Published online Jun 19, 2022. doi: 10.5498/wjp.v12.i6.773
Peer-review started: April 6, 2021
First decision: September 5, 2021
Revised: September 13, 2021
Accepted: May 16, 2022
Article in press: May 16, 2022
Published online: June 19, 2022
Processing time: 433 Days and 15.1 Hours
Although primarily affecting the respiratory system, growing attention is being paid to the neuropsychiatric consequences of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infections. Acute and sub-acute neuropsychiatric manifestations of coronavirus disease 2019 (COVID-19) disease and their mech
Core Tip: While acute neuropsychiatric manifestations of coronavirus disease 2019 (COVID-19) are the object of study, far less is known about long-term neuropsychiatric sequelae of COVID-19 infection. Much of the knowledge about this topic can be drawn from past coronaviruses outbreaks and from the study of the mechanisms through which severe acute respiratory syndrome coronavirus 2 harms the central nervous system. A relevant wave of both psychiatric (anxiety and depressive disorders, post-traumatic syndromes) and neurological symptoms could be expected. There will be a vital need for monitoring and early intervention to minimize this potential burden of neuropsychiatric distress.
- Citation: De Berardis D, Di Carlo F, Di Giannantonio M, Pettorruso M. Legacy of neuropsychiatric symptoms associated with past COVID-19 infection: A cause of concern. World J Psychiatry 2022; 12(6): 773-778
- URL: https://www.wjgnet.com/2220-3206/full/v12/i6/773.htm
- DOI: https://dx.doi.org/10.5498/wjp.v12.i6.773
Starting December 2019, several cases of pneumonia of unknown etiology were reported in Wuhan, China. A novel coronavirus was identified as the cause of such illnesses, and on January 12, China made public the gene sequence of the new severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) coronavirus[1]. On January 30, 2020, the World Health Organization (WHO) declared the outbreak of coronavirus disease 2019 (COVID-19) a Public Health Emergency of International Relevance, and on March 11, 2020, the same organization proclaimed the beginning of the COVID-19 pandemic[1]. It was the start of the global crisis we are still struggling with[2].
Coronaviruses are single-stranded RNA viruses; in the past, they have been responsible for two well-known epidemics: (1) The 2002 SARS, caused by SARS-CoV-1; and (2) The 2012 Middle East Respiratory Syndrome (MERS). Like other coronaviruses, the newly identified SARS-CoV-2 affects the respiratory tract, usually causing mild and self-limiting symptomatology similar to the common cold. In susceptible individuals, the virus can reach the lower respiratory tract causing pneumonia and severe acute respiratory syndrome[3].
However, COVID-19 does not only induce a respiratory syndrome, but it can elude the immune response and spread to distant apparatuses, as the renal and cardiovascular[4] ones. In particular, like SARS and MERS, COVID-19 has been shown to be neuro-invasive[6]. A growing body of literature shows that 27% to 41% of COVID-19 patients may present neuropsychiatric complications during the acute stage of the illness[7]. The most reported ones are anosmia, ageusia, headache, confusion, agitation, cerebrovascular events, encephalopathies, anxiety, depressed mood, impaired memory and insomnia[8-10].
On the contrary, far less is known about long-term neuropsychiatric sequelae of COVID-19 infections[11]. The delayed effect of this pandemic, particularly that on the population’s mental health, will require many months, or even years, to be fully acknowledged. Considering that many millions of people have been affected by COVID-19, this becomes a matter of deep concern. Given the aforementioned observations, this editorial aims at discussing the possible long-term effects of the COVID-19 pandemic on neuropsychiatric health.
Most of the hypotheses about COVID-19 long-term effects on the nervous system can be drawn from evidence on SARS-CoV-1 and MERS neuropsychiatric sequelae. As to SARS-CoV-1, high rates of depression (39%), pain disorders (36.4%), panic disorder (32.5%), and obsessive-compulsive disorder (15.6%) were reported among survivors. The mean time of onset of such complications ranged 31 mo to 50 mo post-infection[12]. According to another study, one year after the SARS-CoV-1 outbreak, 64% of the survivors showed some sign of psychiatric morbidity[13], while 30 mo after the outbreak, the prevalence of any psychiatric disorder was 33.3%[14]. A meta-analysis reported rates of neuropsychiatric sequelae in SARS-CoV-1 and MERS survivors raging 10% to 20%; the symptomology most often displayed was insomnia, anxiety, depression, fatigue, and memory impairment[7].
Moreover, an examination of the literature’s data about the relationship between other non-epidemic coronaviruses and neuropsychiatric consequences can be helpful. Human coronavirus HCoV-NL63 infection was associated with mood disorders and suicide attempts[15]. Furthermore, exposure to viral infections, both in utero and during child development, has been linked to an increased risk for schizophrenia[16,17]. In this regard, when compared to controls, an increase in antibodies for four human coronavirus strains was found in patients with a recent psychotic onset[18]. In light of this, such data suggest a possible relation between coronavirus infection and psychosis that could emerge in the long run from SARS-CoV-2.
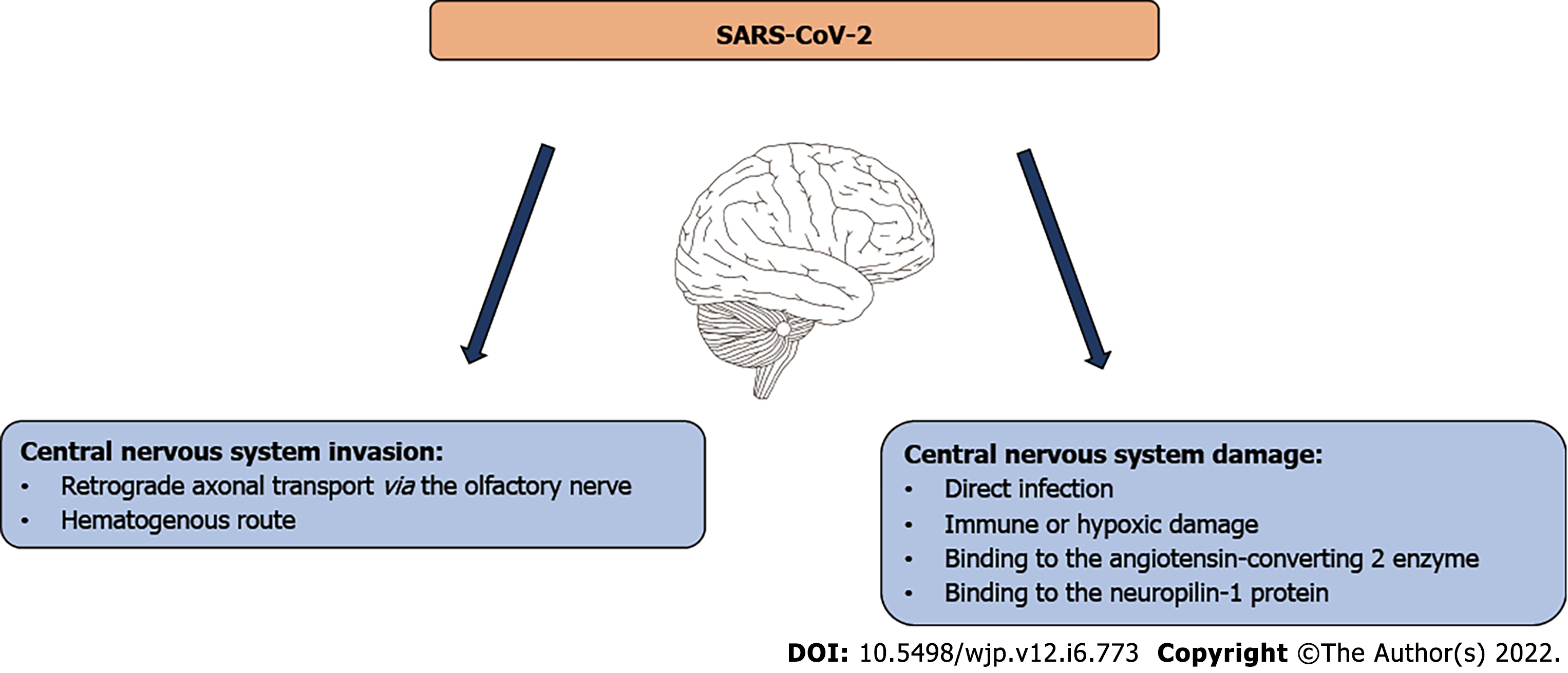
Given the insight drawn from other coronaviruses and considering the mechanisms through which COVID-19 invades and damages the central nervous system (CNS), we can speculate on the long-term neuropsychiatric symptoms this virus may cause. Coronaviruses can spread to the CNS via retrograde axonal transport, from the olfactory nerve, or via the hematogenous route[19] (see Figure 1).
Once in the CNS, the latent virus can be hosted by both neural and immune cells, contributing to the onset of delayed neuropsychiatric complications. There are different pathways through which coronaviruses can affect the CNS, including damages through direct infections, immune or hypoxic damage, and direct binding to the ACE2 enzyme, which is highly expressed by neurons and glia[20]. These pathways were detected both in patients and in experimental animals affected by SARS-CoV-1[21]. Several reports on SARS-CoV-1 and MERS discussing sub-acute demyelinating complications and neuromuscular and neurodegenerative diseases have been published[19,22,23]. Considering the neurotropism of all coronaviruses, we can imagine similar mechanisms and consequences also in COVID-19 patients.
However, SARS-CoV-2 has also shown different mechanisms of neuroinvasiveness. Besides from ACE-2, the neuropilin-1 protein was identified as an additional mediator, facilitating the virus entering the cells[24,25]. This protein is highly expressed in the brain, representing an element of concern, particularly for long-term cognitive sequelae of COVID-19 infections[26]. Early studies showed that cognitive impairment, frequently reported during acute infection, could also persist after recovery. A paper examining patients at a median of 85 d after acute illness showed that 78% of the group reported sustained cognitive difficulties. These deficits did not correlate with depressed mood, fatigue, hospitalization, type of treatment received, acute inflammation, or viremia. If these effects were to extend over time, the impact of SARS-CoV-2 on cognitive functioning might be of great concern[27]. Studies to shed light on SARS-CoV-2 specific neurotropism and its possible neurological consequences are still active[28].
The emergence of post-traumatic stress disorder (PTSD) associated with a prior COVID-19 infection should also be considered. This is because the experience of a potentially severe disease, such as COVID-19, is considered a traumatic event[29]. On the one hand, the infection can lead to brain vulnerabilities that could increase the risk of developing clinically relevant psychological distress. On the other hand, profound stressors linked to the infection, such as medical interventions or isolation, could play a critical role in the development of PTSD as seen for other diseases[30]. This was also demonstrated after the SARS-CoV-1 epidemic, with a 55% rate of PTSD detected among survivors[12]. There are many reports about the emergence of PTSD after a COVID-19 acute infection, and many more are probably yet to come[31,32].
As said, long-term neuropsychiatric complications of COVID-19 infection will remain covert for several months or possibly even several years. Given the global spread of the COVID-19 infection, even if only a small part of the affected people will develop delayed neuropsychiatric sequelae the public health burden generated by these complications will be significant. Thus, we could expect a "crashing wave"[33] of COVID-19 neuropsychiatric consequences, with a plausible relevant impact on countries healthcare resources and on healthcare workers[34] as well. These consequences might be even more severe for those who were already suffering from a psychiatric or neurological disorder[35]. These consequences, hence, might be both psychiatric and neurological. Psychiatric long-term consequences could be observed in the form of an escalation in PTSD, depression and depressive symptoms, anxiety disorders, and perhaps even more severe mental illnesses such as psychosis. A variety of neurological sequelae have also been hypothesized.
This editorial will hopefully encourage many future considerations. Firstly, clinicians should be aware of the distant burden of neuropsychiatric distress that is potentially linked to COVID-19 infections. Careful attention should be given to survivors, in order to prevent or anticipate possible complications. It might be essential to mention an eventual wave of suicidality as the endpoint of unrecognized depressive syndromes or other severe mental distress. A patient's cognitive examination should also be included in long-term monitoring, exploring executive functions, memory, attention, and information processing.
As possible strategies of intervention against this wave, implementation of telehealth and digital medicine should be cited. Although these are promising and effective ways to deliver health assistance, mainly if applied for mental health purposes, they are still underused in many countries[36]. Research carried out during the pandemic's acute outbreak shows promising results in this field[37].
In the event of the likely impact of neuropsychiatric sequelae on the health system, it would be crucial to focus our efforts on strong-effectiveness interventions. Depression, anxiety, PTSD, and other emerging issues should be addressed with evidence-based and easy-delivered treatments. Besides from telehealth platforms, group interventions should also be implemented in response to the expected increase in psychological needs.
As treatment approaches for COVID-19 neuropsychiatric consequences, we would imagine an important role for physical therapies and neuromodulation techniques, such as transcranial magnetic stimulation or transcranial direct current stimulation. Even if there is still no clear evidence, possible applications of neuromodulation techniques have been underlined[38]. Proposed pathways include regulating anti-inflammatory responses through dorsolateral prefrontal cortex stimulation and improving cognitive outcomes and fatigue. Moreover, the body of literature on the effectiveness of those techniques in many neuropsychiatric disorders has been growing, projecting a promising role for the management of long-term COVID-19 psychiatric sequelae[39,40].
In conclusion, all these considerations underline the need for a watchful follow-up on neuropsychiatric symptoms related to COVID-19 in order to understand the trajectories of possible neuropsychiatric outcomes in the future. Careful research, based mainly on longitudinal and prospective studies will be vital in this field, both for clinical and scientific purposes.
Provenance and peer review: Invited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Psychiatry
Country/Territory of origin: Italy
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Navarro-Alvarez N, Mexico A-Editor: Xiao YY S-Editor: Wu YXJ L-Editor: Filipodia P-Editor: Wu YXJ
| 2. | De Berardis D, Fornaro M, Vellante F, Orsolini L, Tomasetti C, Ventriglio A, Giannantonio MD. Earthquakes, economic crisis and, now, COVID-19: the cry of yell of Central Italy. Psychiatry Res. 2020;291:113181. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 3. | Xu Z, Li S, Tian S, Li H, Kong LQ. Full spectrum of COVID-19 severity still being depicted. Lancet. 2020;395:947-948. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 62] [Cited by in RCA: 59] [Article Influence: 11.8] [Reference Citation Analysis (0)] |
| 4. | Yuki K, Fujiogi M, Koutsogiannaki S. COVID-19 pathophysiology: A review. Clin Immunol. 2020;215:108427. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1218] [Cited by in RCA: 1192] [Article Influence: 238.4] [Reference Citation Analysis (0)] |
| 5. | Wauters E, Thevissen K, Wouters C, Bosisio FM, De Smet F, Gunst J, Humblet-Baron S, Lambrechts D, Liston A, Matthys P, Neyts J, Proost P, Weynand B, Wauters J, Tejpar S, Garg AD. Establishing a Unified COVID-19 "Immunome": Integrating Coronavirus Pathogenesis and Host Immunopathology. Front Immunol. 2020;11:1642. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 9] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 6. | Ellul MA, Benjamin L, Singh B, Lant S, Michael BD, Easton A, Kneen R, Defres S, Sejvar J, Solomon T. Neurological associations of COVID-19. Lancet Neurol. 2020;19:767-783. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1512] [Cited by in RCA: 1394] [Article Influence: 278.8] [Reference Citation Analysis (0)] |
| 7. | Rogers JP, Chesney E, Oliver D, Pollak TA, McGuire P, Fusar-Poli P, Zandi MS, Lewis G, David AS. Psychiatric and neuropsychiatric presentations associated with severe coronavirus infections: a systematic review and meta-analysis with comparison to the COVID-19 pandemic. Lancet Psychiatry. 2020;7:611-627. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1673] [Cited by in RCA: 1523] [Article Influence: 304.6] [Reference Citation Analysis (0)] |
| 8. | Mao L, Jin H, Wang M, Hu Y, Chen S, He Q, Chang J, Hong C, Zhou Y, Wang D, Miao X, Li Y, Hu B. Neurologic Manifestations of Hospitalized Patients With Coronavirus Disease 2019 in Wuhan, China. JAMA Neurol. 2020;77:683-690. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4761] [Cited by in RCA: 4704] [Article Influence: 940.8] [Reference Citation Analysis (0)] |
| 9. | Varatharaj A, Thomas N, Ellul MA, Davies NWS, Pollak TA, Tenorio EL, Sultan M, Easton A, Breen G, Zandi M, Coles JP, Manji H, Al-Shahi Salman R, Menon DK, Nicholson TR, Benjamin LA, Carson A, Smith C, Turner MR, Solomon T, Kneen R, Pett SL, Galea I, Thomas RH, Michael BD; CoroNerve Study Group. Neurological and neuropsychiatric complications of COVID-19 in 153 patients: a UK-wide surveillance study. Lancet Psychiatry. 2020;7:875-882. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 866] [Cited by in RCA: 891] [Article Influence: 178.2] [Reference Citation Analysis (0)] |
| 10. | Mirfazeli FS, Sarabi-Jamab A, Jahanbakhshi A, Kordi A, Javadnia P, Shariat SV, Aloosh O, Almasi-Dooghaee M, Faiz SHR. Neuropsychiatric manifestations of COVID-19 can be clustered in three distinct symptom categories. Sci Rep. 2020;10:20957. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 21] [Cited by in RCA: 26] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 11. | Kumar S, Veldhuis A, Malhotra T. Neuropsychiatric and Cognitive Sequelae of COVID-19. Front Psychol. 2021;12:577529. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 65] [Cited by in RCA: 73] [Article Influence: 18.3] [Reference Citation Analysis (0)] |
| 12. | Lam MH, Wing YK, Yu MW, Leung CM, Ma RC, Kong AP, So WY, Fong SY, Lam SP. Mental morbidities and chronic fatigue in severe acute respiratory syndrome survivors: long-term follow-up. Arch Intern Med. 2009;169:2142-2147. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 399] [Cited by in RCA: 493] [Article Influence: 32.9] [Reference Citation Analysis (0)] |
| 13. | Lee AM, Wong JG, McAlonan GM, Cheung V, Cheung C, Sham PC, Chu CM, Wong PC, Tsang KW, Chua SE. Stress and psychological distress among SARS survivors 1 year after the outbreak. Can J Psychiatry. 2007;52:233-240. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 695] [Cited by in RCA: 688] [Article Influence: 38.2] [Reference Citation Analysis (0)] |
| 14. | Mak IW, Chu CM, Pan PC, Yiu MG, Chan VL. Long-term psychiatric morbidities among SARS survivors. Gen Hosp Psychiatry. 2009;31:318-326. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 649] [Cited by in RCA: 617] [Article Influence: 38.6] [Reference Citation Analysis (0)] |
| 15. | Okusaga O, Yolken RH, Langenberg P, Lapidus M, Arling TA, Dickerson FB, Scrandis DA, Severance E, Cabassa JA, Balis T, Postolache TT. Association of seropositivity for influenza and coronaviruses with history of mood disorders and suicide attempts. J Affect Disord. 2011;130:220-225. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 122] [Cited by in RCA: 108] [Article Influence: 7.7] [Reference Citation Analysis (0)] |
| 16. | Brown AS, Derkits EJ. Prenatal infection and schizophrenia: a review of epidemiologic and translational studies. Am J Psychiatry. 2010;167:261-280. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 884] [Cited by in RCA: 944] [Article Influence: 62.9] [Reference Citation Analysis (0)] |
| 17. | Khandaker GM, Zimbron J, Dalman C, Lewis G, Jones PB. Childhood infection and adult schizophrenia: a meta-analysis of population-based studies. Schizophr Res. 2012;139:161-168. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 171] [Cited by in RCA: 185] [Article Influence: 14.2] [Reference Citation Analysis (0)] |
| 18. | Severance EG, Dickerson FB, Viscidi RP, Bossis I, Stallings CR, Origoni AE, Sullens A, Yolken RH. Coronavirus immunoreactivity in individuals with a recent onset of psychotic symptoms. Schizophr Bull. 2011;37:101-107. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 121] [Cited by in RCA: 136] [Article Influence: 9.7] [Reference Citation Analysis (0)] |
| 19. | Desforges M, Le Coupanec A, Dubeau P, Bourgouin A, Lajoie L, Dubé M, Talbot PJ. Human Coronaviruses and Other Respiratory Viruses: Underestimated Opportunistic Pathogens of the Central Nervous System? Viruses. 2019;12. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 590] [Cited by in RCA: 707] [Article Influence: 117.8] [Reference Citation Analysis (0)] |
| 20. | Jha NK, Ojha S, Jha SK, Dureja H, Singh SK, Shukla SD, Chellappan DK, Gupta G, Bhardwaj S, Kumar N, Jeyaraman M, Jain R, Muthu S, Kar R, Kumar D, Goswami VK, Ruokolainen J, Kesari KK, Dua K. Evidence of Coronavirus (CoV) Pathogenesis and Emerging Pathogen SARS-CoV-2 in the Nervous System: A Review on Neurological Impairments and Manifestations. J Mol Neurosci. 2021;71:2192-2209. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 101] [Cited by in RCA: 90] [Article Influence: 22.5] [Reference Citation Analysis (0)] |
| 21. | Netland J, Meyerholz DK, Moore S, Cassell M, Perlman S. Severe acute respiratory syndrome coronavirus infection causes neuronal death in the absence of encephalitis in mice transgenic for human ACE2. J Virol. 2008;82:7264-7275. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 869] [Cited by in RCA: 963] [Article Influence: 56.6] [Reference Citation Analysis (0)] |
| 22. | Arbour N, Day R, Newcombe J, Talbot PJ. Neuroinvasion by human respiratory coronaviruses. J Virol. 2000;74:8913-8921. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 368] [Cited by in RCA: 380] [Article Influence: 15.2] [Reference Citation Analysis (0)] |
| 23. | Kim JE, Heo JH, Kim HO, Song SH, Park SS, Park TH, Ahn JY, Kim MK, Choi JP. Neurological Complications during Treatment of Middle East Respiratory Syndrome. J Clin Neurol. 2017;13:227-233. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 324] [Cited by in RCA: 362] [Article Influence: 45.3] [Reference Citation Analysis (0)] |
| 24. | Daly JL, Simonetti B, Klein K, Chen KE, Williamson MK, Antón-Plágaro C, Shoemark DK, Simón-Gracia L, Bauer M, Hollandi R, Greber UF, Horvath P, Sessions RB, Helenius A, Hiscox JA, Teesalu T, Matthews DA, Davidson AD, Collins BM, Cullen PJ, Yamauchi Y. Neuropilin-1 is a host factor for SARS-CoV-2 infection. Science. 2020;370:861-865. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 669] [Cited by in RCA: 937] [Article Influence: 187.4] [Reference Citation Analysis (0)] |
| 25. | Cantuti-Castelvetri L, Ojha R, Pedro LD, Djannatian M, Franz J, Kuivanen S, van der Meer F, Kallio K, Kaya T, Anastasina M, Smura T, Levanov L, Szirovicza L, Tobi A, Kallio-Kokko H, Österlund P, Joensuu M, Meunier FA, Butcher SJ, Winkler MS, Mollenhauer B, Helenius A, Gokce O, Teesalu T, Hepojoki J, Vapalahti O, Stadelmann C, Balistreri G, Simons M. Neuropilin-1 facilitates SARS-CoV-2 cell entry and infectivity. Science. 2020;370:856-860. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1507] [Cited by in RCA: 1380] [Article Influence: 276.0] [Reference Citation Analysis (0)] |
| 26. | De Berardis D. How concerned should we be about neurotropism of SARS-Cov-2? CNS Spectr. 2020;1-6. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 14] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 27. | Woo MS, Malsy J, Pöttgen J, Seddiq Zai S, Ufer F, Hadjilaou A, Schmiedel S, Addo MM, Gerloff C, Heesen C, Schulze Zur Wiesch J, Friese MA. Frequent neurocognitive deficits after recovery from mild COVID-19. Brain Commun. 2020;2:fcaa205. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 131] [Cited by in RCA: 231] [Article Influence: 46.2] [Reference Citation Analysis (0)] |
| 28. | Wu Y, Xu X, Chen Z, Duan J, Hashimoto K, Yang L, Liu C, Yang C. Nervous system involvement after infection with COVID-19 and other coronaviruses. Brain Behav Immun. 2020;87:18-22. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1219] [Cited by in RCA: 1255] [Article Influence: 251.0] [Reference Citation Analysis (0)] |
| 29. | Chen Y, Huang X, Zhang C, An Y, Liang Y, Yang Y, Liu Z. Prevalence and predictors of posttraumatic stress disorder, depression and anxiety among hospitalized patients with coronavirus disease 2019 in China. BMC Psychiatry. 2021;21:80. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 34] [Cited by in RCA: 42] [Article Influence: 10.5] [Reference Citation Analysis (0)] |
| 30. | Sparks SW. Posttraumatic Stress Syndrome: What Is It? J Trauma Nurs. 2018;25:60-65. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 18] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 31. | Bo HX, Li W, Yang Y, Wang Y, Zhang Q, Cheung T, Wu X, Xiang YT. Posttraumatic stress symptoms and attitude toward crisis mental health services among clinically stable patients with COVID-19 in China. Psychol Med. 2021;51:1052-1053. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 400] [Cited by in RCA: 419] [Article Influence: 104.8] [Reference Citation Analysis (0)] |
| 32. | Wang C, Pan R, Wan X, Tan Y, Xu L, McIntyre RS, Choo FN, Tran B, Ho R, Sharma VK, Ho C. A longitudinal study on the mental health of general population during the COVID-19 epidemic in China. Brain Behav Immun. 2020;87:40-48. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1759] [Cited by in RCA: 1584] [Article Influence: 316.8] [Reference Citation Analysis (0)] |
| 33. | Troyer EA, Kohn JN, Hong S. Are we facing a crashing wave of neuropsychiatric sequelae of COVID-19? Brain Behav Immun. 2020;87:34-39. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 665] [Cited by in RCA: 620] [Article Influence: 124.0] [Reference Citation Analysis (0)] |
| 34. | Tavormina G, Tavormina MGM, Franza F, Aldi G, Amici P, Amorosi M, Anzallo C, Cervone A, Costa D, D'Errico I, De Berardis D, Di Napoli W, Elisei S, Felisio B, Ferella G, Harnic D, Juli MR, Lisa G, Litta A, Marcasciano S, Mazza A, Meloni E, Mendolicchio L, Min MV, Moretti P, Perito M, Russiello M, Sanna JT, Sidari A, Sinisi I, Solomita B, Spurio MG, Stranieri G, Tavormina R, Vacca A, Vellante F, Vitarisi S, Shin YW, Chung S. A New Rating Scale (SAVE-9) to Demonstrate the Stress and Anxiety in the Healthcare Workers During the COVID-19 Viral Epidemic. Psychiatr Danub. 2020;32:5-9. [PubMed] |
| 35. | Martinotti G, Alessi MC, Di Natale C, Sociali A, Ceci F, Lucidi L, Picutti E, Di Carlo F, Corbo M, Vellante F, Fiori F, Tourjansky G, Catalano G, Carenti ML, Incerti CC, Bartoletti L, Barlati S, Romeo VM, Verrastro V, De Giorgio F, Valchera A, Sepede G, Casella P, Pettorruso M, di Giannantonio M. Psychopathological Burden and Quality of Life in Substance Users During the COVID-19 Lockdown Period in Italy. Front Psychiatry. 2020;11:572245. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 39] [Cited by in RCA: 51] [Article Influence: 10.2] [Reference Citation Analysis (0)] |
| 36. | Di Carlo F, Sociali A, Picutti E, Pettorruso M, Vellante F, Verrastro V, Martinotti G, di Giannantonio M. Telepsychiatry and other cutting-edge technologies in COVID-19 pandemic: Bridging the distance in mental health assistance. Int J Clin Pract. 2021;75. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 73] [Cited by in RCA: 105] [Article Influence: 26.3] [Reference Citation Analysis (0)] |
| 37. | Liu S, Yang L, Zhang C, Xiang YT, Liu Z, Hu S, Zhang B. Online mental health services in China during the COVID-19 outbreak. Lancet Psychiatry. 2020;7:e17-e18. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1118] [Cited by in RCA: 1087] [Article Influence: 217.4] [Reference Citation Analysis (0)] |
| 38. | Baptista AF, Baltar A, Okano AH, Moreira A, Campos ACP, Fernandes AM, Brunoni AR, Badran BW, Tanaka C, de Andrade DC, da Silva Machado DG, Morya E, Trujillo E, Swami JK, Camprodon JA, Monte-Silva K, Sá KN, Nunes I, Goulardins JB, Bikson M, Sudbrack-Oliveira P, de Carvalho P, Duarte-Moreira RJ, Pagano RL, Shinjo SK, Zana Y. Applications of Non-invasive Neuromodulation for the Management of Disorders Related to COVID-19. Front Neurol. 2020;11:573718. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 36] [Cited by in RCA: 40] [Article Influence: 8.0] [Reference Citation Analysis (0)] |
| 39. | Martinotti G, Lupi M, Montemitro C, Miuli A, Di Natale C, Spano MC, Mancini V, Lorusso M, Stigliano G, Tambelli A, Di Carlo F, Di Caprio L, Fraticelli S, Chillemi E, Pettorruso M, Sepede G, di Giannantonio M. Transcranial Direct Current Stimulation Reduces Craving in Substance Use Disorders: A Double-blind, Placebo-Controlled Study. J ECT. 2019;35:207-211. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 40] [Article Influence: 6.7] [Reference Citation Analysis (0)] |
| 40. | Lefaucheur JP, André-Obadia N, Antal A, Ayache SS, Baeken C, Benninger DH, Cantello RM, Cincotta M, de Carvalho M, De Ridder D, Devanne H, Di Lazzaro V, Filipović SR, Hummel FC, Jääskeläinen SK, Kimiskidis VK, Koch G, Langguth B, Nyffeler T, Oliviero A, Padberg F, Poulet E, Rossi S, Rossini PM, Rothwell JC, Schönfeldt-Lecuona C, Siebner HR, Slotema CW, Stagg CJ, Valls-Sole J, Ziemann U, Paulus W, Garcia-Larrea L. Evidence-based guidelines on the therapeutic use of repetitive transcranial magnetic stimulation (rTMS). Clin Neurophysiol. 2014;125:2150-2206. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1225] [Cited by in RCA: 1372] [Article Influence: 124.7] [Reference Citation Analysis (0)] |