Published online Nov 19, 2020. doi: 10.5498/wjp.v10.i11.272
Peer-review started: April 12, 2020
First decision: September 11, 2020
Revised: September 25, 2020
Accepted: October 12, 2020
Article in press: October 12, 2020
Published online: November 19, 2020
Processing time: 217 Days and 17.9 Hours
Recently, there has been a range of studies about smartphone-based interventions and monitoring for reducing symptoms of bipolar disorder (BD). However, their efficacy for BD remains unclear.
To compare the effect of smartphone-based interventions and monitoring with control methods in treating patients with BD.
A systematic literature search was performed on PubMed, Embase, Clinical trials, psycINFO, Web of Science, and Cochrane Library. Randomized clinical trials (RCTs) or single-group trials in which smartphone-based interventions and monitoring were compared with control methods or baseline in patients with symptoms of BD were included. Data were synthesized using a random-effects or a fixed-effects model to analyze the effects of psychological interventions and monitoring delivered via smartphone on psychiatric symptoms in patients with BD. The primary outcome measures were set for mania and depression symptoms. Subgroups were created to explore which aspects of smartphone interventions are relevant to the greater or lesser efficacy of treating symptoms.
We identified ten articles, including seven RCTs (985 participants) and three single-group trials (169 participants). Analysis of the between-group study showed that smartphone-based interventions were effective in reducing manic [g = -0.19, 95% confidence interval (CI): -0.33 to -0.04, P = 0.01] and depressive (g = -0.28, 95%CI: -0.55 to -0.01, P < 0.05) symptoms. In within-group analysis, smartphone-based interventions significantly reduced manic (g = 0.17, 95%CI: 0.04 to 0.30, P < 0.01) and depressive (g = 0.48, 95%CI: 0.18 to 0.78) symptoms compared to the baseline. Nevertheless, smartphone-based monitoring systems significantly reduced manic (g = 0.27, 95%CI: 0.02 to 0.51, P < 0.05) but not depressive symptoms. Subgroup analysis indicated that the interventions with psychoeducation had positive effects on depressive (g = -0.62, 95%CI: -0.81 to -0.43, P < 0.01) and manic (g = -0.24, 95%CI: -0.43 to -0.06, P = 0.01) symptoms compared to the controlled conditions, while the interventions without psychoeducation did not (P > 0.05). The contacts between therapists and patients that contributed to the implementation of psychological therapy reduced depression symptoms (g = -0.47, 95%CI: -0.75 to -0.18, P = 0.01).
Smartphone-based interventions and monitoring have a significant positive impact on depressive and manic symptoms of BD patients in between-group and within-group analysis.
Core Tip: To date no study has used meta-analysis to pool the existing evidence to examine the efficacy of smartphone-based interventions and monitoring for bipolar disorder. This is the first systematic review and meta-analysis investigating the effects of interventions and monitoring delivered via smartphone on bipolar disorder.
- Citation: Liu JY, Xu KK, Zhu GL, Zhang QQ, Li XM. Effects of smartphone-based interventions and monitoring on bipolar disorder: A systematic review and meta-analysis. World J Psychiatr 2020; 10(11): 272-285
- URL: https://www.wjgnet.com/2220-3206/full/v10/i11/272.htm
- DOI: https://dx.doi.org/10.5498/wjp.v10.i11.272
Bipolar disorder (BD) is a serious mood disorder that is characterized by depressive, manic, and mixed episodes[1]. It is estimated that the lifetime prevalence of BD is 1.0% for bipolar disorder I and 1.1% for bipolar disorder II[2]. Patients who do not receive adequate and appropriate treatment are then at risk for experiencing plentiful social and occupational impairments, even suicidal behavior[3].
Fortunately, many available treatments aim to cure manic or depressive episodes and stabilize mood[4]. However, there is a range of obstacles towards professional BD treatment. The transportation of mental health services and high-quality medications make treatment unaffordable[5]. Additionally, medication and psychotherapy are not acceptable to some patients who are ashamed of receiving treatment for mood disorder, so the therapeutic effectiveness is limited[6,7]. Therefore, innovative methods of treatment are urgently needed.
Digital technology may represent a feasible and novel solution. The majority of adults own smartphones. In recent years, the number of smartphone users has continually increased[8]. Additionally, using smartphones as a tool for psychological treatment is well-accepted for most people because it is cost-effective[9]. Use of smartphone also breaks the limitation of distance between patients and therapists, therefore it is a viable method to apply smartphones to treat someone who has difficulty in accessing health care[10]. Meanwhile, privacy and individuation are guaranteed in the use of smartphones so that treatment acceptance and compliance are enhanced[11]. Therefore, people can accept smartphone-based interventions at any time they want.
This promising therapeutic potential of smartphones has aroused the interest of different organizations such as governments, advocacy groups, technology companies, and research groups internationally[12,13]. Recently, there has been a range of articles[14-23] about smartphone mental health interventions used for reducing symptoms of BD. Although the idea of smartphone use in health care is becoming more popular, it is difficult to separate actual efficacy from overstated aspirational claims. With thousands of mental disorder treatments readily available, it is urgent to find strong evidence to prove it useful, making sure that people have an understanding of smartphone-based interventions for BD.
Recent meta-analyses have suggested that smartphone interventions can have a positive impact on physical diseases, such as diabetes[24]. Also, the efficacy of smartphone interventions for a series of mood disorders is explained with recent meta-analyses, such as depression, anxiety, and post-traumatic stress disorder[25-27]. To date, no study has used meta-analysis to pool the existing evidence to examine the efficacy of smartphone interventions for BD. Moreover, there are three reviews related to the smartphone monitoring systems collecting data to predict severity of symptoms[28-30]. However, the clinical effect of the smartphone-based monitoring system on symptoms of BD patients has yet to be established. More recently, several single-group trials are relevant to the effectiveness of the smartphone-based intervention for BD. However, no systematic review and meta-analysis has examined the efficacy of the smartphone-based intervention and monitoring for symptoms in single-group trials. Nevertheless, there is evidence that the estimates from high-quality single-group trials can overcome the paucity of prospective randomized evidence. The estimated results may be similar to those of randomized controlled trials (RCTs). Pooling of high-quality single-group trials may be as accurate as pooling of RCTs[31-34].
We conducted the present meta-analysis to provide the first overall estimated effects of smartphone-based interventions and monitoring for reducing symptoms in BD patients. We conducted between-group analyses using the data extracted from the RCTs. We also performed within-group analyses of RCTs and single-group trials. Subgroups were created to explore which aspects of smartphone interventions are relevant to the greater or lesser efficacy of treating symptoms.
This review and meta-analysis followed the PRISMA statement for the transparency and comprehension of the methodology and results reporting[35]. The PROSPERO ID of this meta-analysis is CRD42018092539.
We searched PubMed, Embase, Clinical trials, psycINFO, Web of Science, and Cochrane Library from 1993 to August 1, 2019. In the case of any other eligible studies, we looked up reference lists of related reviews and articles. Besides, key researchers in this field were asked whether they knew about unpublished trials.
The included studies fulfilled the following criteria: (1) All articles in English language; (2) Patients with a diagnosis of BD. Nevertheless, participants with BD and other types of mood disorders that had no influence on the cure of BD at the same time were also included; (3) Intervention: Website, smartphone-based apps, instruction of therapists via smartphone to facilitate psychotherapy; (4) RCTs and single-group studies; and (5) Outcomes: Reported either mania or depression symptom severity scores before and after intervention. The exclusion criteria were: (1) The intervention was not clearly defined; (2) Specific outcomes were not reported; (3) Unavailability of full text; and (4) Studies investigating the feasibility and satisfaction of smartphone-based intervention.
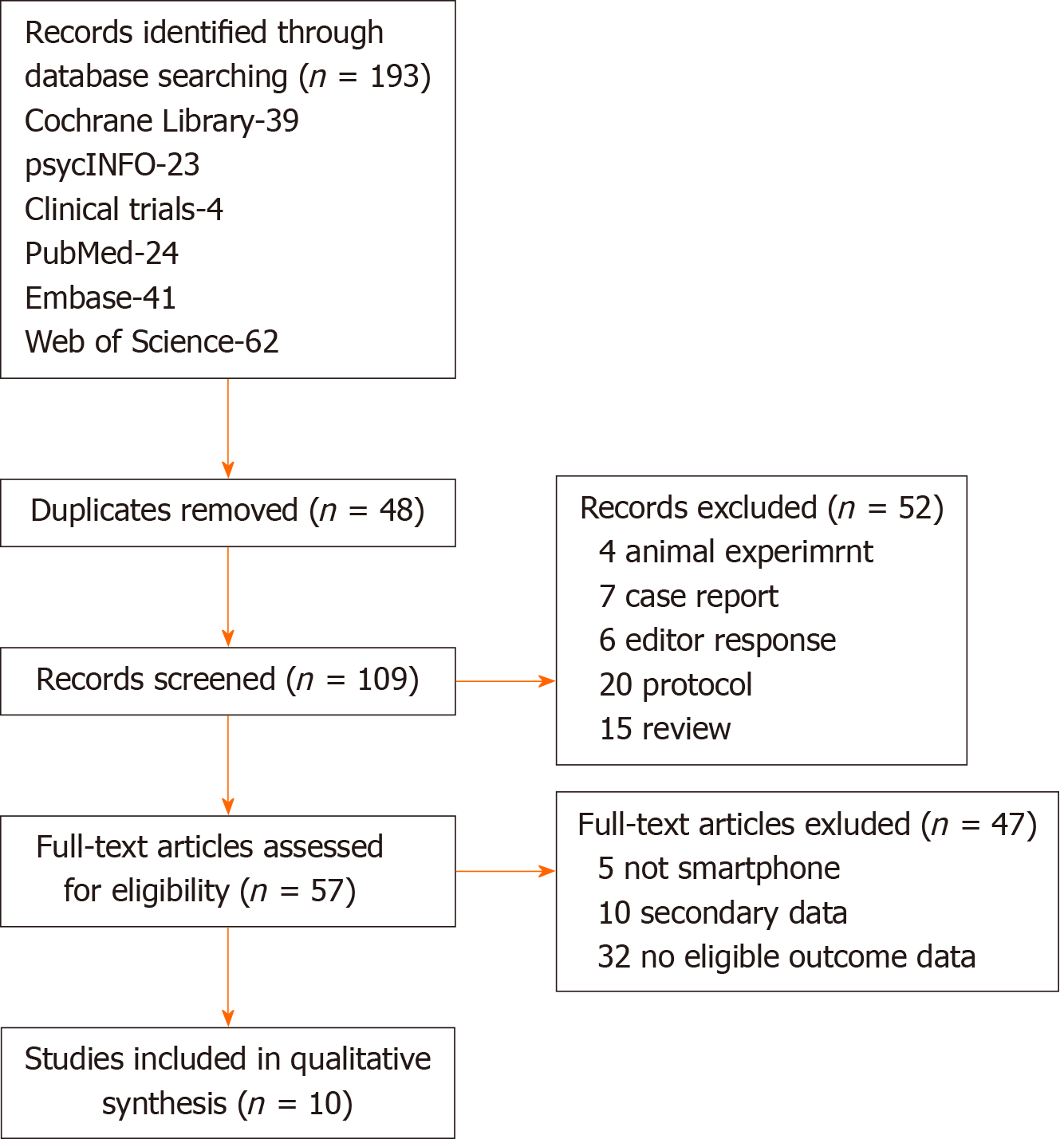
Two authors (Jia-Yuan Liu and Kang-Kang Xu) selected the articles according to the inclusion criteria after retrieval and screening of the relevant citations in full text. To identify the applicable articles, they read the abstracts and titles. A third reviewer resolved any disagreement that emerged in the process of searching and selection. The procedure of specific inclusion and extraction is shown in Figure 1.
An extraction form was used for each article to collect the following data: (1) Participant information: Sample size, mean age, inclusion criteria, and diagnosis; (2) Study design: Trial quality, whether controlled or not; (3) Smartphone intervention: Study duration, details of intervention, and frequency of intervention; and (4) Effects on mania and depression: Changes in total depressive and manic symptoms scored before and after interventions using any clinically validated rating scale.
The Cochrane risk of bias assessment tool was used for assessment of the RCT methodological quality. Bias risk in each domain of selection, performance, detection, attrition, and reporting ranking as high, low, or unknown was assessed independently by two reviewers. And inconsistencies were resolved through discussion. For publication bias, it was inappropriate to make a funnel plot to determine it because the number of included trials was no more than 10[36]. We did not have enough studies to make a meaningful funnel plot that was proposed by Egger et al[37].
Statistical analyses were performed with Review Manager version 5.3 (free software downloaded from http://www.cochrane.org). Between-group analysis was conducted for RCTs. The differences in changes in manic and depressive symptoms between smartphone-based intervention and control groups were pooled for calculation of the overall effect size using Hedges’ g[38] with 95% confidence intervals (CIs). We conducted heterogeneity tests among these studies. In case of I² > 50% and P ≤ 0.05, which indicated the presence of high heterogeneity, we chose a random-effects model; otherwise, we used a fixed-effects model. We next implemented within-group effect size of smartphone-based interventions and monitoring on manic and depressive symptoms. We computed Hedges’ g statistic as the estimate of within-group effect size for changes from pre- to post-treatment with RCTs and the single-group trials. Lastly, we conducted subgroup analyses to investigate the different effects of components of smartphone-based interventions.
A total of 193 articles were retrieved. Eighty-four duplicate articles were excluded. After reading the abstract and title of the remaining 109, we removed 52 case reports, editor responses, reviews, and studies that included animal experiments. Full versions were retrieved for 57 papers, of which ten met eligibility criteria, including seven RCTs and three single-group trials.
Table 1 displays the full details of the included studies. Available data were extracted from seven RCTs with two arms[15-19,21] or three arms[22] and three trials with single arms[14,20,23]. All but five articles had graphically reported data, which were extracted with graphical digitizer (Get Data Graph Digitizer) from the reported figures[14,18,19-21]. Two of the ten eligible studies included patients with BD and patients with other mood disorders[15,21]. Eight studies included only participants with BD diagnosed according to DSM or ICD-10[14,16-20,22,23]. The mean age of the sample ranged from 16 to 59 years (median, 38 years). Three studies were related to monitoring systems[14,18,19]. Three articles highlighted the heterogeneity in the analysis of the depressive symptoms[14,18,19]. The smartphone interventions and monitoring lasted from 4 wk to 12 mo. Manic and depressive symptoms were measured as an outcome in ten articles.
| Ref. | Sample type | n | Age (yr) | Female | Study design | Design | Measure | Smartphone intervention details |
| Depp et al[17] | Outpatient diagnosed with BD | 41, 41 | 47.5 | 58.50% | RCT | 10 wk of PRISM (self-management and monitoring app) vs paper and pencil monitoring | YMRS, MADRS | Mood monitoring and self-management APP |
| Faurholt-Jepsen et al[18] | BD patients previously treated for affective disorder | 85, 44 | 43.1 | 88.40% | RCT | 9 mo of MONARCA II (monitoring app) vs controlled conditions | YMRS, HDRS | Self-monitoring APP |
| Ben-Zeev, et al[15] | People with mental illness | 75, 74 | 49 | 41% | RCT | 3 mo of FOCUS (self-management app) vs clinical treat | PSYRATS, BDI-II | App and phone call from specialist to facilitate APP use |
| Faurholt-Jepsen et al[19] | Outpatients diagnosed with BD | 33, 34 | 29.3 | 67.10% | RCT | 6 mo of MONARCA (self-monitoring app) vs Controlled conditions | YMRS, HAMD-17 | Self-monitoring APP |
| Gliddon et al[22] | Participants with bipolar disorder | 96, 95, 87 | 39.5 | 82% | RCT | 9 mo of Mood Swings 2.0 vs control conditions | YMRS, MADRS | Mood Swing is a web site |
| Celano, et al[16] | BD patients with an acute depressive episode | 14, 11 | 45 | 68% | RCT | 4 wk of telephone-based positive psychology vs the control group | None, QIDS-SR | Phone call from specialist to instruct the self-management |
| Kilbourne, et al[21] | People with unipolar and bipolar disorder | 115, 123 | 41.3 | 66% | RCT | 12 mo of CCM (psychosocial intervention) vs usual care from provider | None, PHQ-9 | Phone call from care manager to facilitate the psychosocial intervention |
| Depp et al[23] | Outpatients with bipolar disorder | 10 | 41 | / | Single-group trials | 2 wk of PRISM (monitoring and self-management app) | YMRS, MADRS | Mood monitoring and self-management APP |
| Beiwinkel, et al[14] | Outpatients with bipolar disorder | 14 | 47.2 | 38% | Single-group trials | 12 mo of a smartphone-based monitoring system | YMRS, HAMD | Monitoring APP |
| Miklowitz et al[20] | Patients with bipolar disorder | 19 | 37.2 | 68.40% | Single-group trials | 4 mo of FIMM (psychoeducation and monitoring) | YMRS, QIDS-SR | Monitoring and self-management APP |
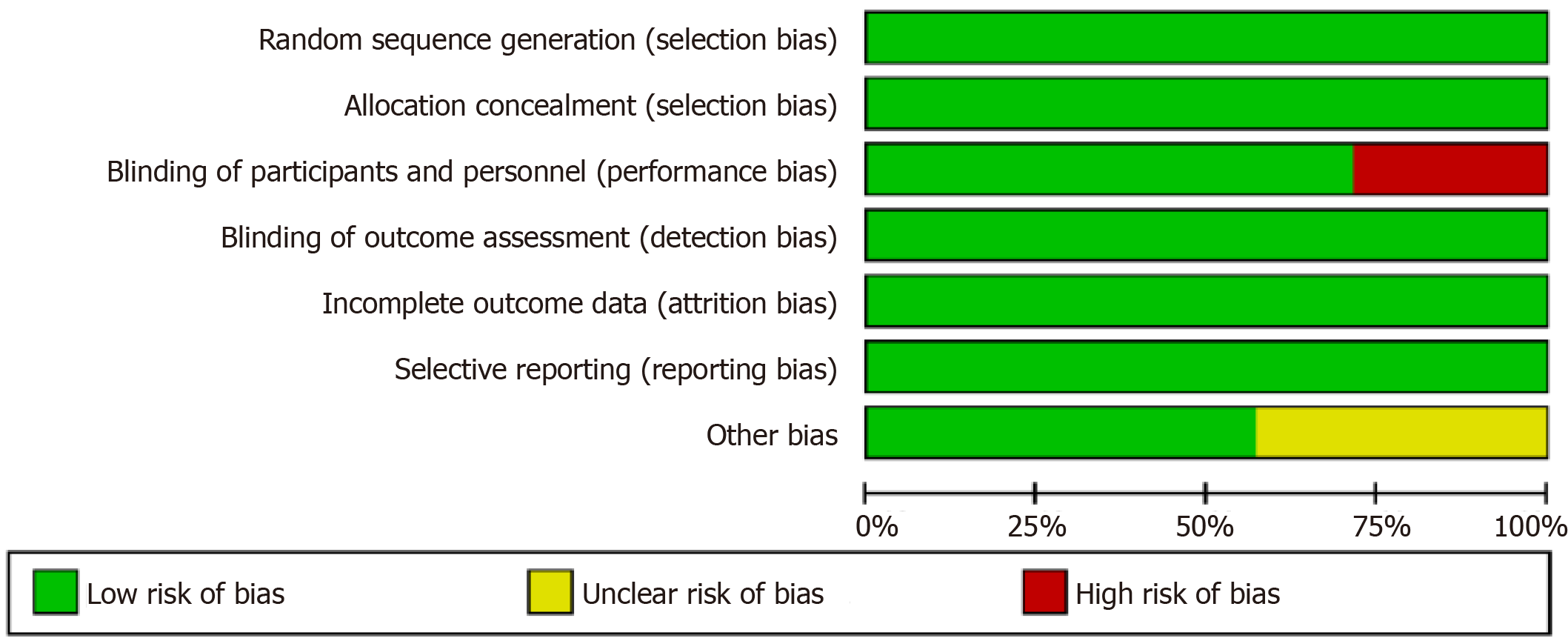
The results from the Cochrane Risk of Bias assessment are displayed in Figure 2. The most frequent risk factor for bias was inadequate blinding of participants and personnel with only five of seven studies using the blinding method for which the participants would not be aware of their treatment or control status, as well as the hypothesized outcomes of the trial.
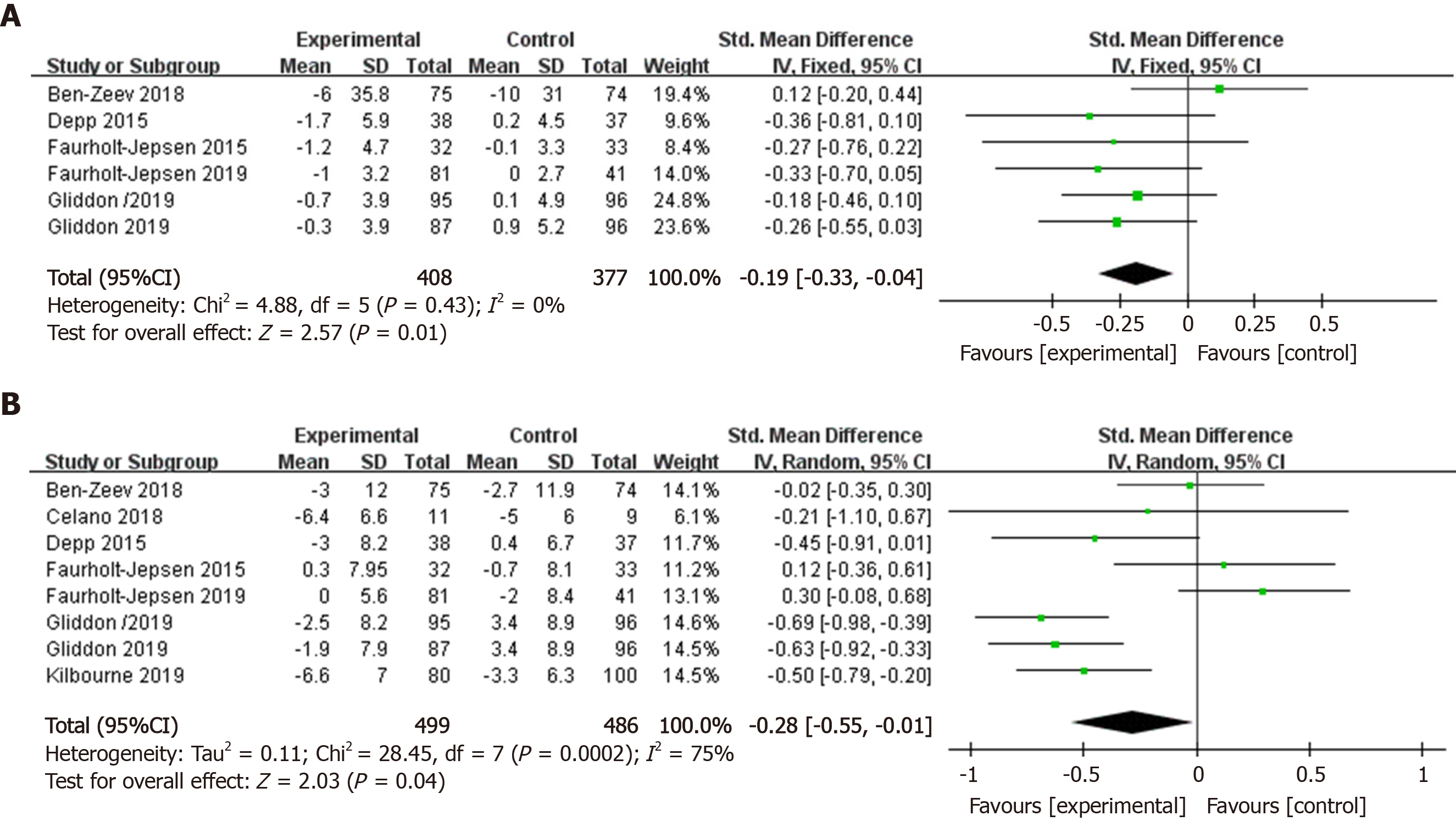
The pooled effect size of smartphone-based interventions on manic symptom changes in comparison to control conditions is shown in Figure 3A. Meta-analysis indicated a positive effect size of smartphone-based interventions for reducing manic symptoms compared to control groups (k = 6, n = 785, g = -0.19, 95%CI: -0.33 to -0.04, P = 0.01, I² = 0). There was no heterogeneity across the studies, therefore, we chose a fixed-effects model. Smartphone-based interventions were significantly more efficacious than control conditions in improving depressive symptoms (k = 8, n = 985, g = -0.28, 95%CI: -0.55 to -0.01, P < 0.05, I² = 75%) (Figure 3B). We found high heterogeneity among the studies. Therefore, sensitivity analyses were conducted to explore the reasons for this high heterogeneity. After excluding one article[18], the heterogeneity was lower, while the pooled effect size was still significant (k = 6, n = 863, g = -0.38, 95%CI: -0.61 to -0.14, P < 0.01, I² = 63%).
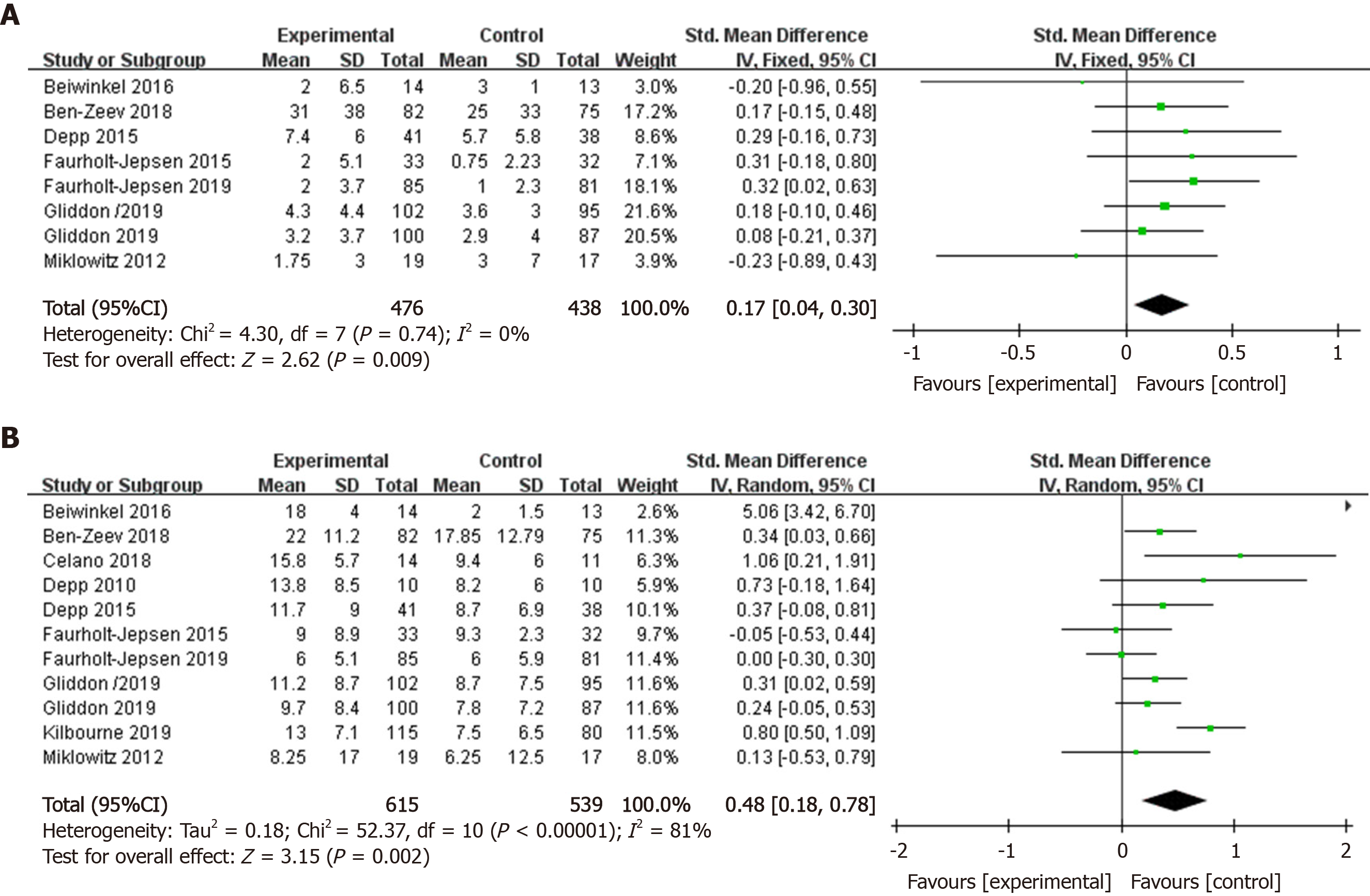
In within-group analysis, comparing changes from baseline to post-treatment scores, smartphone-based interventions resulted in significant improvements in manic symptoms (k = 8, n = 914, g = 0.17, 95%CI: 0.04 to 0.30, P < 0.01, I² = 0) (Figure 4A). Heterogeneity did not exist, and the fixed-effects model was chosen. In within-group analysis, smartphone-based interventions significantly reduced depressive symptoms (k = 11, n = 1154, g = 0.48, 95%CI: 0.18 to 0.78, I² = 81%) after the interventions (Figure 4B). High heterogeneity across article data was found. Therefore, sensitivity analyses were conducted to examine the reasons for the high heterogeneity. After removing two articles[14,21], the heterogeneity was lowered, whereas the effect size was still significant (k = 9, n = 932, g = 0.25, 95%CI: 0.10 to 0.39, I² = 15%).
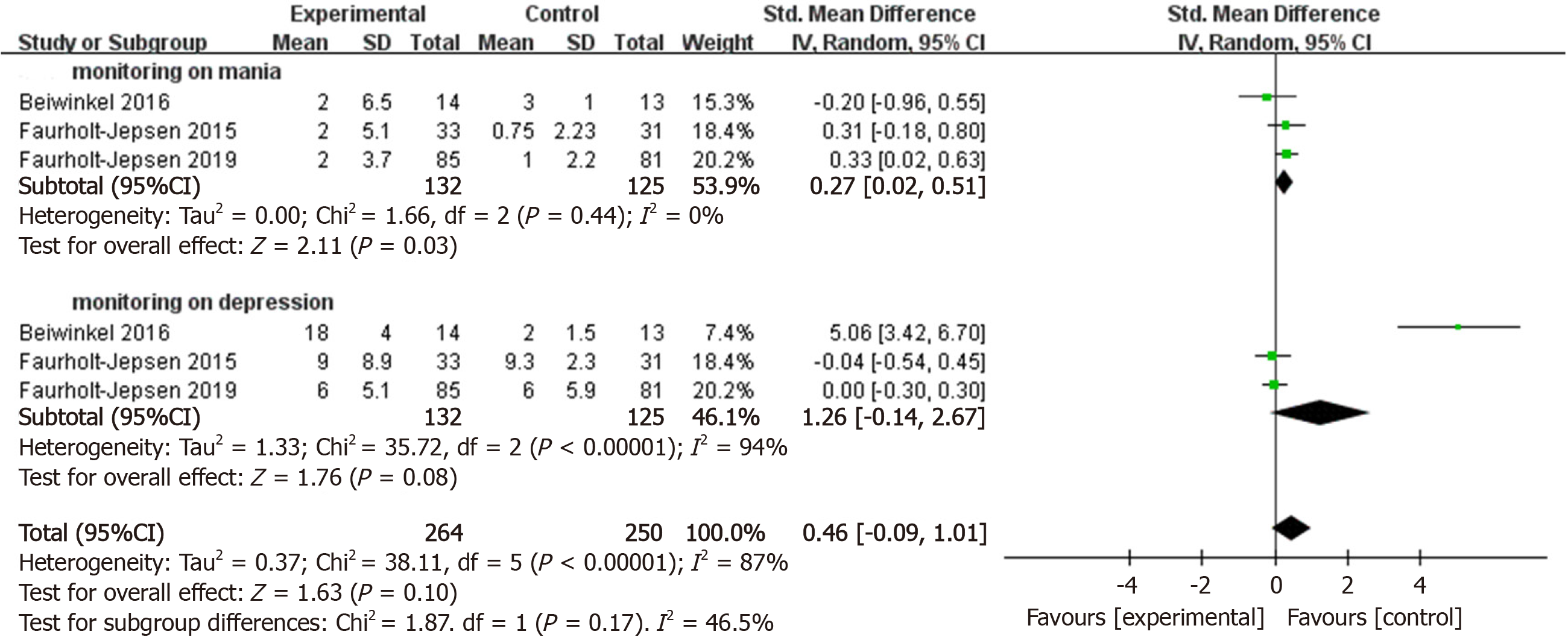
In order to investigate whether monitoring via smartphone had positive effects on manic and depressive symptoms, we performed within-group analyses. Smartphone-based monitoring appeared effective for manic symptoms (k = 3, n = 257, g = 0.27, 95%CI: 0.02 to 0.51, P < 0.05, I² = 0) compared with changes from baseline to post-treatment scores (Figure 5). The pooled effect size from smartphone-based monitoring on depressive symptoms was near to significant (k = 3, n = 257, g = 1.26, 95%CI: -0.14 to 2.67, P = 0.08, I² = 94%).
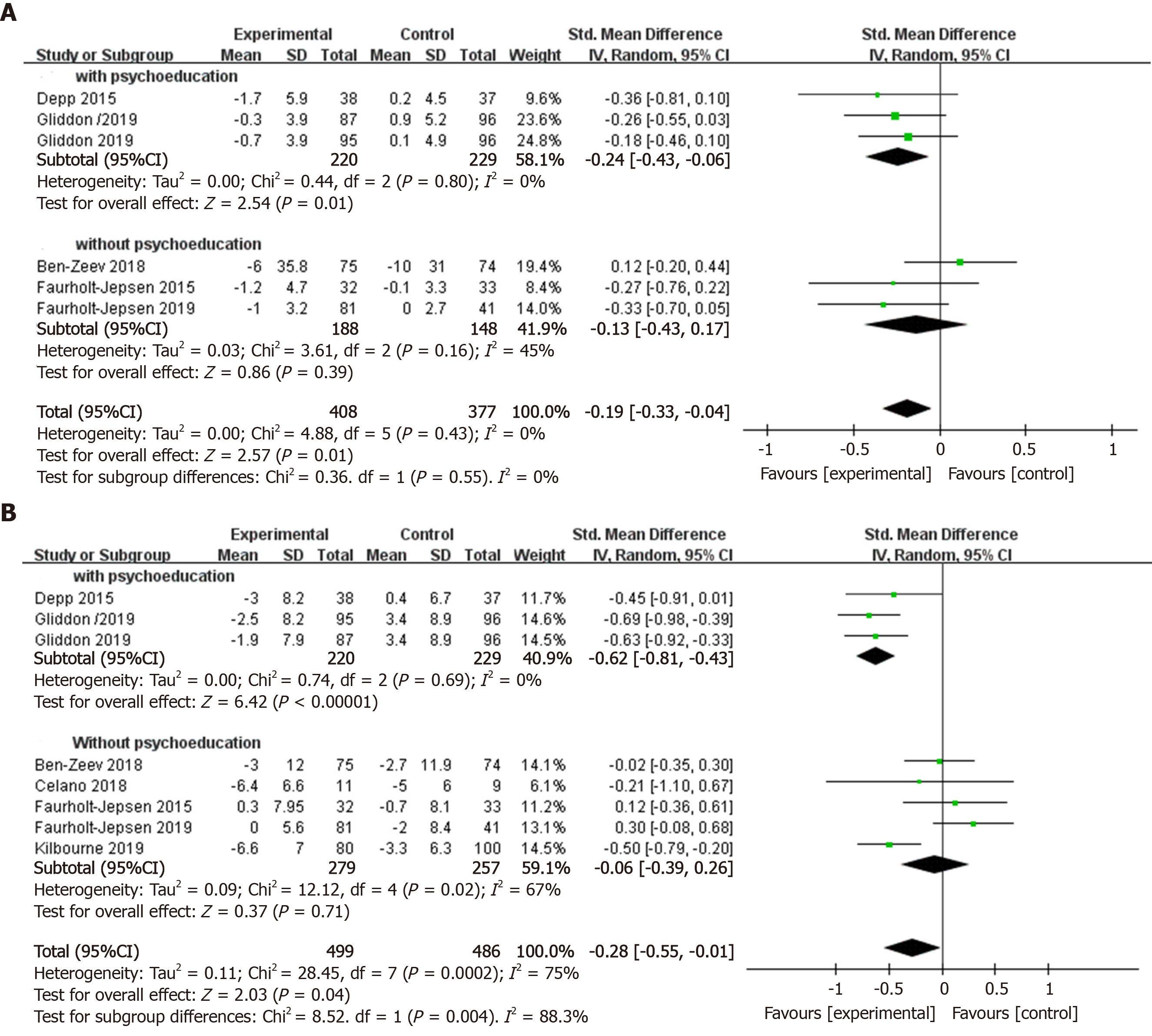
In order to explore which details of smartphone interventions make them effective for manic and depressive symptoms, we conducted further subgroup analyses. Smartphone interventions that involved psychoeducation had positive effects on manic symptoms (k = 3, n = 449, g = -0.24, 95%CI: -0.43 to -0.06, P = 0.01, I² = 0) compared to control groups, while those without psychoeducation did not (k = 3, n = 336, g = -0.13, 95%CI: -0.43 to 0.17, P = 0.39, I² = 45%) (Figure 6A). There was no significant subgroup difference (c² = 0.36, df = 1, P = 0.55) in the effect size obtained for smartphone interventions that involved psychoeducation compared to those without. Our meta-analysis revealed a positive effect size of smartphone mental health interventions for reducing depressive symptoms (k = 3, n = 449, g = 0.62, 95%CI: -0.81 to -0.43, P < 0.01, I² = 0) compared to control groups, while those without psychoeducation were not significantly more efficacious than control conditions in improving depressive symptoms (k = 5, n = 536, g = -0.06, 95%CI: -0.39 to 0.26, P = 0.71, I² =67%) (Figure 6B). There was a significant subgroup difference (c² = 8.52, df = 1, P = 0.004) in the overall effect size gained for smartphone interventions that involved psychoeducation compared to that did not.
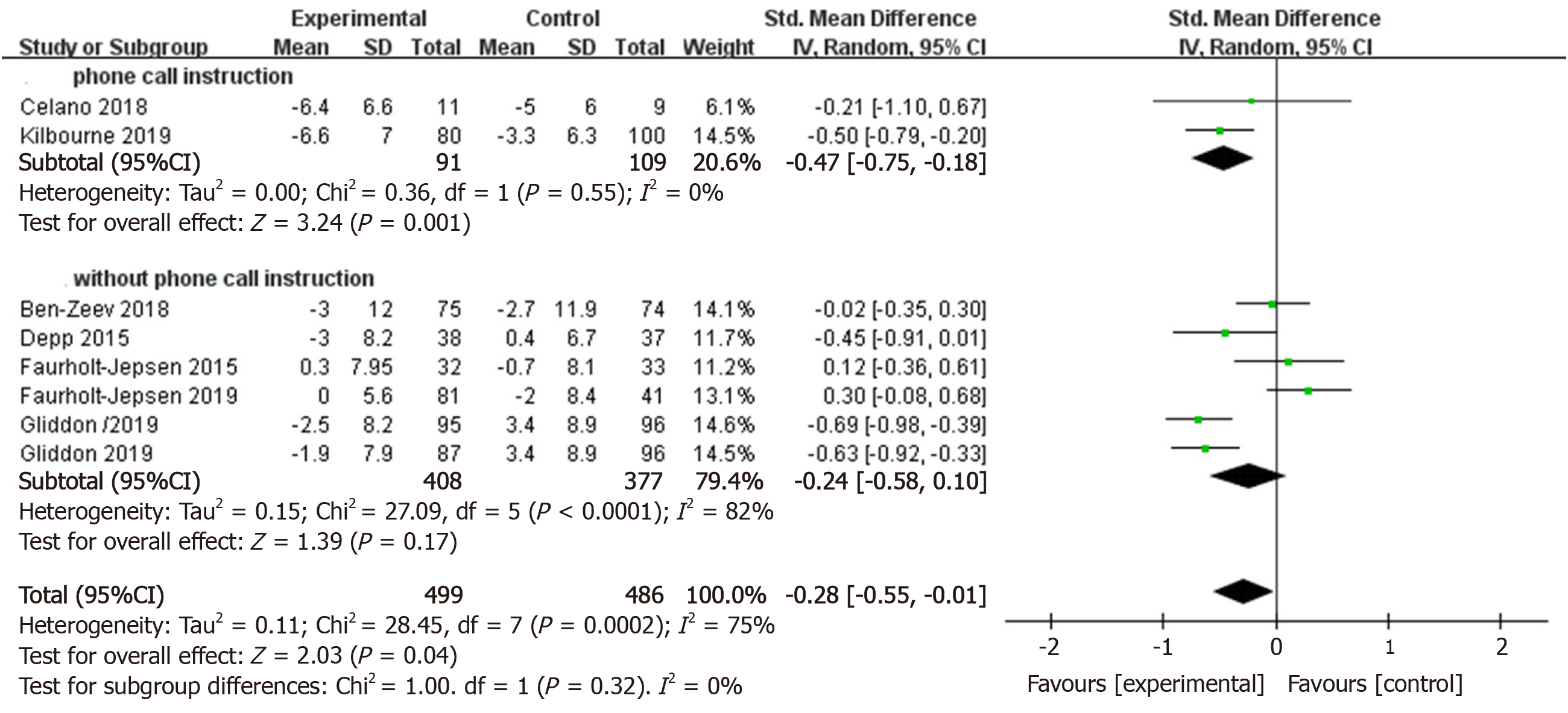
Interventions that involved instruction via smartphone had a significantly great effect size on depression outcomes compared to control conditions (k = 2, n = 200, g = -0.47, 95%CI: -0.75 to -0.18, P = 0.01, I² = 0), whereas those without instruction through smartphone did not reduce manic and depressive symptoms compared to control groups (k = 6, n = 785, g = -0.24, 95%CI: -0.58 to 0.10, P = 0.17, I² = 82%) (Figure 7). There was no significant subgroup difference (c² = 1, df = 1, P = 0.32) in the pooled effect size obtained for interventions that involved instruction via smartphone compared to those that did not.
As far as we know, this is the first meta-analysis to examine the effects of smartphone-based interventions and monitoring on BD. Ten studies with a total sample of 1028 participants who received smartphone-based treatment or monitoring were used for meta-analysis. The studies were comprehensive in this field. The number of included articles for this meta-analysis was similar to that of a previous meta-analysis that found positive effects from smartphone apps across nine studies with 1837 participants with anxiety[25]. The literature base for BD appears larger than that for other affective disorders, such as post-traumatic stress disorder, according to a recent meta-analysis in this field that included only five relevant articles[27]. Furthermore, six of our ten articles were published within the past 5 years[14-16,18,21,22], which means that our analysis reflected the effectiveness of the most updated smartphone-based intervention tools.
Our analysis found that smartphone interventions had a positive effect on BD between and within groups. Meta-analysis indicated a positive effect of smartphone-based interventions for reducing manic (g = -0.19) and depressive (g = -0.28) symptoms compared to control groups. In within-group analyses, the effects of smartphone-based interventions appeared effective for manic (g = 0.17) and depressive (g = 0.48) symptoms. Similar positive effects were observed in the meta-analysis of smartphone interventions for other mood disorders, such as anxiety, depression, post-traumatic stress disorder, and obsessive compulsive disorder[25-27,37]. These findings indicate that delivering psychological treatments via smartphone devices is an efficacious and promising method to treat BD. The potential mechanism by which smartphone interventions reduce symptoms of BD might be explained by using these devices to support and enhance the delivery of existing face-to-face therapy[25]. The use of smartphone-based interventions may provide creative and innovative interventions, filling the gap between feasibility and the demand for treatment[39]. Additionally, interventions via smartphone devices may remedy some limitations of existing traditional therapy in the future, with the advantages of convenience and lower treatment cost.
Our analysis showed that BD participants with mania who used the smartphone monitoring systems experienced benefits (g = 0.27). Meanwhile, a recent review of the smartphone application for mood disorders had similar finding that smartphone application with mood monitoring features reduces depressive symptoms[26]. Additionally, a previous study proposed that using a digital device in itself may produce some psychological benefits[40]. The smartphone-based monitoring system was used to collect data on phone usage, social communication, social activity, and mobility, which were irrelevant to psychotherapy. To some extent, using the smartphone-based monitoring system was equivalent to only using the device itself. Therefore, our results that monitoring systems have positive effect on manic symptoms may contribute to the hypothesis that smartphones may offer some psychological benefits. There were three reviews related to the smartphone monitoring system collecting data to predict severity of symptoms[28-30]. Therefore, we conclude that the monitoring system may contribute to treatment of BD and predictions of clinically assessed depressive and manic symptoms. In the future, using smartphone-based monitoring and treatment simultaneously may form a complete treatment system that is convenient and efficient.
With regards to intervention features, in our subgroup analysis, smartphone interventions that involved psychoeducation had great effects on manic (g = -0.24) and depressive (g = -0.62) symptoms of BD compared to control conditions. A similar finding was reported in a recent meta-analysis about psychoeducation for the management of BD patients[41]. The effects of smartphone interventions that involved instruction from the therapist (g = -0.47) appeared significant, while the effect size of those without instruction was not significant. A previous study found that therapist guidance bolstered the effectiveness of smartphone interventions[42]. Instruction from therapists may be conducive to improvement of patient engagement and completion rate of therapy. Although smartphone-based interventions reduced symptoms, there are numerous factors that may affect outcomes of smartphone interventions. Therefore, to design these interventions to be effective in the future, more analyses are needed.
In general, smartphone-based interventions and monitoring reduced symptoms in BD patients. BD is always associated with poor quality of life in addition to personal suffering from depression[43]. Although there are many treatments for BD, there is a limitation in the availability of therapy. The use of smartphones is accessible and affordable[44], which ensures the implementation of mental health interventions and monitoring for BD. It enhances and facilitates the delivery of existing therapy programs and makes them more acceptable. However, there are some complex issues generated by the use of smartphones and the technology itself, including low resource settings somewhere, privacy policy, clinical utility, commercialization, and evolving technology[45-48]. Therefore, in order to achieve satisfactory therapeutic effects in the use of smartphone interventions for BD patients, the influential factors in the whole treatment process should be studied and resolved in the future. Additionally, communication between the users and designers of smartphone-based interventions is not adequate. In the future, the treatment methods will need to be optimized according to the users’ feedback and the researchers’ thoughts.
Our study had a few limitations. First, two studies in this meta-analysis were considered to have a high risk of bias because of inadequate blinding of participants and personnel[15,18]. Second, the absolute number of available applications is unknown and the applications are frequently updated. It is impossible to examine total smartphone interventions. Third, there were only three eligible articles regarding smartphone-based monitoring patterns[14,18,19], which was not sufficient to provide definitive results. Future research that directly tests the monitoring effectiveness against BD would add value to our results. Lastly, to explore potential factors relevant to smartphone interventions, details about demographics, severity of BD, and engagement need to be collected. Nevertheless, with limited data that can be extracted, we could not conduct subgroup analysis on these variables that might impact statistical results. In the future, a more standard data reporting format needs to be implemented with research data, thus improving the validity and reliability of meta-analysis.
In summary, smartphone-based interventions are effective in reducing manic and depressive symptoms. Nevertheless, the smartphone-based monitoring systems only worked for participants with manic but not depressive symptoms. Our results contribute to the literature on smartphone-based interventions and monitoring for manic and depressive symptoms in BD patients, although much work remains to be done. This meta-analysis shows that smartphone-based intervention and monitoring have the potential to enhance the methods of treatment with its characteristics of low expenditure and highly-convenience in addition to available medications and psychological interventions.
Recently, a range of studies about smartphone-based interventions and monitoring for reducing symptoms of bipolar disorder (BD) have been published. However, their efficacy for BD remains unclear.
The present study aimed to assess randomized controlled trials and single-group trials of smartphone-based interventions and monitoring for reducing the symptoms of BD.
The main objective was to update and evaluate innovative treatment suggestions for BD.
We performed a systematic literature search on PubMed, Embase, Clinical trials, psycINFO, Web of Science, and Cochrane Library. Randomized clinical trials or single-group trials in which smartphone-based interventions and monitoring were compared with control methods or baseline in patients with symptoms of BD were included. We synthesized data using a random-effects or a fixed-effects model by Review Manager version 5.3 to analyze the effects of psychological interventions and monitoring delivered via smartphone on psychiatric symptoms in patients with BD. The primary outcome measures were set for mania and depression symptoms. The subgroups were created to explore which aspects of smartphone interventions are relevant to the greater or lesser efficacy of treating symptoms.
We identified ten articles, including seven randomized clinical trials (985 participants) and three single-group trials (169 participants). Analysis of the between-group study showed that smartphone-based interventions had positive effects in reducing manic (g = -0.19, 95%CI: -0.33 to -0.04, P = 0.01) and depressive (g = -0.28, 95%CI: -0.55 to -0.01, P < 0.05) symptoms. In within-group analysis, smartphone-based interventions significantly reduced manic (g = 0.17, 95%CI: 0.04 to 0.30, P < 0.01) and depressive (g = 0.48, 95%CI: 0.18 to 0.78) symptoms compared to the baseline. Nevertheless, smartphone-based monitoring systems significantly reduced manic (g = 0.27, 95%CI: 0.02 to 0.51, P < 0.05) but not depressive symptoms. Subgroup analysis indicated that the interventions with psychoeducation were effective for depressive (g = -0.62, 95%CI: -0.81 to -0.43, P < 0.01) and manic (g = -0.24, 95%CI: -0.43 to -0.06, P = 0.01) symptoms compared to the controlled conditions, while the interventions without psychoeducation did not (P > 0.05). The contacts between therapists and patients that contributed to the implementation of psychological therapy reduced depression symptoms (g = -0.47, 95%CI: -0.75 to -0.18, P = 0.01).
Smartphone-based interventions and monitoring have a significant positive impact on depressive and manic symptoms of BD patients in between-group and within-group analysis.
The current meta-analysis suggests that smartphone-based interventions provide evidence of any reduction in manic and depressive symptoms. Nevertheless, smartphone-based monitoring systems are only effective for participants with manic but not depressive symptoms. The findings have implied that these digital tools can be used as the clinically future treatments for symptoms of BD. However, future trials need to keep pace with the development of these apps and a better understanding of the numerous factors that influence outcomes of smartphone interventions for BD are also required.
Manuscript source: Unsolicited manuscript
Specialty type: Psychiatry
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Byeon H S-Editor: Zhang L L-Editor: Wang TQ P-Editor: Li JH
| 1. | Müller JK, Leweke FM. Bipolar disorder: clinical overview. Med Monatsschr Pharm. 2016;39:363-369. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 2. | Merikangas KR, Akiskal HS, Angst J, Greenberg PE, Hirschfeld RM, Petukhova M, Kessler RC. Lifetime and 12-month prevalence of bipolar spectrum disorder in the National Comorbidity Survey replication. Arch Gen Psychiatry. 2007;64:543-552. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1830] [Cited by in RCA: 1606] [Article Influence: 89.2] [Reference Citation Analysis (0)] |
| 3. | Nasrallah HA. Consequences of misdiagnosis: inaccurate treatment and poor patient outcomes in bipolar disorder. J Clin Psychiatry. 2015;76:e1328. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 48] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 4. | Morsel AM, Morrens M, Sabbe B. An overview of pharmacotherapy for bipolar I disorder. Expert Opin Pharmacother. 2018;19:203-222. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 12] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 5. | Sulaberidze L, Green S, Chikovani I, Uchaneishvili M, Gotsadze G. Barriers to delivering mental health services in Georgia with an economic and financial focus: informing policy and acting on evidence. BMC Health Serv Res. 2018;18:108. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 6. | Gulliver A, Griffiths KM, Christensen H. Perceived barriers and facilitators to mental health help-seeking in young people: a systematic review. BMC Psychiatry. 2010;10:113. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2156] [Cited by in RCA: 1585] [Article Influence: 105.7] [Reference Citation Analysis (0)] |
| 7. | Pedersen ER, Paves AP. Comparing perceived public stigma and personal stigma of mental health treatment seeking in a young adult sample. Psychiatry Res. 2014;219:143-150. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 99] [Cited by in RCA: 104] [Article Influence: 9.5] [Reference Citation Analysis (0)] |
| 8. | Kim MS. Influence of neck pain on cervical movement in the sagittal plane during smartphone use. J Phys Ther Sci. 2015;27:15-17. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 60] [Cited by in RCA: 47] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 9. | Pratap A, Renn BN, Volponi J, Mooney SD, Gazzaley A, Arean PA, Anguera JA. Using Mobile Apps to Assess and Treat Depression in Hispanic and Latino Populations: Fully Remote Randomized Clinical Trial. J Med Internet Res. 2018;20:e10130. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 89] [Cited by in RCA: 71] [Article Influence: 10.1] [Reference Citation Analysis (0)] |
| 10. | Rawstorn JC, Ball K, Oldenburg B, Chow CK, McNaughton SA, Lamb KE, Gao L, Moodie M, Amerena J, Nadurata V, Neil C, Cameron S, Maddison R. Smartphone Cardiac Rehabilitation, Assisted Self-Management Versus Usual Care: Protocol for a Multicenter Randomized Controlled Trial to Compare Effects and Costs Among People With Coronary Heart Disease. JMIR Res Protoc. 2020;9:e15022. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 17] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 11. | Juarascio AS, Manasse SM, Goldstein SP, Forman EM, Butryn ML. Review of smartphone applications for the treatment of eating disorders. Eur Eat Disord Rev. 2015;23:1-11. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 94] [Cited by in RCA: 85] [Article Influence: 7.7] [Reference Citation Analysis (0)] |
| 12. | Firth J, Torous J, Yung AR. Ecological momentary assessment and beyond: The rising interest in e-mental health research. J Psychiatr Res. 2016;80:3-4. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 39] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 13. | Larsen ME, Nicholas J, Christensen H. Quantifying App Store Dynamics: Longitudinal Tracking of Mental Health Apps. JMIR Mhealth Uhealth. 2016;4:e96. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 121] [Cited by in RCA: 110] [Article Influence: 12.2] [Reference Citation Analysis (0)] |
| 14. | Beiwinkel T, Kindermann S, Maier A, Kerl C, Moock J, Barbian G, Rössler W. Using Smartphones to Monitor Bipolar Disorder Symptoms: A Pilot Study. JMIR Ment Health. 2016;3:e2. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 124] [Cited by in RCA: 107] [Article Influence: 11.9] [Reference Citation Analysis (0)] |
| 15. | Ben-Zeev D, Brian RM, Jonathan G, Razzano L, Pashka N, Carpenter-Song E, Drake RE, Scherer EA. Mobile Health (mHealth) Versus Clinic-Based Group Intervention for People With Serious Mental Illness: A Randomized Controlled Trial. Psychiatr Serv. 2018;69:978-985. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 101] [Cited by in RCA: 112] [Article Influence: 16.0] [Reference Citation Analysis (0)] |
| 16. | Celano CM, Gomez-Bernal F, Mastromauro CA, Beale EE, DuBois CM, Auerbach RP, Huffman JC. A positive psychology intervention for patients with bipolar depression: a randomized pilot trial. J Ment Health. 2020;29:60-68. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 23] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 17. | Depp CA, Ceglowski J, Wang VC, Yaghouti F, Mausbach BT, Thompson WK, Granholm EL. Augmenting psychoeducation with a mobile intervention for bipolar disorder: a randomized controlled trial. J Affect Disord. 2015;174:23-30. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 137] [Cited by in RCA: 119] [Article Influence: 11.9] [Reference Citation Analysis (0)] |
| 18. | Faurholt-Jepsen M, Frost M, Christensen EM, Bardram JE, Vinberg M, Kessing LV. The effect of smartphone-based monitoring on illness activity in bipolar disorder: the MONARCA II randomized controlled single-blinded trial. Psychol Med. 2020;50:838-848. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 61] [Cited by in RCA: 62] [Article Influence: 12.4] [Reference Citation Analysis (0)] |
| 19. | Faurholt-Jepsen M, Frost M, Ritz C, Christensen EM, Jacoby AS, Mikkelsen RL, Knorr U, Bardram JE, Vinberg M, Kessing LV. Daily electronic self-monitoring in bipolar disorder using smartphones - the MONARCA I trial: a randomized, placebo-controlled, single-blind, parallel group trial. Psychol Med. 2015;45:2691-2704. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 125] [Cited by in RCA: 120] [Article Influence: 12.0] [Reference Citation Analysis (0)] |
| 20. | Miklowitz DJ, Price J, Holmes EA, Rendell J, Bell S, Budge K, Christensen J, Wallace J, Simon J, Armstrong NM, McPeake L, Goodwin GM, Geddes JR. Facilitated Integrated Mood Management for adults with bipolar disorder. Bipolar Disord. 2012;14:185-197. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 62] [Cited by in RCA: 59] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 21. | Kilbourne AM, Prenovost KM, Liebrecht C, Eisenberg D, Kim HM, Un H, Bauer MS. Randomized Controlled Trial of a Collaborative Care Intervention for Mood Disorders by a National Commercial Health Plan. Psychiatr Serv. 2019;70:219-224. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 12] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 22. | Gliddon E, Cosgrove V, Berk L, Lauder S, Mohebbi M, Grimm D, Dodd S, Coulson C, Raju K, Suppes T, Berk M. A randomized controlled trial of MoodSwings 2.0: An internet-based self-management program for bipolar disorder. Bipolar Disord. 2019;21:28-39. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 30] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 23. | Depp CA, Mausbach B, Granholm E, Cardenas V, Ben-Zeev D, Patterson TL, Lebowitz BD, Jeste DV. Mobile interventions for severe mental illness: design and preliminary data from three approaches. J Nerv Ment Dis. 2010;198:715-721. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 212] [Cited by in RCA: 179] [Article Influence: 11.9] [Reference Citation Analysis (0)] |
| 24. | Cui M, Wu X, Mao J, Wang X, Nie M. T2DM Self-Management via Smartphone Applications: A Systematic Review and Meta-Analysis. PLoS One. 2016;11:e0166718. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 227] [Cited by in RCA: 168] [Article Influence: 18.7] [Reference Citation Analysis (0)] |
| 25. | Firth J, Torous J, Nicholas J, Carney R, Rosenbaum S, Sarris J. Can smartphone mental health interventions reduce symptoms of anxiety? J Affect Disord. 2017;218:15-22. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 422] [Cited by in RCA: 396] [Article Influence: 49.5] [Reference Citation Analysis (0)] |
| 26. | Firth J, Torous J, Nicholas J, Carney R, Pratap A, Rosenbaum S, Sarris J. The efficacy of smartphone-based mental health interventions for depressive symptoms: a meta-analysis of randomized controlled trials. World Psychiatry. 2017;16:287-298. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 696] [Cited by in RCA: 564] [Article Influence: 70.5] [Reference Citation Analysis (0)] |
| 27. | Goreis A, Felnhofer A, Kafka JX, Probst T, Kothgassner OD. Efficacy of Self-Management Smartphone-Based Apps for Post-traumatic Stress Disorder Symptoms: A Systematic Review and Meta-Analysis. Front Neurosci. 2020;14:3. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 14] [Cited by in RCA: 16] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 28. | Faurholt-Jepsen M, Torri E, Cobo J, Yazdanyar D, Palao D, Cardoner N, Andreatta O, Mayora O, Kessing LV. Smartphone-based self-monitoring in bipolar disorder: evaluation of usability and feasibility of two systems. Int J Bipolar Disord. 2019;7:1. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 27] [Cited by in RCA: 29] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 29. | Faurholt-Jepsen M, Bauer M, Kessing LV. Smartphone-based objective monitoring in bipolar disorder: status and considerations. Int J Bipolar Disord. 2018;6:6. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 72] [Cited by in RCA: 76] [Article Influence: 10.9] [Reference Citation Analysis (0)] |
| 31. | Abraham NS, Byrne CJ, Young JM, Solomon MJ. Meta-analysis of well-designed nonrandomized comparative studies of surgical procedures is as good as randomized controlled trials. J Clin Epidemiol. 2010;63:238-245. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 127] [Cited by in RCA: 148] [Article Influence: 9.3] [Reference Citation Analysis (0)] |
| 32. | Hosono S, Arimoto Y, Ohtani H, Kanamiya Y. Meta-analysis of short-term outcomes after laparoscopy-assisted distal gastrectomy. World J Gastroenterol. 2006;12:7676-7683. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 114] [Cited by in RCA: 97] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 33. | MacLehose RR, Reeves BC, Harvey IM, Sheldon TA, Russell IT, Black AM. A systematic review of comparisons of effect sizes derived from randomised and non-randomised studies. Health Technol Assess. 2000;4:1-154. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 184] [Cited by in RCA: 169] [Article Influence: 7.0] [Reference Citation Analysis (0)] |
| 34. | Yakoub D, Athanasiou T, Tekkis P, Hanna GB. Laparoscopic assisted distal gastrectomy for early gastric cancer: is it an alternative to the open approach? Surg Oncol. 2009;18:322-333. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 88] [Cited by in RCA: 76] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 35. | Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, Ioannidis JP, Clarke M, Devereaux PJ, Kleijnen J, Moher D. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. PLoS Med. 2009;6:e1000100. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11206] [Cited by in RCA: 10999] [Article Influence: 687.4] [Reference Citation Analysis (0)] |
| 36. | Han TW, Jan LY. Making antisense of pain. Nat Neurosci. 2013;16:986-987. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 37. | Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315:629-634. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34245] [Cited by in RCA: 40323] [Article Influence: 1440.1] [Reference Citation Analysis (2)] |
| 38. | Hedges LV, Olkin I. Statistical Methods for Meta-Analysis. 1th ed. Orlando: Academic Press, 2014: 369. |
| 39. | Thara R. Using mobile telepsychiatry to close the mental health gap. Curr Psychiatry Rep. 2012;14:167-168. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 15] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 40. | Torous J, Firth J. The digital placebo effect: mobile mental health meets clinical psychiatry. Lancet Psychiatry. 2016;3:100-102. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 120] [Cited by in RCA: 135] [Article Influence: 15.0] [Reference Citation Analysis (0)] |
| 41. | Soo SA, Zhang ZW, Khong SJ, Low JEW, Thambyrajah VS, Alhabsyi SHBT, Chew QH, Sum MY, Sengupta S, Vieta E, McIntyre RS, Sim K. Randomized Controlled Trials of Psychoeducation Modalities in the Management of Bipolar Disorder: A Systematic Review. J Clin Psychiatry. 2018;79. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 27] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 42. | Linardon J, Cuijpers P, Carlbring P, Messer M, Fuller-Tyszkiewicz M. The efficacy of app-supported smartphone interventions for mental health problems: a meta-analysis of randomized controlled trials. World Psychiatry. 2019;18:325-336. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 299] [Cited by in RCA: 405] [Article Influence: 67.5] [Reference Citation Analysis (0)] |
| 43. | Vieta E, Berk M, Schulze TG, Carvalho AF, Suppes T, Calabrese JR, Gao K, Miskowiak KW, Grande I. Bipolar disorders. Nat Rev Dis Primers. 2018;4:18008. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 353] [Cited by in RCA: 528] [Article Influence: 75.4] [Reference Citation Analysis (0)] |
| 44. | Mantani A, Kato T, Furukawa TA, Horikoshi M, Imai H, Hiroe T, Chino B, Funayama T, Yonemoto N, Zhou Q, Kawanishi N. Smartphone Cognitive Behavioral Therapy as an Adjunct to Pharmacotherapy for Refractory Depression: Randomized Controlled Trial. J Med Internet Res. 2017;19:e373. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 79] [Cited by in RCA: 103] [Article Influence: 12.9] [Reference Citation Analysis (0)] |
| 45. | Bauer M, Glenn T, Geddes J, Gitlin M, Grof P, Kessing LV, Monteith S, Faurholt-Jepsen M, Severus E, Whybrow PC. Smartphones in mental health: a critical review of background issues, current status and future concerns. Int J Bipolar Disord. 2020;8:2. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 101] [Cited by in RCA: 64] [Article Influence: 12.8] [Reference Citation Analysis (0)] |
| 46. | Sinha Deb K, Tuli A, Sood M, Chadda R, Verma R, Kumar S, Ganesh R, Singh P. Is India ready for mental health apps (MHApps)? PLoS One. 2018;13:e0203353. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 22] [Cited by in RCA: 30] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 47. | Nicholas J, Fogarty AS, Boydell K, Christensen H. The Reviews Are in: A Qualitative Content Analysis of Consumer Perspectives on Apps for Bipolar Disorder. J Med Internet Res. 2017;19:e105. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 94] [Cited by in RCA: 78] [Article Influence: 9.8] [Reference Citation Analysis (0)] |
| 48. | Van Ameringen M, Turna J, Khalesi Z, Pullia K, Patterson B. There is an app for that! Depress Anxiety. 2017;34:526-539. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 171] [Cited by in RCA: 134] [Article Influence: 16.8] [Reference Citation Analysis (0)] |