Published online May 19, 2022. doi: 10.5498/wjp.v12.i5.739
Peer-review started: October 28, 2021
First decision: December 12, 2021
Revised: December 24, 2021
Accepted: April 9, 2022
Article in press: April 9, 2022
Published online: May 19, 2022
Processing time: 201 Days and 7.2 Hours
Over the last few decades, 3 pathogenic pandemics have impacted the global population; severe acute respiratory syndrome coronavirus (SARS-CoV), Middle East respiratory syndrome coronavirus (MERS-CoV) and SARS-CoV-2. The global disease burden has attributed to millions of deaths and morbidities, with the majority being attributed to SARS-CoV-2. As such, the evaluation of the mental health (MH) impact across healthcare professionals (HCPs), patients and the general public would be an important facet to evaluate to better understand short, medium and long-term exposures.
To identify and report: (1) MH conditions commonly observed across all 3 pandemics; (2) Impact of MH outcomes across HCPs, patients and the general public associated with all 3 pandemics; and (3) The prevalence of the MH impact and clinical epidemiological significance.
A systematic methodology was developed and published on PROSPERO (CRD42021228697). The databases PubMed, EMBASE, ScienceDirect and the Cochrane Central Register of Controlled Trials were used as part of the data extraction process, and publications from January 1, 1990 to August 1, 2021 were searched. MeSH terms and keywords used included Mood disorders, PTSD, Anxiety, Depression, Psychological stress, Psychosis, Bipolar, Mental Health, Unipolar, Self-harm, BAME, Psychiatry disorders and Psychological distress. The terms were expanded with a ‘snowballing’ method. Cox-regression and the Monte-Carlo simulation method was used in addition to I2 and Egger’s tests to determine heterogeneity and publication bias.
In comparison to MERS and SARS-CoV, it is evident SAR-CoV-2 has an ongoing MH impact, with emphasis on depression, anxiety and post-traumatic stress disorder.
It was evident MH studies during MERS and SARS-CoV was limited in comparison to SARS-CoV-2, with much emphasis on reporting symptoms of depression, anxiety, stress and sleep dis
Core Tip: Global research into exploring pandemics have been conducted for several decades. However, clinical research associated with mental health (MH) impact of Middle East respiratory syndrome, severe acute respiratory syndrome coronavirus (SARS-CoV) and SARS-CoV-2 was limited. This systematic review and meta-analysis is a comparison of the MH impact across, healthcare professionals, patients and the general public using the Monte-Carlo simulation method. Evaluated prevalence of multiple MH variables have been conducted using randomised controlled trials and cross-sectional studies. The study demonstrates the need to conduct comprehensive and longitudinal multi-morbid research to evaluate the true MH impact to aid better future pandemic preparedness. This systematic review and meta-analysis indicate a complex MH impact across all cohorts with the requirement for mechanistic relationships between physical and MH to be explored further.
- Citation: Delanerolle G, Zeng Y, Shi JQ, Yeng X, Goodison W, Shetty A, Shetty S, Haque N, Elliot K, Ranaweera S, Ramakrishnan R, Raymont V, Rathod S, Phiri P. Mental health impact of the Middle East respiratory syndrome, SARS, and COVID-19: A comparative systematic review and meta-analysis. World J Psychiatry 2022; 12(5): 739-765
- URL: https://www.wjgnet.com/2220-3206/full/v12/i5/739.htm
- DOI: https://dx.doi.org/10.5498/wjp.v12.i5.739
Human civilisations have endeavoured various infectious diseases over centuries with multiple causatives, increases in population density, and increases in migration could attribute to increase in risk of emerging infectious diseases leading to global endemics and pandemics. Medicine in the modern era provide solutions to manage and mitigate infectious threats although there are many challenges associated with communicable and non-communicable diseases.
Fast forward to the 21st century, there have been three prominent outbreaks caused by novel coronaviruses[1]. The World Health Organisation (WHO) have classified two of these outbreaks as pandemics. Understanding the coronavirus family to prevent future pandemics would be useful.
The 2003 severe acute respiratory syndrome (SARS)-associated coronavirus (SARS-CoV) comprised of the Middle East respiratory syndrome coronavirus (MERS-CoV) which includes a family of enveloped, single-stranded and diverse RNA viruses consisting of four genera: alpha, beta, gamma and delta (α-, β-, γ- and δ-CoV). Of these, alpha and beta-coronaviruses appear to be more deadly due to its ability to transmit across animals and humans, leading to stronger pathogens. Coronaviruses were first identified in 1965[2]. The SARS-CoV was the first outbreak in 2012. Neither of the outbreaks reached a pandemic status. Genetically similar to SARS-CoV, the severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2), officially declared as a pandemic on March 11, 2020, continues to engulf global populations.
In comparison to the current SARS-CoV-2 pandemic, the SARS-CoV outbreak was effectively managed with aggressive public health measures amongst the countries affected[3]. Although, there are multi-factorial composites to consider to assess physical and mental health impact on the previous and current populations. For example, SARS-CoV reported an incidence and mortality of 8096 and 774 respectively across 29 countries[4].
In contrast, MERS-CoV outbreaks were reported across 27 countries between 2012-2019, mainly within the Middle East, with Saudi Arabia reporting majority of the cases based on WHO data[5]. However, incidence reporting of MERS-CoV over the last 7 years have been sporadic, indicating it is less contagious compared to the current SARS-CoV-2 infection. To date, there have been 2578 reported cases and 888 deaths due to MERS-CoV, with a crude mortality rate of around 34.4%[5]. Management of these infections primarily consist of public health measures to identify and isolate patients and effective infection control measures to reduce transmission rates[6]. Failures in effectively managing these outbreaks have primarily been attributed to the late identification of the disease. Secondary measures include quarantine failures due to non-disclosures by patients and poor communication between officials and the public[7,8].
Most patients with SARS-COV-2 are asymptomatic or develop mild symptoms[9]. However, for a small minority, they are likely to require admission to hospital with severe respiratory compromise which can lead to critical illness with respiratory failure and multiple organ failure[9]. These cases require high-level medical care within an intensive care unit (ICU) setting, including ventilatory support. Dexamethasone and Remdesivir are used alongside supportive measures and have proved effective in reducing mortality and hospital length of stay[10,11]. Interventions such as pruning, which has been recommended in the treatment of severe COVID-19 disease[12], have become common place in ICU settings, but is a labour-intensive procedure, putting further pressure on staff.
The high degree of viral homology between SARS-COV-2 and previous coronavirus outbreaks directed the initial global response to the coronavirus disease 2019 (COVID-19) pandemic[13]. Given the relatively small population sizes involved in the first two novel coronavirus outbreaks, in addition to the geographical areas affected, the global understanding that shaped our response was probably limited in its scope. We recognise now it is in fact the differences, not the similarities, that have driven the rapid spread of the virus, including more prominent community spread and higher transmissibility of SARS-CoV-2, which includes asymptomatic and mildly symptomatic patients not seen in SARS-CoV[14].
The characteristics of the emerging SARS-CoV-2 appears to be changing with the appearance of new variants, which is different to its predecessors, SARS-CoV and MERS-CoV. At the height of the SARS-CoV era, 140 new infections were reported per week, whilst current data suggest SARS-CoV-2 transmits approximately 100000 new infections per week during its peak period between February and May 2020[15,16]. In addition to the common transmission network, viral shedding for SARS-CoV-2 in particular starts prior to symptom onset, which was the opposite with SARS-CoV. Therefore, quarantine measures would have been more effective during SARS-CoV in comparison to SARS-CoV-2.
One of the long-term unknowns about the current pandemic is the physical manifestations and its impact on the mental health as well as the well-being of the public, patients and front-line healthcare professionals (HCPs). Experience from the previous novel coronavirus outbreaks suggests that the psychological impacts will be widespread and long-lasting. Significant psychological symptomatology has been reported in the acute and early recovery phases associated with SARS-CoV[17-22] and MERS-CoV[17,23] in all three groups considered in this review. Importantly, when considering the long-term effects of this pandemic, the impact of the SARS-CoV pandemic was still recorded amongst infected individuals over four years after the reported outbreak, and in some cases with deteriorating symptoms[13].
The morphological and demographic features of the 3 viruses are vital to understand the mental health impact. Physical manifestations drive the mental health impact, often interacting as a planarian.
A systematic review protocol was designed, internally peer-reviewed and published on PROSPERO (CRD42021228697) with a comprehensive search strategy and data extraction method.
This study has 3 primary aims of identifying and reporting: (1) Mental health (MH) conditions commonly observed across all 3 pandemics; (2) Impact of MH outcomes across HCPs, patients and the general public associated with all 3 pandemics; and (3) The prevalence of the MH impact and clinical epidemiological significance.
Multiple databases of PubMed, EMBASE, ScienceDirect and the Cochrane Central Register of Controlled Trials were used to extract relevant data. MeSH terms and keywords used included Mood disorders, PTSD, Anxiety, Depression, Psychological stress, Psychosis, Bipolar, Mental Health, Unipolar, Self-harm, BAME (Black, Asian and Minority Ethnic), Psychiatry disorders and Psychological distress. The terms were expanded with a ‘snowball’ method that has been demonstrated with a PRISMA diagram. All publications that were peer-reviewed in English were included. The final dataset was reviewed independently before the analysis was conducted.
The data synthesis is based on the statistical data extracted from the studies included based on the eligibility criteria developed. This includes data associated with the mean ± SD and median along with q1 (25% quantile) and q3 (75% quantile). Q1 and q3 are novel estimation methods used to improve existing meta-analysis as demonstrated by Wan and colleagues[24]. Most of the studies identified reported multiple MH outcomes such as depression, anxiety and psychological distress among people who experienced MERS, SARS-CoV and SARS-CoV-2. For studies that reported the median along with q1 and q3, the mean ± SD of the studies were estimated from the median, q1 and q3. Therefore, the following equation was used to analyse the data, where the Ф-1 represented the inverse of the standard normal distribution, as described below.
Most MERS-CoV studies only reported SD. Some studies included the median only, and these were transformed to q1 and q3, where the mean ± SD were estimated using the Monte-Carlo simulation method, with the cut off scores of the MH assessments used within the studies. This data was assumed to be normally distributed. Random effects models were used to conduct the meta-analysis to estimate the pooled prevalence. MH assessments reported within the studies included the Impact of Event Scale-Revised (IES-R), Hospital Anxiety and Depression Scale (HADS), Patient Health Questionnaire (PHQ-9), Short Form 36 Health Survey (SF-36), General Anxiety Disorder (GAD-7) and State-Trait Anger Expression Inventory (STAXI). For this we assumed normal distribution of the data. A subgroup analysis was conducted to evaluate any identified heterogeneity. Funnel plots and Egger’s tests were performed to demonstrate publication bias and a sensitivity analysis. A comparative analysis was conducted using the SAR-CoV and SARS-CoV-2 data published by Chau et al[25].
The full data analysis was conducted using the STATA 16.1 software application.
A quality assessment was performed using the Newcastle-Ottawa-Scale (NOS) for studies included systematically (Supplementary Table 1). The NOS is an eight-item scale with three quality parameters: (1) Selection; (2) Comparability; and (3) Outcome. We rated the quality of the studies (good, fair and poor) by allocating each domain with stars in this manner: (1) A Good quality score was awarded 3 or 4 stars in selection, 1 or 2 in comparability, and 2 or 3 stars in outcomes; (2) A Fair quality score was awarded 2 stars in selection, 1 or 2 stars in comparability, and 2 or 3 stars in outcomes; and (3) A Poor quality score was allocated 0 or 1 star(s) in selection, 0 stars in comparability, and 0 or 1 star(s) in outcomes domain.
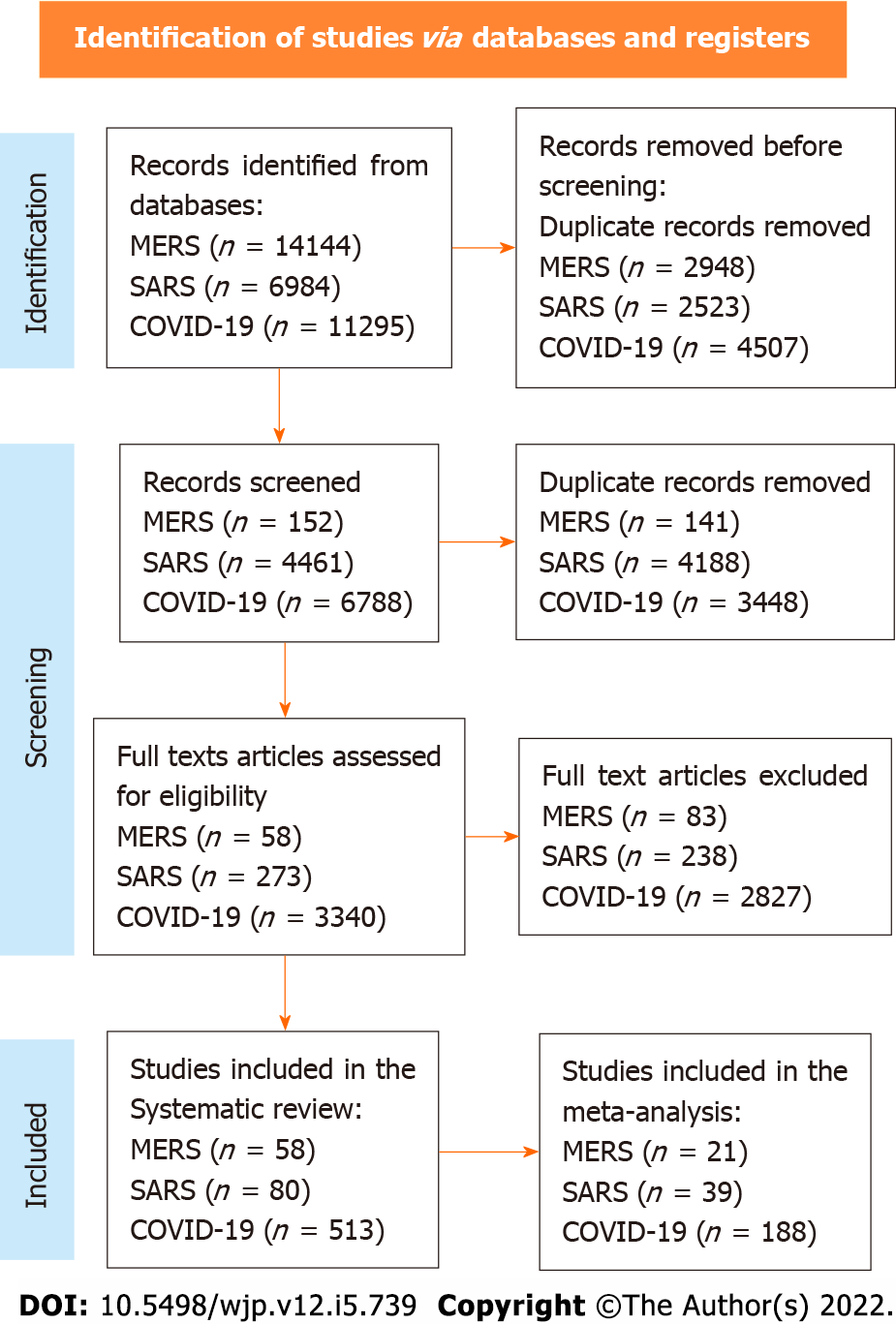
The comprehensive multiple database literature search included publications from January 1, 1990 to August 1, 2021. The PRISMA diagram reflects the total yielded studies and systematic inclusions prior to the completion of the meta-analysis as shown in Figure 1.
A total of 58 studies were included in the systematic review for MERS as shown in Supple
| Study ID | Ref. | Study type | Sample size | Country | Exposure | Outcome | P value | Quality assessment (NOS) |
| 1 | Shin et al[36] | Quantitative | 63 | Korea | MERS patients | PTSD, Sleep problem, anxiety, depression, suicidality, phobic anxiety, addiction, aggression | Not specified | 7 |
| 2 | Um et al[37] | Quantitative | 64 | Korea | MERS patients and HCWs | PTSD, depression | Not specified | 7 |
| 3 | Abolfotouh et al[38] | Quantitative | 1031 | Saudi Arabia | HCWs | Level of Concern | Not specified | 7 |
| 4 | Jung et al[39] | Quantitative | 147 | Korea | HCWs | PTSD | Not specified | 6 |
| 5 | Ahn et al[40] | Quantitative | 63 | Korea | MERS Patients | Suicide, fatigue | Not specified | 6 |
| 6 | Lee et al[41] | Quantitative | 52 | Korea | MERS Patients | Depression, PTSD, fatigue | Not specified | 6 |
| 7 | Kim et al[42] | Quantitative | 112 | Korea | HCWs | PTSD, burnout | Not specified | 7 |
| 8 | Oh et al[43] | Quantitative | 313 | Korea | HCWs | Stress | Stress: 0.066 | 7 |
| 9 | Seo et al[44] | Quantitative | 171 | Korea | HCWs | Burnout | Not specified | 5 |
| 10 | Son et al[45] | Quantitative | 280 | Korea | HCWs and general public | PTSD | Not specified | 6 |
| 11 | Park et al[46] | Quantitative | 187 | Korea | HCWs | Stress | Not specified | 6 |
| 12 | Jeong et al[24] | Qualitative | 1692 | Korea | MERS patients and general public | Anxiety | Not specified | 7 |
| 13 | Al-Rabiaah et al[47] | Quantitative | 174 | Saudi Arabia | General public | Anxiety | Not specified | 7 |
| 14 | Park et al[48] | Quantitative | 63 | Korea | MERS Patients | PTSD, depression | Not specified | 7 |
| 15 | Cho et al[49] | Quantitative | 111 | Korea | General public | PTSD | PTSD: 0.3 | 7 |
| 16 | Kim et al[50] | Quantitative | 27 | Korea | General public | Depression | Not specified | 5 |
| 17 | Lee et al[51] | Quantitative | 359 | Korea | HCWs | PTSD | Not specified | 6 |
| 18 | Kim and Choi[52] | Quantitative | 215 | Korea | HCWs | Burnout, stress | Not specified | 6 |
| 19 | Bukhari et al[53] | Quantitative | 386 | Saudi Arabia | HCWs | Worry | Not specified | 6 |
| 20 | Mollers et al[54] | Quantitative | 72 | Netherlands | General public | PTSD | Not specified | 5 |
| 21 | Kim and Choi[52] | Quantitative | 215 | Korea | HCWs | PTSD: 0.017 | PTSD: 0.017 | 6 |
In relation to the SARS-CoV, the systematic review was conducted on 80 studies, as detailed in Supplementary Table 3, and the meta-analysis included 39 studies, as shown in Table 2.
| Study ID | Ref. | Study type | Sample size | Country/region | Exposure | P value | Quality assessment (NOS) |
| 1 | Kwek et al[20] | Cross-sectional | 360 | Singapore | SARS patients | PTSD: 0.79; Depression: 0.7; Anxiety: 0.51 | 7 |
| 2 | Fang et al[55] | Cross-sectional | 1278 | China | SARS patients | Anxiety: 0.291; Depression: 0.705; PTSD: 0.2 | 8 |
| 3 | Liang[56] | Prospective cohort | 769 | China, Taiwan | SARS patients | PTSD: > 0.05; Anxiety: > 0.05 | 7 |
| 4 | Dang et al[57] | Cross-sectional | 549 | China | General public | Anxiety: < 0.00001; Depression: 0.000361 | 7 |
| 5 | Yip[58] | Prospective cohort | 218 | China, Hong Kong | SARS patients | Not specified | 6 |
| 6 | Cheng et al[59] | Cross-sectional | 10 | China, Hong Kong | SARS patients | Anxiety: > 0.05; Depression: > 0.05 | 5 |
| 7 | Wu et al[60] | Cross-sectional | 286 | China, Hong Kong | SARS patients | PTSD: < 0.001; Depression: < 0.05; Anxiety: < 0.01 | 6 |
| 8 | MaK et al[61] | Retrospective cohort | 126 | China, Hong Kong | SARS patients | Not specified | 5 |
| 9 | Lee et al[62] | Cross-sectional | 10511 | China, Hong Kong | Were not HCWs | Not specified | 7 |
| 10 | Hong et al[63] | Cross-sectional | 1050 | China | SARS patients | PTSD: 0.0323 | 7 |
| 11 | Wang[64] | Prospective cohort | 22 | China | SARS patients | Not specified | 4 |
| 12 | Hu et al[65] | Cross-sectional | 763 | China | Attended hospital for other reasons | Not specified | 5 |
| 13 | Chen et al[66] | Prospective cohort | 325 | China, Taiwan | Non-infected HCWs in the largest obligatory SARS hospital, with high SARS contact | Anxiety: 0.55 Depression: 0.93 | 6 |
| 14 | Ko et al[67] | Cross-sectional | 72 | China, Taiwan | General public of outbreak area | Depression: 0.02 | 5 |
| 15 | Lee et al[21] | Cross-sectional | 114 | China, Hong Kong | General public of outbreak area | Not specified | 6 |
| 16 | Hawryluck et al[68] | Cross-sectional | 652 | Canada, Toronto | General public of outbreak area | Depression: 0.85; PTSD: 0.82 | 7 |
| 17 | Liu et al[69] | Cross-sectional | 96 | China, Beijing | Non-infected HCWs of SARS hospital | Depression: < 0.05 | 7 |
| 18 | Su et al[70] | Prospective cohort | 57 | China, Taiwan | Non-infected HCWs in SARS outbreak region with high exposure risk vs low exposure risk | PTSD: > 0.05; Depression: < 0.05 | 7 |
| 19 | Lam et al[71] | Retrospective cohort | 116 | China, Hong Kong | SARS patients | Not specified | 6 |
| 20 | Shi et al[72] | Prospective cohort | 87 | China, Beijing | SARS outbreak region | Not specified | 5 |
| 21 | Huang et al[73] | Cross-sectional | 4481 | China, Beijing | Were not HCWs | Not specified | 6 |
| 22 | Yu et al[74] | Prospective cohort | 180 | China, Hong Kong | General public of outbreak area | Not specified | 5 |
| 23 | Chang and Sivam[75] | Cross-sectional | 146 | Singapore | General public of outbreak area | Not specified | 5 |
| 24 | Moldofsky and Patcai[76] | Retrospective cohort | 107 | Canada, Toronto | SARS patients, who were HCWs | Not specified | 6 |
| 25 | Sun et al[77] | Prospective cohort | 1557 | China, Xianxi | SARS patients | PTSD: 0.67 | 7 |
| 26 | Lau et al[78] | Cross-sectional | 333 | China, Hong Kong | General public of outbreak area | Not specified | 5 |
| 27 | Reynolds et al[79] | Cross-sectional | 89 | Canada | General public of outbreak area, quarantined; non-infected HCWs in SARS outbreak region, quarantined | Not specified | 5 |
| 28 | Lancee et al[80] | Cross-sectional | 613 | Canada, Toronto | Non-infected HCWs in SARS outbreak region | Not specified | 6 |
| 29 | Lin et al[81] | Cross-sectional | 6280 | China, Taiwan, Taichung | Non-infected HCWs in in region without major SARS outbreak | Not specified | 6 |
| 30 | Gao et al[82] | Prospective cohort | 127 | China, Tianjin | SARS patients | Not specified | 5 |
| 31 | Xu et al[83] | Cross-sectional | 129 | China, Xianxi | Non-infected HCWs in SARS hospital | PTSD: > 0.05 | 6 |
| 32 | Wong et al[84] | Cross-sectional | 0 (?) | China, Hong Kong | Non-infected HCWs from SARS hospitals | Not specified | 4 |
| 33 | Sim et al[85] | Cross-sectional | 90 | Singapore | Non-infected HCWs in SARS outbreak region | Not specified | 5 |
| 34 | Wu et al[19] | Cross-sectional | 133 | China, Beijing | Non-infected HCWs in SARS hospital | Not specified | 6 |
| 35 | Chen et al[86] | Cross-sectional | 103 | China, Taiwan, Kaohsiung | Non-infected HCWs in SARS hospital, with high SARS contact; non-infected HCWs in SARS hospital; with low SARS contact | Not specified | 6 |
| 36 | Tham et al[87] | Cross-sectional | 90 | Singapore | Non-infected HCWs in SARS hospital with extra risk of exposure | Not specified | 5 |
| 37 | Maunder et al[88] | Cross-sectional | 90 | Canada, Toronto | Non-infected HCWs of outbreak area, unspecified (mix of SARS affected and non SARS affected hospitals | PTSD: < 0.01 | 7 |
| 38 | Mak et al[89] | Retrospective cohort | 126 | China, Hong Kong | SARS patient | Not specified | 6 |
| 39 | McAlonan et al[90] | Cross-sectional | 0 (?) | China, Hong Kong | Non-infected HCWs in SARS outbreak region with high exposure risk vs low exposure risk | Not specified | 3 |
A total of 513 studies were included in the systematic review for SARS-CoV-2, as shown in Supplementary Table 4. 287 of these studies are from the meta-analysis conducted by Phiri et al[26]. The meta-analysis was conducted on 188 studies, as demonstrated in Supplementary Table 5.
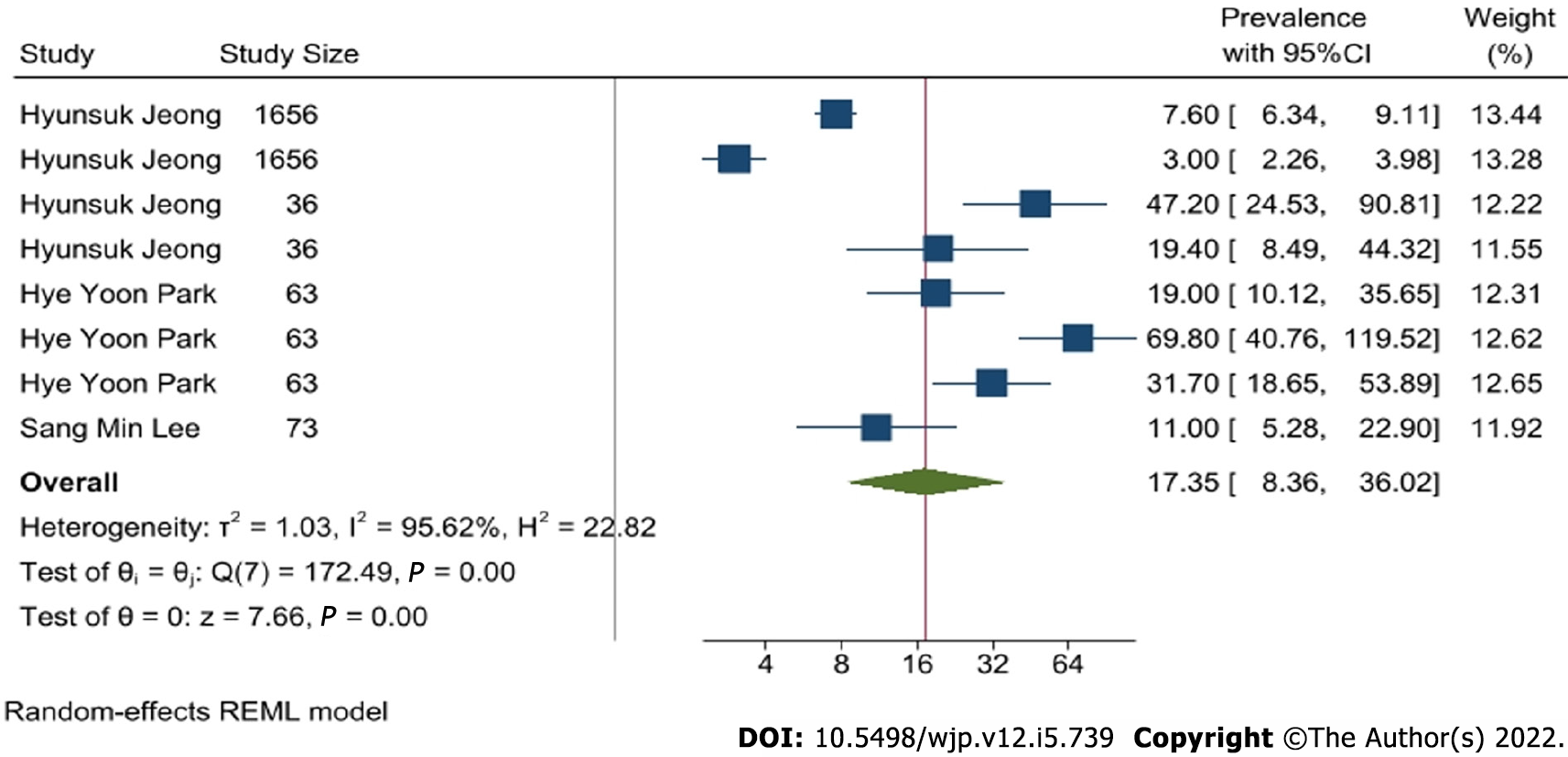
Anxiety: Eight studies reported the prevalence of anxiety during the MERS-CoV outbreak. As demonstrated by Figure 2, the pooled prevalence of anxiety was 17.35% with a 95% confidence interval (CI): 8.36-36.02. A heterogeneity of I2 = 95.62% was identified.
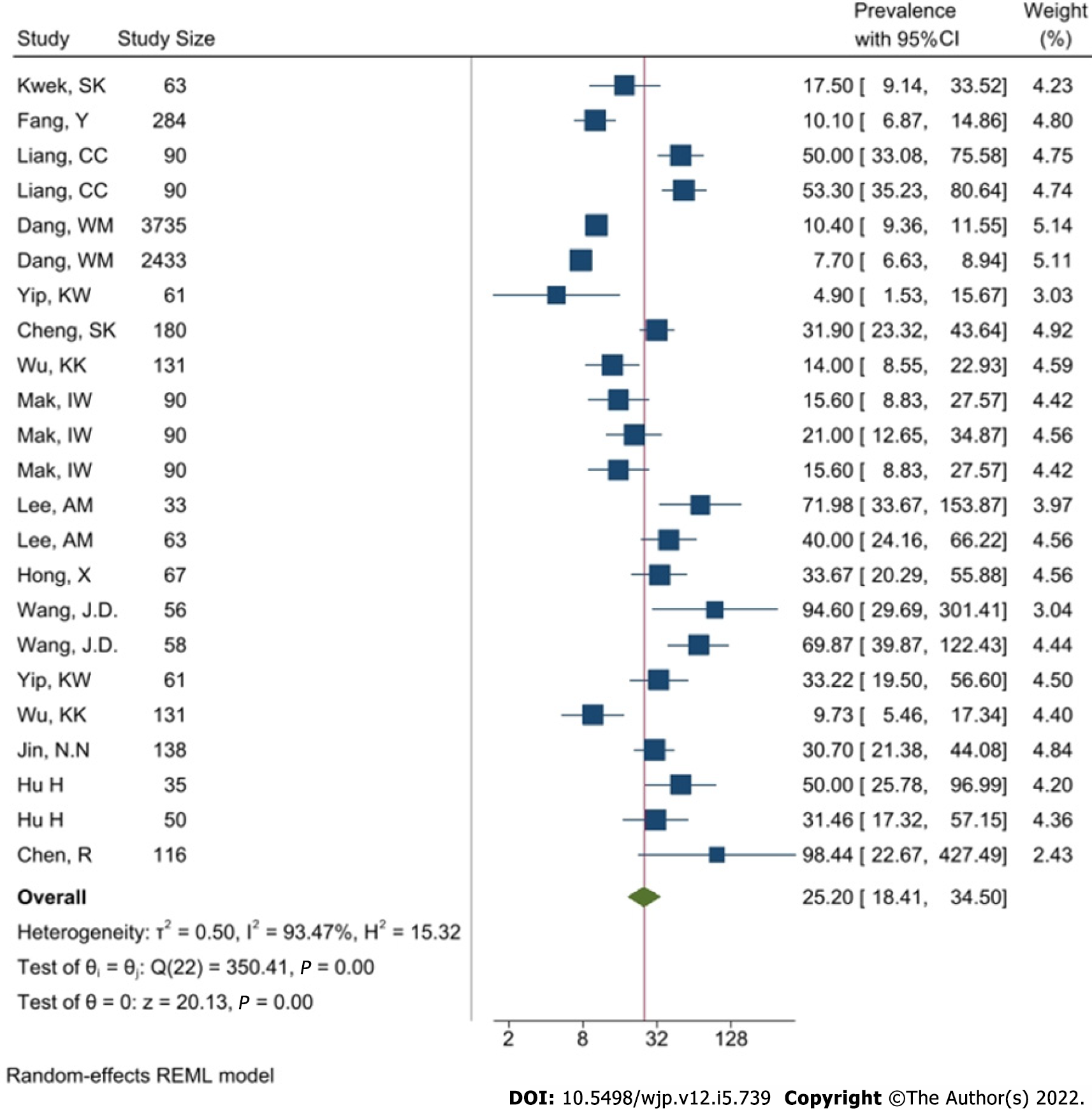
The systematic review indicates 14 studies report the prevalence of anxiety during SARS-CoV, although only 9 report the mean ± SD. Twenty-three studies were included into the meta-analysis. Figure 3 indicates the prevalence of anxiety during SARS-CoV where the pooled prevalence was 25.2%, with a 95%CI of 18.41-34.5. A high heterogeneity of I2 = 93.47% was identified.
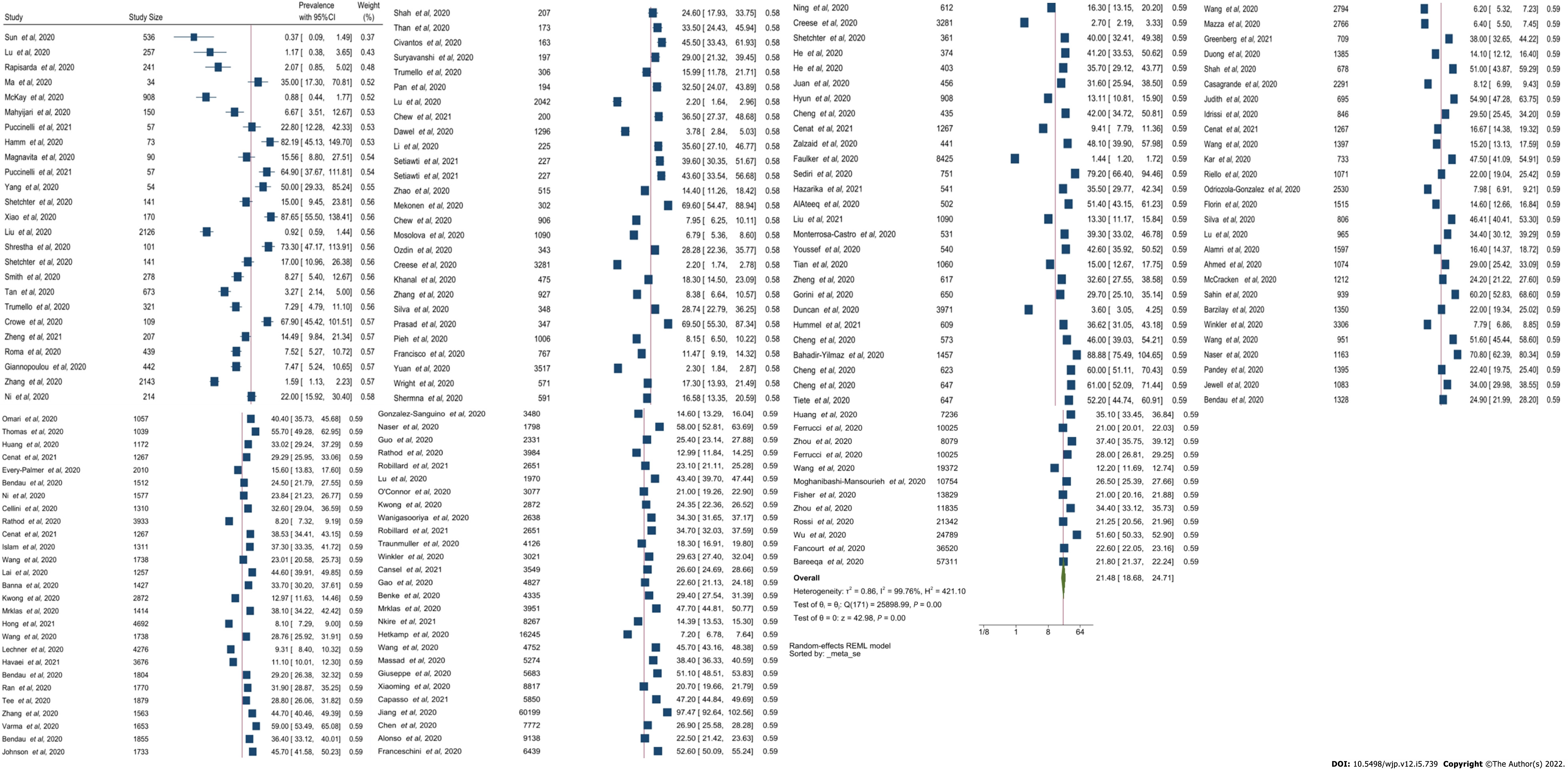
The systematic review identified 175 studies that reported anxiety as an outcome due to SARS-CoV-2 where 40 studies provided mean and SD. By utilizing the Monte-Carlo simulation on the studies that only provide mean and SD, we obtained twenty-five studies that reported the prevalence of anxiety. As for the anxiety resulting from SARS-CoV-2, Figure 4 shows a pooled prevalence of 21.44% with a 95%CI of 18.69-24.61. However, a high heterogeneity of 99.77% was identified.
Based on these results, the prevalence of anxiety during SARS-CoV is more significant in comparison to MERS-CoV and SARS-CoV-2.
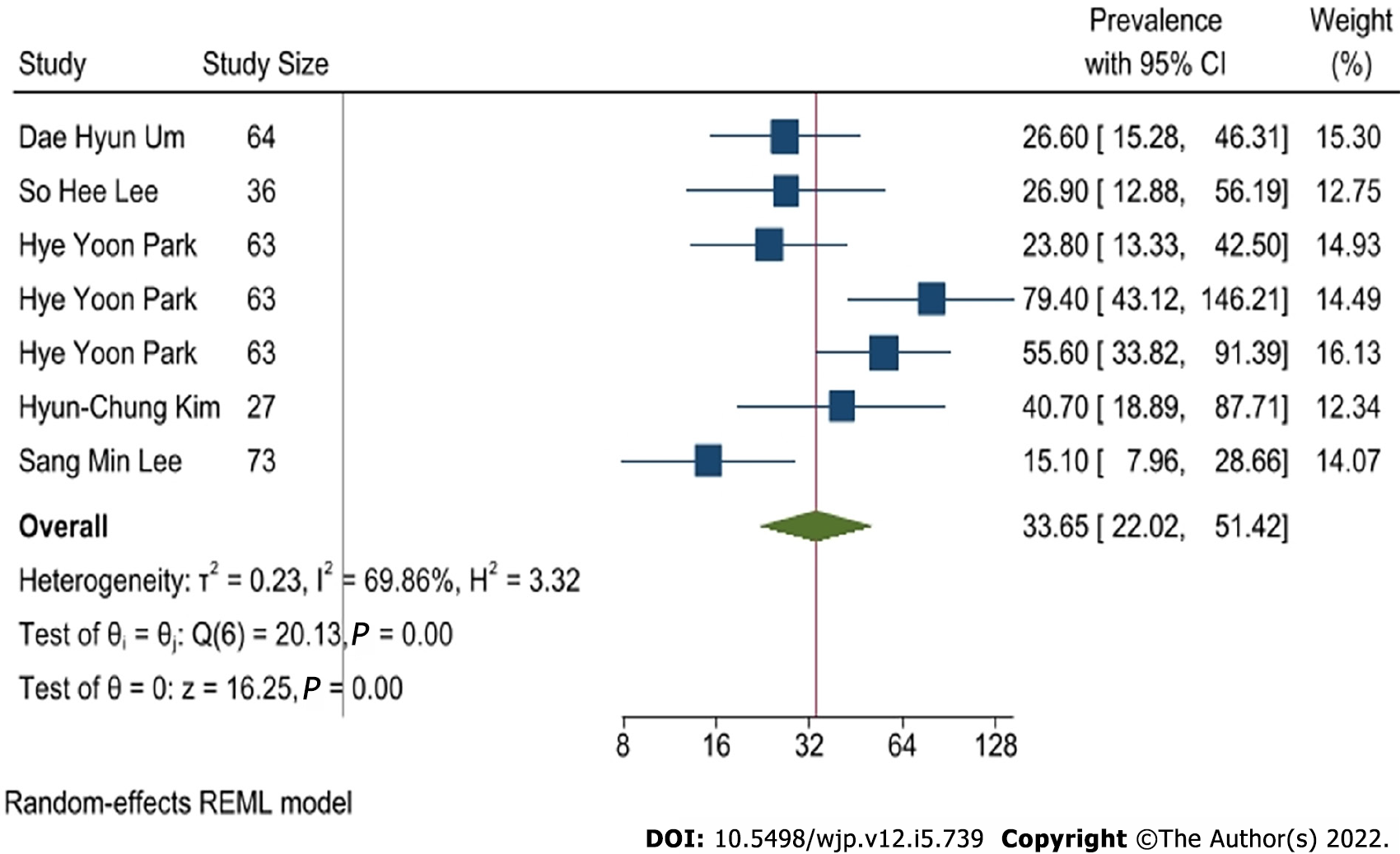
The systematic search for MERS-CoV yielded seven studies reporting depression. The meta-analysis is demonstrated in Figure 5 and shows a pooled prevalence of 33.65%. The 95%CI ranged between 22.02-51.42. A moderate heterogeneity of at I2 = 69.86% was identified.
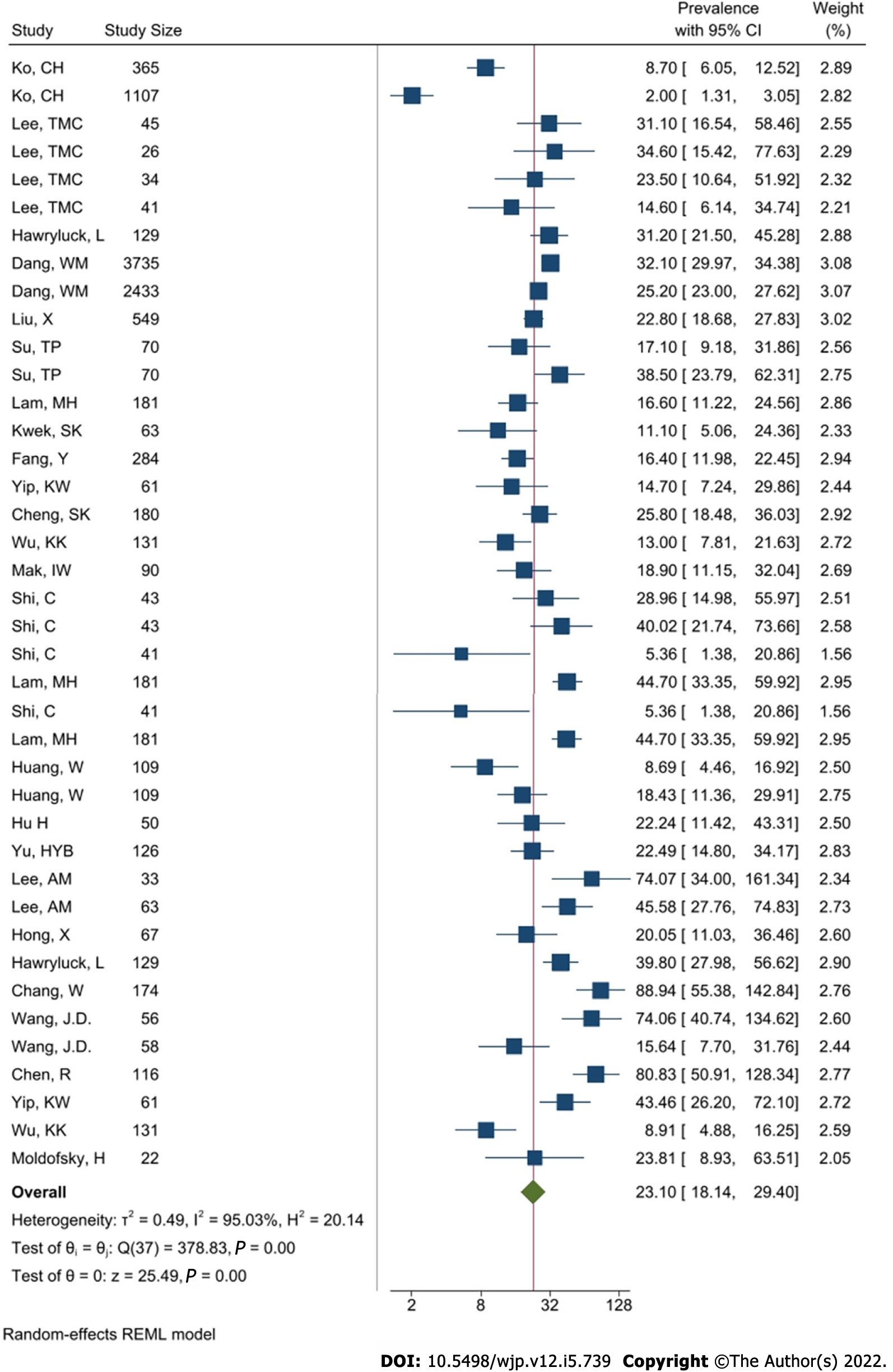
Thirty-eight studies reported the prevalence of depression during the SARS-CoV outbreak. Of these, 23 reported prevalence directly and 15 demonstrated the mean score and SD instead. By using the Monte-Carlo simulation method, thirty-eight results were meta-analysed as demonstrated in Figure 6. The pooled prevalence of depression during the pandemic of SARS-CoV was 23.1%, while the 95%CI was between 18.14-29.4. A high heterogeneity was calculated at I2 = 95.03%.
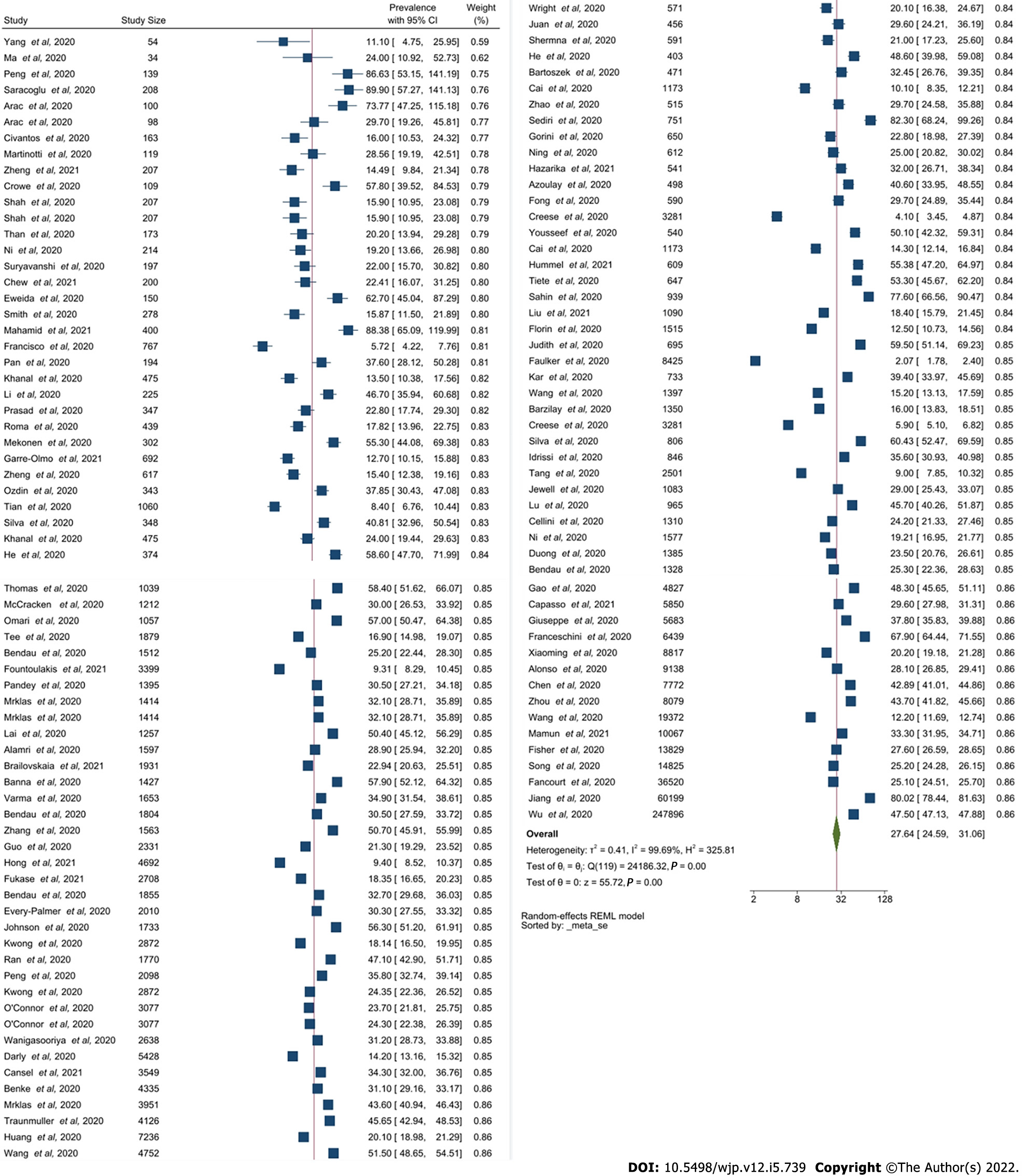
One hundred and twenty-three studies reported on depression during SARS-CoV-2. Of these, 102 reported the prevalence of depression directly and 21 demonstrated mean and SD values only. Figure 7 indicates the pooled prevalence of depression during SARS-CoV-2 was 27.68%, with a 95%CI ranging from 24.67-31.06. A high heterogeneity of I2 = 99.71% was identified.
Based on the analysis, MERS-CoV and SARS-CoV-2 appear to report the highest levels of depression based on the pooled prevalence of 27.64% and 33.65% respectively.
Twenty-seven studies reported post-traumatic stress disorder (PTSD) during the MERS-CoV outbreak. Figure 8 demonstrated a pooled prevalence of 35.97%, with a relatively moderate to high heterogeneity of I2 = 75.2% and a 95%CI ranging between 29.60-43.72.
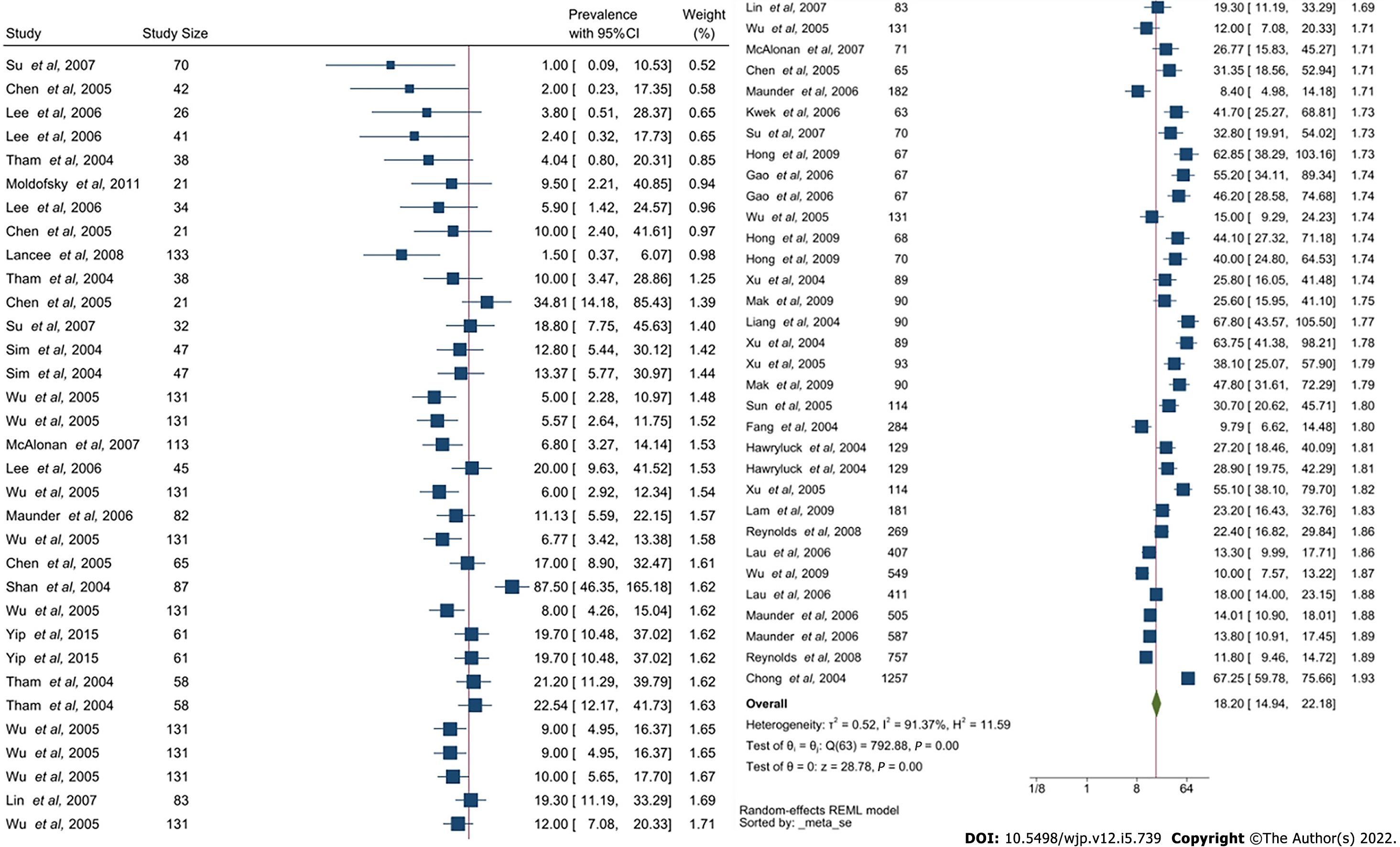
Sixty-four of the studies identified had reported on the prevalence of PTSD during SARS-CoV. Of these, 48 studies reported on the prevalence directly, whilst 17 demonstrated the mean score and the corresponding SD. Figure 9 shows the pooled prevalence of PTSD was 18.2% with a CI of 14.94-22.18 and an elevated heterogeneity of I2 = 91.37%.
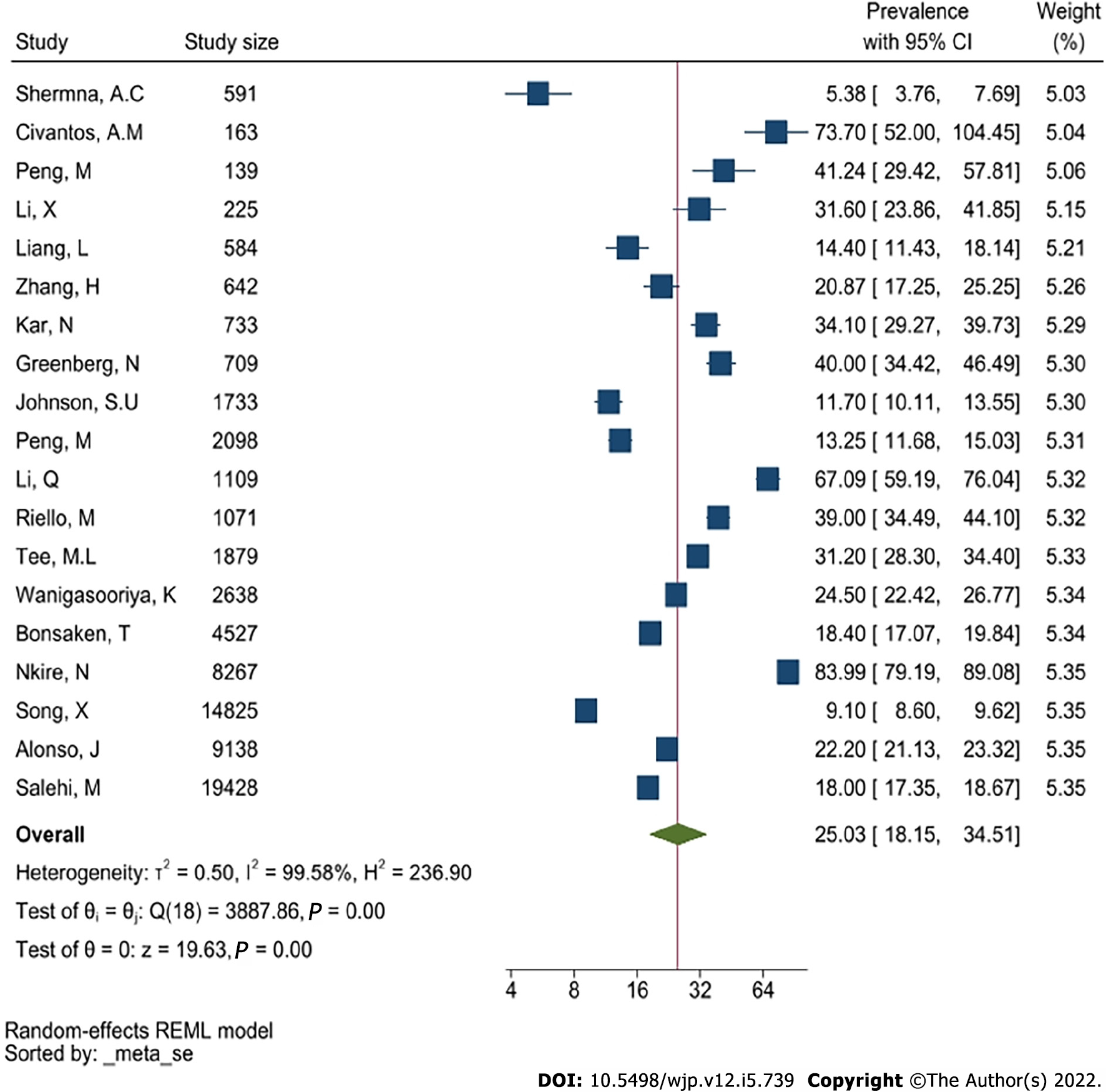
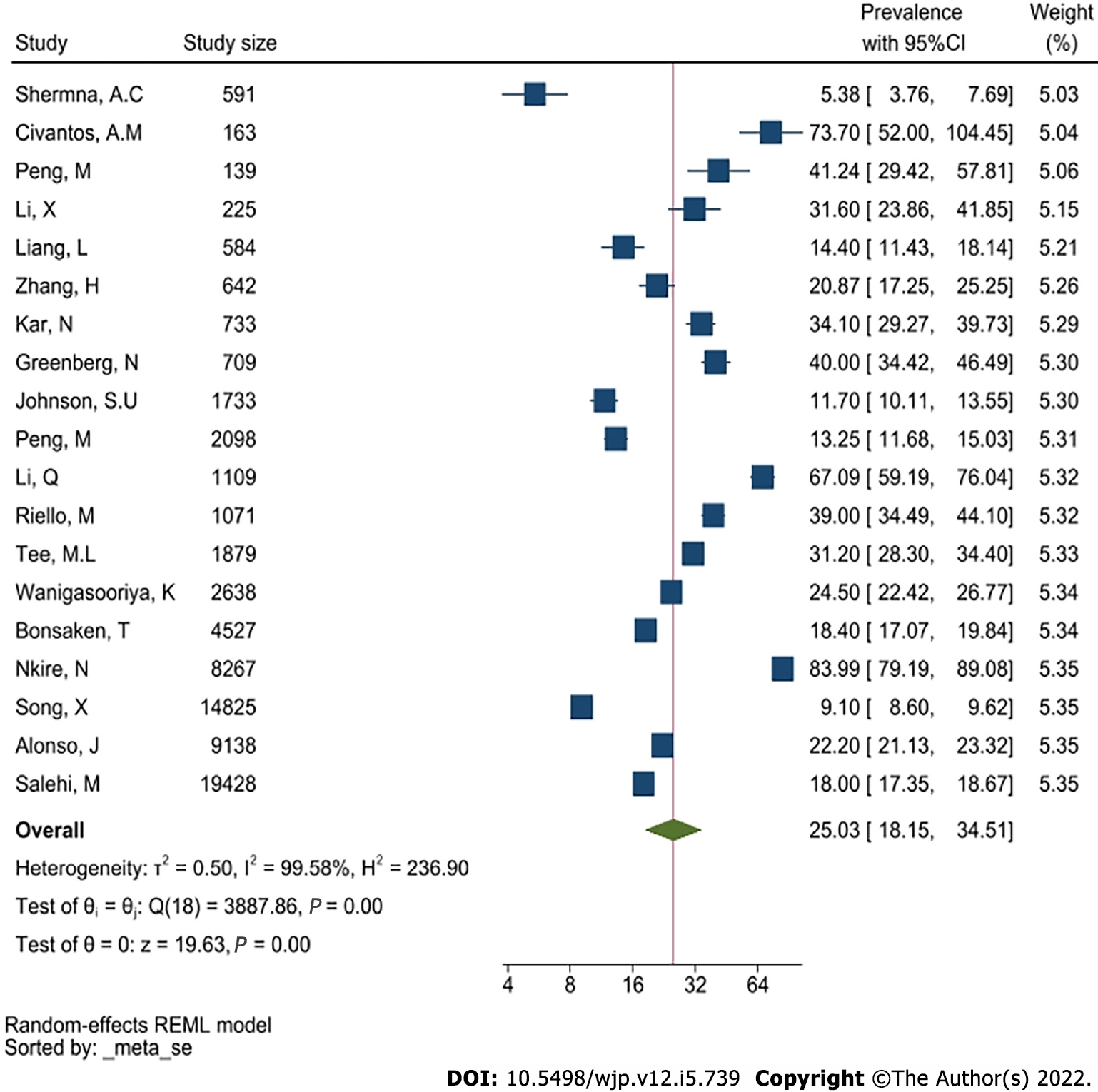
Nineteen studies reported the prevalence of PTSD during SARS-CoV-2. Figure 10 indicates a pooled prevalence of PTSD of 25.03% with a 95%CI ranging between 18.15-34.51. A high heterogeneity of I2 = 99.58% was identified.
Based on the findings, PTSD appears to have been reported for SARS-CoV-2, MERS-CoV and SARS-CoV.
A comparative analysis was completed for each MH variable identified and reported, as demonstrated within Tables 3-5.
| Anxiety | Prevalence (%) | 95%CI | Heterogeneity I2 (%) |
| MERS | 17.35 | 8.36-36.02 | 95.62 |
| SARS-CoV-2 | 21.48 | 18.68-24.71 | 99.76 |
| SARS-CoV | 25.20 | 18.41-34.5 | 93.47 |
| Depression | Prevalence (%) | 95%CI | Heterogeneity I2 (%) |
| MERS | 33.65 | 22.02-51.42 | 69.86 |
| SARS-CoV-2 | 27.64 | 24.59-31.06 | 99.69 |
| SARS-CoV | 23.10 | 18.14-29.4 | 95.03 |
| PTSD | Prevalence (%) | 95%CI | Heterogeneity I2 (%) |
| MERS | 35.97 | 29.6-43.72 | 75.2 |
| SARS-CoV-2 | 25.03 | 18.15-34.51 | 99.58 |
| SARS-CoV | 18.20 | 14.94-22.18 | 91.37 |
Multiple subgroup analyses using age group, cohort and location were conducted as an aim to identify the causation of the heterogeneity reported throughout the meta-analyses.
SARS-CoV-2: The subgroup analysis of age includes 10-19, 20-29, 30-39, 40-49, 50-59, 60-69 (Supplementary Figure 1). In particular, it can be seen from Supplementary Figure 2 that the pooled prevalence for 10–19 year-olds who are likely to have depression due to SARS-CoV-2 is 24.42%. The pooled prevalence for 60–69 years old, on the other hand, was 7.75% with a lower prevalence of depression. Therefore, the details from these analyses demonstrate the statistically reported heterogeneity could be due to the inclusion of multiple age groups.
This is further demonstrated in Supplementary Figure 3, where similar results are indicated for those reporting PTSD among young people, which appears to be higher than the older population (for instance, 32.40% for 20-29 group compared while 5.38% for 50-59 group). However, this is still reflective of a high heterogeneity which could be attributed to the differences in body mass index or race, although, to make a conclusion, further research data is required.
SARS-CoV: The subgroup analysis based on age for the SARS-CoV indicate the prevalence of mental health issues in different age groups during SARS. Supplementary Figure 4 demonstrated that people from 50 to 59 years of age appear to have a higher risk of anxiety (51.62%) in comparison to those between 30-39 (27.4%) as indicated in Supplementary Figure 5. The prevalence of PTSD (Supp
Comparison: Based on the comparison between the 3 meta-analyses, the following results associated with MH outcomes are as indicated within Tables 6-8.
| Subgroup-age | MERS | |||
| Prevalence (%) | 95%CI | Heterogeneity I2 (%) | ||
| Anxiety | 10-19 | - | - | - |
| 20-29 | - | - | - | |
| 30-39 | - | - | - | |
| 40-49 | 18.51 | 8.11-42.23 | 96.43 | |
| 50-59 | - | - | - | |
| Depression | 20-29 | - | - | - |
| 30-39 | - | - | - | |
| 40-49 | 38.45 | 25.81-57.26 | 60.55 | |
| 50-59 | - | - | - | |
| PTSD | 20-29 | 49.70 | 38.2-64.67 | 0 |
| 30-39 | 19.32 | 14.82-25.18 | 0 | |
| 40-49 | 26.69 | 13.21-53.91 | 80.63 | |
| 50-59 | - | - | - | |
| 60-69 | 17.87 | 12.4-25.74 | 0 | |
| Subgroup-age | SARS-CoV-2 | |||
| Prevalence (%) | 95%CI | Heterogeneity I2 (%) | ||
| Anxiety | 10-19 | 34.40 | 33.17-35.68 | 0 |
| 20-29 | 25.70 | 19.38-34.08 | 99.25 | |
| 30-39 | 22.86 | 17.86-29.26 | 99.64 | |
| 40-49 | 15.59 | 9.65-25.17 | 99.66 | |
| 50-59 | 20.13 | 10.43-38.84 | 99.42 | |
| 60-69 | 7.75 | 0.79-76.29 | 99.47 | |
| Depression | 10-19 | 43.91 | 42.12-45.77 | 0 |
| 20-29 | 31.03 | 24.04-40.04 | 99.12 | |
| 30-39 | 30.4 | 25.15-36.74 | 99.48 | |
| 40-49 | 20.0 | 13.26-30.18 | 99.4 | |
| 50-59 | 19.98 | 15.84-25.19 | 92.68 | |
| 60-69 | 4.93 | 3.45-7.05 | 90.00 | |
| PTSD | 20-29 | 32.40 | 6.54-160.49 | 98.29 |
| 30-39 | 21.96 | 12.77-37.78 | 99.33 | |
| 40-49 | 27.72 | 19.88-38.66 | 97.59 | |
| 50-59 | 5.38 | 3.76-7.69 | 0 | |
| 60-69 | - | - | - | |
| Subgroup-age | SARS-CoV | |||
| Prevalence (%) | 95%CI | Heterogeneity I2 (%) | ||
| Anxiety | 10-19 | - | - | - |
| 20-29 | - | - | - | |
| 30-39 | 24.60 | 13.29-45.55 | 85.81 | |
| 40-49 | 15.63 | 10.97-22.26 | 60.57 | |
| 50-59 | 51.62 | 38.53-69.16 | 0 | |
| Depression | 20-29 | - | - | - |
| 30-39 | 27.47 | 16.09-46.9 | 89.58 | |
| 40-49 | 20.30 | 13.36-30.85 | 81.57 | |
| 50-59 | 22.49 | 14.8-34.17 | 0 | |
| 60-69 | 25.85 | 17.69-37.75 | 0 | |
| PTSD | 20-29 | 24.43 | 15.53-38.44 | 72.18 |
| 30-39 | 32.13 | 23.1-44.68 | 89.33 | |
| 40-49 | 11.68 | 8.45-16.15 | 86.20 | |
| 50-59 | 67.80 | 43.57-100 | 0 | |
| 60-69 | 7.54 | 2.64-21.54 | 53.28 | |
SARS-CoV-2: Another facet of the subgroup analysis was based upon the cohorts included within this study, of HCPs, patients and the general public. The MH outcomes are demonstrated in Supplementary Figures 7-9. It is evident that healthcare workers (HCWs) have a higher prevalence of anxiety and depression compared to the general public. The exception to this appears to be the prevalence of PTSD, where the levels appear to be similar for the public and HCWs, at 24.83% and 25.16% respectively.
MERS: Supplementary Figure 10 demonstrates that the general public consists of a smaller pooled prevalence (6.04%) for the MH outcome of anxiety in comparison to patients who contracted MERS-CoV (33.95%), although some of these patients could very well be HCWs themselves. On the contrary, the pooled data for the general public and MERS-CoV survivors indicate a relatively high prevalence of depression (40.7% and 41.69%), while the HCWs appear less likely to have depression (20.52%), as indicated by Supplementary Figure 11. Mild heterogeneity was detected across these 2 groups, with I2 scores of 41.71%, I2 = 71.77%. Therefore, statistically, the data and subsequent results appear to be more conclusive and reliable. Supplementary Figure 12 indicated the prevalence of PTSD between HCWs and the general public. PTSD within the general public appears to be relatively low (19.02%) in comparison to depression. Additionally, depression amongst HCWs is more prevalent (49.87%). Moreover, the heterogeneity (I2 = 0) of this subgroup analysis is negligible, which demonstrates the data are statistically reliable and the conclusions are therefore more conclusive.
SARS-CoV: The subgroup analysis within the SARS-CoV group demonstrated a much higher prevalence of anxiety within HCWs (98.44%) in comparison to the general public (26.19%), as indicated in Supplementary Figure 12. Supplementary Figure 13 indicates that HCWs have a higher prevalence of depression (25.42%) than general public (23.31%) and SARS-CoV patients (21.96%). In contrast, the prevalence of PTSD among HCWs appear to be relatively low (16.97%) in comparison to SARS-CoV patients (19.80%) as well as the general public (18.36%), as indicated in Supplementary Figure 14. However, the heterogeneity score I2 remains high, thus there may be other potential factors that may affect the statistical findings.
Comparison: Based on the subgroup analysis above, Tables 9-11 showcase the prevalence of different MH outcomes among various cohorts. There are similarities and differences. The prevalence of anxiety within the general public during MERS (6.04%) is the lowest across the three outbreaks, while SARS-CoV demonstrates the largest prevalence of anxiety within general public (26.19%). Meanwhile, HCWs who experienced SARS-CoV were likely to have anxiety (98.44%). The prevalence of anxiety within MERS-CoV patients (33.95%) appear to be the most commonly reported MH outcome. MERS-CoV also demonstrates the highest prevalence of depression within the general public and patients, at 40.70% and 41.69% respectively. Based on the current data on SARS-CoV-2, HCWs are more likely to suffer from depression (37.97%). The highest levels of PTSD were found in HCWs during MERS-CoV and MERS-CoV patients (49.87% and 37.7%). SARS-CoV-2 appears to demonstrate that PTSD was experienced by 24.83% the general public.
| Subgroup-occupation | MERS | |||
| Prevalence (%) | 95%CI | Heterogeneity I2 (%) | ||
| Anxiety | General Public | 6.04 | 2.86-12.79 | 93.9 |
| HCW | - | - | - | |
| Patient | 33.95 | 20.65-55.82 | 68.57 | |
| Depression | General Public | 40.70 | 18.89-87.71 | 0 |
| HCW | 20.52 | 11.81-35.67 | 41.71 | |
| Patient | 41.69 | 23.73-73.22 | 71.77 | |
| PTSD | General Public | 19.02 | 14.01-25.81 | 0 |
| HCW | 49.87 | 45.09-55.16 | 0 | |
| Patient | 37.70 | 27.47-51.74 | 0 | |
| Subgroup-occupation | SARS-CoV-2 | |||
| Prevalence (%) | 95%CI | Heterogeneity I2 (%) | ||
| Anxiety | General Public | 21.18 | 17.88-25.09 | 99.82 |
| HCW | 22.35 | 17.42-28.66 | 99.36 | |
| Patient | - | - | - | |
| Depression | General Public | 27.6 | 23.36-32.24 | 99.8 |
| HCW | 27.71 | 23.22-33.08 | 98.79 | |
| Patient | - | - | - | |
| PTSD | General Public | 24.83 | 14.97-41.18 | 99.67 |
| HCW | 25.16 | 16.62-38.08 | 99.33 | |
| Patient | - | - | - | |
| Subgroup-occupation | SARS-CoV | |||
| Prevalence (%) | 95%CI | Heterogeneity I2 (%) | ||
| Anxiety | General Public | 26.19 | 11.93-57.48 | 98.22 |
| HCW | 98.44 | 22.67-427.49 | 0 | |
| Patient | 24.21 | 17.34-33.79 | 85.16 | |
| Depression | General Public | 23.31 | 14.64-37.11 | 97.97 |
| HCW | 25.42 | 13.74-47.03 | 90.29 | |
| Patient | 21.96 | 16.86-28.6 | 78.1 | |
| PTSD | General Public | 18.36 | 13.59-24.81 | 81.69 |
| HCW | 16.97 | 12.28-23.45 | 91.8 | |
| Patient | 19.80 | 14.28-27.46 | 90.44 | |
From Supplementary Figures 15-17 we can see that people who experience MERS are more likely to have depression and PTSD than those who experience SARS-CoV-2 and SARS-CoV (the area of the MERS triangles in Supplementary Figures 15 and 17 are larger than the area of the SARS-CoV-2 and SARS-CoV triangles) while people who experience SARS-CoV may have a higher possibility to have anxiety than the other two (the area of the SARS-CoV triangle in Supplementary Figure 16 is larger the area of the MERS and SARS-CoV2 triangles).
SARS-CoV-2: Another facet of the subgroup analysis was based upon the occupation of the sample and the reporting of MH outcomes as demonstrated in Supplementary Figures 7-9. It is evident that HCWs have a higher prevalence of anxiety and depression compared to the general public. The exception to this appears to be the prevalence of PTSD, where the levels appear to be similar between the public and HCWs, at 24.83% and 25.16% respectively.
MERS: A subgroup analysis based upon the categories of HCWs, patients and the general public associated with the prevalence of MH outcomes further demonstrates variability. Supple
SARS-CoV: The subgroup analysis within the SARS-CoV group demonstrated a much higher prevalence of anxiety within HCWs (98.44%) in comparison to the general public (26.19%), as indicated in Supplementary Figure 13. Supplementary Figure 14 indicates that HCWs have a higher prevalence of depression (25.42%) than the general public (21.96%) and SARS-CoV patients (23.31%). In contrast, the prevalence of PTSD among HCWs appear to be relatively low (16.97%) in comparison to SARS-CoV patients (19.80%) as well as the general public (18.36%), as indicated in Supplementary Figure 15. However, the heterogeneity score I2 remains high, thus there may be other potential factors that may affect the statistical findings.
It can be seen from Supplementary Figure 15 that it is less likely for people who experience SARS-CoV to have depression, while people who experience MERS are the most likely to suffer from depression. In particular, the general public and MERS patients have a greater risk of depression than those who experience SARS-CoV-2 and SARS-CoV. However, people in the outbreak of SARS-CoV are more likely to have anxiety than people in the outbreak of MERS and SARS-CoV-2 (Supp
SARS-CoV-2: From Supplementary Figure 18-20, we can see that people in Canada are more likely to have anxiety (80.85%) and PTSD (83.99%) when they experience SARS-CoV-2, and they also showcase a relative high possibility of having depression (57.90%), while people in Palestine suffer from the highest prevalence of depression (88.38%). On the other hand, people in the United Kingdom have the lowest prevalence of depression (1.44%) among all the countries. And people in the United States and Australia have the lowest prevalence of PTSD (5.38%) and anxiety (3.78%) respectively.
MERS: A subgroup analysis was not conducted due to the studies taking place in South Korea only.
SARS-CoV: Supplementary Figure 21-23 indicate Taipei shows the highest prevalence of depression (38.36%) and anxiety (52.91%) during SARS-CoV. Moreover, people in Kaohsiung/Southern Taiwan also suffer from the highest prevalence of PTSD (45.52%) during SARS-CoV. This indicates that people in the Taiwan area may experience a serious mental health issue due to the outbreak of SARS-CoV. On the other hand, people in Toronto, Singapore and Beijing have the lowest prevalence of PTSD (13.01%), anxiety (17.5%) and depression (21.80%) respectively.
The meta-analyses conducted indicate a high heterogeneity for depression, anxiety and PTSD. This could be due to differences in the reporting criteria and assessment tools used, geographical location and the difference in study designs, which had differing data collection time points. High heterogeneity could cause many studies to fall outside the 95%CI in the conventional funnel plot, which is based on the fixed effects model; therefore, we propose to use the funnel plot based on a random effects model. Both types of funnel plots were compared.
In the fixed effects model, the mean of the underlying model behind each study was fixed; therefore, the measure τ2 for heterogeneity was 0. Since the random effects model assumes that the mean of each study comes from a normal distribution, the DerSimonian and Laird estimates τ2 were calculated to show the heterogeneity between studies. The funnel plot based on the random effects model would include most of the studies and, therefore, make it easier to demonstrate publication bias. The pooled prevalence of the three mental health disorders and the 95%CI of the fixed (solid line) and random effects (dotted line) models were both plotted in Supplementary Figure 24 across all 3 pandemics.
When we looked at the funnel plots using the fixed effects model (solid line), most of the studies are located outside of the 95%CI. It is therefore difficult to find the sign of publication bias. They are masked by the widespread studies. By contrast, most of studies are well located within the 95%CI in the funnel plots using the random effects model (dotted line) except sub figs. Supplementary Figure 25A and B. Supplementary Figure 25C and D are typical examples. The large values of τ2, 1.1110 and 0.4574 confirm the severe heterogeneity, and the random effects model we used addresses this problem well. We can therefore focus on the problem of publication bias.
Based on the 95%CI of the random effects model (dotted line), there is little sign of publication bias in Supplementary Figure 25C-F; the P values of Egger’s test of 0.082, 0.589, 0.146 and 0.539 echo the findings (Table 7). In Supplementary Figure 25G-I, however, there is a sign of publication bias and the P values of the Egger’s test are all less than 0.05, confirming the findings (Table 11).
Even if we used the funnel plot based on the random effects model, many studies in Supplementary Figure 25A and B still fall outside the 95%CI, meaning the random effects model cannot address the problem of heterogeneity well. Further investigation is required. The sign of publication bias is not clear; the P values of Egger’s test are 0.085 and 0.000 respectively for Suppleme
To reduce the unclear impact of studies that fall outside the 95%CI of random effects model in Supplementary Figure 25A and B, further sensitivity analyses, by removing the studies external to the 95%CI range, was demonstrated in Table 12.
| Exposure | Outcome | Prevalence with 95%CI (before) | Prevalence with 95%CI (after) | P value | |
| (g) | SARS-CoV-2 | Anxiety | 21.48 (18.66-24.71) | 25.82 (23.98-27.8) | < 0.05 |
| (h) | SARS-CoV-2 | Depression | 27.64 (24.59-31.06) | 29.3 (26.98-31.81) | > 0.05 |
The prevalence of anxiety and depression under SARS-COV-2 (Supplementary Figure 25A and B) are significantly higher after removing the studies external to the 95%CI, with the result changing from 21.44% (18.69-24.61) to 25.54% (23.28-28.02) and 27.68% (24.67-31.06) to 29.7% (27.25-32.39) respectively. It means that factors associated with heterogeneity, say, the design, population and quality of those studies, may have some impact on the conclusion and a further inspection of the study quality and other factors are needed.
The prevalence of anxiety, depression and PTSD was common across HCWs, patients and the general public. It could be argued HCWs experience psychological burden more profoundly than patients and the general public given that the exposure to negative thoughts would be higher within their work environment. Patients equally could experience a high psychological burden with the exacerbation of their conditions due to a number of factors such as isolation. The general public could equally experience a decline in their mental health due to the lockdown situation in some parts of the world more extensively than others, especially with SARS-CoV-2 as a number of national level lock-downs were imposed in different countries.
The incidence of anxiety across all groups during SARS-CoV-2 (33.16%) was higher in comparison to MERS (17.35%) and SARS-CoV (25.2%). MERS and SARS-CoV-2 demonstrated higher depressive symptoms, at 33.65% and 31.35% respectively, in comparison to SARS-CoV, which reported 23.1%. PTSD was much higher during MERS (35.9%) than SARS-CoV-2 (25.03%) and SARS-CoV (18.2%).
The prevalence of PTSD among HCWs during MERS was 49.87%. The highest prevalence of anxiety for HCWs was during SARS-CoV at 98.44%. Among HCWs, the highest reported prevalence thus far during SARS-CoV-2 appear to be depression and insomnia, at 37.97% and 35.16% respectively. The identified prevalence rates could be influenced directly and indirectly by stigmatisation being an attributor. Stigmatisation within this context could include social processes to discriminate or separate the usual life changes and opportunities. This issue could present a significant barrier in managing access to equitable and quality services. Individual or social construct based beliefs and behaviours could promote social discrimination and moral discredit that may aggravate mental health implications to worsen health outcomes[27]. Interestingly, Dye and colleagues indicated HCWs were unlikely to follow social distancing protocols compared to non-HCWs. This could be associated with bullying as demonstrated by Dye et al[27] Verbal and physical violence was also associated with bullying or harassment scenarios in comparison to MERS or SARS-CoV. This could be further purported with an influx of patients and workload that exacerbates fatigue and insomnia. This finding is consistent with MERS; therefore, it likely to occur with SARS-CoV-2.
Our results indicated age appear to play a role in mental illness manifestations during SARS-CoV-2, although there was insufficient data during MERS and SARS-CoV to conduct a comparative analysis. The pooled prevalence for ages between 20-29 years appear to demonstrate PTSD at 49.7% during MERS and 32.4% in SARS-CoV-2. Other mental illnesses during SARS-CoV-2 appear to be associated with 10 to 19 years of age with a significant prevalence of anxiety of 35.84% and insomnia (23.3%). In addition, depression was reported at 40.94% within the 30-39 age group.
The indirect influence of SARS-CoV-2 is widespread, especially among young people under 40 years old. For children and teenagers, the social isolation and loneliness of being unable to meet with friends will increase the anxiety. Students worry that the epidemic would limit their future choices and future education, employment and housing. Young workers have a higher rate of unemployment because of their immature skills. During MER-CoV, suicidality was reported at 16.62% with a 95%CI of 10.73-25.75, although the age range associated was non-specific.
Studies relating to SARS-CoV and MERs-COV are limited by several aspects, including the geographical constraints and sample sizes. The majority of studies were published in languages other than English. Psychological symptomatologies associated with depression, anxiety, distress, insomnia and fatigue, as well as comorbidities such as PTSD and neuro-psychiatric syndromes such as psychosis, have been reported in patients and HCWs more during the SARS-CoV-2 pandemic[28,29] which could be due to the scope and scale of the incidence and high transmission rates. The effects of mass lock-downs, economic downturns and mass uncertainty and fear within the general population are harder to characterise and assess, but early evidence suggests that rates of mental health disorders within the population will be higher during and following the pandemic[30,31]. More significant findings of severe psychological disorders including post-traumatic stress disorder and suicidal ideation amongst health care workers have been reported at levels greater than or expected to be seen in military veterans[32] or amongst victims of natural disasters[33]. Within the three groups there is likely to be variations in the levels of mental health disorders based on age, race and socio-economic status due to differences in the risk of mortality[34,35].
Non-specific use of MH interventions to support HCPs during each of the coronavirus disease outbreaks demonstrate the lack of preparedness global healthcare systems appeared to have had. Thereby, the ongoing SARS-CoV-2 will continue to impact their MH and overall well-being due to the lack of protective factors and assessments to identify specific risk factors. The available evidence demonstrates safeguarding measures should be considered by healthcare systems to better strategize both collegial support and control steps to support all HCPs.
Several factors, including communication and country, as well as regional directives and their differences, were paramount to the inclusion and exclusion of the evidence within this study. All 3 cohorts included within this study reported their mental health impact differently. Multiple mental health assessments were used; thus, cut-off scores were used to better evaluate and inform the statistical analysis conducted. Unified approaches for the assessment of pandemic-specific or related mental health among HCPs, patients and the public should be considered in the future. This is another factor that led to the observations of high variation in outcomes and risks to medium- to long-term mental health impact.
As vaccines are rolled out globally, it is hoped that pressures on acute medical services due to the SARS-CoV-2 will slowly improve. The aim of this study is to understand and build on our knowledge of the viruses’ impact on mental health, both previously and now, so that we may better manage and prepare to deal with the hidden consequences of this and any future outbreaks. Whilst there are cultural, economic and environmental differences between the countries affected in each pandemic, drawing similarities between the lasting effects on mental health will be important in highlighting where resources and support are needed as we contemplate our recovery–physically, mentally and socially–from this pandemic. The mortality impact of seasonal influenza and a pandemic on the mental health of the general public, patients and HCPs vary.
This study analysed the prevalence of mental health outcomes during the MERS, SARS-CoV and SARS-CoV-2 across multiple cohorts. In terms of mental illness like anxiety, depression and PTSD, the prevalence of depression (33.65% with 95%CI: 22.02-51.42) and PTSD (35.97% with 95%CI: 29.6-43.72) is higher during MERS, while the prevalence of anxiety (33.16% with 95%CI: 25.99-34.5) is higher during SARS-CoV-2. Patients and HCWs are the first and second most likely groups to suffer from mental health problems. Young people are more likely to be caught up in depressive and anxiety emotions than older people.
Developing evidence-based and cohort-specific MH interventions could be a useful way to optimise MH support. HCPs in particular may benefit from this as it could promote better well-being for staff, increasing the efficiency within the work environment.
The severe acute respiratory syndrome (SARS) virus has been present for centuries in different forms. Whilst civilisation has evolved, so has the virus, including its' ability to transmit. Thus, the comparison of the three most recent severe acute respiratory syndrome coronavirus (SARS-CoV) viruses in terms of the mental health implications infused to patients, healthcare professionals (HCPs) and patients is an important facet both clinically and scientifically. As a result, our study explores an important component that hasn't been addressed from a potential disease sequalae perspective.
Our motivation was to demonstrate the trends associated with the mental health prevalence in terms of specific conditions due to the last three virulent strands of SARS-CoV across patient, HCPs and the general public. The specified cohorts have specific behavioural patterns and differing levels of exposure to the virus, thus the risk of infection varies that influences the mental health impact. This would aid in assessing the true mental health impact that health care systems require to support those needing mental health support. The comparison also allows us to predict the trends in mental health impact due to infectious transmissions which ultimately should be addressed as a public health hazard, globally.
The study has three primary aims of identifying and reporting: (1) Mental health conditions commonly observed across all three pandemics; (2) Impact of mental health outcomes across patients, the general public and HCPs associated with all 3 pandemics; and (3) The prevalence of the mental health impact and clinical epidemiological significance.
A systematic methodology was developed and published on PROSPERO (CRD42021228697). The databases PubMed, EMBASE, ScienceDirect and the Cochrane Central Register of Controlled Trials were used as part of the data extraction process, and publications from January 1, 1990 to August 1, 2021 were searched. MeSH terms and keywords used included Mood disorders, PTSD, Anxiety, Depression, Psychological stress, Psychosis, Bipolar, Mental Health, Unipolar, Self-harm, BAME, Psychiatry disorders and Psychological distress. The terms were expanded with a ‘snowballing’ method. Cox-regression and the Monte-Carlo simulation method was used in addition to I2 and Egger’s tests to determine heterogeneity and publication bias.
The results indicated that there is a mental health impact observed among patients, HCPs and the general public at varying levels. This study analysed the prevalence of some mental health outcomes to the outbreaks of Middle East respiratory syndrome (MERS), SARS-CoV and SARS-CoV-2 and compared the prevalence of the participants and the prevalence of different occupational groups and age groups. In terms of mental illness like anxiety, depression and post-traumatic stress disorder (PTSD), the prevalence of depression [33.65% with 95% confidence interval (CI): 22.02-51.42] and PTSD (35.97% with 95%CI: 29.6-43.72) is higher during MERS, while the prevalence of anxiety (33.16% with 95%CI: 25.99-34.5) is higher during SARS-CoV-2. Patients and healthcare workers are the first and second most likely groups to suffer from mental health problems. Young people are more likely to be caught up in depressive and anxiety emotions than older people.
Developing evidence-based and cohort-specific mental health (MH) interventions could be a useful way to optimise MH support. HCPs in particular may benefit from this as it could promote better well-being for staff, increasing the efficiency within the work environment. As vaccines are rolled out globally, it is hoped that pressures on acute medical services due to the SARS-CoV-2 will slowly improve. The aim of this study is to understand and build on our knowledge of the viruses’ impact on mental health, both previously and now, so that we may better manage and prepare to deal with the hidden consequences of this and any future outbreaks. Whilst there are cultural, economic and environmental differences between the countries affected in each pandemic, drawing similarities between the lasting effects on mental health will be important in highlighting where resources and support are needed as we contemplate our recovery–physically, mentally and socially–from this pandemic. The mortality impact of seasonal influenza and a pandemic on the mental health of the general public, patients and HCPs vary.
Studies relating to SARS-CoV and MERS-CoV are limited by several aspects, including the geographical constraints and sample sizes. The majority of studies were published in languages other than English. Psychological symptomatologies associated with depression, anxiety, distress, insomnia and fatigue, as well as comorbidities such as PTSD and neuro-psychiatric syndromes such as psychosis, have been reported in patients and HCWs more during the SARS-CoV-2 pandemic which could be due to the scope and scale of the incidence and high transmission rates. The effects of mass lock-downs, economic downturns and mass uncertainty and fear within the general population are harder to characterise and assess, but early evidence suggests that rates of mental health disorders within the population will be higher during and following the pandemic. We need more comprehensive and longitudinal studies to be conducted to determine the mental health impact in multiple populations globally. This would also aid us to develop better pandemic preparedness frameworks and policies within healthcare systems.
The authors acknowledge the following: Mr Tony Thayanandan, Associate Prof Steven Wai Ho Chau, Dr Sandra Chan, Dr Sheena Au-Yeung, Prof David Kingdon, Miss Natasha Sandle, Associate Prof Oscar Wong, Dr Evelyn Wong and Dr Li Yee Ting for contributions to the SARS-CoV and SARS-CoV-2 datasets that have been peer reviewed and published already. This paper is part of the multifaceted EPIC project that is sponsored by Southern Health NHS Foundation Trust and a collaboration between the University of Oxford, The Alan Turing Institute, Southern University of Science and Technology, China, University College London and University College London Hospitals NHS Foundation Trust.
Provenance and peer review: Invited article; Externally peer reviewed.
Peer-review model: Single blind
Corresponding Author's Membership in Professional Societies: Nursing and Midwifery Council (NMC), No. 98I1393.
Specialty type: Psychiatry
Country/Territory of origin: United Kingdom
Peer-review report’s scientific quality classification
Grade A (Excellent): A, A, A
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Lu C, China; Sageena G, India; Wang MZ, China; Yu L, Singapore S-Editor: Fan JR L-Editor: A P-Editor: Yu HG
| 1. | National Institute of Allergy and Infectious Diseases (NIAID). Coronaviruses [Internet]. [cited 23 December 2021]. Available from: https://www.niaid.nih.gov/diseases-conditions/coronaviruses. |
| 2. | Kahn JS, McIntosh K. History and recent advances in coronavirus discovery. Pediatr Infect Dis J. 2005;24:S223-S227, discussion S226. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 370] [Cited by in RCA: 323] [Article Influence: 16.2] [Reference Citation Analysis (0)] |
| 3. | Bell DM; World Health Organization Working Group on International and Community Transmission of SARS. Public health interventions and SARS spread, 2003. Emerg Infect Dis. 2004;10:1900-1906. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 181] [Cited by in RCA: 177] [Article Influence: 8.9] [Reference Citation Analysis (0)] |
| 4. | World Health Organization (WHO). Summary of probable SARS cases with onset of illness from 1 November 2002 to 31 July 2003. 24 July 2015. [cited 17 January 2021]. Available from: https://www.who.int/publications/m/item/summary-of-probable-sars-cases-with-onset-of-illness-from-1-november-2002-to-31-july-2003. |
| 5. | World Health Organization (WHO). MERS situation update | October 2021. October 2021. [cited 17 December 2021]. Available from: https://applications.emro.who.int/docs/WHOEMCSR471E-eng.pdf?ua=1. |
| 6. | Baharoon S, Memish ZA. MERS-CoV as an emerging respiratory illness: A review of prevention methods. Travel Med Infect Dis. 2019;101520. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 48] [Cited by in RCA: 58] [Article Influence: 9.7] [Reference Citation Analysis (0)] |
| 7. | Memish ZA, Perlman S, Van Kerkhove MD, Zumla A. Middle East respiratory syndrome. Lancet. 2020;395:1063-1077. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 282] [Cited by in RCA: 305] [Article Influence: 61.0] [Reference Citation Analysis (0)] |
| 8. | OECD/KDI. Understanding the Drivers of Trust in Government Institutions in Korea, OECD Publishing, Paris, 2018. |
| 9. | Wu Z, McGoogan JM. Characteristics of and Important Lessons From the Coronavirus Disease 2019 (COVID-19) Outbreak in China: Summary of a Report of 72 314 Cases From the Chinese Center for Disease Control and Prevention. JAMA. 2020;323:1239-1242. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11409] [Cited by in RCA: 11505] [Article Influence: 2301.0] [Reference Citation Analysis (0)] |
| 10. | WHO Rapid Evidence Appraisal for COVID-19 Therapies (REACT) Working Group; Sterne JAC, Murthy S, Diaz JV, Slutsky AS, Villar J, Angus DC, Annane D, Azevedo LCP, Berwanger O, Cavalcanti AB, Dequin PF, Du B, Emberson J, Fisher D, Giraudeau B, Gordon AC, Granholm A, Green C, Haynes R, Heming N, Higgins JPT, Horby P, Jüni P, Landray MJ, Le Gouge A, Leclerc M, Lim WS, Machado FR, McArthur C, Meziani F, Møller MH, Perner A, Petersen MW, Savovic J, Tomazini B, Veiga VC, Webb S, Marshall JC. Association Between Administration of Systemic Corticosteroids and Mortality Among Critically Ill Patients With COVID-19: A Meta-analysis. JAMA. 2020;324:1330-1341. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1683] [Cited by in RCA: 1679] [Article Influence: 335.8] [Reference Citation Analysis (0)] |
| 11. | Beigel JH, Tomashek KM, Dodd LE, Mehta AK, Zingman BS, Kalil AC, Hohmann E, Chu HY, Luetkemeyer A, Kline S, Lopez de Castilla D, Finberg RW, Dierberg K, Tapson V, Hsieh L, Patterson TF, Paredes R, Sweeney DA, Short WR, Touloumi G, Lye DC, Ohmagari N, Oh MD, Ruiz-Palacios GM, Benfield T, Fätkenheuer G, Kortepeter MG, Atmar RL, Creech CB, Lundgren J, Babiker AG, Pett S, Neaton JD, Burgess TH, Bonnett T, Green M, Makowski M, Osinusi A, Nayak S, Lane HC; ACTT-1 Study Group Members. Remdesivir for the Treatment of Covid-19 - Final Report. N Engl J Med. 2020;383:1813-1826. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5711] [Cited by in RCA: 5117] [Article Influence: 1023.4] [Reference Citation Analysis (0)] |
| 12. | Alhazzani W, Møller MH, Arabi YM, Loeb M, Gong MN, Fan E, Oczkowski S, Levy MM, Derde L, Dzierba A, Du B, Aboodi M, Wunsch H, Cecconi M, Koh Y, Chertow DS, Maitland K, Alshamsi F, Belley-Cote E, Greco M, Laundy M, Morgan JS, Kesecioglu J, McGeer A, Mermel L, Mammen MJ, Alexander PE, Arrington A, Centofanti JE, Citerio G, Baw B, Memish ZA, Hammond N, Hayden FG, Evans L, Rhodes A. Surviving Sepsis Campaign: guidelines on the management of critically ill adults with Coronavirus Disease 2019 (COVID-19). Intensive Care Med. 2020;46:854-887. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1239] [Cited by in RCA: 1360] [Article Influence: 272.0] [Reference Citation Analysis (0)] |
| 13. | Lipsitch M, Cohen T, Cooper B, Robins JM, Ma S, James L, Gopalakrishna G, Chew SK, Tan CC, Samore MH, Fisman D, Murray M. Transmission dynamics and control of severe acute respiratory syndrome. Science. 2003;300:1966-1970. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1108] [Cited by in RCA: 886] [Article Influence: 40.3] [Reference Citation Analysis (0)] |
| 14. | Wilder-Smith A, Chiew CJ, Lee VJ. Can we contain the COVID-19 outbreak with the same measures as for SARS? Lancet Infect Dis. 2020;20:e102-e107. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 585] [Cited by in RCA: 538] [Article Influence: 107.6] [Reference Citation Analysis (0)] |
| 15. | World Health Organization (WHO). Consensus document on the epidemiology of severe acute respiratory syndrome (SARS). 2003. [cited 14 May 2020]. Available from: https://www.who.int/csr/sars/WHOconsensus.pdf?ua=1. |
| 16. | Chen J, Lu H, Melino G, Boccia S, Piacentini M, Ricciardi W, Wang Y, Shi Y, Zhu T. COVID-19 infection: the China and Italy perspectives. Cell Death Dis. 2020;11:438. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 67] [Cited by in RCA: 60] [Article Influence: 12.0] [Reference Citation Analysis (0)] |
| 17. | Hung LS. The SARS epidemic in Hong Kong: what lessons have we learned? J R Soc Med. 2003;96:374-378. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 60] [Cited by in RCA: 122] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 18. | Chan SM, Chiu FK, Lam CW, Leung PY, Conwell Y. Elderly suicide and the 2003 SARS epidemic in Hong Kong. Int J Geriatr Psychiatry. 2006;21:113-118. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 167] [Cited by in RCA: 161] [Article Influence: 8.5] [Reference Citation Analysis (0)] |
| 19. | Wu P, Fang Y, Guan Z, Fan B, Kong J, Yao Z, Liu X, Fuller CJ, Susser E, Lu J, Hoven CW. The psychological impact of the SARS epidemic on hospital employees in China: exposure, risk perception, and altruistic acceptance of risk. Can J Psychiatry. 2009;54:302-311. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1086] [Cited by in RCA: 1003] [Article Influence: 62.7] [Reference Citation Analysis (0)] |
| 20. | Kwek SK, Chew WM, Ong KC, Ng AW, Lee LS, Kaw G, Leow MK. Quality of life and psychological status in survivors of severe acute respiratory syndrome at 3 mo postdischarge. J Psychosom Res. 2006;60:513-519. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 90] [Cited by in RCA: 80] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 21. | Lee TM, Chi I, Chung LW, Chou KL. Ageing and psychological response during the post-SARS period. Aging Ment Health. 2006;10:303-311. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 62] [Cited by in RCA: 55] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 22. | Gardner PJ, Moallef P. Psychological impact on SARS survivors: Critical review of the English language literature. Can Psychol. 2015;56:123. [RCA] [DOI] [Full Text] [Cited by in Crossref: 108] [Cited by in RCA: 105] [Article Influence: 10.5] [Reference Citation Analysis (0)] |
| 23. | Jeong H, Yim HW, Song YJ, Ki M, Min JA, Cho J, Chae JH. Mental health status of people isolated due to Middle East Respiratory Syndrome. Epidemiol Health. 2016;38:e2016048. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 623] [Cited by in RCA: 633] [Article Influence: 70.3] [Reference Citation Analysis (0)] |
| 24. | Wan X, Wang W, Liu J, Tong T. Estimating the sample mean and standard deviation from the sample size, median, range and/or interquartile range. BMC Med Res Methodol. 2014;14:135. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3433] [Cited by in RCA: 7017] [Article Influence: 637.9] [Reference Citation Analysis (0)] |
| 25. | Chau SWH, Wong OWH, Ramakrishnan R, Chan SSM, Wong EKY, Li PYT, Raymont V, Elliot K, Rathod S, Delanerolle G, Phiri P. History for some or lesson for all? BMC Public Health. 2021;21:670. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 54] [Cited by in RCA: 44] [Article Influence: 11.0] [Reference Citation Analysis (0)] |
| 26. | Phiri P, Ramakrishnan R, Rathod S, Elliot K, Thayanandan T, Sandle N, Haque N, Chau SW, Wong OW, Chan SS, Wong EK, Raymont V, Au-Yeung SK, Kingdon D, Delanerolle G. An evaluation of the mental health impact of SARS-CoV-2 on patients, general public and healthcare professionals: A systematic review and meta-analysis. EClinicalMedicine. 2021;34:100806. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 96] [Cited by in RCA: 71] [Article Influence: 17.8] [Reference Citation Analysis (0)] |
| 27. | Dye TD, Alcantara L, Siddiqi S, Barbosu M, Sharma S, Panko T, Pressman E. Risk of COVID-19-related bullying, harassment and stigma among healthcare workers: an analytical cross-sectional global study. BMJ Open. 2020;10:e046620. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 138] [Cited by in RCA: 117] [Article Influence: 23.4] [Reference Citation Analysis (0)] |
| 28. | Rogers JP, Chesney E, Oliver D, Pollak TA, McGuire P, Fusar-Poli P, Zandi MS, Lewis G, David AS. Psychiatric and neuropsychiatric presentations associated with severe coronavirus infections: a systematic review and meta-analysis with comparison to the COVID-19 pandemic. Lancet Psychiatry. 2020;7:611-627. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1673] [Cited by in RCA: 1522] [Article Influence: 304.4] [Reference Citation Analysis (0)] |
| 29. | Khan KS, Mamun MA, Griffiths MD, Ullah I. The Mental Health Impact of the COVID-19 Pandemic Across Different Cohorts. Int J Ment Health Addict. 2020;1-7. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 164] [Cited by in RCA: 133] [Article Influence: 26.6] [Reference Citation Analysis (0)] |
| 30. | McIntyre RS, Lee Y. Projected increases in suicide in Canada as a consequence of COVID-19. Psychiatry Res. 2020;290:113104. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 118] [Cited by in RCA: 120] [Article Influence: 24.0] [Reference Citation Analysis (0)] |
| 31. | Huang Y, Zhao N. Generalized anxiety disorder, depressive symptoms and sleep quality during COVID-19 outbreak in China: a web-based cross-sectional survey. Psychiatry Res. 2020;288:112954. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1897] [Cited by in RCA: 2046] [Article Influence: 409.2] [Reference Citation Analysis (0)] |
| 32. | Greenberg N, Weston D, Hall C, Caulfield T, Williamson V, Fong K. Mental health of staff working in intensive care during Covid-19. Occup Med (Lond). 2021;71:62-67. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 223] [Cited by in RCA: 209] [Article Influence: 52.3] [Reference Citation Analysis (0)] |
| 33. | Maunder RG. Was SARS a mental health catastrophe? Gen Hosp Psychiatry. 2009;31:316-317. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 99] [Cited by in RCA: 101] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 34. | Aldridge RW, Lewer D, Katikireddi SV, Mathur R, Pathak N, Burns R, Fragaszy EB, Johnson AM, Devakumar D, Abubakar I, Hayward A. Black, Asian and Minority Ethnic groups in England are at increased risk of death from COVID-19: indirect standardisation of NHS mortality data. Wellcome Open Res. 2020;5:88. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 231] [Cited by in RCA: 212] [Article Influence: 42.4] [Reference Citation Analysis (0)] |
| 35. | Clouston SAP, Natale G, Link BG. Socioeconomic inequalities in the spread of coronavirus-19 in the United States: A examination of the emergence of social inequalities. Soc Sci Med. 2021;268:113554. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 92] [Cited by in RCA: 138] [Article Influence: 27.6] [Reference Citation Analysis (0)] |
| 36. | Shin J, Park HY, Kim JL, Lee JJ, Lee H, Lee SH, Shin HS. Psychiatric morbidity of survivors one year after the outbreak of Middle East respiratory syndrome in Korea, 2015. J Korean Neuropsy Assoc. 2019;58:245-251. |
| 37. | Um DH, Kim JS, Lee HW, Lee SH. Psychological effects on medical doctors from the Middle East Respiratory Syndrome (MERS) outbreak: A comparison of whether they worked at the MERS occurred hospital or not, and whether they participated in MERS diagnosis and treatment. J Korean Neuropsy Assoc. 2017;56:28-34. |
| 38. | Abolfotouh MA, AlQarni AA, Al-Ghamdi SM, Salam M, Al-Assiri MH, Balkhy HH. An assessment of the level of concern among hospital-based health-care workers regarding MERS outbreaks in Saudi Arabia. BMC Infect Dis. 2017;17:4. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 59] [Cited by in RCA: 67] [Article Influence: 8.4] [Reference Citation Analysis (0)] |
| 39. | Jung H, Jung SY, Lee MH, Kim MS. Assessing the Presence of Post-Traumatic Stress and Turnover Intention Among Nurses Post-Middle East Respiratory Syndrome Outbreak: The Importance of Supervisor Support. Workplace Health Saf. 2020;68:337-345. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 68] [Cited by in RCA: 89] [Article Influence: 17.8] [Reference Citation Analysis (0)] |
| 40. | Ahn SH, Kim JL, Kim JR, Lee SH, Yim HW, Jeong H, Chae JH, Park HY, Lee JJ, Lee H. Association between chronic fatigue syndrome and suicidality among survivors of Middle East respiratory syndrome over a 2-year follow-up period. J Psychiatr Res. 2021;137:1-6. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 10] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 41. | Lee SH, Shin HS, Park HY, Kim JL, Lee JJ, Lee H, Won SD, Han W. Depression as a Mediator of Chronic Fatigue and Post-Traumatic Stress Symptoms in Middle East Respiratory Syndrome Survivors. Psychiatry Investig. 2019;16:59-64. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 130] [Cited by in RCA: 143] [Article Influence: 23.8] [Reference Citation Analysis (0)] |
| 42. | Kim Y, Seo E, Seo Y, Dee V, Hong E. Effects of Middle East Respiratory Syndrome Coronavirus on post-traumatic stress disorder and burnout among registered nurses in South Korea. Int J Healthc. 2018;4:27-33. |
| 43. | Oh N, Hong N, Ryu DH, Bae SG, Kam S, Kim KY. Exploring Nursing Intention, Stress, and Professionalism in Response to Infectious Disease Emergencies: The Experience of Local Public Hospital Nurses During the 2015 MERS Outbreak in South Korea. Asian Nurs Res (Korean Soc Nurs Sci). 2017;11:230-236. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 73] [Cited by in RCA: 78] [Article Influence: 9.8] [Reference Citation Analysis (0)] |
| 44. | Seo YE, Kim HC, Yoo SY, Lee KU, Lee HW, Lee SH. Factors Associated with Burnout among Healthcare Workers during an Outbreak of MERS. Psychiatry Investig. 2020;17:674-680. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 16] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 45. | Son H, Lee WJ, Kim HS, Lee KS, You M. Hospital workers’ psychological resilience after the 2015 Middle East respiratory syndrome outbreak. Soc Behav Per Int J. 2019;47:1-3. |
| 46. | Park JS, Lee EH, Park NR, Choi YH. Mental Health of Nurses Working at a Government-designated Hospital During a MERS-CoV Outbreak: A Cross-sectional Study. Arch Psychiatr Nurs. 2018;32:2-6. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 230] [Cited by in RCA: 187] [Article Influence: 26.7] [Reference Citation Analysis (0)] |
| 47. | Al-Rabiaah A, Temsah MH, Al-Eyadhy AA, Hasan GM, Al-Zamil F, Al-Subaie S, Alsohime F, Jamal A, Alhaboob A, Al-Saadi B, Somily AM. Middle East Respiratory Syndrome-Corona Virus (MERS-CoV) associated stress among medical students at a university teaching hospital in Saudi Arabia. J Infect Public Health. 2020;13:687-691. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 213] [Cited by in RCA: 229] [Article Influence: 45.8] [Reference Citation Analysis (0)] |
| 48. | Park HY, Park WB, Lee SH, Kim JL, Lee JJ, Lee H, Shin HS. Posttraumatic stress disorder and depression of survivors 12 mo after the outbreak of Middle East respiratory syndrome in South Korea. BMC Public Health. 2020;20:605. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 66] [Cited by in RCA: 92] [Article Influence: 18.4] [Reference Citation Analysis (0)] |
| 49. | Cho AJ, Lee HS, Lee YK, Jeon HJ, Park HC, Jeong DW, Kim YG, Lee SH, Lee CH, Yoo KD, Wong AK. Post-traumatic stress symptoms in hemodialysis patients with MERS-CoV exposure. Biopsychosoc Med. 2020;14:9. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 9] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 50. | Kim HC, Yoo SY, Lee BH, Lee SH, Shin HS. Psychiatric Findings in Suspected and Confirmed Middle East Respiratory Syndrome Patients Quarantined in Hospital: A Retrospective Chart Analysis. Psychiatry Investig. 2018;15:355-360. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 103] [Cited by in RCA: 88] [Article Influence: 12.6] [Reference Citation Analysis (0)] |
| 51. | Lee SM, Kang WS, Cho AR, Kim T, Park JK. Psychological impact of the 2015 MERS outbreak on hospital workers and quarantined hemodialysis patients. Compr Psychiatry. 2018;87:123-127. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 646] [Cited by in RCA: 638] [Article Influence: 91.1] [Reference Citation Analysis (0)] |
| 52. | Kim JS, Choi JS. Factors Influencing Emergency Nurses' Burnout During an Outbreak of Middle East Respiratory Syndrome Coronavirus in Korea. Asian Nurs Res (Korean Soc Nurs Sci). 2016;10:295-299. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 115] [Cited by in RCA: 135] [Article Influence: 15.0] [Reference Citation Analysis (0)] |
| 53. | Bukhari EE, Temsah MH, Aleyadhy AA, Alrabiaa AA, Alhboob AA, Jamal AA, Binsaeed AA. Middle East respiratory syndrome coronavirus (MERS-CoV) outbreak perceptions of risk and stress evaluation in nurses. J Infect Dev Ctries. 2016;10:845-850. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 79] [Cited by in RCA: 79] [Article Influence: 8.8] [Reference Citation Analysis (0)] |
| 54. | Mollers M, Jonges M, Pas SD, van der Eijk AA, Dirksen K, Jansen C, Gelinck LB, Leyten EM, Thurkow I, Groeneveld PH, van Gageldonk-Lafeber AB, Koopmans MP, Timen A; MERS-CoV Outbreak Investigation Team of the Netherlands. Follow-up of Contacts of Middle East Respiratory Syndrome Coronavirus-Infected Returning Travelers, the Netherlands, 2014. Emerg Infect Dis. 2015;21:1667-1669. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 12] [Cited by in RCA: 11] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 55. | Fang Y, Zhe D, Shuran LI. Survey on mental status of subjects recovered from SARS. Zhongguo Xinli Jiankang Zazhi. 2004;. |
| 56. | Liang CC. Stress reaction, emotional effects and posttraumatic stress disorder in severe acute respiratory syndrome patients: a follow-up study. Unpublished Thesis. National Taipei University of Nursing and Health Sciences, Taiwan, 2004. |
| 57. | Dang WM, Huang YQ, Liu ZR, Li S. Analysis of anxiety and depression symptoms and related factors in three universities during SARS epidemic in Beijing. Zhongguo Xingwei Yixue Zazhi. 2004;13:437-439. |
| 58. | Yip KW. Ten-year Follow-up Study on Psychiatric Morbidity in Survivors of Severe Acute Respiratory Syndrome. Unpublished Thesis. United Chrisian Hospital, Hong Kong 2015. |
| 59. | Cheng SK, Wong CW, Tsang J, Wong KC. Psychological distress and negative appraisals in survivors of severe acute respiratory syndrome (SARS). Psychol Med. 2004;34:1187-1195. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 229] [Cited by in RCA: 207] [Article Influence: 9.9] [Reference Citation Analysis (0)] |
| 60. | Wu KK, Chan SK, Ma TM. Posttraumatic stress after SARS. Emerg Infect Dis. 2005;11:1297-1300. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 134] [Cited by in RCA: 139] [Article Influence: 7.0] [Reference Citation Analysis (0)] |
| 61. | Mak IW, Chu CM, Pan PC, Yiu MG, Chan VL. Long-term psychiatric morbidities among SARS survivors. Gen Hosp Psychiatry. 2009;31:318-326. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 649] [Cited by in RCA: 617] [Article Influence: 38.6] [Reference Citation Analysis (0)] |
| 62. | Lee AM, Wong JG, McAlonan GM, Cheung V, Cheung C, Sham PC, Chu CM, Wong PC, Tsang KW, Chua SE. Stress and psychological distress among SARS survivors 1 year after the outbreak. Can J Psychiatry. 2007;52:233-240. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 695] [Cited by in RCA: 688] [Article Influence: 38.2] [Reference Citation Analysis (0)] |
| 63. | Hong X, Currier GW, Zhao X, Jiang Y, Zhou W, Wei J. Posttraumatic stress disorder in convalescent severe acute respiratory syndrome patients: a 4-year follow-up study. Gen Hosp Psychiatry. 2009;31:546-554. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 124] [Cited by in RCA: 124] [Article Influence: 7.8] [Reference Citation Analysis (0)] |
| 64. | Wang J. Psychological conditions of patients with fever during the epidemic of infectious atypical pneumonia. Chin J Clin Rehabil. 2003;7:4162. |
| 65. | Hu HY, Li M, Zhou L, Zhang H, Wang T. Effect of coping style and social support on the psychologic status in patients with severe acute respiratory syndrome. Chin J Clin Rehabil. 2004;8:1022-1023. |
| 66. | Chen R, Chou KR, Huang YJ, Wang TS, Liu SY, Ho LY. Effects of a SARS prevention programme in Taiwan on nursing staff's anxiety, depression and sleep quality: a longitudinal survey. Int J Nurs Stud. 2006;43:215-225. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 116] [Cited by in RCA: 131] [Article Influence: 6.6] [Reference Citation Analysis (0)] |
| 67. | Ko CH, Yen CF, Yen JY, Yang MJ. Psychosocial impact among the public of the severe acute respiratory syndrome epidemic in Taiwan. Psychiatry Clin Neurosci. 2006;60:397-403. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 163] [Cited by in RCA: 146] [Article Influence: 7.7] [Reference Citation Analysis (0)] |
| 68. | Hawryluck L, Gold WL, Robinson S, Pogorski S, Galea S, Styra R. SARS control and psychological effects of quarantine, Toronto, Canada. Emerg Infect Dis. 2004;10:1206-1212. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1212] [Cited by in RCA: 1233] [Article Influence: 58.7] [Reference Citation Analysis (0)] |
| 69. | Liu X, Kakade M, Fuller CJ, Fan B, Fang Y, Kong J, Guan Z, Wu P. Depression after exposure to stressful events: lessons learned from the severe acute respiratory syndrome epidemic. Compr Psychiatry. 2012;53:15-23. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 630] [Cited by in RCA: 511] [Article Influence: 39.3] [Reference Citation Analysis (0)] |
| 70. | Su TP, Lien TC, Yang CY, Su YL, Wang JH, Tsai SL, Yin JC. Prevalence of psychiatric morbidity and psychological adaptation of the nurses in a structured SARS caring unit during outbreak: a prospective and periodic assessment study in Taiwan. J Psychiatr Res. 2007;41:119-130. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 348] [Cited by in RCA: 322] [Article Influence: 17.9] [Reference Citation Analysis (0)] |
| 71. | Lam MH, Wing YK, Yu MW, Leung CM, Ma RC, Kong AP, So WY, Fong SY, Lam SP. Mental morbidities and chronic fatigue in severe acute respiratory syndrome survivors: long-term follow-up. Arch Intern Med. 2009;169:2142-2147. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 399] [Cited by in RCA: 493] [Article Influence: 32.9] [Reference Citation Analysis (0)] |
| 72. | Shi C, Yu X, Hong N, Chan RC, Chen Y, He Y. Emotional, memory and daily function among health care worker survivors with SARS. Chin Ment Health J. 2011;25:660-665. |
| 73. | Huang W, Hua Q, Wu H, Xu WY, Tian JH, Chen H, Yang FC, Yang S, Liu CH, Li XW, Ji XM, Zhang J. [A study on the differences of emotion and depression between patients as doctor/nurse and others occupation with severe acute respiratory syndrome]. Zhonghua Liu Xing Bing Xue Za Zhi. 2004;25:23-26. [PubMed] |
| 74. | Yu HY, Ho SC, So KF, Lo YL. The psychological burden experienced by Hong Kong midlife women during the SARS epidemic. Stress Health. 2005;21:177-184. |
| 75. | Chang WC, Sivam RW. Constant vigilance: Heritage values and defensive pessimism in coping with severe acute respiratory syndrome in Singapore. Asian J Soc Psychol. 2004;7:35-53. |
| 76. | Moldofsky H, Patcai J. Chronic widespread musculoskeletal pain, fatigue, depression and disordered sleep in chronic post-SARS syndrome; a case-controlled study. BMC Neurol. 2011;11:37. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 433] [Cited by in RCA: 402] [Article Influence: 28.7] [Reference Citation Analysis (0)] |
| 77. | Sun Y, Xu Y, Zhang Kr YH. Follow-up study on PTSD of SARS patients. Chin J Health Educ. 2005;8:572-575. |
| 78. | Lau JT, Yang X, Tsui HY, Pang E, Wing YK. Positive mental health-related impacts of the SARS epidemic on the general public in Hong Kong and their associations with other negative impacts. J Infect. 2006;53:114-124. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 161] [Cited by in RCA: 168] [Article Influence: 8.4] [Reference Citation Analysis (0)] |
| 79. | Reynolds DL, Garay JR, Deamond SL, Moran MK, Gold W, Styra R. Understanding, compliance and psychological impact of the SARS quarantine experience. Epidemiol Infect. 2008;136:997-1007. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 531] [Cited by in RCA: 514] [Article Influence: 28.6] [Reference Citation Analysis (0)] |
| 80. | Lancee WJ, Maunder RG, Goldbloom DS; Coauthors for the Impact of SARS Study. Prevalence of psychiatric disorders among Toronto hospital workers one to two years after the SARS outbreak. Psychiatr Serv. 2008;59:91-95. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 265] [Cited by in RCA: 252] [Article Influence: 14.8] [Reference Citation Analysis (0)] |
| 81. | Lin CY, Peng YC, Wu YH, Chang J, Chan CH, Yang DY. The psychological effect of severe acute respiratory syndrome on emergency department staff. Emerg Med J. 2007;24:12-17. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 155] [Cited by in RCA: 173] [Article Influence: 9.6] [Reference Citation Analysis (0)] |
| 82. | Gao H, Hui W, Lan X, Wei J, Hu YL, Li R, Zhang ZQ, Yuan ST, Jiao ZS. A follow-up study of post-traumatic stress disorder of SARS patients after discharge. Chin J Rehabil Med. 2006;21:1003-1004. |
| 83. | Xu Y, Zhang K, Xue Y. A study on post-traumatic stress reaction of hospital staffs worked in the ward of SARS. Huli Yanjiu. 2004;2:179-181. |
| 84. | Wong S. Psychological reaction of healthcare workers in the outbreak and aftermath of severe acute respiratory syndrome. Unpublished Thesis. The University of Hong Kong, Hong Kong. 2004. [cited 17 January 2021]. Available from: https://www.airitilibrary.com/Publication/alDetailedMesh1?DocID=U0029-1812201200003583. |
| 85. | Sin SS, Huak CY. Psychological impact of the SARS outbreak on a Singaporean rehabilitation department. Int J Ther Rehabil. 2004;11:417-424. |
| 86. | Chen CS, Wu HY, Yang P, Yen CF. Psychological distress of nurses in Taiwan who worked during the outbreak of SARS. Psychiatr Serv. 2005;56:76-79. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 151] [Cited by in RCA: 147] [Article Influence: 7.4] [Reference Citation Analysis (0)] |
| 87. | Tham KY, Tan YH, Loh OH, Tan WL, Ong MK, Tang HK. Psychiatric morbidity among emergency department doctors and nurses after the SARS outbreak. Ann Acad Med Singap. 2004;33:S78-S79. [PubMed] |
| 88. | Maunder RG, Lancee WJ, Balderson KE, Bennett JP, Borgundvaag B, Evans S, Fernandes CM, Goldbloom DS, Gupta M, Hunter JJ, McGillis Hall L, Nagle LM, Pain C, Peczeniuk SS, Raymond G, Read N, Rourke SB, Steinberg RJ, Stewart TE, VanDeVelde-Coke S, Veldhorst GG, Wasylenki DA. Long-term psychological and occupational effects of providing hospital healthcare during SARS outbreak. Emerg Infect Dis. 2006;12:1924-1932. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 863] [Cited by in RCA: 736] [Article Influence: 38.7] [Reference Citation Analysis (0)] |
| 89. | Mak IW, Chu CM, Pan PC, Yiu MG, Ho SC, Chan VL. Risk factors for chronic post-traumatic stress disorder (PTSD) in SARS survivors. Gen Hosp Psychiatry. 2010;32:590-598. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 159] [Cited by in RCA: 160] [Article Influence: 10.7] [Reference Citation Analysis (0)] |
| 90. | McAlonan GM, Lee AM, Cheung V, Cheung C, Tsang KW, Sham PC, Chua SE, Wong JG. Immediate and sustained psychological impact of an emerging infectious disease outbreak on health care workers. Can J Psychiatry. 2007;52:241-247. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 462] [Cited by in RCA: 454] [Article Influence: 25.2] [Reference Citation Analysis (0)] |