Published online Apr 19, 2022. doi: 10.5498/wjp.v12.i4.636
Peer-review started: February 24, 2021
First decision: April 21, 2021
Revised: April 24, 2021
Accepted: March 14, 2022
Article in press: March 14, 2022
Published online: April 19, 2022
Processing time: 412 Days and 23.8 Hours
Sleep problems are particularly prevalent in people with depression or anxiety disorder. Although mindfulness has been suggested as an important component in alleviating insomnia, no comprehensive review and meta-analysis has been conducted to evaluate the effects of different mindfulness-based intervention (MBI) programs on sleep among people with depression or anxiety disorder.
To compare the effects of different MBI programs on sleep among people with depression or anxiety disorder.
Related publications in Embase, Medline, PubMed and PsycINFO databases were systematically searched from January 2010 to June 2020 for randomised controlled trials. Data were synthesized using a random-effects or a fixed-effects model to analyse the effects of various MBI programs on sleep problems among people with depression or anxiety disorder. The fixed-effects model was used when heterogeneity was negligible, and the random-effects model was used when heterogeneity was significant to calculate the standardised mean differences (SMDs) and 95% confidence intervals (CIs).
We identified 397 articles, of which 10 randomised controlled trials, involving a total of 541 participants, were included in the meta-analysis. Studies of internet mindfulness meditation intervention (IMMI), mindfulness meditation (MM), mindfulness-based cognitive therapy (MBCT), mindfulness-based stress reduction (MBSR) and mindfulness-based touch therapy (MBTT) met the inclusion criteria. The greatest effect sizes are reported in favour of MBTT, with SMDs of -1.138 (95%CI: -1.937 to -0.340; P = 0.005), followed by -1.003 (95%CI: -1.645 to -0.360; P = 0.002) for MBCT. SMDs of -0.618 (95%CI: -0.980 to -0.257; P = 0.001) and -0.551 (95%CI: -0.842 to -0.260; P < 0.0001) were reported for IMMI and MBSR in the pooling trials, respectively. Significant effects on sleep problem improvement are shown in all reviewed MBI programs, except MM, for which the effect size was shown to be non-significant.
All MBI programs (MBTT, MBCT, IMMI and MBSR), except MM, are effective options to improve sleep problems among people with depression or anxiety disorder.
Core Tip: This meta-analysis provides evidence as to whether various kinds of mindfulness-based intervention programs can help improve sleep problems among people with common mental disorders. Our study indicated that integrative forms of mindfulness-based intervention programs (including mindfulness-based touch therapy, mindfulness-based cognitive therapy, internet mindfulness meditation intervention, and mindfulness-based stress reduction) have shown promising results. However, using mindfulness meditation solely should lead to insignificant effects.
- Citation: Chan SHW, Lui D, Chan H, Sum K, Cheung A, Yip H, Yu CH. Effects of mindfulness-based intervention programs on sleep among people with common mental disorders: A systematic review and meta-analysis. World J Psychiatry 2022; 12(4): 636-650
- URL: https://www.wjgnet.com/2220-3206/full/v12/i4/636.htm
- DOI: https://dx.doi.org/10.5498/wjp.v12.i4.636
Depression and anxiety disorder, also known as common mental disorders, are conditions that critically affect people’s emotions, energy and ability to function. Approximately 1 in 5 adults were identified as meeting criteria for a common mental disorder over the past 12 mo, with the lifetime prevalence reported as 20.8% and 28.8% for depression and anxiety disorder, respectively[1,2]. Both depression and anxiety disorder are among the top 10 causes of disease burden worldwide[3], prompting the necessity to find ways for better treatment and planning of care.
Insomnia frequently co-occurs with both depression[4] and anxiety disorder[5]. Sleep problems, which include difficulty in falling asleep, early awakening, poor sleep quality, daytime sleepiness and poor adherence to the sleep-wake cycle pattern, are particularly prevalent among people with depression and anxiety disorder[6]. The relationships between insomnia and common mental disorders appear to be bidirectional[7]. Symptoms of anxiety and depression, such as worry and rumination, can contribute to insomnia. Alternatively, insomnia can also increase the likelihood of developing depression or anxiety disorder, possibly due to the psychological distress as well as hormonal and neurochemical disturbances caused by poor sleep[8,9]. Thus, interventions aiming at reducing symptoms of insomnia should provide benefit for the disorder per se[10].
Individuals may consider psychotherapy instead of pharmaceutical treatment, due to possible side effects and potential dependence on medication[11-13]. Cognitive behavioural therapy (CBT) has been substantially confirmed to be an effective psychosocial treatment in managing depression and anxiety[14,15]. In a meta-analysis of 1205 CBT trials for anxiety disorders, results indicated that CBT for anxiety has a moderate effect on sleep[16]. In terms of the treatment of both depression and insomnia, another study found that the addition of CBT for insomnia (known as CBT-I) to antidepressant medication treatment can lead to better treatment outcomes[17]. However, some reviews showed that the effect sizes of CBT for depression have steadily decreased since its inception four decades ago[18,19]. Therefore, merely employing CBT might not be sufficient for managing mood disorders and their corresponding sleep problems.
Due to the limitations of traditional treatments, many people who experience insomnia are willing to consider using complementary and alternative medicine (CAM) as an alternative therapeutic option, including natural herbal products, acupuncture, or mind-body interventions, for example. A national health survey revealed that approximately 1.6 million adults in the United States have used CAM therapies to treat sleep problems[20]. Among different CAM therapies, the mind-body domains are by far the most commonly used[20]. Mindfulness-based interventions (MBIs), as a kind of CAM mind-body treatment with a focus on cultivating a sense of awareness, was originally developed to help people dealing with stress, anxiety, depression, or pain[21]. Mindfulness (Pali: sati) originated from Buddhism. As such, mindfulness can be defined as deliberately cultivating non-judgmental moment-to-moment awareness and experiences, through observing one’s own mind in a detached manner[22]. Various formal and informal mindfulness activities, such as body scan and sitting meditation, are included within the MBIs. Through these practices, the technique of ‘focusing on present moment’ can be acquired based on approach, compassion and decentring[23]. The inquiry process, which assists participants in identifying their thoughts, emotions and behaviours, is also included in these programs to help participants respond with more flexibility and awareness[24].
Conventional MBI has standardised protocols, and typically incorporates three formal mindfulness practices, namely body scan, mindful movement and sitting meditation[23]. A traditional program called mindfulness-based stress reduction (MBSR), kicking off the development of the mindfulness-based program in the health care domain, was first introduced by Kabat-Zinn[22]. It is an 8-wk program using mindfulness meditation (MM) and mindfulness practice in everyday life to relieve stress. Since then, another well-researched program — mindfulness-based cognitive therapy (MBCT) — was developed with comparable structures[25]. It is also an 8-wk program, which includes mindfulness practice and psychoeducation about depression, promoting awareness, acceptance and adaptive reaction towards negative automatic thoughts[25]. Apart from preventing relapse in depression, MBCT is also used to treat patients with psychiatric conditions, like anxiety disorders and post-traumatic stress disorder (PTSD)[26,27].
Since the commencement of MBSR, various forms of mindfulness programs have evolved with different adaptations or modifications, such as the Mindfulness-Based Therapy for Insomnia (MBTI)[28], internet mindfulness meditation intervention (IMMI)[29], Mindfulness Awareness Program (MAP)[30], or mindfulness-based touch therapy (MBTT)[31]. Specifically, MBTI was developed for patients with insomnia. It integrates mindful meditation and behavioural therapy. By promoting awareness and adaptive response towards sleep disturbances, MBTI helps people with chronic insomnia with sleep restrictions and stimulus control[28]. IMMI was developed to offer mindfulness training anytime and anywhere by use of an Internet mode of delivery. IMMI includes six 1-h weekly sessions with 20 min of home-practice meditation between sessions[29]. MAP aims to teach participants principles of mindfulness, develop meditation practice and apply them in daily lives. MAP is mainly conducted in community settings, with a combination of lecture, hands-on practice, group feedback and discussion[30]. MBTT is an 8-wk program that combines components of MBSR and touch therapy. It was inspired by Ogden et al[32]’s model of hierarchical information processing, in which touch stimulus triggers sensorimotor reaction, which is then experienced as emotions and interpreted cognitively. Touch is believed to have healing effects on both the mind and body[31].
At present, various studies have been published for the different MBIs. However, the review type studies usually focus on the conventional programs, like MBSR or MBCT[33,34]. While there are different forms of emerging MBIs in recent years, it is essential to have a comprehensive evaluation on their clinical effectiveness. Moreover, the traditional MBI programs have usually targeted general physical and psychiatric conditions; later on, they were used in the management of various kinds of physical or psychosomatic conditions, and even insomnia problems[35]. Recent meta-analyses indicated that MBIs show promising effects on the reduction of sleep problems[36-39]. However, these meta-analyses focused on the general population only or on people with physical comorbidities, such as cancer and fibromyalgia. Therefore, systematic review and meta-analysis on the effectiveness of the various MBI programs for sleep problems in individuals with depression or anxiety disorders is implied.
The objective of this meta-analysis was to determine and compare the clinical importance of different MBI programs on sleep problems among individuals with common mental disorders. Based on our research, this meta-analysis is uniquely able to fill a crucial gap in the field.
Literature searches were performed according to the 2009 PRISMA Statement for systematic reviews, by two independent researchers (Lui D and Chan H). The search keywords of “mindfulness” and “mood or anxiety or depress*” and “sleep or insomnia” were used to ensure comprehensive coverage. Keyword searches were conducted in Embase, Medline (accessed through EBSCOhost), PubMed and PsycINFO (accessed through ProQuest) databases. Papers published between January 2010 and June 2020 were included. Publications were only restricted to English language and peer-reviewed.
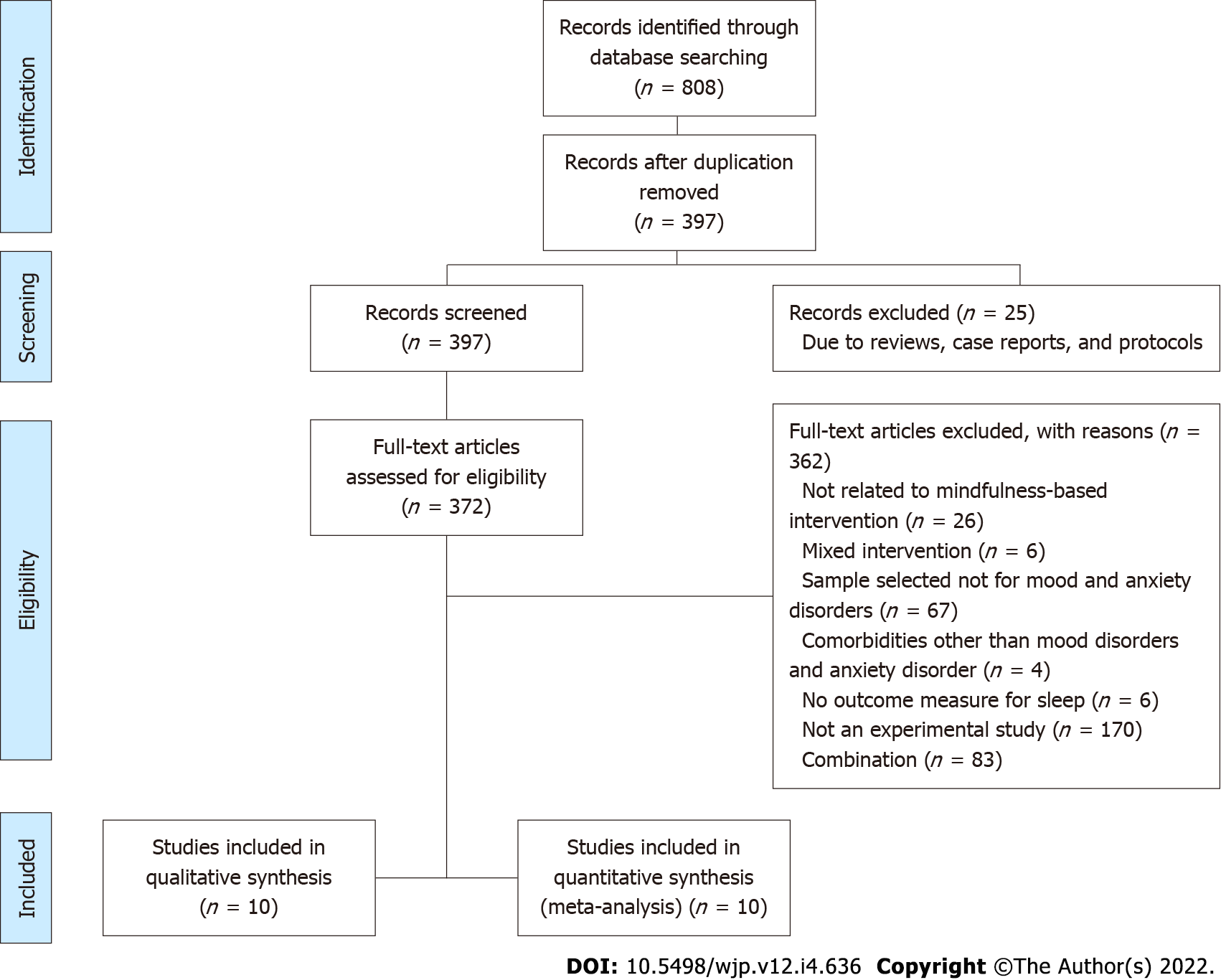
Titles and abstracts were screened, and full texts were selected for further review according to the following criteria. The inclusion criteria were as follows: (1) Experimental study with MBI; (2) Subjects selected for depression or anxiety disorder; (3) Sleep-related data taken at baseline and post-intervention; and (4) Randomised controlled trials (RCTs). The exclusion criteria were as follows: (1) Mixed intervention; or (2) Subjects with comorbidities other than depression or anxiety disorders. The selection criteria were confirmed according to the results of searching. The PRISMA flow diagram is shown in Figure 1.
An extraction form was used for each article to collect the following data: year of publication; subject setting; inclusion and exclusion criteria for participants; sample size for the experimental and control groups; participants’ age and sex; intervention given; and outcome measures related to sleep quality. Relevant statistics and effect sizes were also extracted, if available.
Two reviewers (Lui D and Yip H), working independently, assessed the level of evidence (LoE) and appraisal stage for each of the articles using a standard quality assessment, namely the LoE[40] and revised cochrane risk-of-bias tool for randomised trials (RoB)[41] respectively. The LoE categorizes different experimental studies into different levels on a scale of I to V, with a smaller number indicating a higher LoE. The RoB was used to assess the risk of bias in the RCTs. A series of signalling questions were available in each of the five domains of assessment, and judgements were facilitated by an algorithm that maps responses to the signalling questions to a proposed judgement. Overall risk of bias of the individual study would be reported as “low risk of bias”, “some concerns” or “high risk of bias”. Disagreements between the two independent reviewers were resolved by a third reviewer through a consensus-based discussion.
Statistical analysis of the pooled results was carried out using the Comprehensive Meta-Analysis software version 3.0 (https://www.meta-analysis.com). In nine of the ten studies, standardised mean differences (SMDs) and 95% confidence intervals (CIs) were calculated using post-intervention differences between the mean of mindfulness-based programs and the mean of controls, divided by the pooled standard deviation. No real differences in variability among studies were assumed according to the Cochrane Handbook for Systematic Reviews of Interventions[42]. A global estimation of r = 0.6 was, therefore, used as the correlation coefficient between post-treatment scores. In the remaining study, Cohen’s d was calculated using the two groups, via the one-way F-test using a practical meta-analysis effect size calculator[43]. When there was more than one group compared to the MBI group in the RCT, the non-intervention group was used as the control. The Q-statistic was used as the heterogeneity test, in which a statistically significant level of P < 0.05 indicated the variations in effect sizes were due to heterogeneity rather than sampling error. A random-effects model would be used when there was notable heterogeneity. Random-/fixed-effects models were used as the intervention effects are unlikely to be identical[44] given that there are significant variations in characteristics of each sample population. Publication bias was assessed by funnel plot, trim-and-fill and failsafe N. Unless otherwise specified, all statistical tests were two-sided with a significance level of 0.05.
A total of 808 entries were identified through database searches, and 397 of them were screened after duplicates removed. After reading the abstract and title of the remaining 397, we removed 25 reviews, case reports, and protocols. Full versions were retrieved for 372 papers, after which they were reviewed by two independent researchers (Chan H and Sum K) and disagreements were resolved by a third reviewer (Lui D) on a consensus-based discussion. In total, 362 full articles were excluded for not meeting all the inclusion criteria. Finally, 10 eligible studies were selected for systematic review and meta-analysis (details shown in Figure 1).
Ten studies met the inclusion criteria, overall reporting five different kinds of mindfulness-based programs, including IMMI, MM, MBCT, MBSR and MBTT. Table 1 shows the study characteristics of the 10 trials. The studies were conducted in the United States, Germany, Norway, Australia and Austria, within years that fell between 2010 and 2019. A total of 541 participants were included in the intervention groups and comparison groups. When there were multiple intervention groups, we chose the mindfulness-based programs as the major intervention groups[45-47].
| Ref. | Country | Sample | Age range (mean) | Women, n (%) | Randomisation | Intervention group (comparison group) | Intervention duration | Group size for effect size calculation, n | Drop-out rate1 (%) | Outcome measure for sleep |
| Wahbeh[29], 2018 | United States | Older adult with depression symptoms | 55-80 (64.8) | 21 (81) | R | IMMI (waitlist control) | 6 wk | I = 26 C = 24 | 20.00 | Sleep disturbance, ISI |
| Boettcher et al[50], 2014 | Germany | Community dwellers with anxiety disorders | 18+ (37) | 34 (75.6) | R | IMMI (discussion forum control group) | 8 wk | I = 45 C = 46 | 7.69 | ISI |
| Wahbeh et al[47], 2016 | United States | Combat veterans with post-traumatic stress disorder | 25-65 (I = 53.3; C = 53.0) | 2 (7) | R | MM (sitting quietly) | 6 wk | I = 27 C = 25 | 0 | PSQI |
| Britton et al[49], 2012 | United States | Antidepressant medication users with sleep complaints | 24-61 (47.0) | 21 (80.8) | R | MBCT (control) | 8 wk | I = 14 C = 10 | 7.69 | TIB, TST, SE, SOL, WASO, TWT, Stage 1, SWS, Quality |
| Vøllestad et al[51], 2011 | Norway | Community dwellers with anxiety disorders | 18-65 (42.5) | 26 (66.7) | R | MBSR (waitlist control) | 8 wk | I = 39 C = 37 | 14 | BIS |
| Britton et al[48], 2010 | United States | Community dwellers with partially remitted depression | 33-64 (45.4) | 9 (69.2) | R | MBCT (control) | 8 wk | I = 13 C = 8 | 19.23 | TIB, TST, SE, SOL, WASO, NWAK, Arousals, Stage 1, SWS, Quality |
| Hoge et al[52], 2013 | United States | Referral/community dwellers with generalized anxiety disorder | 18+ (I = 41; C = 37) | 23 (47.9) | R | MBSR (stress management education) | 8 wk | I = 48 C = 45 | 4.30 | Sleep quality, PSQI |
| Horenstein et al[45], 2019 | United States | Adults with social anxiety disorder | 18+ (32.7) | Not specified | R | MBSR (control) | 12 wk | I = 36 C = 36 | 15.28 | Sleep quality, PSQI |
| Pinniger et al[46], 2013 | Australia | Adults with self-reported feelings of stress, anxiety, and/or depression | 18-68 (39.5) | 10 (90.9) | R | MM (waitlist control) | 8 wk | I = 11 C = 23 | 30.60 | Sleeping difficulty/insomnia, ISI |
| Stötter et al[31], 2013 | Austria | Patients of the psychiatric hospital of Hall in Tirol | 18+ (I = 42.8; C = 41.4) | 11 (68.75) | R | MBTT (control) | 8 wk | I = 14 C = 14 | 0 | Sleep-onset disorder, Sleep maintenance disorders, Terminal sleep disorders, HDRS |
Across studies, participants had a range of mean age between 32.7 and 64.8 years. Seven out of ten (70%) of the studies had a majority of female participants. Four out of ten studies (40%) focused on community dwellers with anxiety and/or major depressive disorder. One study included participants of veterans with PTSD. Six out of ten studies reported significant improvement in sleep quality as measured by insomnia severity index (ISI), Pittsburgh sleep quality index (PSQI), Bergen insomnia scale (referred to as BIS), Hamilton depression rating scale (HDRS) and sleep diaries, provided that the P value of the experiment was lower than 0.05. All of the studies were RCTs. The duration of the intervention ranged from 6 wk to 12 wk and delivered over 6 to 12 sessions. Details of intervention techniques and selected outcome measures of each study are provided in Table 2.
| Mindfulness-based program | Intervention components | Selected outcome measures for effect size calculation | Ref. | |
| Intervention group | Comparison group | |||
| IMMI | DI + MM + MPS | WL | ISI | Wahbeh[29], 2018 |
| ME + psychoeducation | DF | ISI | Boettcher et al[50], 2014 | |
| MM | BS | SB | PSQI | Wahbeh et al[47], 2016 |
| BS | BS + SB | PSQI | Wahbeh et al[47], 2016 | |
| BS | SQ | PSQI | Wahbeh et al[47], 2016 | |
| BS + MB + MW + music meditation | WL | ISI | Pinniger et al[46], 2013 | |
| MBCT | MA + HW (Guided audio CD) | Control | Sleep diary | Britton et al[48], 2010 |
| MA (MB + MS + MW + lying + other simple movement) + HW (MM using audio CD + worksheet) | Control | Sleep diary | Britton et al[49], 2012 | |
| MBSR | BS + SM + MB + AR + DI + ME + MMV + HW | WL | Bergen insomnia scale | Vøllestad et al[51], 2011 |
| BS+ BA+ gentle Hatha Yoga | SME | PSQI | Hoge et al[52], 2013 | |
| BS + SM + MS + MPS | WL | PSQI | Horenstein et al[45], 2019 | |
| MBTT | BA + touch + HW + counselling | BMT | HDRS | Stötter et al[31], 2013 |
Results from quality assessments are presented in Tables 3 and 4. All studies were RCTs. All trials had adequate sequence generation, among which five (50%) indicated a concealed allocation[49-51]. As for blinding, two trials adopted double-blind design[48,49], one trial used single-blind design[31] and two used blind evaluators[47,52]. The drop-out rates of the trials ranged from 0% to 30.6%, as shown in Table 1. Of the 10 trials, 3 had low drop-out rates (≤ 5%)[31,47,52] and two had high drop-out rates (≥ 20%)[29,46]. The overall LoE was level II (n = 10), showing that the papers under current review were of high LoE. The overall RoBs were as follows: low (n = 2); some concerns (n = 6); and high (n = 2). The majority of papers showed some concerns of risk of bias, mainly due to bias in the measurement of outcome.
| Ref. | Research design | Level of evidence |
| Wahbeh[29], 2018 | RCT, crossover design | II |
| Boettcher et al[50], 2014 | RCT, crossover design | II |
| Wahbeh et al[47], 2016 | RCT, multi-group pre-/post-test design | II |
| Britton et al[49], 2012 | RCT, pre-/post-test control group design | II |
| Vøllestad et al[51], 2011 | RCT, crossover design | II |
| Britton et al[48], 2010 | RCT, pre-/post-test control group design | II |
| Hoge et al[52], 2013 | RCT, two group pre-/post-test design | II |
| Horenstein et al[45], 2019 | RCT, multi-group pre-/post-test design | II |
| Pinniger et al[46], 2013 | RCT, multi-group pre-/post-test design | II |
| Stötter et al[31], 2013 | RCT, pre-/post-test control group design | II |
| Ref.
| Randomisation process | Deviation from intended intervention | Missing outcome data | Measurement of outcome | Selection of the reported results | Overall |
| Wahbeh[29], 2018 | Low risk | Low risk | Some concerns | Some concerns | Low risk | High |
| Boettcher et al[50], 2014 | Low risk | Low risk | Low risk | Some concerns | Low risk | Some concerns |
| Wahbeh et al[47], 2016 | Low risk | Low risk | Low risk | Some concerns | Low risk | Some concerns |
| Britton et al[49], 2012 | Low risk | Low risk | Low risk | Some concerns | Low risk | Some concerns |
| Vøllestad et al[51], 2011 | Low risk | Low risk | Low risk | Some concerns | Low risk | Some concerns |
| Britton et al[48], 2010 | Low risk | Some concerns | Low risk | Low risk | Low risk | Some concerns |
| Hoge et al[52], 2013 | Low risk | Low risk | Low risk | Low risk | Low risk | Low |
| Horenstein et al[45], 2019 | Low risk | Low risk | Low risk | Some concerns | Low risk | Some concerns |
| Pinniger et al[46], 2013 | Low risk | High risk | Some concerns | Low risk | Low risk | High |
| Stötter et al[31], 2013 | Low risk | Low risk | Low risk | Low risk | Low risk | Low |
This meta-analysis focused on examining the effect at the end point of different mindfulness-based programs, including IMMI, MM, MBCT, MBSR and MBTT, due to variations in follow-up periods and absence of reported follow-up effects in several studies. The overall effect analysed was based on the comparison between different mindfulness-based programs and comparison groups, including discussion forum, waitlist control, slow breathing, stress management education, sitting quietly and basic medicinal therapy. Self-rated outcome measurements were reported in the 10 RCTs assessed, including PSQI, ISI, sleep quality of sleep diary, and sleep maintenance of HDRS. The overall scores of sleep quality were reported in PSQI, ISI, BIS and sleep diaries. On the other hand, there was no overall score on sleep quality presented in HDRS. The component of sleep maintenance in HDRS was, therefore, selected. Sleep maintenance was selected instead of sleep onset and sleep termination, as the level of sleep maintenance better predicts perceived sleep quality[53]. Other outcome measurements which are not self-rated, including sleep onset latency, total sleep time and wake after sleep onset, were not reported in this meta-analysis.
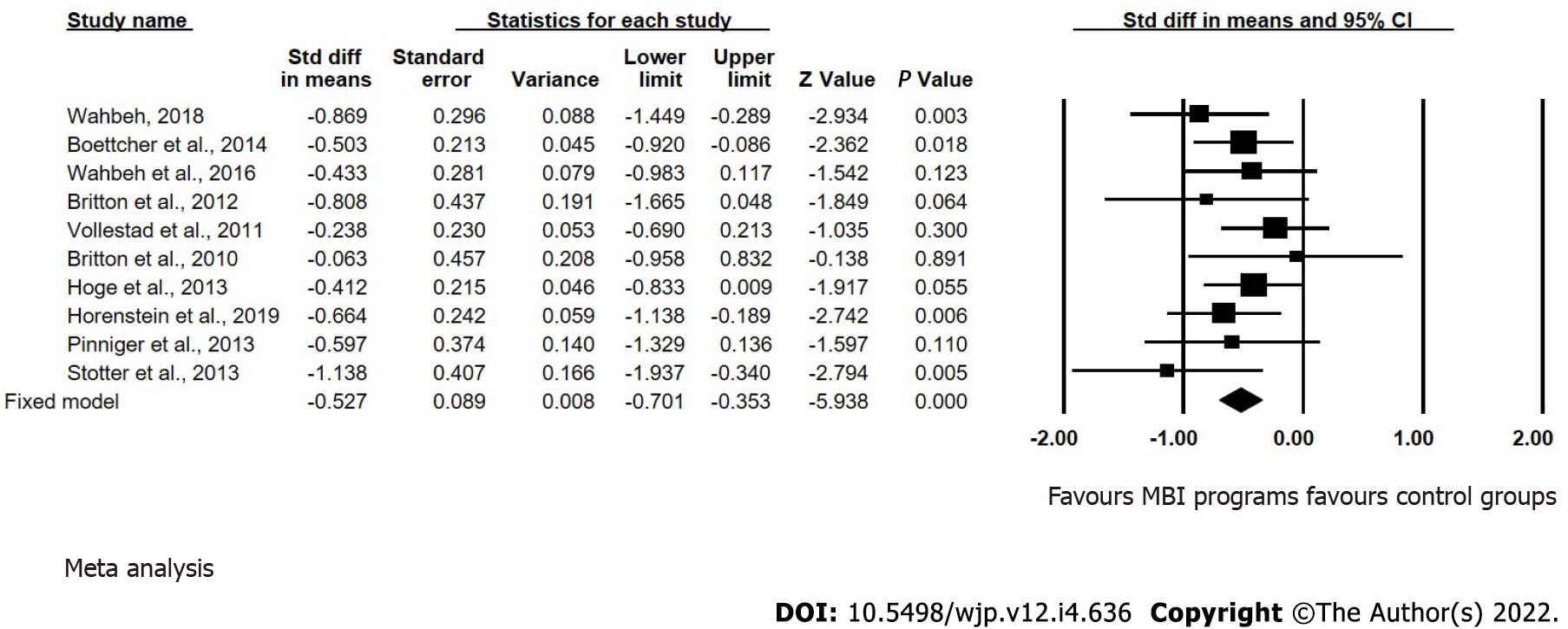
The mean effect sizes on sleep problem improvement of different mindfulness-based programs, as compared with control groups, are provided in Table 5. The forest plot in Figure 2 shows the effect sizes and 95%CIs of the 10 studies assessed. The meta-analysis reveals a moderate pooled effect size (g = -0.527, 95%CI: -0.701 to -0.353) in favor of MBI program. Significant effects on sleep problem improvement were shown in four out of five of the different mindfulness-based programs under review, namely MBTT, MBCT, IMMI and MBSR (reflecting descending order of effect sizes). The greatest effect sizes were reported in favour of MBTT, with SMDs of -1.138 (95%CI: -1.937 to -0.340; P = 0.005), followed by -1.003 (95%CI: -1.645 to -0.360; P = 0.002) for MBCT. SMDs of -0.618 (95%CI: -0.980 to -0.257; P = 0.001) and -0.551 (95%CI: -0.842 to -0.260; P < 0.0001) were reported for IMMI and MBSR in the pooling trials, respectively. However, among the five kinds of mindfulness-based programs under review, the mean effect size for MM on sleep was non-significant, with SMD of -0.264 (95%CI: -0.699 to 0.172; P = 0.236).
| Ref. | Mindfulness-based program | k | Subjects, n | SMD (95%CI) | P value | Overall SMD (95%CI) | Overall P value | Q |
| Wahbeh[29], 2018 | IMMI | 2 | 124 | -0.881 (-1.531 to -0.231) | 0.008 | -0.618 (-0.980 to -0.257) | 0.001 | 0.912 (P = 0.34) |
| Boettcher et al[50], 2014 | -0.500 (-0.935 to -0.066) | 0.024 | ||||||
| Wahbeh et al[47], 2016 | MM | 2 | 86 | -0.267 (-0.814 to 0.279) | 0.337 | -0.264 (-0.699 to 0.172) | 0.236 | 0.001 (P = 0.981) |
| Pinniger et al[46], 2013 | -0.257 (-0.978 to 0.464) | 0.485 | ||||||
| Britton et al[48], 2010 | MBCT | 2 | 43 | -1.073 (-1.953 to -0.192) | 0.017 | -1.003 (-1.645 to -0.360) | 0.002 | 0.052 (P = 0.82) |
| Britton et al[49], 2012 | -0.923 (-1.862 to 0.016) | 0.054 | ||||||
| Hoge et al[52], 2013 | MBSR | 3 | 187 | -0.449 (-0.942 to 0.043) | 0.074 | -0.551 (-0.842 to -0.260) | < 0.0001 | 0.332 (P = 0.847) |
| Horenstein et al[45], 2019 | -0.555 (-1.056 to -0.053) | 0.03 | ||||||
| Vøllestad et al[51], 2011 | -0.660 (-1.178 to -0.141) | 0.013 | ||||||
| Stötter et al[31], 2013 | MBTT | 1 | 28 | -1.138 (-1.937 to -0.340) | 0.005 | -1.138 (-1.937 to -0.340) | 0.005 | 0 (P = 1) |
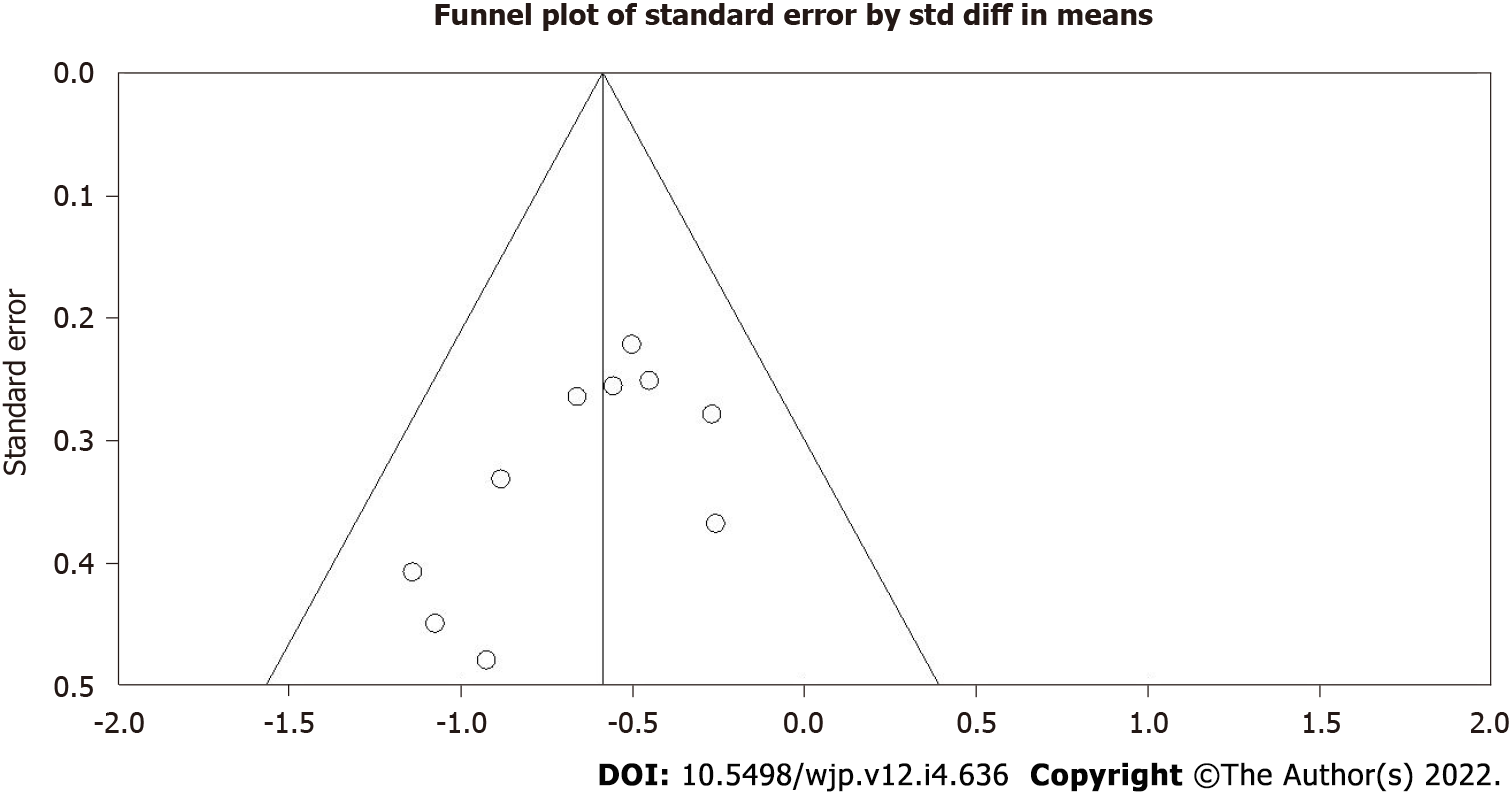
Table 5 shows that all the heterogeneities (Q) were non-significant across the different MBI programs. The non-significant Q-statistics might suggest that the variation in the effect sizes across the studies was simply due to low power but not the study characteristics. Three sets of asymmetry tests — namely, funnel plots of precision, trim-and-fill and failsafe N — were used to estimate the publication bias in each study. Symmetrical distribution of the combined effect size revealed the absence of publication bias upon visual inspection of the funnel plots (Figure 3). To further examine the funnel plot symmetry, Duval and Tweedie’s trim-and-fill procedure was used. No significant adjustment was needed and no study was trimmed due to the absence of unmatched observations from the funnel plots. Failsafe N analyses demonstrated that 96 missing studies with a zero effect size have to be added to reduce the significant overall effect size to statistically non-significant levels.
This meta-analysis showed that MBTT imparts the largest effect on sleep problems among the five different kinds of mindfulness-based programs under review, followed by MBCT, IMMI and MBSR. According to Cohen[54]’s thresholds for interpreting effect size, SMDs smaller than 0.20 would be regarded as small effect size, 0.50 as medium, 0.80 as large and 1.30 as very large. However, it is important to point out that Cohen defined the medium effect size based on his literature review using the Journal of Abnormal and Social Psychology during the 1960s. These small, medium, and large effect sizes are, thus, specific to a particular domain (abnormal and social psychology) and as such these cut-off points should not be treated as absolute or universal. By Cohen’s convention, MBTT and MBCT have large effect sizes. IMMI and MBSR have medium effect sizes, and MM has a small effect size. It should be noted that, despite the large effect size of MBTT on sleep, only one study contributed to this result, while the results of the remaining four different kinds of mindfulness-based programs were supported by at least two or more studies. In addition, the effect of MM on sleep did not reach a significant level, despite having a small effect size. This may be explained by the unexplored improvements in sleep problems in the comparison group, leading to the comparatively non-significant effect of MM. Although previous findings suggested that MM is an effective treatment for insomnia[37], its effect on sleep for people with depression and anxiety disorder remains questionable, as shown in this meta-analysis.
As such, MBTI has been commonly used to treat patients with chronic insomnia or sleep problems[35]. However, many studies involving MBTI[28,55] did not target people with depression or anxiety disorder, so MBTI was not selected in the current meta-analysis (according to the inclusion criteria). When further scrutinized, the goals of MBTI usually aim at promoting the adaptive response towards the emotional distress caused by sleep disturbances and daytime fatigue among people with chronic insomnia. However, the present review study revealed that those MBI programs which can improve sleep problems among people with depression or anxiety disorder may have additional characteristics. More specifically, those MBI programs under review were found to ameliorate both the mood and sleep problems concurrently. In other words, these MBI programs could target both the antecedents and consequences of sleep problems for people with common mental disorders.
MBTT[31] was found to have the largest effect on sleep problems, according to the meta-analysis. MBTT, which is based on mindfulness practice and various forms of massage and bodywork, could improve sleep by restoring interception and sensorimotor processing of individuals with depression and anxiety disorder. Regarding the effect of touch per se, the rhythmic and gentle massage produced a direct bodily and sensory experience[31]. This resulted in an antidepressant effect mediated by restoration of the impaired interoceptive functioning, which is associated with depression and anxiety[56,57], through stimulation of specific mechanoreceptors[58]. Adding to the independent effect of touch, a possible explanation for the synergistic effects of combining mindfulness practice and therapeutic touch is the model of hierarchical information processing, which suggested that mindfulness-based touch intervention gave rise to the integration of sensorimotor bodily experience with mindful cognitive self-awareness[32]. In line with this explanation, a cortical plasticity model suggested that the sensory reorganization sprung from touch therapy was a mechanism for pain remediation[59]. Similarly, considering a previous study documenting the relationship between sensory processing and sleep quality[60], it is plausible that improving sensory processing through a mindfulness-orientated touch approach could, in turn, ameliorate sleep disturbance in people with depression or anxiety disorder.
Besides, we also found that MBCT[48,49] can help improve sleep problems among people with depression or anxiety disorder, with large effect sizes. In addition to traditional mindfulness skills, MBCT incorporates cognitive behavioural skills which can enhance the effectiveness in coping with depressive mood and sleep problems. Despite the interrelated nature of depression and insomnia, it is theoretically debatable whether insomnia should be treated as a distinct diagnosis or a symptom of mood disorders[61]. Considering the complexity of insomnia, Shallcross et al[62] proposed a theoretical model to summarize the utility of MBCT in treating insomnia, suggesting that there are three treatment components (i.e., acceptance, attention control and experiential awareness) with different therapeutic functions across the integrated process model of insomnia. It is worth noting that the model of insomnia is in line with symptoms of people with depression. For example, rumination is associated with both depressive mood and sleep quality[63] and upregulated arousal is linked to sleep problems (e.g., longer sleep latency) in people with depressive syndromes[64,65]. The review studies suggested that MBCT can ameliorate the sleep disturbance of people who have achieved partial remission of depression (both with and without taking an anti-depressant) as well as significant mood improvement. It is possible that MBCT is not only a promising program for depression or insomnia alone, but also for improving sleep problems in people with depression. In addition, recent research has indicated that acceptance lessened the positive relation between awareness and sleep disturbance, with reduced stress level identified as a mediator[66]. This mechanism is consistent with the Monitor and Acceptance Theory[67], which proposes that awareness and acceptance may jointly improve emotional regulation, including that of stress. In this sense, the effectiveness of MBCT to reduce stress[68,69] can partially explain the potential utility of MBCT in improving sleep outcomes.
Therefore, solely utilizing MM[46,47] may not be robust enough to improve sleep problems among people with depression or anxiety disorder, as indicated by the insignificant effect size shown in this study. No wonder recent meta-analyses[70,71] supported that MM is effective in reducing symptoms such as rumination among people with depression or anxiety disorder, but the sleeping problem might be improved in the short-term only. As a bidirectional relationship has been revealed between sleep disturbance and common mental disorders[7], it seems that a more integrated approach should be considered in order to enhance robustness of the intervention effects. For instance, the addition of a touch approach[31], cognitive component[50] or health qigong[72] should help in promoting the effectiveness of mindfulness practice, as applied in different clinical populations. Thus, the evolution of various kinds of integrated MBI programs should mark the necessity for meeting the increasing demand of various physical and mental health problems.
Our analysis showed that the majority of studies were coded as having some concerns by RoB. Most concerns arise from measurement of outcome, as most sleep measurements, such as PSQI, ISI and sleep diary, rely on self-report by the patients. With the awareness of the treatment received, the non-blind allocation should lead to increased risk of bias. In addition, improvements in sleep cannot be merely assessed by objective tools like polysomnography but will also still rely on self-rated assessment tools. Thus, there is a possibility that some studies of good quality are not coded as low RoB due to the strict restrictions in outcome measurement tools, as stated in the RoB tool used in the current study. The studies included in this meta-analysis involved diverse sample populations in various age groups and with different emotional disorders, including mood disorders, anxiety disorders and PTSD. However, the heterogeneities were not significant, despite the variations in study characteristics. This may be explained by the high similarity in outcome measurement tools, among which PSQI, ISI and sleep diary were widely used to assess sleep outcome in the studies. Moreover, many of the studies under review had similar study protocols, and some were even conducted by the same group of researchers. The non-significance in heterogeneity may also be attributed to the low power of the studies. Nevertheless, moderator analysis can be considered in the future for possible effects of the potential moderators.
Although the present meta-analysis suggests considerable clinical benefits of MBTT, MBCT, IMMI and MBSR on sleep among people with depression or anxiety disorder, the findings should be interpreted with caution. It should be noted that this meta-analysis has been primarily concerned with its limited power. A limited number of clinical trials on MBI programs are available in the literature databases, and many of the studies targeted populations with physical complications or other comorbidities. The result was that a relatively small number of trials met inclusion criteria. For example, there was only one study regarding MBTT that could be included. Thus, the effect of MBTT in our meta-analysis was solely determined by one study. The ability of funnel plot to detect publication bias was also restrained by the few number of trials included in our meta-analysis. Thus, there is a need to include larger clinical trials in the future to increase the study power. This analysis has concentrated on studying different kinds of MBI programs but not the specific components in the programs. It caused our study to have low generalizability compared to all the other protocols of the studied programs, because variations exist under the same program between different studies. For instance, gentle Hatha Yoga was included in one study of MBSR[52] but not in other trials[45,51]. Therefore, the effects of the MBI programs in this study are composed of various but nonspecific components. Further studies on specific intervention components, such as body scan, mindful walking, bodily awareness and mindful breathing are required. A further potential limitation of this review stems from the fact that the outcome measures of sleep focus on the subjective measurements only. The discrepancies in sleep measurement may have complicated the comparison. It is suggested that more objective and uniform measurement tools for sleep should be used in future studies in this field to facilitate a larger sample size and power in prospective systematic reviews and meta-analyses. For instance, polysomnography and electrocardiogram use scientific technology to investigate some objective components of sleep and can be considered[49,73]. These could provide more objective evidence than self-rated scales. Lastly, the lack of Asian studies means that we cannot be certain that the findings can be generalized to an Asian population. Studies included in the current review were carried out only in the United States, Germany, Norway, Australia and Austria. More clinical trials in Asian countries are encouraged to increase generalizability of findings from future studies. It is also suggested that a more specific age group could be targeted to study the effect of MBIs on different age groups, like elderly and adolescent.
Despite these limitations, this review study adds to the literature by investigating different kinds of MBI programs on sleep problem among people with common mental disorders. The comprehensive inclusion and exclusion criteria contribute to the uniqueness of this meta-analysis. Studies that included subjects with comorbidities and with mixed intervention were excluded and, at the same time, a wide variety of MBI programs were included. The criteria allowed this meta-analysis to focus more on the effect of different MBI programs in order to fill in a lacuna in the research. Additionally, this meta-analysis has the following strengths. First, it followed the guidelines of the Cochrane Collaboration, which provided a standard process of analysis. The PRISMA Statement was also adopted to support the integrity of its systematic review process. Second, only RCTs were included in this analysis. All the studies analysed had high LoEs and most of them had low to moderate risk of bias. Bias is reduced by study design of adequate concealed allocation and blinding. The high quality of study design of the 10 included studies assured the reliability and validity of their results. Thus, this meta-analysis truly reflects the effect of different MBI programs. Third, all the studies analysed were conducted in the last decade. Since the first introduction of MBCT and MBSR by Kabat-Zinn[22], many innovative forms of MBI have been developed, as mentioned in the introduction. The clinical interest towards MBI has continued throughout the years. The meta-analysis in this paper included studies conducted in 2011-2019, providing up-to-date information about the effect of different MBI programs on sleep among people with depression or anxiety disorders. The meta-analysis in this paper also focused on a specific client group and, as such, was able to provide an updated overview of comparison with traditional MBI and the newly developed programs.
The findings of our comprehensive systematic review and meta-analysis provide preliminary evidence that MBTT, MBCT, IMMI and MBSR are effective options to improve sleep among people with depression and anxiety disorder. MM, which has confirmed to be effective in improving sleep in people with chronic insomnia, may not be effective in our targeted population. Taken together, these results might provide a first step toward designing more integrated effective interventions for this specified clinical population who are suffering from sleep problems. We are hopeful that the findings of our research will inform health practitioners and other researchers on the extent of effectiveness of the different, latest and integrated MBI programs.
Sleep problems are particularly prevalent in people with depression or anxiety disorder. Although mindfulness has been suggested as an important component in alleviating insomnia, no comprehensive review and meta-analysis has been conducted to evaluate the effects of different kinds of mindfulness-based intervention (MBI) programs on sleep among people with depression or anxiety disorder.
The present study aimed to assess randomised controlled trials of various types of MBI programs for improving sleep problems in people with common mental disorders.
The main objective was to evaluate and update evidence of effectiveness of the different, latest and integrated MBI programs.
We performed a systematic literature search on Embase, Medline, PubMed and PsycINFO databases from January 2010 to June 2020 for randomised controlled trials. Data were synthesized using a random-effects or a fixed-effects model to analyse the effects of various MBI programs on sleep problems among people with depression or anxiety disorder. The fixed-effects model was used when heterogeneity was negligible, and the random-effects model was used when heterogeneity was significant to calculate the standardised mean differences (SMDs) and 95% confidence intervals (CIs).
We identified 397 articles, of which 10 randomised controlled trials, involving a total of 541 participants, were included in the meta-analysis. Studies of internet mindfulness meditation intervention (IMMI), mindfulness meditation (MM), mindfulness-based cognitive therapy (MBCT), mindfulness-based stress reduction (MBSR) and mindfulness-based touch therapy (MBTT) met the inclusion criteria. The greatest effect sizes are reported in favour of MBTT, with SMDs of -1.138 (95%CI: -1.937 to -0.340; P = 0.005), followed by -1.003 (95%CI: -1.645 to -0.360; P = 0.002) for MBCT. SMDs of -0.618 (95%CI: -0.980 to -0.257; P = 0.001) and -0.551 (95%CI: -0.842 to -0.260; P = 0.000) were reported for IMMI and MBSR in the pooling trials, respectively. Significant effects on sleep problem improvement are shown in all reviewed MBI programs, except MM, in which its effect size was shown to be non-significant.
This review presents a comprehensive meta-analysis of various forms of MBI programs on helping sleep problems among people with common mental disorders. We found that all MBI programs (in terms of MBTT, MBCT, IMMI and MBSR), except MM, are effective options to improve sleep problems among people with depression or anxiety disorder.
The current meta-analysis suggests that solely utilizing MM may not be robust enough to improve sleep problems among people with depression or anxiety disorder. As a bidirectional relationship was revealed between sleep disturbance and common mental disorders, it seems that a more integrated approach should be considered in order to enhance robustness of the intervention effects.
Provenance and peer review: Invited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Psychiatry
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Kim Y, United States S-Editor: Gao CC L-Editor: A P-Editor: Gao CC
| 1. | Kessler RC, Berglund P, Demler O, Jin R, Merikangas KR, Walters EE. Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication. Arch Gen Psychiatry. 2005;62:593-602. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11472] [Cited by in RCA: 11771] [Article Influence: 588.6] [Reference Citation Analysis (1)] |
| 2. | Steel Z, Marnane C, Iranpour C, Chey T, Jackson JW, Patel V, Silove D. The global prevalence of common mental disorders: a systematic review and meta-analysis 1980-2013. Int J Epidemiol. 2014;43:476-493. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2036] [Cited by in RCA: 1661] [Article Influence: 151.0] [Reference Citation Analysis (0)] |
| 3. | Walker ER, McGee RE, Druss BG. Mortality in mental disorders and global disease burden implications: a systematic review and meta-analysis. JAMA Psychiatry. 2015;72:334-341. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1534] [Cited by in RCA: 1964] [Article Influence: 196.4] [Reference Citation Analysis (0)] |
| 4. | Peterson MJ, Rumble ME, Benca RM. Insomnia and psychiatric disorders. Psychiatr Ann. 2008;38:597-605. [RCA] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 9] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 5. | Papadimitriou GN, Linkowski P. Sleep disturbance in anxiety disorders. Int Rev Psychiatry. 2005;17:229-236. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 155] [Cited by in RCA: 170] [Article Influence: 8.5] [Reference Citation Analysis (0)] |
| 6. | Soehner AM, Harvey AG. Prevalence and functional consequences of severe insomnia symptoms in mood and anxiety disorders: results from a nationally representative sample. Sleep. 2012;35:1367-1375. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 115] [Cited by in RCA: 117] [Article Influence: 9.0] [Reference Citation Analysis (0)] |
| 7. | Fang H, Tu S, Sheng J, Shao A. Depression in sleep disturbance: A review on a bidirectional relationship, mechanisms and treatment. J Cell Mol Med. 2019;23:2324-2332. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 233] [Cited by in RCA: 647] [Article Influence: 107.8] [Reference Citation Analysis (0)] |
| 8. | Irwin MR. Why sleep is important for health: a psychoneuroimmunology perspective. Annu Rev Psychol. 2015;66:143-172. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 482] [Cited by in RCA: 726] [Article Influence: 66.0] [Reference Citation Analysis (0)] |
| 9. | Selsick H, O'regan D. Sleep disorders in psychiatry. BJPsych Adv. 2018;24:273-283. [RCA] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 10. | Mason EC, Harvey AG. Insomnia before and after treatment for anxiety and depression. J Affect Disord. 2014;168:415-421. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 67] [Cited by in RCA: 86] [Article Influence: 7.8] [Reference Citation Analysis (0)] |
| 11. | Choy Y. Managing side effects of anxiolytics. Prim Psychiatry. 2007;14:68-76. |
| 12. | Starcevic V, Brakoulias V, Viswasam K, Berle D. Inconsistent portrayal of medication dependence, withdrawal and discontinuation symptoms in treatment guidelines for anxiety disorders. Psychother Psychosom. 2015;84:379-380. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 10] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 13. | Telang S, Walton C, Olten B, Bloch MH. Meta-analysis: Second generation antidepressants and headache. J Affect Disord. 2018;236:60-68. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 16] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 14. | Twomey C, O'Reilly G, Byrne M. Effectiveness of cognitive behavioural therapy for anxiety and depression in primary care: a meta-analysis. Fam Pract. 2015;32:3-15. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 69] [Cited by in RCA: 74] [Article Influence: 7.4] [Reference Citation Analysis (0)] |
| 15. | Zhang A, Borhneimer LA, Weaver A, Franklin C, Hai AH, Guz S, Shen L. Cognitive behavioral therapy for primary care depression and anxiety: a secondary meta-analytic review using robust variance estimation in meta-regression. J Behav Med. 2019;42:1117-1141. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 58] [Article Influence: 9.7] [Reference Citation Analysis (0)] |
| 16. | Belleville G, Cousineau H, Levrier K, St-Pierre-Delorme ME, Marchand A. The impact of cognitive-behavior therapy for anxiety disorders on concomitant sleep disturbances: a meta-analysis. J Anxiety Disord. 2010;24:379-386. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 54] [Cited by in RCA: 51] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 17. | Manber R, Edinger JD, Gress JL, San Pedro-Salcedo MG, Kuo TF, Kalista T. Cognitive behavioral therapy for insomnia enhances depression outcome in patients with comorbid major depressive disorder and insomnia. Sleep. 2008;31:489-495. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 580] [Cited by in RCA: 595] [Article Influence: 35.0] [Reference Citation Analysis (0)] |
| 18. | Lynch D, Laws KR, McKenna PJ. Cognitive behavioural therapy for major psychiatric disorder: does it really work? Psychol Med. 2010;40:9-24. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 205] [Cited by in RCA: 151] [Article Influence: 10.1] [Reference Citation Analysis (0)] |
| 19. | Johnsen TJ, Friborg O. The effects of cognitive behavioral therapy as an anti-depressive treatment is falling: A meta-analysis. Psychol Bull. 2015;141:747-768. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 168] [Cited by in RCA: 173] [Article Influence: 17.3] [Reference Citation Analysis (0)] |
| 20. | Pearson NJ, Johnson LL, Nahin RL. Insomnia, trouble sleeping, and complementary and alternative medicine: Analysis of the 2002 national health interview survey data. Arch Intern Med. 2006;166:1775-1782. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 215] [Cited by in RCA: 219] [Article Influence: 11.5] [Reference Citation Analysis (0)] |
| 21. | Kabat-Zinn J. Mindfulness-based interventions in context: Past, present, and future. Clin Psychol Sci Pract. 2003;10:144-156. [RCA] [DOI] [Full Text] [Cited by in Crossref: 2119] [Cited by in RCA: 2208] [Article Influence: 100.4] [Reference Citation Analysis (0)] |
| 22. | Kabat-Zinn J. Full catastrophe living: Using the wisdom of your body and mind to face stress, pain, and illness. New York: Delta Books, 1990. |
| 23. | Crane RS, Brewer J, Feldman C, Kabat-Zinn J, Santorelli S, Williams JM, Kuyken W. What defines mindfulness-based programs? Psychol Med. 2017;47:990-999. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 403] [Cited by in RCA: 377] [Article Influence: 47.1] [Reference Citation Analysis (0)] |
| 24. | Baer R, Crane C, Miller E, Kuyken W. Doing no harm in mindfulness-based programs: Conceptual issues and empirical findings. Clin Psychol Rev. 2019;71:101-114. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 146] [Cited by in RCA: 128] [Article Influence: 21.3] [Reference Citation Analysis (0)] |
| 25. | Segal ZV, Williams JMG, Teasdale JD. Mindfulness-based cognitive therapy for depression. 2nd ed. New York: Guilford, 2013. |
| 26. | Ninomiya A, Sado M, Park S, Fujisawa D, Kosugi T, Nakagawa A, Shirahase J, Mimura M. Effectiveness of mindfulness-based cognitive therapy in patients with anxiety disorders in secondary-care settings: A randomized controlled trial. Psychiatry Clin Neurosci. 2020;74:132-139. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 22] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 27. | Boyd JE, Lanius RA, McKinnon MC. Mindfulness-based treatments for posttraumatic stress disorder: a review of the treatment literature and neurobiological evidence. J Psychiatry Neurosci. 2018;43:7-25. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 156] [Cited by in RCA: 183] [Article Influence: 26.1] [Reference Citation Analysis (0)] |
| 28. | Ong JC, Manber R, Segal Z, Xia Y, Shapiro S, Wyatt JK. A randomized controlled trial of mindfulness meditation for chronic insomnia. Sleep. 2014;37:1553-1563. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 184] [Cited by in RCA: 191] [Article Influence: 17.4] [Reference Citation Analysis (0)] |
| 29. | Wahbeh H. Internet Mindfulness Meditation Intervention (IMMI) Improves Depression Symptoms in Older Adults. Medicines (Basel). 2018;5. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 18] [Cited by in RCA: 15] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 30. | Klainin-Yobas P, Kowitlawakul Y, Lopez V, Tang CT, Hoek KE, Gan GL, Lei F, Rawtaer I, Mahendran R. The effects of mindfulness and health education programs on the emotional state and cognitive function of elderly individuals with mild cognitive impairment: A randomized controlled trial. J Clin Neurosci. 2019;68:211-217. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 31] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 31. | Stötter A, Mitsche M, Endler PC, Oleksy P, Kamenschek D, Mosgoeller W, Haring C. Mindfulness-based touch therapy and mindfulness practice in persons with moderate depression. Body Mov Dance Psychother. 2013;8:183-198. [RCA] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 13] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 32. | Ogden P, Minton K, Pain C. Trauma and the body: A sensorimotor approach to psychotherapy. New York: W. W. Norton & Company, 2006. |
| 33. | Fjorback LO, Arendt M, Ornbøl E, Fink P, Walach H. Mindfulness-based stress reduction and mindfulness-based cognitive therapy: a systematic review of randomized controlled trials. Acta Psychiatr Scand. 2011;124:102-119. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 596] [Cited by in RCA: 419] [Article Influence: 29.9] [Reference Citation Analysis (0)] |
| 34. | Querstret D, Morison L, Dickinson S, Cropley M, John M. Mindfulness-based stress reduction and mindfulness-based cognitive therapy for psychological health and well-being in nonclinical samples: A systematic review and meta-analysis. Int J Stress Manag. 2020;27:394-411. [RCA] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 48] [Article Influence: 9.6] [Reference Citation Analysis (1)] |
| 35. | Ong J, Sholtes D. A mindfulness-based approach to the treatment of insomnia. J Clin Psychol. 2010;66:1175-1184. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 64] [Cited by in RCA: 54] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 36. | Chen TL, Chang SC, Hsieh HF, Huang CY, Chuang JH, Wang HH. Effects of mindfulness-based stress reduction on sleep quality and mental health for insomnia patients: A meta-analysis. J Psychosom Res. 2020;135:110144. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 58] [Article Influence: 11.6] [Reference Citation Analysis (0)] |
| 37. | Gong H, Ni CX, Liu YZ, Zhang Y, Su WJ, Lian YJ, Peng W, Jiang CL. Mindfulness meditation for insomnia: A meta-analysis of randomized controlled trials. J Psychosom Res. 2016;89:1-6. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 171] [Cited by in RCA: 131] [Article Influence: 14.6] [Reference Citation Analysis (0)] |
| 38. | Wang YY, Wang F, Zheng W, Zhang L, Ng CH, Ungvari GS, Xiang YT. Mindfulness-Based Interventions for Insomnia: A Meta-Analysis of Randomized Controlled Trials. Behav Sleep Med. 2020;18:1-9. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 47] [Article Influence: 9.4] [Reference Citation Analysis (0)] |
| 39. | Zhang J, Xu R, Wang B, Wang J. Effects of mindfulness-based therapy for patients with breast cancer: A systematic review and meta-analysis. Complement Ther Med. 2016;26:1-10. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 98] [Cited by in RCA: 80] [Article Influence: 8.9] [Reference Citation Analysis (0)] |
| 40. | Howick J, Chalmers I, Glasziou P, Greenhalgh T, Heneghan C, Liberati A, Moschetti I, Phillips B, Thornton H, Goddard O, Hodgkinson M. The Oxford 2011 levels of Evidence: Oxford Centre for Evidence-Based Medicine, 2011. |
| 41. | Higgins JPT, Savović J, Page MJ, Elbers RG, Sterne JAC. Assessing risk of bias in a randomized trial. In: Higgins JPT, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, Welch VA. Cochrane Handbook for Systematic Reviews of Interventions version 60: Cochrane, 2019. |
| 42. | Higgins JPT, Li T, Deeks JJ. Choosing effect measures and computing estimates of effect. In: Higgins JPT, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, Welch VA. Cochrane Handbook for Systematic Reviews of Interventions version 60: Cochrane, 2019. |
| 43. | Lipsey MW, Wilson DB. Practical meta-analysis. Thousand Oaks: Sage Publications, 2009. |
| 44. | Deeks JJ, Higgins JPT, Altman DG. Analysing data and undertaking meta-analyses. In: Higgins JPT, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, Welch VA. Cochrane Handbook for Systematic Reviews of Interventions version 60: Cochrane, 2019. |
| 45. | Horenstein A, Morrison AS, Goldin P, Ten Brink M, Gross JJ, Heimberg RG. Sleep quality and treatment of social anxiety disorder. Anxiety Stress Coping. 2019;32:387-398. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 15] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 46. | Pinniger R, Thorsteinsson EB, Brown RF, Mckinley P. Tango dance can reduce distress and insomnia in people with self-referred affective symptoms. Am J Dance Ther. 2013;35:60-77. [RCA] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 17] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 47. | Wahbeh H, Goodrich E, Goy E, Oken BS. Mechanistic Pathways of Mindfulness Meditation in Combat Veterans With Posttraumatic Stress Disorder. J Clin Psychol. 2016;72:365-383. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 71] [Cited by in RCA: 65] [Article Influence: 7.2] [Reference Citation Analysis (0)] |
| 48. | Britton WB, Haynes PL, Fridel KW, Bootzin RR. Polysomnographic and subjective profiles of sleep continuity before and after mindfulness-based cognitive therapy in partially remitted depression. Psychosom Med. 2010;72:539-548. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 77] [Cited by in RCA: 76] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 49. | Britton WB, Haynes PL, Fridel KW, Bootzin RR. Mindfulness-based cognitive therapy improves polysomnographic and subjective sleep profiles in antidepressant users with sleep complaints. Psychother Psychosom. 2012;81:296-304. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 53] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 50. | Boettcher J, Aström V, Påhlsson D, Schenström O, Andersson G, Carlbring P. Internet-based mindfulness treatment for anxiety disorders: a randomized controlled trial. Behav Ther. 2014;45:241-253. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 151] [Cited by in RCA: 134] [Article Influence: 12.2] [Reference Citation Analysis (0)] |
| 51. | Vøllestad J, Sivertsen B, Nielsen GH. Mindfulness-based stress reduction for patients with anxiety disorders: evaluation in a randomized controlled trial. Behav Res Ther. 2011;49:281-288. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 192] [Cited by in RCA: 162] [Article Influence: 11.6] [Reference Citation Analysis (0)] |
| 52. | Hoge EA, Bui E, Marques L, Metcalf CA, Morris LK, Robinaugh DJ, Worthington JJ, Pollack MH, Simon NM. Randomized controlled trial of mindfulness meditation for generalized anxiety disorder: effects on anxiety and stress reactivity. J Clin Psychiatry. 2013;74:786-792. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 262] [Cited by in RCA: 270] [Article Influence: 22.5] [Reference Citation Analysis (0)] |
| 53. | Libman E, Fichten C, Creti L, Conrod K, Tran DL, Grad R, Jorgensen M, Amsel R, Rizzo D, Baltzan M, Pavilanis A, Bailes S. Refreshing Sleep and Sleep Continuity Determine Perceived Sleep Quality. Sleep Disord. 2016;2016:7170610. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 24] [Cited by in RCA: 30] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 54. | Cohen J. Statistical Power Analysis for the Behavioral Sciences. 2nd ed. Hillsdale: Lawrence Erlbaum Associates Inc., 1988. |
| 55. | Goldstein MR, Turner AD, Dawson SC, Segal ZV, Shapiro SL, Wyatt JK, Manber R, Sholtes D, Ong JC. Increased high-frequency NREM EEG power associated with mindfulness-based interventions for chronic insomnia: Preliminary findings from spectral analysis. J Psychosom Res. 2019;120:12-19. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 20] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 56. | Dunn BD, Stefanovitch I, Evans D, Oliver C, Hawkins A, Dalgleish T. Can you feel the beat? Behav Res Ther. 2010;48:1133-1138. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 182] [Cited by in RCA: 153] [Article Influence: 10.2] [Reference Citation Analysis (0)] |
| 57. | Harshaw C. Interoceptive dysfunction: toward an integrated framework for understanding somatic and affective disturbance in depression. Psychol Bull. 2015;141:311-363. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 181] [Cited by in RCA: 198] [Article Influence: 19.8] [Reference Citation Analysis (0)] |
| 58. | Eggart M, Queri S, Müller-Oerlinghausen B. Are the antidepressive effects of massage therapy mediated by restoration of impaired interoceptive functioning? Med Hypotheses. 2019;128:28-32. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 14] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 59. | Casals-Gutierrez S, Abbey H. Interoception, mindfulness and touch: A meta-review of functional MRI studies. Int J Osteopath Med. 2020;35:22-33. [RCA] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 22] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 60. | Engel-Yeger B, Shochat T. The relationship between sensory processing patterns and sleep quality in healthy adults. Can J Occup Ther. 2012;79:134-141. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 31] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 61. | Harvey AG. Insomnia: symptom or diagnosis? Clin Psychol Rev. 2001;21:1037-1059. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 159] [Cited by in RCA: 165] [Article Influence: 6.9] [Reference Citation Analysis (0)] |
| 62. | Shallcross AJ, Visvanathan PD, Sperber SH, Duberstein ZT. Waking up to the problem of sleep: can mindfulness help? Curr Opin Psychol. 2019;28:37-41. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 39] [Article Influence: 6.5] [Reference Citation Analysis (0)] |
| 63. | Slavish DC, Graham-Engeland JE. Rumination mediates the relationships between depressed mood and both sleep quality and self-reported health in young adults. J Behav Med. 2015;38:204-213. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 50] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 64. | Surova G, Ulke C, Schmidt FM, Hensch T, Sander C, Hegerl U. Fatigue and brain arousal in patients with major depressive disorder. Eur Arch Psychiatry Clin Neurosci. 2021;271:527-536. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 5] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 65. | Ulke C, Sander C, Jawinski P, Mauche N, Huang J, Spada J, Wittekind D, Mergl R, Luck T, Riedel-Heller S, Hensch T, Hegerl U. Sleep disturbances and upregulation of brain arousal during daytime in depressed vs non-depressed elderly subjects. World J Biol Psychiatry. 2017;18:633-640. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 28] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 66. | Lau WKW, Leung MK, Wing YK, Lee TMC. Potential Mechanisms of Mindfulness in Improving Sleep and Distress. Mindfulness (N Y). 2018;9:547-555. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 28] [Cited by in RCA: 38] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 67. | Lindsay EK, Creswell JD. Mechanisms of mindfulness training: Monitor and Acceptance Theory (MAT). Clin Psychol Rev. 2017;51:48-59. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 247] [Cited by in RCA: 343] [Article Influence: 38.1] [Reference Citation Analysis (0)] |
| 68. | Foley E, Baillie A, Huxter M, Price M, Sinclair E. Mindfulness-based cognitive therapy for individuals whose lives have been affected by cancer: a randomized controlled trial. J Consult Clin Psychol. 2010;78:72-79. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 157] [Cited by in RCA: 124] [Article Influence: 8.3] [Reference Citation Analysis (0)] |
| 69. | van Son J, Nyklícek I, Pop VJ, Blonk MC, Erdtsieck RJ, Spooren PF, Toorians AW, Pouwer F. The effects of a mindfulness-based intervention on emotional distress, quality of life, and HbA(1c) in outpatients with diabetes (DiaMind): a randomized controlled trial. Diabetes Care. 2013;36:823-830. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 109] [Cited by in RCA: 106] [Article Influence: 8.8] [Reference Citation Analysis (0)] |
| 70. | Reangsing C, Rittiwong T, Schneider JK. Effects of mindfulness meditation interventions on depression in older adults: A meta-analysis. Aging Ment Health. 2021;25:1181-1190. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 48] [Article Influence: 12.0] [Reference Citation Analysis (0)] |
| 71. | Ren Z, Zhang Y, Jiang G. Effectiveness of mindfulness meditation in intervention for anxiety: A meta-analysis. Acta Psychologica Sinica. 2018;50:283-305. [RCA] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 18] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 72. | Chan SHW, Chan WWK, Chao JYW, Chan PKL. A randomized controlled trial on the comparative effectiveness of mindfulness-based cognitive therapy and health qigong-based cognitive therapy among Chinese people with depression and anxiety disorders. BMC Psychiatry. 2020;20:590. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 13] [Cited by in RCA: 6] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 73. | Smith JH, Baumert M, Nalivaiko E, McEvoy RD, Catcheside PG. Arousal in obstructive sleep apnoea patients is associated with ECG RR and QT interval shortening and PR interval lengthening. J Sleep Res. 2009;18:188-195. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 21] [Article Influence: 1.3] [Reference Citation Analysis (0)] |