Published online Jun 5, 2020. doi: 10.5492/wjccm.v9.i2.31
Peer-review started: December 7, 2019
First decision: January 28, 2020
Revised: April 27, 2020
Accepted: May 12, 2020
Article in press: May 12, 2020
Published online: June 5, 2020
Processing time: 180 Days and 14.3 Hours
A diverse country like India may have variable intensive care units (ICUs) practices at state and city levels.
To gain insight into clinical services and processes of care in ICUs in India, this would help plan for potential educational and quality improvement interventions.
The Indian ICU needs assessment research group of diverse-skilled individuals was formed. A pan- India survey "Indian National ICU Needs" assessment (ININ 2018-I) was designed on google forms and deployed from July 23rd-August 25th, 2018. The survey was sent to select distribution lists of ICU providers from all 29 states and 7 union territories (UTs). In addition to emails and phone calls, social medial applications-WhatsApp™, Facebook™ and LinkedIn™ were used to remind and motivate providers. By completing and submitting the survey, providers gave their consent for research purposes. This study was deemed eligible for category-2 Institutional Review Board exempt status.
There were total 134 adult/adult-pediatrics ICU responses from 24 (83% out of 29) states, and two (28% out of 7) UTs in 61 cities. They had median (IQR) 16 (10-25) beds and most, were mixed medical-surgical, 111(83%), with 108(81%) being adult-only ICUs. Representative responders were young, median (IQR), 38 (32-44) years age and majority, n = 108 (81%) were males. The consultants were, n = 101 (75%). A total of 77 (57%) reported to have 24 h in-house intensivist. A total of 68 (51%) ICUs reported to have either 2:1 or 2≥:1 patient:nurse ratio. More than 80% of the ICUs were open, and mixed type. Protocols followed regularly by the ICUs included sepsis care, ventilator- associated pneumonia (83% each); nutrition (82%), deep vein thrombosis prophylaxis (87%), stress ulcer prophylaxis (88%) and glycemic control (92%). Digital infrastructure was found to be poor, with only 46 % of the ICUs reporting high-speed internet availability.
In this large, national, semi-structured, need-assessment survey, the need for improved manpower including; in-house intensivists, and decreasing patient-to-nurse ratios was evident. Sepsis was the most common diagnosis and quality and research initiatives to decrease sepsis mortality and ICU length of stay could be prioritized. Additionally, subsequent surveys can focus on digital infrastructure for standardized care and efficient resource utilization and enhancing compliance with existing protocols.
Core tip: Intensive care unit (ICU) practices are variable in a vast country like India. Most common admitting diagnosis for ICU is similar to Western reporting in literature. There is variable protocol penetration for processes of care in ICU.
- Citation: Kashyap R, Vashistha K, Saini C, Dutt T, Raman D, Bansal V, Singh H, Bhandari G, Ramakrishnan N, Seth H, Sharma D, Seshadri P, Daga MK, Gurjar M, Javeri Y, Surani S, Varon J, ININ-2018 Investigators Team. Critical care practice in India: Results of the intensive care unit need assessment survey (ININ2018). World J Crit Care Med 2020; 9(2): 31-42
- URL: https://www.wjgnet.com/2220-3141/full/v9/i2/31.htm
- DOI: https://dx.doi.org/10.5492/wjccm.v9.i2.31
Critical care practices vary worldwide and are a reflection of varying epidemiology and existing financial and human resources. Patient outcomes in these centers can vary dramatically due to the influence of interlinked, multiple factors[1].
A diverse country like India, may have variable intensive care units (ICUs) practices in various states, which can be due to differences in; hierarchical arrangements, allocation of resources, patient backgrounds, cultural and clinical practices, and goals or objectives of the caregivers[2]. Although it is imperative to have standardized care of practice to minimize variations and maximize the quality of care delivered to the patients, it is essential to paint a picture in the backdrop keeping in mind the epidemiological context, resource availability, and local practices[3]. In addition, it is crucial to identify and evaluate variables like prevalent clinical practices, protocols, a range of service, human resources and facilities available on a national level to bring forth a prototype which will help in quality control and unification of the care delivery. Studies have been done in developed countries[3,4], and a few more describe the practices in a multinational setting[5-7] but the information is scarce in an Indian setting[2].
Our study aimed to gain insight into clinical services, prevalent practices, processes of care and patient outcomes in ICUs across different regions of India. Studying and analyzing these patterns can potentially help prioritize quality improvement interventions, educate practicing physicians and, create a framework for further studies to fill in the knowledge gap, to further strategize best care practices and act as a paradigm for critical care delivery.
This was a cross-sectional pan-India survey-based study. We created a multidisciplinary, diverse team of qualified individuals who constituted the “Indian ICU needs assessment research group”.
A questionnaire was designed to assess the ICU clinical practices prevalent in the institution followed by the study of the demographics of the institution and the surveyor. Questions were asked regarding the ICU being closed or open, group and type of patients catered to, number of ICU beds, protocols followed in the ICU setting, top diagnoses of the admitted patients, and availability of critical care equipment and technology. Moreover, human resource demographics were explored through variables such as the presence of certified intensivists, residents/fellows, 24-h in-house staff intensivists, patient: Nurse ratio, age of the surveyor, gender, level of training, and years of experience. Outcome variables included average ICU length of stay, mechanical ventilation duration, ICU mortality, sepsis mortality and, mechanical ventilation patient mortality. The functionality of the survey was tested as a pilot among a random group of critical care physicians prior to implementation for internal validity. A sample of the survey is depicted in the E-supplement.
A database of intensivists was identified through critical care societies, social media, and personal networks. The team carried out the study through a survey from July 23rd to August 25th, 2018, through an anonymous questionnaire designed on a Google™ form online and distributed to the critical care providers in 29 states and 7 Union territories (UTs) of India (Figure 1). Various platforms like electronic mail (e-mail), social media applications such as WhatsApp™, Facebook™ and LinkedIn™, were used for dispatching the form and to reach out to potential collaborators for reminder and motivation.
A convenient sample of 134 ICUs was collected through the survey, and the data collected is presented as mean, with standard deviation, or median with interquartile range. Pictorial and graphical representation of the relevant data was done.
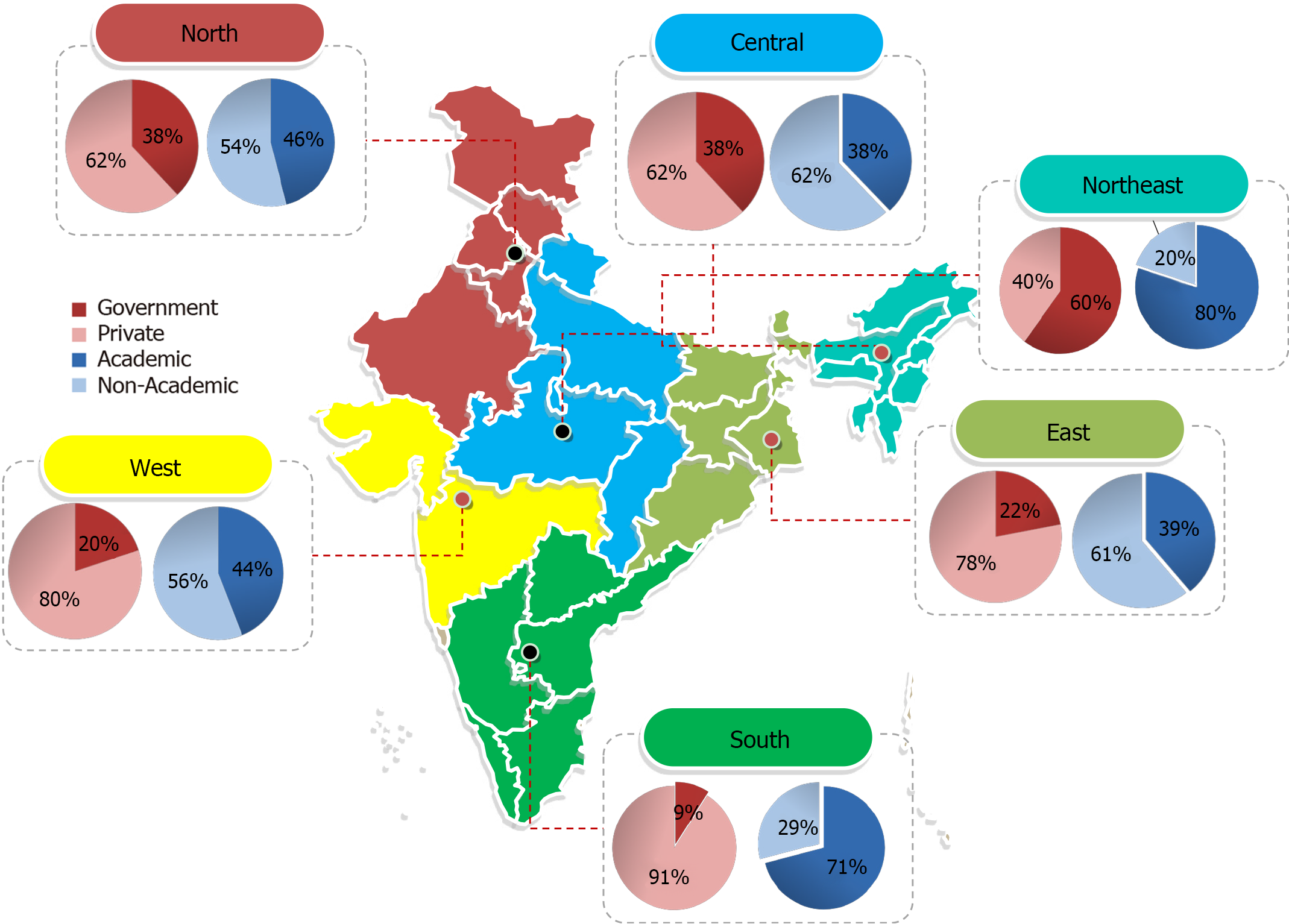
For analysis purposes, we divided India into 6 zones (Figure 2), on the basis of administrative divisions mainly – North, South, West, East, Central, Northeast[8]. Descriptive statistical analysis was used.
By completing and submitting the survey, providers gave their consent to provide pertinent information for research purposes. This study was deemed eligible for category-2 Institutional Review Board exempt status.
Our analysis was based on total 134 adult/adult-pediatrics ICU responses. They represented 61 cities of 24 states, and two UTs of India. The response rate was 83% states and 28% of UTs. Region-wise sample distribution revealed that 39 (29%) of entries belonged to the Northern region, whereas South Indian cities contributed to 34 (25%) entries. Thirteen (10%) from the Central; 25 (19%) from West; while 18 (13%) entries belonged to East and North-East, contributed 5 (4%) of the total of 134 entries.
A vast majority of responders in the survey were young adults, median (IQR), 38 (32-44) years age and predominantly, n = 108 (80%) were males, with a median clinical ICU experience of 8.5 (IQR, 4-14) years. Likewise, most of the responses came from consultants, n = 101 (75%), followed by residents (PGY-3 and above), n = 19 (14%). Most of them were working in mixed medico-surgical ICUs, n = 111(83%) in private academic hospitals, n = 50 (37%) with median (IQR) 16 (10-25) beds. Most of the responders were working in open type of ICU setup, 110 (82%), and only 24 (18%) of them in closed ICUs (Table 1 and Figure 3).
| Demographic variables | Responses in % (n = 134) |
| Age ( yr) | |
| 30-40 | 41 |
| 40-50 | 30.6 |
| 20-30 | 17.2 |
| > 50 | 11.2 |
| Gender | |
| Male | 80.2 |
| Female | 19.4 |
| ICU experience (yr) | |
| < 10 | 61.9 |
| 11-20 | 28.4 |
| 20-30 | 8.2 |
| > 30 | 1.5 |
| Designation | |
| Consultant staff | 75.4 |
| Resident- PGY-3 and above | 14.1 |
| Resident- PGY-1 | 6.7 |
| Resident- PGY-2 | 3.7 |
| Intensive care unit specialty wise distribution | |
| Mixed medical-surgical | 82.8 |
| Medical | 8.2 |
| Others | 6.7 |
| Surgical | 2.2 |
| Institution type | |
| Private/academic | 37.3 |
| Private/non-academic | 36.5 |
| Government/academic | 14.2 |
| Government/non-academic | 11.9 |
| Bed strength | |
| 11-20 | 36.6 |
| < 10 | 26.9 |
| 21-30 | 22.4 |
| > 30 | 14.2 |
| ICU type | |
| Open | 82.1 |
| Closed | 17.9 |
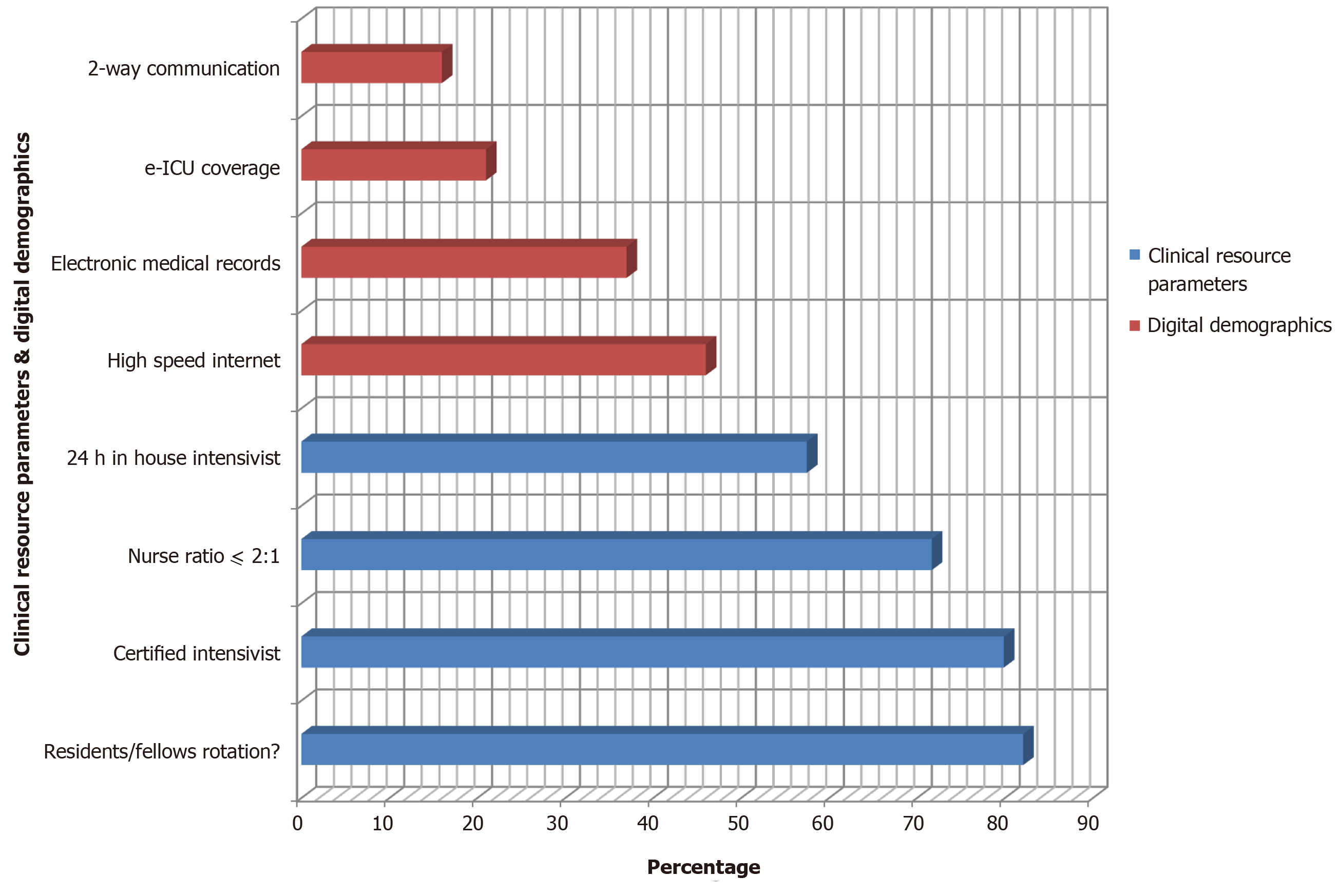
Intensivist and the nurses played a major role in ICU patient care. Most responders (62%), had patient: nurse ratio of 2:1, and only (10%) responders were strictly abiding by 1:1 nursing care. Additionally, 37% of ICUs, which usually had 2:1 patient: nurse ratios, switched to 1:1 for complicated cases. Also, more than 2:1 patient: nurse’s ratios were reported in 24% of ICUs. A total of 107 (80%) reported to have ICU staffed by certified intensivists and 77 (58%), had 24 h in-house intensivist coverage to take care of the patients. The majority of ICUs (n = 110, 82%) ICUs had residents/fellows/ medical students rotating through or cover ICU along with staff intensivists (Table 2 and Figure 4).
| Clinical resource parameters | Responses in % (n = 134) |
| Patient:nurse ratio | |
| Usually 2:1 (for complicated patients 1:1) (n = 49) | 36.6 |
| 2:1 (n = 34) | 25.4 |
| > 2:1 (n = 32) | 23.9 |
| 1:1 (n = 13) | 9.7 |
| No fixed patient:nurse (n = 6) | 4.5 |
| 24 h in-house intensivist (n = 77) | 57.5 |
| Certified intensivist (n = 107) | 79.9 |
| Residents/fellows/medical students rotate through or cover ICU along with staff intensivists (n = 110) | 82.1 |
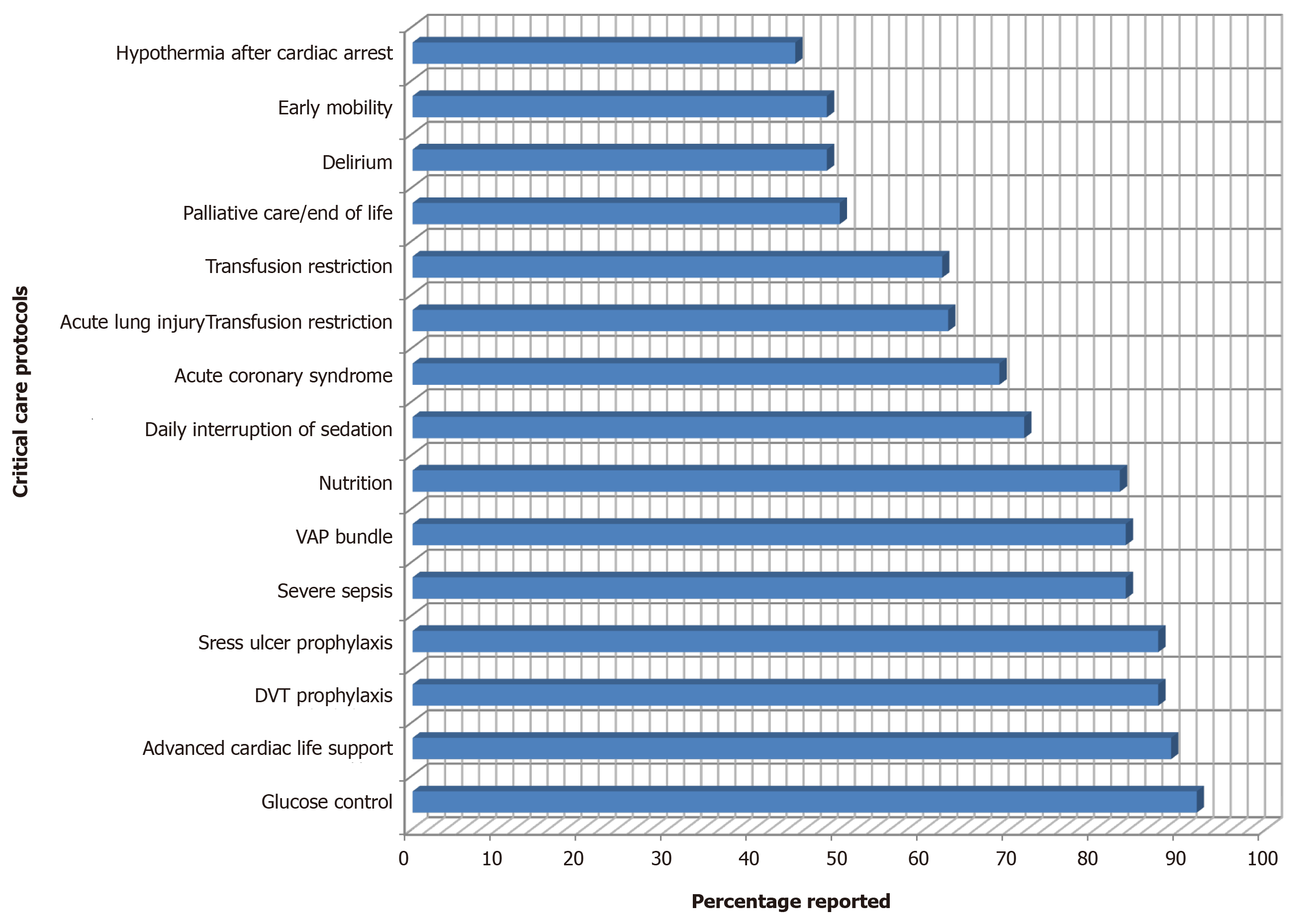
The majority of ICUs had glycemic control (92%) protocols, Advanced Cardiac Life Support (89%), deep vein thrombosis prophylaxis (87%), stress ulcer prophylaxis (87%), sepsis care (84%), ventilator-associated pneumonia (84%) and nutrition (83%) protocols. The least reported protocols included palliative care/end-of-life care (50%), delirium assessment and treatment (49%), early mobility (49%) and targeted temperature management after cardiac arrest (45%) (Table 3 and Figure 5).
| Critical care protocols self-reporting | |||||
| High (%) | Medium (%) | Low (%) | |||
| Glucose control | 91.8 | Daily interruption of sedation | 71.6 | Palliative care/end of life | 50.0 |
| Advanced cardiac life support | 88.8 | Acute coronary syndrome | 68.7 | Delirium | 48.5 |
| DVT prophylaxis | 87.3 | Acute lung injury | 62.7 | Early mobility | 48.5 |
| Stress ulcer prophylaxis | 87.3 | Transfusion restriction | 62 | Hypothermia after cardiac arrest | 44.8 |
| Severe sepsis | 83.5 | ||||
| VAP bundle | 83.5 | ||||
| Nutrition | 82.8 | ||||
In spite, of 60 (46%) hi-speed internet availability the digital infrastructure was reported to be limited. Electronic medical records, n = 49 (37%), tele-ICU coverage, n = 28 (21%) and 2-way communication including webcam, n = 21 (16%) were reported (Table 4).
| Digital demographics | Responses in % (n = 134) |
| High speed internet | 46 |
| Electronic medical records | 37 |
| Tele-ICU Coverage | 21 |
| 2 – way communication (e.g., webcam) | 16 |
The self-reported top admitting diagnosis in our survey study was sepsis, closely followed by respiratory failure (Table 5).
| Common diagnoses (Dx) | No. | % of ICU |
| Most common Dx - septic shock | 116 | 86.57 |
| Respiratory failure | 108 | 80.6 |
| Heart failure | 58 | 43.28 |
| Trauma | 57 | 42.54 |
| Post Op | 59 | 44.03 |
| COPD exacerbation | 72 | 53.73 |
| Electrolyte imbalance | 39 | 29.1 |
| Epilepsy or seizure | 21 | 15.67 |
| Renal failure | 72 | 53.73 |
| Hypotension | 37 | 27.61 |
| Poisoning/substance abuse | 34 | 25.37 |
The self-reported average ICU mortality (n = 95) was median 18% (IQR 11-30); ICU length of stay (n = 112) was 3.5 (4-6) d; mechanical ventilation (MV) duration (n = 98) was median 4 (3-5) d; MV patient mortality (n = 77) was 25% (15%-40%) and sepsis mortality (n = 75) was 30% (20%-40%).
Our survey describes some of the critical care practices in a convenient sample of 134 Indian ICUs, and for a better visualization we aimed to cover the whole country, and data was collected from majority of states and some union territories. We found substantial variation in the representation, with minimal participation being observed from North-East region. The majority of the responders of the survey were young adult men, practicing as intensivists, supporting the notion that the country has been training more individuals in critical care, and expanding its health infrastructure.
The Indian subcontinent has variations abound, and each geographical region in the country blending with its own cultural and regional diversity constructs a polychromatic picture. It is only natural for the country to have diversified patient care practices. While being appreciative of the uniqueness this land offers, it is imperative to be vigilant for any disparities which may compromise the delivery of quality and standardized patient care.
Most of the ICUs we surveyed were mixed (medical-surgical) in nature, open in type with an average number of beds of less than 20 per hospital. More than half of them were privately owned, academic-nonacademic institutions. Likewise, elaborating clinical resource parameters, such as a ≤ 2:1 patient-nurse ratio[9], 24-h certified intensivists, and certified intensivists, are associated with better outcomes in intensive care. The majority of Indian ICUs reported having 1 nurse for two or more patients with only few reporting 1:1 patient-nurse ratio. The new finding is that the majority of the ICUs reported having a certified intensivist, and more than half of them had 24 h-in house intensivist coverage.
In a survey-based study done in India covering 400 ICUs, similar results were reported with average age of responders being 30-40 years, number of ICU beds 10-30, and the majority of the ICUs were open type and mixed in nature[2].
The top admitting diagnosis in our study was sepsis, which was reported across an over whelming majority of all the ICUs closely followed by respiratory failure. This follows global trends. For example, an observational study, collecting data from 10096 patients across different countries, observed the most common diagnosis on admission to be sepsis[10].
Recent reports suggest that standardized protocols and best practice guidelines in the treatment of the critically ill patients in the ICU are associated with more favorable outcomes and decreased ICU-related morbidity and mortality. In our survey, self-reported data suggested that the majority of the ICUs across India followed the glycemic control, Advanced Cardiac Life support, deep vein thrombosis prophylaxis, stress ulcer prophylaxis, severe sepsis, ventilator Associated pneumonia bundle, and nutrition protocols. Some of the protocols that still require widespread penetration and awareness in India included palliative care/end-of-life, delirium, early mobility and targeted temperature management after cardiac arrest.
With the advent of digital revolution in India, we also explored the depth of digital coverage in the ICU. Not aligning with the rapid growth observed in other sectors, less than half of the ICUs reported having high-speed internet with even lesser having electronic medical records, tele-ICU coverage and 2-way communication. A survey of ICUs in medium to low income countries documented an average number of beds being around 10 per ICU, almost 70% of the ICUs were staffed with certified intensivists and 69% of the hospitals had a reliable internet access[7]. In a systematic review done 18 years ago in an attempt to identify physician staffing patterns and clinical outcomes in critically ill patients, the ICU mortality rates ranged from 6%-74% in low intensity staffing and 1%-57% in high intensity staffing ICUs[11]. Outcome data in our study was well within the observed range, reflecting that the majority of the ICUs across the country are adhering to the accepted standard of care, although the self-reported outcomes decrease the validity of these results.
In a descriptive study in the United States of ICUs, the average ICU size was 11.7 ± 7.8 beds per unit, and majority of these hospitals had more than one ICU, followed standard of care protocols, had better patient care delivery, as well as better outcomes, as compared to studies done in low and middle income countries[2,12,13].
Our study has several limitations. First, we had no follow up of initial non-responders. We had a limited sample size, and we used a survey that had not been previously validated in the literature. Other limitations included the documentation of self-reported outcomes reporting, which is similar to previously reported survey-based study from one state in India[14,15]. Also, our study had a limited ability from the surveyor’s side to ensure correct data entry and eliminate bias. For example, the overall penetration of tele-ICUs systems and EMRs in India is extremely low; but the reported fraction of tele-ICU penetration in our study may be higher due to selection bias. However, the strength of this survey is that the ICU data was retrieved from diverse geographical regions, which increase the external validity of the study. In addition, we were appreciated at Society of Critical Care Medicine 2019 conference abstract presentation[16] about the fact that the functionality of the survey was tested as a pilot among a random group of critical care physicians prior to implementation, which adds to the internal validity.
Understanding the epidemiology of the Indian subcontinent is incredibly complex, due to inherent variability and lack of required infrastructure to carry out such large-scale studies. At best, these trends can be used as building blocks to identify the gaps in the understructure, and identify areas to focus on, for improved financial and human resource investments.
In a large nation, semi-structured need assessment survey, the need for improved manpower including; in-house intensivists and decreasing patient-to-nurse ratios are evident. Quality and research initiatives to decrease sepsis mortality and ICU length of stay can be prioritized. Our new theory would be that subsequent surveys can focus on digital infrastructure for standardized care and scarce resources utilization and enhancing the compliance of existing protocols.
With the modernization of medicine and technology, the population is living longer. The patients presenting in hospital have several co-morbid factors and are critically ill on many instances. The developed countries have come with several protocol and best practices, based on the scientific facts and expert guideline. This has shown to save lives and improve the outcomes. When it comes to developing countries, though progress has been made but not much data or information is available.
There is not much data out there regarding standard of practice, variations in practice, clinical services available in the different region of intensive care unit (ICU). We believe that having that knowledge will help in decreasing the variation and improve henceforth help in improving the patient care.
Study was designed to understand the processes, adherence to the guidelines and clinical services available in ICU in different part of India.
This study was cross-sectional pan-India based survey.
Responses were received from 134 adult/pediatric ICU were received. More than 80% of their ICU was either open or transitional. Digital infra-structure and technology was found to be marginal. More than 80% of them were utilizing sepsis care, ventilator-associated pneumonia bundle, deep venous thrombosis prophylaxis, stress ulcer prophylaxis and glycemic control. They have lower nurse to patient ratio. They also have fewer critical care specialist.
There is definitely need for improvement in the digital infra-structure, nurse to patient ratio, critical care physician availability.
Improving the practice gaps can help in improving the patient care, decreasing the hospital and ICU length of stay, decrease in mortality, and improvement in patient outcome.
Manuscript source: Unsolicited manuscript
Specialty type: Critical care medicine
Country/Territory of origin: United States
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Kumar N, Weiss M S-Editor: Ma YJ L-Editor: A E-Editor: Wu YXJ
| 1. | Sakr Y, Moreira CL, Rhodes A, Ferguson ND, Kleinpell R, Pickkers P, Kuiper MA, Lipman J, Vincent JL; Extended Prevalence of Infection in Intensive Care Study Investigators. The impact of hospital and ICU organizational factors on outcome in critically ill patients: results from the Extended Prevalence of Infection in Intensive Care study. Crit Care Med. 2015;43:519-526. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 126] [Cited by in RCA: 148] [Article Influence: 14.8] [Reference Citation Analysis (0)] |
| 2. | Kartik M, Gopal PBN, Amte R. Quality Indicators Compliance Survey in Indian Intensive Care Units. Indian J Crit Care Med. 2017;21:187-191. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 6] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 3. | Checkley W, Martin GS, Brown SM, Chang SY, Dabbagh O, Fremont RD, Girard TD, Rice TW, Howell MD, Johnson SB, O'Brien J, Park PK, Pastores SM, Patil NT, Pietropaoli AP, Putman M, Rotello L, Siner J, Sajid S, Murphy DJ, Sevransky JE; United States Critical Illness and Injury Trials Group Critical Illness Outcomes Study Investigators. Structure, process, and annual ICU mortality across 69 centers: United States Critical Illness and Injury Trials Group Critical Illness Outcomes Study. Crit Care Med. 2014;42:344-356. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 107] [Cited by in RCA: 119] [Article Influence: 10.8] [Reference Citation Analysis (0)] |
| 4. | Fowler RA, Abdelmalik P, Wood G, Foster D, Gibney N, Bandrauk N, Turgeon AF, Lamontagne F, Kumar A, Zarychanski R, Green R, Bagshaw SM, Stelfox HT, Foster R, Dodek P, Shaw S, Granton J, Lawless B, Hill A, Rose L, Adhikari NK, Scales DC, Cook DJ, Marshall JC, Martin C, Jouvet P; Canadian Critical Care Trials Group; Canadian ICU Capacity Group. Critical care capacity in Canada: results of a national cross-sectional study. Crit Care. 2015;19:133. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 40] [Cited by in RCA: 53] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 5. | Chittawatanarat K, Sataworn D, Thongchai C; Thai Society of Critical Care Medicine Study Group. Effects of ICU characters, human resources and workload to outcome indicators in Thai ICUs: the results of ICU-RESOURCE I study. J Med Assoc Thai. 2014;97 Suppl 1:S22-S30. [PubMed] |
| 6. | Murthy S, Leligdowicz A, Adhikari NK. Intensive care unit capacity in low-income countries: a systematic review. PLoS One. 2015;10:e0116949. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 176] [Cited by in RCA: 227] [Article Influence: 22.7] [Reference Citation Analysis (0)] |
| 7. | Vukoja M, Riviello E, Gavrilovic S, Adhikari NK, Kashyap R, Bhagwanjee S, Gajic O, Kilickaya O; CERTAIN Investigators. A survey on critical care resources and practices in low- and middle-income countries. Glob Heart. 2014;9:337-42.e1-5. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 68] [Article Influence: 6.2] [Reference Citation Analysis (0)] |
| 8. | Administrative divisions of India. Available from: https://en.wikipedia.org/wiki/Administrative_divisions_of_India. |
| 9. | Amaravadi RK, Dimick JB, Pronovost PJ, Lipsett PA. ICU nurse-to-patient ratio is associated with complications and resource use after esophagectomy. Intensive Care Med. 2000;26:1857-1862. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 184] [Cited by in RCA: 177] [Article Influence: 7.1] [Reference Citation Analysis (0)] |
| 10. | Vincent JL, Marshall JC, Namendys-Silva SA, François B, Martin-Loeches I, Lipman J, Reinhart K, Antonelli M, Pickkers P, Njimi H, Jimenez E, Sakr Y; ICON investigators. Assessment of the worldwide burden of critical illness: the intensive care over nations (ICON) audit. Lancet Respir Med. 2014;2:380-386. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 606] [Cited by in RCA: 838] [Article Influence: 76.2] [Reference Citation Analysis (0)] |
| 11. | Pronovost PJ, Angus DC, Dorman T, Robinson KA, Dremsizov TT, Young TL. Physician staffing patterns and clinical outcomes in critically ill patients: a systematic review. JAMA. 2002;288:2151-2162. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1104] [Cited by in RCA: 1070] [Article Influence: 46.5] [Reference Citation Analysis (0)] |
| 12. | Groeger JS, Guntupalli KK, Strosberg M, Halpern N, Raphaely RC, Cerra F, Kaye W. Descriptive analysis of critical care units in the United States: patient characteristics and intensive care unit utilization. Crit Care Med. 1993;21:279-291. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 199] [Cited by in RCA: 184] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 13. | Haniffa R, Isaam I, De Silva AP, Dondorp AM, De Keizer NF. Performance of critical care prognostic scoring systems in low and middle-income countries: a systematic review. Crit Care. 2018;22:18. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 31] [Cited by in RCA: 56] [Article Influence: 8.0] [Reference Citation Analysis (0)] |
| 14. | National Center for Chronic Disease Prevention and Health Promotion (US) Office on Smoking and Health. Preventing Tobacco Use Among Youth and Young Adults: A report of the Surgeon General. Atlanta (GA): Centers for Disease Control and Prevention (US); 2012: 16-19. [PubMed] |
| 15. | Saigal S, Sharma JP, Pakhare A, Bhaskar S, Dhanuka S, Kumar S, Sabde Y, Bhattacharya P, Joshi R. Mapping the Characteristics of Critical Care Facilities: Assessment, Distribution, and Level of Critical Care Facilities from Central India. Indian J Crit Care Med. 2017;21:625-633. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 16. | Kashyap R, Saini C, Vashistha K, Dutt T, Raman D, Bansal V, Seth H, Sharma D, Seshadri P, Singh H, Bhandari G, Ramakrishnan N, Daga M, Gurjar M, Javeri Y. 109: Indian ICU needs assessment survey-1: ININ 2018-I. Crit Care Explor. 2019;47:37. [RCA] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 17. | Distribution of participating intensive care unit’s over India’s map. Google Maps.. [accessed December 2019]. Available from: https://www.google.com/maps/d/u/0/edit?mid=1cIgXJUaGSb9afpdR0fv0ee5DWi7EDkkLll=21.715383982952808%2C66.28292755143718z=5. |