Published online May 4, 2017. doi: 10.5492/wjccm.v6.i2.124
Peer-review started: November 2, 2016
First decision: February 17, 2017
Revised: February 25, 2017
Accepted: March 23, 2017
Article in press: March 25, 2017
Published online: May 4, 2017
Processing time: 185 Days and 7.7 Hours
To synthesize the available evidence focusing on morbidities in pediatric survivors of critical illness that fall within the defined construct of postintensive care syndrome (PICS) in adults, including physical, neurocognitive and psychological morbidities.
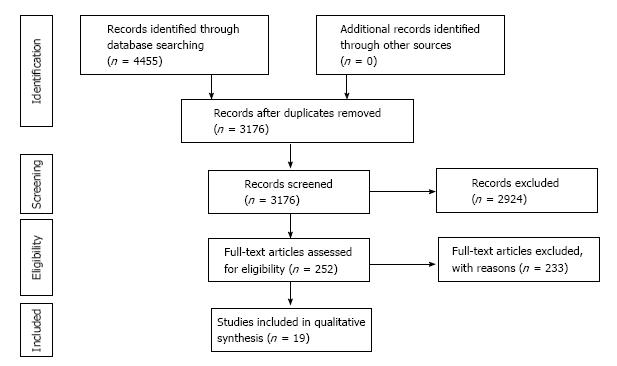
A comprehensive search was conducted in MEDLINE, EMBASE, the Cochrane Library, PsycINFO, and CINAHL using controlled vocabulary and key word terms to identify studies reporting characteristics of PICS in pediatric intensive care unit (PICU) patients. Two reviewers independently screened all titles and abstracts and performed data extraction. From the 3176 articles identified in the search, 252 abstracts were identified for full text review and nineteen were identified for inclusion in the review. All studies reporting characteristics of PICS in PICU patients were included in the final synthesis.
Nineteen studies meeting inclusion criteria published between 1995 and 2016 were identified and categorized into studies reporting morbidities in each of three categories-physical, neurocognitive and psychological. The majority of included articles reported prospective cohort studies, and there was significant variability in the outcome measures utilized. A synthesis of the studies indicate that morbidities encompassing PICS are well-described in children who have survived critical illness, often resolving over time. Risk factors for development of these morbidities include younger age, lower socioeconomic status, increased number of invasive procedures or interventions, type of illness, and increased benzodiazepine and narcotic administration.
PICS-related morbidities impact a significant proportion of children discharged from PICUs. In order to further define PICS in children, more research is needed using standardized tools to better understand the scope and natural history of morbidities after hospital discharge. Improving our understanding of physical, neurocognitive, and psychological morbidities after critical illness in the pediatric population is imperative for designing interventions to improve long-term outcomes in PICU patients.
Core tip: The majority of critically ill children admitted to pediatric intensive care units (PICUs) survive their illness. Therefore, it is critical to address the impact and extent of new or worsening morbidities that these children experience as a consequence of critical illness. Postintensive care syndrome is a well-described phenomenon in adult ICU patients, defining common types of morbidity that can occur after hospitalization. This review provides a synthesis of the available literature describing physical, neurocognitive and psychological morbidities that develop in the pediatric critical care population.
- Citation: Herrup EA, Wieczorek B, Kudchadkar SR. Characteristics of postintensive care syndrome in survivors of pediatric critical illness: A systematic review. World J Crit Care Med 2017; 6(2): 124-134
- URL: https://www.wjgnet.com/2220-3141/full/v6/i2/124.htm
- DOI: https://dx.doi.org/10.5492/wjccm.v6.i2.124
Medical and technological advances over the last several decades have resulted in the lowest rates of mortality in the pediatric intensive care unit (PICU)[1]. Therefore, mortality alone is no longer a sufficient outcome measure for assessing the efficacy of pediatric critical care interventions. Instead, outcomes in pediatric critical care have come to focus on morbidity that exists at and after discharge from the PICU.
The concept of postintensive care syndrome (PICS) is well-described in the adult critical care literature[2]. In 2010, a stakeholder’s meeting defined PICS as “new or worsening impairments in physical, cognitive, or mental health status arising after critical illness and persisting beyond acute care hospitalization”. These stakeholders also identified PICU patients as a subgroup of critically ill patients that deserve increased attention in ICU research and literature.
Studies in adults have demonstrated that a significant number of adult critical care survivors develop long-lasting morbidities after an ICU admission. For example, a study of acute respiratory distress syndrome (ARDS) survivors found that physical impairments occur in greater than 50% of previously healthy patients in the first year after illness[3]. With regard to cognitive impairment, there is evidence of long-lasting mild to moderate cognitive impairment in 24% of ARDS survivors at a median of 6 years after ICU admission[4]. Additionally, a systematic review examining mental health morbidity in adult critical care survivors found a median 28% point prevalence of clinically significant depressive symptoms[5].
Although PICS has drawn attention in the adult ICU, pediatric studies examining morbidity after critical illness are just recently emerging. Moreover, pediatric outcomes after critical illness have not been examined using the lens of PICS, which may be a beneficial approach for uniformly synthesizing available data and designing future studies investigating the effects of pediatric critical illness and treatment. The need to characterize PICS is even more critical due to the high proportion of PICU patients with pre-existing comorbidities that may worsen functional outcomes and quality of life after a PICU stay[6].
The objective of this systematic review is to synthesize the available evidence focusing on morbidities in pediatric survivors of critical illness that fall within the construct of PICS described in the adult literature. With a comprehensive view of new and worsening physical, neurocognitive and mental health morbidities affecting critically ill children, future interventional research can be conducted using common language and tools for measuring outcomes with the eventual goal of mitigating these morbidities.
All prospective, cross-sectional and retrospective studies examining physical, neurocognitive and/or mental health morbidity in pediatric critical care survivors after discharge were included if the study included a heterogeneous PICU sample. Studies focusing on one specific disease or subpopulation were excluded (e.g., patients with traumatic brain injury or congenital heart disease) as the aim of this review was to examine the extent of morbidities mentioned above on as broad a group of pediatric critical care survivors as possible. Studies primarily focusing on families or caregivers, as opposed to children, were not included. In addition, studies in neonates admitted to a neonatal intensive care unit were excluded due to key neurodevelopmental differences between the NICU and PICU population.
The literature search (Appendix A) was conducted on March 28, 2016 with the collaboration of an informationist to identify relevant articles and was applied to MEDLINE, EMBASE, the Cochrane Library, PsycINFO, and CINAHL. Controlled vocabulary, such as Medical Subject Headings and Emtree terms, when appropriate, were used in combination with keywords for the concepts of PICUs and PICS. The concept for PICUs included terms such as pediatric intensive care unit, PICU, and pediatric critical care. The concept for PICS included terms such as PICS and post-ICU syndrome, as well as terms likely to return articles that had a discussion of the physical, cognitive and psychological morbidities associated with a pediatric critical care admission, such as quality of life and wellbeing. An effort was made to account for plurals, acronyms, and synonyms. The search was limited to English-language articles. Search results yielded 3176 results, which were then reviewed by two independent reviewers for eligibility. A total of 252 of these articles met the inclusion criteria and were retrieved for full text review (Figure 1). In addition, references of the included studies and review articles were inspected in order to identify additional relevant studies.
Nineteen studies of critically ill children surviving admission who were followed up after hospital discharge to assess for physical, neurocognitive, and mental health morbidities were included in this review (Table 1)[7-25]. Within each broad morbidity category, heterogeneous patient populations (e.g., age), outcome measures, and follow-up time points were used. Thus, while the authors intended to perform a quantitative synthesis of included studies, this was not possible and a qualitative synthesis was conducted. We categorized included articles by the type of morbidity after pediatric critical illness according to the definition of PICS previously described. The majority of included articles examined physical and psychological morbidity while a small proportion focused on neurocognitive morbidity following PICU admission.
| Ref. | Design | n | Age | Patient sample | Timing of follow-up | Measures used | Main findings |
| Physical morbidity after pediatric critical illness | |||||||
| Als et al[8] | Prospective cohort | 88 (100 controls) | 5-16 yr | PICU admission for ≥ 28 d | 5 mo (median) | Strengths and Difficulties Questionnaire; Chalder Fatigue Scale; Children’s Sleep Habits Questionnaire; Impact of Event Scale | Significant minority of school aged children at risk for short-term physical morbidity |
| Colville et al[13] | Prospective cohort | 97 | > 7 yr | 3 mo and 1 yr | Pediatric QOL Inventory | PQLI scores lower at 3 mo compared to non-clinical community sample but comparable at 1 yr Physical functioning subscale lower in PICU survivors but improved over time | |
| Gemke et al[15] | Prospective cohort | 226 | Children up to 16 yr, excluding infants | 1 yr | Multiattribute health status classification | Health status in 75% of population preserved | |
| Jayashree et al[16] | Prospective cohort | 150 | 1-12 yr | 1 yr | Multiattribute Health Status Classification | QOL preserved in approximately 75% of patients Neurological illness risk factor for decline in QOL | |
| Jones et al[17] | Descriptive study | 1455 | ≥ 6 mo | 6 mo | Health Utilities Index 2 | 27% of children with no impairments | |
| Knoester et al[18] | Prospective cohort | 81 | 1-15 yr | 3 mo and 9 mo | Children’s QOL Questionnaire | Health related QOL improves over time | |
| Namachivayam et al[20] | Cohort study and prospective database review | 4010 | All ages including adults at time of follow-up | 2.5-3 yr (1982); 2.5-6 yr (1995); 0.5-2.9 yr (2005-2006) | Modified Glasgow Outcome Score; Health Status Utility Index | Proportion of survivors with moderate or severe disability ↑ in 2005-2006 compared to 1982 and 1995 | |
| Namachivayam et al[21] | Prospective cohort | 233 | Median 4.2 mo at admission | Long-stay patients | > 6 mo; median of 4 yr | Modified Glasgow Outcome Scale; Health Utilities Index Mark 1 | Long term functional outcome favorable in 50% of survivors QOL poor in 68% |
| Taylor et al[25] | Prospective cohort | 1032 | 0-29 yr | 2-6 yr | Glasgow Outcome Score; Health State Utility Index Mark 1 | Majority of children survive with excellent QOL and functional outcome | |
| Neurocognitive morbidity after pediatric critical illness | |||||||
| Als et al[7] | Prospective cohort | 88 (100 controls) | 5-16 yr | 3-6 mo | Same as Als 2015 | Children have deficits in neuropsychologic performance and school performance | |
| Als et al[9] | Prospective cohort | 23 | 5-16 yr | 1 yr | Cambridge Neuropsychological Automated Battery; Children’s Memory Scale; Wechsler Abbreviated Scale of Intelligence or Wide Range Intelligence Test | Persistently reduced neuropsychological function in PICU survivors | |
| Psychological morbidity after pediatric critical illness | |||||||
| Als et al[8] | Prospective cohort | 88 (+ 100 controls) | 5-16 yr | PICU admission for ≥ 28 d | 5 mo (median) | Strengths and Difficulties Questionnaire; Chalder Fatigue Scale; Children’s Sleep Habits Questionnaire; Impact of Event Scale | Significant minority of school aged children at risk for short-term mental morbidity |
| Bronner et al[10] | Prospective cohort | 36 | 8-17 yr | 3 mo and 9 mo | Dutch Children’s Responses to Trauma Inventory | 34.5% of children had subclinical PTSD 13.8% likely to meet criteria for PTSD | |
| Colville et al[11] | Prospective cohort | 102 | 7-17 yr | 3 mo | ICU Memory Tool; abbreviated Impact of Event Scale | 32% reported delusional memories Post-traumatic stress scores higher in those with delusional memories Longer courses of opiates/benzos associated with delusional memories | |
| Colville et al[12] | Prospective cohort | 66 | 7-17 yr | 3 mo and 12 mo | Children’s Revised Impact of Event Scale | At 3 mo, 32% of children experienced posttraumatic stress symptoms; 26% at 12 mo | |
| Dow et al[14] | Prospective cohort | 59 | 6-16 yr | 6 mo | Children’s PTSD Inventory | Minority (17%-29%) of children met PTSD criteria | |
| Muranjan etal[19] | Prospective cohort | 30 | ≥ 5 yr | Age and sex matched to pediatric general wards patients | 1 mo | Impact of Event Scale; Birleson Depression Scale; Self-Esteem Scale; Therapeutic Interventions Scoring System; Temperament Measurement Schedule | PICU patients subjected to therapeutic interventions have transient psychological impairment following admission |
| Rees et al[22] | Retrospective cohort | 68 | 5-18 yr | Compared to general ward patients | 6-12 mo | Clinician Administered PTSD Scale for Children; Impact of Event Scale; Strengths and Difficulties Questionnaire; Birleson Depression Scale; Revised Children’s Manifest Anxiety Scale; Child Somatization Inventory | 21% of PICU patients developed PTSD compared to none of the ward patients |
| Rennick et al[23] | Prospective cohort | 60 per cohort | 6-17 yr | Age and sex matched to pediatric general wards patients | 6 wk and 6 mo | Invasive Procedure Score; Children’s Impact of Event Scale; Posthospital Behavior Questionnaire; Children’s Health Locus of Control Scale; Child Medical Fear Scale | Regardless of hospital location: greater degree of invasiveness, illness severity and younger age contribute to higher likelihood of posttraumatic stress response after discharge |
| Rennick et al[24] | Prospective cohort | 60 | 6-17 yr | 6 wk and 6 mo | Children’s Impact of Event Scale; Children’s Medical Fears Scale; Children’s Health Locus of Control Scale | Children who have high numbers of invasive procedures at higher risk of developing psychological morbidity 6 wk after discharge | |
Nine studies reported physical and functional morbidity after PICU admission (Table 1). Namachivayam et al[20] examined and compared three different cohorts of PICU patients in the years between 1982 and 2006, evaluating outcomes both at discharge and at follow-up months to years later. The modified Glasgow Outcome Score (MGOS) was used to assess long-term functional outcomes in 4010 patients. Categories included: (1) normal or functionally normal (both intellectually and physically); (2) mildly disabled but likely independent; (3) moderately disabled and dependent on care; (4) severely disabled and totally dependent on care; and (5) death. The MGOS was determined based on parent/guardian interview or patient interview if the patient had reached adulthood and was independent at time of follow-up. The proportion of children with moderate to severe disability at long-term follow up was 8% of 700 children in 1982 and 18% of 717 children in 2005-2006, an increase of 112%. Of note, in 1982 and 1995, a high proportion of children were followed up (100% and 84%, respectively), but 58% of children were lost to follow-up in the 2005-2006 cohort. There was also a shorter period of surveillance (median 1.1 years) in the most recent cohort.
Two years later, Namachivayam et al[21] reported the functional outcomes and quality of life of children admitted to a PICU with a length of stay greater than or equal to 28 d over a period of 20 years. Follow-up after ICU admission was at least 6 mo later with a median of 4 years, and pre-admission health status and long-term functional outcomes were assessed using the MGOS. Greater than 50% of survivors (63/117) had a favorable outcome, meaning that they were likely to lead an independent existence (normal, functionally normal or mild disability). However, more than two-thirds of the initial cohort admitted to the PICU had an unfavorable outcome (moderate or severe disability or death). Notably, 86% of the long-stay patients had pre-existing comorbidities.
Jones et al[17] assessed outcomes at 6 mo after PICU admission based on the Health Utilities Index questionnaires returned by 1455 families of children six months and older. The Health Utilities Index examines sensation, cognition, emotion, pain, mobility and self-care attributes. Sixty-eight percent of children had no mobility impairment. However, the consent rate for follow-up evaluation was only 39% of children who survived to PICU discharge and those who did not provide consent had greater illness severity and were more likely to have previous comorbidities.
Als et al[8] investigated physical well-being from the standpoint of fatigue and sleep difficulty. Eighty-two children admitted between 2007 and 2010 were followed up three to six months after discharge and compared to 93 healthy controls. They found that 38% of critical care survivors were at risk for fatigue disorder compared to 1% of healthy controls using the Chalder Fatigue Score. Additionally, 72% of PICU patients vs 49% of healthy controls were at risk for a sleep disorder. Fatigue was predicted by vulnerability factors, including white race and nonintact homes, while sleep disturbance was not.
Taylor et al[25] evaluated long-term quality of life and functional outcome after pediatric critical illness in children 0 to 29 years of age. The patients were followed up at a median of 3.5 years after PICU discharge. The Glasgow Outcome Score was used to assess functional outcome while the Health State Utility Index (Mark 1) was used to assess quality of life. Of the 1032 children admitted to the PICU in 1995, 868 patients had follow-up data. Only 10% of survivors had an unfavorable outcome likely to lead to dependency on other’s care. The majority of children (84%) also had a favorable quality of life, however, 29% of children survived with disabilities.
In contrast to the traditionally reported parent surveys, Colville and Pierce[13] investigated children’s self-reported quality of life. Ninety-seven children over the age of 7 were followed up at 3 mo and 1 year after PICU discharge with the Pediatric Quality of Life Inventory (physical, emotional, social and school functioning) among other surveys. Children with significant learning difficulties were excluded. At three months after discharge, the Pediatric Quality of Life Inventory scores were lower in the PICU group compared to a non-clinical community group reported in previous literature. One year after discharge, the scores were comparable. The physical functioning subscale scores were lower in the PICU group but improved over time.
Three studies investigated changes in mobility among PICU survivors. Jayashree et al[16] found that mobility was affected in 49% of 150 critically ill children prior to admission while at 1 year after discharge 89% of these children had improving or unchanged mobility. Knoester et al[18] reported similar improvement in mobility when studying previously healthy children admitted unexpectedly to a PICU who were then followed up three and nine months after discharge. In the six to twelve year cohort, parents reported worse motor function at three months but not at nine months; adolescents also self-reported worse motor functioning at three months only. Parents and children who completed questionnaires at both time points demonstrated no difference in overall health related quality of life over time. Gemke et al[15] reported health-related quality of life of 226 patients, excluding infants, one year after PICU admission. Pre-admission health status was estimated based on a questionnaire completed by parents during an interview within 48 h of admission. The multiattribute health status classification (MAHSC) was used as a generic health status measure. At twelve months after discharge, only 10% of patients had deterioration in mobility.
Several other studies evaluating quality of life using various validated measures but only provide an assessment of overall quality of life without results from each category examined (e.g., physical function)[6,26-28].
Two of the included studies described neurocognitive morbidities in PICU patients. In a study of the same PICU cohort and healthy controls described under physical and functional morbidities[8], Als et al[7] evaluated neuropsychological function and academic performance. The children admitted to the PICU were placed into three subgroups: Meningoencephalitis, sepsis, and those with nonneurologic and nonseptic critical illness. The neuropsychologic battery was designed to focus on primarily intellectual function, memory and attention. Both the PICU cohort and the healthy controls had average IQs; however, the PICU cohort scored significantly lower on measures of verbal and visual recall and recognition memory, spatial working memory and working memory capacity, and visual sustained attention. Younger age, lower socioeconomic status and the meningoencephalitis subgroup were significantly associated with more widespread impairment. The academic questionnaire completed by teachers of PICU patients and healthy controls revealed more PICU children with deteriorating academic performance, with the sepsis group showing greatest deterioration, most difficulty with schoolwork completion and attention problems. Interestingly, the nonneurologic/nonseptic critical care cohort did not show any difference in school performance compared to healthy controls.
Finally, in a subsequent prospective follow-up study by Als et al[9], the 23 of 47 children who were identified as neuropsychologically impaired at three to six months following PICU admission were then evaluated 12 mo after PICU discharge in order to better understand the persistence of these impairments. At the three to six month follow-up vs twelve month follow-up, there was no significant change in IQ scores; however, there was improvement in some verbal and visual memory domains. The questionnaires completed by school teachers did not show significant change in children’s global educational progress or learning skills.
Nine studies focused on psychological morbidity in PICU survivors. Most recently, Dow et al[14] explored the prevalence and presentation of posttraumatic stress in 59 school-aged children and adolescents six months after PICU admission lasting at least eight hours. Post-traumatic stress disorder (PTSD) was evaluated using the Children’s PTSD Inventory during a clinician administered interview. Depending on the criteria and algorithm used, the prevalence of PTSD found was 17%-29%. All patients reported the following symptoms most frequently: Inability to recall aspects of the event, hypervigilance, avoidance of thoughts or feelings, physiological reactivity to trauma reminders, and intrusive thoughts or pictures. School-aged children more frequently endorsed avoidance of thoughts and feelings while adolescents more frequently endorsed difficulty concentrating.
Colville and Pierce examined rates and natural history of post-traumatic stress symptoms in families after a pediatric critical care admission, including 66 children at both three and twelve months after PICU discharge[12]. While the study evaluated child-parent pairs, the data for children was reported separately. The Children’s Revised Impact of Event Scale (CRIES-8), a brief, validated scale which detects posttraumatic symptoms and PTSD was chosen as the questionnaire for children. At the three and twelve-month time points, 32% and 26% of children demonstrated symptoms of post-traumatic stress respectively, with no significant change in median score. However, seven children who did not initially score positive at three months after discharge scored positive at twelve months. Of note, those children who scored positive for PTSD at twelve months after discharge had higher scores at three months as well as higher Pediatric Index of Mortality (PIM) scores on admission. The authors suggested that the subjective experience of a child influences likelihood of future distress more so than objective experience (e.g., demographic or medical variables). Participants in the study were also asked what the “worst thing” was during PICU admission. Many of the children pointed to one specific distressing event in the PICU (e.g., hallucinations, waking up and not knowing where their parents were). Interestingly, 35% of children stated that the worst experience occurred outside of the PICU (e.g., the inciting incident that led to admission or deterioration prior to admission).
Four years earlier, Colville et al[11] followed 102 children ages 7 to 17 at a median of 3 mo after PICU discharge to determine if delusional memories from PICU admission were associated with post-traumatic stress symptoms. Children’s memories were characterized using the ICU Memory Tool and the Children’s Revised Impact of Event Scale was used to screen for posttraumatic symptoms. Thirty-two percent of the children had delusional memories, and only two patients reported these memories occurring outside of the time of their PICU stay. A longer course of opiates and benzodiazepines was associated with delusional memories, and children with delusional memories had higher post-traumatic stress scores. There was not, however, a significant association between factual memory and post-traumatic stress symptoms.
A number of the included studies focused on risk factors for psychological morbidity after PICU admission. First, Rennick et al[23] conducted a study in 2002 comparing 120 children six weeks and six months after hospital discharge admitted to either a PICU or a general pediatric ward. Several scales were used to assess the presence and degree of psychological impairment. Regardless of admission location, they found that children with a younger age, greater illness severity, and those subjected to a greater number of invasive procedures had ongoing posttraumatic symptoms, lower sense of control over health, and more medical fears six weeks after hospital discharge. At six months after discharge, only the children who were exposed to higher numbers of invasive procedures had significantly more medical fears and symptoms of posttraumatic stress.
As a follow up to this study, Rennick et al[24] investigated if there was a group at higher risk for developing psychological morbidity after PICU discharge. PICU patients were categorized as high risk (vs low risk) for developing psychological morbidity if they had higher severity of illness and higher number of invasive procedures. Similar to findings in the previous study, it was found that the children with high numbers of invasive procedures were at higher risk of developing psychological problems 6 wk after discharge. At 6 mo after discharge, the high risk group had a significantly higher prevalence of posttraumatic stress symptoms.
In another study of risk factors for psychological morbidity, Muranjan et al[19] enrolled 30 medical patients who survived a PICU admission and compared them to a control group of 30 children admitted to a general pediatric ward. Children were followed up one month after discharge to evaluate psychological symptoms. This study found that children admitted to the PICU and general wards had comparable pre-morbid temperament, as well as self-esteem scale and depression scores. Children admitted to the PICU initially reported more intrusive thoughts compared to the general ward cohort (43% vs 77%, respectively) within the first 24 h after discharge but scores were comparable one month after discharge, suggesting posttraumatic symptoms were short lived. While development of intrusive thoughts correlated with degree of intervention, demographic factors, underlying disease, severity of illness and length of hospitalization did not correlate with degree of psychological morbidity.
In a retrospective cohort, Rees et al[22] aimed to determine if patients discharged from a PICU had greater psychological morbidity compared to children discharged from a general ward. Children ages five and older were included and followed up 6 to 12 mo after discharge. Children with meningococcal disease, terminal illness, an underlying neurologic disorder, or intentional overdose were excluded. Of patients admitted to the PICU, 21% met diagnostic criteria for PTSD with symptoms of irritability and persistent avoidance of reminders of their admission being most prominent; however, only one (vs four) PICU patients was diagnosed with PTSD at the interview. None of the pediatric ward patients developed PTSD, and there was no significant difference between the two groups in scores relating to anxiety, depression or somatization.
Bronner et al[10] compared the development of PTSD in pediatric critical care survivors to children who survived a major fire disaster. This group investigated the presence of PTSD in a cohort of 36 previously healthy children admitted unexpectedly to the PICU three and/or nine months after discharge. Children completed the Dutch Children’s Responses to Trauma Inventory, which identified 34% with at least subclinical PTSD at 3 mo with 14% of those children likely to meet criteria for PTSD. At nine month follow-up, 36% of children had at least subclinical PTSD with 18% of those children likely to meet criteria for PTSD. Only two children had a change in score between the three month and nine month follow-up time points (one going from normal to subclinical, the other subclinical to normal). Compared to survivors of a major fire disaster in the Netherlands, the investigators found that the PTSD scores of children in both groups were comparable. Of note, the PICU population studied in this paper were at risk for possible brain damage, perhaps falsely elevating the number of children who fell into the categories of subclinical PTSD or likely to meet criteria for PTSD due to overlap in symptoms.
Finally, in the same article by Als et al[8] discussing physical morbidity after PICU admission, presence of mental health morbidity was also assessed. A questionnaire was mailed to the families who agreed to participate. Thirty-four percent of children scored at risk for PTSD. In addition, the PICU group scored significantly worse than the control group on the sections of emotional symptoms and hyperactivity. Moreover, twenty percent of the PICU group scored at high risk for a psychological disorder, compared to 9% in the healthy control group. Septic illness was an independent predictor of post-traumatic stress symptoms.
This systematic review summarizes the available literature from nineteen studies investigating outcomes in survivors of pediatric critical illness within the context of PICS. The synthesis revealed that, similar to adult ICU patients, a wide range of physical, neurocognitive and psychological morbidities occur in PICU patients after discharge[29]. The populations investigated encompass a heterogeneous group of subjects with regard to age, type of illness, illness severity, length of hospital stay, and medical interventions. Many, but not all, studies excluded patients with traumatic brain injury or baseline neurocognitive dysfunction. Children were also followed up after hospitalization at different time points, including weeks to months to years later. A major source of heterogeneity was the outcome measures and assessment tools utilized across each category of PICS morbidities. However, this synthesis identifies a critical need to continue to define the landscape of pediatric PICS and guide future research directions by characterizing the types and extent of morbidities that exist in survivors of pediatric critical illness.
Patients and families are substantially impacted by critical illness, and the changing spectrum of critical illness, technological advances, and improved survival has translated to increased morbidity in the pediatric population[1,30]. The sequelae of PICS can lead to reduced quality of life and functional impairments, in addition to increased societal costs[30-32]. Major differences between children and adults with regard to the implications of PICS include increased years of survival with morbidity after critical illness and the complex nature of interactions between PICS and the developing brain.
In several studies investigating physical and functional morbidity in pediatric critical illness survivors, information was gleaned from quality of life surveys that included specific information about physical functioning after PICU admission[13,15-18,21,25]. Multiple screening tools were used to determine the presence or absence of morbidity. Some studies used one follow up time point, which could be within a range of times after PICU discharge, while others used multiple follow up time points. Studies indicated that the minority of survivors of pediatric critical illness have physical morbidities, and if they are present after hospital discharge they decrease over time. For example, one study reporting health related quality of life found that only about 10% of patients (excluding infants) had a deterioration in mobility 1 year after PICU admission, compared to “pre-admission” health status[15]. However, another study comparing PICU populations in 1982 and 2006 did find that a considerably greater percentage of patients had moderate to severe disabilities in 2006 (8% vs 18%)[20]. This is not a surprising finding as more children survive critical illness with improvements in medical care and technology. However, this trend highlights an increased need for early mobilization and acute rehabilitation initiatives in the PICU to decrease the risk of ICU-acquired weakness and potentially increase functional outcomes after discharge[30,33-35].
Of the three broad types of morbidity included in the definition of PICS, this review yielded the fewest number of articles related to neurocognitive morbidity after pediatric critical illness. The same team of authors published two papers assessing the neurocognitive function of school-aged children at 3 to 6 mo and 12 mo after critical illness[7,9]. These patients were compared to healthy controls. While both groups of children had average IQs at the 3 to 6 mo time point, it is important to note that those who survived critical illness had consistently lower scores in verbal and visual domains, particularly in patients who had meningoencephalitis. Moreover, risk factors for greater neurocognitive impairment at time of initial follow up included those of younger age and with lower socioeconomic status. At 12 mo, there was some improvement in verbal and visual domain scores but no significant change in global education progress, suggesting that neurocognitive impairment in certain domains may improve over time, or at least not become worse. Regardless, it is important to consider which children may have more difficulty in school and with certain types of daily tasks after they leave the PICU, whether based on demographics or type of illness, so that they can receive additional educational support once they have returned to school. Large-scale studies are needed and ongoing to better characterize the short and long-term neurocognitive morbidity associated with pediatric critical illness in the developing brain[36].
Although the evidence is limited, psychological morbidity has perhaps been the aspect of PICS that has received the most attention after PICU discharge[8,10-12,14,19,22-24]. All studies included in our review evaluated school-aged patients for post-traumatic stress symptoms, which may be related to “post traumatic stress” being included as a specific term in the search strategy encompassing psychiatric morbidity after PICU admission. However, multiple screening tools were utilized to determine the presence or absence of symptoms. Follow up time points ranged from 6 wk to 12 mo after critical illness. The synthesis of studies suggests that psychological morbidity including post-traumatic stress occurs in one-third of PICU survivors. Of importance, several studies investigating two time points found that post-traumatic stress symptoms seem to attenuate over time.
Several studies also aimed to investigate potential risk factors for developing post-traumatic stress symptoms[8,11,19,23,24]. Septic illness was an independent predictor of post-traumatic stress in one study[8], while three others found that increased numbers of invasive procedures or interventions increased the risk of psychological morbidity[19,23,24]. Delusional memories were associated with increased benzodiazepine or narcotic administration during a PICU course[11]. Benzodiazepines are an independent risk factor for delirium in the adult ICU patient, and emerging evidence in pediatrics suggests a similar association[37,38]. With validated screening tools available to diagnose delirium in the PICU, PICU providers are obligated to address risk factors and treat delirium using non-pharmacologic and pharmacologic therapies in consultation with child psychiatry[39-46]. Sleep disturbances including night terrors are not an uncommon sequelae after ICU discharge in both pediatric and adult patients[8,41,47-49]. An improved understanding of risk factors for psychological morbidity is crucial to facilitate anticipatory guidance for families after a child is discharged from the PICU.
A major barrier to PICS research that is obvious but challenging to resolve is that it is difficult to establish an accurate pre-admission baseline for children admitted to the PICU. Thus, studies that attempt to compare pre-morbid or pre-admission conditions of pediatric patients rely upon either parent and/or child memory of a patient’s functioning prior to admission. Families are likely in a significant state of stress when asked to recount their children’s pre-admission status within the 48 h of admission. Many of the studies in this review used control groups, such as normal pediatric population controls or pediatric ward patients, in order to understand how the trajectory of survivors of pediatric critical illness compared. However, it would be ideal to understand a patient’s trajectory starting before PICU admission, in the PICU, and after discharge from the PICU in order to best understand if morbidities that develop after a PICU admission are persistent and to what degree compared to pre-illness condition.
Another impediment is that many of the measurement tools used to assess quality of life, physical, neurocognitive or psychological morbidity rely primarily on parental assessment. This is necessary in many circumstances when a patient’s developmental level does not allow for him or her to understand or answer questions, but parents were also asked to answer questions or fill out surveys in many circumstances when a child could have done the same. A parent’s response may not accurately represent the thoughts, feelings and experiences of the child. For example, one study found that the agreement between parent and child report is poor[50]. In the future, an effort should be made to include child report when possible.
Finally, none of the studies reviewed discuss the impact of delirium on morbidity experienced by survivors of pediatric critical illness. Delirium is an independent predictor of increased hospital length of stay, prolonged mechanical ventilation, long-term cognitive impairments, and PTSD in adults[51-54]. There is relatively little data on morbidity associated with delirium in the pediatric critically ill population[55]. Case reports and point prevalence studies suggest rates of pediatric delirium between 10% and 30%[38,43,45,56]. As the concept of pediatric delirium becomes better recognized and studied, it will be interesting to understand the interplay between critically ill children diagnosed with delirium and its effect on long-term morbidities.
This systematic review has identified the wide range of morbidities that fall within the construct of PICS in PICU patients. An important next step will be to closely examine what is already known about these physical, neurocognitive and psychological morbidities to define pediatric PICS and come to a consensus on the most relevant and generalizable outcome measures. Ultimately, the aim is to develop interventions both in the PICU and after discharge to help mitigate potential ongoing impairment resulting from critical illness and medical interventions. Many PICUs have already started to address ways to minimize morbidity such as promotion of early mobilization, improved sedation plans, delirium screening and even ICU diaries[57] in an effort to blunt the physically and mentally traumatic effects of critical illness. However, it is important for pediatric intensivists to first acknowledge the morbidity that persists beyond PICU discharge and agree upon consistent language and outcome measures so that effective and targeted interventions will become integrated into part of daily care starting in the PICU.
This systematic review evaluates the presence of PICS in pediatric survivors of critical illness. Physical, neurocognitive, and psychological morbidity affects a significant minority of this vulnerable population. These findings will likely help focus future research efforts on this topic in order to gain a better understanding of which children are most susceptible to developing PICS and of what can be done to mitigate these morbidities.
The authors would like to thank Ms. Carrie Price for guidance with the literature search strategy.
In 2010, an adult consortium developed the concept of postintensive care syndrome (PICS), which encompasses physical, cognitive and mental health morbidities that exist in a high percentage of adults after critical illness. The aim of this current review was to summarize the relevant pediatric literature on these types of morbidities in a general pediatric intensive care unit (PICU) population and understand how widespread this recently described syndrome is among pediatric survivors of critical illness.
Mortality is a rare event in pediatric critical illness, however, it has often been used as an outcome measure in research studies. More appropriate outcome measures include different types of morbidity. It is important to understand what kinds of morbidities burden children after critical illness and how a multidisciplinary team both in the PICU and in follow up settings can mitigate morbidities that develop during and persist after critical illness.
Previous studies have shown different types of morbidity that exist in survivors of pediatric critical illness but there has been no review of pediatric literature through the lens of PICS.
Children who survive pediatric critical illness can develop physical, neurocognitive and/or psychological morbidity after hospital discharge. Knowing this, the authors can better define the extent and natural history of these morbidities and take measures to mitigate morbidity that results from critical illness and its treatment.
PICS: Postintensive care syndrome; PICU: Pediatric intensive care unit.
Herrup et al present a nice and informative overview. The work is well written, based on a systematic literature review, and informative.
Manuscript source: Invited manuscript
Specialty type: Critical care medicine
Country of origin: United States
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P- Reviewer: Classen CF, Greco G, Sarin YK S- Editor: Ji FF L- Editor: A E- Editor: Lu YJ
| 1. | Pollack MM, Holubkov R, Funai T, Clark A, Berger JT, Meert K, Newth CJ, Shanley T, Moler F, Carcillo J. Pediatric intensive care outcomes: development of new morbidities during pediatric critical care. Pediatr Crit Care Med. 2014;15:821-827. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 203] [Cited by in RCA: 252] [Article Influence: 22.9] [Reference Citation Analysis (0)] |
| 2. | Needham DM, Davidson J, Cohen H, Hopkins RO, Weinert C, Wunsch H, Zawistowski C, Bemis-Dougherty A, Berney SC, Bienvenu OJ. Improving long-term outcomes after discharge from intensive care unit: report from a stakeholders’ conference. Crit Care Med. 2012;40:502-509. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1316] [Cited by in RCA: 1724] [Article Influence: 132.6] [Reference Citation Analysis (34)] |
| 3. | van der Schaaf M, Beelen A, Dongelmans DA, Vroom MB, Nollet F. Functional status after intensive care: a challenge for rehabilitation professionals to improve outcome. J Rehabil Med. 2009;41:360-366. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 72] [Cited by in RCA: 82] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 4. | Rothenhäusler HB, Ehrentraut S, Stoll C, Schelling G, Kapfhammer HP. The relationship between cognitive performance and employment and health status in long-term survivors of the acute respiratory distress syndrome: results of an exploratory study. Gen Hosp Psychiatry. 2001;23:90-96. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 217] [Cited by in RCA: 204] [Article Influence: 8.5] [Reference Citation Analysis (0)] |
| 5. | Davydow DS, Gifford JM, Desai SV, Bienvenu OJ, Needham DM. Depression in general intensive care unit survivors: a systematic review. Intensive Care Med. 2009;35:796-809. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 306] [Cited by in RCA: 309] [Article Influence: 19.3] [Reference Citation Analysis (0)] |
| 6. | Polic B, Mestrovic J, Markic J, Mestrovic M, Capkun V, Utrobicic I, Jukica M, Radonic M. Long-term quality of life of patients treated in paediatric intensive care unit. Eur J Pediatr. 2013;172:85-90. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 41] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 7. | Als LC, Nadel S, Cooper M, Pierce CM, Sahakian BJ, Garralda ME. Neuropsychologic function three to six months following admission to the PICU with meningoencephalitis, sepsis, and other disorders: a prospective study of school-aged children. Crit Care Med. 2013;41:1094-1103. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 54] [Cited by in RCA: 80] [Article Influence: 6.7] [Reference Citation Analysis (0)] |
| 8. | Als LC, Picouto MD, Hau SM, Nadel S, Cooper M, Pierce CM, Kramer T, Garralda ME. Mental and physical well-being following admission to pediatric intensive care. Pediatr Crit Care Med. 2015;16:e141-e149. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 60] [Cited by in RCA: 70] [Article Influence: 7.0] [Reference Citation Analysis (0)] |
| 9. | Als LC, Tennant A, Nadel S, Cooper M, Pierce CM, Garralda ME. Persistence of Neuropsychological Deficits Following Pediatric Critical Illness. Crit Care Med. 2015;43:e312-e315. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 25] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 10. | Bronner MB, Knoester H, Bos AP, Last BF, Grootenhuis MA. Posttraumatic stress disorder (PTSD) in children after paediatric intensive care treatment compared to children who survived a major fire disaster. Child Adolesc Psychiatry Ment Health. 2008;2:9. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 50] [Cited by in RCA: 56] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 11. | Colville G, Kerry S, Pierce C. Children’s factual and delusional memories of intensive care. Am J Respir Crit Care Med. 2008;177:976-982. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 129] [Cited by in RCA: 142] [Article Influence: 8.4] [Reference Citation Analysis (0)] |
| 12. | Colville G, Pierce C. Patterns of post-traumatic stress symptoms in families after paediatric intensive care. Intensive Care Med. 2012;38:1523-1531. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 124] [Cited by in RCA: 114] [Article Influence: 8.8] [Reference Citation Analysis (0)] |
| 13. | Colville GA, Pierce CM. Children’s self-reported quality of life after intensive care treatment. Pediatr Crit Care Med. 2013;14:e85-e92. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 63] [Cited by in RCA: 76] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 14. | Dow BL, Kenardy JA, Le Brocque RM, Long DA. The diagnosis of posttraumatic stress disorder in school-aged children and adolescents following pediatric intensive care unit admission. J Child Adolesc Psychopharmacol. 2013;23:614-619. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 14] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 15. | Gemke RJ, Bonsel GJ, van Vught AJ. Long-term survival and state of health after paediatric intensive care. Arch Dis Child. 1995;73:196-201. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 86] [Cited by in RCA: 86] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 16. | Jayshree M, Singhi SC, Malhi P. Follow up of survival and quality of life in children after intensive care. Indian Pediatr. 2003;40:303-309. [PubMed] |
| 17. | Jones S, Rantell K, Stevens K, Colwell B, Ratcliffe JR, Holland P, Rowan K, Parry GJ. Outcome at 6 months after admission for pediatric intensive care: a report of a national study of pediatric intensive care units in the United kingdom. Pediatrics. 2006;118:2101-2108. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 81] [Cited by in RCA: 91] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 18. | Knoester H, Bronner MB, Bos AP, Grootenhuis MA. Quality of life in children three and nine months after discharge from a paediatric intensive care unit: a prospective cohort study. Health Qual Life Outcomes. 2008;6:21. [PubMed] [DOI] [Full Text] |
| 19. | Muranjan MN, Birajdar SB, Shah HR, Sundaraman P, Tullu MS. Psychological consequences in pediatric intensive care unit survivors: the neglected outcome. Indian Pediatr. 2008;45:99-103. [PubMed] |
| 20. | Namachivayam P, Shann F, Shekerdemian L, Taylor A, van Sloten I, Delzoppo C, Daffey C, Butt W. Three decades of pediatric intensive care: Who was admitted, what happened in intensive care, and what happened afterward. Pediatr Crit Care Med. 2010;11:549-555. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 258] [Cited by in RCA: 298] [Article Influence: 19.9] [Reference Citation Analysis (0)] |
| 21. | Namachivayam P, Taylor A, Montague T, Moran K, Barrie J, Delzoppo C, Butt W. Long-stay children in intensive care: long-term functional outcome and quality of life from a 20-yr institutional study. Pediatr Crit Care Med. 2012;13:520-528. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 79] [Cited by in RCA: 95] [Article Influence: 7.3] [Reference Citation Analysis (0)] |
| 22. | Rees G, Gledhill J, Garralda ME, Nadel S. Psychiatric outcome following paediatric intensive care unit (PICU) admission: a cohort study. Intensive Care Med. 2004;30:1607-1614. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 151] [Cited by in RCA: 161] [Article Influence: 7.7] [Reference Citation Analysis (0)] |
| 23. | Rennick JE, Johnston CC, Dougherty G, Platt R, Ritchie JA. Children’s psychological responses after critical illness and exposure to invasive technology. J Dev Behav Pediatr. 2002;23:133-144. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 141] [Cited by in RCA: 137] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 24. | Rennick JE, Morin I, Kim D, Johnston CC, Dougherty G, Platt R. Identifying children at high risk for psychological sequelae after pediatric intensive care unit hospitalization. Pediatr Crit Care Med. 2004;5:358-363. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 68] [Cited by in RCA: 71] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 25. | Taylor A, Butt W, Ciardulli M. The functional outcome and quality of life of children after admission to an intensive care unit. Intensive Care Med. 2003;29:795-800. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 77] [Cited by in RCA: 78] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 26. | Ambuehl J, Karrer A, Meer A, Riedel T, Schibler A. Quality of life of survivors of paediatric intensive care. Swiss Med Wkly. 2007;137:312-316. [PubMed] |
| 27. | Mestrovic J, Kardum G, Sustic A, Polic B, Mestrovic M, Markic J, Zanchi J. Neurodevelopmental disabilities and quality of life after intensive care treatment. J Paediatr Child Health. 2007;43:673-676. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 25] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 28. | Morrison AL, Gillis J, O’Connell AJ, Schell DN, Dossetor DR, Mellis C. Quality of life of survivors of pediatric intensive care. Pediatr Crit Care Med. 2002;3:1-5. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 63] [Cited by in RCA: 61] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 29. | Hashem MD, Nallagangula A, Nalamalapu S, Nunna K, Nausran U, Robinson KA, Dinglas VD, Needham DM, Eakin MN. Patient outcomes after critical illness: a systematic review of qualitative studies following hospital discharge. Crit Care. 2016;20:345. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 128] [Cited by in RCA: 123] [Article Influence: 13.7] [Reference Citation Analysis (0)] |
| 30. | Hopkins RO, Choong K, Zebuhr CA, Kudchadkar SR. Transforming PICU Culture to Facilitate Early Rehabilitation. J Pediatr Intensive Care. 2015;4:204-211. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 56] [Cited by in RCA: 58] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 31. | Iwashyna TJ, Cooke CR, Wunsch H, Kahn JM. Population burden of long-term survivorship after severe sepsis in older Americans. J Am Geriatr Soc. 2012;60:1070-1077. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 299] [Cited by in RCA: 365] [Article Influence: 28.1] [Reference Citation Analysis (0)] |
| 32. | Cheung AM, Tansey CM, Tomlinson G, Diaz-Granados N, Matté A, Barr A, Mehta S, Mazer CD, Guest CB, Stewart TE. Two-year outcomes, health care use, and costs of survivors of acute respiratory distress syndrome. Am J Respir Crit Care Med. 2006;174:538-544. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 375] [Cited by in RCA: 328] [Article Influence: 17.3] [Reference Citation Analysis (0)] |
| 33. | Wieczorek B, Ascenzi J, Kim Y, Lenker H, Potter C, Shata NJ, Mitchell L, Haut C, Berkowitz I, Pidcock F. PICU Up!: Impact of a Quality Improvement Intervention to Promote Early Mobilization in Critically Ill Children. Pediatr Crit Care Med. 2016;17:e559-e566. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 118] [Cited by in RCA: 145] [Article Influence: 16.1] [Reference Citation Analysis (0)] |
| 34. | Wieczorek B, Burke C, Al-Harbi A, Kudchadkar SR. Early mobilization in the pediatric intensive care unit: a systematic review. J Pediatr Intensive Care. 2015;2015:129-170. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 32] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 35. | Choong K, Foster G, Fraser DD, Hutchison JS, Joffe AR, Jouvet PA, Menon K, Pullenayegum E, Ward RE. Acute rehabilitation practices in critically ill children: a multicenter study. Pediatr Crit Care Med. 2014;15:e270-e279. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 36. | Curley MA, Watson RS. Sedation Strategy and Cognitive Outcome After Critical Illness in Early Childhood. gov [Internet]. Bethesda (MD): National Library of Medicine (US) 2000; [cited 2016 Oct 28] Available from: http://clinicaltrials.gov/show/NCT02225041. |
| 37. | Pandharipande P, Cotton BA, Shintani A, Thompson J, Pun BT, Morris JA, Dittus R, Ely EW. Prevalence and risk factors for development of delirium in surgical and trauma intensive care unit patients. J Trauma. 2008;65:34-41. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 320] [Cited by in RCA: 347] [Article Influence: 20.4] [Reference Citation Analysis (0)] |
| 38. | Traube C, Silver G, Reeder RW, Doyle H, Hegel E, Wolfe HA, Schneller C, Chung MG, Dervan LA, DiGennaro JL. Delirium in Critically Ill Children: An International Point Prevalence Study. Crit Care Med. 2017; Epub ahead of print. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 202] [Cited by in RCA: 197] [Article Influence: 24.6] [Reference Citation Analysis (0)] |
| 39. | Clinical practice guidelines for the sustained use of sedatives and analgesics in the critically ill adult. Am J Health Syst Pharm. 2002;59:150-178. [PubMed] |
| 40. | Creten C, Van Der Zwaan S, Blankespoor RJ, Leroy PL, Schieveld JN. Pediatric delirium in the pediatric intensive care unit: a systematic review and an update on key issues and research questions. Minerva Anestesiol. 2011;77:1099-1107. [PubMed] |
| 41. | Kudchadkar SR, Aljohani OA, Punjabi NM. Sleep of critically ill children in the pediatric intensive care unit: a systematic review. Sleep Med Rev. 2014;18:103-110. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 92] [Cited by in RCA: 100] [Article Influence: 9.1] [Reference Citation Analysis (0)] |
| 42. | Kudchadkar SR, Yaster M, Punjabi NM. Sedation, sleep promotion, and delirium screening practices in the care of mechanically ventilated children: a wake-up call for the pediatric critical care community*. Crit Care Med. 2014;42:1592-1600. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 152] [Cited by in RCA: 163] [Article Influence: 14.8] [Reference Citation Analysis (0)] |
| 43. | Smith HA, Boyd J, Fuchs DC, Melvin K, Berry P, Shintani A, Eden SK, Terrell MK, Boswell T, Wolfram K. Diagnosing delirium in critically ill children: Validity and reliability of the Pediatric Confusion Assessment Method for the Intensive Care Unit. Crit Care Med. 2011;39:150-157. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 205] [Cited by in RCA: 224] [Article Influence: 16.0] [Reference Citation Analysis (0)] |
| 44. | Smith HA, Gangopadhyay M, Goben CM, Jacobowski NL, Chestnut MH, Savage S, Rutherford MT, Denton D, Thompson JL, Chandrasekhar R. The Preschool Confusion Assessment Method for the ICU: Valid and Reliable Delirium Monitoring for Critically Ill Infants and Children. Crit Care Med. 2016;44:592-600. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 137] [Cited by in RCA: 159] [Article Influence: 17.7] [Reference Citation Analysis (0)] |
| 45. | Silver G, Traube C, Kearney J, Kelly D, Yoon MJ, Nash Moyal W, Gangopadhyay M, Shao H, Ward MJ. Detecting pediatric delirium: development of a rapid observational assessment tool. Intensive Care Med. 2012;38:1025-1031. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 93] [Cited by in RCA: 106] [Article Influence: 8.2] [Reference Citation Analysis (0)] |
| 46. | Flaigle MC, Ascenzi J, Kudchadkar SR. Identifying Barriers to Delirium Screening and Prevention in the Pediatric ICU: Evaluation of PICU Staff Knowledge. J Pediatr Nurs. 2015;31:81-84. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 50] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 47. | Parsons EC, Hough CL, Vitiello MV, Zatzick D, Davydow DS. Insomnia is associated with quality of life impairment in medical-surgical intensive care unit survivors. Heart Lung. 2015;44:89-94. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 26] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 48. | Parsons EC, Kross EK, Caldwell ES, Kapur VK, McCurry SM, Vitiello MV, Hough CL. Post-discharge insomnia symptoms are associated with quality of life impairment among survivors of acute lung injury. Sleep Med. 2012;13:1106-1109. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 24] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 49. | McKinley S, Fein M, Elliott RM, Elliot D. Sleep During And After Critical Illness And Psychological Health In Recovery. Australian Critical Care. 2013;26:83. [RCA] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 50. | Upton P, Lawford J, Eiser C. Parent-child agreement across child health-related quality of life instruments: a review of the literature. Qual Life Res. 2008;17:895-913. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 491] [Cited by in RCA: 532] [Article Influence: 31.3] [Reference Citation Analysis (0)] |
| 51. | Ely EW, Gautam S, Margolin R, Francis J, May L, Speroff T, Truman B, Dittus R, Bernard R, Inouye SK. The impact of delirium in the intensive care unit on hospital length of stay. Intensive Care Med. 2001;27:1892-1900. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 720] [Cited by in RCA: 728] [Article Influence: 30.3] [Reference Citation Analysis (0)] |
| 52. | Hopkins RO, Jackson JC. Long-term neurocognitive function after critical illness. Chest. 2006;130:869-878. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 228] [Cited by in RCA: 240] [Article Influence: 12.6] [Reference Citation Analysis (0)] |
| 53. | Jackson JC, Obremskey W, Bauer R, Greevy R, Cotton BA, Anderson V, Song Y, Ely EW. Long-term cognitive, emotional, and functional outcomes in trauma intensive care unit survivors without intracranial hemorrhage. J Trauma. 2007;62:80-88. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 60] [Cited by in RCA: 60] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 54. | Thomason JW, Shintani A, Peterson JF, Pun BT, Jackson JC, Ely EW. Intensive care unit delirium is an independent predictor of longer hospital stay: a prospective analysis of 261 non-ventilated patients. Crit Care. 2005;9:R375-R381. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 391] [Cited by in RCA: 386] [Article Influence: 19.3] [Reference Citation Analysis (0)] |
| 55. | Schieveld JN, Leroy PL, van Os J, Nicolai J, Vos GD, Leentjens AF. Pediatric delirium in critical illness: phenomenology, clinical correlates and treatment response in 40 cases in the pediatric intensive care unit. Intensive Care Med. 2007;33:1033-1040. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 140] [Cited by in RCA: 130] [Article Influence: 7.2] [Reference Citation Analysis (0)] |
| 56. | Janssen NJ, Tan EY, Staal M, Janssen EP, Leroy PL, Lousberg R, van Os J, Schieveld JN. On the utility of diagnostic instruments for pediatric delirium in critical illness: an evaluation of the Pediatric Anesthesia Emergence Delirium Scale, the Delirium Rating Scale 88, and the Delirium Rating Scale-Revised R-98. Intensive Care Med. 2011;37:1331-1337. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 67] [Cited by in RCA: 72] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 57. | Knowles RE, Tarrier N. Evaluation of the effect of prospective patient diaries on emotional well-being in intensive care unit survivors: a randomized controlled trial. Crit Care Med. 2009;37:184-191. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 144] [Cited by in RCA: 141] [Article Influence: 8.8] [Reference Citation Analysis (0)] |