Published online Mar 22, 2023. doi: 10.5497/wjp.v12.i2.12
Peer-review started: November 25, 2022
First decision: January 31, 2023
Revised: February 13, 2023
Accepted: March 9, 2023
Article in press: March 9, 2023
Published online: March 22, 2023
Processing time: 115 Days and 12.9 Hours
Fluoroquinolones are a class of broad-spectrum antimicrobials used for various bacterial infections. Frequent use of fluoroquinolones has been questioned due to severe associated adverse effects, including dysglycemia (hypoglycemia or hyperglycemia) due to an alternation in glucose metabolism. Recent clinical trials showed the association of poor clinical outcomes with hypoglycemia in critically ill patients without diabetes. Many predisposing factors worsen fluoroquinolone-induced hypoglycemia, including diabetes, concomitant medication use like sulfonylureas or insulin, renal disease, and the elderly.
We report a case of recurrent hypoglycemia after ciprofloxacin initiation for a 71-year-old, non-diabetic, critically ill patient despite the presence of total parenteral nutrition and nasogastric tube feeding. The adverse drug reaction probability (Naranjo) scale was completed with a probable adverse drug reaction. The hypoglycemia resolved entirely after ciprofloxacin discontinuation.
Although ciprofloxacin-induced hypoglycemia is rare, special consideration is needed for the elderly due to their higher susceptibility to adverse side effects.
Core Tip: Fluoroquinolones are a class of broad-spectrum antimicrobials used to treat various bacterial infections. Frequent use has been doubted due to associated adverse severe effects, including hypoglycemia or hyperglycemia due to an alternation in glucose metabolism. Recent clinical trials showed the association of poor clinical outcomes with hypoglycemia in critically ill patients without diabetes, emphasizing the harm of severe hypoglycemia. Ciprofloxacin has demonstrated the lowest incidence in the class in the diabetic population. We report a case of recurrent ciprofloxacin-induced hypoglycemia for non-diabetic critically ill patient despite total parenteral nutrition and nasogastric tube feeding. The hypoglycemia resolved successfully after ciprofloxacin discontinuation.
- Citation: Dasuqi SA, Alshaer LM, Omran RA, Hamad MA. Recurrent ciprofloxacin induced hypoglycemia in a non-diabetic patient: A case report. World J Pharmacol 2023; 12(2): 12-17
- URL: https://www.wjgnet.com/2220-3192/full/v12/i2/12.htm
- DOI: https://dx.doi.org/10.5497/wjp.v12.i2.12
Fluoroquinolones are broad-spectrum antimicrobials used for different bacterial infections, especially for treating community-acquired pneumonia and intraabdominal and urinary tract infections. Fluoroquinolones exhibit bacteriostatic activity by inhibiting deoxyribonucleic acid (DNA) gyrase, the enzyme responsible for replicating DNA, while their bactericidal activity is achieved by bacterial DNA fragmentation[1].
The frequent use of fluoroquinolones has been questioned due to rare but severe associated adverse effects such as heart valve regurgitation, dysglycemia (hypoglycemia or hyperglycemia) due to alternations in glucose metabolism, and irreversible side effects to the musculoskeletal and nervous systems - most commonly tendonitis and tendon ruptures that can lead to potentially long-lasting disability[2-4]. Adverse drug events (ADEs) can be life-threatening, especially in the critically ill population. Many factors like patient characteristics, environmental factors, and drug classes related to ADEs affect intensive care differently than general care units. Hypoglycemia was associated with increased intensive care unit (ICU) length of stay and increased utilization of mechanical ventilation, catecholamines, and renal replacement therapy[5].
Many predisposing factors are known to increase the incidence of hypoglycemia in patients treated with fluoroquinolones, including diabetes, concomitant use of some medication like sulfonylureas or insulin, renal insufficiency, and elderly (conventionally defined as greater than 65 years old)[6]. We report a case of recurrent hypoglycemia in a non-diabetic patient that resolved successfully after ciprofloxacin discontinuation.
Unexplained recurrent hypoglycemia.
On the first day following abdominal closure, enteral feeding was initiated through a nasogastric tube (NGT), and the following day total parenteral nutrition (TPN) was initiated to augment his nutritional state. As a result, his blood glucose readings rose and were maintained above 99 mg/dL for the rest of his stay. Furthermore, as the patient tolerated the NGT feeding well, it was gradually increased over the following days.
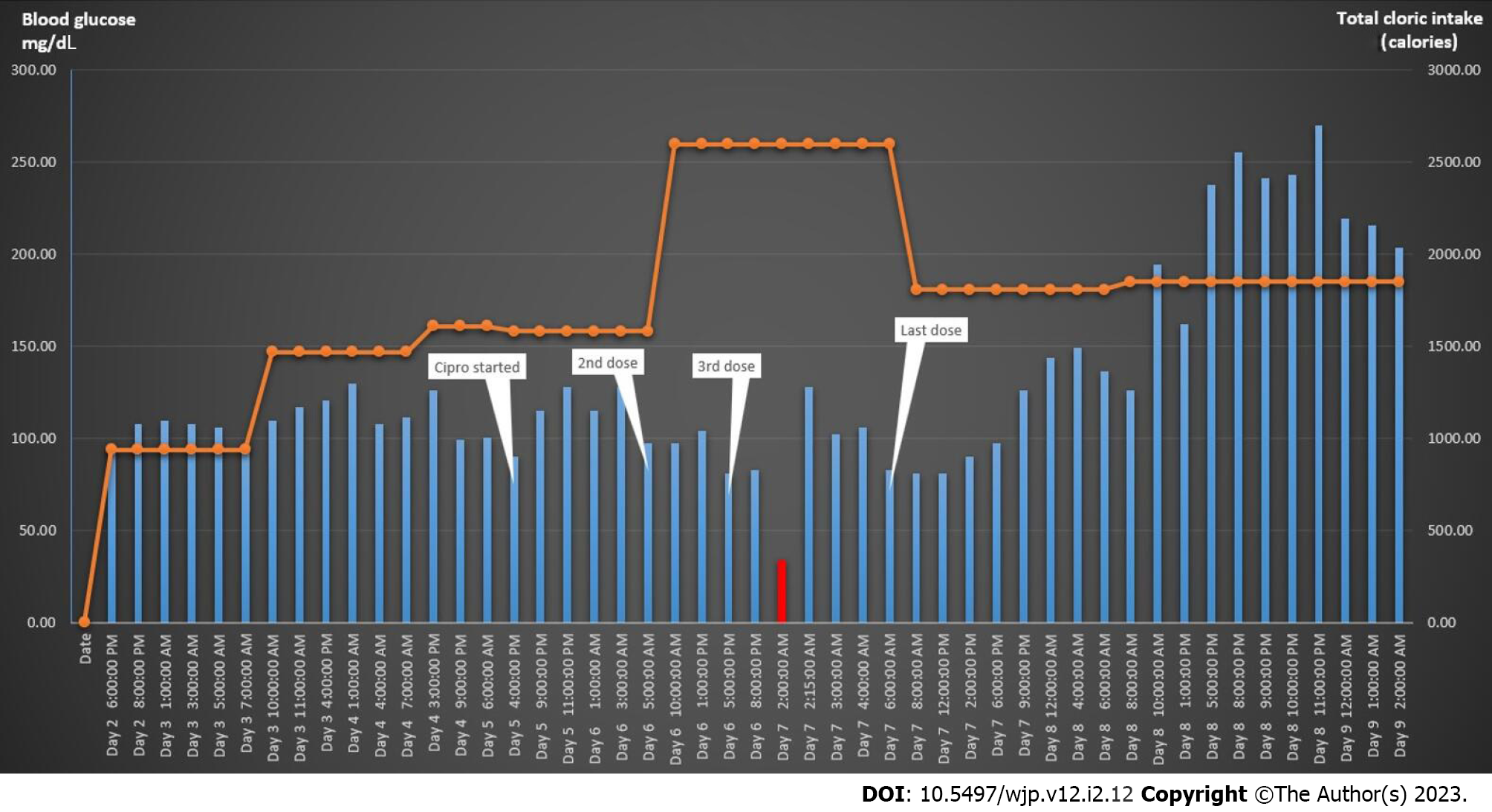
Due to worsening sepsis and increased vasopressor requirements, 400 mg of ciprofloxacin was administered intravenously (IV) every 12 h and adjusted accordingly on day two following surgery, based on a positive culture result. Approximately 30 h later, the patient had an episode of symptomatic hypoglycemia and received 12.5 mg of glucose IV, which somewhat improved his blood glucose level. However, his relatively low blood glucose readings continued despite increasing calories through TPN and NGT feeding. Therefore, Additional dextrose infusion was added to avoid further hypoglycemic episodes. After reviewing all the medications and evaluating his caloric intake during the daily rounds, we suspected that the ciprofloxacin might be the culprit behind the patient’s hypoglycemia. Retrospectively, we examined his most recent blood glucose readings and observed a downward trend in his blood glucose readings that started immediately following the second dose of ciprofloxacin refer to Figure 1. Accordingly, it was discontinued and the antimicrobial strategy was modified.
Our patient was a 71-year-old male who suffered from hypertension, peripheral vascular disease, and dyslipidemia, with a previous history of aortobifemoral bypass surgery. He was admitted to the hospital following a two-month complaint of abdominal pain. On admission his pain was moderate, and he was hemodynamically stable with a blood glucose concentration of 126 mg/dL, Glasgow Coma Scale/Score of 15/15, and unremarkable lab results.
He underwent exploratory laparotomy due to possible bowel ischemia, but only dusky bowel was found with no evidence of perforation or ischemia. His hospital course was complicated, requiring multiple ICU admissions for various reasons including sepsis, septic shock, acute kidney injury (AKI), abdominal fluid collection, and electrolyte imbalances.
One month after his hospital admission, he underwent another exploratory laparotomy due to wound dehiscence and a bowel perforation. Multiple micro-perforations in the small bowel and bowel ischemia were discovered during surgery, the abdomen was kept open, and he required three more surgeries afterward. His final fifth surgery was for abdominal closure.
Not relevant to the case.
Not relevant to the case.
Multiple glucose blood levels were recorded in correlation to ciprofloxacin administration.
Not relevant to the case.
Ciprofloxacin induced hypoglycemia.
Increasing calories through TPN and NGT feeding. Additional dextrose infusion was added as needed to maintain normal blood sugar. After ruling out other possible causes, ciprofloxacin was discontinued.
After 12 h of ciprofloxacin discontinuation, all his readings were 126 mg/dL, and the dextrose infusion was stopped. 24 h later, and despite decreasing the enteral feeding amount due to a high gastric residual resulting in a significant decrease in his total caloric intake, insulin infusion had to be initiated to control his blood glucose readings refer to Figure 1.
Recent clinical trials have shown a connection between poor clinical outcomes and hypoglycemia in critically ill patients without diabetes, emphasizing the harm caused by severe hypoglycemia and challenging the intensive glycemic control strategy to manage both diabetic and sever ill patients. Although hypoglycemia is unusual in patients without diabetes, many etiologies can cause hypoglycemia, including sepsis, liver diseases, malnutrition, alcohol-related illnesses, malignancies, post gastrectomy syndrome, and endocrine disorders[7].
Fluoroquinolones are antibiotics widely used to treat various bacterial infections, but several adverse effects have been reported with their use. In 2018, The US Food and Drug Administration (FDA) announced new drug safety communications regarding fluoroquinolones and the risk of hypoglycemia. Their reports showed that levofloxacin caused most of the incidents, followed by ciprofloxacin. In the end, the FDA strengthened the warnings to the prescriber that fluoroquinolone antibiotics may cause significant reductions in blood sugar and specific mental health side effects[8,9]. Many retrospective studies have shown that fluoroquinolones significantly interfere with glucose homeostasis and insulin secretion, leading to hypoglycemia and hyperglycemia events. The pathophysiological mechanism of hypoglycemia associated with fluoroquinolones is not yet fully understood. However, animal and in vitro studies hypothesized that fluoroquinolones block adenosine triphosphate-sensitive potassium channels in pancreatic β-cells, which in turn leads to an increase in insulin release[10-13].
Two large retrospective cohort studies by Mohr et al[14]and Aspinall et al[15] on diabetic outpatients revealed the high risks of hypoglycemia associated with fluoroquinolone treatment. However, the risk of a clinically-relevant dysglycemic event appears to vary highly among this class of drugs, with significantly greater risks for gatifloxacin and levofloxacin compared to ciprofloxacin. Chou et al[3] conducted a retrospective cohort study among 78433 outpatient diabetic patients for 22 mo; the study results identified an association between fluoroquinolones and a higher risk of hypoglycemia. Moxifloxacin was associated with the highest risk of hypoglycemia, followed by levofloxacin, with ciprofloxacin carrying the least risk[16].
Many case reports have documented levofloxacin-induced hypoglycemia in diabetic patients, and one case report detailed fatal hypoglycemia with ciprofloxacin in a diabetic patient with end-stage renal disease due to diabetic neuropathy[13,17-19].
A 2019 research article suggested an association between ciprofloxacin and hypoglycemia in patients without diabetes. They searched the World Health Organization’s global adverse drug reaction database using “ciprofloxacin” as the medicine name and “hypoglycemia” as the reaction term. A total of 35 cases from 17 countries were found since 1989 for patients without diabetes developed with ciprofloxacin-induced hypoglycemia, with a median time-to-onset of four days. The cases had a median age of 64 years (interquartile range, 50–85) with a balanced male-to-female ratio (but one of the limitations was that hyperinsulinemia or diabetes could not be ruled out)[17].
Our patient’s Naranjo Adverse Drug Reaction Probability Scale was six, which indicates a “probable adverse drug reaction”. However, the Naranjo score may have limitations in evaluating adverse drug reactions in critically ill patients, such as difficulty re-challenging patients, the inapplicability of placebo administration, possible lack of serum drug concentrations, and clarification of objective measurement.
Hyperglycemia is a known metabolic complication of TPN, due to the presence of dextrose as the primary energy source in TPN, that commonly occurs in diabetes mellitus or insulin-resistant patients. It can occur in patients without diabetes as well, with risk increasing due to the presence of other risk factors such as age, illness severity, and TPN infusion rate. Hypoglycemia, by contrast typically occurs in cases of excess insulin administration via parenteral nutrition solution. Usually, the risk of hypoglycemia increases along with certain patient characteristics (e.g. age), medications, and comorbidities (e.g. diabetes mellitus, mechanical ventilation, renal frailer, sepsis, and nutritional status)[12].
In our case, the patient was euglycemic from his initial hospital admission, despite developing severe sepsis and septic shock several times before that latest encounter without any episodes of hypoglycemia that eliminated the severe illness condition as the sole reason for hypoglycemia. Moreover, during the incident mentioned above, and in response to his low blood glucose readings, our medical team, nutritionist, and clinical pharmacist tried to address the issue by increasing the patient’s total caloric intake through various sources, including starting dextrose infusions, maximizing his TPN dose, and diluting all his IV medications in dextrose solutions. The risk of mechanical ventilation and AKI-induced hypoglycemia, as well as other possible comorbidities, are negligible for this case because these comorbidities did not induce hypoglycemic events before initiating ciprofloxacin. The only risk factor that may have predisposed our patient to hypoglycemia while receiving fluoroquinolone was his advanced age of 71. Renal function decreases as part of the usual aging pathophysiology, even without concurrent renal disease. That results in the accumulation of drugs that depends on renal excretion as the primary eliminated route, like ciprofloxacin. Impaired drug clearances affect the kinetics of drugs in prolonged half-lives, high drug serum concentration and increased side effects and toxicity[20].
Interestingly, after stopping ciprofloxacin, he started to become hyperglycemic, and although his caloric intake was reduced as a response, he required insulin infusion to achieve proper glycemic control.
The prevalence of ADEs increases with age due to age-related changes in pharmacokinetics and pharmacodynamics, increasing comorbidity burden, and polypharmacy. This makes older patients more sensitive to the side-effects of medications than their younger counterparts. A trained clinician can predict and detect ADEs in vulnerable patients by maintaining detailed documentation and regularly reviewing all prescribed and over-the-counter medications through standardized medication reconciliation. It is also important to outline clear therapeutic goals and recognize various drugs’ impacts on multiple organ systems for newly prescribed medications[15].
Although ciprofloxacin is rare to cause hypoglycemia, it can lead to fatal complications. Therefore, it should be prescribed carefully, after considering the patient's risk factors, especially the geriatric population who are more susceptible to adverse side-effects.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Endocrinology and metabolism
Country/Territory of origin: Saudi Arabia
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Su G, China S-Editor: Liu JH L-Editor: A P-Editor: Liu JH
| 1. | Silva F, Lourenço O, Queiroz JA, Domingues FC. Bacteriostatic versus bactericidal activity of ciprofloxacin in Escherichia coli assessed by flow cytometry using a novel far-red dye. J Antibiot (Tokyo). 2011;64:321-325. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 62] [Cited by in RCA: 73] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 2. | Watson MR, Ward CT, Prabhakar A, Fiza B, Moll V. Successful Use of Octreotide Therapy for Refractory Levofloxacin-Induced Hypoglycemia: A Case Report and Literature Review. Case Rep Crit Care. 2019;2019:3560608. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 3. | Chou HW, Wang JL, Chang CH, Lee JJ, Shau WY, Lai MS. Risk of severe dysglycemia among diabetic patients receiving levofloxacin, ciprofloxacin, or moxifloxacin in Taiwan. Clin Infect Dis. 2013;57:971-980. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 70] [Cited by in RCA: 80] [Article Influence: 6.7] [Reference Citation Analysis (0)] |
| 4. | United Kingdom governmental official website. Fluoroquinolone antibiotics: new restrictions and precautions for use due to very rare reports of disabling and potentially long-lasting or irreversible side effects. Drug safety update, Medicines & Healthcare products, Regulatory Agency Published March 21, 2019. |
| 5. | Krinsley JS, Grover A. Severe hypoglycemia in critically ill patients: risk factors and outcomes. Crit Care Med. 2007;35:2262-2267. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 461] [Cited by in RCA: 459] [Article Influence: 25.5] [Reference Citation Analysis (0)] |
| 6. | Kelesidis T, Canseco E. Quinolone-induced hypoglycemia: a life-threatening but potentially reversible side effect. Am J Med. 2010;123:e5-e6. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 15] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 7. | Kushimoto S, Abe T, Ogura H, Shiraishi A, Saitoh D, Fujishima S, Mayumi T, Hifumi T, Shiino Y, Nakada TA, Tarui T, Otomo Y, Okamoto K, Umemura Y, Kotani J, Sakamoto Y, Sasaki J, Shiraishi SI, Takuma K, Tsuruta R, Hagiwara A, Yamakawa K, Masuno T, Takeyama N, Yamashita N, Ikeda H, Ueyama M, Fujimi S, Gando S; JAAM FORECAST group. Impact of blood glucose abnormalities on outcomes and disease severity in patients with severe sepsis: An analysis from a multicenter, prospective survey of severe sepsis. PLoS One. 2020;15:e0229919. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 17] [Cited by in RCA: 30] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 8. | FDA reinforces safety information about serious low blood sugar levels and mental health side effects with fluoroquinolone antibiotics; requires label changes, Content current as of: October 7, 2018. Available from: https://www.fda.gov/drugs/drug-safety-and-availability/fda-reinforces-safety-information-about-serious-low-blood-sugar-levels-and-mental-health-side. |
| 9. | Michele G. Sullivan Fluoroquinolones can cause fatal hypoglycemia, FDA warns CHEST® Physician presented by MDedge Publish date: July 11, 2018. |
| 10. | Kelesidis T, Canseco E. Quinolone-induced hypoglycemia: a life-threatening but potentially reversible side effect. Am J Med. 2010;123:e5-e6. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 15] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 11. | Sako A, Yasunaga H, Matsui H, Fushimi K, Hamasaki H, Katsuyama H, Tsujimoto T, Goto A, Yanai H. Hospitalization with hypoglycemia in patients without diabetes mellitus: A retrospective study using a national inpatient database in Japan, 2008-2012. Medicine (Baltimore). 2017;96:e7271. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 20] [Cited by in RCA: 25] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 12. | Watson MR, Ward CT, Prabhakar A, Fiza B, Moll V. Successful Use of Octreotide Therapy for Refractory Levofloxacin-Induced Hypoglycemia: A Case Report and Literature Review. Case Rep Crit Care. 2019;2019:3560608. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 13. | Vallurupalli S, Huesmann G, Gregory J, Jakoby MG 4th. Levofloxacin-associated hypoglycaemia complicated by pontine myelinolysis and quadriplegia. Diabet Med. 2008;25:856-859. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 22] [Cited by in RCA: 20] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 14. | Mohr JF, McKinnon PS, Peymann PJ, Kenton I, Septimus E, Okhuysen PC. A retrospective, comparative evaluation of dysglycemias in hospitalized patients receiving gatifloxacin, levofloxacin, ciprofloxacin, or ceftriaxone. Pharmacotherapy. 2005;25:1303-1309. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 59] [Cited by in RCA: 60] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 15. | Aspinall SL, Good CB, Jiang R, McCarren M, Dong D, Cunningham FE. Severe dysglycemia with the fluoroquinolones: a class effect? Clin Infect Dis. 2009;49:402-408. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 57] [Cited by in RCA: 61] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 16. | Chou HW, Wang JL, Chang CH, Lee JJ, Shau WY, Lai MS. Risk of severe dysglycemia among diabetic patients receiving levofloxacin, ciprofloxacin, or moxifloxacin in Taiwan. Clin Infect Dis. 2013;57:971-980. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 70] [Cited by in RCA: 80] [Article Influence: 6.7] [Reference Citation Analysis (0)] |
| 17. | Lavan AH, Gallagher P. Predicting risk of adverse drug reactions in older adults. Ther Adv Drug Saf. 2016;7:11-22. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 162] [Cited by in RCA: 283] [Article Influence: 31.4] [Reference Citation Analysis (0)] |
| 18. | Berhe A, Russom M, Bahran F, Hagos G. Ciprofloxacin and risk of hypolycemia in non-diabetic patients. J Med Case Rep. 2019;13:142. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 9] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 19. | Matoi A, Taguchi M, Nishi S. Fatal hypoglycemia with ciprofloxacin in a dialysis patient: A case report. Clin Case Rep. 2021;9:1902-1904. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 1] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 20. | Giarratano A, Green SE, Nicolau DP. Review of antimicrobial use and considerations in the elderly population. Clin Interv Aging. 2018;13:657-667. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 29] [Cited by in RCA: 55] [Article Influence: 7.9] [Reference Citation Analysis (0)] |