Published online Aug 4, 2015. doi: 10.5492/wjccm.v4.i3.179
Peer-review started: November 26, 2014
First decision: December 12, 2014
Revised: January 10, 2015
Accepted: April 8, 2015
Article in press: April 9 2015
Published online: August 4, 2015
Processing time: 264 Days and 18 Hours
Cystic fibrosis (CF) is a multisystem disorder with significantly shortened life expectancy. The major cause of mortality and morbidity is lung disease with increasing pulmonary exacerbations and decline in lung function predicting significantly poorer outcomes. The pathogenesis of lung disease in CF is characterised in part by decreased airway surface liquid volume and subsequent failure of normal mucociliary clearance. This leads to accumulation of viscous mucus in the CF airway, providing an ideal environment for bacterial pathogens to grow and colonise, propagating airway inflammation in CF. The use of nebulised hypertonic saline (HTS) treatments has been shown to improve mucus clearance in CF and impact positively upon exacerbations, quality of life, and lung function. Several mechanisms of HTS likely improve outcome, resulting in clinically relevant enhancement in disease parameters related to increase in mucociliary clearance. There is increasing evidence to suggest that HTS is also beneficial through its anti-inflammatory properties and its ability to reduce bacterial activity and biofilm formation. This review will first describe the use of HTS in treatment of CF focusing on its efficacy and tolerability. The emphasis will then change to the potential benefits of aerosolized HTS for the attenuation of receptor mediated neutrophil functions, including down-regulation of oxidative burst activity, adhesion molecule expression, and the suppression of neutrophil degranulation of proteolytic enzymes.
Core tip: The pathogenesis of lung disease in cystic fibrosis (CF) is characterised by decreased airway surface liquid volume and subsequent failure of normal mucociliary clearance. Therapies acting against airway mucus in CF include aerosolized hypertonic saline (HTS). It has been shown that HTS aids mucociliary clearance by restoring the liquid layer lining the airways. However, recent studies are beginning to broaden our view on the beneficial effects of HTS, which now extend to include anti-inflammatory properties. This review aims to discuss the therapeutic benefits of HTS and to identify the potential benefits of aerosolized HTS for attenuation of neutrophil function.
- Citation: Reeves EP, McCarthy C, McElvaney OJ, Vijayan MSN, White MM, Dunlea DM, Pohl K, Lacey N, McElvaney NG. Inhaled hypertonic saline for cystic fibrosis: Reviewing the potential evidence for modulation of neutrophil signalling and function. World J Crit Care Med 2015; 4(3): 179-191
- URL: https://www.wjgnet.com/2220-3141/full/v4/i3/179.htm
- DOI: https://dx.doi.org/10.5492/wjccm.v4.i3.179
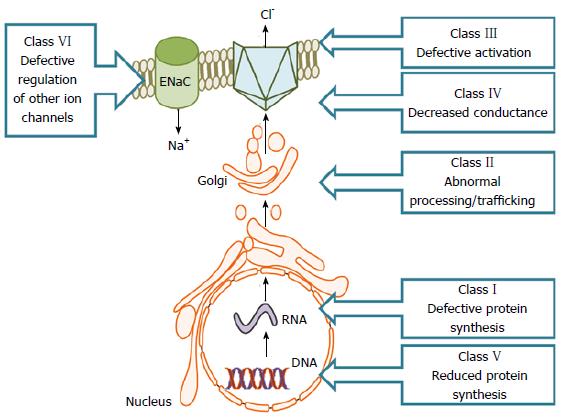
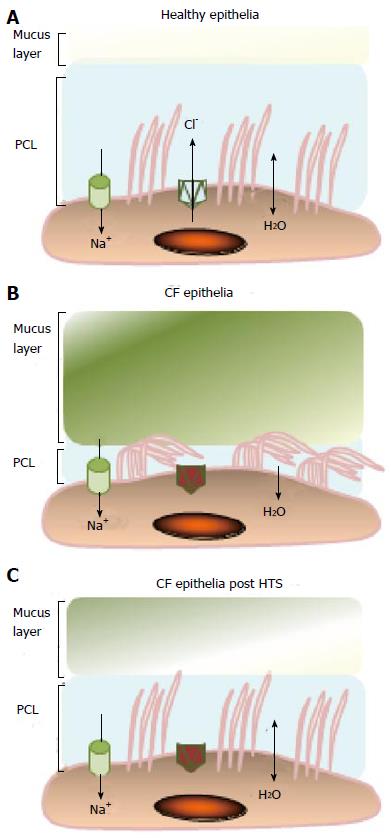
Cystic fibrosis (CF) is a complex genetic disease leading to increased risk of chronic lung disease resulting in terminal respiratory failure[1,2]. CF is an autosomal recessive disorder caused by mutations in the CF transmembrane conductance regulator (CFTR) chloride channel. Over 1900 CFTR mutations leading to defective chloride transport have been identified to date[3] and result in misfolding of the CFTR protein. Reported mutations can be categorised into different classes depending on whether the mutation alters CFTR processing (Classes I, II and V) or results in dysregulated chloride secretion (Classes III, IV, VI) (Figure 1). The most common mutation is deletion of phenylalanine at position 508 (∆F508) which occurs in approximately 70% of patients with CF, and 90% of CF suffers carry one copy[4]. Defects in CFTR protein function not only impact upon cAMP-dependent chloride secretion but also result in increased epithelial sodium channel (ENaC)-mediated ion absorption in the superficial airway epithelium[5,6]. CFTR absence or malfunction causes increased water re-absorption across airway epithelial cells leading to dehydration of the airway surface liquid (ASL) layer, persistent mucus hypersecretion and airflow obstruction[7]. Dehydration of the ASL layer and mucus accumulation has been implicated in exacerbated airway inflammation[8] and decline in lung function predicts significantly poorer outcomes[9]. Therapeutic interventions to improve mucus clearance is a necessary treatment in CF[10]. Hypertonic saline (HTS) at concentrations of 3% or higher is widely used to improve mucociliary clearance, as this increases the tonicity of the ASL creating an osmotic gradient drawing water into the airway hence improving ASL and facilitating removal of airway secretions (Figure 2). Furthermore, HTS improves lung function and quality of life and significantly decreases the frequency of exacerbations[11,12] and is generally well tolerated.
When considering the different immune cells present in the CF lung it has been documented that neutrophils account for approximately 60%-70% of immune cells in CF airway samples[13]. Key studies have demonstrated that infiltration of neutrophils into the airways occurs early in the course of CF lung disease and that neutrophil-released granule proteins, particularly neutrophil elastase (NE), play a crucial pathological role[14,15]. The expression of functional CFTR on the plasma membrane of neutrophils has been the topic of great debate[16-19] with studies specifying intrinsic abnormalities due to a lack of CFTR function[20,21]. Reports on reprogrammed cell activity secondary to chronic bacterial infection and inflammation have also been documented[22]. Moreover, persistent mTOR and CREB pathway activation in CF airway neutrophils[23] and augmented cell surface nutrient transporter expression are consistent with metabolic adaptation[24].
Regardless of the cause of impaired neutrophil activity however, the fundamental consequence is neutrophil mediated tissue proteolysis. Excessive neutrophil recruitment to the lung, results in prolific NE degrading protease activity and inflammation that can eventually become chronic and lead to tissue destruction. The recognition that aerosolized HTS may moderate neutrophil cytotoxicity and may function to restrain an exuberant inflammatory response in CF, provides a possible strategy for mitigating inappropriate neutrophil activity. This review will initially describe the use of HTS in treatment of CF and then extend the focus of HTS beyond mucociliary, to the potential benefits of aerosolized hyperosmolar therapy for the modulation of neutrophil activity within the confines of the CF airways. Our review of the literature was carried out using the MEDLINE database (from 1976 to the year 2014), Google Scholar and The Cochrane Library databases using several appropriate generic terms.
The use of HTS treatments has been shown to improve mucus clearance in CF and impact upon exacerbations, quality of life and improve lung function[12]. Early studies demonstrated an acute dose-response relationship between inhaled saline concentration and mucociliary clearance[25], with short-term HTS administration improving mucociliary clearance and lung function with acceptable tolerability[26]. In 2006, the National Hypertonic Saline in Cystic Fibrosis Study Group provided the first evidence for the long-term efficacy of HTS in individuals with CF. The study randomised 164 patients with CF to receive HTS (7%) or isotonic (0.9%) saline for 48 wk. Using forced vital capacity and forced expiratory volume in 1 s (FEV1) to assess the rate of change of lung function, no significant difference was observed between the two groups, but there was a statistically significant difference in the absolute change in lung function. More importantly, this study demonstrated an impressive reduction in the frequency of exacerbations in the HTS group, with fewer days missed from work or school. Furthermore, significant improvements in quality of life were observed, particularly with regard to mental health on quality of life questionnaires after long-term HTS therapy[12].
A further study by Donaldson et al[26] showed that repeated use of 7% HTS generated both acute and sustained improvements in mucociliary clearance while improving FEV1 following four-times-daily treatment for 14 d, when compared to HTS given in conjunction with the ENaC inhibitor amiloride, however this study lacked a 0.9% saline control group, and as a result the effect of HTS could only be compared to patient baselines. Robinson et al[27], in a study employing radioaerosol technique, examined the acute effect of a single administration by aerosolization of 7% HTS, amiloride, or a combination of HTS and amiloride, or a 0.9% saline control. Results demonstrated that treatment with HTS alone significantly increased mucociliary clearance compared to treatment with HTS/amiloride combined, and both of these therapies were in turn significantly more effective than isotonic saline or amiloride alone.
The efficacy of HTS in improving mucociliary clearance may also be related to the volume administered as studies of 4 mL or 5 mL aerosolized HTS[12,26] recorded smaller improvements in lung function compared to a 10 mL volume[11,28]. In 2011, Dmello et al[29] used a multivariate logistic regression analysis to assess 340 CF exacerbations, 99 of them involving treatment with HTS. The results confirmed the beneficial effect of HTS with regard to reduction of pulmonary exacerbation frequency, even in those with “severe” CF lung disease, categorised as those with an FEV1 below 40%. A further study, on the use of HTS during hospitalization for adult exacerbations of CF showed that nebulized treatment accelerated the recovery of FEV1 to baseline[30]. However, there is conflicting evidence on the effectiveness of HTS upon lung function and FEV1 and a Cochrane review summarising all clinical trials of HTS in CF demonstrated a significant but minimal increase in FEV1 with a mean change of 4.15% after 4 wk, however at 48 wk this was not significant and was reduced to 2.31%[31].
While spirometry, primarily FEV1, represents the measure of lung function used in the majority of HTS studies to date, the use of lung clearance index (LCI), a measure of ventilation inhomogeneity derived from the multiple breath washout test, is increasingly being employed for the early detection of CF respiratory disease[32]. LCI has been shown to be a better predictor of later lung function abnormalities than FEV1[33] and also correlates well with structural changes[34,35]. LCI has been shown to detect treatment responses to HTS in children with CF aged 6-18 years who have normal baseline spirometry[36]. It should be noted that while these studies when analysed together formed the basis for HTS use in the majority of CF centres in Europe and North America, the data for the most part only apply to adults, with a relative lack of evidence for use in children. Studies of HTS use in the CF child population have shown satisfactory safety and tolerability profiles[37-39], but it is still unclear as to whether or not HTS treatment confers a clinical benefit upon this group. This may be in part due to the fact that younger individuals typically have less-advanced lung disease, nonetheless it is still well tolerated even in very young children aged between 12 and 30 mo[38]. Although there is good evidence to suggest that HTS is of benefit regarding the enhancement of mucociliary clearance in adults, one study of HTS in CF children aged between 7-14 years published by Laube et al[40] demonstrated only negligible acute clearance effects, however, it should be noted, that this was a single-dose study. A recent trial, from the North Carolina group at Chapel Hill, of HTS in CF children with normal lung function has shown some interesting results. This trial compares 6% HTS to 0.12% saline, with both arms of the study receiving 4 mL three times daily for four weeks. While mucociliary clearance was largely unaltered at 2 h after the initial dose, a significant acceleration of mucociliary clearance lasting greater than 12 h following the final dose was observed[41]. This sustained effect suggests that single-dose studies may not be ideal predictors of mucociliary clearance in these individuals. A further study, by Amin et al[36] using LCI to evaluate ventilation heterogeneity in individuals aged between 6 and 18 years with CF with normal spirometry, demonstrated a significant improvement in ventilation after four weeks of HTS treatment. Moreover, recent evidence has demonstrated that HTS is also beneficial through its ability to reduce Pseudomonas aeruginosa activity[42] and also to disrupt biofilm formation[43].
Although an acute dose-response relationship between inhaled saline concentration and mucociliary clearance exists, data showing better or worse clinical efficacy with concentrations other than 7% are lacking. In this regard most clinical trials show that both 3% and 7% HTS are more effective than placebo[31], however one clinical trial in a paediatric population demonstrated a superior effect with 3% HTS. In this study, the 3% group had significantly higher FEV1 on day 14 and day 28 compared to the group receiving 7%[44], however this study was not extended beyond 28 d, so it is unclear whether there is a truly superior dose, and the majority of trials have employed 7% HTS. Moreover, the percentage of HTS administered not only has implications for clinical efficacy, but also for patient adherence, since as doses increase (from 3% to 7%), so do nebulisation times, taste and tolerability, all important factors for compliance[45]. A 1997 study by Robinson et al[25] showing increasing levels of sputum clearance with increasing concentrations of saline also noted that factors such as cough and oropharyngeal irritation increased in tandem with sputum clearance, and were highly disconcerting at concentrations approaching 12%, setting the ceiling of tolerability for the study. Tolerability is often a key determinant of the dose selected for an individual patient, with pre-treatment with bronchodilators aimed at facilitating a higher concentration. Roughly 5% of CF patients undergoing treatment with HTS will experience bronchospasm severe enough to restrict use[8]. A commonly-used starting point for HTS is 7%, with bronchodilator pre-treatment, and with the willingness to down-titrate should patient comfort be sufficiently compromised. Administration of 7% HTS in conjunction with 0.1% hyaluronic acid via the aerosolised route has been shown to significantly improve tolerability and pleasantness when compared with 7% HTS alone[46].
Circulating neutrophils are initially found in a resting state, and become primed upon exposure to chemotactic stimuli comprising pathogenic molecules such as N-formyl peptides, cytokines including tumour necrosis factor-α (TNF-α) and chemokines including interleukin (IL)-8[47]. The release of cytokines and chemokines including IL-8 and granulocyte macrophage colony stimulating factor (GM-CSF) by CF epithelial cells functions to signal to circulating immune cells resulting in increased numbers of neutrophils and macrophages localized to the airways[48,49]. IL-8 binds to the chemokine (C-X-C motif) receptor 1 (CXCR1) and CXCR2 on the plasma membrane of neutrophils resulting in cell adhesion[50] and migration[51]. In turn, synthesis and release of TNF-α and IL-1β by recruited macrophages, and NE induced secretion of IL-8 and IL-6 by upper airway epithelial cells, perpetuate the cycle of inflammation[52,53]. In addition, NE activity in BAL fluid is associated with early airways disease in children with CF[54] and both NE and TNF-α up-regulate leukotriene B4 (LTB4) production by macrophages[55,56], the latter a potent lipid inflammatory mediator. It has also been documented that CF lung epithelial cells release IL-8 in the absence of pathogens suggesting a persistent pro-inflammatory state[13,14]. Moreover, upon bacterial challenge studies have shown that the level of IL-8 released in response to infection is significantly increased in CF airway epithelial cells compared to CFTR sufficient cells and this has in part been explained by the plasma membrane surface expression of asialoganglioside 1 and toll-like receptor 4[57,58].
Observations of increased cell migration and neutrophil-dominated chronic airway inflammation at an early age in children with CF[59], supports the need for potential therapies that may target airway inflammatory mediators of neutrophil priming and migration. In this regard the ability of HTS to act as an anti-inflammatory, or alternatively pro-inflammatory agent, was studied by Chan et al[60]. IB3-1 bronchial epithelial cells containing the DF508/W1282X CF mutation were exposed to increasing concentrations of HTS ex vivo and secreted IL-8 levels were quantified. Results revealed that CFTR mutated bronchial epithelial cells produced an exaggerated level of both basal and NaCl-induced IL-8 production, indicating that HTS was acting as a pro-inflammatory stimuli[60]. However, the highest concentration of HTS employed in this study was 125 mmol/L, which is in contrast to the therapeutic concentration of HTS used in vivo (513 mmol/L; 3%). Nevertheless, this effect of HTS was echoed by studies that demonstrated that hyperosmolar solutions stimulated cytokine production by bronchial epithelial cells via p38 mitogen-activated protein kinases activation[61] and in CF bronchial gland cells via the NF-κB pathway[62]. Similarly, a study carried out by Shapiro et al[63] demonstrated that human peripheral blood mononuclear cells exposed to increasing concentrations of NaCl in combination with bacterial lipopolysaccharide or IL-1 exhibited increased protein expression of IL-8, IL-1β and TNF-α.
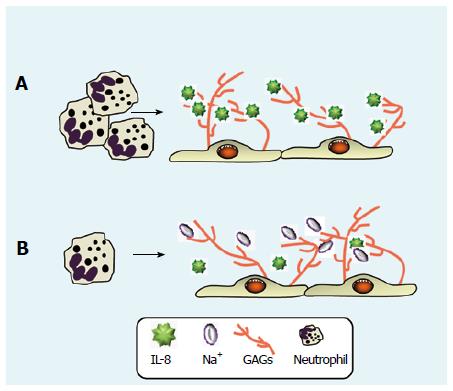
HTS continues to be used as a therapy available for the treatment of patients with CF[64] and in contrast to the HTS-induced increased expression of IL-8 in in vitro studies, a number of in vivo studies have measured IL-8 levels following HTS treatment. These included a long term controlled trial of inhaled HTS in patients with CF, compared to inhaled isotonic saline, with no significant difference in sputum IL-8 levels found between the groups[12]. Two further studies also investigated IL-8 levels in CF sputum post HTS (3% and 7%) nebulisation, with results showing no significant alteration in IL-8 levels[65,66]. Moreover, an investigation designed to assess the effect of 7% HTS on airway inflammation in CF, with outcome measurements including altered IL-8, myeloperoxidase (MPO) and NE levels, revealed no increase in free IL-8 and the study did not support the capacity of HTS to promote inflammation in CF[67]. Furthermore, in human pulmonary microvascular endothelial cells the ability of increasing concentrations of HTS (ranging from 140 mmol/L to 170 mmol/L NaCl) to significantly reduce TNF-α-induced IL-8 release was established[68]. However, the concentration of HTS utilised was far below that used therapeutically. More recently, the functionality of HTS in reducing levels of IL-8 bound to glycosaminoglycans (GAGs) within the CF airways was observed. Within the CF airways, the dehydrated thick mucus contains raised levels of anionic GAGs formed on the surface of bronchial epithelial cell[69], the most abundant including heparan sulphate (HS) and chondroitin sulphate (CS)[70,71]. Of major importance, increased quantities of GAGs have been found in airway samples from individuals with CF[72]. The immobilization of IL-8 by GAGs plays a major role in the establishment of gradients of the chemokine that contribute to the recruitment of neutrophils during inflammatory exacerbations[73]. The use of an IL-8 decoy (PA401) with enhanced GAG binding ability[74], or the removal of HS and CS lead to a significant reduction in the detection of this chemokine[75]. Moreover, disruption of this interaction with increasing ionic concentrations (7% HTS) displaces IL-8 from GAGs, subjecting the former to clearance by proteolytic activity by NE[76] (Figure 3). Although only a small number of patients were recruited to this latter study, and the effect of HTS on other immunomodulatory mediators in the CF airways was not evaluated, results are in line with the ability of aerosolized HTS in an animal model of acute lung injury to reduce levels of the murine analogue of IL-8, cytokine-induced neutrophil chemoattractant-1, by 44%[77].
Pro-inflammatory stimuli, either individually or in combination, can stimulate the neutrophil to change morphology and migrate to the airways, the latter being a multistep process. Initially, after a chemotatic signal is received, the neutrophil reversibly binds to the vascular endothelium through the interactions between P-selectin and E-selectin found on the epithelium, with L-selectin expressed on the neutrophil surface. Rolling of neutrophils involves interaction between these selectins and glycoproteins such as P-selectin glycoprotein ligand (PSGL1) which is expressed by the endothelium and leukocytes. This mediated rolling of the cell allows new bonds to form before breaking of older bonds and shedding of L-selectin[78]. This slow rolling then allows for tighter bonds to form between β2 integrins expressed on the neutrophil surface including CD11b/CD18 and the corresponding ligands, intercellular adhesion molecule-1 (ICAM-1) and ICAM-2. Once neutrophils have adhered to the endothelial wall, tight junctions between endothelial cells become loose and allow transmigration. Neutrophils then follow a gradient of immobilised chemoattractants and travel to the airways along collagen and elastin fibres[78] and movement through the extracellular matrix is facilitated by release of proteolytic enzymes including metalloproteases and NE[79,80].
The capacity of HTS to reduce neutrophil migration as a result of lowering levels of the potent neutrophil chemoattractant IL-8 has been investigated. In this regard, the consequence of disruption of interactions between IL-8 and GAGs within the CF lung was addressed by assessing the chemotactic potency of sputum ex vivo following nebulized HTS treatment, with results demonstrating a reduction in the neutrophil chemotactic index[76]. Although IL-8 is a major chemotactic factor in CF, it is not the only chemoattractant found in the CF airways. Thus this latter study should be extended to evaluate the effect of HTS on additional chemoattractants including levels of formyl peptides, C5a[81], and the more recently described chemotactic peptide, proline-glycine-proline[82]. Nevertheless, in agreement with these latter findings, Aitken et al[65] showed that the percentage of neutrophils in liquefied sputum samples significantly decreased post HTS (3%) nebulization. Moreover, recent data indicates that HTS can inhibit platelet activating factor (PAF) stimulated cell adhesion. In this regard, exposure of neutrophils to PAF characteristically leads to increased CD11b/CD18 surface expression, and adhesion of PAF activated neutrophils was significantly inhibited by pretreatment with HTS, indicating that HTS may influence functional changes in neutrophils[68]. This concept is further supported by a study demonstrating that HTS considerably reduced neutrophil chemotaxis in response to zymosan-activated serum[83]. Moreover, HTS treatment decreased the number of neutrophils migrating to the airways in a rat model[84], and has been shown to reduce neutrophil adhesion and rolling in a murine model[85]. Although this latter study did not evaluate the neutrophil plasma membrane surface expression of either L-selection or CD11b, diminished levels of both adhesion molecules in response to HTS had previously been documented[86,87]. Moreover, while the use of animal models provides in-depth information on the efficacy of HTS usage, they are not representative of human disease and in particular the use of murine models in the study of CF is limited, as CF mice fail to develop spontaneous lung disease or chronic bacterial infection[88].
The process of neutrophil mediated bacterial clearance can be divided into two main procedures, those that are oxygen independent, and those that are oxygen dependent. These two cell processes are tightly regulated, and upon dysregulation, can result in release of reactive oxygen species and proteolytic enzymes to the surrounding lung tissues, as occurs in CF. Reactive oxygen species are produced by reduction of consumed oxygen. This reaction is catalysed by the NADPH oxidase, an enzyme complex that consists of two membrane proteins, p22phox and gp91phox, that constitute the heterodimeric flavoprotein cytochrome b558, and four cytosolic components p67phox, p47phox, p40phox and p21rac (Figure 4). In the resting neutrophil the majority of membrane-associated flavoprotein cytochrome b558 is localised to secondary granules and the plasma membrane, whereas components p67phox, p47phox and p40phox are localised within the cytosol together with GDP-bound p21rac. Upon priming of the neutrophil with proinflammatory stimuli including fMLP or TNF-, partial assembly of the NADPH oxidase occurs involving phosphorylation of p67phox and p47phox followed by translocation to the flavocytochrome. The NADPH oxidase complex becomes fully assembled upon recruitment of GTP-bound p21rac. Upon assembly, the active oxidase reduces NADPH and electrons are transferred via the flavocytochrome across the membrane to oxygen creating superoxide (O2-), which dismutates to hydrogen peroxide (H2O2). H2O2 generated during the oxidative burst has limited bactericidal properties and the best-defined function of H2O2 in the antimicrobial activities of neutrophils comes from the function of H2O2 as a substrate for MPO in the presence of halides [chloride (Cl-)], resulting in the formation of hypochlorous acid (HOCl). HOCl is the most bactericidal oxidant known to be produced by neutrophils and as Dakin’s solution, was extensively used in medicine in the treatment of topical wounds until antibiotics became available. Conversely, neutrophil-derived reactive oxygen species have been implicated in activation of NF-κB, release of pro-inflammatory mediators, inhibition of apoptosis and recurring DNA damage[89].
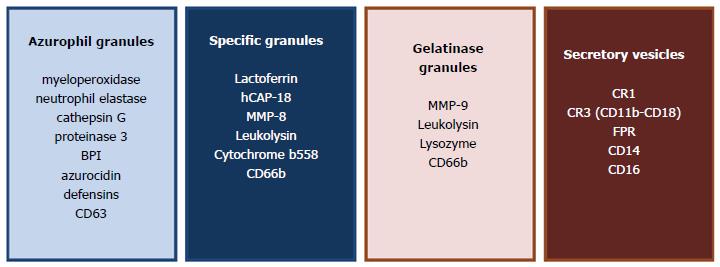
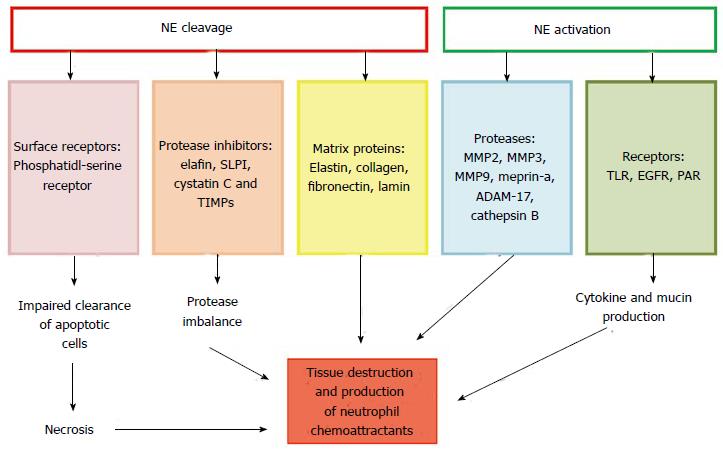
The second mechanism contributing to bacterial killing is mediated by enzymes stored in granules (Figure 5). Essential serine proteases stored in primary granules include NE, cathepsin G and proteinase 3. Each azurophilic granule contains 5.33 mmol/L NE, corresponding to approximately 67000 molecules per granule. NE, protease 3 and cathepsin G, are found in similar amounts and distribution in neutrophils[90], however much of the research has focused on NE as it is the main mediator of proteolysis (Figure 6). As NE up-regulates expression of other proteases it has been suggested that neutralization of NE activity is central to reducing the overall protease burden within the airways[91]. In addition, NE plays a central role in activation of matrix metalloproteinases (MMPs) which are synthesized in an inactive zymogen precursor form[92]. For example, MMP-9 which exists as a pro-form, exhibits a molecular mass of 92 kDa which is cleaved by NE into an active molecule that is 72-kDa in size[93]. In turn, increased levels of active MMP-9 can lead to the increased production of chemotactic peptides[94] and extensive airway remodelling and inflammation[95,96]. Thus, of the serine proteases, NE is the most harmful in the lung[97] and it has been proposed as a target for therapeutic intervention in CF[98,99]. Unopposed NE proteolytic action can degrade molecules important in control of inflammation including receptors[100], particularly those required for clearance of apoptotic neutrophils[101] or bacterial phagocytosis[102,103]. NE can also inactivate and degrade antiproteases including elafin[104], alpha-1 antitrypsin and secretory leukocyte inhibitor[105]. As a consequence of the proteases/antiprotease imbalance, lung tissue is irreversibly damaged, dramatically reducing lung function and ultimately causing respiratory failure[106]. In short, HTS therapies that may modulate exuberant oxidase and degranulation activity may be used as powerful anti-inflammatories within the setting of CF airways disease.
A number of in vitro investigations have documented that sodium chloride slows neutrophil activity[107] and a study evaluating the effect of HTS on the mechanisms of activation of the NADPH oxidase revealed that stimulated translocation of p67phox to the neutrophil membrane in response to PAF was prevented. Moreover, in in vitro cell-free oxidase assays, the membrane content of p67phox post PAF activation was increased in support of oxidase activity, whereas control unstimulated and HTS-PAF activated membranes contained equivalent p67phox protein content[108]. Although these results support the potential of HTS to modulate oxidase activity, the concentration of HTS utilised was 180 mmol/L, which is below therapeutic HTS and therefore higher concentrations of HTS should be investigated to determine the effect on p67phox membrane translocation. Nevertheless, the inhibitory effect of HTS on a second stimuli involving fMLP-induced NADPH oxidase was also confirmed. The described inhibition occurred in a dose-dependent manner with results indicating that transient increases in osmolality caused prolonged suppression of neutrophil O2- production to the outside of the cell, as measured by cytochrome c reduction[83]. The mechanism of inhibition was explored and shown to involve blockade of mitogen activated protein kinase (MAPK) ERK 1/2 and p38 signalling[83]. Moreover, H2O2 production to the outside of the cell post fMLP activation was equally reduced by two concentrations of HTS ([Na+] = 180 mmol/L and 200 mmol/L)[109]. In contrast however, and of major importance, intracellular formation of reactive oxygen species upon bacterial phagocytosis was potentiated with increasing osmolar strength[110]. Despite osmotic down-regulation of p38 and ERK-1, this later study demonstrated enhanced intracellular O2- generation in response to bacterial challenge suggesting that HTS may attenuate tissue injury by compromising neutrophil cytotoxic capacity, and additionally appears to enhance the response to bacteria. This may be a further beneficial role of HTS when aerosolized clinically in CF[110].
With respect to the ability of HTS to modulate the degranulation process, Junger et al[83] demonstrated that neutrophils exposed to > 50 mmol/L HTS alone released increased levels of MPO and NE, however, when cells were exposed simultaneously to inflammatory levels of fMLP and increasing concentrations of HTS, as would be expected in the CF airways, the fMLP-stimulated primary granule release of MPO[20] and NE was inhibited in a dose dependent manner. Moreover, HTS induced changes in the actin cytoskeleton have been reported[111] and linked to the hypertonic inhibition of neutrophil degranulation. HTS instigated a twofold increase in F-actin formation and abrogated the mobilization of all granule types suggesting cytoskeletal remodelling as a key component in the neutrophil-suppressive anti-inflammatory effects of HTS[112]. As neutrophils in individuals with CF demonstrate enhanced secretion of NE and MPO, the potential of aerosolized HTS to prevent primary granule release would have tremendous clinical implications. Furthermore, despite the fact that there is abundant extracellular neutrophil released hCAP-18/LL-37 in the lungs of individuals with CF, the lung fluid from patients exhibits poor antimicrobial activity. A recent study has demonstrated that the antimicrobial activity of endogenous hCAP-18/LL-37 in CF BAL fluid is rendered inactive by binding GAGs but is liberated following nebulized HTS[113]. The effect of HTS on levels of additional antimicrobial peptides and proteins within the CF airways was not evaluated but this study does suggest that a strategy whereby nebulized HTS augments antimicrobial activity may provide optimization of the innate antimicrobial activity in the setting of CF.
HTS treatment is associated with an improvement in lung function and marked benefits with respect to exacerbations[26,114,115]. Significant inflammation in the airways manifests from a very young age in CF most likely due to a combination of intrinsic innate immune dysregulation and infection. The obvious most effective treatment remains correction of CFTR dysfunction at a very early age, thereby curtailing development of airway inflammation. However, in the absence of CFTR ion channel modulators for each individual’s genotype it will remain important to modulate or suppress the inflammatory reactions of the disease. Although in children with CF, the use of inhaled HTS did not reduce the rate of pulmonary exacerbations[116], the described studies in the present review demonstrate dramatic in vitro effects of HTS on neutrophil function, limiting cellular processes that govern airway inflammation including cell adhesion, reactive oxygen species production and protease release. These reports support the concept that HTS may have beneficial anti-inflammatory effects other than simply increasing mucociliary clearance and thus further investigations of the potential mechanisms of this currently available therapy in CF is crucially required.
P- Reviewer: Chen XL, Lin J, Nayci A, Ntoumenopoulos G S- Editor: Tian YL L- Editor: A E- Editor: Wu HL
| 1. | Burns JL, Emerson J, Stapp JR, Yim DL, Krzewinski J, Louden L, Ramsey BW, Clausen CR. Microbiology of sputum from patients at cystic fibrosis centers in the United States. Clin Infect Dis. 1998;27:158-163. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 329] [Cited by in RCA: 312] [Article Influence: 11.6] [Reference Citation Analysis (0)] |
| 2. | Wood RE, Boat TF, Doershuk CF. Cystic fibrosis. Am Rev Respir Dis. 1976;113:833-878. [PubMed] |
| 3. | De Boeck K, Zolin A, Cuppens H, Olesen HV, Viviani L. The relative frequency of CFTR mutation classes in European patients with cystic fibrosis. J Cyst Fibros. 2014;13:403-409. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 114] [Cited by in RCA: 154] [Article Influence: 14.0] [Reference Citation Analysis (0)] |
| 4. | Zielenski J, Tsui LC. Cystic fibrosis: genotypic and phenotypic variations. Annu Rev Genet. 1995;29:777-807. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 424] [Cited by in RCA: 400] [Article Influence: 13.3] [Reference Citation Analysis (0)] |
| 5. | Boucher RC, Stutts MJ, Knowles MR, Cantley L, Gatzy JT. Na+ transport in cystic fibrosis respiratory epithelia. Abnormal basal rate and response to adenylate cyclase activation. J Clin Invest. 1986;78:1245-1252. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 417] [Cited by in RCA: 423] [Article Influence: 10.8] [Reference Citation Analysis (0)] |
| 6. | Stutts MJ, Canessa CM, Olsen JC, Hamrick M, Cohn JA, Rossier BC, Boucher RC. CFTR as a cAMP-dependent regulator of sodium channels. Science. 1995;269:847-850. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 795] [Cited by in RCA: 782] [Article Influence: 26.1] [Reference Citation Analysis (0)] |
| 7. | Matsui H, Grubb BR, Tarran R, Randell SH, Gatzy JT, Davis CW, Boucher RC. Evidence for periciliary liquid layer depletion, not abnormal ion composition, in the pathogenesis of cystic fibrosis airways disease. Cell. 1998;95:1005-1015. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 847] [Cited by in RCA: 821] [Article Influence: 30.4] [Reference Citation Analysis (0)] |
| 8. | Boucher RC. Evidence for airway surface dehydration as the initiating event in CF airway disease. J Intern Med. 2007;261:5-16. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 267] [Cited by in RCA: 270] [Article Influence: 15.0] [Reference Citation Analysis (0)] |
| 9. | McCarthy C, Dimitrov BD, Meurling IJ, Gunaratnam C, McElvaney NG. The CF-ABLE score: a novel clinical prediction rule for prognosis in patients with cystic fibrosis. Chest. 2013;143:1358-1364. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 29] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 10. | O’Sullivan BP, Flume P. The clinical approach to lung disease in patients with cystic fibrosis. Semin Respir Crit Care Med. 2009;30:505-513. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 24] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 11. | Eng PA, Morton J, Douglass JA, Riedler J, Wilson J, Robertson CF. Short-term efficacy of ultrasonically nebulized hypertonic saline in cystic fibrosis. Pediatr Pulmonol. 1996;21:77-83. [PubMed] |
| 12. | Elkins MR, Robinson M, Rose BR, Harbour C, Moriarty CP, Marks GB, Belousova EG, Xuan W, Bye PT. A controlled trial of long-term inhaled hypertonic saline in patients with cystic fibrosis. N Engl J Med. 2006;354:229-240. [PubMed] [DOI] [Full Text] |
| 13. | Hartl D, Griese M, Kappler M, Zissel G, Reinhardt D, Rebhan C, Schendel DJ, Krauss-Etschmann S. Pulmonary T(H)2 response in Pseudomonas aeruginosa-infected patients with cystic fibrosis. J Allergy Clin Immunol. 2006;117:204-211. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 133] [Cited by in RCA: 156] [Article Influence: 7.8] [Reference Citation Analysis (0)] |
| 14. | Birrer P, McElvaney NG, Rüdeberg A, Sommer CW, Liechti-Gallati S, Kraemer R, Hubbard R, Crystal RG. Protease-antiprotease imbalance in the lungs of children with cystic fibrosis. Am J Respir Crit Care Med. 1994;150:207-213. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 270] [Cited by in RCA: 264] [Article Influence: 8.5] [Reference Citation Analysis (0)] |
| 15. | McElvaney NG, Nakamura H, Birrer P, Hébert CA, Wong WL, Alphonso M, Baker JB, Catalano MA, Crystal RG. Modulation of airway inflammation in cystic fibrosis. In vivo suppression of interleukin-8 levels on the respiratory epithelial surface by aerosolization of recombinant secretory leukoprotease inhibitor. J Clin Invest. 1992;90:1296-1301. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 193] [Cited by in RCA: 206] [Article Influence: 6.2] [Reference Citation Analysis (0)] |
| 16. | Di A, Brown ME, Deriy LV, Li C, Szeto FL, Chen Y, Huang P, Tong J, Naren AP, Bindokas V. CFTR regulates phagosome acidification in macrophages and alters bactericidal activity. Nat Cell Biol. 2006;8:933-944. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 409] [Cited by in RCA: 394] [Article Influence: 20.7] [Reference Citation Analysis (0)] |
| 17. | Morris MR, Doull IJ, Dewitt S, Hallett MB. Reduced iC3b-mediated phagocytotic capacity of pulmonary neutrophils in cystic fibrosis. Clin Exp Immunol. 2005;142:68-75. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 37] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 18. | Painter RG, Valentine VG, Lanson NA, Leidal K, Zhang Q, Lombard G, Thompson C, Viswanathan A, Nauseef WM, Wang G. CFTR Expression in human neutrophils and the phagolysosomal chlorination defect in cystic fibrosis. Biochemistry. 2006;45:10260-10269. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 230] [Cited by in RCA: 220] [Article Influence: 11.6] [Reference Citation Analysis (0)] |
| 19. | Yoshimura K, Nakamura H, Trapnell BC, Chu CS, Dalemans W, Pavirani A, Lecocq JP, Crystal RG. Expression of the cystic fibrosis transmembrane conductance regulator gene in cells of non-epithelial origin. Nucleic Acids Res. 1991;19:5417-5423. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 112] [Cited by in RCA: 131] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 20. | Pohl K, Hayes E, Keenan J, Henry M, Meleady P, Molloy K, Jundi B, Bergin DA, McCarthy C, McElvaney OJ. A neutrophil intrinsic impairment affecting Rab27a and degranulation in cystic fibrosis is corrected by CFTR potentiator therapy. Blood. 2014;124:999-1009. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 112] [Cited by in RCA: 137] [Article Influence: 12.5] [Reference Citation Analysis (0)] |
| 21. | Ng HP, Zhou Y, Song K, Hodges CA, Drumm ML, Wang G. Neutrophil-mediated phagocytic host defense defect in myeloid Cftr-inactivated mice. PLoS One. 2014;9:e106813. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 38] [Cited by in RCA: 52] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 22. | Tirouvanziam R, Gernez Y, Conrad CK, Moss RB, Schrijver I, Dunn CE, Davies ZA, Herzenberg LA, Herzenberg LA. Profound functional and signaling changes in viable inflammatory neutrophils homing to cystic fibrosis airways. Proc Natl Acad Sci USA. 2008;105:4335-4339. [PubMed] |
| 23. | Makam M, Diaz D, Laval J, Gernez Y, Conrad CK, Dunn CE, Davies ZA, Moss RB, Herzenberg LA, Herzenberg LA. Activation of critical, host-induced, metabolic and stress pathways marks neutrophil entry into cystic fibrosis lungs. Proc Natl Acad Sci USA. 2009;106:5779-5783. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 74] [Cited by in RCA: 78] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 24. | Laval J, Touhami J, Herzenberg LA, Conrad C, Taylor N, Battini JL, Sitbon M, Tirouvanziam R. Metabolic adaptation of neutrophils in cystic fibrosis airways involves distinct shifts in nutrient transporter expression. J Immunol. 2013;190:6043-6050. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 55] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 25. | Robinson M, Hemming AL, Regnis JA, Wong AG, Bailey DL, Bautovich GJ, King M, Bye PT. Effect of increasing doses of hypertonic saline on mucociliary clearance in patients with cystic fibrosis. Thorax. 1997;52:900-903. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 190] [Cited by in RCA: 187] [Article Influence: 6.7] [Reference Citation Analysis (0)] |
| 26. | Donaldson SH, Bennett WD, Zeman KL, Knowles MR, Tarran R, Boucher RC. Mucus clearance and lung function in cystic fibrosis with hypertonic saline. N Engl J Med. 2006;354:241-250. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 489] [Cited by in RCA: 481] [Article Influence: 25.3] [Reference Citation Analysis (0)] |
| 27. | Robinson M, Regnis JA, Bailey DL, King M, Bautovich GJ, Bye PT. Effect of hypertonic saline, amiloride, and cough on mucociliary clearance in patients with cystic fibrosis. Am J Respir Crit Care Med. 1996;153:1503-1509. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 155] [Cited by in RCA: 151] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 28. | Ballmann M, von der Hardt H. Hypertonic saline and recombinant human DNase: a randomised cross-over pilot study in patients with cystic fibrosis. J Cyst Fibros. 2002;1:35-37. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 46] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 29. | Dmello D, Nayak RP, Matuschak GM. Stratified assessment of the role of inhaled hypertonic saline in reducing cystic fibrosis pulmonary exacerbations: a retrospective analysis. BMJ Open. 2011;1:e000019. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 13] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 30. | Dentice R, Elkins M, Bye P. A randomized trial of hypertonic saline nebulisation during hospitalisation for pulmonary exacerbation in adults with cystic fibrosis. Pedatr Pulmonol. 2012;47:257. [RCA] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 3] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 31. | Wark P, McDonald VM. Nebulised hypertonic saline for cystic fibrosis. Cochrane Database Syst Rev. 2009;CD001506. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 50] [Cited by in RCA: 69] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 32. | Gustafsson PM, Aurora P, Lindblad A. Evaluation of ventilation maldistribution as an early indicator of lung disease in children with cystic fibrosis. Eur Respir J. 2003;22:972-979. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 219] [Cited by in RCA: 224] [Article Influence: 10.7] [Reference Citation Analysis (0)] |
| 33. | Aurora P, Stanojevic S, Wade A, Oliver C, Kozlowska W, Lum S, Bush A, Price J, Carr SB, Shankar A. Lung clearance index at 4 years predicts subsequent lung function in children with cystic fibrosis. Am J Respir Crit Care Med. 2011;183:752-758. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 192] [Cited by in RCA: 176] [Article Influence: 12.6] [Reference Citation Analysis (0)] |
| 34. | Ellemunter H, Fuchs SI, Unsinn KM, Freund MC, Waltner-Romen M, Steinkamp G, Gappa M. Sensitivity of Lung Clearance Index and chest computed tomography in early CF lung disease. Respir Med. 2010;104:1834-1842. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 64] [Cited by in RCA: 69] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 35. | Gustafsson PM, De Jong PA, Tiddens HA, Lindblad A. Multiple-breath inert gas washout and spirometry versus structural lung disease in cystic fibrosis. Thorax. 2008;63:129-134. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 248] [Cited by in RCA: 277] [Article Influence: 15.4] [Reference Citation Analysis (0)] |
| 36. | Amin R, Subbarao P, Jabar A, Balkovec S, Jensen R, Kerrigan S, Gustafsson P, Ratjen F. Hypertonic saline improves the LCI in paediatric patients with CF with normal lung function. Thorax. 2010;65:379-383. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 163] [Cited by in RCA: 166] [Article Influence: 11.1] [Reference Citation Analysis (0)] |
| 37. | Dellon EP, Donaldson SH, Johnson R, Davis SD. Safety and tolerability of inhaled hypertonic saline in young children with cystic fibrosis. Pediatr Pulmonol. 2008;43:1100-1106. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 33] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 38. | Rosenfeld M, Davis S, Brumback L, Daniel S, Rowbotham R, Johnson R, McNamara S, Jensen R, Barlow C, Ratjen F. Inhaled hypertonic saline in infants and toddlers with cystic fibrosis: short-term tolerability, adherence, and safety. Pediatr Pulmonol. 2011;46:666-671. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 22] [Cited by in RCA: 22] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 39. | Subbarao P, Balkovec S, Solomon M, Ratjen F. Pilot study of safety and tolerability of inhaled hypertonic saline in infants with cystic fibrosis. Pediatr Pulmonol. 2007;42:471-476. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 38] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 40. | Laube BL, Sharpless G, Carson KA, Kelly A, Mogayzel PJ. Acute inhalation of hypertonic saline does not improve mucociliary clearance in all children with cystic fibrosis. BMC Pulm Med. 2011;11:45. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 22] [Cited by in RCA: 20] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 41. | Donaldson SD, LaFave C, Wu J, Zeman K, Salazar C, Bennett WD, Davis SD. Sustained effect of hypertonic saline on mucociliary clearance in CF children with mild lung disease. Pedatr Pulmonol. 2013;48:71-102. [DOI] [Full Text] |
| 42. | Havasi V, Hurst CO, Briles TC, Yang F, Bains DG, Hassett DJ, Sorscher E. Inhibitory effects of hypertonic saline on P. aeruginosa motility. J Cyst Fibros. 2008;7:267-269. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 21] [Cited by in RCA: 21] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 43. | Anderson GG, O’Toole GA. Innate and induced resistance mechanisms of bacterial biofilms. Curr Top Microbiol Immunol. 2008;322:85-105. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 133] [Cited by in RCA: 206] [Article Influence: 12.1] [Reference Citation Analysis (0)] |
| 44. | Gupta S, Ahmed F, Lodha R, Gupta YK, Kabra SK. Comparison of effects of 3 and 7% hypertonic saline nebulization on lung function in children with cystic fibrosis: a double-blind randomized, controlled trial. J Trop Pediatr. 2012;58:375-381. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 12] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 45. | Enderby B, Doull I. Hypertonic saline inhalation in cystic fibrosis-salt in the wound, or sweet success. Arch Dis Child. 2007;92:195-196. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 8] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 46. | Buonpensiero P, De Gregorio F, Sepe A, Di Pasqua A, Ferri P, Siano M, Terlizzi V, Raia V. Hyaluronic acid improves “pleasantness” and tolerability of nebulized hypertonic saline in a cohort of patients with cystic fibrosis. Adv Ther. 2010;27:870-878. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 42] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 47. | Mantovani A, Cassatella MA, Costantini C, Jaillon S. Neutrophils in the activation and regulation of innate and adaptive immunity. Nat Rev Immunol. 2011;11:519-531. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2271] [Cited by in RCA: 2141] [Article Influence: 152.9] [Reference Citation Analysis (0)] |
| 48. | Becker MN, Sauer MS, Muhlebach MS, Hirsh AJ, Wu Q, Verghese MW, Randell SH. Cytokine secretion by cystic fibrosis airway epithelial cells. Am J Respir Crit Care Med. 2004;169:645-653. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 105] [Cited by in RCA: 113] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 49. | Perez A, Issler AC, Cotton CU, Kelley TJ, Verkman AS, Davis PB. CFTR inhibition mimics the cystic fibrosis inflammatory profile. Am J Physiol Lung Cell Mol Physiol. 2007;292:L383-L395. [PubMed] |
| 50. | Takami M, Terry V, Petruzzelli L. Signaling pathways involved in IL-8-dependent activation of adhesion through Mac-1. J Immunol. 2002;168:4559-4566. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 64] [Cited by in RCA: 72] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 51. | Hammond ME, Lapointe GR, Feucht PH, Hilt S, Gallegos CA, Gordon CA, Giedlin MA, Mullenbach G, Tekamp-Olson P. IL-8 induces neutrophil chemotaxis predominantly via type I IL-8 receptors. J Immunol. 1995;155:1428-1433. [PubMed] |
| 52. | Bédard M, McClure CD, Schiller NL, Francoeur C, Cantin A, Denis M. Release of interleukin-8, interleukin-6, and colony-stimulating factors by upper airway epithelial cells: implications for cystic fibrosis. Am J Respir Cell Mol Biol. 1993;9:455-462. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 131] [Cited by in RCA: 131] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 53. | Ruef C, Jefferson DM, Schlegel-Haueter SE, Suter S. Regulation of cytokine secretion by cystic fibrosis airway epithelial cells. Eur Respir J. 1993;6:1429-1436. [PubMed] |
| 54. | Sly PD, Gangell CL, Chen L, Ware RS, Ranganathan S, Mott LS, Murray CP, Stick SM. Risk factors for bronchiectasis in children with cystic fibrosis. N Engl J Med. 2013;368:1963-1970. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 423] [Cited by in RCA: 474] [Article Influence: 39.5] [Reference Citation Analysis (0)] |
| 55. | Greally P, Hussein MJ, Cook AJ, Sampson AP, Piper PJ, Price JF. Sputum tumour necrosis factor-alpha and leukotriene concentrations in cystic fibrosis. Arch Dis Child. 1993;68:389-392. [PubMed] |
| 56. | Hubbard RC, Fells G, Gadek J, Pacholok S, Humes J, Crystal RG. Neutrophil accumulation in the lung in alpha 1-antitrypsin deficiency. Spontaneous release of leukotriene B4 by alveolar macrophages. J Clin Invest. 1991;88:891-897. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 125] [Cited by in RCA: 149] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 57. | Greene CM, Carroll TP, Smith SG, Taggart CC, Devaney J, Griffin S, O’neill SJ, McElvaney NG. TLR-induced inflammation in cystic fibrosis and non-cystic fibrosis airway epithelial cells. J Immunol. 2005;174:1638-1646. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 165] [Cited by in RCA: 171] [Article Influence: 8.6] [Reference Citation Analysis (0)] |
| 58. | Saiman L, Prince A. Pseudomonas aeruginosa pili bind to asialoGM1 which is increased on the surface of cystic fibrosis epithelial cells. J Clin Invest. 1993;92:1875-1880. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 246] [Cited by in RCA: 231] [Article Influence: 7.2] [Reference Citation Analysis (0)] |
| 59. | Balough K, McCubbin M, Weinberger M, Smits W, Ahrens R, Fick R. The relationship between infection and inflammation in the early stages of lung disease from cystic fibrosis. Pediatr Pulmonol. 1995;20:63-70. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 239] [Cited by in RCA: 237] [Article Influence: 7.9] [Reference Citation Analysis (0)] |
| 60. | Chan MM, Chmura K, Chan ED. Increased NaCl-induced interleukin-8 production by human bronchial epithelial cells is enhanced by the DeltaF508/W1282X mutation of the cystic fibrosis transmembrane conductance regulator gene. Cytokine. 2006;33:309-316. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 13] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 61. | Hashimoto S, Matsumoto K, Gon Y, Nakayama T, Takeshita I, Horie T. Hyperosmolarity-induced interleukin-8 expression in human bronchial epithelial cells through p38 mitogen-activated protein kinase. Am J Respir Crit Care Med. 1999;159:634-640. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 113] [Cited by in RCA: 120] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 62. | Tabary O, Escotte S, Couetil JP, Hubert D, Dusser D, Puchelle E, Jacquot J. High susceptibility for cystic fibrosis human airway gland cells to produce IL-8 through the I kappa B kinase alpha pathway in response to extracellular NaCl content. J Immunol. 2000;164:3377-3384. [PubMed] |
| 63. | Shapiro L, Dinarello CA. Hyperosmotic stress as a stimulant for proinflammatory cytokine production. Exp Cell Res. 1997;231:354-362. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 98] [Cited by in RCA: 106] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 64. | Goss CH, Ratjen F. Update in cystic fibrosis 2012. Am J Respir Crit Care Med. 2013;187:915-919. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 27] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 65. | Aitken ML, Greene KE, Tonelli MR, Burns JL, Emerson JC, Goss CH, Gibson RL. Analysis of sequential aliquots of hypertonic saline solution-induced sputum from clinically stable patients with cystic fibrosis. Chest. 2003;123:792-799. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 27] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 66. | Suri R, Metcalfe C, Lees B, Grieve R, Flather M, Normand C, Thompson S, Bush A, Wallis C. Comparison of hypertonic saline and alternate-day or daily recombinant human deoxyribonuclease in children with cystic fibrosis: a randomised trial. Lancet. 2001;358:1316-1321. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 99] [Cited by in RCA: 102] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 67. | Suri R, Marshall LJ, Wallis C, Metcalfe C, Bush A, Shute JK. Effects of recombinant human DNase and hypertonic saline on airway inflammation in children with cystic fibrosis. Am J Respir Crit Care Med. 2002;166:352-355. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 49] [Cited by in RCA: 55] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 68. | Banerjee A, Moore EE, McLaughlin NJ, Lee L, Jones WL, Johnson JL, Nydam TL, Silliman CC. Hyperosmolarity attenuates TNF-α-mediated proinflammatory activation of human pulmonary microvascular endothelial cells. Shock. 2013;39:366-372. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 22] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 69. | Reeves EP, Bergin DA, Murray MA, McElvaney NG. The involvement of glycosaminoglycans in airway disease associated with cystic fibrosis. ScientificWorldJournal. 2011;11:959-971. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 18] [Cited by in RCA: 21] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 70. | Solic N, Wilson J, Wilson SJ, Shute JK. Endothelial activation and increased heparan sulfate expression in cystic fibrosis. Am J Respir Crit Care Med. 2005;172:892-898. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 37] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 71. | Suki B, Ito S, Stamenovic D, Lutchen KR, Ingenito EP. Biomechanics of the lung parenchyma: critical roles of collagen and mechanical forces. J Appl Physiol (1985). 2005;98:1892-1899. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 209] [Cited by in RCA: 201] [Article Influence: 10.1] [Reference Citation Analysis (0)] |
| 72. | Hilliard TN, Regamey N, Shute JK, Nicholson AG, Alton EW, Bush A, Davies JC. Airway remodelling in children with cystic fibrosis. Thorax. 2007;62:1074-1080. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 92] [Cited by in RCA: 106] [Article Influence: 5.9] [Reference Citation Analysis (0)] |
| 73. | Proudfoot AE, Handel TM, Johnson Z, Lau EK, LiWang P, Clark-Lewis I, Borlat F, Wells TN, Kosco-Vilbois MH. Glycosaminoglycan binding and oligomerization are essential for the in vivo activity of certain chemokines. Proc Natl Acad Sci USA. 2003;100:1885-1890. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 607] [Cited by in RCA: 602] [Article Influence: 27.4] [Reference Citation Analysis (0)] |
| 74. | McElvaney OJ, O’Reilly N, White M, Lacey N, Pohl K, Gerlza T, Bergin DA, Kerr H, McCarthy C, O’Brien ME. The effect of the decoy molecule PA401 on CXCL8 levels in bronchoalveolar lavage fluid of patients with cystic fibrosis. Mol Immunol. 2015;63:550-558. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 15] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 75. | Frevert CW, Kinsella MG, Vathanaprida C, Goodman RB, Baskin DG, Proudfoot A, Wells TN, Wight TN, Martin TR. Binding of interleukin-8 to heparan sulfate and chondroitin sulfate in lung tissue. Am J Respir Cell Mol Biol. 2003;28:464-472. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 84] [Cited by in RCA: 82] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 76. | Reeves EP, Williamson M, O’Neill SJ, Greally P, McElvaney NG. Nebulized hypertonic saline decreases IL-8 in sputum of patients with cystic fibrosis. Am J Respir Crit Care Med. 2011;183:1517-1523. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 70] [Cited by in RCA: 68] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 77. | Wohlauer M, Moore EE, Silliman CC, Fragoso M, Gamboni F, Harr J, Accurso F, Wright F, Haenel J, Fullerton D. Nebulized hypertonic saline attenuates acute lung injury following trauma and hemorrhagic shock via inhibition of matrix metalloproteinase-13. Crit Care Med. 2012;40:2647-2653. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 33] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 78. | Mandeville JT, Lawson MA, Maxfield FR. Dynamic imaging of neutrophil migration in three dimensions: mechanical interactions between cells and matrix. J Leukoc Biol. 1997;61:188-200. [PubMed] |
| 79. | Delclaux C, Delacourt C, D’Ortho MP, Boyer V, Lafuma C, Harf A. Role of gelatinase B and elastase in human polymorphonuclear neutrophil migration across basement membrane. Am J Respir Cell Mol Biol. 1996;14:288-295. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 309] [Cited by in RCA: 307] [Article Influence: 10.6] [Reference Citation Analysis (0)] |
| 80. | Lin M, Jackson P, Tester AM, Diaconu E, Overall CM, Blalock JE, Pearlman E. Matrix metalloproteinase-8 facilitates neutrophil migration through the corneal stromal matrix by collagen degradation and production of the chemotactic peptide Pro-Gly-Pro. Am J Pathol. 2008;173:144-153. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 96] [Cited by in RCA: 113] [Article Influence: 6.6] [Reference Citation Analysis (0)] |
| 81. | Mackerness KJ, Jenkins GR, Bush A, Jose PJ. Characterisation of the range of neutrophil stimulating mediators in cystic fibrosis sputum. Thorax. 2008;63:614-620. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 23] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 82. | Gaggar A, Jackson PL, Noerager BD, O’Reilly PJ, McQuaid DB, Rowe SM, Clancy JP, Blalock JE. A novel proteolytic cascade generates an extracellular matrix-derived chemoattractant in chronic neutrophilic inflammation. J Immunol. 2008;180:5662-5669. [PubMed] |
| 83. | Junger WG, Hoyt DB, Davis RE, Herdon-Remelius C, Namiki S, Junger H, Loomis W, Altman A. Hypertonicity regulates the function of human neutrophils by modulating chemoattractant receptor signaling and activating mitogen-activated protein kinase p38. J Clin Invest. 1998;101:2768-2779. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 134] [Cited by in RCA: 134] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 84. | Rizoli SB, Kapus A, Fan J, Li YH, Marshall JC, Rotstein OD. Immunomodulatory effects of hypertonic resuscitation on the development of lung inflammation following hemorrhagic shock. J Immunol. 1998;161:6288-6296. [PubMed] |
| 85. | Pascual JL, Ferri LE, Seely AJ, Campisi G, Chaudhury P, Giannias B, Evans DC, Razek T, Michel RP, Christou NV. Hypertonic saline resuscitation of hemorrhagic shock diminishes neutrophil rolling and adherence to endothelium and reduces in vivo vascular leakage. Ann Surg. 2002;236:634-642. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 86. | Angle N, Hoyt DB, Coimbra R, Liu F, Herdon-Remelius C, Loomis W, Junger WG. Hypertonic saline resuscitation diminishes lung injury by suppressing neutrophil activation after hemorrhagic shock. Shock. 1998;9:164-170. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 166] [Cited by in RCA: 160] [Article Influence: 5.9] [Reference Citation Analysis (0)] |
| 87. | Ciesla DJ, Moore EE, Zallen G, Biffl WL, Silliman CC. Hypertonic saline attenuation of polymorphonuclear neutrophil cytotoxicity: timing is everything. J Trauma. 2000;48:388-395. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 81] [Cited by in RCA: 77] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 88. | Fisher JT, Zhang Y, Engelhardt JF. Comparative biology of cystic fibrosis animal models. Methods Mol Biol. 2011;742:311-334. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 68] [Cited by in RCA: 66] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 89. | Yao H, Yang SR, Kode A, Rajendrasozhan S, Caito S, Adenuga D, Henry R, Edirisinghe I, Rahman I. Redox regulation of lung inflammation: role of NADPH oxidase and NF-kappaB signalling. Biochem Soc Trans. 2007;35:1151-1155. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 97] [Cited by in RCA: 112] [Article Influence: 6.6] [Reference Citation Analysis (0)] |
| 90. | Campbell EJ, Campbell MA, Owen CA. Bioactive proteinase 3 on the cell surface of human neutrophils: quantification, catalytic activity, and susceptibility to inhibition. J Immunol. 2000;165:3366-3374. [PubMed] |
| 91. | Geraghty P, Rogan MP, Greene CM, Boxio RM, Poiriert T, O’Mahony M, Belaaouaj A, O’Neill SJ, Taggart CC, McElvaney NG. Neutrophil elastase up-regulates cathepsin B and matrix metalloprotease-2 expression. J Immunol. 2007;178:5871-5878. [PubMed] |
| 92. | Elkington PT, O’Kane CM, Friedland JS. The paradox of matrix metalloproteinases in infectious disease. Clin Exp Immunol. 2005;142:12-20. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 251] [Cited by in RCA: 257] [Article Influence: 12.9] [Reference Citation Analysis (0)] |
| 93. | Ferry G, Lonchampt M, Pennel L, de Nanteuil G, Canet E, Tucker GC. Activation of MMP-9 by neutrophil elastase in an in vivo model of acute lung injury. FEBS Lett. 1997;402:111-115. [PubMed] |
| 94. | Van den Steen PE, Proost P, Wuyts A, Van Damme J, Opdenakker G. Neutrophil gelatinase B potentiates interleukin-8 tenfold by aminoterminal processing, whereas it degrades CTAP-III, PF-4, and GRO-alpha and leaves RANTES and MCP-2 intact. Blood. 2000;96:2673-2681. [PubMed] |
| 95. | Heppner KJ, Matrisian LM, Jensen RA, Rodgers WH. Expression of most matrix metalloproteinase family members in breast cancer represents a tumor-induced host response. Am J Pathol. 1996;149:273-282. [PubMed] |
| 96. | Jackson PL, Xu X, Wilson L, Weathington NM, Clancy JP, Blalock JE, Gaggar A. Human neutrophil elastase-mediated cleavage sites of MMP-9 and TIMP-1: implications to cystic fibrosis proteolytic dysfunction. Mol Med. 2010;16:159-166. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 63] [Cited by in RCA: 83] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 97. | Griese M, Kappler M, Gaggar A, Hartl D. Inhibition of airway proteases in cystic fibrosis lung disease. Eur Respir J. 2008;32:783-795. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 76] [Cited by in RCA: 86] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 98. | Greene CM, McElvaney NG. Proteases and antiproteases in chronic neutrophilic lung disease - relevance to drug discovery. Br J Pharmacol. 2009;158:1048-1058. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 104] [Cited by in RCA: 115] [Article Influence: 7.7] [Reference Citation Analysis (0)] |
| 99. | Kelly E, Greene CM, McElvaney NG. Targeting neutrophil elastase in cystic fibrosis. Expert Opin Ther Targets. 2008;12:145-157. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 60] [Cited by in RCA: 64] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 100. | Vega-Carrascal I, Reeves EP, Niki T, Arikawa T, McNally P, O’Neill SJ, Hirashima M, McElvaney NG. Dysregulation of TIM-3-galectin-9 pathway in the cystic fibrosis airways. J Immunol. 2011;186:2897-2909. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 35] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 101. | Vandivier RW, Fadok VA, Hoffmann PR, Bratton DL, Penvari C, Brown KK, Brain JD, Accurso FJ, Henson PM. Elastase-mediated phosphatidylserine receptor cleavage impairs apoptotic cell clearance in cystic fibrosis and bronchiectasis. J Clin Invest. 2002;109:661-670. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 128] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 102. | Vega-Carrascal I, Bergin DA, McElvaney OJ, McCarthy C, Banville N, Pohl K, Hirashima M, Kuchroo VK, Reeves EP, McElvaney NG. Galectin-9 signaling through TIM-3 is involved in neutrophil-mediated Gram-negative bacterial killing: an effect abrogated within the cystic fibrosis lung. J Immunol. 2014;192:2418-2431. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 38] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 103. | Hartl D, Latzin P, Hordijk P, Marcos V, Rudolph C, Woischnik M, Krauss-Etschmann S, Koller B, Reinhardt D, Roscher AA. Cleavage of CXCR1 on neutrophils disables bacterial killing in cystic fibrosis lung disease. Nat Med. 2007;13:1423-1430. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 217] [Cited by in RCA: 247] [Article Influence: 13.7] [Reference Citation Analysis (0)] |
| 104. | Guyot N, Butler MW, McNally P, Weldon S, Greene CM, Levine RL, O’Neill SJ, Taggart CC, McElvaney NG. Elafin, an elastase-specific inhibitor, is cleaved by its cognate enzyme neutrophil elastase in sputum from individuals with cystic fibrosis. J Biol Chem. 2008;283:32377-32385. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 60] [Cited by in RCA: 70] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 105. | Taggart CC, Lowe GJ, Greene CM, Mulgrew AT, O’Neill SJ, Levine RL, McElvaney NG. Cathepsin B, L, and S cleave and inactivate secretory leucoprotease inhibitor. J Biol Chem. 2001;276:33345-33352. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 138] [Cited by in RCA: 147] [Article Influence: 6.1] [Reference Citation Analysis (0)] |
| 106. | Welsh MJ, Fick RB. Cystic fibrosis. J Clin Invest. 1987;80:1523-1526. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 75] [Cited by in RCA: 80] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 107. | Hampton MB, Chambers ST, Vissers MC, Winterbourn CC. Bacterial killing by neutrophils in hypertonic environments. J Infect Dis. 1994;169:839-846. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 46] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 108. | Sheppard FR, Moore EE, McLaughlin N, Kelher M, Johnson JL, Silliman CC. Clinically relevant osmolar stress inhibits priming-induced PMN NADPH oxidase subunit translocation. J Trauma. 2005;58:752-757; discussion 757. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 14] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 109. | Choi SH, Lee SW, Hong YS, Jeun JM, Min BW. Selective inhibition of polymorphonuclear neutrophils by resuscitative concentration of hypertonic saline. Emerg Med J. 2006;23:119-122. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 12] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 110. | Shields CJ, O’Sullivan AW, Wang JH, Winter DC, Kirwan WO, Redmond HP. Hypertonic saline enhances host response to bacterial challenge by augmenting receptor-independent neutrophil intracellular superoxide formation. Ann Surg. 2003;238:249-257. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 31] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 111. | Ciesla DJ, Moore EE, Musters RJ, Biffl WL, Silliman CA. Hypertonic saline alteration of the PMN cytoskeleton: implications for signal transduction and the cytotoxic response. J Trauma. 2001;50:206-212. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 34] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 112. | Rizoli SB, Rotstein OD, Parodo J, Phillips MJ, Kapus A. Hypertonic inhibition of exocytosis in neutrophils: central role for osmotic actin skeleton remodeling. Am J Physiol Cell Physiol. 2000;279:C619-C633. [PubMed] |
| 113. | Bergsson G, Reeves EP, McNally P, Chotirmall SH, Greene CM, Greally P, Murphy P, O’Neill SJ, McElvaney NG. LL-37 complexation with glycosaminoglycans in cystic fibrosis lungs inhibits antimicrobial activity, which can be restored by hypertonic saline. J Immunol. 2009;183:543-551. [PubMed] |
| 114. | Elkins MR, Bye PT. Inhaled hypertonic saline as a therapy for cystic fibrosis. Curr Opin Pulm Med. 2006;12:445-452. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 54] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 115. | Wark PA, McDonald V, Jones AP. Nebulised hypertonic saline for cystic fibrosis. Cochrane Database Syst Rev. 2005;CD001506. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 29] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 116. | Stanley RB, Becker TS. Injuries of the nasofrontal orifices in frontal sinus fractures. Laryngoscope. 1987;97:728-731. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 147] [Cited by in RCA: 144] [Article Influence: 11.1] [Reference Citation Analysis (0)] |