Published online Apr 26, 2022. doi: 10.5495/wjcid.v12.i1.1
Peer-review started: June 7, 2021
First decision: October 18, 2021
Revised: November 9, 2021
Accepted: March 4, 2022
Article in press: March 4, 2022
Published online: April 26, 2022
Processing time: 322 Days and 7.2 Hours
The introduction of coronavirus disease-2019 (COVID-19) as a global pandemic has contributed to overall morbidity and mortality. With a focus on under
Core Tip: The novel Coronavirus disease-2019 (COVID-19) infection may present as a multiorgan disease, with the lung being the most commonly affected target organ. The clinical presentation, course, and outcome of COVID-19 are heterogeneous. Various imaging modalities can be employed to evaluate different disease stages depending on the affected organ or system, with X-ray, computed tomography, and ultrasound being the most commonly used. Imaging plays an essential role in the primary diagnosis of all manifestations of the disease and its related complications, evaluating disease severity and follow-up. Proper utilization of different imaging modalities and interpretation of the key imaging findings are essential for effective patient management and treatment.
- Citation: Ilieva E, Boyapati A, Chervenkov L, Gulinac M, Borisov J, Genova K, Velikova T. Imaging related to underlying immunological and pathological processes in COVID-19. World J Clin Infect Dis 2022; 12(1): 1-19
- URL: https://www.wjgnet.com/2220-3176/full/v12/i1/1.htm
- DOI: https://dx.doi.org/10.5495/wjcid.v12.i1.1
Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), the etiologic agent of coronavirus disease-2019 (COVID-19), caused a global pandemic dominated by acute respiratory failure mortality. COVID-19 manifestations are heterogeneous and overlapping. Therefore many challenges in the diagnostics and management of COVID-19 are still present[1]. In addition, typical symptoms without positive proof of infection (PCR/antigen tests) make the diagnosis inconclusive. However, a variety of imaging methods and techniques can be used for this purpose. Furthermore, imaging is also essential for classifying and managing patients during the infection.
Typically, imaging studies are carried out to determine the disease stage and estimate the organ involvement and severity. However, the features, such as ground-glass opacities (GGO), consolidations, interstitial fluid shifts, etc., seen on imaging are not unique to COVID-19. Therefore, a combination of the clinical picture and laboratory assessment is necessary to fully evaluate the patient’s state[2].
In the era of COVID-19, radiology plays a crucial role in the disease work-up and follow-up. Initially considered a purely pulmonary process, COVID-19 turned out to be a multisystemic disease that requires a comprehensive imaging approach, involving all techniques and studying all anatomical areas. As the primary manifestation of COVID-19 is a pneumonia-like respiratory process, the radiology modalities most involved in its diagnosis and follow-up are chest imaging, mainly chest X-ray (CXR) and chest computed tomography (CT). Diagnostic imaging capabilities show that CT is more sensitive than the gold standard RT-PCR for diagnosing COVID-19[2,3]. At the same time, it is cheaper and can be performed faster. The CT examination can give a quick, accurate diagnosis of patients, as the PCR test requires hours, even days, to complete as the number of COVID-19 infection cases grow. However, this comes with a large radiation dose, where the capacity is still lacking in many countries[4]. CXR is ubiquitous worldwide, with a 30–70-fold lower amount of radiation. Despite its low sensitivity and specificity, it is commonly performed as an initial investigation in COVID-19[4,5]. It is the modality of choice in the intensive care unit to detect disease progression and assess the position of the individual resuscitation means.
The imaging findings both on CXR and CT can be invaluable, especially for an atypical or organizing pneumonia with bilateral, multifocal randomly scattered GGO, in subpleural, mainly peripheral distribution with thickened pulmonary interstitium giving a reticular pattern, broncho-vascular prominence, and consolidation with increasing severity in the more seriously ill patients[6]. High-resolution CT (HRCT) with its modern available software techniques is the method of choice for an initial examination, staging, and follow-up of patients with suspected COVID infection. CT has higher sensitivity and specificity than radiography. On CT, the main changes are GGO, which tend to be more in the periphery, crazy paving changes are seen in later stages of the disease, thickening of the interstitium is also seen as well as dilation of the terminal lung vessels[7]. For staging of the changes seen on CT, we use the COVID-19 reporting and data system (CO-RADS) classification. It is a standardized classification proposed by the Dutch Radiological Society. It has 6 levels of suspicion from CO-RADS 1 to CO-RADS 6. In CO-RADS 1 patients, the exam is normal or has non-infectious changes. CO-RADS 2 patients have low levels of suspicion, and the visualized changes are consistent with infections other than COVID. CO-RADS 3 patients are those in which the changes are unclear, and there is an indeterminate level of suspicion. CO-RADS 4 and 5 staged patients have high and very high levels of suspicion for COVID- 19 infection, respectively. CO-RADS 6 patients are those who have typical changes and are PCR positive[8].
Chest ultrasound (US) plays a role in emergency settings as a COVID-19 screening technique. However, it is often of limited use as a highly operator-dependent method for lung disease. In addition, point of care echocardiography might have utility in hemodynamically unstable patients.
As stated above, various extrapulmonary manifestations have been reported, including in the gastrointestinal tract, brain, heart, kidneys, or muscles. The identification of most of these pathologies needs imaging, including abdominal CT, US, and magnetic resonance imaging (MRI). Imaging helps detect, diagnose, and assess the virus-induced injury and associated complications of the organs and systems affected by COVID-19. In suspected pulmonary thromboembolism (PTE) cases, CT pulmonary angiography (CTPA) may help correct the diagnosis. PTE is frequently observed in patients with more severe COVID-19 pneumonia involving mainly the segmental (90.2%) and subsegmental arteries (61.0%) of pulmonary segments affected by a consolidation pattern (67.6%)[9].
Furthermore, CXR, chest CT, and echocardiography can readily evaluate the signs of cardiac failure. However, myocardial injury can be best assessed using cardiac MRI. Potential neurovascular complications such as stroke, hemorrhage, or venous sinus thrombosis can be identified by non-enhanced head CT, and in the setting of a suspected infarct, a non-enhanced MRI of the brain can be performed for definitive assessment[10].
The disease may present as a multisystem hyperinflammatory syndrome in pediatric patients, currently termed pediatric multisystem inflammatory syndrome (PMIS). In children with PMIS, a broad spectrum of abdominal abnormalities can be detected by
both abdominal US and CT, with periportal and pericholecystic edema, gallbladder wall, and bowel wall thickening and dilatation, splenic infarcts, hepatosplenomegaly, right lower quadrant mesenteric lymphadenopathy, and free fluid in the pelvis being among the most commonly encountered abnormalities[10,11].
The COVID-19 pandemic has facilitated research on the implementation of artificial intelligence (AI), machine learning, and its subfield deep learning into imaging, which can be used as an essential adjunct or alternative to the diagnosis and follow-up assessment of progression and therapeutic development of the disease[12]. Deep learning is the most successful machine learning technique, which provides helpful analysis to study a large number of chest images that can critically impact the screening of COVID-19. AI algorithms have been developed to help with the early detection of COVID-19 both on CXR and CT. A deep learning model was also trained to discriminate between COVID and non-COVID pneumonia[13]. In line with this, CT pneumonia analysis (developed by Siemens Healthineers and partners) is another algorithm designed to automatically identify and quantify abnormal patterns in the lungs, enabling simple-to-use analysis of non-contrast chest CT scans for research purposes. The results could be used to analyze the severity and progression of abnormalities in patients exhibiting COVID-19 symptoms.
A person infected with SARS-CoV-2 who has not developed any signs or symptoms of COVID-19 is defined as an asymptomatic case. Immunological features, including any of the innate immunity pathways (i.e., natural killer (NK) cells, interferon, and other cytokine production), play a role at the onset of infection[14]. Stage I, or the asymptomatic incubation with or without detectable virus, is the period when treatment for improving immunity is given, such as the use of antiserums (ready-made antibodies from survivors), and is undoubtedly crucial[14]. However, due to the initial pathological changes in the target organs, sometimes imaging studies are the only way of detecting problems.
In asymptomatic individuals, this stage begins with inhalation of the SARS-CoV-2 virus replicating in the epithelial cells of the nasal cavity. It is well-known that the virus primarily uses the receptors for ACE2[15]; thus the first affected cells are ciliated cells. Therefore, PCR for SARS-CoV-2 RNA in nasal swabs can diagnose the virus at this point. The virus is then distributed in the lungs, digestive tract, reproductive system, etc., while innate immune tolerance is minimal[15].
It has been shown that asymptomatic persons can be infectious and secrete SARS-CoV-2, promoting the dissemination of COVID-19 – a significant concern from an epidemiological point of view. Moreover, while asymptomatic, some patients present with substantial lung changes, for example, when they seek medical attention. This observation requires a stringent search and examination of the interactions of proven infected persons with COVID-19 to diagnose asymptomatic infections[14].
According to the literature and personal experience of our team, the incidence of asymptomatic occurring COVID-19 infection is much higher, about four times more common than symptomatic moderate to severe ongoing cases[16]. The described histological changes in the respiratory system in an asymptomatic case of COVID-19 infection based on autopsy and biopsy are exceptional[17]. The only way to examine histological changes, mainly of the lung, in asymptomatic infection in the early stages of the disease is to take a biopsy for other pathological processes, “accidental” sampling of COVID-19, most often in the case of neoplastic diseases in which surgeries were performed for lung tumors at a time when superimposed infections were not recognized[16-20].
The main morphological changes found in routine histopathological examinations in the lungs are edema, proteinaceous exudate, focal reactive hyperplasia of pneumocytes, some with viral inclusions, and polymorphonuclear inflammatory infiltration composed mainly of lymphocytes and multinucleated giant cells. Hyaline membranes are scattered or not apparent in the early (asymptomatic) stage of COVID-19 infection, unlike in acute respiratory distress syndrome (ARDS). In addition, histologically, protein and fibrin exudates can be found in the lung parenchyma, as well as diffuse thickening of the alveolar walls, consisting of proliferating interstitial fibroblasts and type II pneumocystic hyperplasia, with random cell atypia and multinucleated giant cells, indicating varying degrees of the proliferative phase of diffuse alveolar damage. In some areas, an abundance of alveolar macrophages can be found together with type II pneumocystic hyperplasia[17,18,21].
Most patients with COVID-19 infection are diagnosed with pneumonia. The patients who have no symptoms could be transmitters. However, some asymptomatic patients progress quickly, even to ARDS. In asymptomatic patients, radiography has lower sensitivity and specificity than CT. In patients with slight changes, X-ray imaging can appear normal. This is why CT is the preferred method for diagnosis. Based on the published data, to date, almost all patients with COVID-19 have characteristic changes on CT[8,22].
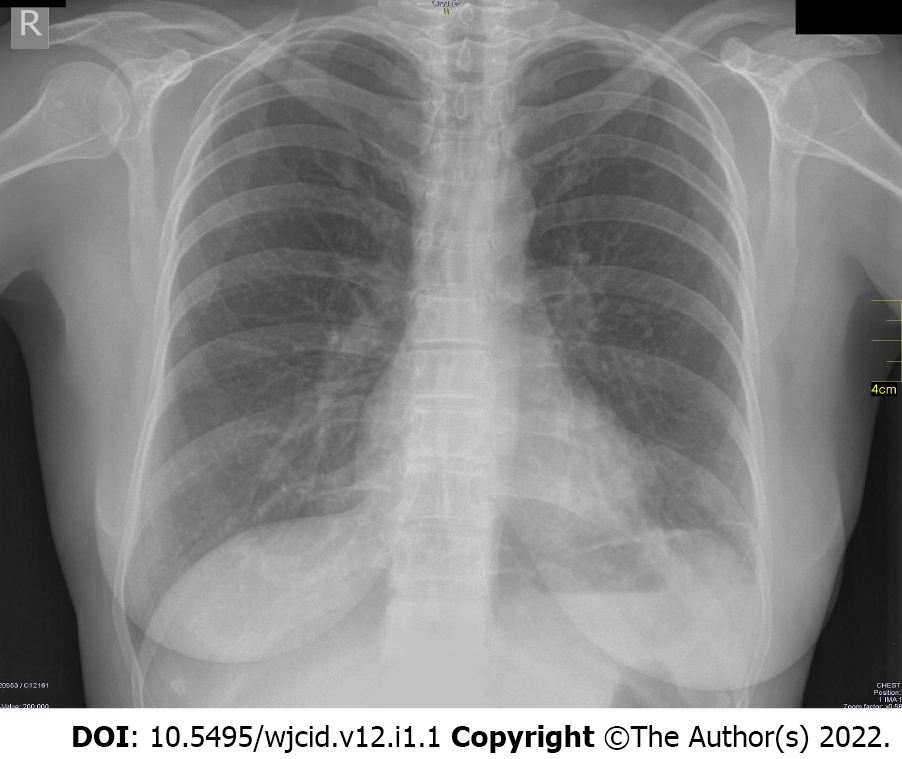
The X-ray of a 60-year-old female patient is presented in Figure 1. The patient had no symptoms, but a positive PCR test was performed because her husband had COVID pneumonia. Her X-ray showed no abnormalities. This is a typical case of an asymptomatic patient with negative radiography.
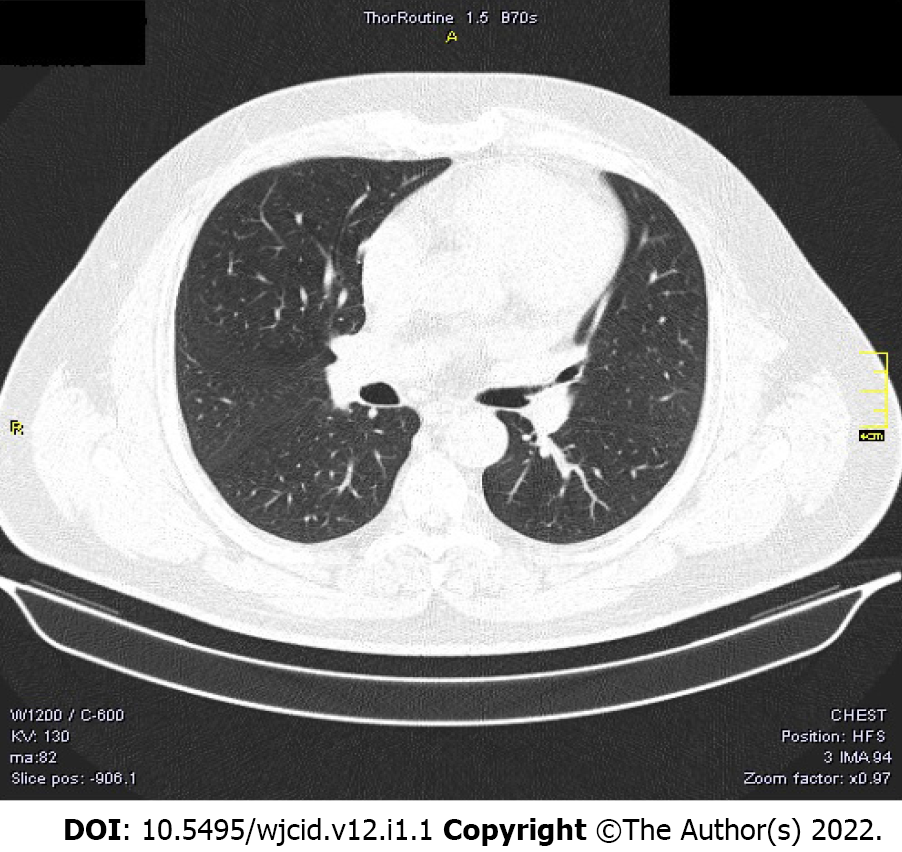
We also present the CT scan of a 45-year-old male, shown in Figure 2. He had no symptoms but a positive PCR test because he had been in contact with a verified COVID-19 patient. Both lungs showed no abnormalities, no infiltrates, no GGO, and no pleural effusions.
Atypical clinical findings in pregnant women with COVID-19 may increase the difficulty in establishing the diagnosis. Recently, data have demonstrated that pregnant women are more vulnerable to severe COVID-19, the development of complications, and death. CT is the favored approach for detecting pulmonary involvement early, especially in asymptomatic cases[22]. In asymptomatic children or those with atypical presentation of COVID-19, CT may be beneficial, especially in sparing time while waiting for PCR results or false-negative results.
In the case of pregnant women or children, it is always preferred to perform CT instead of waiting because any delay in confirming the diagnosis and management of the disease can be fatal and can contribute to the spread of the virus. Furthermore, the CT results in asymptomatic COVID-19 are usually distinct from the normal appearance, where the most common findings are GGO and consolidations in the lungs[22].
The onset of pneumonia in COVID-19 includes extreme antigen presentation, followed by enhanced production of C-reactive protein, D-dimer, and liver amino-transferases, accompanied by infiltrates in the lungs, representing involvement of antigen-presenting cells, T-helper cells, B cells, and NK cells[14].
The virus spreads across the airways in the respiratory tract and further to the gastrointestinal tract. It activates robust innate immune reactions. Nasal secretion, sputum or swabs contain SARS-CoV-2 but also early immune response molecules. Cytokine production during this stage may predict the clinical presentation and the subsequent disease course[23]. Significant amounts of interferon type I can confine the infection within the lungs, which is valid for approximately 80% of affected patients. Most of those with typical COVID-19 pneumonia on conservative symptomatic treatment can stay at home. However, about 20% of infected patients will progress to the next severe stage of the disease. Around 2% will develop life-threatening illnesses[23].
However, we have to keep in mind that COVID-19 pneumonia is a heterogeneous disease. It may include tracheobronchitis, vascular injury, and capillary microthrombi, along with inflammation[23]. Active injury leads to chronic and permanent lung trauma. The late effects of SARS-CoV-2 on the lungs have not been elucidated, but fibrosis development is suggestive.
Histologically, a hallmark of typical viral pneumonia is the interstitial nature of the inflammatory reaction. In addition, the most common morphologic changes in the lungs correlate with ARDS, which is described in the next section (Severe cases of COVID-19). On the other hand, no apparent morphological changes were observed in cardiac tissue due to the direct action of the coronavirus[17]. However, other findings established on necropsy material taken at autopsy are hypertrophy of cardiomyocytes with microscopic evidence of acute ischemia due to hypertensive heart disease and coronary artery atherosclerosis, but no other substantial damage[5].
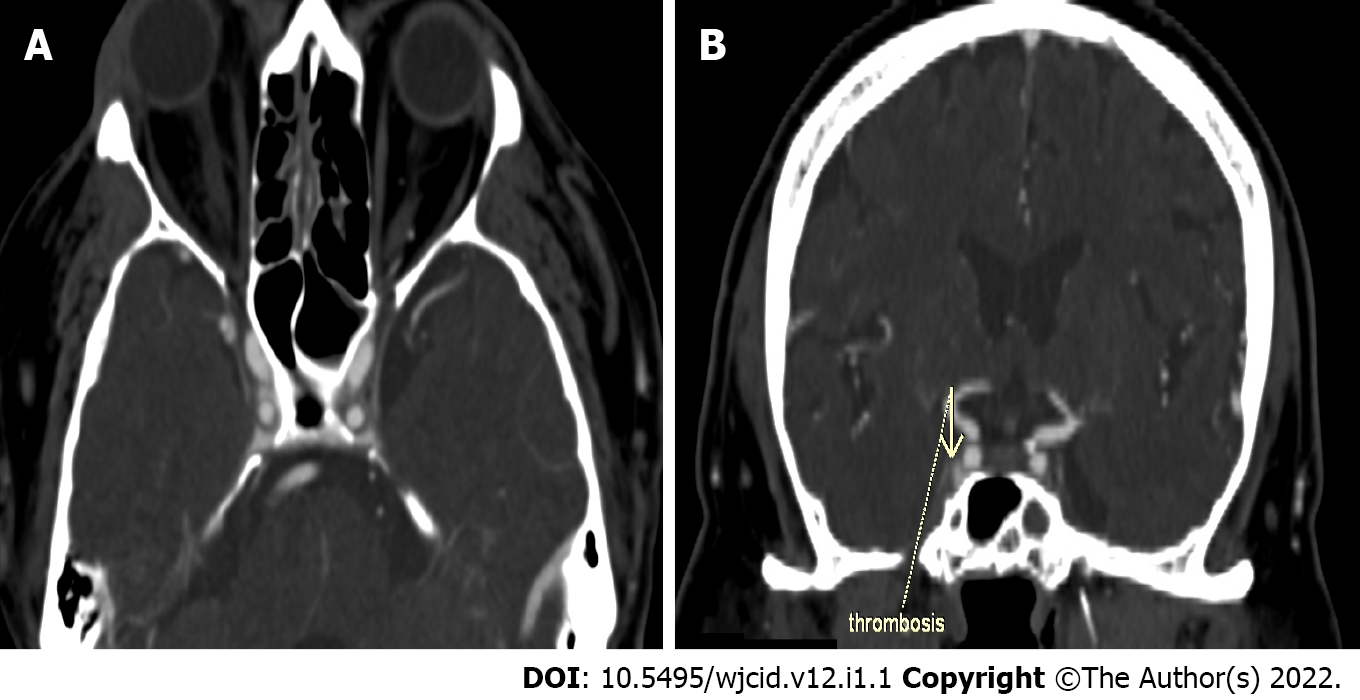
Interestingly, we documented a case of sinus cavernosus thrombosis in a 49-year-old man hospitalized with COVID-19 pneumonia. One week after hospitalization, he lost vision in his right eye, and presented with exophthalmos and swelling of the soft tissues around the eye. CT with contrast enhancement was performed immediately after the onset of symptoms. Thrombosis of the right sinus cavernosus is presented in Figure 3A and B.
COVID-19 pneumonia is classified as atypical pneumonia because it overlaps with the radiographic findings seen in interstitial pneumonia, including other coronavirus infections (SARS, MERS)[24,25]. Therefore, imaging methods are the first choice for diagnosing COVID-19 pneumonia including CXR and chest CT, with CT being a more sensitive and specific method than CXR, especially in the early stages of the disease[5].
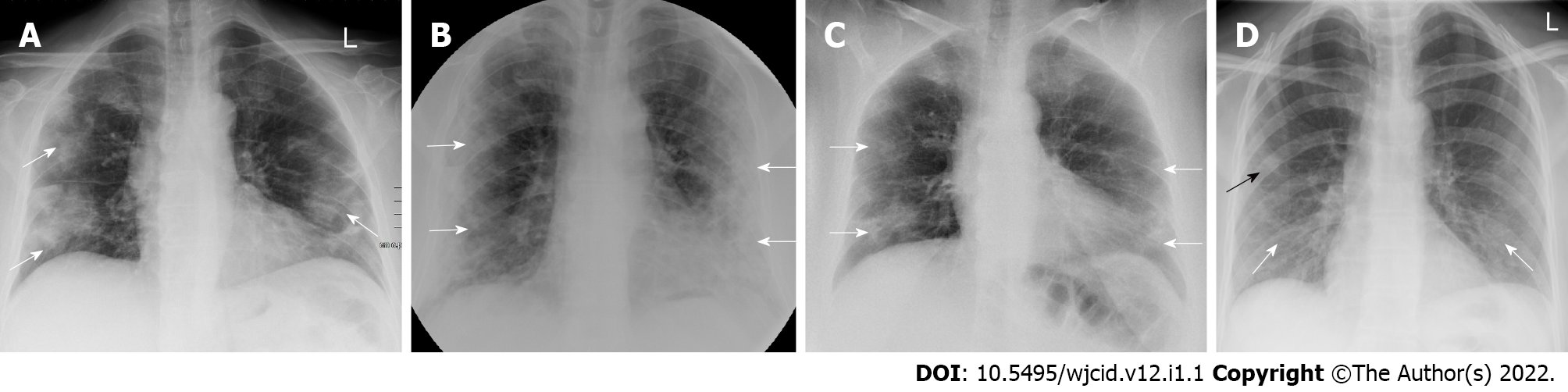
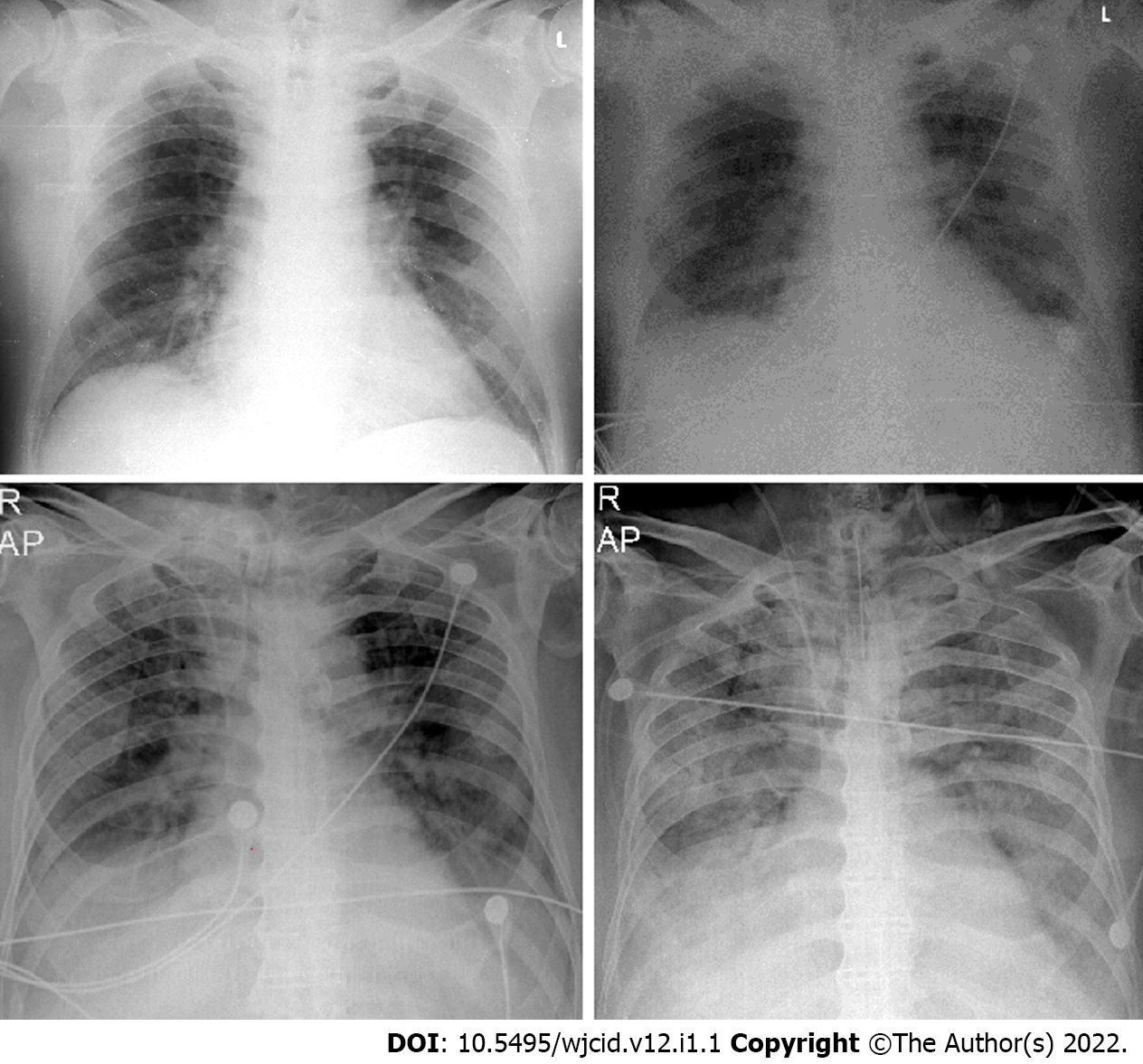
Imaging findings on conventional radiography range from normal findings to diffuse changes in the lung parenchyma. Patients with multiple comorbidities are more likely to have bilateral and diffuse lesions. Findings considered as highly specific for COVID-19 pneumonia on CRX are GGO (Figure 4A) and areas of non-segmental consolidation of parenchyma (Figure 4B) with peripheral and caudal distribution[26]. These findings are most pronounced 10-12 d after the onset of symptoms[27]. Additional findings are confluent ill-defined patchy opacities (Figure 4C), an interstitial lung pattern, decreased lung attenuation, inhomogeneous and linear parenchymal opacities (Figure 4D), and often different features are combined.
On the one hand, for intensive care unit patients, CRX plays a crucial role in detecting disease progression and assessing the position of the individual resuscitation means - endotracheal tubes, drains, and venous sources as it is performed at the patient’s bedside with a mobile X-ray machine[26].
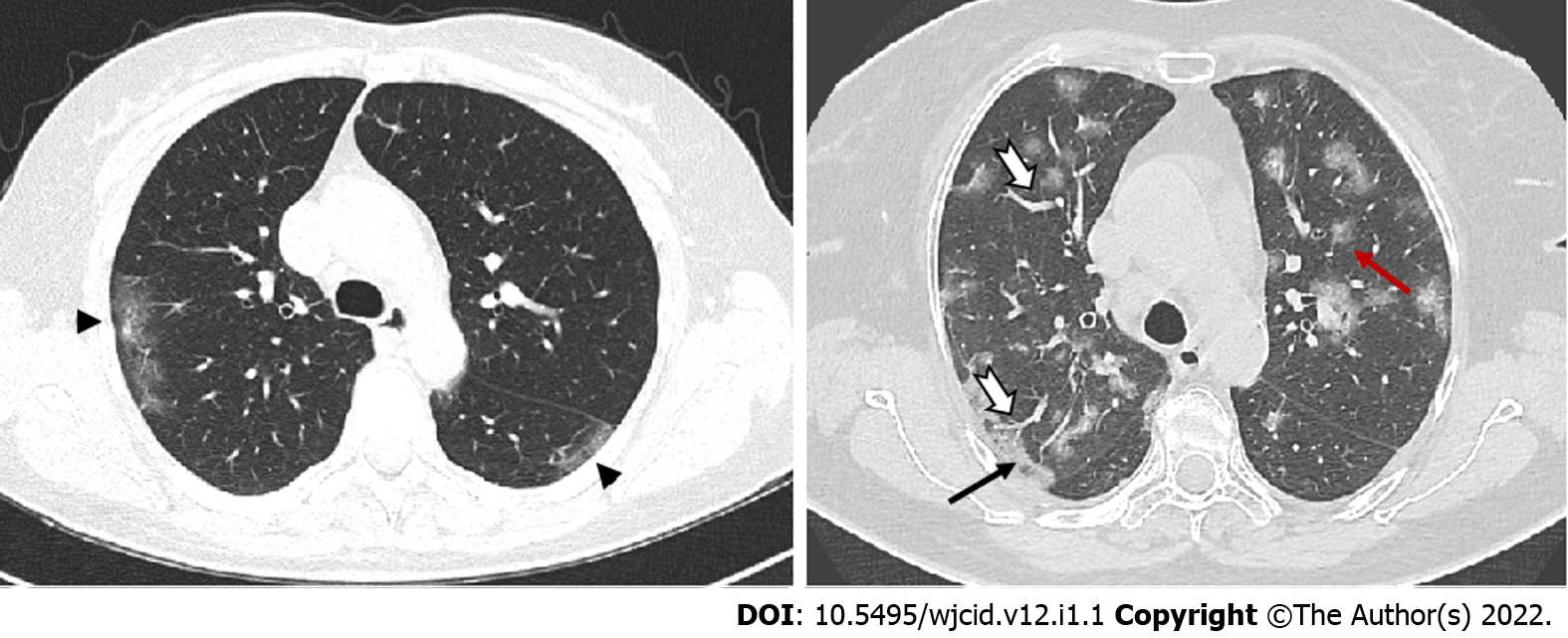
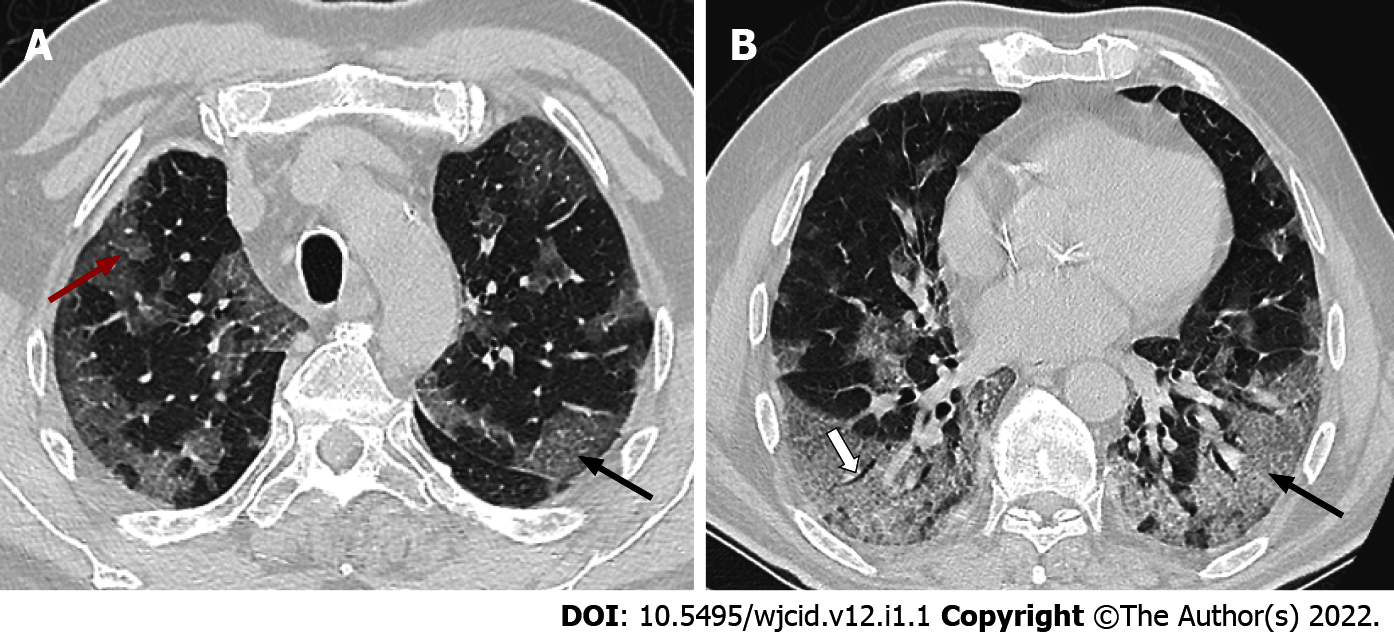
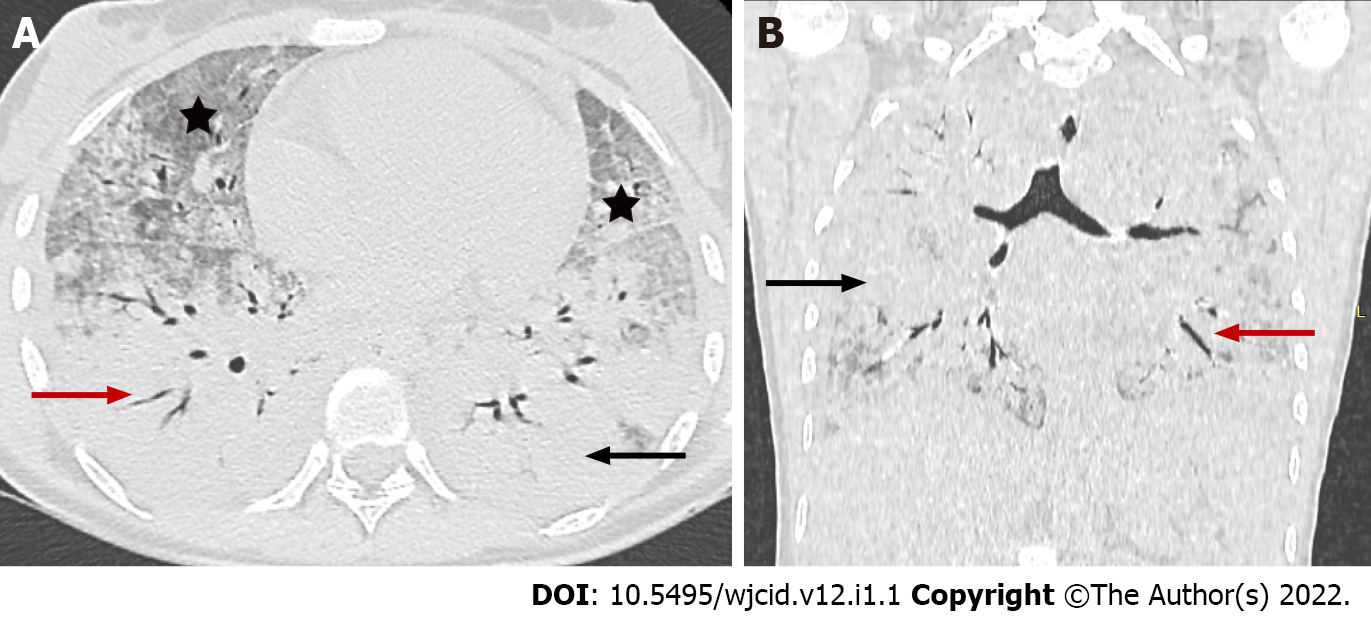
On the other hand, CT is a vital component in the diagnosis of suspected COVID-19 infection. CT features vary with the patient’s age, immunity status, disease stage, underlying diseases, and drug interventions at the time of scanning[28]. CT findings considered "typical" for COVID-19 pneumonia include GGO, parenchymal consolidations, and crazy-paving pattern (Figure 5)[29]. The changes are usually multifocal, bilateral with a peripheral subpleural distribution predominantly in the posterior segments of the inferior lobes[30,31].
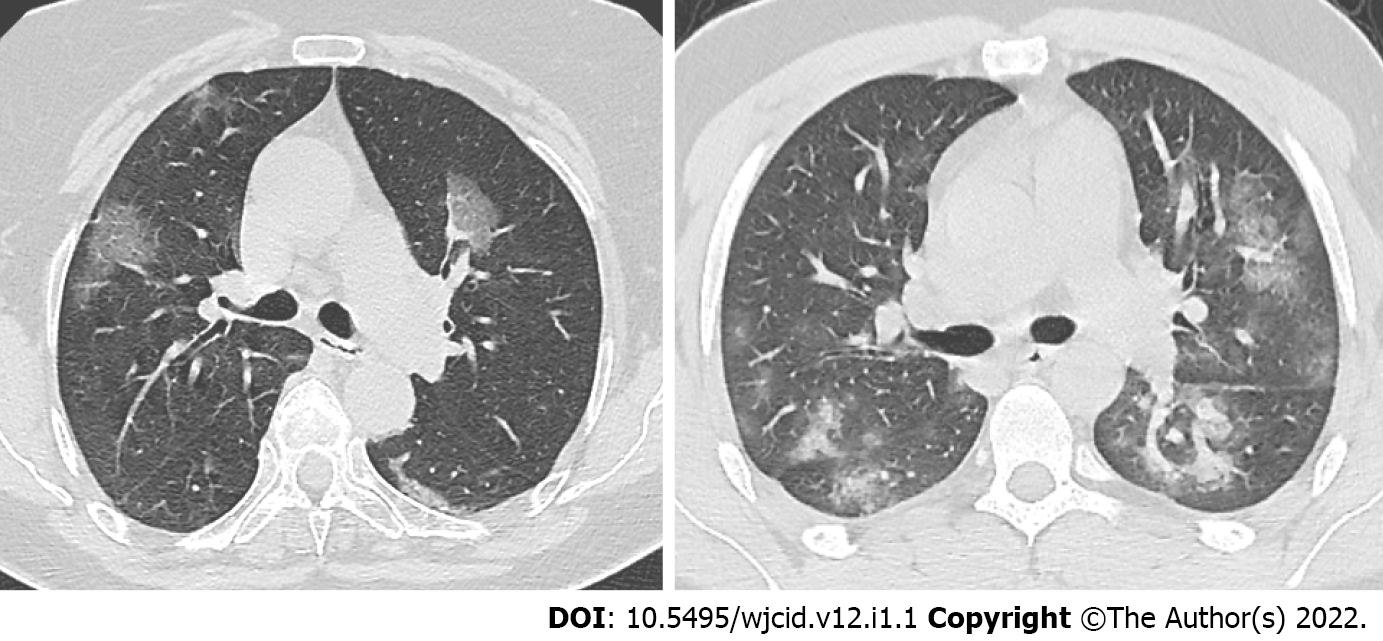
A GGO is the most frequent and earliest finding defined as increased attenuation on CT, which does not obscure the bronchovascular structures. It can be observed in three typical patterns: rounded, linear and crazy paving[30] (Figure 6). In the area of GGO, widening of vessels and traction bronchiectasis are commonly seen[32,33]. GGO with reticular interstitial thickening, known as crazy-paving, is defined as thickening of the pulmonary interstitium with thickened interlobular septae and visualization of intralobular pulmonary septae[34]. Crazy paving may be seen with areas of GGO or consolidation in the subacute to chronic phase of the disease[35] (Figure 7).
By definition, consolidation is a homogenous increase in the lung parenchyma's attenuation with obscuration of the underlying vessels (Figure 8) and bronchi[34]. Therefore, it is considered a sign of disease progression, especially in the intermediate and late stages of the disease[30,34].
The distribution of lung abnormalities was recorded as predominantly subpleural (involving mainly the peripheral one-third of the lung), random (without predilection for subpleural or central regions), or diffuse (continuous involvement without respect to lung segments)[33] (Figure 5). Additional CT features of COVID-19 pneumonia include vascular dilation, bronchial wall thickening, and traction bronchiectasis within the areas of GGO, architectural distortion with reticular thickening and subpleural bands formation, halo sign, or reversed halo sign (Figure 9). Changes considered atypical for COVID-19 pneumonia include lobar or segmental consolidations, small nodules (centrilobular lung nodules and tree-in-bud opacities), pulmonary cavitation, lymphadenopathy, and the presence of pleural or pericardial effusions[34].
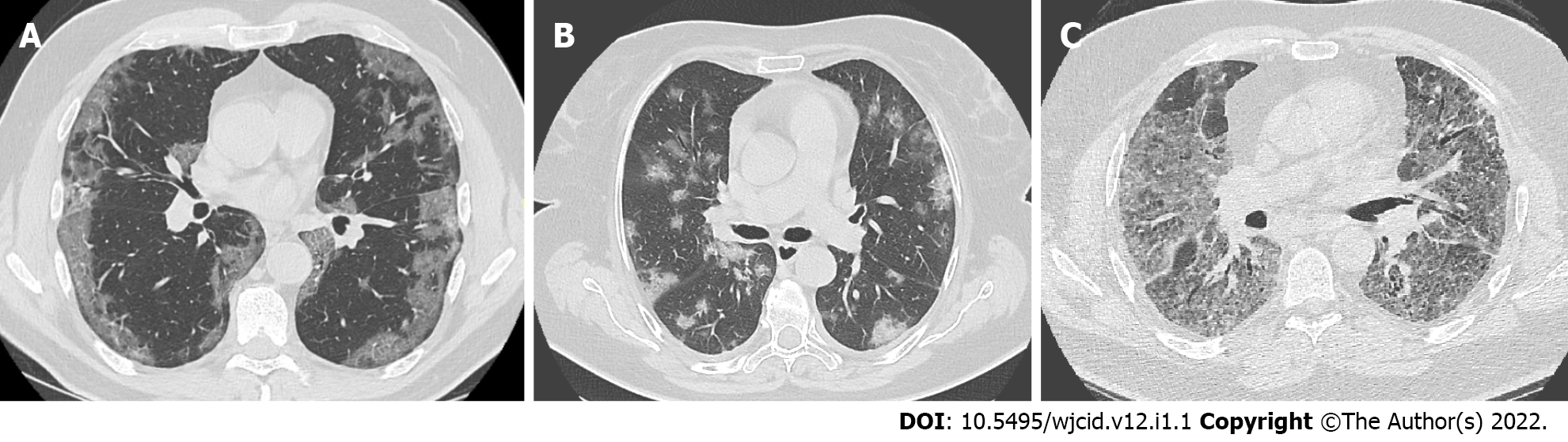
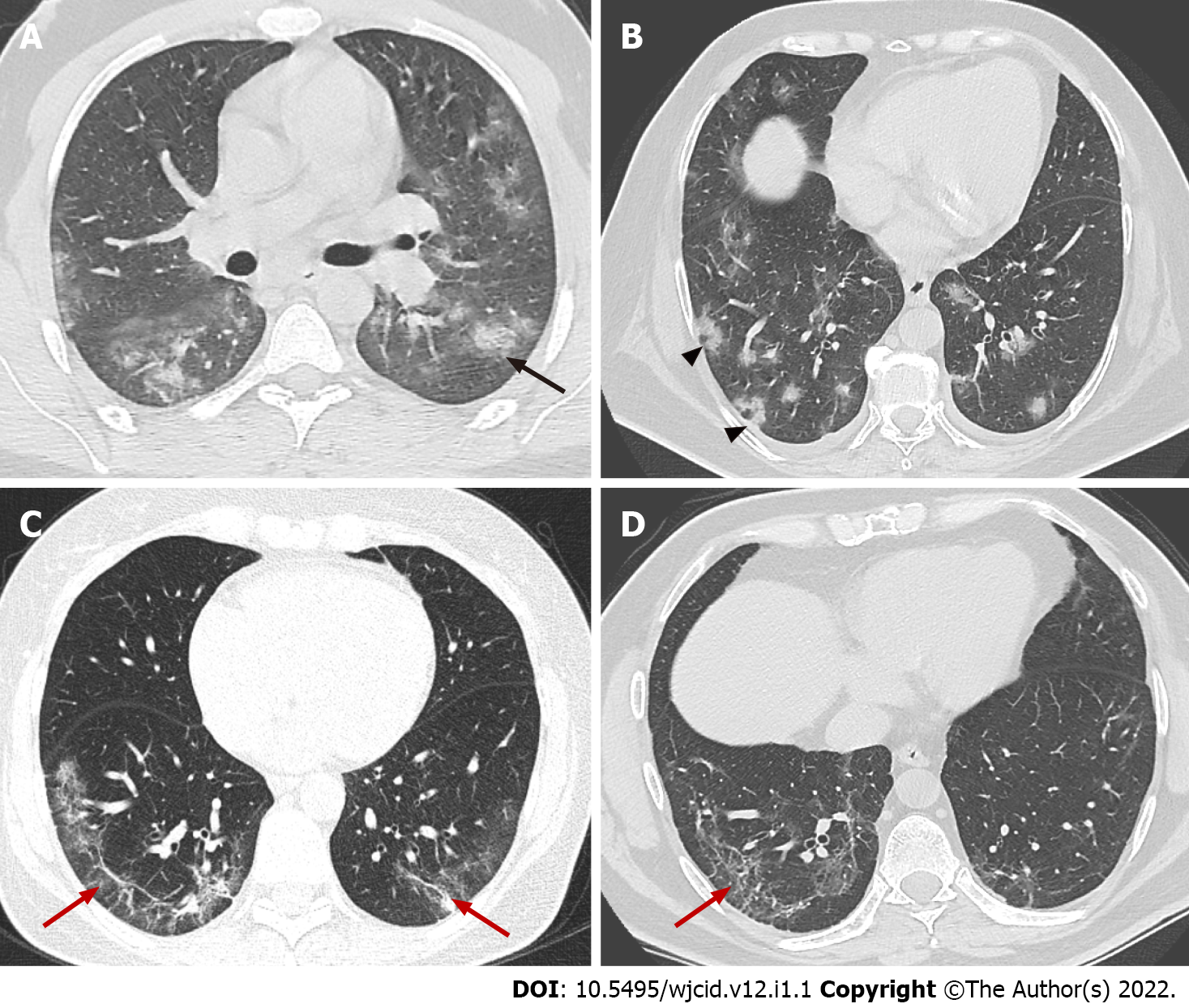
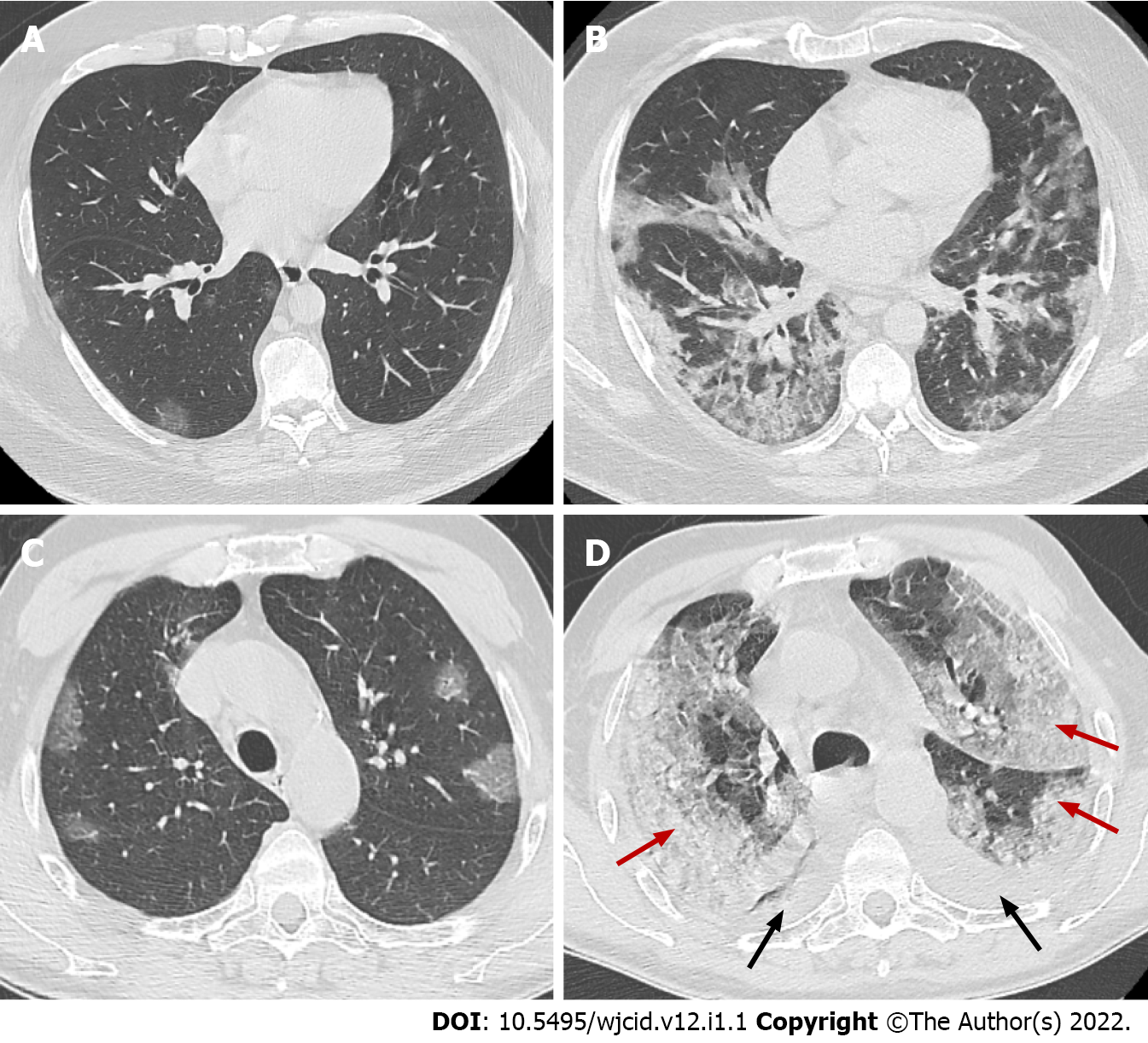
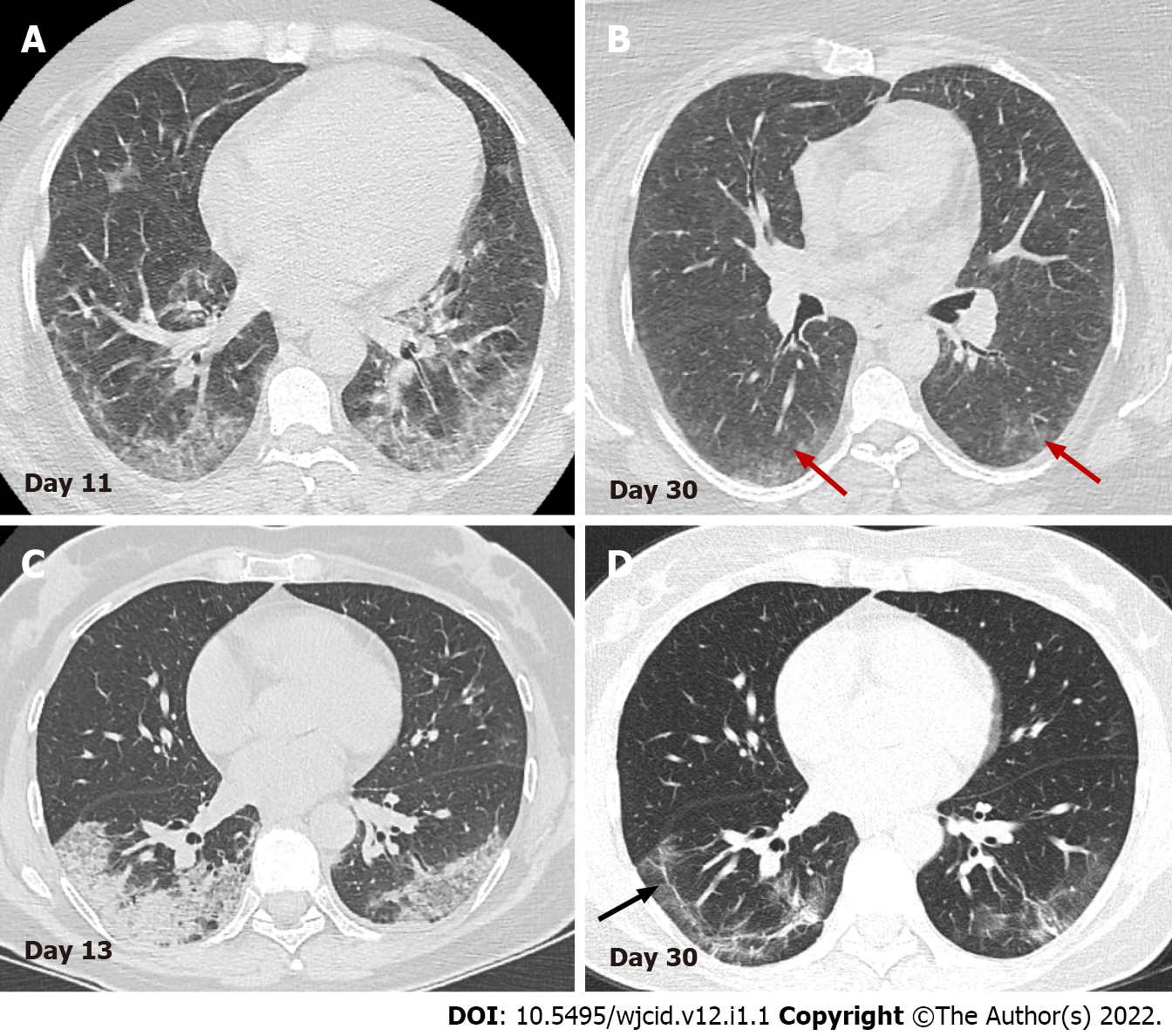
CT findings also vary depending on the onset of clinical symptoms. Approximately four stages of COVID-19 on chest CT have been described: (1) Early stage (0-5 d after onset of symptoms) marked by either normal or predominantly GGO (Figure 10); (2) Progressive stage (5-8 d after onset of symptoms) marked by enhanced GGO and a crazy-paving look (Figure 11A and B); (3) Peak stage (9-13 d after onset of symptoms) characterized by progressive consolidation (Figure 11C and D); and (4) Late stage (≥ 14 d after the onset of symptoms) denoted by a gradual decrease in consolidation and GGO, although signs of fibrosis (including parenchymal bands, architectural distortion, and traction bronchiectasis) may occur[31,36-39] (Figure 12). It should also be remembered that the temporal development and degree of lung defects are heterogeneous among different individuals, depending on the disease severity[31,36]. Similar findings can be observed in other viral types of pneumonia, pneumonia caused by Mycoplasma or Chlamydia, vasculitis, and connective tissue disease. Therefore, the clinical-laboratory correlation with the radiological finding is essential for the diagnosis of COVID-19 pneumonia.
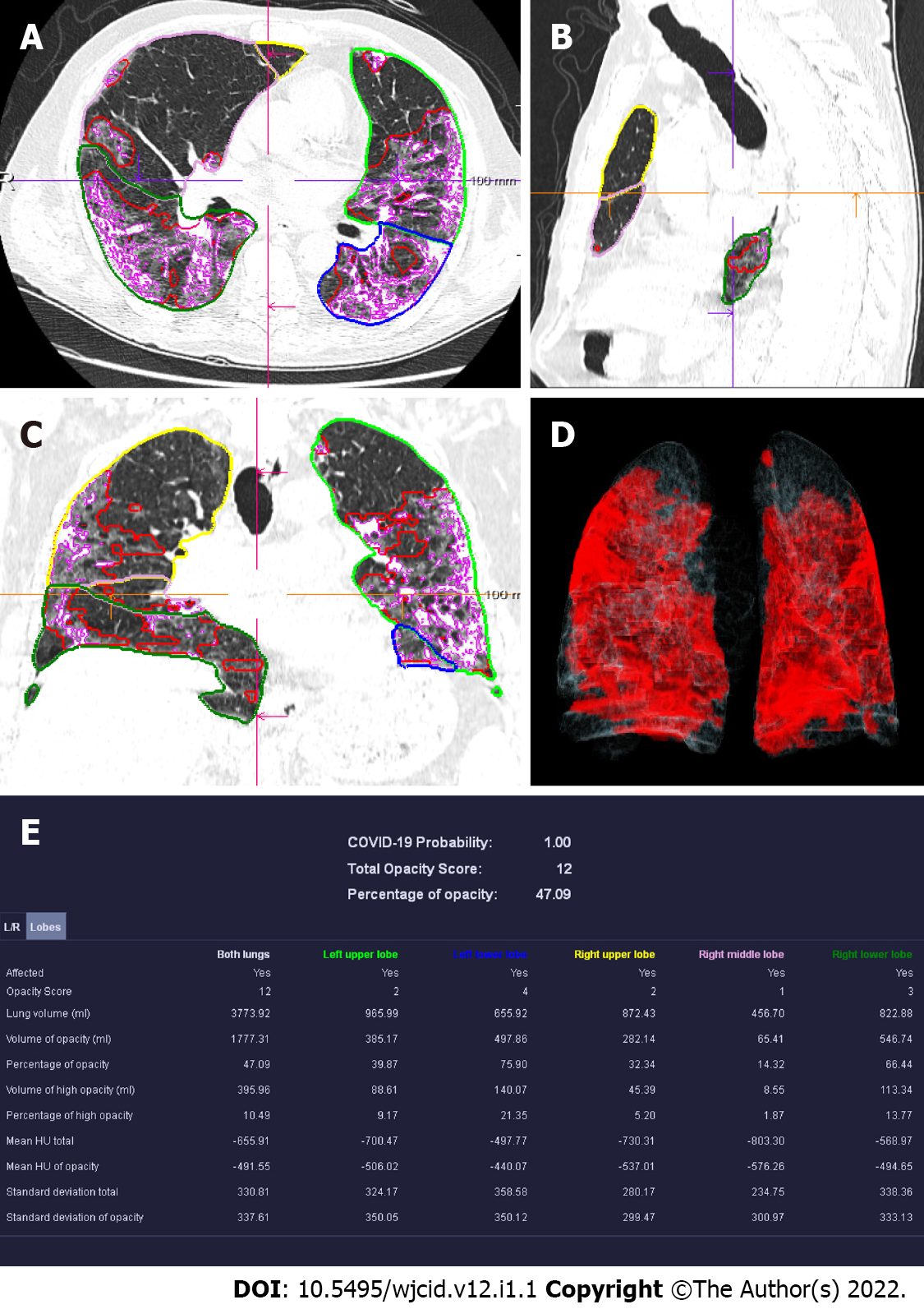
CT scanning can be a useful tool in evaluating the individual disease burden[40]. The quantitative severity can be assessed using a visual method or software that determines the percentage of affected lung volumes using deep learning algorithms[41,42]. Furthermore, the severity of lung involvement on CT correlates with the severity of the disease. It can be measured by scoring the percentages of each of the five lobes that are involved and can range from 0 (no involvement) to 25 (maximum involvement) when all five lobes show more than 75% involvement[41] (Figure 13).
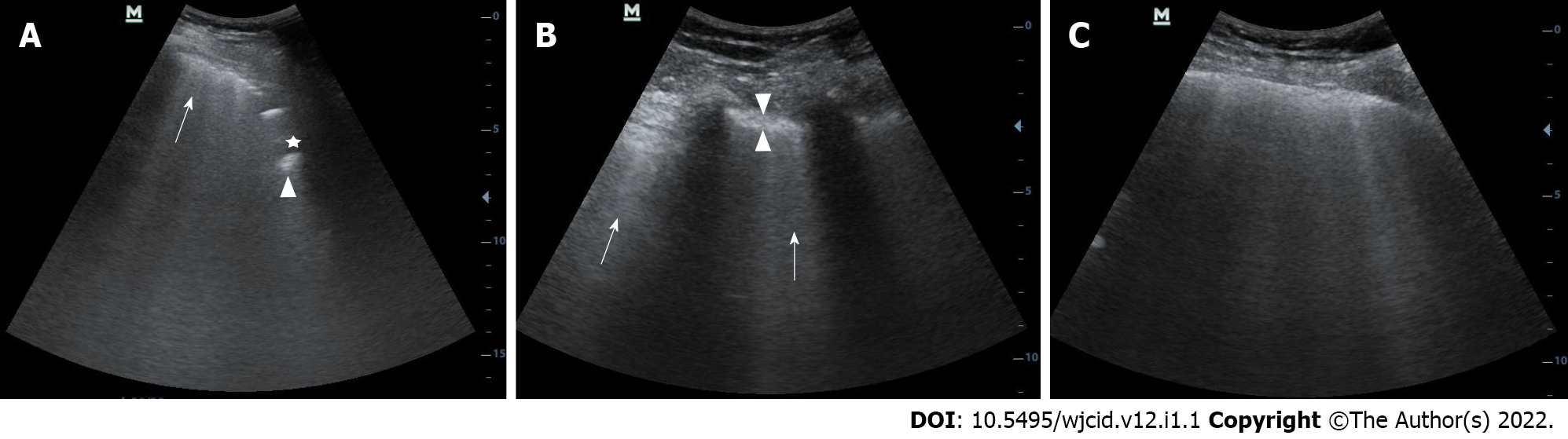
Lung ultrasound is increasingly used as a complementary method in diagnosing COVID-19 pneumonia. It allows assessment of both the lung parenchyma and the pleural space with the ability of bedside and real-time assessment of pulmonary function and changes. In addition, US can easily distinguish normally aerated from pathologically altered lung parenchyma. The most common findings observed in interstitial pneumonia are irregularly thickened pleura, B-lines, and subpleural consolidations of the parenchyma[43,44].
B-lines are vertical hyperechoic artifacts arising from the pleura that resemble a comet tail (Figure 14A) and move with the lung sliding. The increase in subpleural lung density (in the absence of consolidated tissue) may lead to the coalescence of many vertical artifacts in more extended echogenic patterns and a single homogeneous subpleural echogenic area can be seen. This phenomenon is known as “white lung”[44] (Figure 14B). In addition to B-lines, small, oval subpleural consolidations are visible in the parenchyma (Figure 14C). With disease progression to ARDS, the number of B-lines and parenchymal consolidations increases with the formation of sizeable gravitational consolidation[44], and the characteristic lung sliding is no longer visible. In the recovery phase of the disease, the consolidations and B-lines gradually disappear. Instead, A-line artifacts found in normally aerated parenchyma reappear and lung sliding is improved.
In some cases, COVID-19 pneumonia proceeds to the typical complications such as ARDS and cytokine storm. ARDS remains the most frequent immunopathological complication in SARS-CoV-2, SARS-CoV, and MERS-CoV viruses. The cytokine storm is one of the critical pathways for ARDS[45]. Both ARDS and cytokine storm represent an unregulated autoimmune inflammatory response arising from the release of significant quantities of pro-inflammatory cytokines (such as IFNg, IFNa, IL-1β, IL-6, IL-12, IL-18, IL-33, TNF-5-007, TGFβ, etc.) and chemokines (C-C Motif Chemokine Ligand 2 (CCL2), CCL3, CCL5, C-X-C motif ligand 8 (CXCL8), CXCL9, CXCL10, etc.) from immune or viral-infected cells[46]. Therefore, it is essential that these factors be detected and evaluated early. Thus, the appropriate therapy can be administered.
Histological examination of lung specimens in patients with severe infection is characterized by severe and extensive diffuse alveolar damage, fibromyxoid exudates, interstitial and intra-alveolar edema. However, in one of the cases described in the literature, the respiratory bronchial mucosa was intact, without evidence of squamous metaplasia. This is a significant difference compared with the pathology observed in the first epidemic of SARS[48]. In such patients, it is often found denuded with necrosis of type I pneumocytes and the formation of hyaline membrane and the proliferation of type II pneumocytes, which indicate ARDS in the acute stage without evidence of interstitial organization[17,21]. In addition, there is diffuse thickening of alveolar walls due to congestion, and patchy to mild mononuclear inflammatory infiltrate comprised of lymphocytes, macrophages, and some plasma cells. Perivascular lymphocyte aggregates have also been identified[47]. No eosinophils or neutrophils were identified, but if these are found, they usually suggest secondary bacterial infection[21,47]. Occasionally, in proliferated alveolar epithelial cells, viral inclusions in intranuclear and/or intracytoplasmic and multinucleated syncytial cells with atypical enlarged pneumocytes can be seen characterized by large eosinophilic nuclei with prominent nucleoli and granular cytoplasm (probably representing a viral effect similar to that reported in the first SARS epidemic)[17,47-49]. Common in ARDS, pulmonary thrombi and microangiopathy may be noted within a few small pulmonary artery branches and pleural adhesions[21,47]. This thrombotic process may involve activation of megakaryocytes, probably those that are naturally found in the lung, with platelet aggregation and platelet formation, in addition to fibrin deposition. The formation of small vascular thrombi in the lungs is often accompanied by focal alveolar hemorrhage[47,49].
With regard to imaging, COVID-19 related ARDS is diagnosed when a patient with confirmed COVID-19 infection meets the Berlin 2012 ARDS diagnostic criteria: acute hypoxemic respiratory failure; presentation within one week of worsening respiratory symptoms; bilateral airspace disease on CRX, CT, or US that is not fully explained by effusions, lung collapse, or nodules; and cardiac failure is not the primary cause of acute hypoxemic respiratory failure[50,51]. The risk factors for patients with COVID-19 to develop ARDS in the course of the disease are older age, concomitant conditions – most often hypertension and diabetes, and specific clinical symptoms on initial presentation such as marked dyspnea and fever ≥ 39°C[52]. However, clinical manifestations may be relatively mild regarding the severity of imaging findings in COVID-19[53].
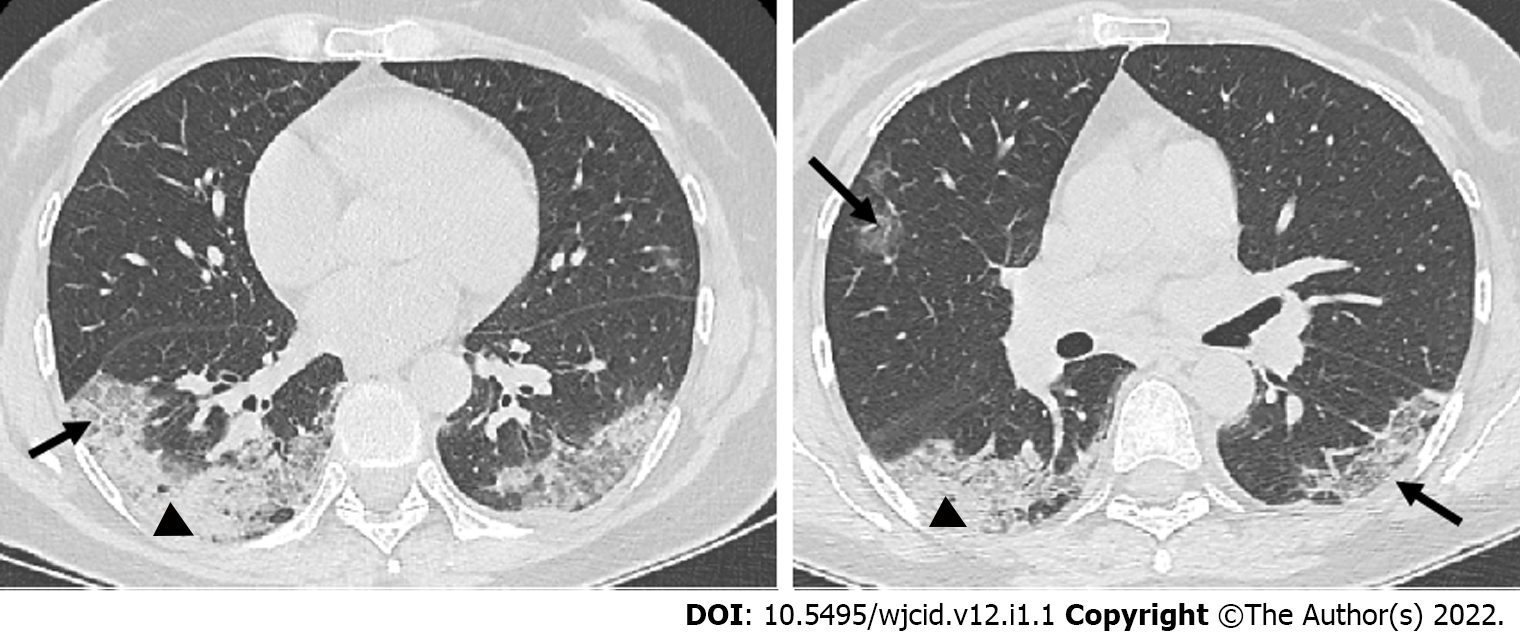
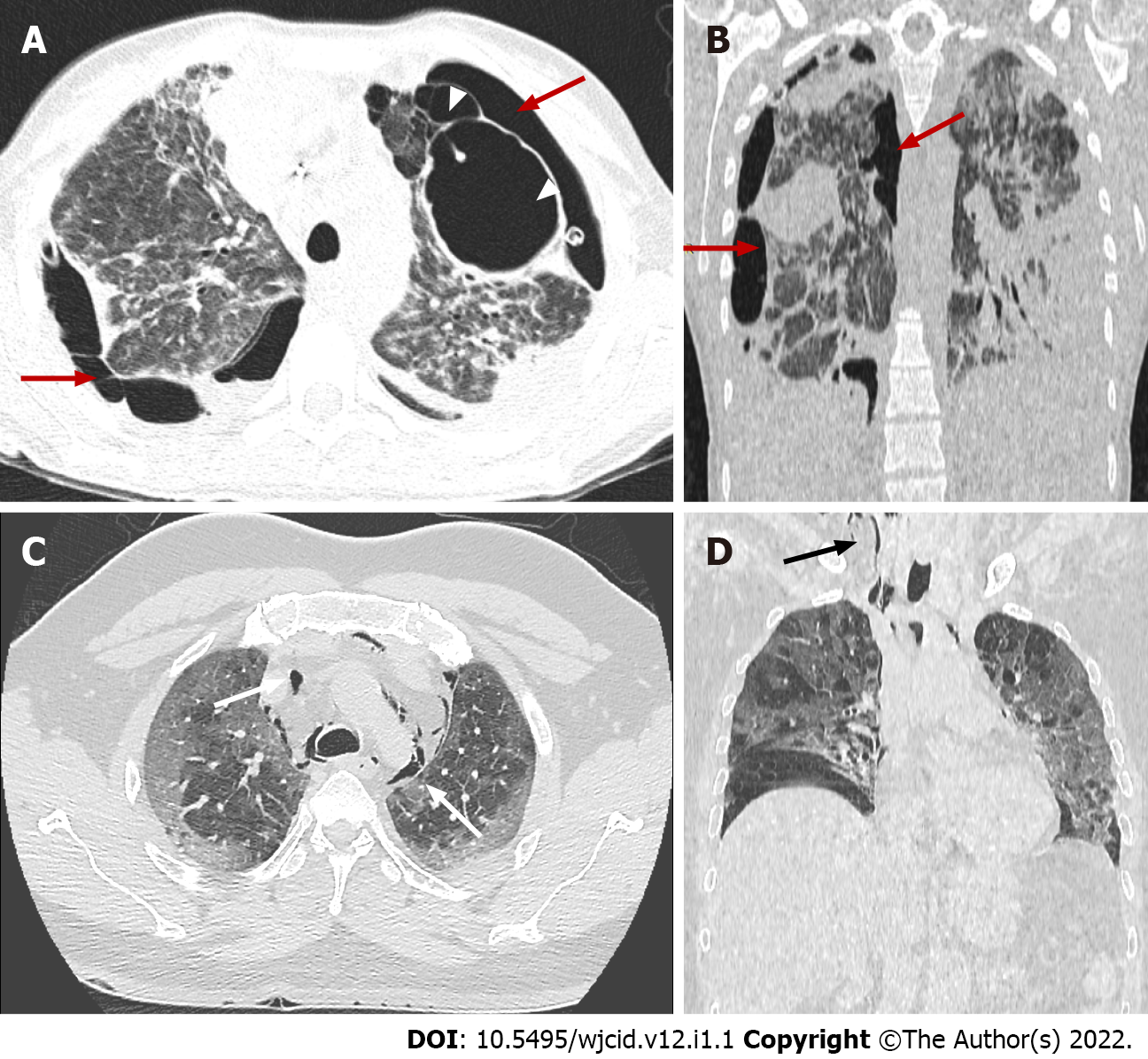
Imaging studies have an essential role in the initial evaluation of the pattern and extent of lung involvement and in the follow-up of hospitalized patients. Chest radiographic findings of ARDS are non-specific and resemble those of typical pulmonary edema or pulmonary hemorrhage with diffuse, patchy or homogeneous, bilateral, and coalescent opacities[54] (Figures 15 and 16). Radiography in the first 24 h of deterioration may be unchanged[55]. CT imaging features depend on the phase of the disease[56]. In the early exudative stage (first week), CT scans usually display a non-homogeneous distribution and ventrodorsal gradient of density. More dense consolidations are observed in dependent regions, extensive GGO, and comparatively regular or hyper-inflated parenchyma (in the case of mechanical ventilation) in non-dependent areas[54] (Figure 17).
In the late fibrotic phase (over two weeks), CT appearance can be variable. Complete resolution may occur in some cases, but the coarse reticular pattern and ground-glass opacification in the anterior (non-dependent) part of the lungs are considered more typical CT features. Pulmonary cysts of varying sizes and bullae have also been reported, which probably developed due to prolonged ventilation[56]. Subsequent imaging studies can show the development of pneumomediastinum, pneumothorax (often hypertensive in mechanically ventilated patients), and subcutaneous emphysema[54] (Figure 18).
The cytokine storm causes ARDS and multiorgan failure, leading to death in severe cases of coronavirus infections[45]. Although COVID-19 is known to cause pulmonary disease, including pneumonia and ARDS, various extrapulmonary manifestations of COVID-19 have been reported, affecting the gastrointestinal tract, brain, heart, kidneys, or muscles. Therefore, imaging helps to estimate the presence of complications and the extend of COVID-19.
Histologically, there is no noticeable viral cytopathic effect on the heart in the case of moderate infection on light microscopy[21,47]. However, liver biopsy specimens in patients with COVID-19 showed moderate fatty degeneration of hepatocytes and mild lobular and portal activity with slight interstitial mononuclear inflammatory infiltrates, indicating that the injury that could have been caused by either COVID-19 infection or drug-induced liver injury.
Тhe pathogenesis of kidney injury due to COVID-19 is not well-described. However, it seems to be multifactorial, involving mechanisms related to systemic hypoxia, coagulation disorders, inflammatory changes, or even cell destruction due to viruses. According to the literature, renal impairment was related to multiple organ failure[57]. Furthermore, post-mortem examination of the kidney from a patient who died of COVID-19 infection demonstrated that viral antigens accumulated in the renal tubules, inducing acute kidney injury[57].
Histological examination confirmed that a diffuse proximal tubular lesion, loss of brush border, non-isometric vacuolar degeneration, and a small area of necrosis were observed. In addition, interstitial inflammation and hemorrhage were found in some of the published cases, probably due to secondary bacterial infection[58]. However, most of these findings are caused by comorbidities. The renal changes described above may be directly due to COVID-19 infection. These pathological observations may only provide a basis for further study and investigation of COVID-19[58].
The main focus of COVID-19 is respiratory system complications, which are also a leading factor determining the severity of the disease course. More and more is known about the pathophysiology of the disease and the mechanism of lung damage. However, the extrapulmonary manifestations of the disease remain unclear, which in some cases is decisive for the disease course[59]. Cardiovascular complications are receiving increasing attention, and according to various studies range from 30 to 78%[60-62]. Cardiovascular disease (CVD) is known to be one of the main risk factors for severe disease. A study of 44672 patients with COVID-19 infection in China showed that a history of concomitant CVD was associated with nearly five-fold higher mortality (10.5% vs 2.3%) than patients without a history of CVD[63]. In addition, increasing evidence suggests that the virus may directly affect the cardiovascular system and lead to complications such as myocarditis, acute coronary syndrome, arrhythmias, and venous thromboembolism[64].
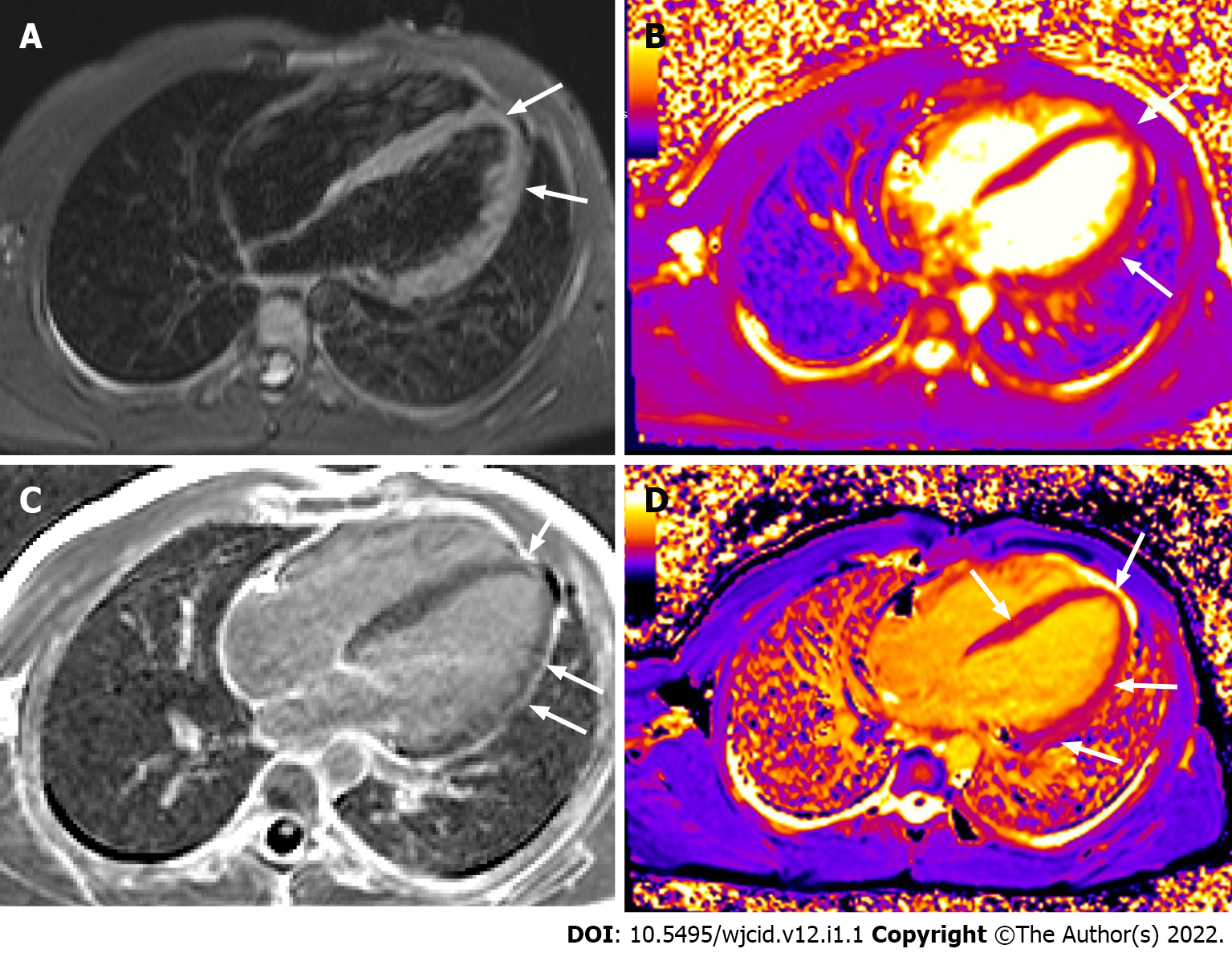
Cardiomagnetic resonance imaging (CMR) represents the gold standard in assessing the structure and function of the heart and provides information on the tissue characteristics of the myocardium. That, together with its non-invasive nature and lack of ionizing radiation, makes it essential for both early diagnosis and monitoring of cardiac complications due to COVID-19.
The pathogenesis of cardiac damage is currently unclear. However, presumed mechanisms include direct viral invasion, cytokine-mediated injury, a mismatch between needs and oxygen supply, and ischemic impairment resulting from microvascular thrombosis[65,66].
The CMR findings in the acute phase of the disease reported so far are based on small groups of patients. The presence of myocardial edema is a characteristic feature observed in almost all reported cases[67-70]. In a review of 31 publications with 51 patients, only one patient did not have edema at baseline, and two patients developed reversible edema within two weeks[68].
The extent of edema varies - from diffuse to limited to separate segments of the myocardium - most often in the LV inferior wall regions, the mid inferoseptal regions, and the apical region[68]. Another characteristic CMR sign is late gadolinium enhancement (LGE) of the myocardium due to necrosis/fibrosis following nonischemic myocardial injury localized at the sub-epicardial and/or intramural regions in the non-coronary territory. The presence and extent of zones of LGE correlate with the prognosis[68]. An additional feature in the acute phase of the disease is diffuse hypokinesis of the left and/or right ventricle and, much less frequently, segmental hypokinesis[68].
Similar CMR findings - edema, necrosis/fibrosis, and impaired systolic function are also found in patients following COVID-19 infection[62,67,69-71]. Signs of persistent inflammation with prolonged T2 relaxation time due to edema, prolonged T1 relaxation time and LGE with a different distribution, and pericardial enhancement are seen. In some cases, reduced ejection fraction[62] is found.
The cytokine storm is one of the leading causes of disseminated intravascular coagulation (DIC) affecting the entire organism. Pro-inflammatory cytokines, such as TNFa and IL-1, are able to inhibit endogenic anticoagulation. Inflammation injures the endothelium and results in activation of tissue plasminogen activator, which may explain the rise in D-dimer and fibrin degradation products[72,73]. In summary, COVID-19 is associated with a hypercoagulable disease and an elevated risk of thromboembolic complications.
The histological findings in organs other than lungs do not indicate significant changes directly related to COVID-19. However, the most commonly observed histological changes were due to thrombotic microangiopathy involving the lungs, spleen, and kidney. The most common complications which have been described in the literature include acute limb ischemia, aortic and mesenteric thrombosis, myocardial and brain infarction, and DIC[74].
A retrospective study on CTPA reported that pulmonary embolism in COVID-19 patients appears to be primarily distributed in the segmental arteries of the right lung[75]. Furthermore, only the determination of D-dimer and IL-6 at admission to CT scan appears to differentiate patients with pulmonary embolism from patients with a negative CT pulmonary angiogram. However, inter-individual heterogeneity calls for the establishment of cut-off values in COVID-19 patients in future research[76].
The pre-pandemic understanding of the predictive value of perfusion scintigraphy in assessing chronic thromboembolic disease and chronic thromboembolic pulmonary hypertension is well-established. Dhawan et al[75] proposed perfusion imaging as a triage tool for post-COVID-19 recovery. They suggested the potential of perfusion imaging to examine the in situ thrombotic small vessel signature of COVID-19. It is widely accepted that in situ thrombotic microbial pulmonary hypertension is present. Thus, lung perfusion imaging provides a primary triage instrument within the broader panel of investigations to enhance understanding of the natural history of thromboembolic phenomena in COVID-19 and distinguish hemodynamic sequelae from deconditioning dysfunctional breathing-related functional limitations. The authors also suggest that such imaging should be incorporated in routine post-COVID-19 follow-up pathways[75].
Early observed changes in critical organs such as lungs, kidneys, blood vessels, etc., might benefit the timely and appropriate treatment of COVID-19 to alleviate the complications and avoid fatal outcomes. Along with typical clinical and imaging results, atypical results are also beneficial. Early detection of pathological changes at different stages of life-threatening COVID-19 can improve patient management, treatment, and outcome.
Provenance and peer review: Unsolicited article; externally peer reviewed.
Peer-review model: Single blind
Specialty type: Infectious diseases
Country/Territory of origin: Bulgaria
Peer-review report’s scientific quality classification
Grade A (Excellent): A
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Bhatt KP, Omar BJ S-Editor: Liu JH L-Editor: Webster JR P-Editor: Liu JH
| 1. | WHO Headquarters. Clinical management of COVID-19. Interim guidance 2020; last access on 28/01/2021 Available from: https://www.who.int/publications/i/item/WHO-2019-nCoV-clinical-2021-2. |
| 2. | Ai T, Yang Z, Hou H, Zhan C, Chen C, Lv W, Tao Q, Sun Z, Xia L. Correlation of Chest CT and RT-PCR Testing for Coronavirus Disease 2019 (COVID-19) in China: A Report of 1014 Cases. Radiology. 2020;296:E32-E40. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3614] [Cited by in RCA: 3285] [Article Influence: 657.0] [Reference Citation Analysis (0)] |
| 3. | Fang Y, Zhang H, Xie J, Lin M, Ying L, Pang P, Ji W. Sensitivity of Chest CT for COVID-19: Comparison to RT-PCR. Radiology. 2020;296:E115-E117. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2088] [Cited by in RCA: 1873] [Article Influence: 374.6] [Reference Citation Analysis (2)] |
| 4. | Lin EC. Radiation risk from medical imaging. Mayo Clin Proc. 2010;85:1142-6; quiz 1146. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 306] [Cited by in RCA: 342] [Article Influence: 22.8] [Reference Citation Analysis (0)] |
| 5. | Borakati A, Perera A, Johnson J, Sood T. Diagnostic accuracy of X-ray versus CT in COVID-19: a propensity-matched database study. BMJ Open. 2020;10:e042946. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 93] [Cited by in RCA: 68] [Article Influence: 13.6] [Reference Citation Analysis (0)] |
| 6. | Sohail S. Rational and practical use of imaging in COVID-19 pneumonia. Pak J Med Sci. 2020;36:S130-S133. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 6] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 7. | Chervenkov L, Doykova K, Tsvetkova S. HRCT diagnosis and CORADS classification in patients with COVID-19 infection (2020) Rentgenologiya i radiologiya. ISSN 0486-400X, pp 220-223. |
| 8. | Ai T, Yang Z, Hou H, Zhan C, Chen C, Lv W, Tao Q, Sun Z, Xia L. Correlation of Chest CT and RT-PCR Testing for Coronavirus Disease 2019 (COVID-19) in China: A Report of 1014 Cases. Radiology. 2020;296:E32-E40. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3614] [Cited by in RCA: 3285] [Article Influence: 657.0] [Reference Citation Analysis (0)] |
| 9. | Cavagna E, Muratore F, Ferrari F. Pulmonary Thromboembolism in COVID-19: Venous Thromboembolism or Arterial Thrombosis? Radiol Cardiothorac Imaging. 2020;2:e200289. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 33] [Cited by in RCA: 37] [Article Influence: 7.4] [Reference Citation Analysis (0)] |
| 10. | Revzin MV, Raza S, Srivastava NC, Warshawsky R, D'Agostino C, Malhotra A, Bader AS, Patel RD, Chen K, Kyriakakos C, Pellerito JS. Multisystem Imaging Manifestations of COVID-19, Part 2: From Cardiac Complications to Pediatric Manifestations. Radiographics. 2020;40:1866-1892. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 64] [Cited by in RCA: 63] [Article Influence: 12.6] [Reference Citation Analysis (0)] |
| 11. | Hameed S, Elbaaly H, Reid CEL, Santos RMF, Shivamurthy V, Wong J, Jogeesvaran KH. Spectrum of Imaging Findings at Chest Radiography, US, CT, and MRI in Multisystem Inflammatory Syndrome in Children Associated with COVID-19. Radiology. 2021;298:E1-E10. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 88] [Cited by in RCA: 82] [Article Influence: 20.5] [Reference Citation Analysis (0)] |
| 12. | Desai SB, Pareek A, Lungren MP. Deep learning and its role in COVID-19 medical imaging. Intell Based Med. 2020;3:100013. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 41] [Cited by in RCA: 27] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 13. | Bai HX, Wang R, Xiong Z, Hsieh B, Chang K, Halsey K, Tran TML, Choi JW, Wang DC, Shi LB, Mei J, Jiang XL, Pan I, Zeng QH, Hu PF, Li YH, Fu FX, Huang RY, Sebro R, Yu QZ, Atalay MK, Liao WH. Artificial Intelligence Augmentation of Radiologist Performance in Distinguishing COVID-19 from Pneumonia of Other Origin at Chest CT. Radiology. 2020;296:E156-E165. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 260] [Cited by in RCA: 250] [Article Influence: 50.0] [Reference Citation Analysis (0)] |
| 14. | Velikova TV, Kotsev SV, Georgiev DS, Batselova HM. Immunological aspects of COVID-19: What do we know? World J Biol Chem. 2020;11:14-29. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 29] [Cited by in RCA: 28] [Article Influence: 5.6] [Reference Citation Analysis (1)] |
| 15. | Mason RJ. Pathogenesis of COVID-19 from a cell biology perspective. Eur Respir J. 2020;55. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 446] [Cited by in RCA: 514] [Article Influence: 102.8] [Reference Citation Analysis (1)] |
| 16. | Ouyang W, Yu J, Zhang J, Xie C. Alert to Potential Contagiousness: A Case of Lung Cancer With Asymptomatic Severe Acute Respiratory Syndrome Coronavirus 2 Infection. J Thorac Oncol. 2020;15:e82-e83. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 13] [Cited by in RCA: 12] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 17. | Tian S, Hu W, Niu L, Liu H, Xu H, Xiao SY. Pulmonary Pathology of Early-Phase 2019 Novel Coronavirus (COVID-19) Pneumonia in Two Patients With Lung Cancer. J Thorac Oncol. 2020;15:700-704. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 927] [Cited by in RCA: 1000] [Article Influence: 200.0] [Reference Citation Analysis (0)] |
| 18. | Al-Tawfiq JA. Asymptomatic coronavirus infection: MERS-CoV and SARS-CoV-2 (COVID-19). Travel Med Infect Dis. 2020;35:101608. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 127] [Cited by in RCA: 127] [Article Influence: 25.4] [Reference Citation Analysis (0)] |
| 19. | Joob B, Wiwanitkit V. Pulmonary Pathology of Early Phase 2019 Novel Coronavirus Pneumonia. J Thorac Oncol. 2020;15:e67. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 10] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 20. | Zhu J, Zhang Y, Gao XH, Xi EP. Coronavirus Disease 2019 or Lung Cancer: A Differential Diagnostic Experience and Management Model From Wuhan. J Thorac Oncol. 2020;15:e141-e142. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 12] [Cited by in RCA: 10] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 21. | Barton LM, Duval EJ, Stroberg E, Ghosh S, Mukhopadhyay S. COVID-19 Autopsies, Oklahoma, USA. Am J Clin Pathol. 2020;153:725-733. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 529] [Cited by in RCA: 606] [Article Influence: 121.2] [Reference Citation Analysis (0)] |
| 22. | Liu H, Liu F, Li J, Zhang T, Wang D, Lan W. Clinical and CT imaging features of the COVID-19 pneumonia: Focus on pregnant women and children. J Infect. 2020;80:e7-e13. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 221] [Cited by in RCA: 263] [Article Influence: 52.6] [Reference Citation Analysis (0)] |
| 23. | Borczuk AC, Salvatore SP, Seshan SV, Patel SS, Bussel JB, Mostyka M, Elsoukkary S, He B, Del Vecchio C, Fortarezza F, Pezzuto F, Navalesi P, Crisanti A, Fowkes ME, Bryce CH, Calabrese F, Beasley MB. COVID-19 pulmonary pathology: a multi-institutional autopsy cohort from Italy and New York City. Mod Pathol. 2020;33:2156-2168. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 295] [Cited by in RCA: 339] [Article Influence: 67.8] [Reference Citation Analysis (0)] |
| 24. | Cleverley J, Piper J, Jones MM. The role of chest radiography in confirming covid-19 pneumonia. BMJ. 2020;370:m2426. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 125] [Cited by in RCA: 94] [Article Influence: 18.8] [Reference Citation Analysis (0)] |
| 25. | Kooraki S, Hosseiny M, Myers L, Gholamrezanezhad A. Coronavirus (COVID-19) Outbreak: What the Department of Radiology Should Know. J Am Coll Radiol. 2020;17:447-451. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 272] [Cited by in RCA: 280] [Article Influence: 56.0] [Reference Citation Analysis (0)] |
| 26. | Cozzi D, Albanesi M, Cavigli E, Moroni C, Bindi A, Luvarà S, Lucarini S, Busoni S, Mazzoni LN, Miele V. Chest X-ray in new Coronavirus Disease 2019 (COVID-19) infection: findings and correlation with clinical outcome. Radiol Med. 2020;125:730-737. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 155] [Cited by in RCA: 181] [Article Influence: 36.2] [Reference Citation Analysis (0)] |
| 27. | Wong HYF, Lam HYS, Fong AH, Leung ST, Chin TW, Lo CSY, Lui MM, Lee JCY, Chiu KW, Chung TW, Lee EYP, Wan EYF, Hung IFN, Lam TPW, Kuo MD, Ng MY. Frequency and Distribution of Chest Radiographic Findings in Patients Positive for COVID-19. Radiology. 2020;296:E72-E78. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 832] [Cited by in RCA: 827] [Article Influence: 165.4] [Reference Citation Analysis (1)] |
| 28. | Jin YH, Cai L, Cheng ZS, Cheng H, Deng T, Fan YP, Fang C, Huang D, Huang LQ, Huang Q, Han Y, Hu B, Hu F, Li BH, Li YR, Liang K, Lin LK, Luo LS, Ma J, Ma LL, Peng ZY, Pan YB, Pan ZY, Ren XQ, Sun HM, Wang Y, Wang YY, Weng H, Wei CJ, Wu DF, Xia J, Xiong Y, Xu HB, Yao XM, Yuan YF, Ye TS, Zhang XC, Zhang YW, Zhang YG, Zhang HM, Zhao Y, Zhao MJ, Zi H, Zeng XT, Wang XH; , for the Zhongnan Hospital of Wuhan University Novel Coronavirus Management and Research Team, Evidence-Based Medicine Chapter of China International Exchange and Promotive Association for Medical and Health Care (CPAM). A rapid advice guideline for the diagnosis and treatment of 2019 novel coronavirus (2019-nCoV) infected pneumonia (standard version). Mil Med Res. 2020;7:4. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 881] [Cited by in RCA: 1137] [Article Influence: 227.4] [Reference Citation Analysis (0)] |
| 29. | Caruso D, Polidori T, Guido G, Nicolai M, Bracci B, Cremona A, Zerunian M, Polici M, Pucciarelli F, Rucci C, Dominicis C, Girolamo MD, Argento G, Sergi D, Laghi A. Typical and atypical COVID-19 computed tomography findings. World J Clin Cases. 2020;8:3177-3187. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 32] [Cited by in RCA: 27] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 30. | Bernheim A, Mei X, Huang M, Yang Y, Fayad ZA, Zhang N, Diao K, Lin B, Zhu X, Li K, Li S, Shan H, Jacobi A, Chung M. Chest CT Findings in Coronavirus Disease-19 (COVID-19): Relationship to Duration of Infection. Radiology. 2020;295:200463. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1728] [Cited by in RCA: 1597] [Article Influence: 319.4] [Reference Citation Analysis (1)] |
| 31. | Pan F, Ye T, Sun P, Gui S, Liang B, Li L, Zheng D, Wang J, Hesketh RL, Yang L, Zheng C. Time Course of Lung Changes at Chest CT during Recovery from Coronavirus Disease 2019 (COVID-19). Radiology. 2020;295:715-721. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1617] [Cited by in RCA: 1761] [Article Influence: 352.2] [Reference Citation Analysis (0)] |
| 32. | Kovács A, Palásti P, Veréb D, Bozsik B, Palkó A, Kincses ZT. The sensitivity and specificity of chest CT in the diagnosis of COVID-19. Eur Radiol. 2021;31:2819-2824. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 73] [Cited by in RCA: 105] [Article Influence: 21.0] [Reference Citation Analysis (0)] |
| 33. | Kanne JP, Little BP, Chung JH, Elicker BM, Ketai LH. Essentials for Radiologists on COVID-19: An Update-Radiology Scientific Expert Panel. Radiology. 2020;296:E113-E114. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 367] [Cited by in RCA: 421] [Article Influence: 84.2] [Reference Citation Analysis (0)] |
| 34. | Hansell DM, Bankier AA, MacMahon H, McLoud TC, Müller NL, Remy J. Fleischner Society: glossary of terms for thoracic imaging. Radiology. 2008;246:697-722. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2471] [Cited by in RCA: 2674] [Article Influence: 157.3] [Reference Citation Analysis (0)] |
| 35. | Nagpal P, Narayanasamy S, Vidholia A, Guo J, Shin KM, Lee CH, Hoffman EA. Imaging of COVID-19 pneumonia: Patterns, pathogenesis, and advances. Br J Radiol. 2020;93:20200538. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 33] [Cited by in RCA: 28] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 36. | Kwee TC, Kwee RM. Chest CT in COVID-19: What the Radiologist Needs to Know. Radiographics. 2020;40:1848-1865. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 263] [Cited by in RCA: 250] [Article Influence: 50.0] [Reference Citation Analysis (0)] |
| 37. | Wang Y, Dong C, Hu Y, Li C, Ren Q, Zhang X, Shi H, Zhou M. Temporal Changes of CT Findings in 90 Patients with COVID-19 Pneumonia: A Longitudinal Study. Radiology. 2020;296:E55-E64. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 493] [Cited by in RCA: 591] [Article Influence: 118.2] [Reference Citation Analysis (0)] |
| 38. | Pan Y, Guan H, Zhou S, Wang Y, Li Q, Zhu T, Hu Q, Xia L. Initial CT findings and temporal changes in patients with the novel coronavirus pneumonia (2019-nCoV): a study of 63 patients in Wuhan, China. Eur Radiol. 2020;30:3306-3309. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 564] [Cited by in RCA: 632] [Article Influence: 126.4] [Reference Citation Analysis (0)] |
| 39. | Guan CS, Lv ZB, Yan S, Du YN, Chen H, Wei LG, Xie RM, Chen BD. Imaging Features of Coronavirus disease 2019 (COVID-19): Evaluation on Thin-Section CT. Acad Radiol. 2020;27:609-613. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 106] [Cited by in RCA: 121] [Article Influence: 24.2] [Reference Citation Analysis (0)] |
| 40. | Francone M, Iafrate F, Masci GM, Coco S, Cilia F, Manganaro L, Panebianco V, Andreoli C, Colaiacomo MC, Zingaropoli MA, Ciardi MR, Mastroianni CM, Pugliese F, Alessandri F, Turriziani O, Ricci P, Catalano C. Chest CT score in COVID-19 patients: correlation with disease severity and short-term prognosis. Eur Radiol. 2020;30:6808-6817. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 507] [Cited by in RCA: 459] [Article Influence: 91.8] [Reference Citation Analysis (0)] |
| 41. | Li K, Fang Y, Li W, Pan C, Qin P, Zhong Y, Liu X, Huang M, Liao Y, Li S. CT image visual quantitative evaluation and clinical classification of coronavirus disease (COVID-19). Eur Radiol. 2020;30:4407-4416. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 458] [Cited by in RCA: 459] [Article Influence: 91.8] [Reference Citation Analysis (0)] |
| 42. | Lessmann N, Sánchez CI, Beenen L, Boulogne LH, Brink M, Calli E, Charbonnier JP, Dofferhoff T, van Everdingen WM, Gerke PK, Geurts B, Gietema HA, Groeneveld M, van Harten L, Hendrix N, Hendrix W, Huisman HJ, Išgum I, Jacobs C, Kluge R, Kok M, Krdzalic J, Lassen-Schmidt B, van Leeuwen K, Meakin J, Overkamp M, van Rees Vellinga T, van Rikxoort EM, Samperna R, Schaefer-Prokop C, Schalekamp S, Scholten ET, Sital C, Stöger JL, Teuwen J, Venkadesh KV, de Vente C, Vermaat M, Xie W, de Wilde B, Prokop M, van Ginneken B. Automated Assessment of COVID-19 Reporting and Data System and Chest CT Severity Scores in Patients Suspected of Having COVID-19 Using Artificial Intelligence. Radiology. 2021;298:E18-E28. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 100] [Cited by in RCA: 98] [Article Influence: 24.5] [Reference Citation Analysis (0)] |
| 43. | Peng QY, Wang XT, Zhang LN; Chinese Critical Care Ultrasound Study Group (CCUSG). Findings of lung ultrasonography of novel corona virus pneumonia during the 2019-2020 epidemic. Intensive Care Med. 2020;46:849-850. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 469] [Cited by in RCA: 509] [Article Influence: 101.8] [Reference Citation Analysis (1)] |
| 44. | Soldati G, Smargiassi A, Inchingolo R, Buonsenso D, Perrone T, Briganti DF, Perlini S, Torri E, Mariani A, Mossolani EE, Tursi F, Mento F, Demi L. Is There a Role for Lung Ultrasound During the COVID-19 Pandemic? J Ultrasound Med. 2020;39:1459-1462. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 298] [Cited by in RCA: 312] [Article Influence: 62.4] [Reference Citation Analysis (0)] |
| 45. | Van de Veerdonk F, Netea MG, van Deuren M, van den Hoogen FHJ, de Mast Q, Bruggemann R, van der Hoeven H. Kinins and Cytokines in COVID-19: A Comprehensive Pathophysiological Approach. 2020. [DOI] [Full Text] |
| 46. | Li X, Geng M, Peng Y, Meng L, Lu S. Molecular immune pathogenesis and diagnosis of COVID-19. J Pharm Anal. 2020;10:102-108. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1000] [Cited by in RCA: 937] [Article Influence: 187.4] [Reference Citation Analysis (0)] |
| 47. | Fox SE, Akmatbekov A, Harbert JL, Li G, Quincy Brown J, Vander Heide RS. Pulmonary and cardiac pathology in African American patients with COVID-19: an autopsy series from New Orleans. Lancet Respir Med. 2020;8:681-686. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 738] [Cited by in RCA: 903] [Article Influence: 180.6] [Reference Citation Analysis (0)] |
| 48. | Nicholls JM, Poon LL, Lee KC, Ng WF, Lai ST, Leung CY, Chu CM, Hui PK, Mak KL, Lim W, Yan KW, Chan KH, Tsang NC, Guan Y, Yuen KY, Peiris JS. Lung pathology of fatal severe acute respiratory syndrome. Lancet. 2003;361:1773-1778. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 799] [Cited by in RCA: 872] [Article Influence: 39.6] [Reference Citation Analysis (0)] |
| 49. | Xu Z, Shi L, Wang Y, Zhang J, Huang L, Zhang C, Liu S, Zhao P, Liu H, Zhu L, Tai Y, Bai C, Gao T, Song J, Xia P, Dong J, Zhao J, Wang FS. Pathological findings of COVID-19 associated with acute respiratory distress syndrome. Lancet Respir Med. 2020;8:420-422. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5228] [Cited by in RCA: 5782] [Article Influence: 1156.4] [Reference Citation Analysis (2)] |
| 50. | Gibson PG, Qin L, Puah SH. COVID-19 acute respiratory distress syndrome (ARDS): clinical features and differences from typical pre-COVID-19 ARDS. Med J Aust. 2020;213:54-56.e1. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 238] [Cited by in RCA: 429] [Article Influence: 85.8] [Reference Citation Analysis (0)] |
| 51. | ARDS Definition Task Force. Ranieri VM, Rubenfeld GD, Thompson BT, Ferguson ND, Caldwell E, Fan E, Camporota L, Slutsky AS. Acute respiratory distress syndrome: the Berlin Definition. JAMA. 2012;307:2526-2533. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1812] [Cited by in RCA: 4296] [Article Influence: 330.5] [Reference Citation Analysis (0)] |
| 52. | Wu C, Chen X, Cai Y, Xia J, Zhou X, Xu S, Huang H, Zhang L, Du C, Zhang Y, Song J, Wang S, Chao Y, Yang Z, Xu J, Chen D, Xiong W, Xu L, Zhou F, Jiang J, Bai C, Zheng J, Song Y. Risk Factors Associated With Acute Respiratory Distress Syndrome and Death in Patients With Coronavirus Disease 2019 Pneumonia in Wuhan, China. JAMA Intern Med. 2020;180:934-943. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4960] [Cited by in RCA: 5517] [Article Influence: 1103.4] [Reference Citation Analysis (1)] |
| 53. | Li X, Ma X. Acute respiratory failure in COVID-19: is it "typical" ARDS? Crit Care. 2020;24:198. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 440] [Cited by in RCA: 446] [Article Influence: 89.2] [Reference Citation Analysis (0)] |
| 54. | Zompatori M, Ciccarese F, Fasano L. Overview of current lung imaging in acute respiratory distress syndrome. Eur Respir Rev. 2014;23:519-530. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 62] [Cited by in RCA: 78] [Article Influence: 7.1] [Reference Citation Analysis (0)] |
| 55. | Desai SR. Acute respiratory distress syndrome: imaging of the injured lung. Clin Radiol. 2002;57:8-17. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 71] [Cited by in RCA: 62] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 56. | Sheard S, Rao P, Devaraj A. Imaging of acute respiratory distress syndrome. Respir Care. 2012;57:607-612. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 63] [Cited by in RCA: 74] [Article Influence: 5.7] [Reference Citation Analysis (0)] |
| 57. | Duarte PMA, Bastos Filho FAG, Duarte JVA, Duarte BA, Duarte IA, Lemes RPG, Duarte FB. Renal changes in COVID-19 infection. Rev Assoc Med Bras (1992). 2020;66:1335-1337. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 58. | Su H, Yang M, Wan C, Yi LX, Tang F, Zhu HY, Yi F, Yang HC, Fogo AB, Nie X, Zhang C. Renal histopathological analysis of 26 postmortem findings of patients with COVID-19 in China. Kidney Int. 2020;98:219-227. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1054] [Cited by in RCA: 1269] [Article Influence: 253.8] [Reference Citation Analysis (0)] |
| 59. | Babapoor-Farrokhran S, Gill D, Walker J, Rasekhi RT, Bozorgnia B, Amanullah A. Myocardial injury and COVID-19: Possible mechanisms. Life Sci. 2020;253:117723. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 228] [Cited by in RCA: 308] [Article Influence: 61.6] [Reference Citation Analysis (0)] |
| 60. | Guo T, Fan Y, Chen M, Wu X, Zhang L, He T, Wang H, Wan J, Wang X, Lu Z. Cardiovascular Implications of Fatal Outcomes of Patients With Coronavirus Disease 2019 (COVID-19). JAMA Cardiol. 2020;5:811-818. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2516] [Cited by in RCA: 2842] [Article Influence: 568.4] [Reference Citation Analysis (0)] |
| 61. | Giustino G, Croft LB, Stefanini GG, Bragato R, Silbiger JJ, Vicenzi M, Danilov T, Kukar N, Shaban N, Kini A, Camaj A, Bienstock SW, Rashed ER, Rahman K, Oates CP, Buckley S, Elbaum LS, Arkonac D, Fiter R, Singh R, Li E, Razuk V, Robinson SE, Miller M, Bier B, Donghi V, Pisaniello M, Mantovani R, Pinto G, Rota I, Baggio S, Chiarito M, Fazzari F, Cusmano I, Curzi M, Ro R, Malick W, Kamran M, Kohli-Seth R, Bassily-Marcus AM, Neibart E, Serrao G, Perk G, Mancini D, Reddy VY, Pinney SP, Dangas G, Blasi F, Sharma SK, Mehran R, Condorelli G, Stone GW, Fuster V, Lerakis S, Goldman ME. Characterization of Myocardial Injury in Patients With COVID-19. J Am Coll Cardiol. 2020;76:2043-2055. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 228] [Cited by in RCA: 289] [Article Influence: 57.8] [Reference Citation Analysis (0)] |
| 62. | Puntmann VO, Carerj ML, Wieters I, Fahim M, Arendt C, Hoffmann J, Shchendrygina A, Escher F, Vasa-Nicotera M, Zeiher AM, Vehreschild M, Nagel E. Outcomes of Cardiovascular Magnetic Resonance Imaging in Patients Recently Recovered From Coronavirus Disease 2019 (COVID-19). JAMA Cardiol. 2020;5:1265-1273. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1240] [Cited by in RCA: 1468] [Article Influence: 293.6] [Reference Citation Analysis (0)] |
| 63. | Wu Z, McGoogan JM. Characteristics of and Important Lessons From the Coronavirus Disease 2019 (COVID-19) Outbreak in China: Summary of a Report of 72 314 Cases From the Chinese Center for Disease Control and Prevention. JAMA. 2020;323:1239-1242. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11409] [Cited by in RCA: 11506] [Article Influence: 2301.2] [Reference Citation Analysis (0)] |
| 64. | Driggin E, Madhavan MV, Bikdeli B, Chuich T, Laracy J, Biondi-Zoccai G, Brown TS, Der Nigoghossian C, Zidar DA, Haythe J, Brodie D, Beckman JA, Kirtane AJ, Stone GW, Krumholz HM, Parikh SA. Cardiovascular Considerations for Patients, Health Care Workers, and Health Systems During the COVID-19 Pandemic. J Am Coll Cardiol. 2020;75:2352-2371. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1381] [Cited by in RCA: 1366] [Article Influence: 273.2] [Reference Citation Analysis (0)] |
| 65. | Bavishi C, Bonow RO, Trivedi V, Abbott JD, Messerli FH, Bhatt DL. Special Article - Acute myocardial injury in patients hospitalized with COVID-19 infection: A review. Prog Cardiovasc Dis. 2020;63:682-689. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 209] [Cited by in RCA: 207] [Article Influence: 41.4] [Reference Citation Analysis (0)] |
| 66. | Lippi G, Lavie CJ, Sanchis-Gomar F. Cardiac troponin I in patients with coronavirus disease 2019 (COVID-19): Evidence from a meta-analysis. Prog Cardiovasc Dis. 2020;63:390-391. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 406] [Cited by in RCA: 477] [Article Influence: 95.4] [Reference Citation Analysis (0)] |
| 67. | Inciardi RM, Lupi L, Zaccone G, Italia L, Raffo M, Tomasoni D, Cani DS, Cerini M, Farina D, Gavazzi E, Maroldi R, Adamo M, Ammirati E, Sinagra G, Lombardi CM, Metra M. Cardiac Involvement in a Patient With Coronavirus Disease 2019 (COVID-19). JAMA Cardiol. 2020;5:819-824. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1111] [Cited by in RCA: 1270] [Article Influence: 254.0] [Reference Citation Analysis (0)] |
| 68. | Ho JS, Sia CH, Chan MY, Lin W, Wong RC. Coronavirus-induced myocarditis: A meta-summary of cases. Heart Lung. 2020;49:681-685. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 69] [Cited by in RCA: 98] [Article Influence: 19.6] [Reference Citation Analysis (0)] |
| 69. | Blondiaux E, Parisot P, Redheuil A, Tzaroukian L, Levy Y, Sileo C, Schnuriger A, Lorrot M, Guedj R, Ducou le Pointe H. Cardiac MRI in Children with Multisystem Inflammatory Syndrome Associated with COVID-19. Radiology. 2020;297:E283-E288. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 129] [Cited by in RCA: 165] [Article Influence: 33.0] [Reference Citation Analysis (0)] |
| 70. | Clark DE, Parikh A, Dendy JM, Diamond AB, George-Durrett K, Fish FA, Fitch W, Hughes SG, Soslow JH. COVID-19 Myocardial Pathology Evaluated Through scrEening Cardiac Magnetic Resonance (COMPETE CMR). medRxiv. 2020;. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 11] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 71. | Huang L, Zhao P, Tang D, Zhu T, Han R, Zhan C, Liu W, Zeng H, Tao Q, Xia L. Cardiac Involvement in Patients Recovered From COVID-2019 Identified Using Magnetic Resonance Imaging. JACC Cardiovasc Imaging. 2020;13:2330-2339. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 389] [Cited by in RCA: 394] [Article Influence: 78.8] [Reference Citation Analysis (0)] |
| 72. | Levi M, Thachil J, Iba T, Levy JH. Coagulation abnormalities and thrombosis in patients with COVID-19. Lancet Haematol. 2020;7:e438-e440. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 878] [Cited by in RCA: 1062] [Article Influence: 212.4] [Reference Citation Analysis (0)] |
| 73. | Belen-Apak FB, Sarıalioğlu F. Pulmonary intravascular coagulation in COVID-19: possible pathogenesis and recommendations on anticoagulant/thrombolytic therapy. J Thromb Thrombolysis. 2020;50:278-280. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 59] [Cited by in RCA: 57] [Article Influence: 11.4] [Reference Citation Analysis (0)] |
| 74. | Avila J, Long B, Holladay D, Gottlieb M. Thrombotic complications of COVID-19. Am J Emerg Med. 2021;39:213-218. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 86] [Cited by in RCA: 92] [Article Influence: 23.0] [Reference Citation Analysis (0)] |
| 75. | Dhawan RT, Gopalan D, Howard L, Vicente A, Park M, Manalan K, Wallner I, Marsden P, Dave S, Branley H, Russell G, Dharmarajah N, Kon OM. Beyond the clot: perfusion imaging of the pulmonary vasculature after COVID-19. Lancet Respir Med. 2021;9:107-116. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 115] [Cited by in RCA: 115] [Article Influence: 28.8] [Reference Citation Analysis (0)] |
| 76. | Espallargas I, Rodríguez Sevilla JJ, Rodríguez Chiaradía DA, Salar A, Casamayor G, Villar-Garcia J, Rodó-Pin A, Marsico S, Carbullanca S, Ramal D, Del Carpio LA, Gayete Á, Maiques JM, Zuccarino F. CT imaging of pulmonary embolism in patients with COVID-19 pneumonia: a retrospective analysis. Eur Radiol. 2021;31:1915-1922. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 13] [Cited by in RCA: 19] [Article Influence: 3.8] [Reference Citation Analysis (0)] |