Educ Behav. 2021;48:20-28. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 29] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 62. | Ali AM, Alkhamees AA, Hori H, Kim Y, Kunugi H. The Depression Anxiety Stress Scale 21: Development and Validation of the Depression Anxiety Stress Scale 8-Item in Psychiatric Patients and the General Public for Easier Mental Health Measurement in a Post COVID-19 World. Int J Environ Res Public Health. 2021;18. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 44] [Cited by in RCA: 40] [Article Influence: 10.0] [Reference Citation Analysis (0)] |
| 63. | Qiu J, Shen B, Zhao M, Wang Z, Xie B, Xu Y. A nationwide survey of psychological distress among Chinese people in the COVID-19 epidemic: implications and policy recommendations. Gen Psychiatr. 2020;33:e100213. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2636] [Cited by in RCA: 2196] [Article Influence: 439.2] [Reference Citation Analysis (0)] |
| 64. | Vanaken L, Scheveneels S, Belmans E, Hermans D. Validation of the Impact of Event Scale With Modifications for COVID-19 (IES-COVID19). Front Psychiatry. 2020;11:738. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 48] [Cited by in RCA: 62] [Article Influence: 12.4] [Reference Citation Analysis (0)] |
| 65. | Rossi R, Socci V, Pacitti F, Di Lorenzo G, Di Marco A, Siracusano A, Rossi A. Mental Health Outcomes Among Frontline and Second-Line Health Care Workers During the Coronavirus Disease 2019 (COVID-19) Pandemic in Italy. JAMA Netw Open. 2020;3:e2010185. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 559] [Cited by in RCA: 537] [Article Influence: 107.4] [Reference Citation Analysis (0)] |
| 66. | Ransing R, Dashi E, Rehman S, Mehta V, Chepure A, Kilic O, Hayatudeen N, Orsolini L, Vahdani B, Adiukwu F, Gonzalez-Diaz JM, Larnaout A, Pinto da Costa M, Grandinetti P, Soler-Vidal J, Bytyçi DG, Shalbafan M, Nofal M, Pereira-Sanchez V, Ramalho R. COVID-19 related mental health issues: a narrative review of psychometric properties of scales and methodological concerns in scale development. Australas Psychiatry. 2021;29:326-332. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 2] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 67. | Lin YH, Chen CY, Wu SI. Efficiency and Quality of Data Collection Among Public Mental Health Surveys Conducted During the COVID-19 Pandemic: Systematic Review. J Med Internet Res. 2021;23:e25118. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 17] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 68. | Zhou P, Silverstein KA, Gao L, Walton JD, Nallu S, Guhlin J, Young ND. Detecting small plant peptides using SPADA (Small Peptide Alignment Discovery Application). BMC Bioinformatics. 2013;14:335. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 84] [Cited by in RCA: 79] [Article Influence: 6.6] [Reference Citation Analysis (0)] |
| 69. | Akbarialiabad H, Taghrir MH, Abdollahi A, Ghahramani N, Kumar M, Paydar S, Razani B, Mwangi J, Asadi-Pooya AA, Malekmakan L, Bastani B. Long COVID, a comprehensive systematic scoping review. Infection. 2021;49:1163-1186. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 224] [Cited by in RCA: 209] [Article Influence: 52.3] [Reference Citation Analysis (1)] |
| 70. | Buttery S, Philip KEJ, Williams P, Fallas A, West B, Cumella A, Cheung C, Walker S, Quint JK, Polkey MI, Hopkinson NS. Patient symptoms and experience following COVID-19: results from a UK-wide survey. BMJ Open Respir Res. 2021;8. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 16] [Cited by in RCA: 47] [Article Influence: 11.8] [Reference Citation Analysis (0)] |
| 71. | Kopanczyk R, Kumar N, Papadimos T. Post-Acute COVID-19 Syndrome for Anesthesiologists: A Narrative Review and a Pragmatic Approach to Clinical Care. J Cardiothorac Vasc Anesth. 2022;36:2727-2737. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 8] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 72. | Ortona E, Malorni W. Long COVID: to investigate immunological mechanisms and sex/gender related aspects as fundamental steps for tailored therapy. Eur Respir J. 2022;59. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 62] [Article Influence: 15.5] [Reference Citation Analysis (0)] |
| 73. | Aiyegbusi OL, Hughes SE, Turner G, Rivera SC, McMullan C, Chandan JS, Haroon S, Price G, Davies EH, Nirantharakumar K, Sapey E, Calvert MJ; TLC Study Group. Symptoms, complications and management of long COVID: a review. J R Soc Med. 2021;114:428-442. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 385] [Cited by in RCA: 527] [Article Influence: 131.8] [Reference Citation Analysis (0)] |
| 74. | Davis HE, Assaf GS, McCorkell L, Wei H, Low RJ, Re'em Y, Redfield S, Austin JP, Akrami A. Characterizing long COVID in an international cohort: 7 months of symptoms and their impact. EClinicalMedicine. 2021;38:101019. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1118] [Cited by in RCA: 1556] [Article Influence: 389.0] [Reference Citation Analysis (0)] |
| 75. | Vanichkachorn G, Newcomb R, Cowl CT, Murad MH, Breeher L, Miller S, Trenary M, Neveau D, Higgins S. Post-COVID-19 Syndrome (Long Haul Syndrome): Description of a Multidisciplinary Clinic at Mayo Clinic and Characteristics of the Initial Patient Cohort. Mayo Clin Proc. 2021;96:1782-1791. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 119] [Cited by in RCA: 125] [Article Influence: 31.3] [Reference Citation Analysis (0)] |
| 76. | Orrù G, Bertelloni D, Diolaiuti F, Mucci F, Di Giuseppe M, Biella M, Gemignani A, Ciacchini R, Conversano C. Long-COVID Syndrome? Healthcare (Basel). 2021;9. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 75] [Cited by in RCA: 75] [Article Influence: 18.8] [Reference Citation Analysis (0)] |
| 77. | Graham EL, Clark JR, Orban ZS, Lim PH, Szymanski AL, Taylor C, DiBiase RM, Jia DT, Balabanov R, Ho SU, Batra A, Liotta EM, Koralnik IJ. Persistent neurologic symptoms and cognitive dysfunction in non-hospitalized Covid-19 "long haulers". Ann Clin Transl Neurol. 2021;8:1073-1085. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 418] [Cited by in RCA: 451] [Article Influence: 112.8] [Reference Citation Analysis (0)] |
| 78. | Iwu CJ, Iwu CD, Wiysonge CS. The occurrence of long COVID: a rapid review. Pan Afr Med J. 2021;38:65. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 20] [Cited by in RCA: 19] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 79. | Jarrott B, Head R, Pringle KG, Lumbers ER, Martin JH. "LONG COVID"-A hypothesis for understanding the biological basis and pharmacological treatment strategy. Pharmacol Res Perspect. 2022;10:e00911. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 19] [Cited by in RCA: 74] [Article Influence: 24.7] [Reference Citation Analysis (0)] |
| 80. | Malik P, Patel K, Pinto C, Jaiswal R, Tirupathi R, Pillai S, Patel U. Post-acute COVID-19 syndrome (PCS) and health-related quality of life (HRQoL)-A systematic review and meta-analysis. J Med Virol. 2022;94:253-262. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 70] [Cited by in RCA: 363] [Article Influence: 90.8] [Reference Citation Analysis (0)] |
| 81. | Carod-Artal FJ. [Post-COVID-19 syndrome: epidemiology, diagnostic criteria and pathogenic mechanisms involved]. Rev Neurol. 2021;72:384-396. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 72] [Article Influence: 18.0] [Reference Citation Analysis (0)] |
| 82. | Schou TM, Joca S, Wegener G, Bay-Richter C. Psychiatric and neuropsychiatric sequelae of COVID-19 - A systematic review. Brain Behav Immun. 2021;97:328-348. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 126] [Cited by in RCA: 266] [Article Influence: 66.5] [Reference Citation Analysis (0)] |
| 83. | Kingstone T, Taylor AK, O'Donnell CA, Atherton H, Blane DN, Chew-Graham CA. Finding the 'right' GP: a qualitative study of the experiences of people with long-COVID. BJGP Open. 2020;4. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 151] [Cited by in RCA: 194] [Article Influence: 38.8] [Reference Citation Analysis (0)] |
| 84. | Tabacof L, Tosto-Mancuso J, Wood J, Cortes M, Kontorovich A, McCarthy D, Rizk D, Rozanski G, Breyman E, Nasr L, Kellner C, Herrera JE, Putrino D. Post-acute COVID-19 Syndrome Negatively Impacts Physical Function, Cognitive Function, Health-Related Quality of Life, and Participation. Am J Phys Med Rehabil. 2022;101:48-52. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 123] [Cited by in RCA: 206] [Article Influence: 68.7] [Reference Citation Analysis (0)] |
| 85. | Naeije R, Caravita S. Phenotyping long COVID. Eur Respir J. 2021;58. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 37] [Cited by in RCA: 71] [Article Influence: 17.8] [Reference Citation Analysis (0)] |
| 86. | Martín Giménez VM, de Las Heras N, Ferder L, Lahera V, Reiter RJ, Manucha W. Potential Effects of Melatonin and Micronutrients on Mitochondrial Dysfunction during a Cytokine Storm Typical of Oxidative/Inflammatory Diseases. Diseases. 2021;9. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 21] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 87. | Francisqueti-Ferron FV, Garcia JL, Ferron AJT, Nakandakare-Maia ET, Gregolin CS, Silva JPDC, Dos Santos KC, Lo ÂTC, Siqueira JS, de Mattei L, de Paula BH, Sarzi F, Silva CCVA, Moreto F, Costa MR, Ferreira ALA, Minatel IO, Corrêa CR. Gamma-oryzanol as a potential modulator of oxidative stress and inflammation via PPAR-y in adipose tissue: a hypothetical therapeutic for cytokine storm in COVID-19? Mol Cell Endocrinol. 2021;520:111095. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 21] [Cited by in RCA: 13] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 88. | Clough E, Inigo J, Chandra D, Chaves L, Reynolds JL, Aalinkeel R, Schwartz SA, Khmaladze A, Mahajan SD. Mitochondrial Dynamics in SARS-COV2 Spike Protein Treated Human Microglia: Implications for Neuro-COVID. J Neuroimmune Pharmacol. 2021;16:770-784. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 45] [Cited by in RCA: 49] [Article Influence: 12.3] [Reference Citation Analysis (0)] |
| 89. | Cumpstey AF, Clark AD, Santolini J, Jackson AA, Feelisch M. COVID-19: A Redox Disease-What a Stress Pandemic Can Teach Us About Resilience and What We May Learn from the Reactive Species Interactome About Its Treatment. Antioxid Redox Signal. 2021;35:1226-1268. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 28] [Article Influence: 7.0] [Reference Citation Analysis (0)] |
| 90. | Wood E, Hall KH, Tate W. Role of mitochondria, oxidative stress and the response to antioxidants in myalgic encephalomyelitis/chronic fatigue syndrome: A possible approach to SARS-CoV-2 'long-haulers'? Chronic Dis Transl Med. 2021;7:14-26. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 24] [Cited by in RCA: 64] [Article Influence: 12.8] [Reference Citation Analysis (0)] |
| 91. | Yuan Y, Liu ZH, Zhao YJ, Zhang Q, Zhang L, Cheung T, Jackson T, Jiang GQ, Xiang YT. Prevalence of Post-traumatic Stress Symptoms and Its Associations With Quality of Life, Demographic and Clinical Characteristics in COVID-19 Survivors During the Post-COVID-19 Era. Front Psychiatry. 2021;12:665507. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 19] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 92. | Lu X, Xie Y, Feng H, Liu Z, Ouyang K, Hou B, Wang M, Kong Z, Zhu Z, Dao W, Zhou Y, Cao J, Long J, Xu Y, Liu Y, Yin X. Psychological impact on COVID-19 patients during the outbreak in China: A case-control study. Psychiatry Res. 2021;305:114180. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 5] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 93. | Mohammadian Khonsari N, Shafiee G, Zandifar A, Mohammad Poornami S, Ejtahed HS, Asayesh H, Qorbani M. Comparison of psychological symptoms between infected and non-infected COVID-19 health care workers. BMC Psychiatry. 2021;21:170. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 23] [Cited by in RCA: 19] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 94. | Bonazza F, Borghi L, di San Marco EC, Piscopo K, Bai F, Monforte AD, Vegni E. Psychological outcomes after hospitalization for COVID-19: data from a multidisciplinary follow-up screening program for recovered patients. Res Psychother. 2020;23:491. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 12] [Cited by in RCA: 10] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 95. | Carazo S, Pelletier M, Talbot D, Jauvin N, De Serres G, Vézina M. Psychological Distress of Healthcare Workers in Québec (Canada) During the Second and the Third Pandemic Waves. J Occup Environ Med. 2022;64:495-503. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 10] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 96. | Naharci MI, Veizi BGY, Katipoglu B, Tasci I. Psychological Burden among Community-dwelling Older Adults with and without a History of a Recent Covid-19 Infection. Clin Gerontol. 2022;45:120-129. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 8] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 97. | Moni MA, Lin PI, Quinn JMW, Eapen V. COVID-19 patient transcriptomic and genomic profiling reveals comorbidity interactions with psychiatric disorders. Transl Psychiatry. 2021;11:160. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 19] [Cited by in RCA: 14] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 98. | Fällmar D, Rostami E, Kumlien E, Ashton NJ, Jackmann S, Pavel R, Blennow K, Hultström M, Lipcsey M, Frithiof R, Westman G, Zetterberg H, Wikström J, Virhammar J. The extent of neuroradiological findings in COVID-19 shows correlation with blood biomarkers, Glasgow coma scale score and days in intensive care. J Neuroradiol. 2021;. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 11] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 99. | Mohan N, Fayyaz MA, Del Rio C, Khurana NKRS, Vaidya SS, Salazar E, Joyce J, Ali AA. Neurological manifestations and neuroimaging findings in patients with SARS-CoV2-a systematic review. Egypt J Neurol Psychiatr Neurosurg. 2021;57:68. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 100. | Ashrafi F, Ommi D, Zali A, Khani S, Soheili A, Arab-Ahmadi M, Behnam B, Nohesara S, Semnani F, Fatemi A, Salari M, Jalili Khoshnood R, Vahidi M, Ayoobi-Yazdi N, Hosseini Toudeshki S, Sobhrakhshankhah E. Neurological Manifestations and their Correlated Factors in COVID-19 Patients; a Cross-Sectional Study. Arch Acad Emerg Med. 2021;9:e34. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
| 101. | Houben-Wilke S, Goërtz YM, Delbressine JM, Vaes AW, Meys R, Machado FV, van Herck M, Burtin C, Posthuma R, Franssen FM, Vijlbrief H, Spies Y, van 't Hul AJ, Spruit MA, Janssen DJ. The Impact of Long COVID-19 on Mental Health: Observational 6-Month Follow-Up Study. JMIR Ment Health. 2022;9:e33704. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 84] [Article Influence: 28.0] [Reference Citation Analysis (0)] |
| 102. | Herbert C, El Bolock A, Abdennadher S. How do you feel during the COVID-19 pandemic? BMC Psychol. 2021;9:90. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 18] [Cited by in RCA: 28] [Article Influence: 7.0] [Reference Citation Analysis (0)] |
| 103. | Helms J, Kremer S, Merdji H, Schenck M, Severac F, Clere-Jehl R, Studer A, Radosavljevic M, Kummerlen C, Monnier A, Boulay C, Fafi-Kremer S, Castelain V, Ohana M, Anheim M, Schneider F, Meziani F. Delirium and encephalopathy in severe COVID-19: a cohort analysis of ICU patients. Crit Care. 2020;24:491. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 238] [Cited by in RCA: 235] [Article Influence: 47.0] [Reference Citation Analysis (0)] |
| 104. | Parma V, Ohla K, Veldhuizen MG, Niv MY, Kelly CE, Bakke AJ, Cooper KW, Bouysset C, Pirastu N, Dibattista M, Kaur R, Liuzza MT, Pepino MY, Schöpf V, Pereda-Loth V, Olsson SB, Gerkin RC, Rohlfs Domínguez P, Albayay J, Farruggia MC, Bhutani S, Fjaeldstad AW, Kumar R, Menini A, Bensafi M, Sandell M, Konstantinidis I, Di Pizio A, Genovese F, Öztürk L, Thomas-Danguin T, Frasnelli J, Boesveldt S, Saatci Ö, Saraiva LR, Lin C, Golebiowski J, Hwang LD, Ozdener MH, Guàrdia MD, Laudamiel C, Ritchie M, Havlícek J, Pierron D, Roura E, Navarro M, Nolden AA, Lim J, Whitcroft KL, Colquitt LR, Ferdenzi C, Brindha EV, Altundag A, Macchi A, Nunez-Parra A, Patel ZM, Fiorucci S, Philpott CM, Smith BC, Lundström JN, Mucignat C, Parker JK, van den Brink M, Schmuker M, Fischmeister FPS, Heinbockel T, Shields VDC, Faraji F, Santamaría E, Fredborg WEA, Morini G, Olofsson JK, Jalessi M, Karni N, D'Errico A, Alizadeh R, Pellegrino R, Meyer P, Huart C, Chen B, Soler GM, Alwashahi MK, Welge-Lüssen A, Freiherr J, de Groot JHB, Klein H, Okamoto M, Singh PB, Hsieh JW; GCCR Group Author, Reed DR, Hummel T, Munger SD, Hayes JE. More Than Smell-COVID-19 Is Associated With Severe Impairment of Smell, Taste, and Chemesthesis. Chem Senses. 2020;45:609-622. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 252] [Cited by in RCA: 343] [Article Influence: 68.6] [Reference Citation Analysis (0)] |
| 105. | Özçelik Korkmaz M, Eğilmez OK, Özçelik MA, Güven M. Otolaryngological manifestations of hospitalised patients with confirmed COVID-19 infection. Eur Arch Otorhinolaryngol. 2021;278:1675-1685. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 54] [Cited by in RCA: 95] [Article Influence: 19.0] [Reference Citation Analysis (0)] |
| 106. | Hampshire A, Trender W, Chamberlain SR, Jolly AE, Grant JE, Patrick F, Mazibuko N, Williams SC, Barnby JM, Hellyer P, Mehta MA. Cognitive deficits in people who have recovered from COVID-19. EClinicalMedicine. 2021;39:101044. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 367] [Cited by in RCA: 348] [Article Influence: 87.0] [Reference Citation Analysis (0)] |
| 107. | Taquet M, Luciano S, Geddes JR, Harrison PJ. Bidirectional associations between COVID-19 and psychiatric disorder: retrospective cohort studies of 62 354 COVID-19 cases in the USA. Lancet Psychiatry. 2021;8:130-140. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 736] [Cited by in RCA: 943] [Article Influence: 235.8] [Reference Citation Analysis (0)] |
| 108. | Zimmermann P, Pittet LF, Curtis N. Long covid in children and adolescents. BMJ. 2022;376:o143. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 36] [Article Influence: 12.0] [Reference Citation Analysis (0)] |
| 109. | Stephenson T, Shafran R, De Stavola B, Rojas N, Aiano F, Amin-Chowdhury Z, McOwat K, Simmons R, Zavala M; Consortium C; Ladhani SN; CLoCk Consortium members. Long COVID and the mental and physical health of children and young people: national matched cohort study protocol (the CLoCk study). BMJ Open. 2021;11:e052838. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 78] [Cited by in RCA: 74] [Article Influence: 18.5] [Reference Citation Analysis (0)] |
| 110. | Esposito S, Principi N, Azzari C, Cardinale F, Di Mauro G, Galli L, Gattinara GC, Fainardi V, Guarino A, Lancella L, Licari A, Mancino E, Marseglia GL, Leonardi S, Nenna R, Zampogna S, Zona S, Staiano A, Midulla F. Italian intersociety consensus on management of long covid in children. Ital J Pediatr. 2022;48:42. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 38] [Cited by in RCA: 43] [Article Influence: 14.3] [Reference Citation Analysis (0)] |
| 111. | Goldman RD. Long COVID in children. Can Fam Physician. 2022;68:263-265. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 11] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 112. | Borel M, Xie L, Kapera O, Mihalcea A, Kahn J, Messiah SE. Long-term physical, mental and social health effects of COVID-19 in the pediatric population: a scoping review. World J Pediatr. 2022;18:149-159. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 21] [Cited by in RCA: 26] [Article Influence: 8.7] [Reference Citation Analysis (0)] |
| 113. | Cohen K, Ren S, Heath K, Dasmariñas MC, Jubilo KG, Guo Y, Lipsitch M, Daugherty SE. Risk of persistent and new clinical sequelae among adults aged 65 years and older during the post-acute phase of SARS-CoV-2 infection: retrospective cohort study. BMJ. 2022;376:e068414. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 45] [Cited by in RCA: 113] [Article Influence: 37.7] [Reference Citation Analysis (0)] |