Published online Nov 5, 2021. doi: 10.5495/wjcid.v11.i3.38
Peer-review started: June 27, 2021
First decision: July 31, 2021
Revised: August 14, 2021
Accepted: October 15, 2021
Article in press: October 15, 2021
Published online: November 5, 2021
Processing time: 127 Days and 10.6 Hours
Human papillomavirus (HPV) is one of the most common sexually transmitted viruses nowadays.
To analyze the prevalence of HPV infection in human immunodeficiency virus (HIV)-positive patients and the risk factors associated with this infection through a review of studies published in the period from January 2010 to April 2020.
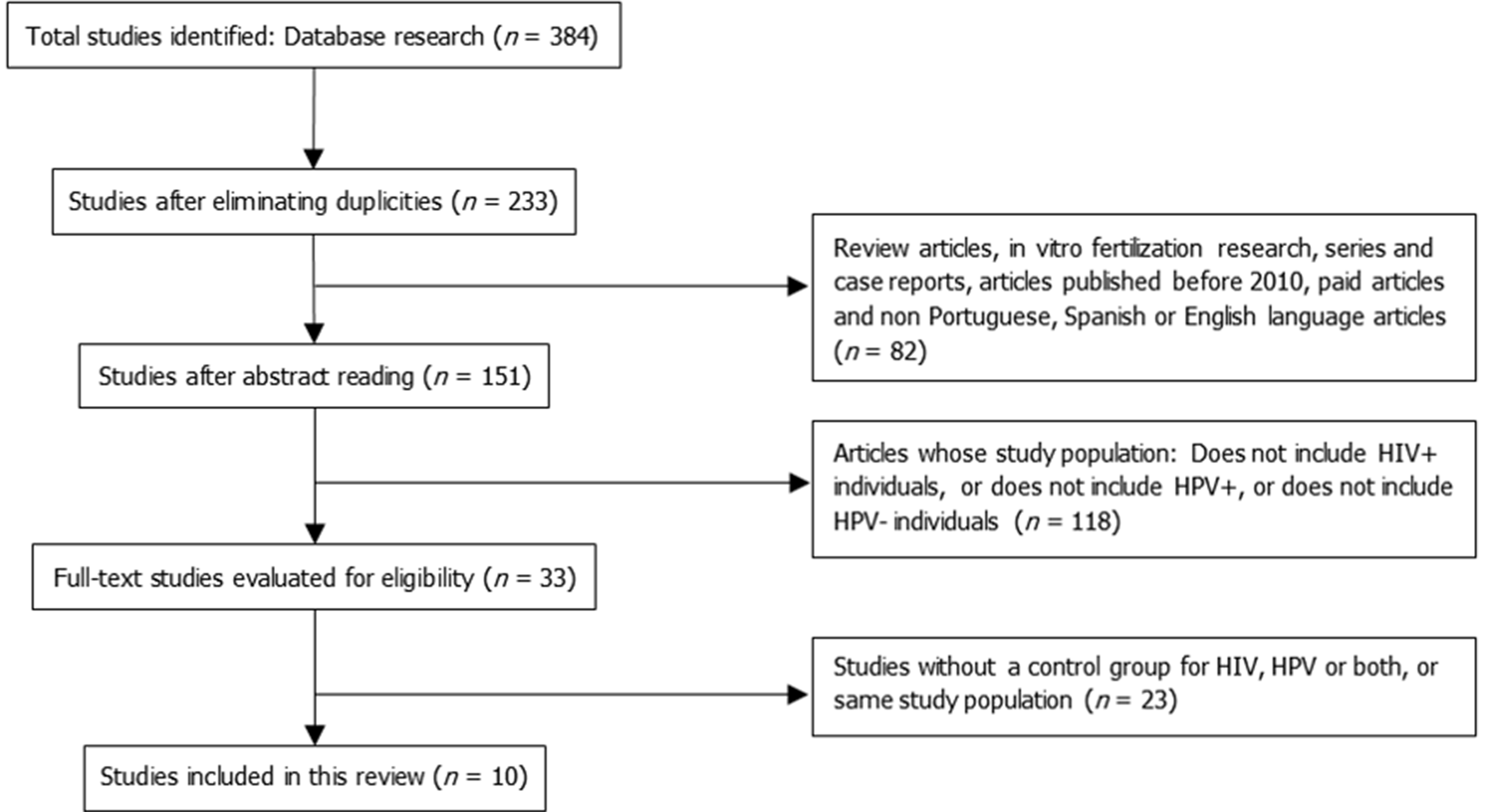
A total of 384 articles were initially identified in our searches, of which ten were selected according to previously defined eligibility criteria.
Anal intercourse, absence of condom use, multiple partners, other specific sexual and life habits, and HIV infection are among the risk factors associated with anal HPV infection.
In general, there is a higher prevalence of anal HPV infection among HIV-positive patients, mostly in individuals over 30 years old, those with multiple partners, those who had an early homosexual debut, and cigarette, alcohol, and drug users.
Core Tip: Human papillomavirus (HPV) is among the most common sexually transmitted viruses today. This systematic review aimed to analyze the prevalence of HPV infection in patients infected with human immunodeficiency virus (HIV) as well as the risk factors associated. Number of partners, absence of condom use, anal intercourse, multiple partners, sexual and life habits, and HIV infection are among the risk factors associated with anal HPV. There is a higher prevalence of anal HPV in patients infected with HIV, those with multiple partners, alcohol and drug users, and those with early age of first sexual intercourse with same-sex individuals.
- Citation: Santos CDPC, Brandão CC, Mota FS, Ferreira IS, Oliveira CNT, Souza CL, Freire de Melo F, Oliveira MV. Prevalence of anal human papillomavirus infection in patients with human immunodeficiency virus infection: A systematic review. World J Clin Infect Dis 2021; 11(3): 38-48
- URL: https://www.wjgnet.com/2220-3176/full/v11/i3/38.htm
- DOI: https://dx.doi.org/10.5495/wjcid.v11.i3.38
Sexually transmitted infections (STIs) are among the most prevalent diseases, and human immunodeficiency virus (HIV) infection affects millions of people worldwide. In 2019, 1.7 million people were infected by HIV, which illustrates the relevance of this infection[1,2]. Another common STI is caused by human papillomavirus (HPV), which has a close relationship with the emergence of cancer in the perianal region, especially in individuals with weakened immune system, such as those who are seropositive for HIV[3].
The HPV is a DNA virus that causes a variety of benign and malignant lesions on the skin and mucous membranes[4]. More than 150 HPV types have been described, among which the HPV 16 and 18 are the most frequent and pathogenic types as they infect the genital tract and are associated with a high risk of oncogenesis.
In immunocompetent individuals, HPV is usually eliminated within 18 mo after infection, without clinical manifestations, and can be transmitted during this period. In addition, unprotected sexual intercourses, having multiple of partners, early initiation of sexual activity, and lack of immunization greatly contribute to the viral dissemination[4].
The most frequent clinical presentation of HPV is the cutaneous wart, with an estimated incidence of 7%-10% in the European population and of 1% in the American population. In immunosuppressed patients, these numbers are 50- to 100-fold higher, reaching more than 90% after 15 years of transplantation[5].
Another important feature is the association between HPV infection and carcinomas, among which cervical carcinoma is widely studied. However, this relationship is also well established in the anal region, with similarities between the lesions and the characteristics of the epithelia observed in those anatomical sites. Furthermore, the progression of the malignant lesions has similitudes between both regions as well[6-8].
HIV-seropositive patients have a higher risk of contamination by HPV because both infections have similar predisposing factors related to sexual habits. In addition, the persistence of HPV infection and a greater variety of HPV serotypes are observed in the HIV seropositive population[9,10].
The coinfection with HIV and HPV favors HPV DNA mutations, making this virus more pathogenic, regardless of the HIV viral load. The infection associated with immunosuppression can cause lesions with a higher carcinogenic potential, which implies greater aggressiveness of cell lesions and a worse prognosis[11,12].
The progression of HPV infection is established as the immunological damage associated with HIV infection progression. Papillomavirus persistence is inversely related to CD4+ T lymphocyte count and directly proportional to HIV load. In immunosuppressed people, the HPV recurrence rate becomes high[13,14].
In the general population, HPV-associated squamous cell carcinoma in the anal region is rare. However, anal cancer is more prevalent in HIV seropositive populations, men who have sex with men, and women with a history of cancer in the genital region[6,8,15,16].
Several studies have been pointing out the relationship between HIV and HPV, indicating a higher risk of papillomavirus infection in individuals with immune suppression. In this sense, it is essential to compile results of studies evaluating the coinfection with these viruses and demonstrating associated risk factors that contribute to the occurrence of anal changes by HPV. The aim of this systematic review was to verify the prevalence of anal HPV in HIV-seropositive patients as well as to list risk factors associated with this event.
This is a systematic review conducted in accordance with the PRISMA recommenda
We selected articles on the prevalence and risk factors associated with HPV infection in anal and perianal sites in HIV-seropositive patients from January 2010 to April 2020 that were published in English, Portuguese, and Spanish.
Original research articles on clinical, experimental, and retrospective studies were included, and review articles, in vitro fertilization research, case series, and case reports were excluded. Articles that were not open access were not considered in this review.
The population chosen for this review was HIV- and HPV-seropositive patients, and all studies that only included individuals infected with HIV or HPV alone were excluded. We also excluded all articles that involved individuals under the age of 18.
The articles that comprise the present review deal with the investigation of risk factors associated with HIV-seropositive patients with HPV coinfection at perianal site.
The search for articles was conducted from March to April 2020, in the Scientific Electronic Library Online (SCIELO), United States National Library of Medicine (PubMed), and Virtual Health Library databases. In a strategy for searching data in all the bases, the following descriptors were used: HIV infections, papilloma virus infections, and anal canal.
Three authors independently carried out the selection of articles: Brandão CC, Ferreira IS, and Mota FS, co-authors of this paper. Then, duplicate articles were excluded and articles whose abstract did not address risk factors for HPV coinfection in anal/perianal sites in HIV seropositive patients were eliminated as well. Finally, the articles were fully read, including only those that addressed the topic of interest. The interpretative ambiguities and/or doubts were solved by consensus among the authors.
After reading the articles, the main data of each study were extracted, such as author(s), year of publication, factors associated with patients with viral coinfection, and prevalence data of the populations, described in Table 1.
| Ref. | Location | n | Study design | Predominant age | Predominant number of lifetime partners | Prevalence of anal HPV infection in HIV+ patients | Prevalence of anal HPV infection in HIV- patients |
| Li et al[17], 2016 | China | 889 | Transversal | ≤ 39 yr old: 79.53% | 6-30: 58.71% | 82.69% | 62.81% |
| Wirtz et al[18], 2015 | Moscow, Russia | 124 | Transversal | ≤ 35 yr old: 82.1% | α ≥ 5: 64.5% | 50% | 30.30% |
| Hu et al[21], 2013 | Beijing, China | 671 | Transversal | Median: 28 yr old | - | 82.10% | 57.50% |
| Lin et al[19], 2018 | Taiwan | 279 | Transversal | < 30 yr old: 71% | < 10: 81.0% | 85.30% | 73.30% |
| Welling et al[25], 2015 | Amsterdam | 778 | Prospective cohort | Median: 38 yr old | > 100: 64.42% | 69% | 45% |
| Wiley et al[24], 2013 | United States | 1262 | Multicenter cohort | ≤ 59 yr old: 71% | Average: 270 | 91% | 70% |
| Zhang et al[22], 2014 | Shenzhen, China | 408 | Transversal | 20-39 yr old: 88.9% | Median: 3 | 71.40% | 33.80% |
| Ren et al[26], 2017 | China | 164 | Transversal | ≤ 34 yr old: 91.4% | γ ≥ 1: 92.9% | 81% | 48.20% |
| Nowak et al[20], 2016 | Nigeria | 154 | Transversal | ≤ 29 yr old: 81.1% | ≤ 50: 75.32% | 91.10% | 40.60% |
| Somia et al[23], 2018 | Southeast Asia | 392 | Prospective cohort | ≥ 30 yr old: 58.2% | Median: 42.5 | 89.80% | 65.30% |
Among the studies that compose this review, the cross-sectional ones have a greater risk of bias due to confounding factors, especially the lack of control methods used as statistical modeling. In cohort studies, the greatest risk of bias is identified as loss to follow-up. However, it is important to indicate that these biases were not able to significantly change conclusions, which can be verified through the coincident findings in the studies, regardless of the method used and the sample involved.
After applying the uniterms, 384 articles were found (4 in SciELO, 159 in PubMed, and 221 in BVS). Following the elimination of duplicate articles and analysis taking into consideration the eligibility criteria, ten articles were selected to compose the present review. Figure 1 shows the steps of this selection process.
All articles were published in English from 2013 to 2018, evenly distributed over this period.
Concerning the geographical areas where the studies analyzed were performed, there was a prevalence of studies conducted in Asia (70%), most of which were conducted in China. None of the studies that comprise this review was carried out in the Brazilian population.
Most articles (70%) used the cross-sectional methodological approach. All studies were conducted with groups of men who have sex with men (MSM) aged 18 years or older. The instruments used by the researchers included self-administered questionnaires and/or interviews that covered sociodemographic information and sexual behavior, which were used as variables associated with anal HPV infection. Most articles also assessed the relationship between the infection and lifestyle habits.
As for the sociodemographic aspects, no standardization of analyses such as age range and education level was verified within the selected studies. In 40% of the studies, most participants were less than 29 years old. Regarding education, half of the analyzed articles revealed a higher prevalence of individuals with complete or ongoing higher education.
The isolated or concomitant use of alcohol, cigarettes, and illicit drugs was little explored in the articles.
Regarding the number of homosexual partners of the participants in the studies which make up this analysis, less than half indicated data about the number of lifetime partners and a minority stratified this data into shorter periods (3 mo, 6 mo, and 12 mo prior to the date of the study).
As for the age of first sexual intercourse with same-sex partners, half of the studies did not analyze this characteristic in their populations. Moreover, the other half evidenced divergent results, partly indicating age over 18 and partly indicating age under 18.
Overall, the studies were in agreement regarding the prevalence of anal HPV infection in HIV-seropositive patients, whereas the same levels of agreement were not found for anal HPV infection in HIV-seronegative patients (Table 1).
When analyzing the ten studies selected in this review, it was observed that none of them was conducted in Brazil. The methodological criteria listed for eligibility and the search mechanisms established here might have been responsible for this exclusion, especially concerning the non-inclusion of articles that were not open access.
Another important characteristic of this review was that most studies were cross-sectional. This methodological proposal is easier to execute, but it limits the evaluation of causality. The cause-and-effect relationship between the studied diseases is thus impaired, mainly because both diseases have similar epidemiological characteristics, and this kind of study does not offer a progressive perspective of the outcomes evaluated within the natural history of the disease.
In 40% of the studies[17-20], most patients were less than 29 years old. In the other studies, there was a wide variation in age classification, with two articles[21,22] reporting median ages of 28 and 29 years, respectively, and three articles[23-25] indicated a median age of greater than or equal to 30 years old.
Li et al[17], Wiley et al[24], and Ren et al[26] performed a more refined analytical approach in their studies, presenting more consistent results that indicate associations between age group and HPV infection. The research done by Wiley et al[24] demonstrated that patients aged between 40 and 69 years are more prone to infection by oncogenic high-risk HPV serotypes. The study by Ren et al[26], in its turn, showed that 78.6% of the MSM aged 35 years or older had anal HPV infection, a higher prevalence compared to all younger age groups. Li et al[17] showed that participants under the age of 29 had a 66.7% prevalence rate for HPV infection in the anal region.
The second point regarding socio-demographic criteria was education. The authors' reports diversified the approach to this assessment. The level of education of the population investigated by Li et al[17], Wirtz et al[18], Lin et al[19], Somia et al[23], and Ren et al[26] revealed a preponderance of individuals with completed or in training Higher Education. Conversely, Nowak et al[20] and Zhang et al[22] had the majority of individuals surveyed with lower educational levels.
The article by Lin et al[19] found a statistically significant association between high level of education and prevalence of anal HPV (P = 0.001). The studies by Li et al[17] and Somia et al[23] evaluated the educational level as a possible explanatory variable for the presence of high-risk oncogenic HPV but they found no statistically significant association. The other studies only described the participants' schooling. The lack of standardization of the studies regarding the stratification of variables and the number of patients included hindered further inferential discussions.
Variables such as marital status, ethnicity, and skin color were only little explored in the studies listed in this review, which unfortunately does not allow us to make further inferences about them as possible risk factors associated with the occurrence of anal changes associated with HPV infection in HIV-positive individuals.
In the articles that make up this systematic review, little was explored about the relationship between smoking and use of illicit drugs and the presence of anal HPV infection. Furthermore, all the studies that assessed smoking found a higher frequency of tobacco use among HIV-positive individuals. Welling et al[25] demonstrated, through multivariate analysis, a relationship between HIV and HPV serological statuses and smoking. They have found that 23.5% of the HIV-seronegative and HPV-positive patients smoke (P = 0.467), whereas in seropositive patients for both viruses the percentage is 41.8% (P = 0.075). It demonstrates that smoking is a habit related to HPV and HIV infections, a finding reinforced in the study by Wiley et al[24], which reported that smoking habit is directly related to a higher prevalence of positive tests for low- and high-risk HPV (P = 0.04).
Regarding illicit drug use, Lin et al[19] and Hu et al[21] identified that individuals who use illicit drugs had a higher odds of HIV infection, HPV infection, or co-infection with both viruses.
The number of partners was a factor evaluated with regard to sexual habits. Three studies investigated the number of partners that respondents had throughout their lives. The study by Lin et al[19] used the parameters of less than 10 partners and 10 or more partners throughout life, and no statistically significant association was found regarding HPV prevalence. Nowak et al[20], on the other hand, found a significant relationship between having a greater number of sexual partners and the prevalence of high-risk HPV. The study showed that having a lifetime number of more than 50 partners is associated with a greater risk of infection (P = 0.02). Additionally, Li et al[17] demonstrated that individuals who had an above-30 lifetime number of partners had a higher risk of HPV infection (P = 0.02) than those who had up to 30 partners throughout their lives. Welling et al[25] found a statistically significant relationship between HIV seronegative participants who have reported over-500 lifetime number of partners and low-risk HPV infection (P < 0.001), with no significant association identified among participants without HIV infection.
The study by Wiley et al[24] observed a higher prevalence of HPV infection among men who had more than 30 partners throughout their lives (P < 0.05). Hu et al[21], Zhang et al[22], and Somia et al[23] indicated in their studies that the number of sexual partners that respondents ever had is an important factor for HIV and HPV infection but it should be noted that these studies found no statistically significant associations regarding this variable. All the other articles that comprise this review did not assess the relationship of lifetime number of partners with HPV infection; they did so by considering shorter periods of 6, 12, and 24 mo prior to application.
Another variable that has been evaluated is the age of initiation of sexual life among homosexual individuals. Li et al[17], Wirtz et al[18], Nowak et al[20], Somia et al[23], and Ren et al[26] assessed in their studies the age of sexual intercourse debut, but this parameter was not significantly associated with a higher prevalence of HPV infection in any of these studies.
Another factor evaluated was the practice of receptive and insertive anal sex. In the study by Lin et al[19], 82.1% of the subjects practiced receptive anal sex. Moreover, they have also found a higher prevalence of receptive anal sex among HPV-positive individuals than among HPV-negative people (91.3% vs 75.6%, P = 0.01). The study by Hu et al[21] revealed that 83.7% of the HIV-seropositive patients practiced receptive and insertive anal sex; in contrast, these sexual practices were reported by 58.2% of the HIV-seronegative patients (P < 0.01), and no statistically significant relationship was found between this variable and the prevalence of HPV in this study. Another important data observed by Li et al[17] was that 65.51% of individuals who always use condoms during anal intercourse had HPV infection. Somia et al[23] reported that HIV-seropositive individuals are more likely to use condoms, corresponding to 69.2% of the studied sample (P = 0.02), and no statistical significance was found in the association between this parameter and HPV prevalence.
The most important risk factor identified for HPV infection after analyzing the articles was HIV seropositivity. In all articles, HIV-seropositive patients had a higher prevalence of HPV infection than HIV-negative individuals. The study by Hu et al[21] described that immunosuppression due to HIV infection increases not only the risk of HPV infection, but also the persistence of infection and reactivation of latent infection status. This study also found that people at higher risk of acquiring HIV infection are also at higher risk to be infected with HPV, since both infections are associated with high-risk sexual habits. The study by Ren et al[26] further demonstrated that HIV-seropositive MSM were 4.1 times more likely to be infected with any HPV serotype in the anal region compared to HIV seronegative MSM.
Two studies stood out for bringing very specific data on the topic. Lin et al[19] compared HIV-seropositive and HIV-seronegative individuals and found that HIV-positive individuals had infections with more than one HPV serotype. Likewise, Wiley et al[24] found that men who were not infected with HIV had a 1.8-fold higher odd of having infections with a single HPV serotype than HIV carriers.
In 20% of the articles analyzed, it was possible to observe that HIV-seropositive individuals had a higher risk for infection by high-risk HPV serotypes, especially serotypes 16 and 18. Wiley et al[24] found in their sample that 31% of the HIV patients were infected with HPV serotype 16 or 18, while, for HIV-negative patients, the percentage was 20%. The trial by Lin et al[19] attested that recent studies detected that HIV-seropositive men with HPV serotype 16 infection showed a higher affinity of the virus to the cells of the anal epithelium, which might be an excellent marker for predicting anal precancerous lesions. The results obtained by Wirtz et al[18] revealed that positivity for HPV 16 and 18 was associated with individual behaviors such as the number of male sexual partners, the greater number of stable partners with this same infection, and the use of lubricants incompatible with latex condom, which potentially facilitates exposure to HPV infection during anal intercourse.
All the studies listed here compared the prevalence of HPV infection in the anal region of HIV-seropositive and HIV-seronegative patients. The studies by Li et al[17], Wirtz et al[18], Hu et al[21], Somia et al[23], Wiley et al[24], and Welling et al[25] obtained similar results regarding the rates of HPV infection among HIV-positive and HIV-negative individuals, showing that this prevalence ranged from 18.6% to 24.6%, being higher for HIV seropositive people. In the same way, the studies by Nowak et al[20], Zhang et al[22], and Ren et al[26] also found a considerable difference between HIV-positive and HIV-negative individuals, but at higher levels, ranging from 32.8% to 37.6%. Only the study by Lin et al[19] found a smaller difference in anal HPV prevalence in HIV seropositive compared to seronegative individuals (12%). The studies showed statistical significance, except for the articles by Wirtz et al[18] and Welling et al[25], which did not indicate the significance test value for HPV infection.
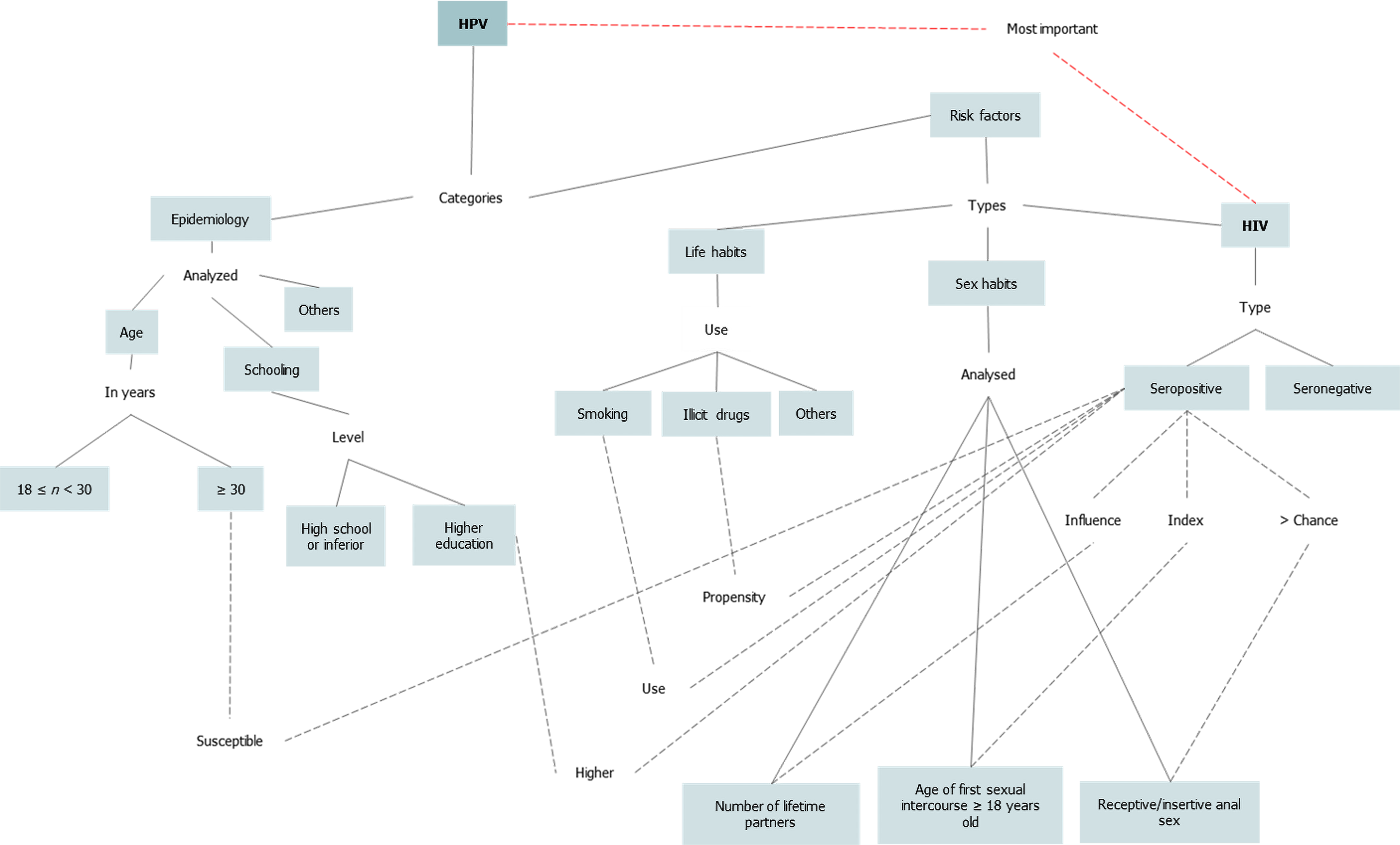
After the analysis of the articles included in this review, it was possible to establish a concept map that traces the relationship between the presence of HPV infection and the risk factors associated with this infection (Figure 2).
The concept map shown here establishes the relationship between HIV and HPV infections, assessing several other risk factors in individuals with coinfection that may increase the prevalence of anal changes. Overall, this review has shown that individuals aged 30 years or older and with higher levels of education have been found to be more susceptible to HIV. The use of cigarettes, illicit drugs, having more sexual partners throughout life, starting sexual intercourses with same-sex partners at an earlier age, and performing receptive anal sex were also related to a greater propensity to HIV infection (represented by blue lines in Figure 2). As can be observed, the number of lines that focus on the HIV risk factor makes us infer that HIV seropositive patients have a higher prevalence of HPV infection, which have been represented by the red line in the Figure 2.
This review sought to address the HPV prevalence among HIV seropositive patients. After applying all methodological criteria, only ten articles were selected, and all of them addressed risk factors linked to a higher prevalence of HPV infection in individuals infected with HIV. We initially expected a greater number of articles, which may indicate the need for further studies on this theme.
As expected, after a thorough reading of the selected articles, this study reinforced the understanding that the most important factor for the presence of anal HPV infection is HIV seropositivity. The studies used here always compared this relationship between HIV-positive and HIV-negative individuals, but other factors that further increase the risk of HPV infection were also assessed, such as age, smoking, alcohol intake and use of illicit drugs, multiple partners, early age for homosexual debut, and number of homosexual partners.
The importance of studying HPV lies in the fact that it is an agent legitimately associated with the occurrence of cancer, including anal cancer. It becomes even more important when there are individuals who are under a risk condition that greatly increases the chance of occurrence of this event, such as HIV-seropositive individuals. Thus, with regard to public health management, it is extremely important to recommend a close follow-up of these people, which can change the natural history of HPV disease. This review points out associated factors which in many cases can be modified, which has the potential to greatly contribute to reducing the incidence of high-grade lesions and anal cancer.
In addition, regarding overall patient management, it is possible to reduce the risk of infection by vaccination of groups that are more vulnerable to HPV-mediated high-grade lesions and cancer. The public health system in Brazil currently offers the quadrivalent vaccine for boys and girls aged 9 to 14 years, and this vaccination should be extended to groups of patients that are more susceptible to poorer HPV-related outcomes emphasized in this study.
The articles involved in this review lacked more refined statistical analysis and this decreased the possibility of making some inferences which were previously expected in the methodological planning process.
Sexually transmitted infections are among the most prevalent diseases worldwide, which is considered a public health issue. In immunocompetent individuals, human papillomavirus (HPV) is usually eliminated within 18 mo after infection. However, several studies have been pointing out the relationship between the infection by HIV and HPV, indicating a higher risk of papillomavirus infection in individuals with immune suppression. HPV has also a close relationship with the emergence of cancer in the perianal region, especially in individuals with weakened immune system, such as those who are seropositive for HIV.
In the above-mentioned context, it is essential to compile results of studies evaluating the coinfection with these viruses and demonstrating associated risk factors that contribute to the occurrence of anal changes by HPV. Since HPV is an agent legitimately associated with the occurrence of cancer, in public health management, it is extremely important to recommend a close follow-up of these people, which can change the natural history of HPV disease.
This study aimed to explore the prevalence of anal HPV infection in HIV-seropositive patients as well as to list risk factors associated with this event.
For this systematic review, PRISMA recommendation was followed. Articles on the prevalence and risk factors associated with HPV infection in anal and perianal sites in HIV-seropositive patients from January 2010 to April 2020 that were published in English, Portuguese, and Spanish were selected and analyzed.
Ten articles were selected, and all of them addressed risk factors linked to a higher prevalence of HPV infection in individuals infected with HIV. This study reinforced the understanding that the most important factor for the presence of anal HPV infection is HIV seropositivity.
The analysis of the articles points to a higher prevalence of anal HPV infection in patients infected with HIV, those with multiple partners, alcohol and drug users, and those with early age of first sexual intercourse with same-sex individuals. Number of partners, absence of condom use, anal intercourse, multiple partners, sexual and life habits and HIV are among the risk factors associated with anal HPV infection.
We initially expected a greater number of articles, which may indicate the need for further studies on this theme. This review points out associated factors which in many cases can be modified, which has the potential to greatly contribute to reducing the incidence of high-grade lesions and anal cancer.
Manuscript source: Unsolicited manuscript
Specialty type: Infectious diseases
Country/Territory of origin: Brazil
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): 0
Grade D (Fair): D, D
Grade E (Poor): 0
P-Reviewer: Han J S-Editor: Liu M L-Editor: Wang TQ P-Editor: Liu M
| 1. | Nadal SR, Nadal CRM. Infecções sexualmente transmissíveis em proctologia. 1th ed. Rio de Janeiro: Di Livros, 2019; 39-114. |
| 2. | UNAIDS. UNAIDS DATA 2020. [cited 5 January 2021] Available from: https://www.unaids.org/en/topic/data. |
| 3. | Capobiango A, Silva Filho AL da, Tarcizo Afonso N. Diagnóstico de HPV anal em mulheres com NIC: prevenção de câncer do ânus? Rev bras colo-proctol. 2009;29:443-450. [DOI] [Full Text] |
| 4. | BRASIL. Ministério da Saúde. Guia prático sobre HPV: perguntas e respostas. [cited 5 January 2021]. Available from: https://www.linguee.com/english-portuguese/translation/required+changes.html. |
| 5. | das Graças PLM, dos Santos Júnior GF, Porro AM, Tomimori J. Infecção pelo papilomavírus humano: etiopatogenia, biologia molecular e manifestações clínicas. Anais Brasileiros de Dermatologia. 2011;86:306-317. [RCA] [DOI] [Full Text] [Cited by in Crossref: 63] [Cited by in RCA: 73] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 6. | Júlio César M, Santos Jr. Câncer ano-reto-cólico - aspectos atuais: I - câncer anal. Rev bras. colo-proctol. 2007;27:219-223. [DOI] [Full Text] |
| 7. | Carvalho NS, Ferreira AM, Bueno CC. HPV infection and intraepithelial lesions from the anal region: how to diagnose? Braz J Infect Dis. 2011;15:473-477. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 6] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 8. | Duarte BF, Silva MAB da, Germano S, Leonart MSS. Diagnóstico do câncer anal na coinfecção pelo papiloma vírus humano (HPV) e pelo vírus da imunodeficiência humana (HIV). Rev Inst Adolfo Lutz. 2016;75:1-9. [DOI] [Full Text] |
| 9. | Entiauspe LG, Teixeira LO, Mendoza-Sassi RA, Gonçalves CV, Gonçalves P, de Martinez AMB. Papilomavírus humano: prevalência e genótipos encontrados em mulheres HIV positivas e negativas, em um centro de referência no extremo Sul do Brasil. Revista da Sociedade Brasileira de Medicina Tropical. 2010;43:260-263. [RCA] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 10] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 10. | Hidalgo-Tenorio C, de Jesus SE, Esquivias J, Pasquau J. Alta prevalencia e incidencia de lesiones precursoras de cáncer anal asociada a la infección por VPH en mujeres VIH positivas en la era tardía del TAR. Enferm Infecc Microbiol Clin. 2018;36:555-562. [RCA] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 10] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 11. | Vaz LP, Saddi VA, Amaral WN, Manoel WJ. Epidemiologia da infecção pelo HPV em mulheres infectadas pelo HIV. FEMINA. 2011;39:35-40. [DOI] [Full Text] |
| 12. | Bonilha JL, Yakabe MF, Camargo BF, Martins EKL, Ribeiro MCA, Costa-Neto JM, Galão EA, Mota MTO, Rahal P. Incidência de HPV em colo do útero de gestantes HIV positivas atendidas no Hospital de Base de São José do Rio Preto. SP. EINSTEIN. 2009;7:334-340. [RCA] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 13. | Cruz FJ, Melo VH. Fatores associados à persistência da infecção pelo HPV na cérvice uterina. FEMINA. 2010;38: 422-427. [DOI] [Full Text] |
| 14. | Fedrizzi EN, Schlup CG, Menezes ME, Ocampos M. Infecção pelo Papilomavírus humano (HPV) em mulheres de Florianópolis, Santa Catarina. DST j bras doenças sex transm. 2011;73-79. [RCA] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 15. | Nadal SR, Manzione CR. Papilomavirus humano e o câncer anal. Rev bras colo-proctol. 2006;26:204-207. [DOI] [Full Text] |
| 16. | Donà MG, Benevolo M, Latini A, Rollo F, Colafigli M, Frasca M, Zaccarelli M, Giglio A, Moretto D, Pescarmona E, Cristaudo A, Giuliani M. Anal cytological lesions and HPV infection in individuals at increased risk for anal cancer. Cancer Cytopathol. 2018;126:461-470. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 18] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 17. | Li X, Li M, Yang Y, Zhong X, Feng B, Xin H, Li Z, Jin Q, Gao L. Anal HPV/HIV co-infection among Men Who Have Sex with Men: a cross-sectional survey from three cities in China. Sci Rep. 2016;6:21368. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 32] [Cited by in RCA: 37] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 18. | Wirtz AL, Zelaya CE, Peryshkina A, McGowan I, Cranston RD, Latkin C, Galai N, Mogilniy V, Dzhigun P, Kostetskaya I, Beyrer C. Anal human papillomavirus and HIV: A cross-sectional study among men who have sex with men in Moscow, Russia, 2012-2013. Euro Surveill. 2015;20:21095. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 10] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 19. | Lin CC, Hsieh MC, Hung HC, Tsao SM, Chen SC, Yang HJ, Lee YT. Human papillomavirus prevalence and behavioral risk factors among HIV-infected and HIV-uninfected men who have sex with men in Taiwan. Medicine (Baltimore). 2018;97:e13201. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 14] [Cited by in RCA: 14] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 20. | Nowak RG, Gravitt PE, He X, Ketende S, Dauda W, Omuh H, Blattner WA, Charurat ME; TRUST Study Group. Prevalence of Anal High-Risk Human Papillomavirus Infections Among HIV-Positive and HIV-Negative Men Who Have Sex With Men in Nigeria. Sex Transm Dis. 2016;43:243-248. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 38] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 21. | Hu Y, Qian HZ, Sun J, Gao L, Yin L, Li X, Xiao D, Li D, Sun X, Ruan Y, Milam DF, Pan SW, Shao Y, Vermund SH. Anal human papillomavirus infection among HIV-infected and uninfected men who have sex with men in Beijing, China. J Acquir Immune Defic Syndr. 2013;64:103-114. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 54] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 22. | Zhang DY, Yin YP, Feng TJ, Hong FC, Jiang N, Wang BX, Chen XS. HPV infections among MSM in Shenzhen, China. PLoS One. 2014;9:e96364. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 20] [Cited by in RCA: 25] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 23. | Somia IKA, Teeratakulpisarn N, Jeo WS, Yee IA, Pankam T, Nonenoy S, Trachuntong D, Mingkwanrungrueng P, Sukmawati MDD, Ramautarsing R, Nilasari H, Hairunisa N, Azwa I, Yunihastuti E, Merati TP, Phanuphak P, Palefsky J, Phanuphak N; ANSAP Study Group. Prevalence of and risk factors for anal high-risk HPV among HIV-negative and HIV-positive MSM and transgender women in three countries at South-East Asia. Medicine (Baltimore). 2018;97:e9898. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 28] [Cited by in RCA: 23] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 24. | Wiley DJ, Li X, Hsu H, Seaberg EC, Cranston RD, Young S, D'Souza G, Martínez-Maza O, DeAzambuja K, Chua K, Hussain SK, Detels R. Factors affecting the prevalence of strongly and weakly carcinogenic and lower-risk human papillomaviruses in anal specimens in a cohort of men who have sex with men (MSM). PLoS One. 2013;8:e79492. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 27] [Cited by in RCA: 28] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 25. | Welling CA, Mooij SH, van der Sande MA, van Rooijen MS, Vermeulen-Oost WF, King AJ, van Eeden A, Heideman DA, Stolte IG, Schim van der Loeff MF. Association of HIV Infection With Anal and Penile Low-Risk Human Papillomavirus Infections Among Men Who Have Sex With Men in Amsterdam: The HIV & HPV in MSM Study. Sex Transm Dis. 2015;42:297-304. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 13] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 26. | Ren X, Ke W, Zheng H, Yang L, Huang S, Qin X, Yang B, Zou H. Human Papillomavirus Positivity in the Anal Canal in HIV-Infected and HIV-Uninfected Men Who Have Anal Sex with Men in Guangzhou, China: Implication for Anal Exams and Early Vaccination. Biomed Res Int. 2017;2017:2641259. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 12] [Article Influence: 1.5] [Reference Citation Analysis (0)] |