Published online Jun 19, 2021. doi: 10.5498/wjp.v11.i6.201
Peer-review started: February 15, 2021
First decision: March 30, 2021
Revised: April 7, 2021
Accepted: May 20, 2021
Article in press: May 20, 2021
Published online: June 19, 2021
Processing time: 116 Days and 1.2 Hours
Depression is a common mental disorder and one of the leading causes of disability around the world. Monoaminergic antidepressants often take weeks to months to work and are not effective for all patients. This has led to a search for a better understanding of the pathogenesis of depression as well as to the development of novel antidepressants. One such novel antidepressant is ketamine, which has demonstrated both clinically promising results and contributed to new explanatory models of depression, including the potential role of neuroplasticity in depression. Early clinical trials are now showing promising results of serotonergic psychedelics for depression; however, their mechanism of action remains poorly understood. This paper seeks to review the effect of depression, classic antidepressants, ketamine, and serotonergic psychedelics on markers of neuroplasticity at a cellular, molecular, electrophysiological, functional, structural, and psychological level to explore the potential role that neuroplasticity plays in the treatment response of serotonergic psychedelics.
Core Tip: Depression is a common mental disorder and one of the leading causes of disability around the world. Monoaminergic antidepressants often take weeks to months to work and are not effective for all patients. This review specifically compares the effects of serotonergic psychedelics with other antidepressants on plasticity at multiple levels of nervous system functioning.
- Citation: Artin H, Zisook S, Ramanathan D. How do serotonergic psychedelics treat depression: The potential role of neuroplasticity. World J Psychiatr 2021; 11(6): 201-214
- URL: https://www.wjgnet.com/2220-3206/full/v11/i6/201.htm
- DOI: https://dx.doi.org/10.5498/wjp.v11.i6.201
Depression is a common mental disorder, and considered to be a major contributor to the overall global burden of disease, affecting an estimated 300 million people worldwide[1]. We have known for more than 60 years that medications with antidepressant action increase monoaminergic transmission[2]. Since imipramine was first introduced in 1957, numerous antidepressants have been developed with increasing specificity for the monoamine systems, including agents selective for serotonin, dopamine and norepinephrine. Surprisingly, while these agents lead to an immediate change in monoaminergic neurotransmission, they typically require at least 4 wk of treatment before leading to beneficial effects, and they are only effective around 30%-40% of the time. These observations have led to the conclusion that, rather than treating a “serotonin deficit” (or some other monoamine deficit) antidepressants may work by promoting some form of neuroplasticity in brain circuits that are relevant to depression[3].
Neuroplasticity is a general term that encompasses molecular, cellular, electrophysiological, structural, functional and psychological changes in the brain. Neuroplasticity underlies our ability to learn and is important for recovery after injury[4]. However, the neuroplasticity model of depression suggests that maladaptive plasticity can also lead to problems, such as those that occur in major depressive disorder (MDD). Antidepressants may work in part by harnessing the power of neuroplasticity to change brain circuits driving maladaptive cognitions and behaviors and thereby improve symptoms[5]. This neuroplasticity-based theory of depression and antidepressant action may also provide an explanatory model for how the novel antidepressant, ketamine, exerts its antidepressant effects.
Ketamine modulates glutamate receptors: It is a non-competitive antagonist at the glutamate N-methyl-D-aspartate (NMDA) receptors (and its metabolite, hydroxy-norketamine acts on AMPA receptors). It has been utilized for decades as a dissociative anesthetic. In the early 2000s, the intravenous formulation was discovered to have rapid antidepressant effects at sub-anesthetic doses[6]. Since then, numerous randomized controlled trials have replicated ketamine’s antidepressant effects[7-9]. In the last few years the S+ enantiomer of ketamine, esketamine, has received an FDA indication for treatment resistant depression and acute MDD with suicidal ideation or behavior. Due to its non-traditional mechanism of action as well as its rapid effects, ketamine has broadened our understanding of the possible mechanisms behind depression and antidepressant action; and has contributed to the shift in focus from monoamine functioning to neuroplasticity as a target for antidepressant action.
Since the emergence of glutamatergic agents as new approaches to the treatment of MDD, we have also witnessed renewed enthusiasm for the potential therapeutic role of serotonergic psychedelics. Serotonergic psychedelics encompass a broad category of compounds including lysergic acid diethylamide (LSD), psilocybin, mescaline, dimethyltryptamine (DMT, an active ingredient of ayahuasca), and other derivates that induce non-ordinary states of consciousness, and act as agonists or partial-agonists at the serotonin 2A (5-HT2A) receptor[10-12]. Serotonergic psychedelics have been used for thousands of years in traditional medicine and religious ceremonial settings[11]. In the 1940s, LSD played an increasingly important role in the field of psychiatry in clinical and research settings until the end of the 1960s when psychedelics were made illegal and clinical research abruptly ceased[13]. More recently, clinical research with serotonergic psychedelics has slowly started to reappear. Recent clinical research in the context of psychedelic-assisted psychotherapy, has demonstrated the efficacy of psilocybin in treatment resistant depression[14], in MDD[15], and in cancer-related anxiety and depression, with positive effects lasting up to several months after treatment[16]. Similarly recent trials with ayahuasca in recurrent MDD and in treatment resistant MDD suggest its potential efficacy for MDD[17]. Although clinical trials with LSD are limited, a randomized control double-blind crossover study of LSD in healthy subjects demonstrated lasting changes in positive attitudes about life, positive mood changes, positive social effect and positive changes in well-being[18]. It is important to note that psychedelics may also be associated with transient anxiety, negative affect, and psychosis, which appears to be more common in unprepared users or users with vulnerability to psychosis, however there is no evidence of prolonged psychotic reactions in modern clinical trials when individuals are properly screened[19]. While these early findings suggest that psychedelics may have a potential therapeutic benefit in certain patient populations, the antidepressant mechanism of serotonergic psychedelics remains poorly understood.
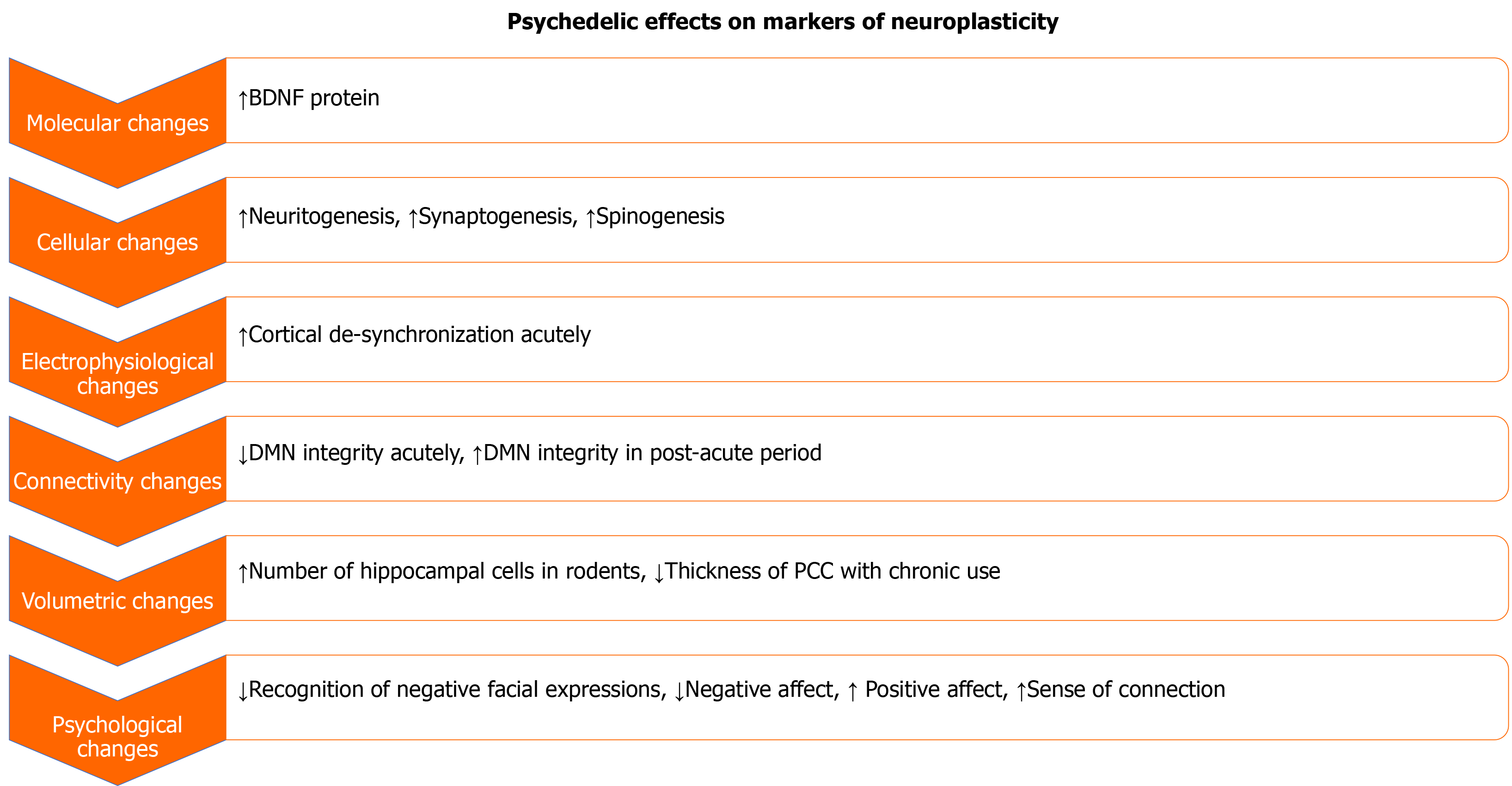
One hypothesis is that all antidepressants share, in common, efficacy in driving neuroplasticity relevant to depression circuits. This paper seeks to briefly review the changes in neuroplasticity associated with MDD, and the larger established literature demonstrating the role that neuroplasticity plays in the therapeutic effect of classic antidepressants and ketamine. We will use this as a basis for exploring what is known about serotonergic psychedelics on markers of neuroplasticity (Figure 1).
Neurotrophic factors play an important role in neuroplasticity. Neurotrophic factors are a family of molecules that, by binding to specific neurotrophic receptors, support growth, survival, differentiation and synaptic plasticity of neurons. Brain derived neurotrophic factor (BDNF) is a key neurotrophic factor involved in most forms of synaptic plasticity. By binding to its corresponding receptor tropomyosin receptor kinase B (TrkB), BDNF activates intracellular pathways that play an important role in the survival and differentiation of neurons and during synaptogenesis[20-22].
Alterations in BDNF-TrkB signaling have been associated with depression in both humans and animals models[23]. In multiple rodent models of chronic, intermittent, or social defeat stress, BDNF-TrkB signaling has been found to be decreased in the prefrontal cortex (PFC) and hippocampus[24,25]. Chronic stress also may increase BDNF/synaptic plasticity in the amygdala and nucleus accumbens[25], suggestive of maladaptive plasticity. In humans, decreased blood levels of BDNF, and cortical expression of BDNF (measured in postmortem studies) have been noted in subjects with MDD[26,27]. Lower levels of BDNF and TrkB expression have also been found in the hippocampus and PFC of subjects who had died by suicide[28].
Typical antidepressants seem to work in part by activating BDNF/TrkB pathways. Chronic antidepressant treatment has been shown to increase BDNF and TrkB receptor mRNA expression in the hippocampus[29] and heterozygous BDNF knockout mice show an impaired antidepressant response[24]. The antidepressant effect of ketamine has also been associated with an increase in BDNF levels in several studies[30,31] and as with typical antidepressants, heterozygous BDNF knockout mice do not show the typical anti-depressant effects of ketamine[32]. Moreover, NMDA antagonists (e.g., memantine) that do not increase BDNF also do not show antidepressant effects, providing further evidence that it is the mechanism of plasticity, rather than NMDA antagonism, that mediates the antidepressant effects of ketamine[33]. This is further bolstered by recent evidence that direct activation of AMPA receptors by a metabolite of ketamine, hydroxy-nor-ketamine, may be sufficient to increase BDNF and induce an antidepressant response[30]. Down-stream from BDNF, there is much evidence that antidepressants like ketamine work via TrkB-induced activation of mTOR[34,35]. In animal models, this mTOR pathway seems critical for the rapid effects of ketamine[36].
In vitro research suggests serotonergic psychedelics can also rapidly increase BDNF levels[37]. Cortical neurons were treated with DOI (a psychedelic amphetamine), DMT or LSD for 24 h before measuring BDNF gene and protein expression using droplet digital polymerase chain reaction and enzyme-linked immunosorbent assay, respectively. Although serotonergic psychedelics did not increase the presence of the BDNF transcript they did result in a 2-fold increase in BDNF protein levels[37]. In human trials, a study in Brazil demonstrated that a single dose of ayahuasca in healthy controls (HCs) and patients with treatment resistant depression led to higher levels of serum BDNF which has been previously negatively correlated with depressive symptoms[38]. Similarly, a recent study of low doses of LSD demonstrated increased serum BDNF levels in HCs at 4 h and 6 h after administration, compared to placebo[39].
There is a large body of literature demonstrating that chronic stress, of various forms, leads to atrophy of prefrontal and hippocampal dendrites[40-43] and synapse loss in those brain regions[44-46]. By contrast, chronic stress models show increased spine density in the basolateral amygdala and nucleus accumbens[47,48]. Postmortem studies in humans are limited but have demonstrated similar findings. For example, there is reduced dendritic branching in the hippocampus and PFC[49] with reduced synapse number in the PFC of depressed subjects[50]. In rodent models of depression, there is evidence that chronic antidepressant treatment can block or reverse some of the above noted changes, including dendritic atrophy and spine loss in the hippocampus and the PFC[51]. Ketamine has also been observed to rapidly increase the number of spine synapses in layer V neurons of the mPFC of rodents in association with its antidepressant behavioral response, and with a similar time course in which the antidepressant effects occur[36,52,53].
Recent research on serotonergic psychedelics suggests that they, likewise, promote rapid dendritic and axonal remodeling. A detailed in vitro report observed increased dendritic arbor complexity when cortical neurons were treated with the serotonergic psychedelics (DMT, DOI, LSD, and psilocin) as well as the entactogen (MDMA) which appeared to arise from an increase in number of dendritic branches and the total length of branches[37]. The effects were even greater to those seen when cortical neurons were treated with ketamine at similar doses. These effects were not observed after treatment with serotonin or D-amphetamine. The in vivo effects of serotonergic psychedelics on neuritogenesis were measured in this study and drosophila larvae treated with LSD and DOI were observed to have increased dendritic branching of class 1 sensory neurons. Serotonergic psychedelics also had an effect on spinogenesis in rat cortical cultures treated with DOI, DMT, and LSD showed an increase of dendritic spines, with LSD doubling the number of spines observed. Adult rats treated with an intraperitoneal dose of DMT also showed a significant increase in synaptic spine density in the PFC 24 h after dosing, coupled with an increase in excitatory post synaptic currents (EPSCs). Interestingly, the effect on neuritogenesis and spinogenesis in cortical neurons was blocked by a TrkB antagonist, ANA-12 and by treatment with rapamycin, an mTOR inhibitor. Thus, this study demonstrated rapid effects of serotonergic psychedelics on neuritogenesis and synaptogenesis are likely mediated by TrkB and mTOR pathways. The effects of serotonergic psychedelics on neuritogenesis and spinogenesis in cultured rat cortical neurons was also reduced by inhibition of the 5-HT2A receptor with ketanserin, a 5-HT 2A receptor antagonist, suggesting that activation of 5-HT2A receptor by serotonergic psychedelics may play a role in their neuritogenesis and synpatogenic properties[37].
We have described above how ketamine and serotonergic psychedelics have been shown to promote rapid synaptic plasticity, with this plasticity possibly mediated via BDNF/TrkB and mTOR pathways. However, one question is why ketamine and serotonergic psychedelics have such rapid effects on plasticity. One hypothesis is that they do so because they induce molecular/cellular correlates of plasticity while simultaneously activating brain circuits in ways that amplifies or drives activity-dependent plasticity[22].
To understand how serotonergic psychedelics might result in rapid plasticity, we reviewed the evidence around whether such agents modify brain activity in a way that, like ketamine, might drive activity-dependent plasticity. Ketamine has long been shown to increase cortical excitability[54]. These changes may occur by suppressing activity of inhibitory neurons preferentially[55-57], resulting in an overall state of disinhibition. More recent work has shown that that ketamine-induced antidepressant effects are specifically linked with inhibition of somatostatin neurons[58] resulting in increases in excitability of parvalbumin in addition to glutamatergic neurons and thus protection of spines that would otherwise have been pruned[59]. Evidence from humans corroborates that there is a net increase in both glutamate and GABA (gamma-aminobutyric acid) concentrations in PFC measured using proton spectroscopy after ketamine suggesting that, in humans too, there is a relative disinhibition of prefrontal cortical activity[60]. This data is verified using in vivo electrophysiology as well. Multiple studies, across both humans and animals, suggest that ketamine (and its metabolite, hydroxy-norketamine) results in a clear increase in gamma activity (30-80 Hz activity, a useful index of an increase in cortical excitability[61,62].
Some research suggests that serotonergic psychedelic drugs may directly modulate prefrontal cortical activity, leading to activity-dependent plasticity, via 5-HT2A receptor activation in the cortex, though it appears to do so in a way very different then ketamine[63]. The 5-HT2A receptor is expressed in deep layer V pyramidal neurons and GABAergic (particularly parvalbumin, PV+) neurons[63,64]. Activation of the 5-HT2A receptor depolarizes and directly excites a subpopulation of deep Layer V pyramidal neurons[65,66], leading to an increase in glutamatergic EPSCs[67-70]. There are reports that pyramidal neurons show both increases and decreases in spiking in response to 5-HT2A agonists, though typically a higher proportion of pyramidal neurons are increased[71-73]. However, unlike ketamine, serotonergic psychedelics like DOI and 5-MeO-DMT actually reduce low-frequency oscillations[71,72] and gamma oscillations[73]. Data from humans also shows that serotonergic psychedelics are all associated with a broadband reduction of power less than 100 Hz[74-77].
In summary, while there is some preliminary evidence that both ketamine and serotonergic psychedelics increase molecular and cellular aspects of synaptic plasticity (activation of BDNF/TrkB pathways; increased synapse/dendritic structure), the mechanisms by which ketamine and serotonergic do this seem to be quite different. With ketamine, there is evidence of an increase in gamma activity/excitability in the cortex, which could serve to activate activity-dependent mechanisms of plasticity and may explain some of the rapid effects observed. With serotonergic psychedelic agents, changes in activity have been shown for certain deep pyramidal cells, but overall evidence from in vivo studies suggests that there is not a global level of disinhibition or increase in neural synchrony as a general or wide-spread phenomenon during psychedelics exposure.
Neuroplasticity may also be observed on the level of changes in brain networks[78]. The literature suggests that symptoms of depression are associated with network alterations in “default-mode” brain networks, as well as in salience, affective and cognitive control/executive function brain networks[79]. The default mode network (DMN) defined by the anterior medial PFC, posterior cingulate cortex (PCC) and angular gyrus has consistently demonstrated altered connectivity in depression[80]. The normal functioning of the DMN has been associated with self-referential processes, which may be maladaptively heightened in patients with depression[81]. Processes such as maladaptive rumination that are associated with depression, and involve a repetitive reflection of negative thoughts and emotions[82], are associated with hyper connectivity of the DMN both in depressed patients and healthy subjects[83].
It is likely that a simple linear relationship between increased or decreased connectivity in the DMN being correlated to depression and antidepressant response is over-simplified, and instead antidepressant therapies may work to reconfigure the default mode towards healthier patterns. In that vein, antidepressants have been found to affect and normalize altered DMN connectivity. In a study of healthy volunteers a two week administration of the serotonin-norepinephrine reuptake inhibitor (SNRI) duloxetine was found to reduce default mode connectivity in healthy individuals during rest[84]. In a study of 41 patients with dysthymic disorder, a depressive disorder similar to MDD, who were found to have alteration of DMN activity compared to normal controls, 10 wk of treatment with duloxetine was found to normalize function in the DMN, compared to placebo which had no such effect[85]. Ketamine has also been associated with circuit level changes in the DMN. In a randomized, placebo-controlled, double-blind, crossover study in healthy subjects, ketamine was found to decrease functional connectivity of the DMN to the dmPFC[86]. A different study comparing HCs with patients with MDD measured functional connectivity at baseline and at 2 and 10 d after ketamine infusion. In subjects with MDD, connectivity between the insula and the DMN was normalized compared with HCs 2 d post ketamine infusion. This change was reversed after 10 d, a typical time course when the effects of ketamine begin to diminish and did not appear in either of the placebo scans, indicating this effect was an important aspect of the antidepressant function of ketamine[87].
Serotonergic psychedelics clearly alter DMN function and connectivity. A number of studies using LSD[88,89], psilocybin[90-92] and ayahuasca[93-95] have observed changes in functional connectivity of the DMN, and a common finding is an acute decrease in the integrity of the DMN. There are few studies that have looked at longer-term changes in DMN activity or connectivity. However, one study showed that in patients with depression treated with psilocybin, DMN integrity has been observed to increase or normalize in the post-acute period (1-d post-dose) accompanied by improvements in mood, and DMN normalization was predictive of treatment response at five weeks[96]. It is striking that in the early studies serotonergic psychedelics seem to have longer lasting treatment response than typically seen in ketamine studies, although clearly more evidence is required.
Depression and antidepressant treatment have also been associated with neuroplastic changes at the volumetric level. One area that has been heavily implicated in being involved in depression is the hippocampus. Reductions of hippocampal volume have been seen in cynomolgus monkeys and in mice[46], and in humans reduction of hippocampal volume is one of the most common brain changes associated with depression and chronic stress[97,98]. The hippocampus (and medial temporal lobe) is a key part of the human default-mode-network, and stress-induced alterations in this structure may contribute to some of the network-changes observed above. Other consistently reported grey matter abnormalities associated with depression in humans include decreased volumes of the cingulate cortex, the PFC, the orbitofrontal cortex, amygdala, and the basal ganglia[99]. White matter lesions have also been demonstrated in depression and have been demonstrated as being especially prominent in late-life depression[100].
Amazingly, antidepressants have been shown to normalize hippocampal volume. One study found increased right hippocampal volumes in female responders compared to non-responders after eight weeks of treatment with the selective serotonin reuptake inhibitor (SSRI) fluoxetine[101]. Other studies have demonstrated that patients treated with antidepressants who do not remit have lower bilateral hippocampal volumes at baseline and follow-up compared to remitted patients[102], though not all studies have found this relationship[103]. Studies investigating the effect of ketamine on structural brain changes are limited, although one study investigating the use of repeated ketamine treatment in patients with MDD observed increases in the volumes of the amygdala and hippocampus after just 6 ketamine infusions[104]. Studies on structural changes associated with serotonergic psychedelics are even more limited particularly with regards to humans with depression. However, in rodent models of trace fear conditioning, mice injected with low doses of psilocybin exhibited faster extinguishing of fear conditioning and an increased number of cells in the hippocampus compared to mice injected with saline or high dose psilocybin[105]. In non-depressed patients, one study found that 22 regular users of ayahuasca had thinning in the PCC and noted that cortical thickness values in the PCC were inversely correlated with personality traits measuring religiousness, transpersonal feelings and spirituality[106].
Plasticity can also relate to psychological changes in emotional, self, and social processing, which all play an important role in depression and antidepressant responses. Several studies have demonstrated that individuals with MDD demonstrate a bias towards negative emotional information compared to HCs[107,108]. Depression is also associated with perseverative negative ruminations[109]. Depression can also affect social processing, and has been associated with diminished desire for socialization, increased sensitivity to rejection, reduced cooperativeness, and impairment in understanding how others are feeling[110].
Antidepressants have been associated with changes in emotional processing[111], including changes in positive emotional recall with SSRIs and SNRIs in healthy volunteers, and changes in recognition of emotional facial expression, with the SSRI citalopram and the SNRI reboxetine reducing the identification of the negative facial expressions of harm and fear[112]. Ketamine may also lead to changes in these psychological processes. In a double-blind, placebo-controlled crossover study of 33 individuals with treatment-resistant MDD and 24 HCs, participants received ketamine and placebo infusions 2 wk apart, and functional magnetic resonance imaging scans were conducted at baseline and 2 days after each infusion during an attentional bias dot probe task with emotional face stimuli using “happy”, “angry” or “neutral” faces across multiple time points. Ketamine infusion was found to have opposite effects on brain activation in regions associated with emotional processing in MDD vs HC participants, and in participants with MDD led to similar brain activity as HCs after placebo suggesting a possible “normalizing” effect on emotional processing in patients with MDD[113].
Serotonergic psychedelics also result in sustained and profound changes in emotional processing and sociability. LSD and psilocybin have been observed to decrease the recognition of negative facial expressions in healthy participants[114,115]. Another study of healthy participants looking at changes in affect one week and one month after administration of psilocybin observed that negative affect decreased 1 wk after administration of psilocybin and positive affect increased, and while the changes in negative affect normalized after 1 mo, changes in positive affect persisted[116]. Beyond this, other unique psychological changes have been associated with serotonergic psychedelics, including a shift from a sense of disconnection from oneself, others, and the world to a sense of connection, and from avoidance of emotion to acceptance[117]. Both LSD and psilocybin have also been shown to acutely increase emotional empathy, and LSD was found to increase prosocial behavior on a social value orientation test. One unique property of serotonergic psychedelics is the experience of ego-dissolution which may occur during peak psychedelic experiences or “mystical experiences” where one experiences a loosening sense of boundaries between themselves and the world and a sense of unity and interconnectedness. It is possible that this subjective experience may in part account for shifting the relationship to one’s sense of self and towards one’s sense of connection with others. It is interesting that the quality of the subjective “peak experience” has been associated with therapeutic efficacy[118]. Indeed, one plausible explanation for why serotonergic psychedelic agents are effective is that they evoke psychological experiences acutely while (at a molecular/cellular level) activating mechanisms of plasticity that help to engrain these experiences in long-term memory.
There is increasing evidence that psychedelic agents may induce rapid synaptic plasticity, and that this plasticity may be a key mechanism by which they can exert long-term antidepressant effects. However, it is important to note that plasticity is not, by itself, an inherently “anti-depressant” action. Indeed, as reviewed above, depression, anxiety and PTSD can, themselves, be caused or exacerbated by maladaptive forms of plasticity. Thus, the particular locus of this plasticity (neuronal sub-type, brain region, large-scale brain network) is important in understanding how such drugs cure depression. Psychedelic agents affect the brain in very different ways than ketamine (both when measured at the level of single units and local field potentials, or fMRI). However, longer-term changes in default-mode-network function may be a common endpoint linking both ketamine and psychedelic drugs in explaining antidepressant function of both agents. It is also vitally important to consider the psychedelic experience itself. The psychedelic experience has been described by some participants as being among the most meaningful or spiritually significant experiences of their lives[119]. If psychedelic agents produce these altered brain states, while simultaneously activating molecular/cellular cascades linked with plasticity, it could, indeed, provide a completely unique way of rapidly consolidating the effects of the experience for long-term retention. Trauma provides an example of how a single event, linked to mechanisms of plasticity, can cause long-term detrimental effects on brain and behavior[120]. Serotonergic psychedelics may well be the opposite — a pharmacologically-induced state of altered consciousness in which experiences are consolidated due to heightened mechanisms of synaptic plasticity.
Many questions remain. First, the question of to what extent neuroplasticity plays a role in depression. MDD is a complex disorder, and numerous factors play a role in its development including genetic, epigenetic, developmental, inflammatory, endocrine and psychological changes. A complete model of depression would account for how these various factors interlink to lead to the ultimate outcome of depression. Similarly, the question exists of to what extent neuroplasticity plays a role in the therapeutic effect of serotonergic psychedelics. The question also remains as to whether the therapeutic effect of serotonergic psychedelics is dissociable from the drugs subjective effects. While it is likely that neuroplasticity plays a role in the antidepressant treatment response of serotonergic psychedelics, further research is warranted to better characterize the other factors that play a role.
Manuscript source: Invited manuscript
Specialty type: Psychiatry
Country/Territory of origin: United States
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Brog NA, Zhang D S-Editor: Gao CC L-Editor: A P-Editor: Li JH
| 1. | Herrman H, Kieling C, McGorry P, Horton R, Sargent J, Patel V. Reducing the global burden of depression: a Lancet-World Psychiatric Association Commission. Lancet. 2019;393:e42-e43. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 121] [Cited by in RCA: 249] [Article Influence: 41.5] [Reference Citation Analysis (0)] |
| 2. | Cahn C. Roland Kuhn, 1912-2005. Neuropsychopharmacology. 2006;31:1096-1096. [RCA] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 3. | Harmer CJ, Duman RS, Cowen PJ. How do antidepressants work? Lancet Psychiatry. 2017;4:409-418. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 346] [Cited by in RCA: 373] [Article Influence: 46.6] [Reference Citation Analysis (0)] |
| 4. | Sharma N, Classen J, Cohen LG. Neural plasticity and its contribution to functional recovery. Handbook of Clinical Neurology. Elsevier, 2013: 3-12. |
| 5. | Albert PR. Adult neuroplasticity: A new “cure” for major depression? J Psychiatry Neurosci. 2019;44:147-150. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 28] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 6. | Berman RM, Cappiello A, Anand A, Oren DA, Heninger GR, Charney DS, Krystal JH. Antidepressant effects of ketamine in depressed patients. Biol Psychiatry. 2000;47:351-354. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2441] [Cited by in RCA: 2757] [Article Influence: 110.3] [Reference Citation Analysis (0)] |
| 7. | Murrough JW, Iosifescu DV, Chang LC, Al Jurdi RK, Green CE, Perez AM, Iqbal S, Pillemer S, Foulkes A, Shah A, Charney DS, Mathew SJ. Antidepressant efficacy of ketamine in treatment-resistant major depression: a two-site randomized controlled trial. Am J Psychiatry. 2013;170:1134-1142. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 762] [Cited by in RCA: 870] [Article Influence: 72.5] [Reference Citation Analysis (0)] |
| 8. | Matveychuk D, Thomas RK, Swainson J, Khullar A, MacKay MA, Baker GB, Dursun SM. Ketamine as an antidepressant: overview of its mechanisms of action and potential predictive biomarkers. Ther Adv Psychopharmacol. 2020;10:2045125320916657. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 91] [Cited by in RCA: 112] [Article Influence: 22.4] [Reference Citation Analysis (0)] |
| 9. | Zarate CA Jr, Singh JB, Carlson PJ, Brutsche NE, Ameli R, Luckenbaugh DA, Charney DS, Manji HK. A randomized trial of an N-methyl-D-aspartate antagonist in treatment-resistant major depression. Arch Gen Psychiatry. 2006;63:856-864. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2275] [Cited by in RCA: 2591] [Article Influence: 136.4] [Reference Citation Analysis (0)] |
| 10. | Halberstadt AL. Recent advances in the neuropsychopharmacology of serotonergic hallucinogens. Behav Brain Res. 2015;277:99-120. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 191] [Cited by in RCA: 212] [Article Influence: 21.2] [Reference Citation Analysis (0)] |
| 11. | Nichols DE. Psychedelics. Pharmacol Rev. 2016;68:264-355. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1216] [Cited by in RCA: 1030] [Article Influence: 114.4] [Reference Citation Analysis (0)] |
| 12. | López-Giménez JF, González-Maeso J. Hallucinogens and serotonin 5-HT2A receptor-mediated signaling pathways. Current Topics in Behavioral Neurosciences. Springer Verlag, 2018: 45-73. |
| 13. | Sessa B. The History of Psychedelics in Medicine. In: von Heyden M., Jungaberle H., Majić T. Handbuch Psychoaktive Substanzen. Berlin, Heidelberg, Springer, 2016. |
| 14. | Carhart-Harris RL, Bolstridge M, Rucker J, Day CM, Erritzoe D, Kaelen M, Bloomfield M, Rickard JA, Forbes B, Feilding A, Taylor D, Pilling S, Curran VH, Nutt DJ. Psilocybin with psychological support for treatment-resistant depression: an open-label feasibility study. Lancet Psychiatry. 2016;3:619-627. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 691] [Cited by in RCA: 911] [Article Influence: 101.2] [Reference Citation Analysis (0)] |
| 15. | Davis AK, Barrett FS, May DG, Cosimano MP, Sepeda ND, Johnson MW, Finan PH, Griffiths RR. Effects of Psilocybin-Assisted Therapy on Major Depressive Disorder: A Randomized Clinical Trial. JAMA Psychiatry. 2021;78:481-489. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 922] [Cited by in RCA: 720] [Article Influence: 180.0] [Reference Citation Analysis (0)] |
| 16. | Ross S, Bossis A, Guss J, Agin-Liebes G, Malone T, Cohen B, Mennenga SE, Belser A, Kalliontzi K, Babb J, Su Z, Corby P, Schmidt BL. Rapid and sustained symptom reduction following psilocybin treatment for anxiety and depression in patients with life-threatening cancer: a randomized controlled trial. J Psychopharmacol. 2016;30:1165-1180. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1162] [Cited by in RCA: 964] [Article Influence: 107.1] [Reference Citation Analysis (0)] |
| 17. | Palhano-Fontes F, Barreto D, Onias H, Andrade KC, Novaes MM, Pessoa JA, Mota-Rolim SA, Osório FL, Sanches R, Dos Santos RG, Tófoli LF, de Oliveira Silveira G, Yonamine M, Riba J, Santos FR, Silva-Junior AA, Alchieri JC, Galvão-Coelho NL, Lobão-Soares B, Hallak JEC, Arcoverde E, Maia-de-Oliveira JP, Araújo DB. Rapid antidepressant effects of the psychedelic ayahuasca in treatment-resistant depression: a randomized placebo-controlled trial. Psychol Med. 2019;49:655-663. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 367] [Cited by in RCA: 469] [Article Influence: 78.2] [Reference Citation Analysis (0)] |
| 18. | Schmid Y, Liechti ME. Long-lasting subjective effects of LSD in normal subjects. Psychopharmacology (Berl). 2018;235:535-545. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 131] [Cited by in RCA: 144] [Article Influence: 20.6] [Reference Citation Analysis (0)] |
| 19. | Krebs TS, Johansen PØ. Psychedelics and mental health: a population study. PLoS One. 2013;8:e63972. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 168] [Cited by in RCA: 222] [Article Influence: 18.5] [Reference Citation Analysis (0)] |
| 20. | Hofer MM, Barde YA. Brain-derived neurotrophic factor prevents neuronal death in vivo. Nature. 1988;331:261-262. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 373] [Cited by in RCA: 374] [Article Influence: 10.1] [Reference Citation Analysis (0)] |
| 21. | Nawa H, Takei N. BDNF as an anterophin; a novel neurotrophic relationship between brain neurons. Trends Neurosci. 2001;24:683-684. [RCA] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 41] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 22. | Lu B. BDNF and activity-dependent synaptic modulation. Learn Mem. 2003;10:86-98. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 723] [Cited by in RCA: 741] [Article Influence: 33.7] [Reference Citation Analysis (0)] |
| 23. | Castrén E, Rantamäki T. The role of BDNF and its receptors in depression and antidepressant drug action: Reactivation of developmental plasticity. Dev Neurobiol. 2010;70:289-297. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 602] [Cited by in RCA: 643] [Article Influence: 42.9] [Reference Citation Analysis (0)] |
| 24. | Duman RS, Monteggia LM. A neurotrophic model for stress-related mood disorders. Biol Psychiatry. 2006;59:1116-1127. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2372] [Cited by in RCA: 2481] [Article Influence: 130.6] [Reference Citation Analysis (0)] |
| 25. | Krishnan V, Nestler EJ. The molecular neurobiology of depression. Nature. 2008;455:894-902. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2243] [Cited by in RCA: 2075] [Article Influence: 122.1] [Reference Citation Analysis (0)] |
| 26. | Pandey GN, Ren X, Rizavi HS, Conley RR, Roberts RC, Dwivedi Y. Brain-derived neurotrophic factor and tyrosine kinase B receptor signalling in post-mortem brain of teenage suicide victims. Int J Neuropsychopharmacol. 2008;11:1047-1061. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 138] [Cited by in RCA: 140] [Article Influence: 8.2] [Reference Citation Analysis (0)] |
| 27. | Hayley S, Du L, Litteljohn D, Palkovits M, Faludi G, Merali Z, Poulter MO, Anisman H. Gender and brain regions specific differences in brain derived neurotrophic factor protein levels of depressed individuals who died through suicide. Neurosci Lett. 2015;600:12-16. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 49] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 28. | Dwivedi Y, Rizavi HS, Conley RR, Roberts RC, Tamminga CA, Pandey GN. Altered gene expression of brain-derived neurotrophic factor and receptor tyrosine kinase B in postmortem brain of suicide subjects. Arch Gen Psychiatry. 2003;60:804-815. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 612] [Cited by in RCA: 625] [Article Influence: 28.4] [Reference Citation Analysis (0)] |
| 29. | Dias BG, Banerjee SB, Duman RS, Vaidya VA. Differential regulation of brain derived neurotrophic factor transcripts by antidepressant treatments in the adult rat brain. Neuropharmacology. 2003;45:553-563. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 208] [Cited by in RCA: 211] [Article Influence: 9.6] [Reference Citation Analysis (0)] |
| 30. | Zanos P, Thompson SM, Duman RS, Zarate CA Jr, Gould TD. Convergent Mechanisms Underlying Rapid Antidepressant Action. CNS Drugs. 2018;32:197-227. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 121] [Cited by in RCA: 129] [Article Influence: 18.4] [Reference Citation Analysis (0)] |
| 31. | Björkholm C, Monteggia LM. BDNF - a key transducer of antidepressant effects. Neuropharmacology. 2016;102:72-79. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 493] [Cited by in RCA: 699] [Article Influence: 69.9] [Reference Citation Analysis (0)] |
| 32. | Autry AE, Adachi M, Nosyreva E, Na ES, Los MF, Cheng PF, Kavalali ET, Monteggia LM. NMDA receptor blockade at rest triggers rapid behavioural antidepressant responses. Nature. 2011;475:91-95. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1592] [Cited by in RCA: 1484] [Article Influence: 106.0] [Reference Citation Analysis (1)] |
| 33. | Gideons ES, Kavalali ET, Monteggia LM. Mechanisms underlying differential effectiveness of memantine and ketamine in rapid antidepressant responses. Proc Natl Acad Sci U S A. 2014;111:8649-8654. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 145] [Cited by in RCA: 182] [Article Influence: 16.5] [Reference Citation Analysis (0)] |
| 34. | Jernigan CS, Goswami DB, Austin MC, Iyo AH, Chandran A, Stockmeier CA, Karolewicz B. The mTOR signaling pathway in the prefrontal cortex is compromised in major depressive disorder. Prog Neuropsychopharmacol Biol Psychiatry. 2011;35:1774-1779. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 344] [Cited by in RCA: 321] [Article Influence: 22.9] [Reference Citation Analysis (0)] |
| 35. | Abelaira HM, Réus GZ, Neotti MV, Quevedo J. The role of mTOR in depression and antidepressant responses. Life Sci. 2014;101:10-14. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 116] [Cited by in RCA: 148] [Article Influence: 13.5] [Reference Citation Analysis (0)] |
| 36. | Li N, Lee B, Liu RJ, Banasr M, Dwyer JM, Iwata M, Li XY, Aghajanian G, Duman RS. mTOR-dependent synapse formation underlies the rapid antidepressant effects of NMDA antagonists. Science. 2010;329:959-964. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2352] [Cited by in RCA: 2230] [Article Influence: 148.7] [Reference Citation Analysis (0)] |
| 37. | Ly C, Greb AC, Cameron LP, Wong JM, Barragan EV, Wilson PC, Burbach KF, Soltanzadeh Zarandi S, Sood A, Paddy MR, Duim WC, Dennis MY, McAllister AK, Ori-McKenney KM, Gray JA, Olson DE. Psychedelics Promote Structural and Functional Neural Plasticity. Cell Rep. 2018;23:3170-3182. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 360] [Cited by in RCA: 659] [Article Influence: 94.1] [Reference Citation Analysis (0)] |
| 38. | de Almeida RN, Galvão ACM, da Silva FS, Silva EADS, Palhano-Fontes F, Maia-de-Oliveira JP, de Araújo LB, Lobão-Soares B, Galvão-Coelho NL. Modulation of Serum Brain-Derived Neurotrophic Factor by a Single Dose of Ayahuasca: Observation From a Randomized Controlled Trial. Front Psychol. 2019;10:1234. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 109] [Cited by in RCA: 112] [Article Influence: 18.7] [Reference Citation Analysis (0)] |
| 39. | Hutten NRPW, Mason NL, Dolder PC, Theunissen EL, Holze F, Liechti ME, Varghese N, Eckert A, Feilding A, Ramaekers JG, Kuypers KPC. Low Doses of LSD Acutely Increase BDNF Blood Plasma Levels in Healthy Volunteers. ACS Pharmacol Transl Sci. 2021;4:461-466. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 36] [Cited by in RCA: 91] [Article Influence: 18.2] [Reference Citation Analysis (0)] |
| 40. | Cook SC, Wellman CL. Chronic stress alters dendritic morphology in rat medial prefrontal cortex. J Neurobiol. 2004;60:236-248. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 509] [Cited by in RCA: 562] [Article Influence: 26.8] [Reference Citation Analysis (0)] |
| 41. | Sousa N, Lukoyanov NV, Madeira MD, Almeida OF, Paula-Barbosa MM. Reorganization of the morphology of hippocampal neurites and synapses after stress-induced damage correlates with behavioral improvement. Neuroscience. 2000;97:253-266. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 555] [Cited by in RCA: 567] [Article Influence: 22.7] [Reference Citation Analysis (0)] |
| 42. | Magariños AM, McEwen BS. Stress-induced atrophy of apical dendrites of hippocampal CA3c neurons: involvement of glucocorticoid secretion and excitatory amino acid receptors. Neuroscience. 1995;69:89-98. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 667] [Cited by in RCA: 685] [Article Influence: 22.8] [Reference Citation Analysis (0)] |
| 43. | Watanabe Y, Gould E, McEwen BS. Stress induces atrophy of apical dendrites of hippocampal CA3 pyramidal neurons. Brain Res. 1992;588:341-345. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 868] [Cited by in RCA: 901] [Article Influence: 27.3] [Reference Citation Analysis (0)] |
| 44. | Ota KT, Liu RJ, Voleti B, Maldonado-Aviles JG, Duric V, Iwata M, Dutheil S, Duman C, Boikess S, Lewis DA, Stockmeier CA, DiLeone RJ, Rex C, Aghajanian GK, Duman RS. REDD1 is essential for stress-induced synaptic loss and depressive behavior. Nat Med. 2014;20:531-535. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 208] [Cited by in RCA: 209] [Article Influence: 19.0] [Reference Citation Analysis (0)] |
| 45. | Goldwater DS, Pavlides C, Hunter RG, Bloss EB, Hof PR, McEwen BS, Morrison JH. Structural and functional alterations to rat medial prefrontal cortex following chronic restraint stress and recovery. Neuroscience. 2009;164:798-808. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 260] [Cited by in RCA: 266] [Article Influence: 16.6] [Reference Citation Analysis (0)] |
| 46. | Qiao H, Li MX, Xu C, Chen HB, An SC, Ma XM. Dendritic Spines in Depression: What We Learned from Animal Models. Neural Plast. 2016;2016:8056370. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 211] [Cited by in RCA: 315] [Article Influence: 35.0] [Reference Citation Analysis (0)] |
| 47. | Mitra R, Jadhav S, McEwen BS, Vyas A, Chattarji S. Stress duration modulates the spatiotemporal patterns of spine formation in the basolateral amygdala. Proc Natl Acad Sci U S A. 2005;102:9371-9376. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 446] [Cited by in RCA: 487] [Article Influence: 24.4] [Reference Citation Analysis (0)] |
| 48. | Zhang JY, Liu TH, He Y, Pan HQ, Zhang WH, Yin XP, Tian XL, Li BM, Wang XD, Holmes A, Yuan TF, Pan BX. Chronic Stress Remodels Synapses in an Amygdala Circuit-Specific Manner. Biol Psychiatry. 2019;85:189-201. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 74] [Cited by in RCA: 121] [Article Influence: 20.2] [Reference Citation Analysis (0)] |
| 49. | Hercher C, Canetti L, Turecki G, Mechawar N. Anterior cingulate pyramidal neurons display altered dendritic branching in depressed suicides. J Psychiatr Res. 2010;44:286-293. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 44] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 50. | Kang HJ, Voleti B, Hajszan T, Rajkowska G, Stockmeier CA, Licznerski P, Lepack A, Majik MS, Jeong LS, Banasr M, Son H, Duman RS. Decreased expression of synapse-related genes and loss of synapses in major depressive disorder. Nat Med. 2012;18:1413-1417. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 484] [Cited by in RCA: 609] [Article Influence: 46.8] [Reference Citation Analysis (0)] |
| 51. | Duman CH, Duman RS. Spine synapse remodeling in the pathophysiology and treatment of depression. Neurosci Lett. 2015;601:20-29. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 201] [Cited by in RCA: 198] [Article Influence: 19.8] [Reference Citation Analysis (0)] |
| 52. | Zhang J, Qu Y, Chang L, Pu Y, Hashimoto K. (R)-Ketamine Rapidly Ameliorates the Decreased Spine Density in the Medial Prefrontal Cortex and Hippocampus of Susceptible Mice After Chronic Social Defeat Stress. Int J Neuropsychopharmacol. 2019;22:675-679. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 28] [Cited by in RCA: 38] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 53. | Phoumthipphavong V, Barthas F, Hassett S, Kwan AC. Longitudinal Effects of Ketamine on Dendritic Architecture In Vivo in the Mouse Medial Frontal Cortex. eNeuro. 2016;3. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 71] [Cited by in RCA: 97] [Article Influence: 10.8] [Reference Citation Analysis (0)] |
| 54. | Breier A, Malhotra AK, Pinals DA, Weisenfeld NI, Pickar D. Association of ketamine-induced psychosis with focal activation of the prefrontal cortex in healthy volunteers. Am J Psychiatry. 1997;154:805-811. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 297] [Cited by in RCA: 271] [Article Influence: 9.7] [Reference Citation Analysis (0)] |
| 55. | Homayoun H, Moghaddam B. NMDA receptor hypofunction produces opposite effects on prefrontal cortex interneurons and pyramidal neurons. J Neurosci. 2007;27:11496-11500. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1039] [Cited by in RCA: 943] [Article Influence: 52.4] [Reference Citation Analysis (0)] |
| 56. | Moghaddam B, Adams B, Verma A, Daly D. Activation of glutamatergic neurotransmission by ketamine: a novel step in the pathway from NMDA receptor blockade to dopaminergic and cognitive disruptions associated with the prefrontal cortex. J Neurosci. 1997;17:2921-2927. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1233] [Cited by in RCA: 1296] [Article Influence: 46.3] [Reference Citation Analysis (0)] |
| 57. | Zhang B, Yang X, Ye L, Liu R, Ye B, Du W, Shen F, Li Q, Guo F, Liu J, Li Y, Xu Z, Liu Z. Ketamine activated glutamatergic neurotransmission by GABAergic disinhibition in the medial prefrontal cortex. Neuropharmacology. 2020;108382. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 24] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 58. | Ali F, Gerhard DM, Sweasy K, Pothula S, Pittenger C, Duman RS, Kwan AC. Ketamine disinhibits dendrites and enhances calcium signals in prefrontal dendritic spines. Nat Commun. 2020;11:72. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 80] [Cited by in RCA: 145] [Article Influence: 29.0] [Reference Citation Analysis (0)] |
| 59. | Ng LHL, Huang Y, Han L, Chang RC, Chan YS, Lai CSW. Ketamine and selective activation of parvalbumin interneurons inhibit stress-induced dendritic spine elimination. Transl Psychiatry. 2018;8:272. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 44] [Cited by in RCA: 61] [Article Influence: 8.7] [Reference Citation Analysis (0)] |
| 60. | Milak MS, Rashid R, Dong Z, Kegeles LS, Grunebaum MF, Ogden RT, Lin X, Mulhern ST, Suckow RF, Cooper TB, Keilp JG, Mao X, Shungu DC, Mann JJ. Assessment of Relationship of Ketamine Dose With Magnetic Resonance Spectroscopy of Glx and GABA Responses in Adults With Major Depression: A Randomized Clinical Trial. JAMA Netw Open. 2020;3:e2013211. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 29] [Cited by in RCA: 44] [Article Influence: 8.8] [Reference Citation Analysis (0)] |
| 61. | Zanos P, Moaddel R, Morris PJ, Georgiou P, Fischell J, Elmer GI, Alkondon M, Yuan P, Pribut HJ, Singh NS, Dossou KS, Fang Y, Huang XP, Mayo CL, Wainer IW, Albuquerque EX, Thompson SM, Thomas CJ, Zarate CA Jr, Gould TD. NMDAR inhibition-independent antidepressant actions of ketamine metabolites. Nature. 2016;533:481-486. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 922] [Cited by in RCA: 1171] [Article Influence: 130.1] [Reference Citation Analysis (0)] |
| 62. | Nugent AC, Ballard ED, Gould TD, Park LT, Moaddel R, Brutsche NE, Zarate CA Jr. Ketamine has distinct electrophysiological and behavioral effects in depressed and healthy subjects. Mol Psychiatry. 2019;24:1040-1052. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 171] [Cited by in RCA: 165] [Article Influence: 27.5] [Reference Citation Analysis (0)] |
| 63. | Andrade C, Rao NS. How antidepressant drugs act: A primer on neuroplasticity as the eventual mediator of antidepressant efficacy. Indian J Psychiatry. 2010;52:378-386. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 52] [Cited by in RCA: 77] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 64. | Willins DL, Deutch AY, Roth BL. Serotonin 5-HT2A receptors are expressed on pyramidal cells and interneurons in the rat cortex. Synapse. 1997;27:79-82. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 65. | Lambe EK, Goldman-Rakic PS, Aghajanian GK. Serotonin induces EPSCs preferentially in layer V pyramidal neurons of the frontal cortex in the rat. Cereb Cortex. 2000;10:974-980. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 55] [Cited by in RCA: 68] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 66. | Béïque JC, Imad M, Mladenovic L, Gingrich JA, Andrade R. Mechanism of the 5-hydroxytryptamine 2A receptor-mediated facilitation of synaptic activity in prefrontal cortex. Proc Natl Acad Sci U S A. 2007;104:9870-9875. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 146] [Cited by in RCA: 166] [Article Influence: 9.2] [Reference Citation Analysis (0)] |
| 67. | Aghajanian GK, Marek GJ. Serotonin and hallucinogens. Neuropsychopharmacology. 1999;21:16S-23S. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 151] [Cited by in RCA: 155] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 68. | Zhou FM, Hablitz JJ. Activation of serotonin receptors modulates synaptic transmission in rat cerebral cortex. J Neurophysiol. 1999;82:2989-2999. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 160] [Cited by in RCA: 188] [Article Influence: 7.2] [Reference Citation Analysis (0)] |
| 69. | Muschamp JW, Regina MJ, Hull EM, Winter JC, Rabin RA. Lysergic acid diethylamide and [-]-2,5-dimethoxy-4-methylamphetamine increase extracellular glutamate in rat prefrontal cortex. Brain Res. 2004;1023:134-140. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 79] [Cited by in RCA: 84] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 70. | Andrade R. Serotonergic regulation of neuronal excitability in the prefrontal cortex. Neuropharmacology. 2011;61:382-386. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 143] [Cited by in RCA: 124] [Article Influence: 8.9] [Reference Citation Analysis (0)] |
| 71. | Celada P, Puig MV, Díaz-Mataix L, Artigas F. The hallucinogen DOI reduces low-frequency oscillations in rat prefrontal cortex: reversal by antipsychotic drugs. Biol Psychiatry. 2008;64:392-400. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 88] [Cited by in RCA: 96] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 72. | Riga MS, Lladó-Pelfort L, Artigas F, Celada P. The serotonin hallucinogen 5-MeO-DMT alters cortico-thalamic activity in freely moving mice: Regionally-selective involvement of 5-HT1A and 5-HT2A receptors. Neuropharmacology. 2018;142:219-230. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 34] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 73. | Wood J, Kim Y, Moghaddam B. Disruption of prefrontal cortex large scale neuronal activity by different classes of psychotomimetic drugs. J Neurosci. 2012;32:3022-3031. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 126] [Cited by in RCA: 115] [Article Influence: 8.8] [Reference Citation Analysis (0)] |
| 74. | Riba J, Anderer P, Morte A, Urbano G, Jané F, Saletu B, Barbanoj MJ. Topographic pharmaco-EEG mapping of the effects of the South American psychoactive beverage ayahuasca in healthy volunteers. Br J Clin Pharmacol. 2002;53:613-628. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 91] [Cited by in RCA: 90] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 75. | Muthukumaraswamy SD, Carhart-Harris RL, Moran RJ, Brookes MJ, Williams TM, Errtizoe D, Sessa B, Papadopoulos A, Bolstridge M, Singh KD, Feilding A, Friston KJ, Nutt DJ. Broadband cortical desynchronization underlies the human psychedelic state. J Neurosci. 2013;33:15171-15183. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 248] [Cited by in RCA: 304] [Article Influence: 25.3] [Reference Citation Analysis (0)] |
| 76. | Carhart-Harris RL, Muthukumaraswamy S, Roseman L, Kaelen M, Droog W, Murphy K, Tagliazucchi E, Schenberg EE, Nest T, Orban C, Leech R, Williams LT, Williams TM, Bolstridge M, Sessa B, McGonigle J, Sereno MI, Nichols D, Hellyer PJ, Hobden P, Evans J, Singh KD, Wise RG, Curran HV, Feilding A, Nutt DJ. Neural correlates of the LSD experience revealed by multimodal neuroimaging. Proc Natl Acad Sci U S A. 2016;113:4853-4858. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 377] [Cited by in RCA: 488] [Article Influence: 54.2] [Reference Citation Analysis (0)] |
| 77. | Kometer M, Pokorny T, Seifritz E, Volleinweider FX. Psilocybin-induced spiritual experiences and insightfulness are associated with synchronization of neuronal oscillations. Psychopharmacology (Berl). 2015;232:3663-3676. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 92] [Cited by in RCA: 109] [Article Influence: 10.9] [Reference Citation Analysis (0)] |
| 78. | Carlson PJ, Singh JB, Zarate CA Jr, Drevets WC, Manji HK. Neural circuitry and neuroplasticity in mood disorders: insights for novel therapeutic targets. NeuroRx. 2006;3:22-41. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 109] [Cited by in RCA: 114] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 79. | Goldstein-Piekarski AN, Williams LM. A neural circuit-based model for depression anchored in a synthesis of insights from functional neuroimaging. In: João Q, André F C, Carlos A Jr Z. Neurobiology of Depression: Road to Novel Therapeutics. Elsevier, 2019: 241-256. |
| 80. | Hamilton JP, Farmer M, Fogelman P, Gotlib IH. Depressive Rumination, the Default-Mode Network, and the Dark Matter of Clinical Neuroscience. Biol Psychiatry. 2015;78:224-230. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 516] [Cited by in RCA: 569] [Article Influence: 56.9] [Reference Citation Analysis (0)] |
| 81. | Sheline YI, Barch DM, Price JL, Rundle MM, Vaishnavi SN, Snyder AZ, Mintun MA, Wang S, Coalson RS, Raichle ME. The default mode network and self-referential processes in depression. Proc Natl Acad Sci U S A. 2009;106:1942-1947. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 942] [Cited by in RCA: 1077] [Article Influence: 67.3] [Reference Citation Analysis (0)] |
| 82. | Nolen-Hoeksema S, Wisco BE, Lyubomirsky S. Rethinking Rumination. Perspect Psychol Sci. 2008;3:400-424. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2624] [Cited by in RCA: 2877] [Article Influence: 287.7] [Reference Citation Analysis (0)] |
| 83. | Berman MG, Peltier S, Nee DE, Kross E, Deldin PJ, Jonides J. Depression, rumination and the default network. Soc Cogn Affect Neurosci. 2011;6:548-555. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 341] [Cited by in RCA: 409] [Article Influence: 27.3] [Reference Citation Analysis (0)] |
| 84. | van Wingen GA, Tendolkar I, Urner M, van Marle HJ, Denys D, Verkes RJ, Fernández G. Short-term antidepressant administration reduces default mode and task-positive network connectivity in healthy individuals during rest. Neuroimage. 2014;88:47-53. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 53] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 85. | Posner J, Hellerstein DJ, Gat I, Mechling A, Klahr K, Wang Z, McGrath PJ, Stewart JW, Peterson BS. Antidepressants normalize the default mode network in patients with dysthymia. JAMA Psychiatry. 2013;70:373-382. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 176] [Cited by in RCA: 198] [Article Influence: 16.5] [Reference Citation Analysis (0)] |
| 86. | Scheidegger M, Walter M, Lehmann M, Metzger C, Grimm S, Boeker H, Boesiger P, Henning A, Seifritz E. Ketamine decreases resting state functional network connectivity in healthy subjects: implications for antidepressant drug action. PLoS One. 2012;7:e44799. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 177] [Cited by in RCA: 197] [Article Influence: 15.2] [Reference Citation Analysis (0)] |
| 87. | Evans JW, Szczepanik J, Brutsché N, Park LT, Nugent AC, Zarate CA Jr. Default Mode Connectivity in Major Depressive Disorder Measured Up to 10 Days After Ketamine Administration. Biol Psychiatry. 2018;84:582-590. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 118] [Cited by in RCA: 125] [Article Influence: 17.9] [Reference Citation Analysis (0)] |
| 88. | Müller F, Dolder PC, Schmidt A, Liechti ME, Borgwardt S. Altered network hub connectivity after acute LSD administration. Neuroimage Clin. 2018;18:694-701. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 95] [Cited by in RCA: 108] [Article Influence: 15.4] [Reference Citation Analysis (0)] |
| 89. | Speth J, Speth C, Kaelen M, Schloerscheidt AM, Feilding A, Nutt DJ, Carhart-Harris RL. Decreased mental time travel to the past correlates with default-mode network disintegration under lysergic acid diethylamide. J Psychopharmacol. 2016;30:344-353. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 61] [Cited by in RCA: 68] [Article Influence: 7.6] [Reference Citation Analysis (0)] |
| 90. | Carhart-Harris RL, Erritzoe D, Williams T, Stone JM, Reed LJ, Colasanti A, Tyacke RJ, Leech R, Malizia AL, Murphy K, Hobden P, Evans J, Feilding A, Wise RG, Nutt DJ. Neural correlates of the psychedelic state as determined by fMRI studies with psilocybin. Proc Natl Acad Sci U S A. 2012;109:2138-2143. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 802] [Cited by in RCA: 656] [Article Influence: 50.5] [Reference Citation Analysis (0)] |
| 91. | Barrett FS, Krimmel SR, Griffiths RR, Seminowicz DA, Mathur BN. Psilocybin acutely alters the functional connectivity of the claustrum with brain networks that support perception, memory, and attention. Neuroimage. 2020;218:116980. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 84] [Cited by in RCA: 109] [Article Influence: 21.8] [Reference Citation Analysis (0)] |
| 92. | Tagliazucchi E, Carhart-Harris R, Leech R, Nutt D, Chialvo DR. Enhanced repertoire of brain dynamical states during the psychedelic experience. Hum Brain Mapp. 2014;35:5442-5456. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 206] [Cited by in RCA: 231] [Article Influence: 21.0] [Reference Citation Analysis (0)] |
| 93. | Pasquini L, Palhano-Fontes F, Araujo DB. Subacute effects of the psychedelic ayahuasca on the salience and default mode networks. 2020 Preprint. Available from: medRxiv:19007542. [DOI] [Full Text] |
| 94. | Palhano-Fontes F, Andrade KC, Tofoli LF, Santos AC, Crippa JA, Hallak JE, Ribeiro S, de Araujo DB. The psychedelic state induced by ayahuasca modulates the activity and connectivity of the default mode network. PLoS One. 2015;10:e0118143. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 255] [Cited by in RCA: 250] [Article Influence: 25.0] [Reference Citation Analysis (0)] |
| 95. | Dos Santos RG, Balthazar FM, Bouso JC, Hallak JE. The current state of research on ayahuasca: A systematic review of human studies assessing psychiatric symptoms, neuropsychological functioning, and neuroimaging. J Psychopharmacol. 2016;30:1230-1247. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 91] [Cited by in RCA: 78] [Article Influence: 8.7] [Reference Citation Analysis (0)] |
| 96. | Carhart-Harris RL, Roseman L, Bolstridge M, Demetriou L, Pannekoek JN, Wall MB, Tanner M, Kaelen M, McGonigle J, Murphy K, Leech R, Curran HV, Nutt DJ. Psilocybin for treatment-resistant depression: fMRI-measured brain mechanisms. Sci Rep. 2017;7:13187. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 217] [Cited by in RCA: 329] [Article Influence: 41.1] [Reference Citation Analysis (0)] |
| 97. | Malykhin NV, Carter R, Seres P, Coupland NJ. Structural changes in the hippocampus in major depressive disorder: contributions of disease and treatment. J Psychiatry Neurosci. 2010;35:337-343. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 146] [Cited by in RCA: 163] [Article Influence: 10.9] [Reference Citation Analysis (0)] |
| 98. | Belleau EL, Treadway MT, Pizzagalli DA. The Impact of Stress and Major Depressive Disorder on Hippocampal and Medial Prefrontal Cortex Morphology. Biol Psychiatry. 2019;85:443-453. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 209] [Cited by in RCA: 350] [Article Influence: 58.3] [Reference Citation Analysis (0)] |
| 99. | Dai L, Zhou H, Xu X, Zuo Z. Brain structural and functional changes in patients with major depressive disorder: a literature review. PeerJ. 2019;7:e8170. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 36] [Cited by in RCA: 70] [Article Influence: 11.7] [Reference Citation Analysis (0)] |
| 100. | Herrmann LL, Le Masurier M, Ebmeier KP. White matter hyperintensities in late life depression: a systematic review. J Neurol Neurosurg Psychiatry. 2008;79:619-624. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 356] [Cited by in RCA: 335] [Article Influence: 19.7] [Reference Citation Analysis (0)] |
| 101. | Dusi N, Barlati S, Vita A, Brambilla P. Brain Structural Effects of Antidepressant Treatment in Major Depression. Curr Neuropharmacol. 2015;13:458-465. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 76] [Cited by in RCA: 80] [Article Influence: 8.0] [Reference Citation Analysis (0)] |
| 102. | Colle R, Dupong I, Colliot O, Deflesselle E, Hardy P, Falissard B, Ducreux D, Chupin M, Corruble E. Smaller hippocampal volumes predict lower antidepressant response/remission rates in depressed patients: A meta-analysis. World J Biol Psychiatry. 2018;19:360-367. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 29] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 103. | Vythilingam M, Vermetten E, Anderson GM, Luckenbaugh D, Anderson ER, Snow J, Staib LH, Charney DS, Bremner JD. Hippocampal volume, memory, and cortisol status in major depressive disorder: effects of treatment. Biol Psychiatry. 2004;56:101-112. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 342] [Cited by in RCA: 327] [Article Influence: 15.6] [Reference Citation Analysis (0)] |
| 104. | Zhou YL, Wu FC, Liu WJ, Zheng W, Wang CY, Zhan YN, Lan XF, Ning YP. Volumetric changes in subcortical structures following repeated ketamine treatment in patients with major depressive disorder: a longitudinal analysis. Transl Psychiatry. 2020;10:264. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 20] [Cited by in RCA: 37] [Article Influence: 7.4] [Reference Citation Analysis (0)] |
| 105. | Catlow BJ, Song S, Paredes DA, Kirstein CL, Sanchez-Ramos J. Effects of psilocybin on hippocampal neurogenesis and extinction of trace fear conditioning. Exp Brain Res. 2013;228:481-491. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 122] [Cited by in RCA: 183] [Article Influence: 15.3] [Reference Citation Analysis (0)] |
| 106. | Bouso JC, Palhano-Fontes F, Rodríguez-Fornells A, Ribeiro S, Sanches R, Crippa JA, Hallak JE, de Araujo DB, Riba J. Long-term use of psychedelic drugs is associated with differences in brain structure and personality in humans. Eur Neuropsychopharmacol. 2015;25:483-492. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 112] [Cited by in RCA: 135] [Article Influence: 13.5] [Reference Citation Analysis (0)] |
| 107. | Dalgleish T, Watts FN. Biases of attention and memory in disorders of anxiety and depression. Clin Psychol Rev. 1990;10:589-604. [RCA] [DOI] [Full Text] [Cited by in Crossref: 242] [Cited by in RCA: 211] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 108. | Mathews A, MacLeod C. Cognitive approaches to emotion and emotional disorders. Annu Rev Psychol. 1994;45:25-50. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 617] [Cited by in RCA: 553] [Article Influence: 17.8] [Reference Citation Analysis (0)] |
| 109. | Segerstrom SC, Tsao JCI, Alden LE, Craske MG. Worry and rumination: Repetitive thought as a concomitant and predictor of negative mood. Cognit Ther Res. 2000;24:671-88. [DOI] [Full Text] |
| 110. | Kupferberg A, Bicks L, Hasler G. Social functioning in major depressive disorder. Neurosci Biobehav Rev. 2016;69:313-332. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 296] [Cited by in RCA: 414] [Article Influence: 46.0] [Reference Citation Analysis (0)] |
| 111. | Pringle A, Harmer CJ. The effects of drugs on human models of emotional processing: an account of antidepressant drug treatment. Dialogues Clin Neurosci. 2015;17:477-487. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 24] [Cited by in RCA: 23] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 112. | Harmer CJ, Shelley NC, Cowen PJ, Goodwin GM. Increased positive vs negative affective perception and memory in healthy volunteers following selective serotonin and norepinephrine reuptake inhibition. Am J Psychiatry. 2004;161:1256-1263. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 390] [Cited by in RCA: 400] [Article Influence: 19.0] [Reference Citation Analysis (0)] |
| 113. | Reed JL, Nugent AC, Furey ML, Szczepanik JE, Evans JW, Zarate CA Jr. Ketamine normalizes brain activity during emotionally valenced attentional processing in depression. Neuroimage Clin. 2018;20:92-101. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 34] [Cited by in RCA: 56] [Article Influence: 8.0] [Reference Citation Analysis (0)] |
| 114. | Kometer M, Schmidt A, Bachmann R, Studerus E, Seifritz E, Vollenweider FX. Psilocybin biases facial recognition, goal-directed behavior, and mood state toward positive relative to negative emotions through different serotonergic subreceptors. Biol Psychiatry. 2012;72:898-906. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 168] [Cited by in RCA: 210] [Article Influence: 16.2] [Reference Citation Analysis (0)] |
| 115. | Dolder PC, Schmid Y, Müller F, Borgwardt S, Liechti ME. LSD Acutely Impairs Fear Recognition and Enhances Emotional Empathy and Sociality. Neuropsychopharmacology. 2016;41:2638-2646. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 144] [Cited by in RCA: 177] [Article Influence: 19.7] [Reference Citation Analysis (0)] |
| 116. | Barrett FS, Doss MK, Sepeda ND, Pekar JJ, Griffiths RR. Emotions and brain function are altered up to one month after a single high dose of psilocybin. Sci Rep. 2020;10:2214. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 86] [Cited by in RCA: 208] [Article Influence: 41.6] [Reference Citation Analysis (0)] |
| 117. | Watts R, Day C, Krzanowski J, Nutt D, Carhart-Harris R. Patients’ Accounts of Increased “Connectedness” and “Acceptance” After Psilocybin for Treatment-Resistant Depression. J Humanist Psychol. 2017;57:520-564. [RCA] [DOI] [Full Text] [Cited by in Crossref: 179] [Cited by in RCA: 181] [Article Influence: 22.6] [Reference Citation Analysis (0)] |
| 118. | Roseman L, Nutt DJ, Carhart-Harris RL. Quality of Acute Psychedelic Experience Predicts Therapeutic Efficacy of Psilocybin for Treatment-Resistant Depression. Front Pharmacol. 2017;8:974. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 243] [Cited by in RCA: 444] [Article Influence: 63.4] [Reference Citation Analysis (0)] |
| 119. | Griffiths RR, Richards WA, McCann U, Jesse R. Psilocybin can occasion mystical-type experiences having substantial and sustained personal meaning and spiritual significance. Psychopharmacology (Berl). 2006;187:268-83; discussion 284. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 728] [Cited by in RCA: 787] [Article Influence: 41.4] [Reference Citation Analysis (0)] |
| 120. | Mahan AL, Ressler KJ. Fear conditioning, synaptic plasticity and the amygdala: implications for posttraumatic stress disorder. Trends Neurosci. 2012;35:24-35. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 393] [Cited by in RCA: 428] [Article Influence: 30.6] [Reference Citation Analysis (0)] |