Published online Jan 19, 2021. doi: 10.5498/wjp.v11.i1.13
Peer-review started: October 23, 2020
First decision: December 4, 2020
Revised: December 16, 2020
Accepted: December 27, 2020
Article in press: December 27, 2020
Published online: January 19, 2021
Processing time: 79 Days and 18.7 Hours
Social engagement-important for health and well-being-can be difficult for people with schizophrenia. Past research indicates that despite expressing interest in social interactions, people with schizophrenia report spending less time with others and feeling lonely. Social motivations and barriers may play an important role for understanding social engagement in schizophrenia.
To investigate how people with schizophrenia describe factors that impede and promote social engagement.
We interviewed a community sample of people with (n = 35) and without (n = 27) schizophrenia or schizoaffective disorder about their social interactions with friends and family over the past week and planned social activities for the coming week. We reviewed the interview transcripts and developed a novel coding system to capture whether interactions occurred, who had initiated the contact, and frequency of reported social barriers (i.e., internal, conflict-based, logistical) and social motivations (i.e., instrumental, affiliative, obligation-based). We also assessed symptoms and functioning.
People with schizophrenia were less likely than people without schizophrenia to have spent time with friends [t (51.04) = 2.09, P = 0.042, d = 0.51)], but not family. People with schizophrenia reported more social barriers than people without schizophrenia [F (1, 60) = 10.55, P = 0.002, ηp2 = 0.15)] but did not differ in reported social motivations. Specifically, people with schizophrenia reported more internal [t (45.75) = 3.40, P = 0.001, d = 0.83)] and conflict-based [t (40.11) = 3.03, P = 0.004, d = 0.73)] barriers than people without schizophrenia. Social barriers and motivations were related to real-world social functioning for people with schizophrenia, such that more barriers were associated with more difficulty in close relationships (r = -0.37, P = 0.027) and more motivations were associated with better community functioning (r = 0.38, P = 0.024).
These findings highlight the importance of assessing first person accounts of social barriers and motivations to better understand social engagement in schizophrenia.
Core Tip: We examined factors that may impede and promote social engagement in schizophrenia. We coded social barriers and motivations from transcribed negative symptoms interviews. We found that barriers, such as conflicts with other people or negative beliefs about the self, were prominent in schizophrenia. Interestingly, when explicitly prompted, people with schizophrenia reported interest in and motivation for social interactions. Nevertheless, social barriers may get in the way of them following through.
- Citation: Weittenhiller LP, Mikhail ME, Mote J, Campellone TR, Kring AM. What gets in the way of social engagement in schizophrenia? World J Psychiatr 2021; 11(1): 13-26
- URL: https://www.wjgnet.com/2220-3206/full/v11/i1/13.htm
- DOI: https://dx.doi.org/10.5498/wjp.v11.i1.13
Social engagement is a central part of life and is linked to many benefits, such as wellbeing, health, and longevity[1]. Unfortunately, limited social engagement is common in schizophrenia[2] and people with schizophrenia often miss out on the benefits of such engagement. In this study, we sought to determine contributing factors to limited social engagement in schizophrenia. Specifically, we examined how people with and without schizophrenia talk about their social engagement with friends and family to better understand factors that motivate such engagement and barriers that might get in the way.
Why might people with schizophrenia engage in fewer social interactions? Limited social engagement may be indicative of social disinterest[3]. Indeed, people with schizophrenia report spending less time around others and set fewer social goals compared to people without schizophrenia[4-6]. However, other evidence indicates that people with schizophrenia describe social relationships as equally important[7,8] and express as much interest in social activity compared to people without schizophrenia[4,9]. Moreover, people with schizophrenia report a similar or even greater preference to be with others as those without schizophrenia when they find themselves alone[10,11]. People with schizophrenia also express more social interest than those with other psychiatric illnesses[12]. Even as people with schizophrenia profess an interest in social interactions, they also report feeling lonely[5,13-15], suggesting they have social needs that are not being met. Insofar as diminished interest does not fully account for limited social engagement in schizophrenia, we sought to examine other possible barriers. Understanding what might get in the way of social engagement in schizophrenia can be an important first step toward helping people with schizophrenia obtain the myriad benefits of social interactions.
Barriers that may interfere with social engagement in schizophrenia include internal states, conflicts with others, or logistical factors. Prior research has identified several possible internal barriers in schizophrenia, including low self-esteem, internalized stigma, and defeatist performance beliefs[16-19]. Symptoms may also interfere with social engagement: Greater positive symptoms are associated with lower relationship satisfaction[20], and greater negative symptoms are associated with smaller social network sizes[21,22].
Conflicts with others, whether in the form of disagreements, social discrimination, or stigma-related rejection, may also interfere with social engagement. For example, families with a person with schizophrenia report more frequent arguments and heightened tension than other families[23]. People with schizophrenia are often reluctant to disclose their illness to friends, fearing that once they do, they will be rejected[24].
Logistical barriers, such as limited financial means, may also get in the way of social engagement. People with schizophrenia are more likely to be unemployed[25], which could restrict social network size and variety[26]. Social activities that require money or transportation may also be less accessible[27].
Considering what motivates people to form and maintain relationships is also important for understanding social engagement. Some motivations for relationships are instrumental, arising from a desire for social activity to acquire tangible benefits[28,29]. In this way, relationships are a means to an end. As caregivers of people with schizophrenia are at times responsible for meeting various needs of their loved ones[30], the desire for assistance may be a motivation for social engagement.
Alternatively, social relationships can be motivating in and of themselves[29,31]. Affiliative motivations focus on companionship, mutual care, and the exchange of emotions as drivers of engagement with others. People with schizophrenia report wanting social relationships and even consider them a primary source of meaning[32], suggesting that affiliative motivations are an important aspect of social engagement. Another type of social motivation is obligation-based, which refers to the desire to meet personally or societally determined standards of appropriate social behavior[33], or how a person “should” behave. Because it is considered normative to have relationships, people with schizophrenia report this as an important indication of health[34].
How people with schizophrenia describe their social experiences can offer a window into social barriers and motivations and provide an important perspective for understanding social engagement. Of the few studies in schizophrenia that have used such an approach, most have focused on lexical characteristics of speech, linguistic abnormalities, word counts, or speech coherence and appropriateness[35-40]. A notable exception is the work of Lysaker et al[41], who assessed social worth, social closeness, and personal agency in spoken narratives of people with schizophrenia. The more frequently people with schizophrenia referred to these social themes in their narratives, the better their social functioning.
We sought to answer four questions about social engagement in schizophrenia. First, we asked whether people with and without schizophrenia differed in the frequency and initiation of interactions with family and friends in the past week. Second, we asked whether people with and without schizophrenia differed in reported types of social barriers and motivations. Third, we asked whether social barriers and motivations differed by relationship type (friends, family). Fourth, we asked whether social barriers and motivations were related to functioning and symptoms for people with schizophrenia.
Thirty-five people with schizophrenia (n = 26) or schizoaffective disorder (n = 9) and 27 people without a schizophrenia spectrum disorder participated. People with schizophrenia and schizoaffective disorder did not differ from one another on any demographic, clinical, or coded variable; we collapsed across these groups for analyses. Participants were recruited from board and care homes, nonprofit agencies, and Craigslist and were part of the multi-site study that developed the Clinical Assessment Interview for Negative Symptoms[42]. The data presented here do not overlap with that study.
Diagnoses were confirmed using the Structured Clinical Interview for DSM-IV Axis I Disorders (SCID-I/P)[43]. For controls, we administered the SCID non-patient version (SCID-I/NP)[44] to confirm absence of schizophrenia spectrum disorders. Any participant with a history of head injury or neurological disorder, a current mood episode, or substance use disorder within the past six months was not invited to participate. All participants provided written informed consent. As shown in Table 1, the groups did not differ in age, sex, race, marital status, education, or estimated intelligence quotient (measured by the Wechsler Test of Adult Reading[45]).
| Schizophrenia | Control | |
| Age (in year) | 45.20 (10.96) | 45.11 (8.51) |
| Sex, n (%) | 12 Female (34.3) | 10 Female (37.0) |
| Race, n (%) | ||
| White | 18 (51.4) | 8 (29.6) |
| Black | 9 (25.7) | 10 (37.0) |
| Asian | 2 (5.7) | 3 (11.1) |
| Pacific Islander | 1 (2.9) | 0 (0) |
| Multiracial | 2 (5.7) | 15 (8.5) |
| Ethnicity: Hispanic/Latino, n (%) | 3 (8.6) | 4 (14.8) |
| Education (in year) | 14.32 (2.80) | 14.96 (2.79) |
| Employed, n (%) | 16 (45.7) | 15 (55.6) |
| Marital status | ||
| Married | 14.3% | 29.6% |
| Widowed | 2.9% | 0% |
| Divorced/Separated | 17.1% | 22.2% |
| Never married | 65.7% | 44.4% |
| Unknown | 0% | 3.7% |
| Percent employed | 45.7% | 55.6% |
| WTAR | 104.12 (15.18) | 102.67 (12.45) |
| Diagnosis | Schizophrenia: 74.3% | -- |
| Schizoaffective: 25.7% | ||
| Duration of illness (in year) | 22.52 (12.42) | -- |
| BPRS | 46.03 (11.81) | -- |
| RFS | ||
| Working productivity | 4.43 (2.12) | -- |
| Independent living skills | 5.37 (1.57) | -- |
| Immediate social network | 5.20 (1.62) | -- |
| Extended social network | 4.37 (1.94) | -- |
| CAINS-EXP | 1.21 (0.82) | 0.56 (0.59) |
| CAINS-MAPa | 1.87 (0.71) | 1.00 (0.68) |
Clinical Assessment Interview for Negative Symptoms beta version: Trained raters administered the beta version of the Clinical Assessment Interview for Negative Symptoms (CAINS), and the interviews were videotaped. The CAINS includes several manualized open-ended probes for each item with additional questions asked as needed for clarity. The CAINS-beta differs from the final CAINS[46] in length (16 rather than 13 items) and in the inclusion of separate questions about romantic relationships.
We examined responses to the first five items of the CAINS-beta. The first three items assessed social motivation and enjoyment in (1) family; (2) romantic relationships; and (3) friendships. Participants were asked to describe their social interactions over the preceding week (e.g., Have you been motivated to be around or in touch with your family/partner/friends in the past week?). The fourth item asked participants to describe pleasure experienced in past week social activities (e.g., Did you have any enjoyable interactions with other people?), and the fifth item asked about expected pleasure from social activities over the next week (e.g., What do you think you will enjoy doing in the next week with other people?).
Interview coding: Interviews were transcribed and coded by trained research assistants. We developed a coding manual containing definitions and examples for all variables, and four raters, blind to diagnostic status, did the coding. A different rater reviewed all data for entry accuracy and coding manual adherence.
Mirroring the final CAINS[46], marital relationships were included with family items, and dating relationships were included with friend items. For friends and family, coders rated “whether any interaction had occurred” over the past week—including phone calls, text messages, e-mails, or in-person contact—dichotomously (present, absent). When an interaction was reported, “initiation” was coded on a 3-point scale: (1) Social partner(s) initiated all interactions; (2) Participant initiated some and social partner initiated some; and (3) Participant initiated all interactions.
Coders determined which type of social barrier or motivation a statement referred to and then computed the total number of social barriers and motivations of each type. Social barriers were defined as causing an interaction to be cut short or to not occur at all. Coders counted the frequencies of three types of barriers. Internal barriers included psychological states and beliefs that prevented interaction, including negative self-perceptions or self-stigma (e.g., “No one would want to be my friend”), psychiatric symptoms, negative beliefs about social interactions (e.g., “People just let you down”), and having goals or priorities that took precedence over social interaction (e.g., “I want to finish my degree before I look for a relationship”). Conflict-based barriers included discrimination (e.g., “My parents disowned me because I’m gay”), rejection (e.g., “She said she didn’t want to date anymore”), and social conflict (e.g., “All we ever do is fight”). Logistical barriers referred to geographic distance, lack of time, mismatched schedules, non-psychiatric illness, lack of financial resources, or perceived lack of access to an appropriate social partner.
Coders also computed the frequencies of three types of social motivations. Instrumental motivations included tangible benefits (e.g., a relative paying for rent) and perceived benefits to a participant’s physical or mental wellbeing or personal development (e.g., “She keeps me sane”). Affiliative motivations included positive attributes of interaction partners (e.g., “He’s funny”), social support, acceptance of self (e.g., “I feel like I can be myself around them”), physical intimacy, and avoidance of loneliness and social isolation. Obligation-based motivations included a desire to provide something to an interaction partner (e.g., “I want to be a positive role model for my sister”), or expectations of normative behavior (e.g., “I called my friend on her birthday because it is the polite thing to do”). Finally, we counted the total number of words participants uttered using the Linguistic Inquiry and Word Count program[47].
Clinical ratings: We measured functioning using the Role Functioning Scale[48] with its 1 (minimal functioning) to 7 (optimal functioning) point scale. The Role Functioning Scale contains four subscales—working productivity, independent living and self-care, immediate social network relationships, and extended social network relationships. We assessed symptoms using a 24-item version of the Brief Psychiatric Rating Scale rated on a 7-point scale[49].
We conducted independent samples t-tests and chi-square tests to compare demographics, word count, contact, and initiation. For barriers and motivations, we conducted 2 Group (schizophrenia, control) X 2 Relationship Type (family, friends) X 3 Barrier (internal, logistical, conflict-based) or Motivation Type (instrumental, affiliative, obligation-based) mixed effect analyses of variance. Sphericity violations were Greenhouse-Geisser corrected; effect sizes are reported as Cohen’s d and partial eta squared (ηp2). We computed Pearson correlations between barriers, motivations, functioning, and symptoms within the schizophrenia group.
Two coders rated a third of interviews (equal numbers of people with and without schizophrenia) to assess inter-rater agreement. Coders achieved a high rate of agreement, with intraclass correlations[50] ranging from 0.83-1.00.
People with (M = 1652.66, SD = 958.25) and without (M = 1348.08, SD = 926.58) schizophrenia did not differ significantly in the amount of words spoken during the interview [t (59) = 1.25, P = 0.22, d = 0.32)]. Thus, any group differences in coded barriers and motivations were not a function of fewer words uttered by either group. We also found no significant differences between men and women for any variable, and thus we collapsed across sex for subsequent analyses.
Both groups were just as likely to have interacted with family over the past week, but people with schizophrenia were less likely to have interacted with friends compared to controls, [t (51.04) = 2.09, P = 0.042, d = 0.51]. People with schizophrenia were no more likely to be living with family than those without schizophrenia [t (59) = -0.96, P = 0.34, d = 0.25)], suggesting that greater ease of access did not contribute to rates of reported family interactions for the schizophrenia group. When interactions did occur, the groups were equally likely to have initiated interactions with family. However, people with schizophrenia were less likely to have initiated interactions with friends, [t (46) = 2.75, P = 0.008, d = 0.80].
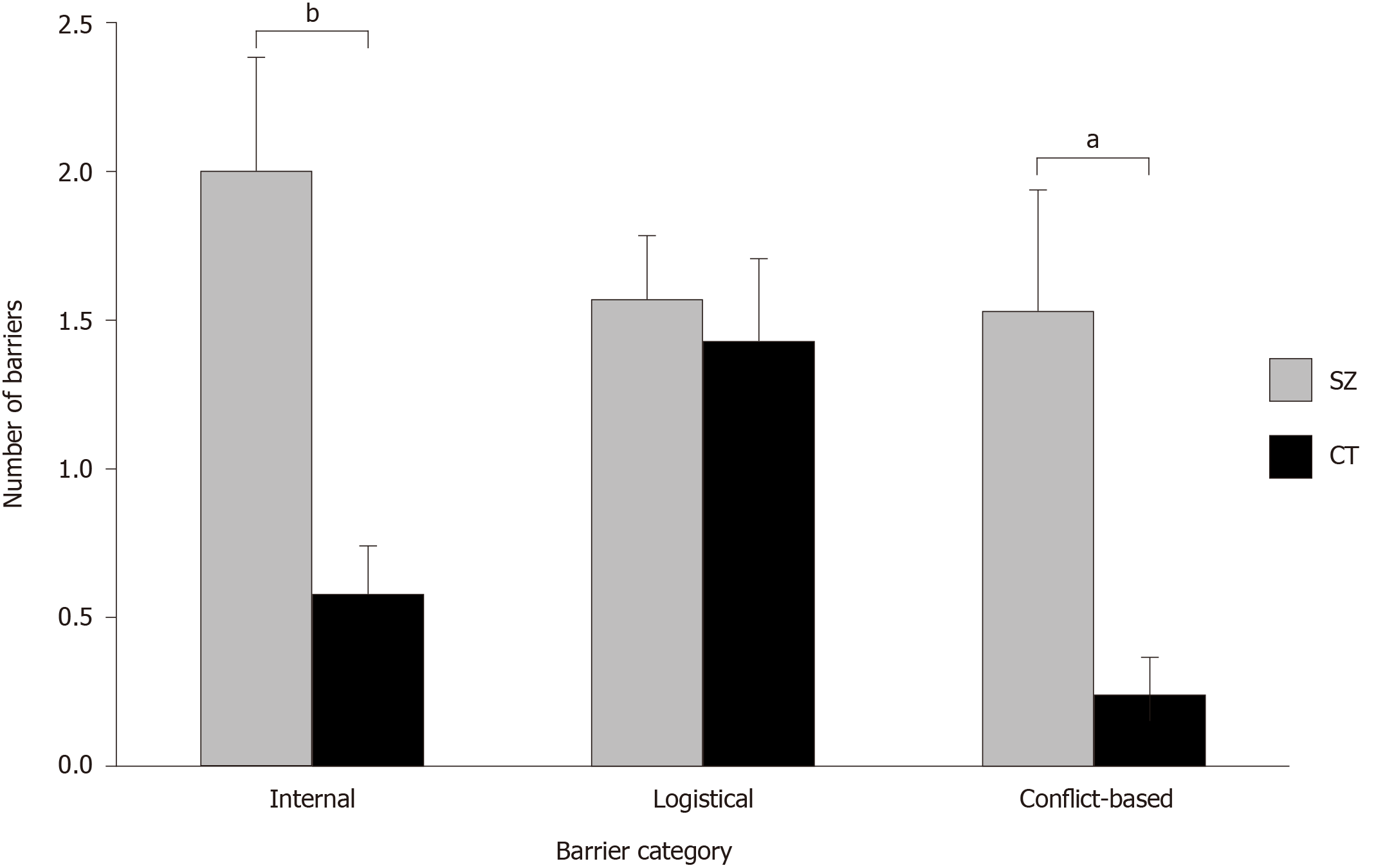
We found a significant group main effect [F (1, 60) = 10.55, P = 0.002, ηp2 = 0.15)], indicating that people with schizophrenia reported more barriers overall than people without schizophrenia (see Table 2). However, the Group X Barrier Type interaction was also significant [F (2, 120) = 3.27, P = 0.041, ηp2 = 0.05)], indicating that the group differences depended upon barrier type. As shown in Figure 1, people with schizophrenia reported more internal [t (45.75) = 3.40, P = 0.001, d = 0.83) and conflict-based barriers [t (40.11) = 3.03, P = 0.004, d = 0.73)] than people without schizophrenia; the groups did not differ in reported logistical barriers.
| Schizophrenia | Control | P value | Cohen’s d | |
| Contact | 1.84 (0.23) | 1.93 (0.18) | 0.09 | 0.43 |
| Initiation | 1.75 (0.66) | 2.03 (0.66) | 0.11 | 0.42 |
| Barriers | ||||
| Internal | 2.00 (2.28) | 0.57 (0.86) | 0.001 | 0.83 |
| Logistical | 1.57 (1.26) | 1.43 (1.46) | 0.68 | 0.11 |
| Conflict-based | 1.53 (2.40) | 0.24 (0.64) | 0.004 | 0.73 |
| Motivations | ||||
| Instrumental | 0.90 (1.10) | 0.69 (0.91) | 0.41 | 0.21 |
| Affiliative | 8.27(5.67) | 8.98 (4.15) | 0.59 | 0.14 |
| Obligation-based | 3.09 (4.57) | 3.39 (4.06) | 0.79 | 0.07 |
We also found a significant relationship type main effect [F (1, 60) = 10.35, P = 0.002, ηp2 = 0.15)], indicating that all participants reported more barriers for friends than family [t (61) = 3.36, P = 0.001, d = 0.43)]. However, this was qualified by a significant Relationship Type X Barrier Type interaction [F (2, 120) = 3.78, P = 0.026, ηp2 = 0.06)]. As shown in Table 3, whereas logistical and conflict-based barriers were similar across friends and family, all participants reported more internal barriers for friends than for family [t (61) = 4.10, P < 0.001, d = 0.52)].
| Friends | Family | P value | Cohen’s d | |
| Barriers | ||||
| Internal | 1.09 (1.60) | 0.29 (0.69) | 0.001 | 0.52 |
| Logistical | 0.85 (1.02) | 0.65 (0.91) | 0.26 | 0.15 |
| Conflict-based | 0.52 (1.55) | 0.44 (0.81) | 0.68 | 0.05 |
| Motivations | ||||
| Instrumental | 0.51 (0.67) | 0.30 (0.64) | 0.048 | 0.26 |
| Affiliative | 4.82 (3.25) | 3.76 (3.05) | 0.037 | 0.28 |
| Obligation-based | 0.38 (0.66) | 0.55 (0.78) | 0.23 | 0.15 |
Neither the group main effect [F (1, 60) = 0.17, P = 0.68, ηp2 = 0.003)], nor the Group X Motivation Type interaction were significant [F (1, 60) = 1.92, P = 0.17, ηp2 = 0.03)]. However, the motivation type main effect was significant [F (1.10, 65.89) = 143.42, P < 0.001, ηp2 = 0.71)]; all participants reported more affiliative than instrumental [t (61) = 12.07, P < 0.001, d = 1.53)] or obligation-based [t (61) = 8.36, P < 0.001, d = 1.06)] motivations (see Table 2). In addition, participants reported more obligation-based than instrumental motivations [t (61) = 4.14, P < 0.001, d = 0.53)].
This finding was qualified by a significant Relationship Type X Motivation Type interaction [F (1.19, 71.41) = 4.14, P = 0.039, ηp2 = 0.07)]. Whereas obligation-based motivations were similar across friends and family, all participants reported more instrumental [t (61) = 2.02, P = 0.048, d = 0.26)] and affiliative motivations [t (61) = 2.14, P = 0.037, d = 0.28)] for friends than for family.
As shown in Table 4, barriers and motivations were significantly associated with functioning. Internal and conflict-based barriers were moderately, negatively correlated with independent living skills, indicating that the more difficulties people with schizophrenia experienced with self-care, the greater the number of internal and conflict-based barriers they reported. More logistical barriers were associated with greater difficulties with close others. Motivations were moderately related to social functioning; in particular, more affiliative motivations were associated with significantly better social functioning within the broader community.
| Barriers | Motivations | |||||
| Internal | Logistical | Conflict-based | Instrumental | Affiliative | Obligation-based | |
| Role Functioning Scale | ||||||
| Working productivity | 0.03 | 0.13 | -0.20 | -0.01 | 0.23 | 0.06 |
| Independent living/self-care | -0.36a | 0.02 | -0.43b | -0.08 | -0.26 | -0.22 |
| Immediate social network | -0.16 | -0.37a | -0.18 | -0.08 | 0.01 | -0.16 |
| Extended social network | -0.18 | 0.12 | -0.20 | -0.10 | 0.38a | 0.22 |
| BPRS | 0.25 | -0.14 | 0.50b | 0.20 | -0.03 | -0.001 |
Interestingly, only conflict-based barriers were significantly related to total symptoms (but not negative or positive symptoms separately), suggesting that other types of barriers/motivations may be somewhat independent of symptom severity.
We investigated reported barriers to and motivations for social engagement in people with and without schizophrenia. Despite describing social engagement with the same number of words, people with schizophrenia reported more social barriers than those without schizophrenia, yet just as many social motivations. Importantly, social barriers and motivations were also related to functioning. Our findings suggest that particular types of social barriers and motivations may impede social engagement for people with schizophrenia and impact real-world social behavior, and they provide valuable information on directions for improving social engagement.
Consistent with previous research[51], we found that people with schizophrenia were less likely to have interacted with or initiated contact with friends over the past week compared to controls. However, we found no differences in contact or initiation with family. These findings are clinically important, as frequency of contact with friends is more predictive of clinical recovery than contact with family[52]. Moreover, evidence suggests that people with schizophrenia lose connections with close friends early in the course of illness[51], which may contribute to limited social engagement over the illness course[53].
Compared to controls, people with schizophrenia reported experiencing more internal barriers and conflict-based barriers. These findings are consistent with evidence that people with psychotic disorders feel less at ease and more threatened while in the company of others compared to people without psychotic disorders[11]. It is possible that people with schizophrenia are more sensitive to perceiving negativity in social encounters; however, it is also possible that negative attitudes are borne from actual social rejection.
Although speculative, conflict-based barriers may be associated with stigma-based rejection. Heightened discrimination and rejection that people with schizophrenia face may perpetuate negative beliefs about social interactions, resulting in a cycle of negative social experiences. It would be helpful for future work to explore the origins and bidirectional causality of conflicts involving people with schizophrenia. Impairments in social cognitive processes (e.g., social cue perception, empathy), which we did not assess, could make resolving disagreements more challenging for people with schizophrenia[54]. Examining linkages between social barriers and stigma-based rejection is an important direction for future research.
Both groups reported more barriers to interactions with friends than with family, and this was particularly evident for internal barriers. Friendships are inherently more difficult since they are not “built in” and thus require more effort to establish and maintain. Family members may reach out frequently even if their loved one has negative beliefs about interactions. By contrast, friends may not put in this effort. Coupled with our finding that people with schizophrenia were less likely to interact with friends and also that barriers were more common for interactions with friends, it seems especially important to study friendships in future studies.
Interestingly, we found that people with schizophrenia reported being comparably motivated for friend and family interactions as people without schizophrenia. This finding may seem at odds with other studies indicating that people with schizophrenia have deficits in social motivation[55-57]. Two methodological differences may account for this discrepancy. First, similar to Gard et al[4], we asked people to report on their actual, “real-life” social interactions over the past week following several guided prompts. By contrast, laboratory studies of social motivation use tasks of simulated social interactions. Second, we coded actual behavior (e.g., went to dinner with family) as well as articulated motives (e.g., reported desire to see family). This approach differs from studies of effort expenditure[56,58] that focus on behavioral action. It will be informative in future studies to examine social motivations using a variety of approaches, such as ecological momentary assessment, passive mobile data collection, or virtual reality techniques[59]. Moreover, it will be essential to replicate this finding with a larger sample, as social motivation difficulties, like any deficit in schizophrenia, are not observed in all people with the diagnosis.
We found that both groups reported more affiliative and instrumental motivations for friendships than family relationships, which is noteworthy since people with schizophrenia were less likely to have had contact with friends. That is, people with schizophrenia reported being motivated to interact with friends for affiliative and instrumental reasons as much as controls, yet they were less likely to have done so over the past week. This finding highlights an important disconnect between reported interest and actual behavior for people with schizophrenia[59-61]. Although experiencing motivation for friendships may provide entry to important support that comes from friendships[62-65], receipt likely requires contact with friends. Understanding how internal or conflict-based social barriers can be reduced will likely help increase contact and benefits from friends.
We also found that barriers and motivations were associated with real-world functioning for people with schizophrenia. Because navigating the social world is important for autonomous living, conflict-based barriers, such as stigma and rejection, may make it more challenging for people with schizophrenia to maneuver bureaucratic systems or manage shopping or transportation. Similarly, internal barriers, like negative beliefs about the self, may be detrimental to the self-efficacy necessary to pursue independent living[66].
Encouragingly, we found no group differences in reported logistical barriers, perhaps because the groups did not differ in education or employment status. Nevertheless, for people with schizophrenia, logistical barriers were associated with functioning in close relationships. Although finances are but one type of logistical barrier, limited means can make it more difficult for people with schizophrenia to afford social activities or access transportation. Relatedly, unemployment[25] or lessened community integration[67] may make it challenging to get in touch with or visit other people.
The more that people with schizophrenia were motivated by the interpersonal aspects of relationships, the better their functioning in wider spheres of social contact such as clubs, churches, or social recreational activities. Perhaps people who value the relational aspects of social interactions seek out more opportunities for contact with members of their communities. Given the cross-sectional and correlational nature of our data, however, it is impossible to assess directionality. Nevertheless, social integration in different spheres is an important predictor of quality of life[18].
Fortunately, many of the barriers that we have identified are already the targets of current treatments. For example, internal barriers, such as negative beliefs about relationships, have been targeted in Cognitive Behavioral Therapy for negative symptoms. Cognitive Behavioral Social Skills Training’s[68,69] emphasis on communication and assertiveness skills and family therapy’s focus on problem solving may assist with conflict-based barriers[70].
Although these findings provide an important step towards understanding what hinders and helps people with schizophrenia build social engagement, they should be considered in the context of limitations. First, our assessment of barriers and motivations was limited to participants’ responses to the CAINS. Because specific barriers or motivations were not asked about explicitly, we may have undercounted, and we may not have captured all types of barriers (e.g., social anxiety). Nevertheless, the CAINS includes more questions about social interactions than most clinical interviews, and thus the corpus of reported social engagement was richer than it might have been with a different interview.
Second, although we assessed the presence of barriers and motivations, we did not assess their relative contributions to impeding social engagement. For instance, although geographic distance (logistical barrier) and negative beliefs (internal barrier) may have been reported, it is possible that the negative beliefs were more impeding than distance. Third, the CAINS assessed the preceding and upcoming week, thus limiting the time period for reporting on social engagement. On the other hand, the strength of this approach is that it reduced difficulties and biases associated with retrospective reports. Fourth, all participants were taking antipsychotic medication so we cannot ascertain what, if any, impact medications may have had on participant responses. Finally, we did not assess related constructs, such as social network size, and thus future studies would benefit from investigating these alongside motivations and barriers to better understand the relationships between them.
In summary, we found that people with schizophrenia were less likely to interact with and initiate contact with friends compared to people without schizophrenia even as they did not differ in contact with family. Our findings suggest that certain types of social barriers get in the way of social engagement in schizophrenia, including barriers involving the self and conflicts with others. Importantly, social barriers and motivations were also related to real world functioning, suggesting that asking people to describe their social lives is linked to independent assessments of functioning. Together, our approach illustrates the benefits of simply asking people to describe their social lives and suggests that efforts to help mitigate social barriers might improve social engagement.
Though limited social engagement is common in schizophrenia, the reasons for this remain unclear. People with schizophrenia report a desire to be with others, and yet spend more time alone.
Better understanding of the factors that contribute to limited social engagement can be an important first step toward helping people with schizophrenia to meet their social needs.
To identify and compare motivations and barriers for social engagement with friends and family among those with and without schizophrenia.
Thirty-five people with schizophrenia or schizoaffective disorder and 27 nonclinical controls were recruited from the community to participate in this study. Participants completed measures of symptoms and functioning, as well as a negative symptoms interview, which asked participants to describe their engagement in and motivation for social activities in the past and upcoming weeks. Using a novel coding system, we coded the frequency with which participants described six types of social motivations and barriers.
People with schizophrenia were less likely to interact with and initiate contact with friends, but not family, compared to nonclinical controls. The groups differed in reported barriers, such that people with schizophrenia reported more internal and conflict-based barriers than those without schizophrenia. People with and without schizophrenia reported similar numbers and types of motivations for social engagement. Barriers and motivations were associated with symptoms and functioning.
This study suggests that barriers, such as conflicts with other people or negative beliefs about the self may interfere with social engagement in schizophrenia. People with schizophrenia report interest and motivation for social interactions, but social barriers may get in the way of them following through.
Further exploration of social barriers in terms of types, frequency, and relative contribution to limiting social engagement is warranted.
The authors thank research assistants Apoorva Polisetty, Gregory Devine, Dania Smithstein, and Iliana Lopez Yanez, who helped with coding, and Gillian Chen, Renata Botello, Anna Deal, Janae Spinato, Alexandria Tu, Maryanna Winslow, and Alexandra Jensen, who helped with interview transcription. We also thank the people who chose to participate in this study.
Manuscript source: Unsolicited manuscript
Corresponding Author's Membership in Professional Societies: The Society for Affective Science; Society for Research in Psychopathology; and Society for Personality and Social Psychology.
Specialty type: Psychology
Country/Territory of origin: United States
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Khan MM S-Editor: Zhang L L-Editor: A P-Editor: Li JH
| 1. | Holt-Lunstad J, Smith TB, Baker M, Harris T, Stephenson D. Loneliness and social isolation as risk factors for mortality: a meta-analytic review. Perspect Psychol Sci. 2015;10:227-237. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2370] [Cited by in RCA: 2946] [Article Influence: 294.6] [Reference Citation Analysis (0)] |
| 2. | Hooley JM, Blaney PH, Krueger RF, Millon T. Social functioning and schizophrenia. Blaney PH, Krueger RF, Millon T. Oxford textbook of psychopathology. 3rd ed. New York: Oxford University Press 2015; 353-382. |
| 3. | Kirkpatrick B, Fenton WS, Carpenter WT, Marder SR. The NIMH-MATRICS consensus statement on negative symptoms. Schizophr Bull. 2006;32:214-219. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 849] [Cited by in RCA: 968] [Article Influence: 50.9] [Reference Citation Analysis (0)] |
| 4. | Gard DE, Sanchez AH, Cooper K, Fisher M, Garrett C, Vinogradov S. Do people with schizophrenia have difficulty anticipating pleasure, engaging in effortful behavior, or both? J Abnorm Psychol. 2014;123:771-782. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 91] [Cited by in RCA: 118] [Article Influence: 10.7] [Reference Citation Analysis (0)] |
| 5. | Kasanova Z, Oorschot M, Myin-Germeys I. Social anhedonia and asociality in psychosis revisited. An experience sampling study. Psychiatry Res. 2018;270:375-381. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 34] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 6. | Mote J, Fulford D. Ecological momentary assessment of everyday social experiences of people with schizophrenia: A systematic review. Schizophr Res. 2020;216:56-68. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 72] [Cited by in RCA: 68] [Article Influence: 13.6] [Reference Citation Analysis (0)] |
| 7. | McCann E. The sexual and relationship needs of people who experience psychosis: quantitative findings of a UK study. J Psychiatr Ment Health Nurs. 2010;17:295-303. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 34] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 8. | Medeiros-Ferreira L, Navarro-Pastor JB, Zúñiga-Lagares A, Romaní R, Muray E, Obiols JE. Perceived needs and health-related quality of life in people with schizophrenia and metabolic syndrome: a "real-world" study. BMC Psychiatry. 2016;16:414. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 5] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 9. | Blanchard JJ, Park SG, Catalano LT, Bennett ME. Social affiliation and negative symptoms in schizophrenia: Examining the role of behavioral skills and subjective responding. Schizophr Res. 2015;168:491-497. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 51] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 10. | Edwards CJ, Cella M, Emsley R, Tarrier N, Wykes THM. Exploring the relationship between the anticipation and experience of pleasure in people with schizophrenia: An experience sampling study. Schizophr Res. 2018;202:72-79. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 33] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 11. | Schneider M, Reininghaus U, van Nierop M, Janssens M, Myin-Germeys I; GROUP Investigators. Does the Social Functioning Scale reflect real-life social functioning? An experience sampling study in patients with a non-affective psychotic disorder and healthy control individuals. Psychol Med. 2017;47:2777-2786. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 48] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 12. | Morrison KE, Pinkham AE, Penn DL, Kelsven S, Ludwig K, Sasson NJ. Distinct profiles of social skill in adults with autism spectrum disorder and schizophrenia. Autism Res. 2017;10:878-887. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 38] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 13. | Gard DE, Kring AM. Emotion in the daily lives of schizophrenia patients: context matters. Schizophr Res. 2009;115:379-380. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 22] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 14. | Oorschot M, Lataster T, Thewissen V, Lardinois M, Wichers M, van Os J, Delespaul P, Myin-Germeys I. Emotional experience in negative symptoms of schizophrenia--no evidence for a generalized hedonic deficit. Schizophr Bull. 2013;39:217-225. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 115] [Cited by in RCA: 135] [Article Influence: 11.3] [Reference Citation Analysis (0)] |
| 15. | Stain HJ, Galletly CA, Clark S, Wilson J, Killen EA, Anthes L, Campbell LE, Hanlon MC, Harvey C. Understanding the social costs of psychosis: the experience of adults affected by psychosis identified within the second Australian National Survey of Psychosis. Aust N Z J Psychiatry. 2012;46:879-889. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 105] [Cited by in RCA: 114] [Article Influence: 8.8] [Reference Citation Analysis (0)] |
| 16. | Campellone TR, Sanchez AH, Kring AM. Defeatist Performance Beliefs, Negative Symptoms, and Functional Outcome in Schizophrenia: A Meta-analytic Review. Schizophr Bull. 2016;42:1343-1352. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 83] [Cited by in RCA: 94] [Article Influence: 10.4] [Reference Citation Analysis (0)] |
| 17. | Grant PM, Beck AT. Asocial beliefs as predictors of asocial behavior in schizophrenia. Psychiatry Res. 2010;177:65-70. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 56] [Cited by in RCA: 60] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 18. | Killaspy H, White S, Lalvani N, Berg R, Thachil A, Kallumpuram S, Nasiruddin O, Wright C, Mezey G. The impact of psychosis on social inclusion and associated factors. Int J Soc Psychiatry. 2014;60:148-154. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 46] [Cited by in RCA: 44] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 19. | Lysaker PH, Davis LW, Warman DM, Strasburger A, Beattie N. Stigma, social function and symptoms in schizophrenia and schizoaffective disorder: associations across 6 mo. Psychiatry Res. 2007;149:89-95. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 138] [Cited by in RCA: 139] [Article Influence: 7.7] [Reference Citation Analysis (0)] |
| 20. | Angell B, Test MA. The relationship of clinical factors and environmental opportunities to social functioning in young adults with schizophrenia. Schizophr Bull. 2002;28:259-271. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 47] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 21. | Giacco D, McCabe R, Kallert T, Hansson L, Fiorillo A, Priebe S. Friends and symptom dimensions in patients with psychosis: a pooled analysis. PLoS One. 2012;7:e50119. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 49] [Cited by in RCA: 47] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 22. | Hamilton NG, Ponzoha CA, Cutler DL, Weigel RM. Social networks and negative vs positive symptoms of schizophrenia. Schizophr Bull. 1989;15:625-633. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 61] [Cited by in RCA: 53] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 23. | Young L, Murata L, McPherson C, Jacob JD, Vandyk AD. Exploring the Experiences of Parent Caregivers of Adult Children With Schizophrenia: A Systematic Review. Arch Psychiatr Nurs. 2019;33:93-103. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 35] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 24. | Boucher ME, Groleau D, Whitley R. Recovery and severe mental illness: The role of romantic relationships, intimacy, and sexuality. Psychiatr Rehabil J. 2016;39:180-182. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 24] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 25. | Evensen S, Wisløff T, Lystad JU, Bull H, Ueland T, Falkum E. Prevalence, Employment Rate, and Cost of Schizophrenia in a High-Income Welfare Society: A Population-Based Study Using Comprehensive Health and Welfare Registers. Schizophr Bull. 2016;42:476-483. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 92] [Cited by in RCA: 111] [Article Influence: 12.3] [Reference Citation Analysis (0)] |
| 26. | Topor A, Ljungqvist I, Strandberg EL. The costs of friendship: severe mental illness, poverty and social isolation. Psychosis. 2016;8:336-345. [RCA] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 21] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 27. | Mood C, Jonsson JO. The Social Consequences of Poverty: An Empirical Test on Longitudinal Data. Soc Indic Res. 2016;127:633-652. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 74] [Cited by in RCA: 33] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 28. | Dijkstra JK, Kretschmer T, Lindenberg S, Veenstra R. Hedonic, instrumental, and normative motives: Differentiating patterns for popular, accepted, and rejected adolescents. J Early Adolesc. 2014;35:308-328. [DOI] [Full Text] |
| 29. | Rempel JK, Holmes JG, Zanna MP. Trust in close relationships. J Pers Soc Psychol. 1985;49:95-112. [RCA] [DOI] [Full Text] [Cited by in Crossref: 1328] [Cited by in RCA: 1340] [Article Influence: 33.5] [Reference Citation Analysis (0)] |
| 30. | Awad AG, Voruganti LN. The burden of schizophrenia on caregivers: a review. Pharmacoeconomics. 2008;26:149-162. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 466] [Cited by in RCA: 453] [Article Influence: 26.6] [Reference Citation Analysis (0)] |
| 31. | Baumeister RF, Leary MR. The need to belong: desire for interpersonal attachments as a fundamental human motivation. Psychol Bull. 1995;117:497-529. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10054] [Cited by in RCA: 6555] [Article Influence: 218.5] [Reference Citation Analysis (0)] |
| 32. | Eklund M, Hermansson A, Håkansson C. Meaning in life for people with schizophrenia: Does it include occupation? J Occup Sci. 2012;19:93-105. [DOI] [Full Text] |
| 33. | Lindenberg S, Steg L. Normative, gain and hedonic goal frames guiding environmental behavior. J Soc Issues. 2007;63:117-137. [DOI] [Full Text] |
| 34. | Boydell KM, Gladstone BM, Crawford ES. The dialectic of friendship for people with psychiatric disabilities. Psychiatr Rehabil J. 2002;26:123-131. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 31] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 35. | Bowie CR, Gupta M, Holshausen K. Disconnected and underproductive speech in schizophrenia: unique relationships across multiple indicators of social functioning. Schizophr Res. 2011;131:152-156. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 39] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 36. | Buck B, Penn DL. Lexical Characteristics of Emotional Narratives in Schizophrenia: Relationships with Symptoms, Functioning, and Social Cognition. J Nerv Ment Dis. 2015;203:702-708. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 46] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 37. | Gruber J, Kring AM. Narrating emotional events in schizophrenia. J Abnorm Psychol. 2008;117:520-533. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 15] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 38. | Holshausen K, Harvey PD, Elvevåg B, Foltz PW, Bowie CR. Latent semantic variables are associated with formal thought disorder and adaptive behavior in older inpatients with schizophrenia. Cortex. 2014;55:88-96. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 55] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 39. | Minor KS, Bonfils KA, Luther L, Firmin RL, Kukla M, MacLain VR, Buck B, Lysaker PH, Salyers MP. Lexical analysis in schizophrenia: how emotion and social word use informs our understanding of clinical presentation. J Psychiatr Res. 2015;64:74-78. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 41] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 40. | Raffard S, D'Argembeau A, Lardi C, Bayard S, Boulenger JP, Van der Linden M. Narrative identity in schizophrenia. Conscious Cogn. 2010;19:328-340. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 107] [Cited by in RCA: 113] [Article Influence: 7.1] [Reference Citation Analysis (0)] |
| 41. | Lysaker PH, Buck KD, Hammoud K, Taylor AC, Roe D. Associations of symptoms, psychosocial function and hope with qualities of self-experience in schizophrenia: comparisons of objective and subjective indicators of health. Schizophr Res. 2006;82:241-249. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 50] [Cited by in RCA: 46] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 42. | Horan WP, Kring AM, Gur RE, Reise SP, Blanchard JJ. Development and psychometric validation of the Clinical Assessment Interview for Negative Symptoms (CAINS). Schizophr Res. 2011;132:140-145. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 205] [Cited by in RCA: 233] [Article Influence: 16.6] [Reference Citation Analysis (0)] |
| 43. | First MB, Spitzer RL, Gibbon M, Williams JBW. Structured clinical interview for DSM–IV–TR axis I disorders, research version, patient edition. (SCID-I/P). New York: Biometrics Research 2002; . |
| 44. | First MB, Spitzer RL, Gibbon M, Williams JBW. Structured clinical interview for DSM-IV-TR axis I disorders, research version, non-patient edition. (SCID-I/NP). New York: Biometrics Research 2002; . |
| 45. | Wechsler D. Wechsler Test of Adult Reading: WTAR. San Antonio, TX: Psychological Corporation 2001; . |
| 46. | Kring AM, Gur RE, Blanchard JJ, Horan WP, Reise SP. The Clinical Assessment Interview for Negative Symptoms (CAINS): final development and validation. Am J Psychiatry. 2013;170:165-172. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 439] [Cited by in RCA: 553] [Article Influence: 46.1] [Reference Citation Analysis (0)] |
| 47. | Pennebaker JW, Booth RJ, Boyd RL, Francis ME. Linguistic Inquiry and Word Count: LIWC2015. Austin, TX: Pennebaker Conglomerates (www.LIWC.net), 2015.. |
| 48. | Goodman SH, Sewell DR, Cooley EL, Leavitt N. Assessing levels of adaptive functioning: the Role Functioning Scale. Community Ment Health J. 1993;29:119-131. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 196] [Cited by in RCA: 210] [Article Influence: 6.6] [Reference Citation Analysis (0)] |
| 49. | Ventura J, Lukoff D, Neuchterlein KH, Liberman P, Green MF, Shaner A. Appendix 1: Brief Psychiatric Rating Scale (BPRS) Expanded version 4.0: Scales, anchor points and administration manual. Int J Meth Psychiatr Res. 1993;3:227-243. |
| 50. | Shrout PE, Fleiss JL. Intraclass correlations: uses in assessing rater reliability. Psychol Bull. 1979;86:420-428. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14247] [Cited by in RCA: 14663] [Article Influence: 1629.2] [Reference Citation Analysis (0)] |
| 51. | Gayer-Anderson C, Morgan C. Social networks, support and early psychosis: a systematic review. Epidemiol Psychiatr Sci. 2013;22:131-146. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 226] [Cited by in RCA: 207] [Article Influence: 17.3] [Reference Citation Analysis (0)] |
| 52. | Bjornestad J, Hegelstad WTV, Joa I, Davidson L, Larsen TK, Melle I, Veseth M, Johannessen JO, Bronnick K. "With a little help from my friends" social predictors of clinical recovery in first-episode psychosis. Psychiatry Res. 2017;255:209-214. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 30] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 53. | Kotov R, Fochtmann L, Li K, Tanenberg-Karant M, Constantino EA, Rubinstein J, Perlman G, Velthorst E, Fett AJ, Carlson G, Bromet EJ. Declining Clinical Course of Psychotic Disorders Over the Two Decades Following First Hospitalization: Evidence From the Suffolk County Mental Health Project. Am J Psychiatry. 2017;174:1064-1074. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 66] [Cited by in RCA: 70] [Article Influence: 8.8] [Reference Citation Analysis (0)] |
| 54. | Green MF, Horan WP, Lee J. Social cognition in schizophrenia. Nat Rev Neurosci. 2015;16:620-631. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 564] [Cited by in RCA: 713] [Article Influence: 71.3] [Reference Citation Analysis (0)] |
| 55. | Campellone TR, Kring AM. Anticipated pleasure for positive and negative social interaction outcomes in schizophrenia. Psychiatry Res. 2018;259:203-209. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 23] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 56. | Campellone TR, Truong B, Gard D, Schlosser DA. Social motivation in people with recent-onset schizophrenia spectrum disorders. J Psychiatr Res. 2018;99:96-103. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 18] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 57. | Engel M, Fritzsche A, Lincoln TM. Anticipation and experience of emotions in patients with schizophrenia and negative symptoms. An experimental study in a social context. Schizophr Res. 2016;170:191-197. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 40] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 58. | de la Asuncion J, Docx L, Sabbe B, Morrens M, de Bruijn ER. Converging evidence of social avoidant behavior in schizophrenia from two approach-avoidance tasks. J Psychiatr Res. 2015;69:135-141. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 33] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 59. | Fulford D, Campellone T, Gard DE. Social motivation in schizophrenia: How research on basic reward processes informs and limits our understanding. Clin Psychol Rev. 2018;63:12-24. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 62] [Cited by in RCA: 88] [Article Influence: 12.6] [Reference Citation Analysis (0)] |
| 60. | Barch DM, Gold JM, Kring AM. Paradigms for Assessing Hedonic Processing and Motivation in Humans: Relevance to Understanding Negative Symptoms in Psychopathology. Schizophr Bull. 2017;43:701-705. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 21] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 61. | Kring AM, Barch DM. The motivation and pleasure dimension of negative symptoms: neural substrates and behavioral outputs. Eur Neuropsychopharmacol. 2014;24:725-736. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 207] [Cited by in RCA: 264] [Article Influence: 24.0] [Reference Citation Analysis (0)] |
| 62. | Brown BB, Feldman SS, Elliott GR. Peer groups and peer cultures. Feldman SS, Elliott GR. At the threshold: The developing adolescent. Cambridge, MA: Harvard Univeristy Press 1990; 171-196. |
| 63. | Chopik WJ. Associations among relational values, support, health, and well-being across the adult lifespan. J Soc Pers Relat. 2017;24:408-422. [DOI] [Full Text] |
| 64. | Hirsch JK, Barton AL. Positive social support, negative social exchanges, and suicidal behavior in college students. J Am Coll Health. 2011;59:393-398. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 92] [Cited by in RCA: 77] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 65. | Semmer NK, Elfering A, Jacobshagen N, Perrot T, Beehr TA, Boos N. The emotional meaning of instrumental social support. Int J Stress Manag. 2008;15:235-251. [RCA] [DOI] [Full Text] [Cited by in Crossref: 139] [Cited by in RCA: 141] [Article Influence: 8.3] [Reference Citation Analysis (0)] |
| 66. | Jana AK, Ram D, Praharaj SK. Empowerment and its associations in schizophrenia: a cross-sectional study. Community Ment Health J. 2014;50:697-701. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 67. | Turner N, Ferguson L, Hill M, Nesbitt T, O'Callaghan E, O'Mahony P, Clarke M. An exploratory study of the extent of social inclusion among people with psychosis and psychotic-related conditions. Int J Soc Psychiatry. 2017;63:195-202. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 68. | Granholm E, Holden J, Link PC, McQuaid JR. Randomized clinical trial of cognitive behavioral social skills training for schizophrenia: improvement in functioning and experiential negative symptoms. J Consult Clin Psychol. 2014;82:1173-1185. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 91] [Cited by in RCA: 102] [Article Influence: 9.3] [Reference Citation Analysis (0)] |
| 69. | Granholm EL, McQuaid JR, Holden JL. Cognitive-behavioral social skills training for schizophrenia: A practical treatment guide. New York, NY: The Guilford Press, 2016. |
| 70. | Girón M, Fernández-Yañez A, Mañá-Alvarenga S, Molina-Habas A, Nolasco A, Gómez-Beneyto M. Efficacy and effectiveness of individual family intervention on social and clinical functioning and family burden in severe schizophrenia: a 2-year randomized controlled study. Psychol Med. 2010;40:73-84. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 60] [Cited by in RCA: 51] [Article Influence: 3.4] [Reference Citation Analysis (0)] |