Published online Nov 4, 2016. doi: 10.5492/wjccm.v5.i4.212
Peer-review started: May 17, 2016
First decision: July 5, 2016
Revised: July 20, 2016
Accepted: August 6, 2016
Article in press: August 8, 2016
Published online: November 4, 2016
Processing time: 170 Days and 10.8 Hours
To investigate the use of a multidisciplinary, longitudinal simulation to educate pediatric residents and nurses on management of pediatric diabetic ketoacidosis.
A multidisciplinary, multiple step simulation course was developed by faculty and staff using a modified Delphi method from the Pediatric Simulation Center and pediatric endocrinology department. Effectiveness of the simulation for the residents was measured with a pre- and post-test and a reference group not exposed to simulation. A follow up post-test was completed 3-6 mo after the simulation. Nurses completed a survey regarding the education activity.
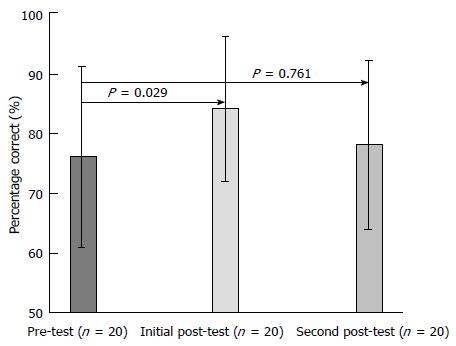
Pediatric and medicine-pediatric residents (n = 20) and pediatric nurses (n = 25) completed the simulation course. Graduating residents (n = 16) were used as reference group. Pretest results were similar in the control and intervention group (74% ± 10% vs 76% ± 15%, P = 0.658). After completing the intervention, participants improved in the immediate post-test in comparison to themselves and the control group (84% ± 12% post study; P < 0.05). The 3-6 mo follow up post-test results demonstrated knowledge decay when compared to their immediate post-test results (78% ± 14%, P = 0.761). Residents and nurses felt the interdisciplinary and longitudinal nature of the simulation helped with learning.
Results suggest a multidisciplinary, longitudinal simulation improves immediate post-intervention knowledge but important knowledge decay occurs, future studies are needed to determine ways to decrease this decay.
Core tip: Our paper describes how an interprofessional simulation improved the understanding of the medically complex disorder of pediatric diabetic ketoacidosis (DKA). This was shown in our data collection both by improvements in test scores from pre-simulation to post-simulation, as well as when compared to the control group. Few studies have looked at simulation as an educational tool for DKA. Our simulation course identified gaps in knowledge, communication, and patient care. Therefore, demonstrating that interprofessional simulation is a useful tool to teach a team based approach and focus on communication between nursing staff and physicians when taking care of critically ill children.
- Citation: Larson-Williams LM, Youngblood AQ, Peterson DT, Zinkan JL, White ML, Abdul-Latif H, Matalka L, Epps SN, Tofil NM. Interprofessional, multiple step simulation course improves pediatric resident and nursing staff management of pediatric patients with diabetic ketoacidosis. World J Crit Care Med 2016; 5(4): 212-218
- URL: https://www.wjgnet.com/2220-3141/full/v5/i4/212.htm
- DOI: https://dx.doi.org/10.5492/wjccm.v5.i4.212
Diabetic ketoacidosis (DKA) is a life threatening condition that results from a lack of insulin and one of the more common causes of pediatric intensive care unit (ICU) admissions[1-4]. Without insulin, counter-regulatory hormones increase leading to an accelerated, potentially fatal, catabolic state[5-7]. If treatment including insulin, electrolyte replacement, and fluids are administered appropriately, the catabolic process can be reversed[6-8]. DKA occurs in approximately 29% of patients with new onset type 1 diabetes mellitus and in 10% of patients with new onset type 2 diabetes mellitus[4,6]. Mortality related to DKA is less than 5% with 90% due to cerebral edema[1,3,4,6,7]. Other complications that increase risk for morbidity and mortality include electrolyte abnormalities, acute renal failure and acute pancreatitis[1,5,7]. In order to decrease these, early recognition and appropriate ICU management is required[4,6-9].
Resident education of DKA largely consists of lectures, reading articles, and informal instruction from pediatric faculty and senior residents. Nursing education is less formal, often through self-directed learning, computer-based training and informal bedside teaching. Simulation based learning is an effective tool to supplement traditional teaching methods due to it providing a safe learning environment learners, incorporating aspects of adult learning theory and promoting multidisciplinary learning[10-15].
In an effort to standardize DKA education and focus on interprofessional teaching, we created a multistep, longitudinal simulation course. The scenario begins at diagnosis of DKA, proceeds through a standardized treatment course including management of fluids, insulin, electrolyte replacement, monitoring for complications, and finishes when the patient transitions to subcutaneous insulin. Our primary hypothesis is that pediatric residents exposed to this multidisciplinary, longitudinal simulation improve their DKA knowledge compared to our reference group, graduating senior residents not exposed to the intervention. Our secondary hypothesis is that by conducting the intervention in an inter-disciplinary fashion, both nurses and physicians will better understand each other’s roles in the care of patients with DKA.
Pediatric and combined medicine/pediatric residents participated in the simulation course as part of their scheduled endocrinology rotation and were invited during their elective rotations if they were not already scheduled for endocrinology. Graduating third year pediatric residents and fourth year medicine/pediatric residents prior to initiation of this course were the reference group. Pediatric nurses from the intensive care unit and step down unit participated with the residents. Sessions were conducted approximately once a month from September 2013 through March 2015.
The research was approved by Institutional Review Board at the University of Alabama in Birmingham. A scripted scenario was developed by simulation and endocrinology experts by a modified Delphi process to provide a uniform educational experience for our participants. An accelerated time sequence was used. The scenario was a patient with new onset diabetes in DKA. Once the diagnosis was confirmed, a plan of care was constructed with the nurses to include patient monitoring, administration of medications, correction of electrolyte imbalances, and schedule for lab draws. Participants were required to manage electrolyte abnormalities, administer appropriate fluid management, and monitor glycemic control while on an insulin drip. All participants were confronted with development of cerebral edema during the care of their patient. The simulated patient’s response was based on the provider’s reactions to changes in labs and clinical course. Actions performed were documented using a structured checklist created by endocrinologists. Once the patient met appropriate criteria, the resident provided instruction to the nurses regarding transition to subcutaneous insulin. Following the case, there was a participant-centered debriefing led by a content expert in pediatric endocrinology and a simulation nurse educator. Key points in the diagnosis and management of DKA were covered.
The effectiveness of the simulation for the residents was measured based on a pre- and post-test created by endocrinology and educational experts. Participants completed a pre-test prior to the simulation (Table 1). The same post-test was given immediately after completion of the simulation and a second retention post-test was administered three to six months after the course. The reference group completed the same test in their last month of residency. The nursing staff completed a survey following the conclusion of the scenario and debriefing session.
| Demographic information | |
| 1 What year in residency are you? | |
| PGY1 PGY2 PGY3 PGY4 | |
| 2 Circle the residency program you are currently enrolled in. | |
| Pediatrics Med-Peds Emergency medicine | |
| 3 Have you done an endocrine rotation during your residency? | |
| Yes No | |
| (1) If yes, what year in your training did you do this rotation? | |
| PGY1 PGY2 PGY3 PGY4 | |
| 4 Do you personally have type 1 diabetes? | |
| Yes No | |
| (1) If yes, have you ever been treated for DKA? | |
| Yes No | |
| 5 Have you ever actively cared for a family member or close friend with diabetes? | |
| Yes No | |
| 6 Have you ever cared for a patient with DKA during your training? | |
| Yes No | |
| (1) If yes, what rotations did you take care of these patients? Please list the rotations | |
| (2) Approximately how many patients have you cared with DKA | |
| 0-5 patients 5-10 patients 10-20 patients > 20 patients | |
| Test questions (1correct answers, some questions have more than one answer) 1 Match the best words that define diabetic ketoacidosis (DKA) with the appropriate lab value | |
| A Dehydration | (1) BS > 200 mg/dL1 |
| B Ketosis1 | (2) Bicarb < 19, Ph < 7.35 |
| C Acidosis1 | (3) Urine or serum ketones1 |
| D Polydipsia | (4) Bicarb < 15, pH < 7.31 |
| E Vomiting | (5) Spec grav > 1.030 |
| F Hyperglycemia1 | (6) Glycosuria |
| 2 Which of the following signs/symptoms best describes a patient with DKA? | |
| A Vomiting/diarrhea, hypokalemia | |
| B Fever, leukocytosis | |
| C Rapid deep breathing, altered mental status, vomiting, polyuria1 | |
| D Polyuria, polydipsia, nocturia | |
| 3 Which of the following is not a known complication that can occur during management of DKA? | |
| A Cerebral Edema | |
| B Hypokalemia | |
| C Pancreatitis | |
| D Hematuria1 | |
| E Rhabdomyolysis | |
| F Hypercholermic metabolic acidosis | |
| G Mucormycosis | |
| 4 Which of the following explanations best explains the best initial therapy for DKA after initial fluid resuscitation? | |
| A Continuous IVF with 1/2NS or NS to replace fluid losses over 48 h, insulin gtt at 0.1 units/kg per hour1 | |
| B Continuous IVF with 1/2NS or NS to replace fluid losses over 48 h, insulin gtt at 0.05 units/kg per hour | |
| C Maintenance IVF with 1/2NS or NS, insulin gtt at 0.1 units/kg per hour | |
| D Maintenance IVF with 1/2NS or NS, IV insulin bolus followed by insulin gtt at 0.1 units/kg per hour | |
| E Twice maintenance IVF with 1/2NS or NS, insulin gtt at 0.1 units/kg per hour | |
| F Sodium bicarbonate administration, IV insulin bolus IV followed by insulin gtt at 0.1 units/kg per hour, maintenance fluids with 1/2NS or NS | |
| 5 What labs and how often should labs be drawn on a patient in DKA, including D-sticks? | |
| A D-sticks Q1H, serum electrolytes Q4H | |
| B D-sticks Q15 minutes, serum electrolytes Q2H | |
| (1) D-sticks Q1H, serum electrolytes Q2H initially then Q4H once steady improvement is noted1 | |
| (2) D-sticks Q1H, serum electrolytes Q2H twice, then Q6H once steady improvement is noted | |
| 6 When should the patient’s neurological status be assessed? | |
| A On admission, every hour during treatment, as needed for acute changes1 | |
| B Every hour during treatment | |
| C On admission, every hour for the first four hours of treatment and then as needed for acute changes | |
| D On admission and as needed for acute changes | |
| 7 When should dextrose be added to your treatment of DKA? | |
| A When blood sugar drops by more than 100 mg/dL in an hour | |
| B When blood sugar is less than or equal to 250 mg/dL | |
| C When blood sugar drops by more than 75 mg/dL in an hour | |
| D When blood sugar is less than or equal to 300 mg/dL | |
| E A and B | |
| F A and D1 | |
| G C and D | |
| H B and C | |
| 8 When should potassium not be added to the IVF? | |
| A When potassium is < 5.5 | |
| B When patient has urinated | |
| C When no EKG abnormalities are noted on cardiac monitor | |
| D When patient has evidence of acute renal failure on lab evaluation1 | |
| 9 Identify three signs/symptoms of cerebral edema | |
| A Headache1 | |
| B Altered mental status1 | |
| C Hyperactivity | |
| D Hypotension | |
| E Bradycardia1 | |
| F Tachycardia | |
| 10 Over what period of time should you correct a patient in DKA’s dehydration? | |
| A Immediately | |
| B Over 12 h | |
| C Over 24 h | |
| D Over 48 h1 | |
| E Over 72 h | |
| 11 When is the patient at the greatest risk for developing cerebral edema? | |
| A On admission/before treatment | |
| B At initiation of treatment | |
| C Several hours into treatment1 | |
| D At the time of transition | |
| 12 Describe the process of how to transition a patient off an insulin drip onto SQ insulin (Do not need to describe calculating doses of insulin. Just the basic process) | |
| A Order food tray, when food arrives, administer long acting insulin and mealtime SQ insulin, allow patient to eat, approximately one hour later discontinue the insulin gtt, and remove dextrose from fluids1 | |
| B Discontinue insulin gtt, administer long acting insulin when arrives | |
| C Administer long acting SQ insulin, one hour later allow patient to eat and administer mealtime insulin, discontinue insulin gtt, remove dextrose from fluids | |
| D Order food tray, when food arrives, allow patient to eat, administer long acting insulin and mealtime SQ insulin, approximately one hour later discontinue the insulin gtt | |
| 13 When should the insulin drip be stopped during the treatment of DKA? | |
| A When the blood sugar drops by > 200 mg/dL | |
| B During transport | |
| C When the bicarb is 19 | |
| D When long acting SQ insulin has been given in consultation with endocrine1 | |
| 14 Which of the following therapies is appropriate treatment of DKA? | |
| A Bicarb administration | |
| B Several hour delay or interruption in receiving insulin gtt | |
| C Rapid drop in glucose during treatment | |
| D Multiple fluid boluses at the beginning of treatment unless patient is hemodynamically unstable | |
| E Starting the insulin drip one hour after IV fluid hydration has been initiated1 | |
| 15 On a scale from 1 to 5, how beneficial did you find the simulation exercise? | |
| 1 2 3 4 5 | |
| Least helpful Most helpful | |
| 16 How would you improve this simulation exercise? (add this to the immediate post-test and not the one done at 3-6 mo) | |
Statistical analysis was performed using SPSS software (Chicago, IL). A χ2 test evaluated for categorical differences between the intervention and reference groups of residents. Paired and unpaired t tests compared test scores both within the intervention group and reference group respectively. A P value of < 0.05 was considered statistically significant. Feedback comments were evaluated for common themes.
Forty-five subjects participated including twenty residents and twenty-five nurses. Seventeen monthly sessions were conducted. The reference group was 72% (16/22) of senior residents in their last month of training (June 2013). No personal history of diabetes mellitus type 1 was reported. Only one participant cared for a family member with diabetes. Exposure to these patients prior to the simulation was not significantly different amongst the two populations. Table 2 shows the demographics.
| Category | Control Group (n = 16) | Intervention Group (n = 20) | P value |
| Residency training year | 0.003 | ||
| PGY 2 | 0 (0) | 8 (40) | |
| PGY 3/4 | 16 (100) | 12 (60) | |
| Type of residency | 0.192 | ||
| Pediatric | 13 (81) | 19 (95) | |
| Medicine-pediatric | 3 (19) | 1 (5) | |
| Treated DKA in residency | 16 (100) | 20 (100) | 0.192 |
| Endocrine rotation only | 2 (13) | 4 (20) | |
| ICU rotation only | 5 (31) | 1 (5) | |
| Both endocrine and ICU rotation | 6 (37) | 9 (45) | |
| Other (ED, night float) | 3 (19) | 6 (30) | |
| Estimated number of patients treated with DKA | 0.825 | ||
| 1-10 | 2 (13) | 4 (20) | |
| 10-20 | 8 (50) | 9 (45) | |
| > 20 | 6 (37) | 7 (35) |
There was no statistical difference between the reference group’s knowledge assessment test and the intervention group’s pre-test, 75% ± 10% vs 77% ± 15%, P = 0.66. Figure 1 shows the assessment scores of the intervention group at the three time periods tests; pre-test, initial post-test and 4-6 mo follow-up test. There was a significant improvement after the intervention but knowledge decay at the follow-up assessment. In addition, the intervention group had significant improvement in their test scores when compared to the reference group after the intervention (75% ± 10% vs 84% ± 12%, P = 0.02). While overall score did not improve between the pre-test and the second post-test in the simulation group, specific questions involving fluid management and cerebral edema noted sustained improvement. This improvement is also noted when compared to the reference group.
No insulin or bicarbonate boluses were administered during any of the simulation activities. Only four participants administered more than one fluid bolus. All participants recognized the possibility of cerebral edema and 80% (16/20) of residents communicated this to the parent. Only half completed a neurological exam despite the concern for cerebral edema.
Ninety-two percent (23/25) of nurses were from the step down ICU and 8% (2/25) were from the pediatric ICU. The majority were new critical care nurses with 80% (20/25) having < 5 years of experience. Sixty-four percent of (16/25) cared for < 5 patients per month with DKA. All nursing participants found the experience positive and provided a better understanding of the diagnosis and management of DKA. Ninety-six percent (24/25) of believed the simulation to be more beneficial than previous education on DKA. Residents echoed this positive response with all identifying the simulation as beneficial especially the interdisciplinary nature of the course.
Qualitative analysis found the following overall learning themes: (1) activity “felt like real life” by having the residents and nurses’ work together; (2) longitudinal progression of events allowed learners to see a patient in different stages of treatment; (3) debriefing discussions regarding pathophysiology and linking it to treatment was helpful; and (4) early recognition of cerebral edema and management. Suggestions for improvement included: (1) utilize electronic order entry system; (2) provide written handouts; and (3) participate in the simulation earlier in training.
A multidisciplinary, longitudinal simulation can improve understanding of a medically complex disorder such as DKA. This is demonstrated by improvements in test scores from pre-simulation to initial post-simulation as well as when compared to the reference group. Certain aspects of DKA management including fluid administration and cerebral edema recognition showed sustained improvement. In an environment where patient exposure is often fragmented due to nursing shift schedules and duty hour restrictions, the longitudinal nature of this course allows participants to see a patient from initial diagnosis until transition to subcutaneous insulin. This aspect along with the multidisciplinary approach makes it unique amongst previously described studies[12-19].
Volkova et al[14] designed a multidisciplinary approach for implementation of DKA guidelines. Internal medicine residents were educated via computer based testing/supportive reading materials and separate nursing education was conducted through lectures/reading materials. Documentation of compliance to guidelines and knowledge assessments were performed on the residents. Improvement in both areas was noted. Our studied allowed for simultaneous learning analogous to patient care which added benefit in that healthcare professionals learn firsthand the complexities of effective communication when taking care of critically ill patients. Fung et al[15] conducted a systemic review regarding the use of interdisciplinary and interprofessional simulation as an education tool for crisis resource management. Specific gains including improvement in team communication and subsequently overall patient care were noted in three of the studies reviewed. Interprofessional simulation also provides a forum for learners to practice leadership roles in emergency situations. Brown et al[16] in 2014 demonstrated that a multidisciplinary simulation could be used to improve radiation oncology resident training for medical emergencies.
Few studies have looked specifically at simulation as a DKA educational tool. Schneider Sarver et al[17] developed a three part simulation involving management of an adolescent patient with mild, moderate, and severe DKA for nursing students which showed knowledge improvement. Lee Chin et al[18] compared high-fidelity simulation vs case-based learning modules for DKA and thyroid storm for senior pharmacy students. Both groups demonstrated knowledge improvements but the simulation group had higher post-test scores. Problem-based DKA simulation case series for medical students supplementing their basic science material or computer-based simulations as part of an outpatient endocrine rotation showed knowledge gains compared to traditional learning methods[19,20].
Our simulation course identified knowledge, communication and patient care gaps. For example, only half of residents completed a thorough neurological exam despite clinical evidence concerning for cerebral edema. When asked about this during debriefing, residents identified wanting to “rush” through the exam and not identifying a need to perform a more thorough exam. All nursing participants notified the resident physicians regarding the patient’s clinical changes consistent with cerebral edema but only a few clearly communicated their concern was cerebral edema. Another example of communication breakdown was timing of insulin drip initiation in regards to fluid boluses and initiation of intravenous fluids. Sometimes fluid boluses and insulin drips were administered around the same time without clarification asked for by the nursing staff or provided by the prescribers. Per 2014 International Society for Pediatric and Adolescent Diabetes guidelines, delaying insulin drip initiation 1-2 h after beginning fluid resuscitation therapy can help decrease the risk of cerebral edema[4].
Knowledge decay over time has been reported as a concern in medical education literature[21,22]. In adult advanced life support training a recent review demonstrated that knowledge and skill decay can occur as quickly as six weeks after initial training with more significant decay noted at 6-12 mo which can be attenuated if subjects have more clinical topic exposure[21]. Doumouras et al[22] specifically discussed the use of simulation and retention of knowledge and skills for crisis resource management training and showed retention of skills, particularly team based skills, was maintained if a repeated intervention was utilized. These findings may help explain the lack of sustained knowledge improvement in our population. The exposure of our cohort to DKA patients between the conclusion of the simulation and the second post-test was not documented. Residents with more exposure to these patients to reinforce skills learned during the simulation may have performed better on the second post-test. Along those same lines, no structured reinforcement was offered between the conclusion of the simulation and the second post-test and this may have improved retention scores.
While our paper looks at the improvement of pediatric DKA management through simulation, we saw different methods utilized in each scenario. This difference in management of DKA in the pediatric population has been seen in other areas as well. Skitch and Valani[23] looked at the protocols of thirteen pediatric tertiary centers in Canada and reported many differences in the management of DKA. In comparison, a survey in pediatric centers in the Italian Society for Pediatric Diabetology and Endocrinology recognized significant differences in DKA management among their centers as well[24]. Both articles reference the need for evidence-based guidelines to be utilized across the board for best practice[23,24]. Although, DKA is managed through different methods, preventative care for these patients is of utmost importance. Crossen et al[25] concluded that signs of impending DKA were seen in children with type I diabetes who had recent emergency department visits and had infrequent subspecialty primary care visits. Chafe et al[26] utilized a focus study group of patients and families to identify ways to reduce episodes of DKA in the youth population. This project identified factors that put the youth at increased risks and recognized areas to improve those odds.
Limitations of this study included the relatively small number of participants especially in regards to numbers in the individual groups; reference, intervention and nurses. Recruitment of participants was limited due to the complex scheduling issues that are faced by both nursing staff and resident physicians. Other limitations include the reliance on participants to accept the realism in simulation activities. We chose to use a high-fidelity mannequin for the simulation to help reduce these issues. Each debriefing was designed to cover certain basic topics with all participants however may not have been identical. Finally, we did not assess if this intervention helped in actual care of patients with DKA.
Our study demonstrates that an interprofessional, longitudinal simulation improves short term understanding regarding the management of pediatric DKA. Subjectively, nurses found the interprofessional simulation improved their knowledge as well. It may be a useful tool to teach a team based approach and focus on communication between nursing staff and physicians when taking care of critically ill children. Unfortunately knowledge gains were not sustained at the 3-6 mo follow up sessions. Further studies are needed to investigate the impact of this simulation on patient care, specific changes in healthcare provider practices, and methods to reduce knowledge decay.
Diabetic ketoacidosis (DKA) is the most common pediatric endocrine emergency and understanding its management is important for the healthcare team. Experience and training in DKA management is variable and often separated by healthcare disciplines. Simulation may be an important tool to help standardize DKA training.
Inter-disciplinary training with simulation is becoming an important way to train medical providers.
This is the first article to evaluate the role of inter-disciplinary simulation training in the management of pediatric DKA. Important knowledge gains were seen after the intervention but were not sustained on 3 mo follow-up.
Simulation is important tool in medical education and its role continues to expand.
Nice research dealing with a public health problem.
Manuscript source: Invited manuscript
Specialty type: Critical care medicine
Country of origin: United States
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): D
Grade E (Poor): 0
P- Reviewer: Sergi CM, Tarantino G, Wang R S- Editor: Ji FF L- Editor: A E- Editor: Wu HL
| 1. | Kitabchi AE, Umpierrez GE, Murphy MB, Barrett EJ, Kreisberg RA, Malone JI, Wall BM. Hyperglycemic crises in diabetes. Diabetes Care. 2004;27 Suppl 1:S94-102. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 112] [Cited by in RCA: 113] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 2. | Klein M, Sathasivam A, Novoa Y, Rapaport R. Recent consensus statements in pediatric endocrinology: a selective review. Endocrinol Metab Clin North Am. 2009;38:811-825. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 3. | Rewers A. Current controversies in treatment and prevention of diabetic ketoacidosis. Adv Pediatr. 2010;57:247-267. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 4. | Wolfsdorf JI, Allgrove J, Craig ME, Edge J, Glaser N, Jain V, Lee WW, Mungai LN, Rosenbloom AL, Sperling MA. ISPAD Clinical Practice Consensus Guidelines 2014. Diabetic ketoacidosis and hyperglycemic hyperosmolar state. Pediatr Diabetes. 2014;15 Suppl 20:154-179. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 221] [Cited by in RCA: 223] [Article Influence: 20.3] [Reference Citation Analysis (0)] |
| 5. | Rosenbloom AL. The management of diabetic ketoacidosis in children. Diabetes Ther. 2010;1:103-120. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 57] [Cited by in RCA: 59] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 6. | Wolfsdorf J, Craig ME, Daneman D, Dunger D, Edge J, Lee W, Rosenbloom A, Sperling M, Hanas R. Diabetic ketoacidosis in children and adolescents with diabetes. Pediatr Diabetes. 2009;10 Suppl 12:118-133. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 179] [Cited by in RCA: 185] [Article Influence: 11.6] [Reference Citation Analysis (0)] |
| 7. | Sherry NA, Levitsky LL. Management of diabetic ketoacidosis in children and adolescents. Paediatr Drugs. 2008;10:209-215. [PubMed] |
| 8. | Hsia DS, Tarai SG, Alimi A, Coss-Bu JA, Haymond MW. Fluid management in pediatric patients with DKA and rates of suspected clinical cerebral edema. Pediatr Diabetes. 2015;16:338-344. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 24] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 9. | Watts W, Edge JA. How can cerebral edema during treatment of diabetic ketoacidosis be avoided? Pediatr Diabetes. 2014;15:271-276. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 23] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 10. | Grant DJ, Marriage SC. Training using medical simulation. Arch Dis Child. 2012;97:255-259. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 21] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 11. | Weinberg ER, Auerbach MA, Shah NB. The use of simulation for pediatric training and assessment. Curr Opin Pediatr. 2009;21:282-287. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 107] [Cited by in RCA: 103] [Article Influence: 6.4] [Reference Citation Analysis (0)] |
| 12. | Okuda Y, Bryson EO, DeMaria S, Jacobson L, Quinones J, Shen B, Levine AI. The utility of simulation in medical education: what is the evidence? Mt Sinai J Med. 2009;76:330-343. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 583] [Cited by in RCA: 579] [Article Influence: 38.6] [Reference Citation Analysis (0)] |
| 13. | Tofil NM, Morris JL, Peterson DT, Watts P, Epps C, Harrington KF, Leon K, Pierce C, White ML. Interprofessional simulation training improves knowledge and teamwork in nursing and medical students during internal medicine clerkship. J Hosp Med. 2014;9:189-192. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 63] [Cited by in RCA: 59] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 14. | Volkova NB, Fletcher CC, Tevendale RW, Munyaradzi SM, Elliot S, Peterson MW. Impact of a multidisciplinary approach to guideline implementation in diabetic ketoacidosis. Am J Med Qual. 2008;23:47-55. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 11] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 15. | Fung L, Boet S, Bould MD, Qosa H, Perrier L, Tricco A, Tavares W, Reeves S. Impact of crisis resource management simulation-based training for interprofessional and interdisciplinary teams: A systematic review. J Interprof Care. 2015;29:433-444. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 113] [Cited by in RCA: 117] [Article Influence: 11.7] [Reference Citation Analysis (0)] |
| 16. | Brown LC, Laack TA, Ma DJ, Olivier KR, Laack NN. Multidisciplinary medical simulation: a novel educational approach to preparing radiation oncology residents for oncologic emergent on-call treatments. Int J Radiat Oncol Biol Phys. 2014;90:705-706. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 9] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 17. | Schneider Sarver PA, Senczakowicz EA, Slovensky BM. Development of simulation scenarios for an adolescent patient with diabetic ketoacidosis. J Nurs Educ. 2010;49:578-586. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 8] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 18. | Lee Chin K, Ling Yap Y, Leng Lee W, Chang Soh Y. Comparing effectiveness of high-fidelity human patient simulation vs case-based learning in pharmacy education. Am J Pharm Educ. 2014;78:153. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 25] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 19. | Nandate K, Abola R, Murray WB, Whitfield C, Lang C, Sinz E. Simulation of diabetic ketoacidosis for cellular and molecular basics of medical practice. Simul Healthc. 2009;4:232-236. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 20. | Wong RW, Lochnan HA. A web-based simulation of a longitudinal clinic used in a 4-week ambulatory rotation: a cohort study. BMC Med Educ. 2009;9:8. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 21. | Yang CW, Yen ZS, McGowan JE, Chen HC, Chiang WC, Mancini ME, Soar J, Lai MS, Ma MH. A systematic review of retention of adult advanced life support knowledge and skills in healthcare providers. Resuscitation. 2012;83:1055-1060. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 235] [Cited by in RCA: 196] [Article Influence: 15.1] [Reference Citation Analysis (0)] |
| 22. | Doumouras AG, Keshet I, Nathens AB, Ahmed N, Hicks CM. A crisis of faith? A review of simulation in teaching team-based, crisis management skills to surgical trainees. J Surg Educ. 2012;69:274-281. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 50] [Cited by in RCA: 46] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 23. | Skitch SA, Valani R. Treatment of Pediatric Diabetic Ketoacidosis in Canada: A Review of Treatment Protocols from Canadian Pediatric Emergency Departments. CJEM. 2015;17:656-661. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 24. | Zucchini S, Scaramuzza AE, Bonfanti R, Buono P, Cardella F, Cauvin V, Cherubini V, Chiari G, d’Annunzio G, Frongia AP. A Multicenter Retrospective Survey regarding Diabetic Ketoacidosis Management in Italian Children with Type 1 Diabetes. J Diabetes Res. 2016;2016:5719470. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 18] [Cited by in RCA: 22] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 25. | Crossen SS, Wilson DM, Saynina O, Sanders LM. Outpatient Care Preceding Hospitalization for Diabetic Ketoacidosis. Pediatrics. 2016;137:pii: e20153497. [PubMed] |
| 26. | Chafe R, Albrechtsons D, Hagerty D, Newhook LA. Reducing episodes of diabetic ketoacidosis within a youth population: a focus group study with patients and families. BMC Res Notes. 2015;8:395. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.4] [Reference Citation Analysis (0)] |