Published online Jun 19, 2022. doi: 10.5498/wjp.v12.i6.801
Peer-review started: September 24, 2021
First decision: January 12, 2022
Revised: January 26, 2022
Accepted: May 14, 2022
Article in press: May 14, 2022
Published online: June 19, 2022
Processing time: 263 Days and 6.4 Hours
Test anxiety is prevalent among medical students and leads to impaired academic performance. Test-related attentional bias has been identified as an important maintaining factor in test-anxious individuals.
To evaluate whether hypnosis and progressive muscle relaxation (PMR) could modify medical college students’ test anxiety and attentional bias.
A total of 598 medical students were screened. The participants were divided into higher and lower test anxiety groups according to their scores on the test anxiety scale (TAS). Ninety medical college students with high TAS score were randomly assigned to a hypnosis or PMR group. Another 45 students with low TAS score were included, forming a baseline control group. The intervention was conducted weekly for 6 wk, and each session lasted approximately 30 min. The total intervention time and the number of intervention sessions for the hypnosis and PMR groups were equal. Data were collected at the pretest, posttest, and 2-mo follow-up.
Hypnosis group participants had a significantly lower TAS score at posttest (t = -21.827, P < 0.001) and at follow-up (t = -14.824, P < 0.001), compared to that at pretest. PMR group participants also had a significantly lower TAS score at posttest (t = -10.777, P < 0.001) and at follow-up (t = -7.444, P < 0.001), compared to that at pretest. At the posttest level, the hypnosis group had a significantly lower TAS score than the PMR group (t = -3.664, P < 0.001). At the follow-up level, the hypnosis group also had a significantly lower TAS score than the PMR group (t = -2.943, P = 0.004). Clinically significant improvement was found in both the hypnosis and PMR groups (hypnosis = 64.0%; PMR = 62.22%). Hypnosis was more effective than PMR in reducing test anxiety among medical college students. Hypnosis could modify attentional bias toward threatening stimuli, but PMR could not.
These results suggest that attentional bias plays an important role in test anxiety treatment.
Core Tip: We wanted to explore whether hypnosis and progressive muscle relaxation (PMR) could modify medical college students’ test anxiety and related attentional bias toward threatening stimuli. We found that hypnosis was more effective than PMR in reducing test anxiety in medical students, and hypnosis could modify attentional bias toward threatening stimuli, but PMR could not. These results suggest that attentional bias plays an important role in the treatment of test anxiety.
- Citation: Zhang Y, Yang XX, Luo JY, Liang M, Li N, Tao Q, Ma LJ, Li XM. Randomized trial estimating effects of hypnosis versus progressive muscle relaxation on medical students’ test anxiety and attentional bias. World J Psychiatry 2022; 12(6): 801-813
- URL: https://www.wjgnet.com/2220-3206/full/v12/i6/801.htm
- DOI: https://dx.doi.org/10.5498/wjp.v12.i6.801
Medical education has always been regarded by students as a high-pressure environment[1], and the incidence rate of test anxiety among medical students is 25%-56%[2]. Research has demonstrated a series of adverse effects associated with test anxiety, such as impaired academic achievement and mental health problems[3,4]. Test anxiety comprises two interdependent factors: Emotionality (or physiology) and worry (or cognition)[5,6]. Emotionality, or physiology, involves awareness of physiological arousal associated with test situations: Increased heart rate, perspiration, muscle tension, and blood pressure[7]. Worry, or cognition, is a psychological phenomenon related to the overwhelming distress associated with testing situations[8].
There are different interventions for test anxiety that target either emotionality or cognition. For instance, progressive muscle relaxation (PMR) is a common behavioral approach to easing physiological reactivity to test situations. PMR targets emotionality/physiology rather than worry/cognition[9]. Several studies have suggested that PMR effectively reduces test anxiety in students[9,10]. Cognitive methods, on the other hand, aim at reducing the psychological detriments of test anxiety[11]. A recent study provided evidence for the utility of integrating integrated imagery work with cognitive-behavioral therapy for treating test anxiety[12]. Recently, a meta-analysis of the efficacy of interventions for test-anxious university students found that although interventions were superior to control conditions in reducing test anxiety, overall confidence should be tempered. The authors concluded that other psychological interventions for test anxiety are needed in future studies[13].
Hypnosis is “a state of consciousness involving focused attention and reduced peripheral awareness characterized by an enhanced capacity for response to suggestion”[14]. There are different types of hypnosis, i.e., waking or active-alert[15]. The present study employed the traditional definition of hypnosis. Hypnosis is a rapid and cost-effective intervention for anxiety and anxiety-related disorders[16]. During a hypnotic induction phase, a state of relaxation can be induced by maintaining eye fixation, following suggestions of calmness, closing the eyes, and imagery. A core component of hypnosis seems to involve facilitating a state of focused attention in a suggested direction that supports emotional well-being[17]. We therefore proposed that both the relaxation and cognitive components of hypnosis can make it effective in reducing test anxiety.
Attentional bias is believed to be associated with the onset and maintenance of anxiety[18]. Its effect is that anxious individuals tend to direct their attention toward and maintain attentional focus on threat-related stimuli, at the expense of attending to other more critical stimuli in the environment[19]. The same is true for test anxiety; highly test-anxious individuals demonstrate an attentional bias to threat and test-related information[20,21]. Recent research has shown that experimentally manipulating attentional bias away from a threat is effective for the individuals preparing for an exam[22]. Hypnosis also can treat individuals with test anxiety by modifying their attentional bias via hypnotic suggestion. For example, the participants received hypnotic suggestions to remain calm and relaxed when they received information related to the exam or got to the situation related to the exam. Further, they could no longer fixate their attention on the information. That is, they could no longer have attentional bias toward the information.
According to attention theory, visual memory is closely related to attentional bias[23], and attentional bias may reflect facilitated orienting of attention to negative information or slowed attentional disengagement from negative information[24]. Although various experimental paradigms have been used to evaluate attentional bias, most of them have not been able to differentiate its two mechanisms[9]. A recently-developed odd-one-out visual search task seems to have uncovered the specific processes underlying attentional bias[25]. In this paradigm, participants were presented with a matrix of stimuli and asked whether the matrix included one stimulus from a different category. The anxious participants demonstrated speeded detection of and slowed disengagement from the threatening stimuli[25].
Attentional bias may be considered an essential target in treating test anxiety. This study was designed as a pilot randomized clinical trial comparing the effects of hypnosis to PMR for test anxiety and the associated attentional bias. The hypnosis developed by this study was intended to target the two components of test anxiety: Emotionality/physiology and worry/cognition, while the PMR targeted only emotionality/physiology. PMR involves the voluntary stretching and relaxing of large muscle groups[26]. We hypothesized that both hypnosis and PMR would reduce anxiety symptoms. Yet, only hypnosis participants demonstrated a significant change in attentional bias to test-related stimuli, compared with those receiving PMR. To the best of our knowledge, this study is the first to use hypnosis to help individuals reduce test anxiety and attentional bias toward threatening stimuli. This is also the first study to use PMR to reduce attentional bias in students, although several studies have found that PMR effectively reduces test anxiety[10,27].
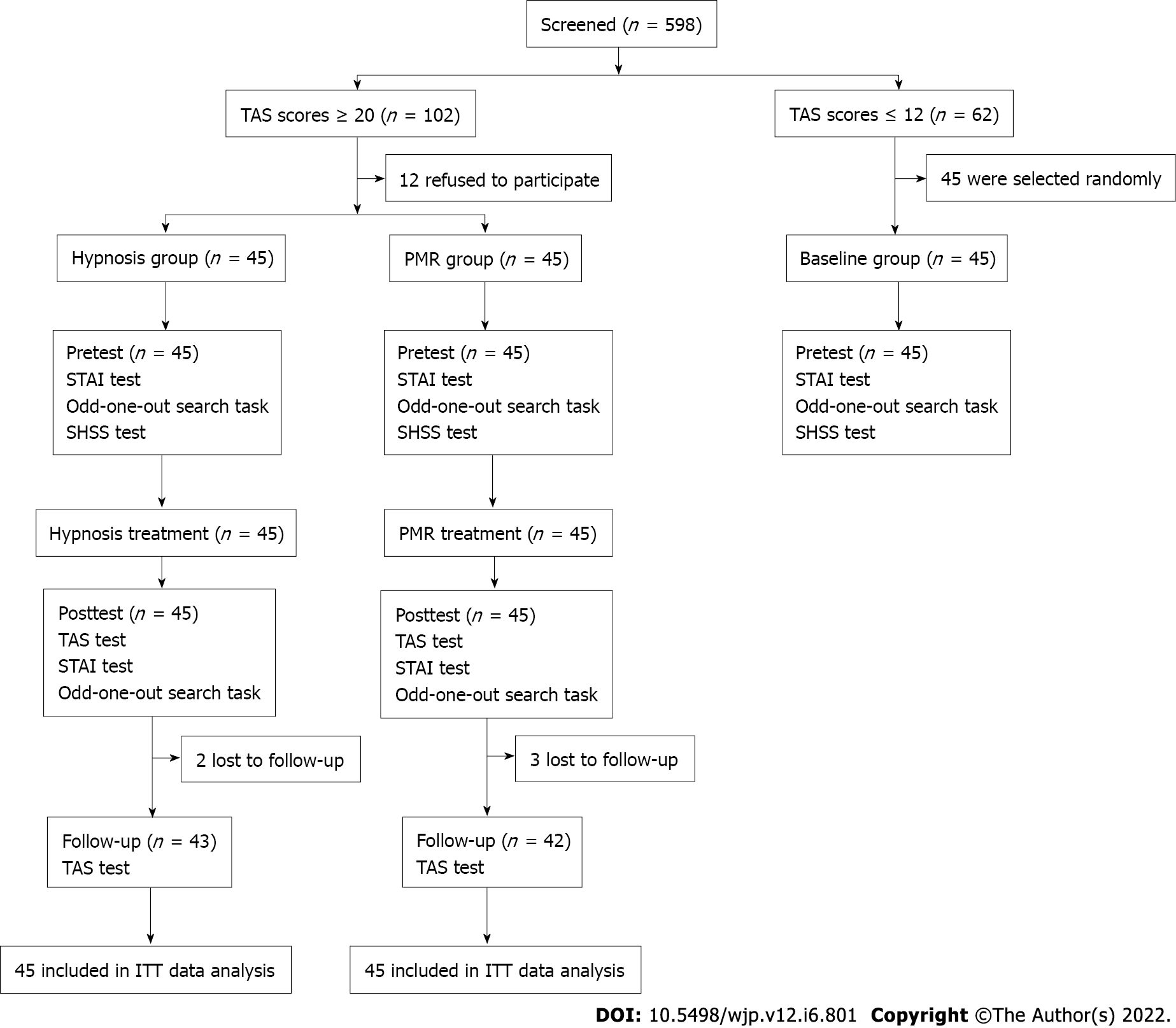
The study was conducted at Anhui Medical University in China. The participants were college students. A total of 598 medical students were screened. The participants were divided into higher and lower test anxiety groups according to their scores on the test anxiety scale (TAS)[28]. The inclusion criteria were: Participants with a TAS score higher than 20 formed a high-anxiety group (n = 102), while participants with a score lower than 12 formed a low-anxiety group (n = 62). Twelve participants in the high-anxiety group refused to participate in the study. The remaining 90 participants were randomly assigned to either a hypnosis group or a PMR group, with 45 students in each group. Forty-five of 62 participants with low test anxiety scores were randomly selected for baseline comparisons (control group). The purpose of using the baseline control group was to explore whether the highly test-anxious individuals in both the hypnosis and PMR groups showed an attentional bias to test-related information at the pretest, compared to the participants with low test anxiety. Randomization was performed by the project leader using a computer-generated random list of numbers. Randomization information was sealed in sequentially numbered boxes that were identical in appearance.
The exclusion criteria were: The therapist (the first author) conducted a semi-structured interview to ensure that none of the participants had a history of psychiatric or neurological disease, medication use, or chronic illness, or a current major psychiatric disorder. The study was approved by Anhui Medical University’s Human Ethics Committee (Trial Registration: ChiCTR1900025058). All participants provided written informed consent and were paid 180 Chinese Yuan for participating in the study. Participants, therapists, and independent evaluators were blinded to the study arm.
There were two groups with high test anxiety in this study: The hypnosis group and the PMR group. The low-test anxiety group served as a baseline control group. This was a randomized clinical trial in which two treatment conditions (hypnosis and PMR) were compared with a baseline condition at a ratio of 1:1:1. A series of face-to-face assessments were performed at pretest and posttest, and a follow-up at 2 mo after the intervention (mailed responses). Given that group interventions on test anxiety reduction produced more significant effects than individual interventions[11], group interventions were conducted for the purposes of this study. Data was collected between February 2018 and May 2019.
The intervention sessions took place in a quiet classroom in the university. The intervention was conducted weekly for 6 wk, and each session lasted approximately 30 min. The total intervention time and number of intervention sessions for the hypnosis and PMR groups were equal.
Hypnosis group: An experienced hypnosis therapist conducted the hypnosis. Using a standard hypnotic induction procedure, the students were induced into a hypnotic state[29]. This procedure took approximately 15 min. The participants were then given hypnotic suggestions of mild to high test anxiety exposure, with imagery. In the meantime, the participants were given suggestions of relaxation and pleasant experiences. Suggestions were also made to change the participants’ cognition and attention on the test (see more details in Supplementary material).
PMR group: The participants in the PMR group received PMR training with the guidance of a relaxation therapist. The procedure was initially developed by Jacobson[30] and was standardized by Bernstein and Borkovec[31]. Although several studies have attempted to combine PMR with guided imagery to expose patients to specific positive thoughts[32], this study utilized the PMR procedure based on Jacobson[30]’s theory and technique. The PMR technique mainly involved standardized and validated methods[31,33]. During the PMR exercises, the participants deliberately applied tension to specific muscle groups and then released it. The tension-relaxation response started with the hands, moved through the whole body, and ended with the feet.
Control group: Those with low TAS scores, who were included for baseline comparisons, received no intervention. Group hypnosis and group PMR were performed by a hypnosis specialist (Li XM) and a PMR therapist (Zhang Y). These individuals’ mean duration of practice in psychiatry was 9 years. Each therapist received 20 h of additional training specific to the requirements of the study. To ensure adherence to the treatments, the therapists followed manuals for hypnosis and PMR and completed a checklist recording the techniques used in treatments.
Primary outcome measure: The TAS was designed to evaluate test anxiety[34]. The scale contains 37 true-false statements on test-taking, and the total number of “true” checks represents the TAS. The interpretation of TAS scores is as follows: 0 to 12 indicates no or mild test anxiety, 13 to 20 indicates moderate test anxiety, and > 20 signifies severe test anxiety. This study made use of an adapted Chinese version of the TAS that showed sufficient and comparable reliability and validity[28].
Attentional bias was evaluated by the odd-one-out search task adapted from the procedure used by Rinck et al[25]. The participant was seated approximately 50 cm from a 17-inch computer screen. Each trial started with a fixation cross (500 ms) in the screen center, followed by a 2 × 2 matrix of four words. The participant was instructed to determine whether there was a target word that belonged to a different category within the matrix by pressing ‘A’ (yes) or ‘L’ (no). The matrix contained four words with the same category or three words with the same category and a target word with a different category. The matrix remained on the screen until a response was given. The words represented three categories of emotional relevance: Threatening words related to the test (n = 60), positive words related to positive emotion (n = 60), and neutral words such as ‘furniture’ and ‘natural environment’ (n = 120). Attentional bias was assessed: Accelerated detection and slowed disengagement. Eighty trials assessed speeded detection as follows: (1) Twenty trials presented the matrix containing three neutral words and one positive word; (2) Twenty trials showed the matrix containing three neutral words and one threatening word; and (3) Forty trials presented the matrix containing four neutral words. Eighty trials assessed slowed disengagement as follows: (1) Twenty trials showed the matrix containing three positive words and one neutral word; (2) Twenty trials presented the matrix containing three threatening words and one neutral word; (3) Twenty trials showed the matrix containing four positive words; and (4) Twenty trials presented the matrix containing four threatening words.
The location of the target word in each matrix was random for each trial and each participant. All participants engaged in both sessions, and the order of the sessions was counterbalanced across the participants. We conducted a pilot study on a sample of 45 college students to validate all words with a 9-point Likert scale assessing valence and arousal levels.
Secondary outcome measures: The state-trait anxiety inventory (STAI) consists of two sub-scales[35]. One scale assesses the temporary condition of state anxiety, while the other scale evaluates the long-standing quality of trait anxiety. Each scale contains 20 statements rated on a 4-point Likert scale ranging from 0 (almost never) to 3 (almost always). A higher score indicates higher anxiety. We used a validated Chinese version of the STAI with satisfying reliability and validity[36].
Before the intervention, the hypnotic susceptibility of participants, regarded as a control variable, was evaluated using the Stanford Hypnotic Susceptibility Scale (SHSS), Form C[29]. The scale consists of 12 motor items. The participant receives one score if they follow the motor suggestion and produce the movement. The total score is 12, and a higher score suggests greater hypnotic susceptibility.
The power of the sample size was calculated using G*power software. We used an independent sample t-test between the hypnosis and PMR groups for sample size estimation with a power of 0.90 at P = 0.05 using a two-sided test. Moreover, we adjusted for any drop-outs at the rate of 15% during the follow-up test, resulting in the final sample size of 135 participants.
Statistical analyses were conducted using SPSS 20.0. The intention-to-treat analyses were conducted on data from all participants who completed the pretest assessments. The missing data were treated using the last observation carried forward for those who did not complete the follow-up test. First, one-way analysis of variance (ANOVA) was conducted to test baseline differences among the three groups. At the pretest, planned comparisons were conducted between higher and lower test anxiety groups and the hypnosis and PMR groups. Then, the TAS measures were subject to a two-factor mixed design with treatment conditions as the between-group and time as the repeated measure factor. Differences in the TAS measures were compared using analysis of covariance (ANCOVA) with lysergic acid diethylamide post hoc comparisons on the adjusted means. Third, to test potential training effects, ANCOVA was performed to compare the hypnosis and PMR groups, using posttest scores as dependent variables and the corresponding pretest scores as covariate. Finally, a reliable change index (RCI) for TAS scores from pretreatment to posttest was computed using the formula reported by Jacobson and Truax[37]. Participants with an RCI score greater than a 1.96 reduction in TAS score at posttest were regarded as having a clinically significant improvement. Effect sizes were reported as partial eta squared (ηp2), eta squared (η2), Cohen’s d, or Cramer’s φ. Categorical data were analyzed using χ2 tests. Significance was defined at P = 0.05.
The enrollment of participants and the study flow are shown in Figure 1. A total of 135 participants were assigned to three groups: Hypnosis, PMR, and control groups. Characteristics of the participants are presented in Table 1. The results of ANOVA conducted on the pretest scores in TAS, STAI, and attentional bias measures are shown in Table 1. For attentional bias measures on speeded detection trials, the speeded detection score is reaction time for neutral words - reaction time for threatening stimuli or positive words. On slowed disengagement trials, the slowed disengagement score is reaction time for threatening stimuli or positive stimuli - reaction time for neutral stimuli. One-way ANOVA was significant for: TAS (F = 1008.808, P < 0.001), STAI-trait (F = 401.431, P < 0.001), STAI-state (F = 385.483, P < 0.001), speeded detection to threatening stimuli (F = 401.431, P < 0.001), speeded detection to positive stimuli (F = 401.431, P < 0.001), slowed disengagement from threatening stimuli (F = 401.431, P < 0.001), and slowed disengagement from positive stimuli (F = 401.431, P < 0.001). There were significant differences between the higher and lower test anxiety groups in the planned comparisons, while there were no significant differences between the hypnosis and PMR groups at pretest. Given that test anxiety is a situation-specific disorder[13], this study also considered when assessments were made. The three groups did not differ in the number of days until the next exam at pretest (F = 1.786, P > 0.05), posttest (F = 2.384, P > 0.05), or follow-up (F = 2.730, P > 0.05).
| Control (n = 45) | Hypnosis (n = 45) | PMR (n = 45) | Hypnosis & PMR vs control | Hypnosis vs PMR | ||||||||
| M | SD | M | SD | M | SD | t/χ2 | P value | Cohen’s d/Cramer’s φ | t/χ2 | P value | Cohen’s d/Cramer’s φ | |
| Female, n | 17 | 27 | 26 | 5.35 | 0.02 | 0.19 | 0.05 | 0.83 | 0.02 | |||
| Age | 20.94 | 0.94 | 20.76 | 1.05 | 20.84 | 0.85 | 0.13 | 0.90 | 0.08 | -0.44 | 0.66 | 0.08 |
| Education | 14.71 | 0.84 | 14.80 | 1.14 | 14.96 | 0.82 | -0.97 | 0.33 | 0.18 | -0.76 | 0.45 | 0.16 |
| SHSS | 8.08 | 1.92 | 7.88 | 1.80 | 7.57 | 1.45 | 1.13 | 0.26 | 0.19 | 0.91 | 0.37 | 0.18 |
| TAS score | 8.66 | 1.33 | 23.74 | 1.63 | 23.97 | 2.42 | 45.03 | < 0.001 | 8.77 | 0.53 | 0.60 | 0.11 |
| STAI score | ||||||||||||
| Trait | 36.78 | 1.75 | 49.38 | 3.14 | 50.20 | 2.47 | 28.14 | < 0.001 | 5.51 | 1.38 | 0.17 | 0.29 |
| State | 36.06 | 1.89 | 48.34 | 2.92 | 49.14 | 2.59 | 27.59 | < 0.001 | 5.33 | 1.37 | 0.17 | 0.29 |
| Speeded detection | ||||||||||||
| Threatening words | -6.99 | 212.68 | -381.10 | 159.76 | -397.49 | 189.92 | -10.37 | < 0.001 | 1.89 | -0.94 | 0.35 | 0.19 |
| Positive words | -403.62 | 163.41 | -219.88 | 170.82 | -226.21 | 254.62 | 4.95 | < 0.001 | 0.94 | -0.14 | 0.89 | 0.03 |
| Slowed disengagement | ||||||||||||
| Threatening words | 111.19 | 341.38 | 379.48 | 437.92 | 431.94 | 386.65 | 4.14 | < 0.001 | 0.78 | 0.62 | 0.55 | 0.13 |
| Positive words | 100.93 | 291.41 | -173.90 | 353.80 | -113.31 | 403.44 | -3.80 | < 0.001 | 0.72 | 0.76 | 0.45 | 0.16 |
The difference in TAS scores between the two groups was analyzed using 2 (group: Hypnosis and PMR) × 3 (time: Pretest, posttest, and follow-up) repeated measures ANOVA. Significant primary effects of time (F = 334.444, P < 0.001, ηp2 = 0.792) and group (F = 10.619, P = 0.002, ηp2 = 0.108), and the significant interaction effect between time and group (F = 8.869, P = 0.002, ηp2 = 0.092) were revealed.
A simple effect analysis was conducted at each level of the group variable. The results are summarized as follows: (1) For the hypnosis group, a significant effect of time was revealed (F = 304.878, P < 0.001, ηp2 = 0.874), and the paired t-test suggested that the participants had a significantly lower TAS score at posttest [t = -21.827, P < 0.001, Cohen’s d = 4.111, 95% confidence interval (CI): 10.218-12.297] and at follow-up (t = -14.824, P < 0.001, Cohen’s d = 3.108, 95%CI: 6.567-8.632), compared with that at pretest. The participants had a significantly higher TAS score at follow-up compared with posttest [t = 10.551, P < 0.001, Cohen’s d =1.110, 95%CI: (-4.356)-(-2.959)]; and (2) For the PMR group, a significant effect of time was revealed (F = 93.195, P < 0.001, ηp2 = 0.679), and the paired t-test suggested that the participants had a significantly lower TAS score at posttest (t = -10.777, P < 0.001, Cohen’s d = 2.067, 95%CI: 6.620-9.665) and at follow-up (t = -7.444, P < 0.001, Cohen’s d = 1.408, 95%CI: 3.896-6.789), compared with that at pretest. The participants had a significantly higher TAS score at follow-up compared with posttest [t = 22.164, P < 0.001, Cohen’s d = 0.572, 95%CI: (-3.055)-(-2.545)].
The simple effect analysis at each level of time variable was conducted by planned t-test. At the posttest level, the hypnosis group had a significantly lower TAS score than the PMR group [t = -3.664, P < 0.001, Cohen’s d = 0.772, 95%CI: (-5.156)-(-1.530)]. At the follow-up level, the hypnosis group also had a significantly lower TAS score than the PMR group [t = -2.943, P = 0.004, Cohen’s d = 0.621, 95%CI:
The two higher test anxiety groups were compared with regard to their post-test scores of attentional bias and STAI, including pre-test scores as covariate. The results are displayed in Table 2. On speeded detection trials, the hypnosis group was slower in detecting threatening stimuli and faster in detecting positive words than the PMR group. On slowed disengagement trials, the hypnosis group had a faster reaction time to threatening stimuli (one-tailed P = 0.035) or to positive words than the PMR group.
| Hypnosis (n = 45) | PMR (n = 45) | ANCOVA | |||||
| M | SD | M | SD | F | P value | η2 | |
| Speeded detection | |||||||
| threatening words | -346.00 | 279.88 | -91.86 | 199.57 | 30.35 | < 0.001 | 0.26 |
| Positive words | -203.59 | 299.03 | -300.54 | 242.72 | 10.03 | 0.002 | 0.10 |
| Slowed disengagement | |||||||
| threatening words | 260.04 | 398.21 | 387.18 | 420.11 | 3.36 | 0.070 | 0.04 |
| Positive words | -4.78 | 369.07 | -117.22 | 372.78 | 11.46 | 0.001 | 0.12 |
| STAI scores | |||||||
| State | 35.11 | 2.53 | 36.32 | 1.92 | 6.04 | 0.02 | 0.07 |
| Trait | 38.21 | 2.51 | 38.39 | 2.34 | 0.12 | 0.73 | 0.001 |
The average posttest scores on state anxiety and trait anxiety are presented in Table 2. The table shows that the hypnosis group had a lower state anxiety score than the PMR group, while there was no significant difference in the trait anxiety scores of the two groups. Additionally, we compared the differences in attentional bias and STAI scores between pretest and posttest. For the hypnosis group, there were significant differences between pretest and posttest in speeded detection of threatening words (t = -9.143, P < 0.001, Cohen’s d = 1.600), speeded detection of positive words (t = 3.010, P = 0.004, Cohen’s d = 0.384), slowed disengagement from threatening words (t = -4.444, P < 0.001, Cohen’s d = 0.285), and slowed disengagement from positive words (t = 3.865, P < 0.001, Cohen’s d = 0.468). However, for the PMR group, there were no significant differences in any of the above scores (P > 0.05). For the hypnosis group, there were significant differences between pretest and posttest in trait anxiety (t = 608.99, P < 0.001, Cohen’s d = 4.815) and in state anxiety (t = 150.83, P < 0.001, Cohen’s d = 5.491). For the PMR group, there were significant differences between pretest and posttest in trait anxiety (t = 42.481, P < 0.001, Cohen’s d = 3.969) and in state anxiety (t = 27.646, P < 0.001, Cohen’s d = 4.864).
The results show that 39 participants in the hypnosis group (86.67%) and 28 participants in the PMR group (62.22%) met the criteria for clinically significant change (RCI score greater than 1.96 in TAS score at posttest; χ2= 7.07, P = 0.008).
This study investigated the efficacy of hypnosis and PMR for treating individuals with test anxiety. Both treatments appeared sound and demonstrated high within-group effect size in primary outcomes of test anxiety after intervention and at 2-mo follow-up. An important finding is that hypnosis was more effective than PMR in reducing attentional bias to threatening stimuli. For the group comparisons at pretest, the highly test-anxious individuals in both the hypnosis and PMR groups showed an attentional bias to threat and test-related information, consistent with previous studies[20,21]. Moreover, the higher test anxiety groups had significantly higher trait and state anxiety than the lower test anxiety group. Previous studies have also found positive correlations between the test anxiety score and STAI[4].
Compared with the pretest, the test anxiety of participants in both the hypnosis and PMR groups significantly decreased after 6-wk intervention and at 2-mo follow-up. Our data add to evidence from previous randomized controlled trials showing that hypnosis and PMR effectively reduce test anxiety[10,27]. Notably, the hypnosis group demonstrated lower test anxiety than the PMR group at posttest and at follow-up. This finding suggests that, in the present study, hypnosis was more effective than PMR in reducing test anxiety. Furthermore, analyses exploring clinically significant change showed that 86.67% of participants in the hypnosis group and 62.22% of those in the PMR group exhibited clinically significant reductions in test anxiety from baseline to posttest. This difference in response rates was statistically significant, demonstrating that hypnosis outperformed PMR in test anxiety symptom reduction. In the hypnotic state, the participants were given suggestions of relaxation that produced positive and pleasant experiences. This method could help individuals reduce anxiety in a relaxed state and facilitate the link between anxious situations and pleasurable experiences. By establishing conditioning, individuals learn to anticipate pleasant experiences following threatening stimuli such as test situations. These findings have the important clinical implication that a combination of hypnosis and other psychotherapies would be more productive in treating anxiety disorders than hypnosis alone. Indeed, a previous study suggested that combined treatment using cognitive behavior therapy and hypnosis produces better effects than hypnosis alone[38].
Both the hypnosis and PMR groups demonstrated reduced trait anxiety and state anxiety at the posttest compared with the pretest, suggesting that test anxiety is relevant to both trait and state anxiety. Interestingly, state anxiety was reduced more in the hypnosis group than in the PMR group, while there was no significant difference in trait anxiety between the two groups at the posttest. State anxiety is unstable and specific to certain situations, which seems to make it more sensitive to training and intervention. This finding is consistent with previous studies reporting more beneficial effects from intervention on state anxiety than on trait anxiety[39].
Notably, this study investigated the attentional bias of test-anxious students by calculating two indices: Speeded detection and slowed disengagement. After the intervention, the individuals in the hypnosis group demonstrated reduced detection speed and slowed disengagement toward threatening stimuli. Significantly, the hypnosis group showed a reversed speeded detection of and delayed disengagement from positive stimuli after the intervention. Taken together, hypnosis appears to help individuals be less sensitive to threatening stimuli but more sensitive to positive stimuli, an effect more significant than PMR intervention.
These findings prove that hypnosis effectively reduced attentional bias to threatening stimuli and increased attentional bias to positive stimuli. In contrast, the PMR had little effect in lowering attentional bias to threatening stimuli. Hypnosis relies on hypnotic and posthypnotic suggestions to modify participants’ cognition and attention, whereas PMR is merely a relaxation technique that can affect the physiological and emotional components of test anxiety[5,6]. However, PMR may have little impact on cognition and attention. Two significant components of hypnosis are cognition and relaxation; combining those two components would be more effective in reducing anxiety[40].
General cognitive models of anxiety suggest that anxious individuals tend to direct their attention toward threatening information in the environment[41,42], thereby facilitating the development and maintenance of the anxious state[43]. Several studies have emphasized the vital influence of attentional bias on anxiety[44,45]. Mathews and MacLeod[46] further indicated that attentional bias has causal effects on vulnerability to anxiety. Therefore, attentional bias should be regarded as an essential target in treatment, and various training paradigms such as attentional bias modification have, in fact, been developed to target it, with promising effects in reducing test anxiety[22] and other disorders[47,48].
Our findings indicate that hypnosis, targeting both muscle relaxation and attentional bias, could decrease anxiety vulnerability to test-related stimuli and reduce attentional bias toward test-related stimuli. With hypnotic suggestions, the participants could remain calm and relaxed when facing information related to the exam, and thus they could cease fixating on the information. However, the PMR, which targeted muscle relaxation, could only change anxiety vulnerability and not attentional bias. All these suggest that it is crucial to look for an underlying mechanism as a target for prevention and treatment.
Hypnosis is not effective for everybody, because some patients respond quickly to hypnotic suggestions, while others are unaffected[49]. It appears that hypnotic susceptibility may affect the outcome, and it is an important control variable. Hypnotic susceptibility indicates proneness to accepting suggestions in and out of hypnosis[50]. Fortunately, there was no significant difference in hypnotic susceptibility among the three groups, and thus the influence of hypnotic susceptibility on the treatment can be ignored.
This study concluded that hypnosis is efficacious in treating test anxiety by reducing anxiety vulnerability and attentional bias to threatening stimuli. However, it had several limitations. First, we did not examine participants’ physiological indices, such as skin conductance response, blood pressure, and heart rate. This would provide an objective measure more sensitive to the changes induced by the intervention. Moreover, a lack of physiological measures also makes it difficult to differentiate whether hypnosis did better than PMR due to better physical relaxation or attentional bias, or maybe some other factor. Second, the study did not evaluate the influence of the intervention on exam performance. Finally, we only considered a 2-mo follow-up, leaving the long-term effects of hypnosis in this context inconclusive.
Hypnosis is more effective than PMR in reducing test anxiety in medical students; hypnosis could modify attentional bias toward threatening stimuli, but PMR could not. The reason for this may be that the hypnosis developed in this study targeted both anxiety symptoms and attentional bias, suggesting that targeting attentional bias is an important factor in treating test anxiety or other anxiety disorders. Additionally, hypnosis integrated with some form of therapy may have enhanced effects on mental disorders.
Test anxiety is prevalent among medical students and leads to impaired academic performance. Test-related attentional bias has been identified as an important maintaining factor in test-anxious individuals.
The present study aimed to evaluate whether hypnosis and progressive muscle relaxation (PMR) could modify medical college students’ test anxiety and attentional bias.
This study was designed as an initial pilot randomized clinical trial comparing the effects of hypnosis to the effects of PMR on test anxiety and its associated attentional bias. This study is the first to use hypnosis to help individuals reduce test anxiety and attentional bias toward threatening stimuli, and is also the first to use PMR to reduce attentional bias in students.
A total of 598 medical students were screened. The participants were divided into higher and lower test anxiety groups according to their scores on the test anxiety scale (TAS). Ninety medical college students with high TAS scores were randomly assigned to a hypnosis or PMR group. Another 45 students with low TAS scores were included for baseline control group. The intervention was conducted weekly for 6 wk, and each session lasted approximately 30 min. The total intervention time and the number of intervention sessions were matched between the hypnosis and PMR groups. Data were collected at pretest, posttest, and 2-mo follow-up.
Hypnosis group participants had a significantly lower TAS score at posttest (t = -21.827, P < 0.001) and at follow-up (t = -14.824, P < 0.001), compared with that at pretest. PMR group participants also had a significantly lower TAS score at posttest (t = -10.777, P < 0.001) and at follow-up (t = -7.444, P < 0.001), compared with that at pretest. At the posttest level, the hypnosis group had a significantly lower TAS score than the PMR group (t = -3.664, P < 0.001). At the follow-up level, the hypnosis group also had a significantly lower TAS score than the PMR group (t = -2.943, P = 0.004). Clinically significant improvement was found in both the hypnosis and PMR groups (hypnosis = 64.0%; PMR = 62.22%). Hypnosis was more effective than PMR in reducing test anxiety among medical college students. Hypnosis could modify attentional bias toward threatening stimuli, but PMR could not.
Hypnosis is more effective than PMR in reducing test anxiety in medical students; hypnosis could modify attentional bias toward threatening stimuli, but PMR could not. Additionally, hypnosis integrated with some form of therapy may have enhanced effects on mental disorders. Our findings have important implications for the design and optimization of hypnotic treatments for anxiety disorders.
This study concluded that hypnosis is efficacious in treating test anxiety by reducing anxiety vulnerability and attentional bias to threatening stimuli. The findings imply that attentional bias can be an important target in future research on treating test anxiety or other anxiety disorders.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Corresponding Author’s Membership in Professional Societies: Anhui Medical University.
Specialty type: Psychiatry
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): A
Grade B (Very good): B, B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Cotez CM, Brazil; Gupta A, United States; Pervin Z, United States; Stoyanov D, Bulgaria A-Editor: Yao QG S-Editor: Wang JJ L-Editor: Wang TQ P-Editor: Wang JJ
| 1. | Khoshhal KI, Khairy GA, Guraya SY, Guraya SS. Exam anxiety in the undergraduate medical students of Taibah University. Med Teach. 2017;39:S22-S26. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 23] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 2. | Yusoff MS, Esa AR, Mat Pa MN, Mey SC, Aziz RA, Abdul Rahim AF. A longitudinal study of relationships between previous academic achievement, emotional intelligence and personality traits with psychological health of medical students during stressful periods. Educ Health (Abingdon). 2013;26:39-47. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 29] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 3. | de Hullu E, Sportel BE, Nauta MH, de Jong PJ. Cognitive bias modification and CBT as early interventions for adolescent social and test anxiety: Two-year follow-up of a randomized controlled trial. J Behav Ther Exp Psychiatry. 2017;55:81-89. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 34] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 4. | Szafranski DD, Barrera TL, Norton PJ. Test anxiety inventory: 30 years later. Anxiety Stress Coping. 2012;25:667-677. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 52] [Cited by in RCA: 34] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 5. | Krispenz A, Dickhäuser O. Effects of an Inquiry-Based Short Intervention on State Test Anxiety in Comparison to Alternative Coping Strategies. Front Psychol. 2018;9:201. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 12] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 6. | StoÈber J, Pekrun R. Advances in test anxiety research. Anxiety Stress Coping. 2004;17:205-211. [RCA] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 30] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 7. | Reiss N, Warnecke I, Tibubos AN, Tolgou T, Luka-Krausgrill U, Rohrmann S. Effects of cognitive-behavioral therapy with relaxation vs. imagery rescripting on psychophysiological stress responses of students with test anxiety in a randomized controlled trial. Psychother Res. 2019;29:974-985. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 4] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 8. | Shi Z, Gao X, Zhou R. Emotional working memory capacity in test anxiety. Learn Individ Differ. 2014;32:178-183. [RCA] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 14] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 9. | Hollitt S, Kemps E, Tiggemann M, Smeets E, Mills JS. Components of attentional bias for food cues among restrained eaters. Appetite. 2010;54:309-313. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 85] [Cited by in RCA: 94] [Article Influence: 6.3] [Reference Citation Analysis (1)] |
| 10. | Zargarzadeh M, Shirazi M. The effect of progressive muscle relaxation method on test anxiety in nursing students. Iran J Nurs Midwifery Res. 2014;19:607-612. [PubMed] |
| 11. | Ergene T. Effective interventions on test anxiety reduction: A meta-analysis. Sch Psychol Int. 2003;24:313-328. [RCA] [DOI] [Full Text] [Cited by in Crossref: 162] [Cited by in RCA: 167] [Article Influence: 18.6] [Reference Citation Analysis (0)] |
| 12. | Prinz JN, Bar-Kalifa E, Rafaeli E, Sened H, Lutz W. Imagery-based treatment for test anxiety: A multiple-baseline open trial. J Affect Disord. 2019;244:187-195. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 12] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 13. | Huntley CD, Young B, Temple J, Longworth M, Smith CT, Jha V, Fisher PL. The efficacy of interventions for test-anxious university students: A meta-analysis of randomized controlled trials. J Anxiety Disord. 2019;63:36-50. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 21] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 14. | Elkins GR, Barabasz AF, Council JR, Spiegel D. Advancing research and practice: the revised APA Division 30 definition of hypnosis. Int J Clin Exp Hypn. 2015;63:1-9. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 205] [Cited by in RCA: 234] [Article Influence: 23.4] [Reference Citation Analysis (0)] |
| 15. | Mendoza ME, Capafons A. Valencia Model of Waking Hypnosis: Background, Research, and Clinical Applications. Am J Clin Hypn. 2018;61:108-124. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 3] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 16. | Daitch C. Hypnotherapeutic treatment for anxiety-related relational discord: a short-term hypnotherapeutic protocol. Am J Clin Hypn. 2014;56:325-342. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 4] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 17. | Mende M. Hypnosis: State of the art and perspectives for the twenty-first century. Contemp Hypn. 2009;26:179-184. [DOI] [Full Text] |
| 18. | Cisler JM, Koster EH. Mechanisms of attentional biases towards threat in anxiety disorders: An integrative review. Clin Psychol Rev. 2010;30:203-216. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1137] [Cited by in RCA: 1073] [Article Influence: 71.5] [Reference Citation Analysis (0)] |
| 19. | Bar-Haim Y, Lamy D, Pergamin L, Bakermans-Kranenburg MJ, van IJzendoorn MH. Threat-related attentional bias in anxious and nonanxious individuals: a meta-analytic study. Psychol Bull. 2007;133:1-24. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2300] [Cited by in RCA: 2395] [Article Influence: 133.1] [Reference Citation Analysis (0)] |
| 20. | Dong Y, De Beuckelaer A, Yu L, Zhou R. Eye-movement evidence of the time-course of attentional bias for threatening pictures in test-anxious students. Cogn Emot. 2017;31:781-790. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 13] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 21. | Zhang X, Dong Y, Zhou R. Examination Stress Results in Attentional Bias and Altered Neural Reactivity in Test-Anxious Individuals. Neural Plast. 2018;2018:3281040. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 16] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 22. | Cai W, Pan Y, Chai H, Cui Y, Yan J, Dong W, Deng G. Attentional bias modification in reducing test anxiety vulnerability: a randomized controlled trial. BMC Psychiatry. 2018;18:1. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 43] [Cited by in RCA: 100] [Article Influence: 14.3] [Reference Citation Analysis (0)] |
| 23. | Oberauer K. Working Memory and Attention - A Conceptual Analysis and Review. J Cogn. 2019;2:36. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 198] [Cited by in RCA: 194] [Article Influence: 32.3] [Reference Citation Analysis (0)] |
| 24. | Posner MI, Petersen SE. The attention system of the human brain. Annu Rev Neurosci. 1990;13:25-42. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4739] [Cited by in RCA: 4490] [Article Influence: 128.3] [Reference Citation Analysis (0)] |
| 25. | Rinck M, Reinecke A, Ellwart T, Heuer K, Becker ES. Speeded detection and increased distraction in fear of spiders: evidence from eye movements. J Abnorm Psychol. 2005;114:235-248. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 111] [Cited by in RCA: 105] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 26. | Ozhanli Y, Akyuz N. The Effect of Progressive Relaxation Exercise on Physiological Parameters, Pain and Anxiety Levels of Patients Undergoing Colorectal Cancer Surgery: A Randomized Controlled Study. J Perianesth Nurs. 2022;37:238-246. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 12] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 27. | Sezgin N, Özcan B. The effect of Progressive Muscular Relaxation and Emotional Freedom Techniques on test anxiety in high school students: a randomized controlled trial. Energy Psychol J. 2009;1:23-29. [RCA] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 17] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 28. | Wang C. Reliability and validity of test anxiety scale-Chinese version. Chin Mental Health J. 2001;8:96-97. |
| 29. | Weitzenhoffer AM, Hilgard ER. Stanford hypnotic susceptibility scale, form C. Palo Alto: Consulting Psychologists Press, 1962. |
| 30. | Jacobson E. Electrical measurements concerning muscular contraction (tonus) and the cultivation of relaxation in man: relaxation times of individuals. Am J Physiol. 1934;108:573-580. [RCA] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 19] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 31. | Bernstein DA, Borkovec TD. Progressive Relaxation Training. Champaign: Research Press, 1973. |
| 32. | Baider L, Uziely B, De-Nour AK. Progressive muscle relaxation and guided imagery in cancer patients. Gen Hosp Psychiatry. 1994;16:340-347. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 82] [Cited by in RCA: 83] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 33. | Bernstein DA, Carlson CR. Progressive relaxation: abbreviated methods. In: Lehrer PM, Woolfolk RL. Principles and practice of stress management. New York: Guilford Press, 1993: 53-87. |
| 34. | Sarason IG. The test anxiety scale: concept and research. 1977. |
| 35. | Spielberger CD, Gorsuch RL, Lushene RE, Vagg PR, Jacobs GA. Manual for the state-trait anxiety inventory sTAI (Form Y). Palo Alto: Consulting Psychologists Press, 1983. |
| 36. | Li W, Qian M. Revised norm of State-Trait Anxiety Inventory in Chinese college students. Acta Scientiarum Naturalium Universitatis Pekinensis. 1995;31:108-112. |
| 37. | Jacobson NS, Truax P. Clinical significance: a statistical approach to defining meaningful change in psychotherapy research. J Consult Clin Psychol. 1991;59:12-19. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 173] [Cited by in RCA: 555] [Article Influence: 16.3] [Reference Citation Analysis (0)] |
| 38. | Boutin GE, Tosi DJ. Modification of irrational ideas and test anxiety through rational stage directed hypnotherapy [RSDH]. J Clin Psychol. 1983;39:382-391. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 39. | Coppola L, Montanaro F. Effect of a homeopathic-complex medicine on state and trait anxiety and sleep disorders: a retrospective observational study. Homeopathy. 2013;102:254-261. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 40. | Sapp M. Hypnotherapy and test anxiety: Two cognitive-behavioral constructs: The effects of hypnosis in reducing test anxiety and improving academic achievement in college students. Australas J Clin Exp Hypn. 1991;12:25-31. |
| 41. | Körner A, Strack F. Specifying separation: avoidance, abstraction, openness to new experiences. Behav Brain Sci. 2021;44:e12. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 42. | Theodore K, Johnson S, Chalmers-Brown A, Doherty R, Harrop C, Ellett L. Quality of life and illness beliefs in individuals with early psychosis. Soc Psychiatry Psychiatr Epidemiol. 2012;47:545-551. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 27] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 43. | Hofmann SG. Cognitive factors that maintain social anxiety disorder: a comprehensive model and its treatment implications. Cogn Behav Ther. 2007;36:193-209. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 763] [Cited by in RCA: 604] [Article Influence: 33.6] [Reference Citation Analysis (0)] |
| 44. | de Voogd EL, Wiers RW, Prins PJM, de Jong PJ, Boendermaker WJ, Zwitser RJ, Salemink E. Online attentional bias modification training targeting anxiety and depression in unselected adolescents: Short- and long-term effects of a randomized controlled trial. Behav Res Ther. 2016;87:11-22. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 49] [Cited by in RCA: 61] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 45. | Mathews A, Mogg K, Kentish J, Eysenck M. Effect of psychological treatment on cognitive bias in generalized anxiety disorder. Behav Res Ther. 1995;33:293-303. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 163] [Cited by in RCA: 147] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 46. | Mathews A, MacLeod C. Induced processing biases have causal effects on anxiety. Cogn Emot. 2002;16:331-354. [RCA] [DOI] [Full Text] [Cited by in Crossref: 387] [Cited by in RCA: 346] [Article Influence: 15.0] [Reference Citation Analysis (0)] |
| 47. | Clarke PJ, Bedford K, Notebaert L, Bucks RS, Rudaizky D, Milkins BC, MacLeod C. Assessing the Therapeutic Potential of Targeted Attentional Bias Modification for Insomnia Using Smartphone Delivery. Psychother Psychosom. 2016;85:187-189. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 35] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 48. | Kuckertz JM, Amir N. Attention bias modification for anxiety and phobias: current status and future directions. Curr Psychiatry Rep. 2015;17:9. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 49] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 49. | Kirsch I, Braffman W. Imaginative suggestibility and hypnotizability. Curr Dir Psychol Sci. 2001;10:57-61. [RCA] [DOI] [Full Text] [Cited by in Crossref: 68] [Cited by in RCA: 71] [Article Influence: 7.9] [Reference Citation Analysis (0)] |
| 50. | Lynn SJ, Green JP. The sociocognitive and dissociation theories of hypnosis: toward a rapprochement. Int J Clin Exp Hypn. 2011;59:277-293. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 48] [Article Influence: 3.4] [Reference Citation Analysis (0)] |