Published online Feb 4, 2014. doi: 10.5492/wjccm.v3.i1.42
Revised: October 12, 2013
Accepted: November 15, 2013
Published online: February 4, 2014
Processing time: 282 Days and 7.2 Hours
Management of sedation in the critical care unit is an ongoing challenge. Benzodiazepines have been commonly used as sedatives in critically ill patients. The pharmacokinetic and pharmacodynamic properties that make benzodiazepines effective and safe in critical care sedation include rapid onset of action and decreased respiratory depression. Alprazolam is a commonly used benzodiazepine that is prescribed for anxiety and panic disorders. It is frequently prescribed in the outpatient setting. Its use has been reported to result in a relatively high rate of dependence and subsequent withdrawal symptoms. Symptoms of alprazolam withdrawal can be difficult to recognize and treat in the critical care setting. In addition, other benzodiazepines may also be ineffective in treating alprazolam withdrawal. We present a case of alprazolam withdrawal in a critically ill trauma patient who failed treatment with lorazepam and haloperidol. Subsequent replacement with alprazolam resulted in significant improvement in the patient’s medication use and clinical status.
Core tip: Withdrawal from drugs and alcohol is a common phenomenon in the intensive care unit. Benzodiazepines are commonly used for both alcohol and benzodiazepine withdrawal. The pharmacokinetics and pharmacodynamics among drugs within this class vary. The failure of lorazepam to treat withdrawal of alprazolam is demonstrated in this case study.
- Citation: Sachdev G, Gesin G, Christmas AB, Sing RF. Failure of lorazepam to treat alprazolam withdrawal in a critically ill patient. World J Crit Care Med 2014; 3(1): 42-44
- URL: https://www.wjgnet.com/2220-3141/full/v3/i1/42.htm
- DOI: https://dx.doi.org/10.5492/wjccm.v3.i1.42
Benzodiazepines have been commonly used as sedatives in critically ill patients and also used extensively in the treatment of depression, anxiety, and panic disorders[1]. Key pharmacokinetic and pharmacodynamic properties of benzodiazepines include a rapid onset of action, decreased respiratory depression, higher ratio of lethal dose to effective dose, and a greater therapeutic dose margin between anxiolysis and sedation.
Alprazolam is a commonly used benzodiazepine for anxiety and panic disorders. It has been reported to have a relatively high occurrence of dependence and withdrawal symptoms[2,3]. Symptoms of alprazolam withdrawal can be difficult to recognize and treat in the critical care setting. In addition, other benzodiazepines may be ineffective in treating alprazolam withdrawal. We present a case of alprazolam withdrawal in a critically ill trauma patient who failed treatment with lorazepam.
A 28-year-old male was involved in a motor vehicle crash. After assessment and stabilization in the trauma bay he was noted to have an altered level of consciousness, mild traumatic brain injury with small subarachnoid hemorrhage, grade II splenic laceration and ethanol level of 221 mg/dL. The patient required emergent splenic artery embolization for a decreasing hematocrit. Subsequently, he was admitted to the trauma intensive care unit and started on an alcohol withdrawal protocol which included lorazepam administered on an as needed symptom-directed schedule.
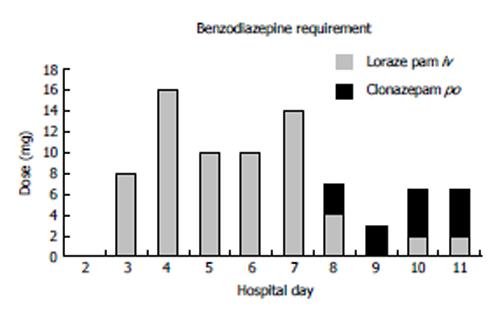
By hospital day 3, the patient became extremely agitated requiring multiple doses of intravenous lorazepam (2 mg times four doses) (Figure 1). Over the next 5 d, the patient required escalating doses of lorazepam to control his agitation (2 mg 6-7 times per day). Symptoms necessitating pharmacologic intervention included tachycardia, hypertension, confusion, slurred speech and pulling of his catheter and naso-enteric feeding tube.
On hospital day 8, a family member reported that the patient takes alprazolam 1 mg by mouth three times daily as a home medication. Following discussion with the clinical pharmacist member of the multi-professional critical care team, the patient was immediately started on clonazepam 1 mg three times a day. Following the first dose of clonazepam at noon, the patient received only one as needed dose of lorazepam that evening. On hospital day nine, no as needed lorazepam doses were required and only one was administered on hospital day 10. Despite an improving mental status, the patient remained confused. Thus, lorazepam was discontinued and the clonazepam dose was increased to 1.5 mg three times daily. On hospital day eleven, the patient again became acutely agitated and received lorazepam and multiple doses of haloperidol. By hospital day thirteen, his clonazepam was increased to 2 mg three times a day. The patient was less agitated and was transferred to an intermediate care unit.
Although improved, the patient remained restless and intermittently agitated. He required haloperidol 3 mg three times a day to control his agitation. Over the next 2 wk, the patient did not require any as needed benzodiazepines or haloperidol for acute agitation. The scheduled haloperidol was tapered and discontinued by discharge at hospital day 25. The clonazepam dose was tapered by 50% each week, and the patient was discharged to a rehabilitation facility on clonazepam 0.5 mg twice daily.
In comparison to other benzodiazepines, alprazolam may be associated with a higher propensity for addiction and result in more severe withdrawal symptoms. The prevalence of rebound anxiety is higher with benzodiazepines that have a short to intermediate half-life compared to those with a long half-life[4,5]. The effectiveness of other benzodiazepines at treating alprazolam withdrawal has been studied. The triazole ring found in alprazolam may have a significantly greater binding affinity for a subgroup of benzodiazepine receptors in areas of the brain that are not generally influenced by other benzodiazepines[6]. A review of eight case reports of alprazolam withdrawal published between 1984 and 1986 combined with six unpublished cases reported to the manufacturer provide early evidence of unique properties related to this agent. Chlordiazepoxide and diazepam were both found to be ineffective in preventing withdrawal symptoms in two separate cases. This review has been cited as providing clinical evidence to suggest that there is incomplete cross-tolerance between alprazolam and other benzodiazepines[7]. More recent review has shown that despite over prescription of benzodiazepines, withdrawal and dependence can be reduced by shorter duration prescriptions and withdrawal can be prevented by judicious weaning[8].
Differentiating withdrawal symptoms from pre-hospital substance use from those associated with the physiologic response to trauma can be difficult in critically ill patients since they are similar. In this patient, confusion, slurred speech, restlessness, and hypertension were thought to be related to alcohol withdrawal and tachycardia was presumed to be a presenting sign of a splenic bleeding. Although the patient was appropriately started on a symptom-directed alcohol withdrawal protocol at the time of admission, lorazepam was not effective in abating his agitation.
Lorazepam was clearly ineffective in treating this patient’s alprazolam withdrawal. This is consistent with a previous report of a critically ill patient who exhibited alprazolam withdrawal despite large doses of lorazepam and diazepam[9]. Initiation of clonazepam on hospital day eight was associated with a reduction in lorazepam requirements (Figure 1). Although clonazepam was used, it is likely that alprazolam would have also been effective as a rapid response is often observed with reinstitution of the drug[4,5]. Clonazepam was chosen because it has an intermediate to long half-life ranging from 17-60 h and is associated with less rebound anxiety and withdrawal symptoms in comparison to shorter acting agents such as alprazolam[4,5]. Furthermore, it has been used successfully for the management of alprazolam detoxification. This substitution in alprazolam-dependent patients has been shown to be safe and effective[5,10].
Given the unique characteristics and pharmacodynamics properties of alprazolam, reinstitution of this medication or substitution with clonazepam on a milligram per milligram basis are the preferred management strategies for trauma patients admitted with a history of pre-hospital alprazolam use to prevent withdrawal. Furthermore, consideration should be given to the high potential for therapeutic failure of other benzodiazepines in this patient population. This approach may prevent confusion with physiologic responses to injury and reduce the overall benzodiazepine requirement. This report highlights the need for obtaining an accurate medication history, as well as recognizing the physiologic effects related to injury, substance withdrawal, and medication administration. As such, we recommend a multi-professional approach with input from physicians, nurses, and clinical pharmacists to optimize these processes.
The authors present a case of alprazolam withdrawal in a critically ill trauma patient who failed treatment with lorazepam and haloperidol.
After assessment and stabilization in the trauma bay he was noted to have an altered level of consciousness, mild traumatic brain injury with small subarachnoid hemorrhage, grade II splenic laceration and ethanol level of 221 mg/dL.
The patient required emergent splenic artery embolization for a decreasing hematocrit.
The patient was admitted to the trauma intensive care unit and started on an alcohol withdrawal protocol which included lorazepam administered on an as needed symptom-directed schedule.
It has been used successfully for the management of alprazolam detoxification. This substitution in alprazolam-dependent patients has been shown to be safe and effective.
This report highlights the need for obtaining an accurate medication history, as well as recognizing the physiologic effects related to injury, substance withdrawal, and medication administration.
The authors well explained the failure of lorazepam to treat alprazolam withdrawal. This manuscript reports a case report on failure of lorazepam to treat alprazolam withdrawal in a critically ill trauma patient. The reason for this was well explained. Clonazepam was effective in the patient.
P- Reviewer: Lee MG S- Editor: Zhai HH L- Editor: A E- Editor: Liu SQ
| 1. | Barr J, Fraser GL, Puntillo K, Ely EW, Gélinas C, Dasta JF, Davidson JE, Devlin JW, Kress JP, Joffe AM. Clinical practice guidelines for the management of pain, agitation, and delirium in adult patients in the intensive care unit. Crit Care Med. 2013;41:263-306. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2333] [Cited by in RCA: 2409] [Article Influence: 200.8] [Reference Citation Analysis (0)] |
| 2. | Klein E. The role of extended-release benzodiazepines in the treatment of anxiety: a risk-benefit evaluation with a focus on extended-release alprazolam. J Clin Psychiatry. 2002;63 Suppl 14:27-33. [PubMed] |
| 3. | Trevor AJ, Way WL. Sedative-hypnotic drugs. Basic and Clinical Pharmacology, 6th edition. East Norwalk, CT: Appleton & Lange 1995; 333-349. |
| 4. | Chouinard G. Issues in the clinical use of benzodiazepines: potency, withdrawal, and rebound. J Clin Psychiatry. 2004;65 Suppl 5:7-12. [PubMed] |
| 5. | Patterson JF. Withdrawal from alprazolam dependency using clonazepam: clinical observations. J Clin Psychiatry. 1990;51 Suppl:47-49; discussion 50-53. [PubMed] |
| 6. | Browne JL, Hauge KJ. A review of alprazolam withdrawal. Drug Intell Clin Pharm. 1986;20:837-841. [PubMed] |
| 7. | Albeck JH. Withdrawal and detoxification from benzodiazepine dependence: a potential role for clonazepam. J Clin Psychiatry. 1987;48 Suppl:43-49. [PubMed] |
| 8. | Ashton H. The diagnosis and management of benzodiazepine dependence. Curr Opin Psychiatry. 2005;18:249-255. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 272] [Cited by in RCA: 253] [Article Influence: 12.7] [Reference Citation Analysis (0)] |
| 9. | Freda JJ, Bush HL, Barie PS. Alprazolam withdrawal in a critically ill patient. Crit Care Med. 1992;20:545-546. [PubMed] |
| 10. | Patterson JF. Alprazolam dependency: use of clonazepam for withdrawal. South Med J. 1988;81:830-831, 836. [PubMed] |