Published online Feb 21, 2019. doi: 10.5492/wjccm.v8.i2.9
Peer-review started: December 13, 2018
First decision: January 5, 2019
Revised: January 24, 2019
Accepted: January 29, 2019
Article in press: January 30, 2019
Published online: February 21, 2019
Processing time: 70 Days and 9.4 Hours
In-hospital cardiac arrest (IHCA) portends a poor prognosis and survival to discharge rate. Prognostic markers such as interleukin-6, S-100 protein and high sensitivity C reactive protein have been studied as predictors of adverse outcomes after return of spontaneous circulation (ROSC); however; these variables are not routine laboratory tests and incur additional cost making them difficult to incorporate and less attractive in assessing patient’s prognosis. The neutrophil-lymphocyte ratio (NLR) is a marker of adverse prognosis for many cardiovascular conditions and certain types of cancers and sepsis. We hypothesize that an elevated NLR is associated with poor outcomes including mortality at discharge in patients with IHCA.
To determine the prognostic significance of NLR in patients suffering IHCA who achieve ROSC.
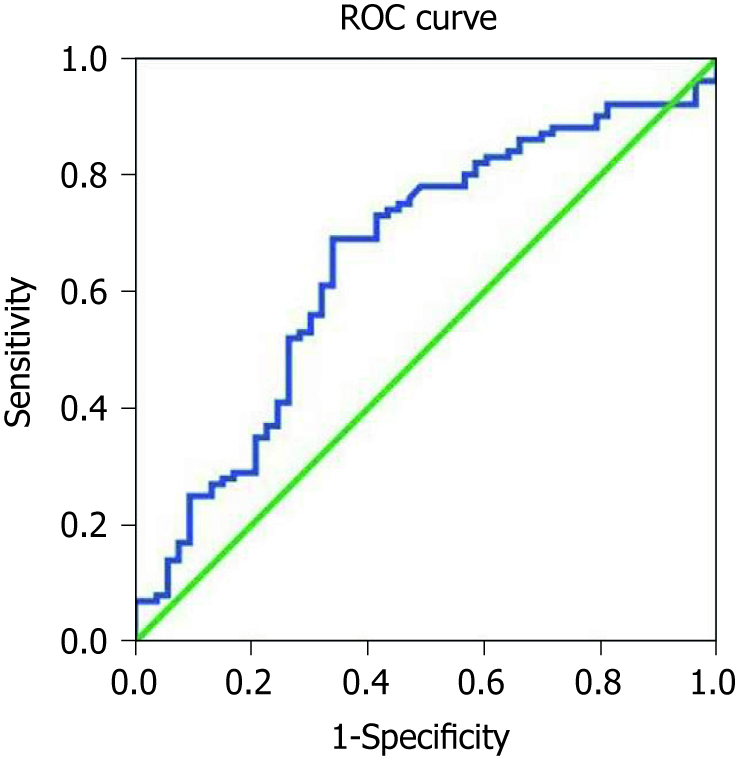
A retrospective study was performed on all patients who had IHCA with the advanced cardiac life support protocol administered in a large urban community United States hospital over a one-year period. Patients were divided into two groups based on their NLR value (NLR < 4.5 or NLR ≥ 4.5). This cutpoint was derived from receiving operator characteristic curve analysis (area under the curve = 0.66) and provided 73% positive predictive value, 82% sensitivity and 42% specificity for predicting in-hospital death after IHCA. The primary outcome was death or discharge at 30 d, whichever came first.
We reviewed 153 patients with a mean age of 66.1 ± 16.3 years; 48% were female. In-hospital mortality occurred in 65%. The median NLR in survivors was 4.9 (range 0.6-46.5) compared with 8.9 (0.28-96) in non-survivors (P = 0.001). A multivariable logistic regression model demonstrated that an NLR above 4.55 [odds ratio (OR) = 5.20, confidence interval (CI): 1.5-18.3, P = 0.01], older age (OR = 1.03, CI: 1.00-1.07, P = 0.05), and elevated serum lactate level (OR = 1.20, CI: 1.03-1.40, P = 0.02) were independent predictors of death.
An NLR ≥ 4.5 may be a useful marker of increased risk of death in patients with IHCA.
Core tip: Patients who have an in-hospital cardiac arrest (IHCA) event often have poor prognosis and their survival to discharge rates are dismal. Despite advancements in resuscitation, including the use of target temperature management, the prognosis for these patients has not improved over the past 30 years. Markers that are inexpensive and easy to use that may provide some prognostic information after an IHCA event are needed. A neutrophil-lymphocyte ratio greater than 4.5 may be a useful prognostic tool and marker for increased risk of death in patients with IHCA. In addition, older age, elevated serum lactate level were also independent predictors of death.
- Citation: Patel VH, Vendittelli P, Garg R, Szpunar S, LaLonde T, Lee J, Rosman H, Mehta RH, Othman H. Neutrophil-lymphocyte ratio: A prognostic tool in patients with in-hospital cardiac arrest. World J Crit Care Med 2019; 8(2): 9-17
- URL: https://www.wjgnet.com/2220-3141/full/v8/i2/9.htm
- DOI: https://dx.doi.org/10.5492/wjccm.v8.i2.9
In-hospital cardiac arrest (IHCA) events account for 370000 to 750000 events annually in the United States and a number much larger globally[1]. Major advances have been made in resuscitation with the advent of target temperature management, rapid response and code teams nationwide in hospitals based on recommendations of the Joint Commission[2]. The vast majority of patients who achieve sustained return of spontaneous circulation (ROSC) from IHCA, however, die before hospital discharge and their prognosis has not changed over the past 30 years[1].
Survival to discharge is estimated to be about 18%[3], and at one year and three years to be 6.6% and 5.2%[4]. Several clinical factors are of prognostic significance after such an event, including type of initial cardiac rhythm[5,6], age, comorbidities, duration of cardiopulmonary resuscitation, and implementation of target temperature management in appropriate candidates[7]. Post-arrest immune-inflammatory markers including interleukin-6 and high sensitivity C-reactive protein (CRP)[8] as well as markers of neuronal damage such serum neuron-specific enolase concentrations[9] and S-100 protein[10] have also shown some promise as prognostic markers after ROSC. Many of these biochemical assays are not routinely performed and have to be specifically ordered at a specialized laboratory, adding cost and time delay in receiving the results. These delays preclude their value in the routine care of these sick patients.
Studies of routinely available lab measures have demonstrated that high blood glucose[11], low potassium[12], high platelet count[13] and high lactate[14] levels are all associated with poor prognosis in patients with cardiac arrest. Recently, a high neutrophil-lymphocyte ratio (NLR) has emerged as a marker of poor prognosis for several cardiovascular and non-cardiovascular conditions[15-21]. While the therapies available, demographics of patients and survival rates are different with in and out of hospital cardiac arrest, a NLR > 6 was found to be associated with mortality independent of epinephrine administration[22] in patients with out of hospital cardiac arrest. The degree of abnormalities i.e., elevated glucose, low potassium, high platelet count and high NLR are all directly proportional to the acuteness and the severity of stress during IHCA driven by high catecholamine levels, whereas NLR values were also affected by inflammation. We chose to study the prognostic relevance of high NLR in IHCA patients beyond other routinely available laboratory measures and evaluate whether adrenergic drive or inflammation was the more important underlying mechanism associated with in-hospital death in these patients.
The study was carried out after obtaining approval from the IRB at Ascension St John Hospital, Detroit, Michigan. We performed retrospective chart review of patients ages 18 years or older at our institution who had sustained ROSC after an IHCA event (Jan 2015 to December 2015). We defined an IHCA event by the Utstein’s criteria as the lack of a cardiac mechanical activity as confirmed by unresponsiveness, absence of a detectable pulse and apnea in patients with a pulse at time of admission[23]. Patients were excluded if they had an out-of-hospital cardiac arrest (n = 102), was a ”do not resuscitate” status prior to event (n = 8), or had missing information (n = 18).
Data on demographics, medical history, physical examination, laboratory and imaging findings, initial cardiac rhythm, treatment, adverse events and outcomes were collected using retrospective chart review and entered into Excel™ database. Complete blood count with differential and other laboratory information collected during 24 h of the IHCA event were recorded. If there were multiple values of the same laboratory measure during first 24 h, only the first value of these measures i.e., closest to IHCA event was entered into the dataset and used for this analysis.
We compared the characteristics of patients who died versus those who survived after ROSC following IHCA. Variables are presented as mean with standard deviation or median with range or interquartile range (IQR) for continuous variables and as counts and percentages for categorical variables. Univariable analysis was doing using Student’s t-test, the Mann-Whitney U test (for non-normally distributed variables) and the chi-squared test. Multivariable analysis was performed using logistic regression model to adjust for baseline confounders and identify independent predictors of in-hospital mortality. Analyses were performed using SPSS (IBM, Armonk, NY, United States), version 25 and a P value of < 0.05 was considered to be statistically significant.
Patients who achieved ROSC after IHCA and later died were more likely to be older and/or had pulseless electrical activity or asystole as the initial recorded rhythm (Table 1). Similarly, lower blood pH and higher serum potassium and higher serum lactate levels were associated with in-hospital death in these patients whereas no relationship was observed for serum glucose level and platelet count. The median NLR was higher in non-survivors [8.94 (IQR): 5.1-18.9] compared with survivors [4.94 (IQR: 3.4-12.7), P = 0.001].
| Survivor | Non survivor | P valuea | |
| Age (yr)1 | 61.6 ± 17.0 | 68.5 ± 15.6 | 0.01 |
| Male | 34.2 % (27) | 65.8% (52) | 0.9 |
| Female | 35.1% (26) | 64.9% (48) | |
| Baseline laboratory values | |||
| Potassium (mmol/L)1 | 4.3 ± 1.1 | 4.6 ± 1.1 | 0.05 |
| Serum lactate (mmol/L)1 | 5.0 ± 3.7 | 8.6 ± 7.0 | 0.001 |
| Glucose (mg/dL)1 | 171 ± 86 | 184 ± 114 | 0.5 |
| Platelet (thousand/cu mm)1 | 217 ± 122 | 201 ± 121 | 0.47 |
| pH1 | 7.3 ± 0.15 | 7.2 ± 0.2 | 0.03 |
| Initial cardiac rhythm | |||
| Pulseless electrical activity | 33.7% (34) | 66.3% (67) | 0.49 |
| Ventricular fibrillation | 54.5% (6) | 45.5% (5) | |
| Pulseless ventricular tachycardia | 50% (3) | 50% (3) | |
| Asystole | 34.8% (8) | 65.2% (15) | |
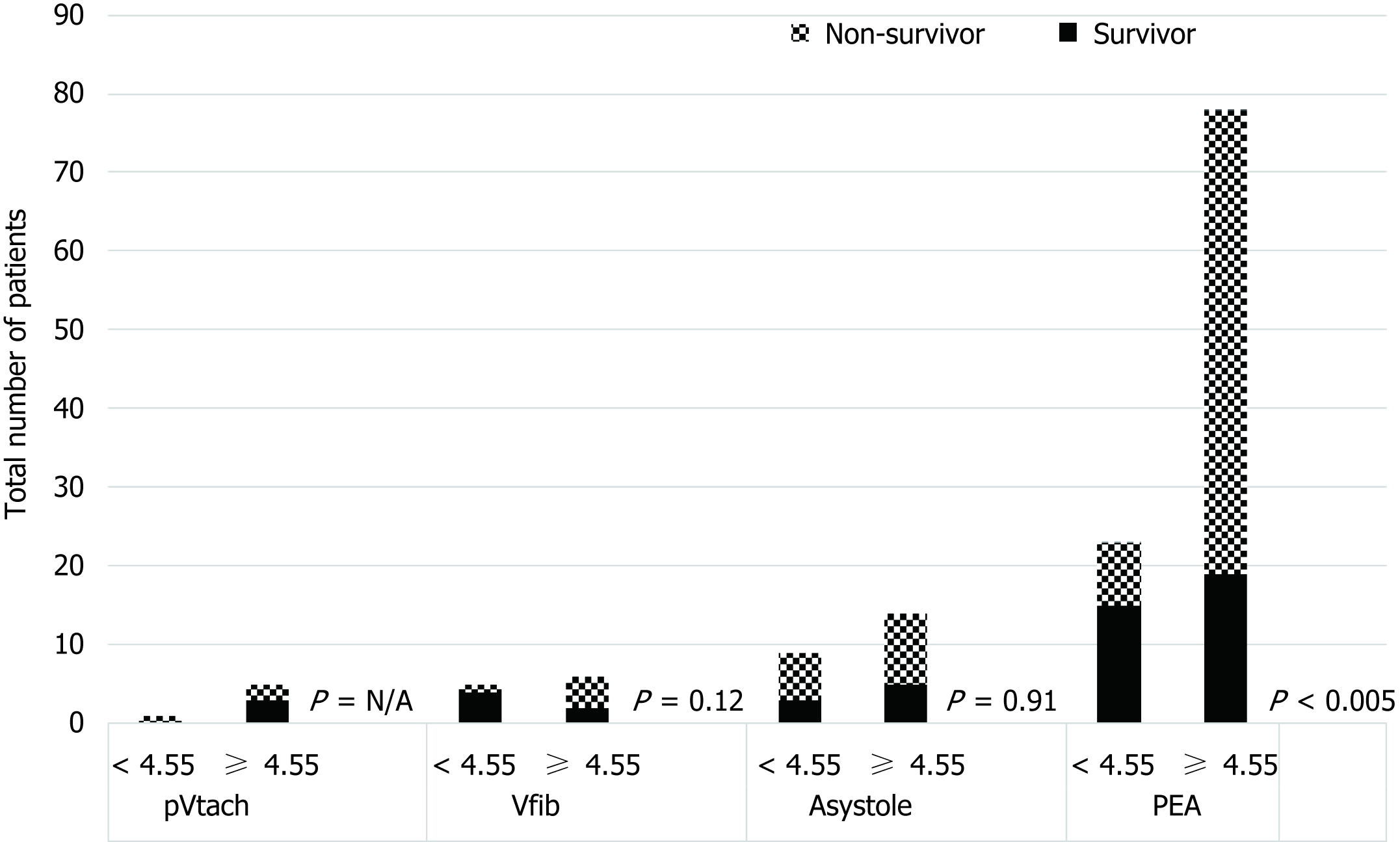
An NLR cut-off of 4.55 derived from receiver operating characteristic analysis (area under the curve = 0.66), provided 73% positive predictive value, 82% sensitivity and 42% specificity for predicting in-hospital death after ROSC following IHCA, (Figure 1). In hospital mortality was higher in patients with NLR ≥ 4.55 compared with those with NLR < 4.55 (82% vs 45%, P = 0.02) (Figure 2). From multivariable logistic regression, an NLR ≥ 4.55 [odds ratio (OR) = 5.2, CI: 1.5-18.3, P = 0.01], older age (OR = 1.03, CI: 1.00-1.07, P = 0.05), and an elevated serum lactate level (OR = 1.2, CI: 1.03-1.4, P = 0.02) as independent predictors of death (Table 2). Type of cardiac rhythm, pH and potassium did not remain significant predictors.
Our study shows that patients with ROSC after IHCA had very high mortality with two-thirds of these patients dying before hospital discharge. In-hospital mortality was significantly higher in patients with older age, initial rhythm that showed pulseless electrical activity or asystole and those with abnormal routinely performed laboratory markers such as NLR ≥ 4.55, increased potassium, elevated lactate and lower blood pH. After adjustment for other risk factors, multivariate analysis identified NLR ≥ 4.55, lower blood pH and older age as independent risk factors for mortality. Markers associated with acute stress during IHCA such as glucose, potassium and platelet level were less useful predictors of mortality compared to non-inflammatory markers such as serum lactate level that reflected the end-result of the metabolic derangement.
The range of sensitivity and specificity of neuron specific enolase with a cutoff level of 33 mg/L as a biomarker for worse neurologic injury after cardiac arrest is reported to be 72%-80% and 84%-100% respectively[24]. The false positive rate of neuron specific enolase is 0%-23%. Similarly the reported range of sensitivity and specificity of S-100 with a cutoff range of 0.2-1.5 mg/L as an adverse marker of neurologic injury after cardiac arrest is 72%-80% and 85%-100% respectively with a 0%-16% false positive rate[24]. Timing of measurement as well a target temperature management or lack of has been shown to have an effect on the sensitivity and specificity of neuron specific enolase and S-100 as biomarkers[25]. For example, in hypothermic patients at 24 h S-100 had a specificity of 100% and sensitivity of 30% compared to 100% and 59% respectively in normothermic patients. At 48 h, the specificity and sensitivity of S-100 in hypothermic patients was 96% and 22% respectively compared to 100% and 88% in normothermic patients[25]. In our study, we found that NLR measured within 24 h of IHCA of greater than or equal to 4.5 has a 82% sensitivity, 42% specificity and a 73% positive predictive value to be a marker of mortality. While it should be noted that a NLR ≥ 4.55 is not specific for absence of mortality with many false positives, the association of high sensitivity and positive predictive value with modest specificity correlate well with the literature showing similar findings in other clinical conditions. Recently, a study on out of hospital cardiac arrest and targeted temperature management showed NLR cut off value of 6 at 72 h after ROSC was achieved with a sensitivity and specificity of 89% and 47% respectively[26].
Inflammatory and non-inflammatory markers are associated with poor prognosis among patients with out-of-hospital cardiac arrest and other cardiovascular and non-cardiovascular conditions. Inflammatory markers including NLR have been studied in multiple cardiac and non-cardiac diseases recently[15-21]. Elevated white blood counts are associated with a higher risk of death among patients with acute myocardial infarction[23]. Recently, a high NLR, available as a part of routine laboratory tests has been shown to be marker associated with poor prognosis among patients with several conditions including acute coronary syndromes[15], venous thromboembolism[16], atrial fibrillation[17], certain types of cancers[18], severe aortic stenosis[19], heart failure[20] and sepsis[21]. Similarly, elevations of other immune-inflammatory markers including interleukin-6 and high sensitivity CRP[8] have also shown some promise as prognostic markers after ROSC. Our study extends the paradigm of the prognostic significance of NLR seen in other cardiovascular conditions to patients with ROSC after IHCA.
Other laboratory non-inflammatory markers such as high blood glucose[11], low potassium[12], high platelet count[13], and high lactate[14] levels as well as markers of neuronal damage such serum neuron-specific enolase concentrations[9] and S-100 protein[10] have also shown to be potentially associated with adverse prognosis in patients with cardiac arrest. With the exception of high lactate, we did not find any independent association of other routinely available laboratory values (blood glucose, serum potassium or platelet count) with in-hospital mortality in patients with ROSC after IHCA.
Two underlying mechanisms that have been postulated to explain the association of various laboratory values and outcomes are stress-induced stimulation of intrinsic adrenergic sympathetic nerves and propagation of the inflammatory cascade. Severe adrenergic stress during IHCA driven by high catecholamine levels elevates blood glucose, platelet count and NLR while depressing serum potassium. In contrast, NLR values also increase in the inflammatory response to IHCA. Our finding of independent correlation of NLR but not of other routinely available laboratory tests may suggest a more important mechanistic role of inflammation than adrenergic sympathetic activation. This hypothesis, however, and whether targeting inflammation following ROSC leads to improved mortality remains to be further confirmed in future studies.
Finally, the association of lactate level with mortality after cardiac arrest and ROSC warrants further discussion. Lactic acid is produced in tissues and organs during periods of hypoperfusion and ischemia[27]. In addition, lactic acid hepatic clearance is impaired in cases of shock liver often a common accompaniment of cardiac arrest. Epinephrine injections inherently used during resuscitation also have been shown to elevate lactic acid[28]. Thus, lactic acid elevation following a cardiac arrest is the end-result of the above underlying mechanisms and higher levels of lactic acid are expected with longer duration of resuscitation and hypoperfusion in cardiac arrest and ROSC[29]. It is not difficult, therefore, to envision why the initial lactic acid level in patients with IHCA and ROSC predicted an increased risk of death.
Our study should be viewed in light of its limitations. This study is a single center retrospective study with modest number of cases and thus subject to missing and incomplete information and our findings should be considered as hypothesis-generating. We did not evaluate the prognostic significance of other biomarkers i.e., CRP, various cytokines, serum neuron-specific enolase concentrations and S-100 protein. Most of these values, however, are not routinely collected and/or have to be sent to specialized laboratories for testing, precluding their value in contemporary practice.
In conclusion, in patients with ROSC after IHCA, in-hospital mortality was high. Our data showed that NLR may be a useful marker of increased risk of in-hospital death in these patients, and thus has potential to improve clinical decision making and family’s understanding of risk of in-hospital death after IHCA. Further study in a large cohort of patients with ROSC after IHCA is needed to confirm our findings and to evaluate if targeting inflammation may help improve mortality in these patients.
Mortality and morbidity after having an in hospital cardiac arrest (IHCA) event are high. Despite the advent of therapeutic modalities such as target temperature management and increased access to rapid response and code blue teams, the survival rates after IHCA are dismal. Markers of poor survival after IHCA have been evaluated and include S-100 and serum neuron-specific enolase concentrations. However, this and many other markers are often analyzed at specialized laboratories and may have a time delay in response. Their routine use is therefore limited.
The main motivation for the study was to evaluate whether neutrophil-lymphocyte ratio (NLR), an easy to obtain marker can be used to gain prognostic information after IHCA patients achieve return of spontaneous circulation (ROSC). Previously, NLR has been evaluated as a marker of poor prognosis for several cardiovascular and non-cardiovascular conditions. Interestingly, a high NLR in patients with out of hospital cardiac arrest (OHCA) has been shown to have increased mortality. It is essential to investigate whether NLR provides any prognostic information in IHCA patients as they are often sicker, older and have poor survival compared to patients with OHCA.
The main objective was to determine the value of an elevated NLR in predicting survival to discharge in patients with IHCA. Furthermore, we evaluated whether a high adrenergic drive or inflammation may be associated with the mechanism associated with IHCA. As a result, we looked at the initial cardiac rhythm and other laboratory values such as potassium, lactate, glucose and platelet level as this may be evaluated in future research as therapeutic targets for improving survival after IHCA.
A retrospective chart review was conducted at our institution of all patients over 18 years of age who has sustained ROSC after IHCA events. Medical records were reviewed for demographics, history and physical examination, laboratory and imaging findings as well as initial cardiac rhythm and outcomes were collected. Of note, the laboratory data was collected during 24 h of the IHCA being recorded.
The main finding out this study was that a NLR cut-off of 4.55 derived from receiver operating characteristic analysis (area under the curve = 0.66), provided 73% positive predictive value, 82% sensitivity, 42% specificity predicting in-hospital death. Multivariable logistic regression analysis yielded an NLR ≥ 4.55 [odds ratio (OR) = 5.2, confidence interval (CI): 1.5-18.3, P = 0.01], older age (OR = 1.03, CI: 1.00-1.07, P = 0.05), and an elevated serum lactate level (OR = 1.2, CI: 1.03-1.4, P = 0.02) as independent predictors of death. Older individuals, or those with pulseless electrical activity and/or asystole as the initial cardiac rhythm were more likely to have died from IHCA despite achieving ROSC. A limitation of this paper is that it did not evaluate the prognostic significance of other biomarkers such as S-100, serum neuron-specific enolase amongst others compared to NLR. Our study was also a single center retrospective study with modest number of cases and as results our findings should be considered as hypothesis-generating.
The new findings of our study are that an increased NLR may be a marker of decreased survival in patients with ROSC after IHCA. NLR may have some utility in improving clinical decision making and family’s understanding of risk of death after IHCA. This study proposes that modulating inflammation may improve mortality in patients after an IHCA event.
The authors suggest using NLR as a tool to further assist in prognosticating patients with ROSC after IHCA. Future investigations may look to compare NLR values and survival before and after currently accepted interventions such as target temperature management or even after modulation of inflammation, a cascade which is less well understood but likely plays a detrimental role in the outcome after IHCA.
Manuscript source: Unsolicited manuscript
Specialty type: Critical care medicine
Country of origin: United States
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C, C
Grade D (Fair): D
Grade E (Poor): 0
P- Reviewer: Cascella M, Inchauspe AA, Sanfilippo F, Zhao L S- Editor: Yan JP L- Editor: A E- Editor: Song H
| 1. | Sandroni C, Nolan J, Cavallaro F, Antonelli M. In-hospital cardiac arrest: Incidence, prognosis and possible measures to improve survival. Intensive Care Med. 2007;33:237-245. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 409] [Cited by in RCA: 441] [Article Influence: 23.2] [Reference Citation Analysis (0)] |
| 2. | Morrison LJ, Neumar RW, Zimmerman JL, Link MS, Newby LK, McMullan PW, Hoek TV, Halverson CC, Doering L, Peberdy MA, Edelson DP; American Heart Association Emergency Cardiovascular Care Committee, Council on Cardiopulmonary, Critical Care, Perioperative and Resuscitation, Council on Cardiovascular and Stroke Nursing, Council on Clinical Cardiology, and Council on P. Strategies for improving survival after in-hospital cardiac arrest in the United States: 2013 consensus recommendations: A consensus statement from the American Heart Association. Circulation. 2013;127:1538-1563. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 204] [Cited by in RCA: 226] [Article Influence: 18.8] [Reference Citation Analysis (0)] |
| 3. | Nadkarni VM, Larkin GL, Peberdy MA, Carey SM, Kaye W, Mancini ME, Nichol G, Lane-Truitt T, Potts J, Ornato JP, Berg RA; National Registry of Cardiopulmonary Resuscitation Investigators. First documented rhythm and clinical outcome from in-hospital cardiac arrest among children and adults. JAMA. 2006;295:50-57. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 857] [Cited by in RCA: 829] [Article Influence: 43.6] [Reference Citation Analysis (0)] |
| 4. | Booth CM, Boone RH, Tomlinson G, Detsky AS. Is this patient dead, vegetative, or severely neurologically impaired? Assessing outcome for comatose survivors of cardiac arrest. JAMA. 2004;291:870-879. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 382] [Cited by in RCA: 368] [Article Influence: 17.5] [Reference Citation Analysis (0)] |
| 5. | Garcia S, Drexel T, Bekwelem W, Raveendran G, Caldwell E, Hodgson L, Wang Q, Adabag S, Mahoney B, Frascone R, Helmer G, Lick C, Conterato M, Baran K, Bart B, Bachour F, Roh S, Panetta C, Stark R, Haugland M, Mooney M, Wesley K, Yannopoulos D. Early Access to the Cardiac Catheterization Laboratory for Patients Resuscitated From Cardiac Arrest Due to a Shockable Rhythm: The Minnesota Resuscitation Consortium Twin Cities Unified Protocol. J Am Heart Assoc. 2016;5:pii: e002670. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 57] [Cited by in RCA: 73] [Article Influence: 8.1] [Reference Citation Analysis (0)] |
| 6. | Doshi P, Patel K, Banuelos R, Darger B, Baker S, Chambers KA, Thangam M, Gates K. Effect of Therapeutic Hypothermia on Survival to Hospital Discharge in Out-of-hospital Cardiac Arrest Secondary to Nonshockable Rhythms. Acad Emerg Med. 2016;23:14-20. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 8] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 7. | Huang Y, He Q, Yang LJ, Liu GJ, Jones A. Cardiopulmonary resuscitation (CPR) plus delayed defibrillation versus immediate defibrillation for out-of-hospital cardiac arrest. Cochrane Database Syst Rev. 2014;CD009803. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 22] [Cited by in RCA: 18] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 8. | Samborska-Sablik A, Sablik Z, Gaszynski W. The role of the immuno-inflammatory response in patients after cardiac arrest. Arch Med Sci. 2011;7:619-626. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 30] [Cited by in RCA: 33] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 9. | Sulaj M, Saniova B, Drobna E, Schudichova J. Serum neuron specific enolase and malondialdehyde in patients after out-of-hospital cardiac arrest. Cell Mol Neurobiol. 2009;29:807-810. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 12] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 10. | Hachimi-Idrissi S, Van der Auwera M, Schiettecatte J, Ebinger G, Michotte Y, Huyghens L. S-100 protein as early predictor of regaining consciousness after out of hospital cardiac arrest. Resuscitation. 2002;53:251-257. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 54] [Cited by in RCA: 54] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 11. | Beiser DG, Carr GE, Edelson DP, Peberdy MA, Hoek TL. Derangements in blood glucose following initial resuscitation from in-hospital cardiac arrest: A report from the national registry of cardiopulmonary resuscitation. Resuscitation. 2009;80:624-630. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 80] [Cited by in RCA: 71] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 12. | Kjeldsen K. Hypokalemia and sudden cardiac death. Exp Clin Cardiol. 2010;15:e96-e99. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 13. | Chung SP, Yune HY, Park YS, You JS, Hong JH, Kong T, Park JW, Chung HS, Park I. Usefulness of mean platelet volume as a marker for clinical outcomes after out-of-hospital cardiac arrest: A retrospective cohort study. J Thromb Haemost. 2016;14:2036-2044. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 10] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 14. | Wang CH, Huang CH, Chang WT, Tsai MS, Yu PH, Wu YW, Hung KY, Chen WJ. Monitoring of serum lactate level during cardiopulmonary resuscitation in adult in-hospital cardiac arrest. Crit Care. 2015;19:344. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 21] [Cited by in RCA: 34] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 15. | Zhou D, Wan Z, Fan Y, Zhou J, Yuan Z. A combination of the neutrophil-to-lymphocyte ratio and the GRACE risk score better predicts PCI outcomes in Chinese Han patients with acute coronary syndrome. Anatol J Cardiol. 2015;15:995-1001. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 12] [Cited by in RCA: 13] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 16. | Barker T, Rogers VE, Henriksen VT, Brown KB, Trawick RH, Momberger NG, Lynn Rasmussen G. Is there a link between the neutrophil-to-lymphocyte ratio and venous thromboembolic events after knee arthroplasty? A pilot study. J Orthop Traumatol. 2016;17:163-168. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 23] [Cited by in RCA: 20] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 17. | Saliba W, Barnett-Griness O, Elias M, Rennert G. Neutrophil to lymphocyte ratio and risk of a first episode of stroke in patients with atrial fibrillation: A cohort study. J Thromb Haemost. 2015;13:1971-1979. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 39] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 18. | Grenader T, Waddell T, Peckitt C, Oates J, Starling N, Cunningham D, Bridgewater J. Prognostic value of neutrophil-to-lymphocyte ratio in advanced oesophago-gastric cancer: Exploratory analysis of the REAL-2 trial. Ann Oncol. 2016;27:687-692. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 55] [Cited by in RCA: 84] [Article Influence: 9.3] [Reference Citation Analysis (0)] |
| 19. | Avci A, Elnur A, Göksel A, Serdar F, Servet I, Atilla K, Mustafa TM, Cuneyt T, Yeliz G, Mustafa B, Metin EA. The relationship between neutrophil/lymphocyte ratio and calcific aortic stenosis. Echocardiography. 2014;31:1031-1035. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 31] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 20. | Benites-Zapata VA, Hernandez AV, Nagarajan V, Cauthen CA, Starling RC, Tang WH. Usefulness of neutrophil-to-lymphocyte ratio in risk stratification of patients with advanced heart failure. Am J Cardiol. 2015;115:57-61. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 99] [Cited by in RCA: 109] [Article Influence: 10.9] [Reference Citation Analysis (0)] |
| 21. | Terradas R, Grau S, Blanch J, Riu M, Saballs P, Castells X, Horcajada JP, Knobel H. Eosinophil count and neutrophil-lymphocyte count ratio as prognostic markers in patients with bacteremia: A retrospective cohort study. PLoS One. 2012;7:e42860. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 101] [Cited by in RCA: 121] [Article Influence: 9.3] [Reference Citation Analysis (0)] |
| 22. | Weiser C, Schwameis M, Sterz F, Herkner H, Lang IM, Schwarzinger I, Spiel AO. Mortality in patients resuscitated from out-of-hospital cardiac arrest based on automated blood cell count and neutrophil lymphocyte ratio at admission. Resuscitation. 2017;116:49-55. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 35] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 23. | Jacobs I, Nadkarni V, Bahr J, Berg RA, Billi JE, Bossaert L, Cassan P, Coovadia A, D'Este K, Finn J, Halperin H, Handley A, Herlitz J, Hickey R, Idris A, Kloeck W, Larkin GL, Mancini ME, Mason P, Mears G, Monsieurs K, Montgomery W, Morley P, Nichol G, Nolan J, Okada K, Perlman J, Shuster M, Steen PA, Sterz F, Tibballs J, Timerman S, Truitt T, Zideman D; International Liaison Committee on Resuscitation; American Heart Association; European Resuscitation Council; Australian Resuscitation Council; New Zealand Resuscitation Council; Heart and Stroke Foundation of Canada; InterAmerican Heart Foundation; Resuscitation Councils of Southern Africa; ILCOR Task Force on Cardiac Arrest and Cardiopulmonary Resuscitation Outcomes. Cardiac arrest and cardiopulmonary resuscitation outcome reports: Update and simplification of the Utstein templates for resuscitation registries: A statement for healthcare professionals from a task force of the International Liaison Committee on Resuscitation (American Heart Association, European Resuscitation Council, Australian Resuscitation Council, New Zealand Resuscitation Council, Heart and Stroke Foundation of Canada, InterAmerican Heart Foundation, Resuscitation Councils of Southern Africa). Circulation. 2004;110:3385-3397. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1109] [Cited by in RCA: 1274] [Article Influence: 63.7] [Reference Citation Analysis (0)] |
| 24. | Scolletta S, Donadello K, Santonocito C, Franchi F, Taccone FS. Biomarkers as predictors of outcome after cardiac arrest. Expert Rev Clin Pharmacol. 2012;5:687-699. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 50] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 25. | Tiainen M, Roine RO, Pettilä V, Takkunen O. Serum neuron-specific enolase and S-100B protein in cardiac arrest patients treated with hypothermia. Stroke. 2003;34:2881-2886. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 242] [Cited by in RCA: 246] [Article Influence: 11.2] [Reference Citation Analysis (0)] |
| 26. | Kim HJ, Park KN, Kim SH, Lee BK, Oh SH, Moon HK, Jeung KW, Choi SP, Cho IS, Youn CS. Association between the neutrophil-to-lymphocyte ratio and neurological outcomes in patients undergoing targeted temperature management after cardiac arrest. J Crit Care. 2018;47:227-231. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 18] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 27. | Correction. Circulation. 2015;131:e535. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 13] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 28. | Donnino MW, Miller J, Goyal N, Loomba M, Sankey SS, Dolcourt B, Sherwin R, Otero R, Wira C. Effective lactate clearance is associated with improved outcome in post-cardiac arrest patients. Resuscitation. 2007;75:229-234. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 118] [Cited by in RCA: 137] [Article Influence: 7.6] [Reference Citation Analysis (0)] |
| 29. | Starodub R, Abella BS, Grossestreuer AV, Shofer FS, Perman SM, Leary M, Gaieski DF. Association of serum lactate and survival outcomes in patients undergoing therapeutic hypothermia after cardiac arrest. Resuscitation. 2013;84:1078-1082. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53] [Cited by in RCA: 60] [Article Influence: 5.0] [Reference Citation Analysis (0)] |