Published online Feb 19, 2022. doi: 10.5498/wjp.v12.i2.338
Peer-review started: July 6, 2021
First decision: September 5, 2021
Revised: September 18, 2021
Accepted: January 14, 2022
Article in press: January 14, 2022
Published online: February 19, 2022
Processing time: 225 Days and 17.2 Hours
Frontline nurses in Wuhan directly fighting severe acute respiratory syndrome coronavirus-2 diseases are at a high risk of infection and are extremely susceptible to psychological stress, especially due to the global coronavirus disease 2019 (COVID-19) pandemic. The psychological after-effects of this public health emergency on frontline nurses will last for years.
To assess factors influencing post-traumatic stress disorder (PTSD) among frontline nurses in Wuhan 6 mo after the COVID-19 pandemic began.
A total of 757 frontline nurses from five hospitals in Wuhan, China, participated in an online survey from July 27 to August 13, 2020. This cross-sectional online study used a demographic information questionnaire, the PTSD Checklist for the Diagnostic and Statistical Manual of Mental Disorders, the Connor-Davidson Resilience Scale, and the Patient Health Questionnaire-4. The chi-square test and logistic regression were used to analyze the association of demographics, COVID-19-related variables, and PTSD. Logistic regression was also conducted to investigate which variables were associated with PTSD outcomes.
A total of 13.5%, 24.3%, and 21.4% of the frontline nurses showed symptoms of PTSD, depression, and anxiety, respectively. The multivariate logistic regression analysis showed that the following factors were strongly associated with PTSD: Having a relative, friend, or colleague who died of COVID-19; experiencing stigma; or having psychological assistance needs, depressive symptoms or anxiety. Showing resilience and receiving praise after the COVID-19 outbreak were protective factors.
Frontline nurses still experienced PTSD (13.5%) six months after the COVID-19 outbreak began. Peer support, social support, official recognition, reward mechanisms, exercise, better sleep, and timely provision of information (such as vaccine research progress) by the government via social media, and adequate protective supplies could mitigate the level of PTSD among nurses responding to COVID-19. Stigmatization, depression, and anxiety might be associated with a greater risk of PTSD among nurses.
Core Tip: The mental health of frontline nurses in Wuhan has been significantly affected by the coronavirus disease (COVID-19). This study aims to evaluate the influencing factors of post-traumatic stress disorder (PTSD) among frontline nurses in Wuhan six months after the COVID-19 pandemic began and implement a mental health plan. The prevalence rates of PTSD, depression and anxiety among frontline nurses were 13.5%, 24.3%, and 21.4%, respectively. The risk factors for nurses to develop PTSD are the death of a relative, friend, or colleague from COVID-19, stigma, depression, and anxiety. Resilience and reward mechanisms are protective factors to prevent PTSD.
- Citation: Zhou ZQ, Yuan T, Tao XB, Huang L, Zhan YX, Gui LL, Li M, Liu H, Li XD. Cross-sectional study of traumatic stress disorder in frontline nurses 6 mo after the outbreak of the COVID-19 in Wuhan. World J Psychiatry 2022; 12(2): 338-347
- URL: https://www.wjgnet.com/2220-3206/full/v12/i2/338.htm
- DOI: https://dx.doi.org/10.5498/wjp.v12.i2.338
A novel coronavirus disease (COVID-19) was first reported in December 2019 in Wuhan, China. The World Health Organization (WHO) Director-General announced that the COVID-19 outbreak was a public health emergency of international concern on 30 January 2020[1]. As of 14 August 2020, 20439814 confirmed cases and 744385 confirmed deaths had been reported by the WHO, and the disease eventually spread to more than 216 countries, areas, or territories[2]. Increasing demand for the care of COVID-19 patients and high morbidity and mortality continue to challenge the global health system.
Wuhan was considered a high-risk area for COVID-19. According to the daily report on COVID-19 statistics released by the National Health Commission of China, as of 24:00 on February 24, 2020, Wuhan had a total of 47071 confirmed cases and a total of 2043 deaths[3]. To efficiently stop the spread of COVID-19, medical staff fought the disease. However, there were a total of 3387 cases of COVID-19 infection among medical staff in mainland China. More than 90% of medical staff infections occurred in Hubei Province, mainly in Wuhan[4]. While rescuing lives, frontline medical staff witnessed the clinical reactions and deaths of numerous patients with severe cases of COVID-19.
An overwhelming workload, shortage of medical supplies, insufficient rest, high risk of infection, stigma, and fear of infection of family members or friends increase the risk of post-traumatic stress disorder (PTSD) among frontline nurses. PTSD[5,6] is a mental disorder characterized by intrusive thoughts, avoidance, cognitive and mood disturbances, and arousal symptoms that may be experienced after traumatic life events, such as threats of severe injury, death, war, sexual offenses, and terrible catastrophes.
Due to the COVID-19 pandemic, frontline nurses were considered susceptible to PTSD. Studies on the COVID-19 outbreak in China[7], Spain[8], Italy[9], Jordan[10], and the United States[11] have discussed how the battle against COVID-19 caused anxiety, depression, and PTSD symptoms among frontline nurses.
Studies on the impact of severe acute respiratory syndrome (SARS)[12], Middle East respiratory syndrome[13], and influenza A[14] found that one to two years after a disease outbreak, frontline nurses endured symptoms of anxiety, depression, and PTSD. However, there is little information available on the long-term impact of PTSD on frontline nurses who treated SARS patients during the COVID-19 outbreak.
This study aims to investigate the influencing factors of PTSD six months after the COVID-19 outbreak among frontline nurses who were exposed to COVID-19. It is imperative to provide mental health support for frontline nurses, and facilitate their psychological recovery from PTSD related to the COVID-19 pandemic.
The study was reviewed and approved by the Ethics Committee of the Union Hospital affiliated to Tongji Medical College, Huazhong University of Science and Technology (Approval number 2020-0189). This study was conducted according to the principles of the Declaration of Helsinki.
The research team assessed the traumatic stress disorder of frontline nurses who worked in Wuhan during the outbreak through a cross-sectional survey using social media (such as WeChat and QQ) six months after the outbreak, from July 27 to August 13, 2020. Before starting the investigation, all participants had to give their informed consent, and the purpose of the study was explained. The participants could exit the survey at any time.
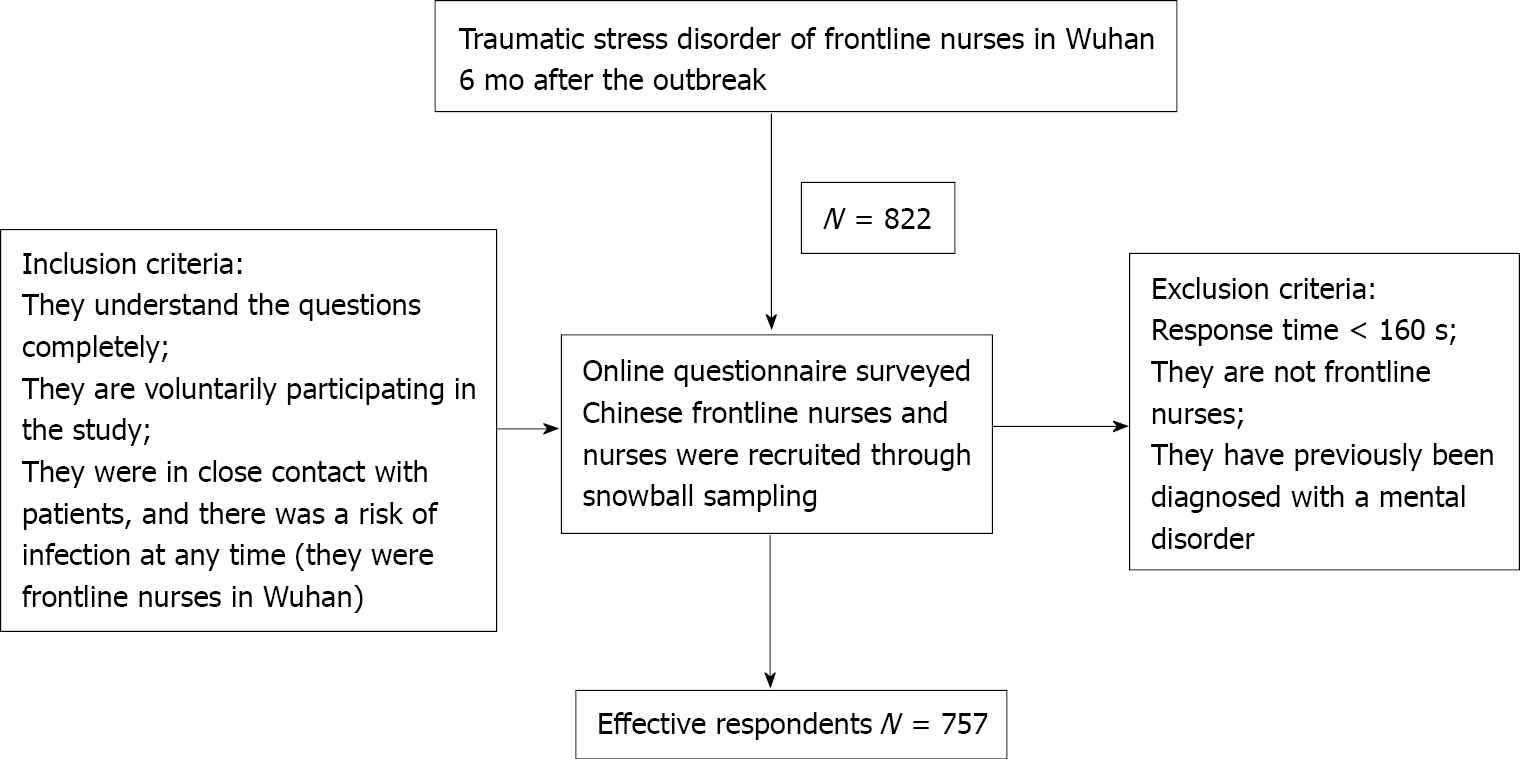
The study recruited 822 first-line medical staff from six tertiary general hospitals. After those who met the exclusion criteria were removed, 92.1% (757 out of 822) of the staff were included in the statistical analyses. A total of 274 participants (36.2%) were from Zhongnan Hospital of Wuhan University, 149 (19.7%) were from Tongji Hospital, Tongji Medical College, Huazhong University of Science and Technology, 39 (5.2%) were from Wuhan Central Hospital, 150 (19.8%) were from Wuhan Jin Yin Tan Hospital (Wuhan Medical Treatment Center), 104 (13.7%) were from Wuhan Third Hospital, and 41 (5.4%) were from Renmin Hospital of Wuhan University. The participants worked in Wuhan during the height of the pandemic from January to February 2020. The inclusion and exclusion criteria are presented in Figure 1. The demographics of the study participants are presented in Table 1.
| Variables | Characteristics | Total n (%) | PTSD n (%) | χ2 | P value | |
| No | Yes | |||||
| Sex | Male | 69 (9.1) | 64 (8.5) | 5 (0.7) | 2.526 | 0.112 |
| Female | 688 (90.9) | 591 (78.1) | 97 (12.8) | |||
| Age | < 25 | 132 (17.4) | 116 (15.3) | 16 (2.1) | 3.859 | 0.452 |
| 26-30 | 232 (30.6) | 205 (27.1) | 27 (3.6) | |||
| 31-35 | 183 (24.2) | 156 (20.6) | 27 (3.6) | |||
| 36-40 | 88 (11.6) | 71 (9.4) | 17 (2.2) | |||
| > 40 | 122 (16.1) | 107 (14.1) | 15 (2.0) | |||
| Marital status | Married | 492 (65.0) | 422 (55.7) | 70 (9.2) | 0.684 | 0.408 |
| Single/Divorced/Other | 265 (35.0) | 233 (30.8) | 32 (42.2) | |||
| Education | Secondary education | 98 (12.9) | 82 (10.8) | 16 (2.1) | 0.842 | 0.656 |
| Bachelor’s degree | 585 (77.3) | 508 (67.1) | 77 (10.2) | |||
| Postgraduate/Doctoral degree | 74 (9.8) | 65 (8.6) | 9 (1.2) | |||
| Working years | 0-2 | 114 (15.1) | 101 (13.3) | 13 (1.7) | 1.289 | 0.863 |
| 3-5 | 148 (19.6) | 128 (16.9) | 20 (2.6) | |||
| 6-10 | 219 (28.9) | 191 (25.2) | 28 (3.7) | |||
| 11-20 | 178 (23.5) | 150 (19.8) | 28 (3.7) | |||
| ≥ 20 | 98 (12.9) | 85 (11.2) | 13 (1.7) | |||
| Previous anti-epidemic experience | No | 694 (97.1) | 600 (79.3) | 94 (12.4) | 0.035 | 0.851 |
| Yes | 63 (8.3) | 55 (7.3) | 8 (1.1) | |||
| Nurse infected by COVID-19 | No | 732 | 634 | 98 | 0.141 | 0.707 |
| Yes | 25 | 21 | 4 | |||
| A relative, friend or colleague died of COVID-19 | No | 611 (80.7) | 542 (71.6) | 69 (9.1) | 12.929 | 0.000b |
| Yes | 146 (19.3) | 113 (14.9) | 33 (4.4) | |||
| Experienced stigma | No | 596 (78.7) | 536 (70.8) | 60 (7.9) | 27.902 | 0.000b |
| Yes | 161 (21.3) | 119 (15.7) | 42 (5.5) | |||
| Received praise | No | 504 (66.6) | 425 (56.1) | 79 (10.4) | 6.262 | 0.012a |
| Yes | 253 (33.4) | 230 (30.4) | 23 (3.0) | |||
| Resilience (CD-RISC-10) | < 30 | 540 (71.3) | 442 (58.4) | 98 (12.9) | 35.297 | 0.000b |
| ≥ 30 | 217 (28.7) | 213 (28.1) | 4 (0.5) | |||
| Depression (PHQ-2) | < 3 | 573 (75.7) | 541 (71.5) | 32 (4.2) | 125.861 | 0.000b |
| ≥ 3 | 184 (24.3) | 114 (15.1) | 70 (9.2) | |||
| Anxiety (GAD-2) | < 3 | 595 (78.6) | 558 (73.7) | 37 (4.9) | 125.549 | 0.000b |
| ≥ 3 | 162 (21.4) | 97 (12.8) | 65 (8.6) | |||
This questionnaire collected information on the participants’ general characteristics, including age, sex, and job-related information, and COVID-related information.
The PTSD Checklist for the Diagnostic and Statistical Manual of Mental Disorders[15] was used to measure the post-traumatic stress disorder of frontline nurses in Wuhan six months after the outbreak. This scale has been widely and commonly used in previous studies[16]. The scale consists of 20 items scored on a Likert-type scale ranging from 0 = “not at all” to 4 = “extremely”. The total scores range from 0 to 80, with higher scores indicating more severe symptoms (cutoff score ≥ 33). These statements are classified into four distinct domains: Re-experiencing (5 items, score 0 to 20); avoidance (2 items, score 0 to 8); negative alteration in cognition and mood (6 items, score 0 to 24) and arousal (7 items, 0 to 28).
The psychometric properties of the Connor-Davidson Resilience Scale (CD-RISC 10) are well documented. The CD-RISC 10[17], in its Chinese version[18], was used to assess psychological resilience, especially the ability to cope with adversity. The 10 self-report items are scored on a Likert-type scale from 0 = “not true at all” to 4 = “true nearly all the time”. The total score ranges from 0 to 40, and higher scores indicate better resilience (cutoff score ≥ 30).
The Patient Health Questionnaire-4 (PHQ-4)[19], including the PHQ-2 and Generalized Anxiety Disorder-2 (GAD-2), were used to assess both depression and anxiety disorders, respectively. The Chinese versions[20] have been validated and widely used. The PHQ-2 and GAD-2 use two core criteria to assess the levels of major depressive disorder and anxiety, respectively. Each item is scored on a 4-point Likert-type scale from 0 = “not at all” to 3 = “nearly every day”. The total score ranges from 0 to 6, and higher scores indicate greater levels of depression and anxiety (cutoff score ≥ 3).
Data were analyzed using IBM SPSS version 21.0 (Chicago, IL, United States). Frequencies and percentages were calculated for the categorical data. The chi-square test was used to verify differences in the categorical variables between groups. Binary logistic regression analyses were used to explore the factors impacting post-traumatic stress, such as demographics, anxiety, depression, and resilience. The test level was P = 0.05; that is, a P-value of less than 0.05 was considered statistically significant.
A total of 757 participants were included in this investigation. The mean age was 32.60 years (SD = 7.64). The mean working time was 10.16 years (SD = 8.28). The study sample consisted of 688 women (86.4%) and 69 men (13.6%). The demographics of the participants are presented in Table 1.
The mean PTSD, resilience, depression, and anxiety scores were 17.74 ± 11.87, 25.29 ± 6.95, 1.75 ± 1.43, and 1.70 ± 1.43, respectively. A total of 13.5% of the sample met the symptom criteria for PTSD. The prevalence of depression was 24.3%, and 21.4% of the participants had anxiety symptoms. The proportion of frontline nurses in Wuhan enrolled in this survey who scored above the established cutoff for resilience was 28.7%.
Six items found significant differences between nurses with post-traumatic stress disorder, including having a relative, friend, or colleague who died of COVID-19, experiencing stigma, receiving praise, showing resilience, having depression symptoms, and having anxiety symptoms. No differences were observed between groups in sex, age, education, marital status, working years, or previous anti-epidemic experience (all P < 0.05) (Table 1).
Six items were significantly associated with PTSD among nurses, including having a relative, friend, or colleague who died of COVID-19, experiencing stigma, receiving praise, showing resilience, having depression symptoms, and having anxiety symptoms (P < 0.05). No differences were observed between groups in gender, age, marital status, education, working years, or previous anti-epidemic experience (P > 0.05) (Table 1).
As shown in Table 2, several variables were found to be associated with a higher risk of PTSD, such as having a relative, friend, or colleague who died of COVID-19 [odds ratio (OR): 2.226, P < 0.01], experiencing stigma (OR: 3.038, P < 0.01), not receiving praise (OR: 0.442, P < 0.01), lacking resilience (OR: 0.190, P < 0.01), having depressive symptoms (OR: 3.625, P < 0.01), and having anxiety symptoms (OR: 3.849, P < 0.01).
| B | SE | Wald | Sig | Exp (B) | 95% Confidence interval | ||
| Lower bound | Upper bound | ||||||
| A relative, friend or colleague died of COVID-19 (No) | 0.800 | 0.283 | 7.969 | 0.005 | 2.226 | 1.277 | 3.879 |
| Experienced stigma (No) | 1.111 | 0.270 | 16.974 | 0.000 | 3.038 | 1.791 | 5.154 |
| Received praised (No) | -0.816 | 0.288 | 8.042 | 0.005 | 0.442 | 0.252 | 0.777 |
| Resilience < 30 | -1.662 | 0.540 | 9.475 | 0.002 | 0.190 | 0.066 | 0.547 |
| Depression < 3 | 1.288 | 0.322 | 15.962 | 0.000 | 3.625 | 1.927 | 6.818 |
| Anxiety < 3 | 1.348 | 0.321 | 17.678 | 0.000 | 3.849 | 2.053 | 7.214 |
| Constant | -5.010 | 0.999 | 25.134 | 0.000 | 0.007 | ||
This study found that six months after the COVID-19 outbreak began in Wuhan, China, the prevalence of PTSD, depression, and anxiety among frontline nurses were 13.5%, 24.3%, and 21.4%, respectively. The following factors were associated with a greater likelihood of having PTSD: Having a relative, friend, or colleague who died of COVID-19; experiencing stigma; having depression symptoms; and having anxiety symptoms. Showing resilience and receiving praise after the COVID-19 outbreak were helpful in prevent PTSD.
The incidence of PTSD among frontline nurses was lower at the time of the survey than at the initial stage of the COVID-19 outbreak (16.83%-71.5%)[21-25]. A possible reason might be that the nurses may have been under less psychological stress six months after the outbreak than they were during the initial period, which was also found in Cai et al[7]’s research.
It is important to note that the participants who had a relative, friend, or colleague who died of COVID-19 were more likely to report high levels of PTSD. In contrast, no differences in the history of personal infection were observed between those who did not have PTSD. This study highlights that exposure to high-risk work environments (such as directly caring for infected patients) was not the main determinant of adverse psychological outcomes. This result was also found 13 to 26 mo after the SARS outbreak[26] among medical staff at Toronto hospitals that treated SARS patients. A previous study showed[27] that during the SARS outbreak, the death of colleagues created a stressful atmosphere in the hospital. It is also possible that the death of a relative, friend, or colleague places a heavy psychological burden on nurses[28]. These trends may be explained by peer support promoting adaptive coping.
Stigmatization was found to be predictive of a high level of PTSD. Frontline nurses at hospitals are vulnerable to stigmatization, loneliness, and exclusion due to working in areas with the highest incidence of COVID-19. COVID-19-related fear may have led the nurses to be isolated from other individuals, which may also have had different effects on their social support. Experience of stigma can have long-term adverse effects on nurses’ mental health. Such effects were examined by Liu et al[29], Zandifar et al[30], and Röhr et al[31].
The logistic regression analysis showed that the nurses who had received praise from government agencies were less likely to report high levels of PTSD. Frontline nurses who are officially recognized, which is common in Chinese society, have a strong sense of being protected and supported by organizations. Such recognition may play an important role in experiencing satisfaction through continued working in these settings. Previous studies[32,33] reported that people with severe PTSD symptoms performed better than those without PTSD symptoms in reward trials. In response to the ongoing psychological effects among nurses after the COVID-19 outbreak, official recognition and reward mechanisms appear to be needed.
Psychological resilience was a significant protective factor for PTSD among the frontline nurses six months after the COVID-19 outbreak. Lutha and Cicchetti[34] refers to an individual’s ability to positively adjust after trauma and respond to adverse experiences. Psychological resilience research[35] during the COVID-19 epidemic showed that more frequent exposure to the outdoors and sunlight, more exercise, greater perceived social support, better sleep, and more frequent prayer may contribute to greater psychological resilience.
One study[36] conducted in China during the COVID-19 outbreak showed that increased distress, decreased sleep quality and increased self-efficacy could cause anxiety among medical staff, which could affect their mental health. Making difficult ethical decisions regarding the distribution of medical supplies, the lack of personal equipment, and progress in COVID-19 vaccine research made medical staff particularly vulnerable to mental health problems. Therefore, reasonable rest time and shifts, a safe work environment, the satisfaction of basic needs, and the availability of information on vaccine research progress may help reduce stress among nurses. Previous studies[37-39] also found that anxiety could lead to PTSD, exacerbated by the effects of a higher frequency of social media exposure. Notably, having up-to-date authoritative and true information about COVID-19 on social media may reduce the rate of PTSD.
Several limitations of this survey must be mentioned. First, since the COVID-19 pandemic has had a long-term negative psychological impact on nurses, longitudinal research should be conducted in the future. Second, the research may have been biased because the participants were not recruited randomly. Third, due to the endpoint of the study, the challenges and opportunities of vaccination remain unknown.
Six months after the COVID-19 outbreak began, frontline nurses were still experiencing pandemic-related distress, which could lead to long-term PTSD. Our findings indicated that peer support, social support, exercise, better sleep, official recognition, and reward mechanisms should be prioritized to alleviate the negative psychological responses of nurses dealing with the pandemic. Our study further shows that the timely provision of information (such as vaccine research progress) by the government on social media and adequate protective supplies might mitigate the level of PTSD among nurses responding to COVID-19. Stigmatization, depression, and anxiety might be associated with a greater risk of PTSD among nurses.
The worldwide spread of coronavirus disease 2019 (COVID-19) is an international public health emergency posing challenges for health care systems. The mental health of nurses was significantly affected by this crisis, and nurses played a crucial role in successfully fighting the COVID-19 pandemic.
Few studies have focused on the risk of post-traumatic stress disorder (PTSD) among frontline nurses six months after the COVID-19 outbreak. Our research group aimed to investigate the prevalence of PTSD among nurses and the implementation of mental health programs.
This study aimed to evaluate the factors associated with PTSD, determine what psychosocial support nurses need, and identify ways to reduce the level of PTSD among nurses responding to the COVID-19 pandemic in Wuhan, China.
A total of 757 frontline nurses from six tertiary general hospitals in Wuhan, China, were recruited. The structured questionnaire included a demographic information section, the PTSD Checklist for Diagnostic and Statistical Manual of Mental Disorders, the Connor-Davidson Resilience Scale, the Patient Health Questionnaire-4, and COVID-19-related items. The cross-sectional survey was conducted from July 27 to August 13, 2020, via social media.
This study found that six months after the COVID-19 outbreak in Wuhan, China, the prevalence of PTSD, depression, and anxiety among frontline nurses was 13.5%, 24.3%, and 21.4%, respectively. The following factors were associated with a greater likelihood of having PTSD: Having a relative, friend, or colleague who died of COVID-19; experiencing stigma; having depressive symptoms, and having anxiety symptoms. Showing resilience and receiving praise after the COVID-19 outbreak were helpful in preventing PTSD.
Frontline nurses still experienced long-term pandemic-related distress six months after the COVID-19 outbreak. Peer support, social support, official recognition, reward mechanisms, better sleep, exercise, and the timely provision of information (such as vaccine research progress) by the government on social media, and adequate protective supplies could mitigate the level of PTSD among nurses responding to COVID-19. Stigmatization, depression, and anxiety might be associated with a greater risk of PTSD among nurses.
Considering the long-term adverse effects of PTSD on frontline nurses, longitudinal studies should be conducted in the future. Additional research is needed to better understand whether the vaccine could mitigate the negative impact on the mental health of nurses and other populations.
The authors would like to thank all the participants for their cooperation.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Psychiatry
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Mitra AK S-Editor: Wang JJ L-Editor: A P-Editor: WangJJ
| 1. | World Health Organization. Listings of WHO’s response to COVID-19. [cited 6 June 2021]. Available from: https://www.who.int/news/item/29-06-2020-covidtimeline. |
| 2. | World Health Organization. Weekly operational update on COVID-19. [cited 6 June 2021]. Available from: https://www.who.int/docs/default-source/coronaviruse/situation-reports/wou-28-august-approved.pdf?sfvrsn=d9e49c20_2. |
| 3. | National Health Commission of the People’s Republic of China. The latest situation of the novel coronavirus pneumonia epidemic. [cited 6 June 2021]. Available from: http://www.nhc.gov.cn/xcs/yqtb/202003/9d462194284840ad96ce75eb8e4c8039.shtml. |
| 4. | Cao GW, Zhang BX, Chen XP. [Consideration on improving public health emergency management ability of current medical health system]. Zhonghua Liu Xing Bing Xue Za Zhi. 2020;41:1588-1594. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
| 5. | American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5). Arlington: American Psychiatric Publishing, 2013. |
| 6. | Bisson JI, Cosgrove S, Lewis C, Robert NP. Post-traumatic stress disorder. BMJ. 2015;351:h6161. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 147] [Cited by in RCA: 149] [Article Influence: 14.9] [Reference Citation Analysis (0)] |
| 7. | Cai Z, Cui Q, Liu Z, Li J, Gong X, Liu J, Wan Z, Yuan X, Li X, Chen C, Wang G. Nurses endured high risks of psychological problems under the epidemic of COVID-19 in a longitudinal study in Wuhan China. J Psychiatr Res. 2020;131:132-137. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 118] [Cited by in RCA: 112] [Article Influence: 22.4] [Reference Citation Analysis (0)] |
| 8. | Alonso J, Vilagut G, Mortier P, Ferrer M, Alayo I, Aragón-Peña A, Aragonès E, Campos M, Cura-González ID, Emparanza JI, Espuga M, Forjaz MJ, González-Pinto A, Haro JM, López-Fresneña N, Salázar ADM, Molina JD, Ortí-Lucas RM, Parellada M, Pelayo-Terán JM, Pérez-Zapata A, Pijoan JI, Plana N, Puig MT, Rius C, Rodríguez-Blázquez C, Sanz F, Serra C, Kessler RC, Bruffaerts R, Vieta E, Pérez-Solà V; MINDCOVID Working group. Mental health impact of the first wave of COVID-19 pandemic on Spanish healthcare workers: A large cross-sectional survey. Rev Psiquiatr Salud Ment (Engl Ed). 2021;14:90-105. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 67] [Cited by in RCA: 123] [Article Influence: 24.6] [Reference Citation Analysis (0)] |
| 9. | Rossi R, Socci V, Pacitti F, Mensi S, Di Marco A, Siracusano A, Di Lorenzo G. Mental Health Outcomes Among Healthcare Workers and the General Population During the COVID-19 in Italy. Front Psychol. 2020;11:608986. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 68] [Cited by in RCA: 62] [Article Influence: 12.4] [Reference Citation Analysis (0)] |
| 10. | Shahrour G, Dardas LA. Acute stress disorder, coping self-efficacy and subsequent psychological distress among nurses amid COVID-19. J Nurs Manag. 2020;28:1686-1695. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 87] [Cited by in RCA: 152] [Article Influence: 30.4] [Reference Citation Analysis (0)] |
| 11. | Sagherian K, Steege LM, Cobb SJ, Cho H. Insomnia, fatigue and psychosocial well-being during COVID-19 pandemic: A cross-sectional survey of hospital nursing staff in the United States. J Clin Nurs. 2020;. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 63] [Cited by in RCA: 132] [Article Influence: 26.4] [Reference Citation Analysis (0)] |
| 12. | Lancee WJ, Maunder RG, Goldbloom DS; Coauthors for the Impact of SARS Study. Prevalence of psychiatric disorders among Toronto hospital workers one to two years after the SARS outbreak. Psychiatr Serv. 2008;59:91-95. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 265] [Cited by in RCA: 252] [Article Influence: 14.8] [Reference Citation Analysis (0)] |
| 13. | Oh MD, Park WB, Park SW, Choe PG, Bang JH, Song KH, Kim ES, Kim HB, Kim NJ. Middle East respiratory syndrome: what we learned from the 2015 outbreak in the Republic of Korea. Korean J Intern Med. 2018;33:233-246. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 158] [Cited by in RCA: 146] [Article Influence: 20.9] [Reference Citation Analysis (0)] |
| 14. | Tang L, Pan L, Yuan L, Zha L. Prevalence and related factors of post-traumatic stress disorder among medical staff members exposed to H7N9 patients. Int J Nurs Sci. 2017;4:63-67. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 52] [Cited by in RCA: 64] [Article Influence: 7.1] [Reference Citation Analysis (0)] |
| 15. | Blevins CA, Weathers FW, Davis MT, Witte TK, Domino JL. The Posttraumatic Stress Disorder Checklist for DSM-5 (PCL-5): Development and Initial Psychometric Evaluation. J Trauma Stress. 2015;28:489-498. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2127] [Cited by in RCA: 3069] [Article Influence: 306.9] [Reference Citation Analysis (0)] |
| 16. | Liu N, Zhang F, Wei C, Jia Y, Shang Z, Sun L, Wu L, Sun Z, Zhou Y, Wang Y, Liu W. Prevalence and predictors of PTSS during COVID-19 outbreak in China hardest-hit areas: Gender differences matter. Psychiatry Res. 2020;287:112921. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1017] [Cited by in RCA: 878] [Article Influence: 175.6] [Reference Citation Analysis (0)] |
| 17. | Connor KM, Davidson JR. Development of a new resilience scale: the Connor-Davidson Resilience Scale (CD-RISC). Depress Anxiety. 2003;18:76-82. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4591] [Cited by in RCA: 5195] [Article Influence: 247.4] [Reference Citation Analysis (0)] |
| 18. | Meng M, He J, Guan Y, Zhao H, Yi J, Yao S, Li L. Factorial Invariance of the 10-Item Connor-Davidson Resilience Scale Across Gender Among Chinese Elders. Front Psychol. 2019;10:1237. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 28] [Cited by in RCA: 33] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 19. | Löwe B, Wahl I, Rose M, Spitzer C, Glaesmer H, Wingenfeld K, Schneider A, Brähler E. A 4-item measure of depression and anxiety: validation and standardization of the Patient Health Questionnaire-4 (PHQ-4) in the general population. J Affect Disord. 2010;122:86-95. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1176] [Cited by in RCA: 1582] [Article Influence: 105.5] [Reference Citation Analysis (0)] |
| 20. | Zhang WR, Wang K, Yin L, Zhao WF, Xue Q, Peng M, Min BQ, Tian Q, Leng HX, Du JL, Chang H, Yang Y, Li W, Shangguan FF, Yan TY, Dong HQ, Han Y, Wang YP, Cosci F, Wang HX. Mental Health and Psychosocial Problems of Medical Health Workers during the COVID-19 Epidemic in China. Psychother Psychosom. 2020;89:242-250. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 801] [Cited by in RCA: 879] [Article Influence: 175.8] [Reference Citation Analysis (0)] |
| 21. | Caillet A, Coste C, Sanchez R, Allaouchiche B. Psychological Impact of COVID-19 on ICU Caregivers. Anaesth Crit Care Pain Med. 2020;39:717-722. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 46] [Cited by in RCA: 69] [Article Influence: 13.8] [Reference Citation Analysis (0)] |
| 22. | Dobson H, Malpas CB, Burrell AJ, Gurvich C, Chen L, Kulkarni J, Winton-Brown T. Burnout and psychological distress amongst Australian healthcare workers during the COVID-19 pandemic. Australas Psychiatry. 2021;29:26-30. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 138] [Cited by in RCA: 130] [Article Influence: 32.5] [Reference Citation Analysis (0)] |
| 23. | Wang YX, Guo HT, Du XW, Song W, Lu C, Hao WN. Factors associated with post-traumatic stress disorder of nurses exposed to corona virus disease 2019 in China. Medicine (Baltimore). 2020;99:e20965. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 65] [Cited by in RCA: 70] [Article Influence: 14.0] [Reference Citation Analysis (0)] |
| 24. | Si MY, Su XY, Jiang Y, Wang WJ, Gu XF, Ma L, Li J, Zhang SK, Ren ZF, Ren R, Liu YL, Qiao YL. Psychological impact of COVID-19 on medical care workers in China. Infect Dis Poverty. 2020;9:113. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 93] [Cited by in RCA: 123] [Article Influence: 24.6] [Reference Citation Analysis (0)] |
| 25. | Lai J, Ma S, Wang Y, Cai Z, Hu J, Wei N, Wu J, Du H, Chen T, Li R, Tan H, Kang L, Yao L, Huang M, Wang H, Wang G, Liu Z, Hu S. Factors Associated With Mental Health Outcomes Among Health Care Workers Exposed to Coronavirus Disease 2019. JAMA Netw Open. 2020;3:e203976. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5313] [Cited by in RCA: 4375] [Article Influence: 875.0] [Reference Citation Analysis (0)] |
| 26. | Maunder RG, Lancee WJ, Balderson KE, Bennett JP, Borgundvaag B, Evans S, Fernandes CM, Goldbloom DS, Gupta M, Hunter JJ, McGillis Hall L, Nagle LM, Pain C, Peczeniuk SS, Raymond G, Read N, Rourke SB, Steinberg RJ, Stewart TE, VanDeVelde-Coke S, Veldhorst GG, Wasylenki DA. Long-term psychological and occupational effects of providing hospital healthcare during SARS outbreak. Emerg Infect Dis. 2006;12:1924-1932. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 863] [Cited by in RCA: 737] [Article Influence: 38.8] [Reference Citation Analysis (0)] |
| 27. | Phua DH, Tang HK, Tham KY. Coping responses of emergency physicians and nurses to the 2003 severe acute respiratory syndrome outbreak. Acad Emerg Med. 2005;12:322-328. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 106] [Cited by in RCA: 120] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 28. | Styra R, Hawryluck L, Robinson S, Kasapinovic S, Fones C, Gold WL. Impact on health care workers employed in high-risk areas during the Toronto SARS outbreak. J Psychosom Res. 2008;64:177-183. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 184] [Cited by in RCA: 180] [Article Influence: 10.6] [Reference Citation Analysis (0)] |
| 29. | Liu X, Kakade M, Fuller CJ, Fan B, Fang Y, Kong J, Guan Z, Wu P. Depression after exposure to stressful events: lessons learned from the severe acute respiratory syndrome epidemic. Compr Psychiatry. 2012;53:15-23. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 630] [Cited by in RCA: 511] [Article Influence: 39.3] [Reference Citation Analysis (0)] |
| 30. | Zandifar A, Badrfam R, Mohammadian Khonsari N, Mohammadi MR, Asayesh H, Qorbani M. Prevalence and Associated Factors of Posttraumatic Stress Symptoms and Stigma among Health Care Workers in Contact with COVID-19 Patients. Iran J Psychiatry. 2020;15:340-350. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 24] [Cited by in RCA: 34] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 31. | Röhr S, Müller F, Jung F, Apfelbacher C, Seidler A, Riedel-Heller SG. [Psychosocial Impact of Quarantine Measures During Serious Coronavirus Outbreaks: A Rapid Review]. Psychiatr Prax. 2020;47:179-189. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 105] [Cited by in RCA: 130] [Article Influence: 26.0] [Reference Citation Analysis (0)] |
| 32. | Myers CE, Moustafa AA, Sheynin J, Vanmeenen KM, Gilbertson MW, Orr SP, Beck KD, Pang KC, Servatius RJ. Learning to obtain reward, but not avoid punishment, is affected by presence of PTSD symptoms in male veterans: empirical data and computational model. PLoS One. 2013;8:e72508. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 35] [Cited by in RCA: 43] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 33. | Boukezzi S, Baunez C, Rousseau PF, Warrot D, Silva C, Guyon V, Zendjidjian X, Nicolas F, Guedj E, Nazarian B, Trousselard M, Chaminade T, Khalfa S. Posttraumatic Stress Disorder is associated with altered reward mechanisms during the anticipation and the outcome of monetary incentive cues. Neuroimage Clin. 2020;25:102073. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 16] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 34. | Lutha SS, Cicchetti D. The construct of resilience: implications for interventions and social policies. Dev Psychopathol. 2000;12:857-885. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1220] [Cited by in RCA: 789] [Article Influence: 31.6] [Reference Citation Analysis (0)] |
| 35. | Killgore WDS, Taylor EC, Cloonan SA, Dailey NS. Psychological resilience during the COVID-19 Lockdown. Psychiatry Res. 2020;291:113216. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 387] [Cited by in RCA: 334] [Article Influence: 66.8] [Reference Citation Analysis (0)] |
| 36. | Xiao H, Zhang Y, Kong D, Li S, Yang N. The Effects of Social Support on Sleep Quality of Medical Staff Treating Patients with Coronavirus Disease 2019 (COVID-19) in January and February 2020 in China. Med Sci Monit. 2020;26:e923549. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 277] [Cited by in RCA: 635] [Article Influence: 127.0] [Reference Citation Analysis (0)] |
| 37. | Gao J, Zheng P, Jia Y, Chen H, Mao Y, Chen S, Wang Y, Fu H, Dai J. Mental health problems and social media exposure during COVID-19 outbreak. PLoS One. 2020;15:e0231924. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1367] [Cited by in RCA: 1299] [Article Influence: 259.8] [Reference Citation Analysis (0)] |
| 38. | Hou F, Bi F, Jiao R, Luo D, Song K. Gender differences of depression and anxiety among social media users during the COVID-19 outbreak in China:a cross-sectional study. BMC Public Health. 2020;20:1648. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 109] [Cited by in RCA: 150] [Article Influence: 30.0] [Reference Citation Analysis (0)] |
| 39. | Choi DH, Yoo W, Noh GY, Park K. The impact of social media on risk perceptions during the MERS outbreak in South Korea. Comput Human Behav. 2017;72:422-431. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 159] [Cited by in RCA: 118] [Article Influence: 14.8] [Reference Citation Analysis (0)] |