Published online Sep 9, 2025. doi: 10.5492/wjccm.v14.i3.103402
Revised: February 26, 2025
Accepted: April 1, 2025
Published online: September 9, 2025
Processing time: 242 Days and 18.9 Hours
In recent years, the utilization of telemedicine in emergency situations, parti
To compare the effectiveness of video-instructed DA-CPR and audio-instructed DA-CPR in terms of survival rates to hospital discharge.
We conducted a comprehensive search of electronic databases, including Pub
Our research strategy yielded 537 references. After the final analysis, we selected 27 articles from the PubMed database that met our inclusion criteria. The mean age of the included participants was 37.1 years. The study presents compelling evidence in favor of video-instructed DA-CPR, showing a significant improve
DA-CPR plays a crucial role in the chain of survival for out-of-hospital cardiac arrest patients. Extensive research has consistently demonstrated its effectiveness in increasing bystander-initiated CPR and improving patient outcomes. Ongoing technological advancements, such as video calls and automated external defibrillator in
Core Tip: This systematic review provides an in-depth analysis of the effectiveness of video-assisted cardiopulmonary resuscitation (CPR) compared to audio-assisted CPR. The findings conclude that video-assisted dispatcher CPR significantly enhances the quality of chest compressions and improves survival to hospital discharge. However, the implementation of video-assisted CPR may lead to delays in initiating compressions by dispatchers and presents challenges such as the need for reliable technological infrastructure and comprehensive dispatcher training.
- Citation: Hussain S, Soldera J. Telemedicine in cardiac arrest protocols: Comparative impact of video and audio dispatcher assistance. World J Crit Care Med 2025; 14(3): 103402
- URL: https://www.wjgnet.com/2220-3141/full/v14/i3/103402.htm
- DOI: https://dx.doi.org/10.5492/wjccm.v14.i3.103402
Cardiopulmonary resuscitation (CPR) is a life-saving intervention used when an individual’s heart stops or beats irregularly. Dispatcher-assisted CPR (DA-CPR) is crucial in delivering prompt and adequate instructions to bystanders amidst these high-stress situations[1]. The dispatcher, frequently a skilled medical professional, directs the bystander through CPR steps until professional assistance arrives. While audio instructions have traditionally been the standard for delivering DA-CPR guidance, recent studies investigate the potential advantages of incorporating video-based in
The efficacy of DA-CPR relies on the dispatcher’s ability to deliver clear, accurate, and easily understandable in
The transition to video-based instruction in DA-CPR is grounded in acknowledging that visual information can significantly improve the comprehension and retention of intricate tasks[6,7]. Although audio instructions remain invaluable, particularly in scenarios without visual cues, video instruction introduces an extra dimension of clarity and precision. Visual cues allow bystanders to grasp the accurate hand placement, compression technique, and rhythm, offering a more tangible and intuitive understanding of the life-saving procedure[8,9]. Furthermore, video instruction in DA-CPR can potentially alleviate the risks of misinterpretation or miscommunication often associated with audio-only guidance. Challenges such as language barriers, background noise, or high-stress environments may impede the precise communication and understanding of verbal instructions. In contrast, video instructions overcome linguistic barriers by providing a universally comprehensible visual representation of the CPR process[7,10,11].
This research not only delves into the comparative effectiveness of video and audio instruction in DA-CPR scenarios but also prompts a more extensive exploration of the role of technology in enhancing emergency response protocols. With ongoing advancements in communication technology, seamlessly integrating video-based instruction into emergency medical services (EMS) procedures becomes increasingly plausible. However, a comprehensive assessment of potential logistical challenges is essential, ensuring that the advantage of these technological enhancements significantly outweighs any potential drawbacks. Recent developments in research are beginning to illuminate the comparative efficacy of video and audio instructions in the context of DA-CPR scenarios. This systematic review aims to provide persuasive evidence supporting video-instructed DA-CPR, indicating a noteworthy disparity in survival rates to discharge compared to audio instructions.
The following systematic review was performed in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analysis guidelines[12]. In October 2023, a search was conducted in the electronic database PubMed/Medline using the following command: (“cardiac arrest” OR “arrest call” OR “arrest team”) AND (“telemedicine” OR “video” OR “telecardiology”). Medical Subject Headings terms, and Boolean operators for comprehensive retrieval of relevant literature.
Studies that estimated the impact of DA-CPR guidance through video instruction or audio instruction on the quality of CPR performed were included. The research question was designed using a Population Intervention Comparator Outcomes strategy: (1) Population: Bystanders performing CPR in both real-life situations and simulated environments; (2) Video-instructed DA-CPR; (3) Audio-instructed DA-CPR; and (4) Quality of chest compression, time-related quality parameters, correct hand positioning during CPR, survival to hospital discharge, perception of stiffness, and good neurological outcome at hospital discharge.
The studies included were either randomized clinical trials or case-control studies. Exclusion criteria included studies that did not report data or measures for our selected outcomes, studies focusing on telephonic assisted call arrest pro
After excluding duplicates, two authors independently reviewed the titles and abstracts of all potentially relevant citations. Subsequently, a thorough assessment of the complete texts was conducted to determine their suitability for inclusion in the systematic review. Any disagreements were resolved between the authors.
Two authors independently recorded the relevant data into an Excel spreadsheet, including baseline characteristics and demographic information of the study populations, outcomes measured such as quality of chest compression, time-related quality parameters, correct hand positioning during CPR, survival to hospital discharge, and perception of stiffness, and good neurological outcome at hospital discharge, and details about the assessment of the risk of bias.
Two investigators evaluated bias risk independently, verifying the results through cross-checking. The evaluation followed the guidelines outlined in the Cochrane Handbook version 5.1.0 for assessing bias risk in the included trial. Other designs were evaluated using the National Heart, Lung, and Blood Institute tool.
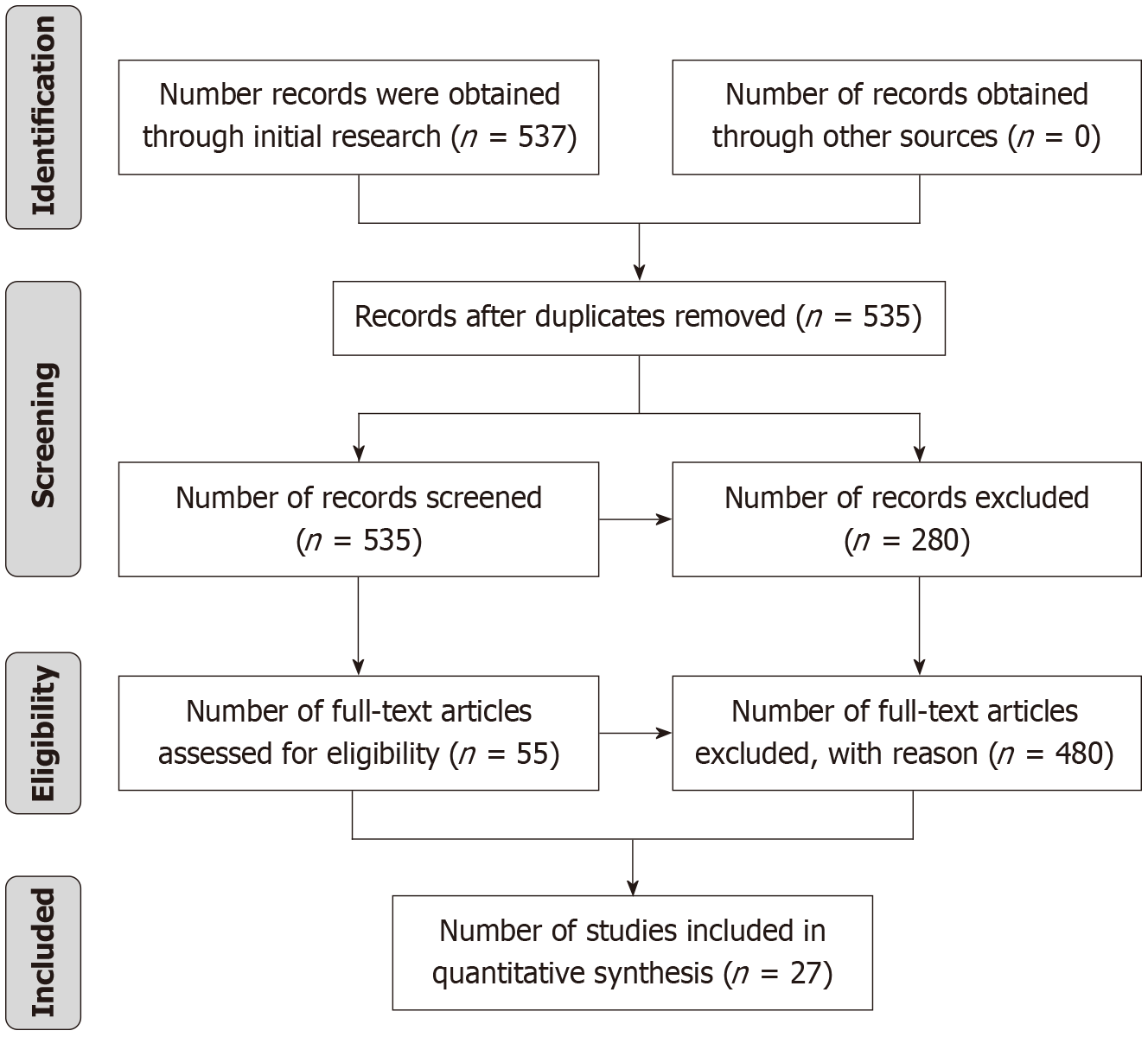
The search command was run on October 28th 2023 and retrieved 537 references conducted on the. Following an initial assessment, two duplicate studies were excluded. Subsequently, a preliminary screening of titles and abstracts excluded 480 references due to not meeting the inclusion criteria. This entire process is visually represented in Figure 1 with a Preferred Reporting Items for Systematic Reviews and Meta-Analysis guidelines diagram. Ultimately, 27 articles aligned with the inclusion criteria and were assimilated into the systematic review.
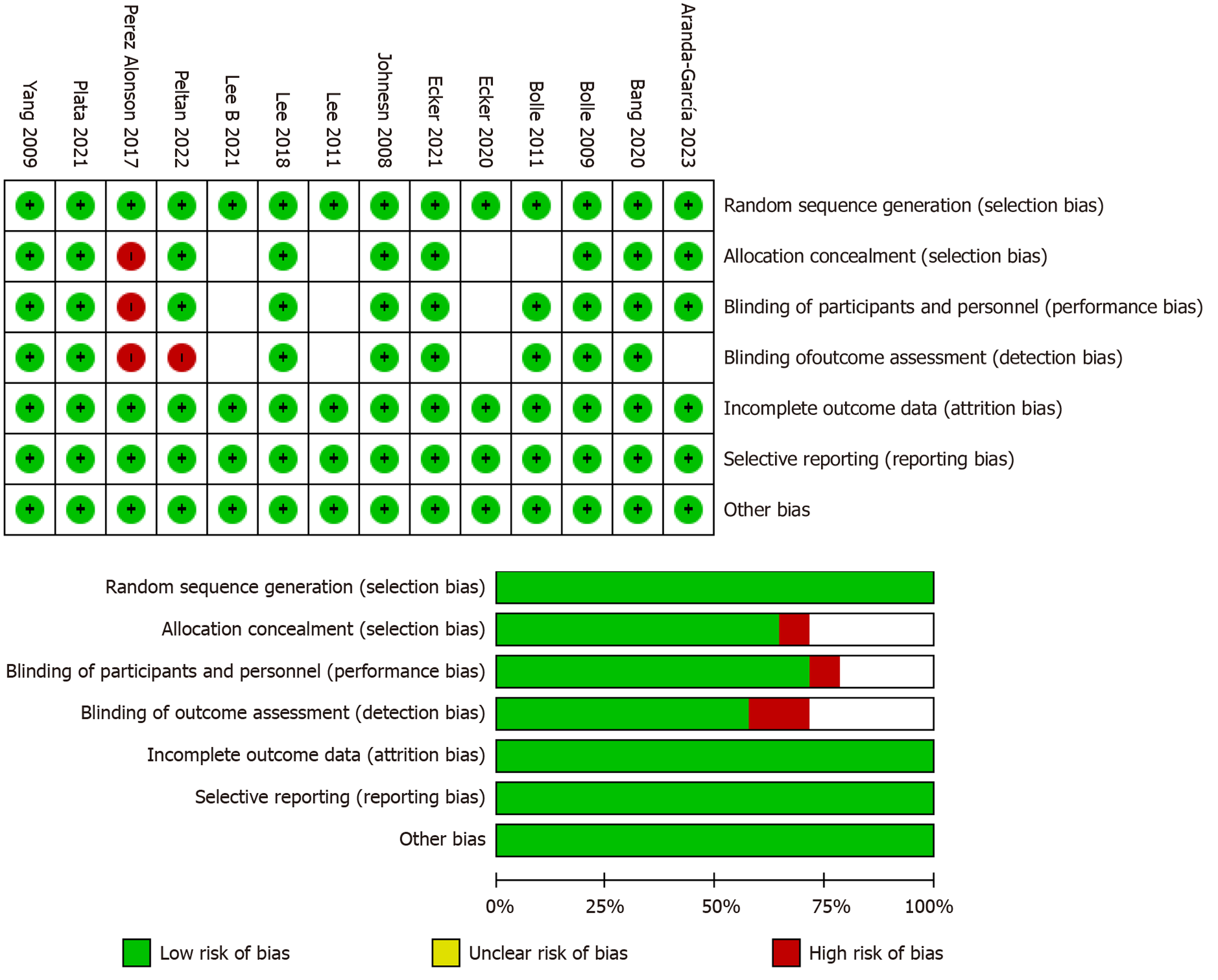
Bias was meticulously evaluated in the incorporated studies is assessed using the Cochrane risk bias tool for randomized controlled trials[13] and is graphically portrayed in Figure 2. Among the fourteen randomized control trials scrutinised, the majority exhibited low risks in domains of selection, attrition, reporting, and other biases. However, aberrancies were noted[14,15], which demonstrated elevated risks of selection, performance, and detection biases, vi
During the compilation of results, a few different themes emerged one being the provision of CPR through telematics such as Google glasses (GGs)[14], which showed promising results with a 100% successful defibrillation rate achieved through wearable technology. Similarly, the comparative analysis between smart glasses-video assistance (SG-VA) and smartphone-audio assistance in basic life support (BLS) tasks revealed significant enhancements with SG-VA[16]. The study concluded statistically significant results in SG-VA groups across the BLS metric such as including protocol completion, airway management, breathing assessment, automated external defibrillator (AED) pad placement, and bystander communication. Another pilot simulation study assessed the feasibility of smart glasses in providing BLS and operating an AED to fishermen in a simulated out-of-hospital cardiac arrest (OHCA) on the boat[17]. The largest difference was found in the variable “correct hand position during cardiac compressions”, with 33% incorrect hand position during CPR according to the on-scene instructor, while the dispatcher considered it correct in 100% of the par
The second theme prevalent through the systematic review was the use of smartphones in providing effective CPR vs conventional audio assistance and the effects of video quality on the provision of effective CPR in life-threatening medical emergencies. Plata et al’s research[18] on video-assisted CPR underscored the significance of video quality, suggesting that even low-quality video may facilitate accurate CPR evaluations. Whereas another study emphasized the importance of standardized filming protocols for effective CPR, indicating that live video communications could enhance chest compressions compared to telephone-instructed CPR protocols[19]. Moreover, a few studies investigated the effect of CPR through cellular phone livestream instruction by EMS and concluded that the live stream feature helps in the identification of correct and incorrect compression frequency, compression depth, and compression point by EMS dispatching staff during telephone-assisted CPR (T-CPR)[20]. On the other hand, a similar study compared the CPR performance between VA-CPR and audio coaching, which showed Video coaching improved CPR performance in terms of com
Nonetheless, these findings collectively delineate the diverse landscape of technological interventions in CPR and defibrillation, each presenting distinct advantages and limitations in improving patient outcomes. The mean age of participants included in the review was 37.1 years. Tables 1-3[7-9,14-35] provides comprehensive insights into the indi
| Ref. | Ecker et al[20], 2020 | Perry et al[19], 2020 | Johnsen et al[24], 2008 | Lee et al[11], 2011 | Peltan et al[15], 2022 | Lee et al[9], 2021 | Sonkin et al[21], 2022 | Meinich-Bache et al[25], 2018 | Kim et al[8], 2021 | |||||||||
| Comparators | Video | Audio | Control | Video | Audio | Filming | Video | Video | Audio | Telemedicine | Control | Video | Audio | Video | Video | Smartphone | BLS | |
| Country | Germany | Israel | Norway | South Korea | United States | South Korea | Israel | Norway | South Korea | |||||||||
| Study period | 2018-2020 | 2018-2019 | 2006-2007 | May 2010 to June 2010 | 2017-2018 | 2018-2019 | 2020-2021 | 2017-2018 | 2015-2016 | |||||||||
| Study design | Randomised controlled simulation trial | A simulation study | A simulation study | Randomised controlled simulation trial | Multicenter randomized controlled trial | Retrospective cohort study | A Simulation study | A Simulation study | Retrospective cohort study | |||||||||
| Sample size | 50 | 50 | 50 | 14 | 17 | 18 | 6 | 39 | 39 | 35 | 36 | 387 | 1722 | 43 | 19 | 199 | 417 | |
| Participants | Adult volunteers | Medical technicians | Dispatchers | Adult volunteers | Physician | adult patients with OHCA | Active paramedics | Bystander and dispatcher | Adult patients with OHCA | |||||||||
| Inclusion criteria | Adult volunteers were recruited from the streets surrounding the hospital. Exclusion criteria included age less than 18 and more than 65 years, healthcare providers (medical practitioners, nurses, paramedics), pregnancy, cardiovascular or musculoskeletal diseases, or any other medical condition preventing performance of CPR over 8 minutes | Twenty-five emergency medical technicians acted as EMDs in the three conditions. A mannequin measured five factors that determined the effectiveness of the chest compressions | All had previously assisted CPR in their ordinary work. None of them had used video for dispatcher instructions prior to the trials | The volunteers were lay people without any previous CPR training. The subjects who had difficulty performing compression-only CPR due to their physical condition, those who were not familiar with cellularphone usage and those who had difficulty watching a video on a cellular phone due to poor vision were excluded from the study | All personnel involved in ward-based IHCA resuscitation at each study site were eligible to participate in the study. Composition and training of these ad hoc resuscitation teams varied by study site | After excluding unknown, nonbystander-witnessed arrest cases, and EMS-witnessed arrests cases (n = 2648), presumed non-cardiac etiology (n = 256), and pediatric cases (n = 28), 2109 cases were eligible for the final analysis | Active paramedics at MDA ambulance teams at the time of the study | No specefic criteria | We include adult patients (n = 18) with OHCA of medicalcauses and EMS-attended and dispatchedin. SALS isanadvanced field resuscitation including drug administration by paramedics with video communication-based direct medical direction | |||||||||
| Age (years) | 32.92 (12.5) | 37.6 (13.9) | 36.7 (13.9) | NR | NR | NR | 33.5 | 56.6 ± 7.2 | 55.3 ± 6.2 | NR | NR | 64.9 ± 16.2 | 72.2 ± 14.7 | NR | NR | NR | 82 (77-87) | 80 (72-86) |
| BMI (kg/m2) | 24.2 (5.7) | 23.7 (3.6) | 23.4 (3.7) | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR |
| Male | 19 (38) | 15 (30) | 13 (26) | NR | NR | NR | 1 | 20 (51.3) | 19 (48.7) | NR | NR | 263 (68) | 1087 (63.1) | 30 (70) | NR | NR | 79 (39.7) | 207 (49.6) |
| Female | 31 (62) | 35 (70) | 37 (74) | NR | NR | NR | 5 | 19 (48.7) | 20 (51.3) | NR | NR | 124 (32.0) | 635 (36.9) | 13(30) | NR | NR | 120 (60.3) | 210 (50.4) |
| Has provided CPR | 1 (2) | 1 (2) | 1 (2) | NR | NR | NR | NR | 39 | 39 | NR | NR | NR | NR | 32 | NR | NR | NR | NR |
| Witnessed an emergency | 5 (10) | 8 (16) | 6 (12) | NR | NR | NR | NR | 39 | 39 | NR | NR | NR | NR | 32 | NR | NR | NR | NR |
| Had first aid course | 47 (94) | 47 (94) | 50 (100) | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | 32 | NR | NR | NR | NR |
| Ref. | Linderoth et al[22], 2021 | Ofoma et al[26], 2022 | Plata et al[18], 2021 | Lee et al[27], 2021 | Aranda-García et al[16], 2023 | Pérez Alonso et al[14], 2017 | Lee et al[28], 2020 | Ecker et al 2021[35] | Yang et al[29], 2009 | ||||||||
| Comparators | Video | Telemedicine | No telemedicine | Video | V-DACPR with rapid transition | V-DACPR with delayed transition | C-DACPR | Video | Audio | GG | Control | Video | Audio | Audio and video telephony | Video | Audio | |
| Country | Denmark | United States | Germany | South Korea | Spain | Spain | Seoul, South Korea | Germany | Taiwan | ||||||||
| Study period | 2019-2021 | July 1, 2017, and December 31, 2019 | September 2019 to February 2020 | October 2019 to July 2020 | 2021-2022 | November 2014 to July 2015 | 2017 | August to September 2018 | 2009 | ||||||||
| Study design | Retrospective study | A prospective, voluntary, multi-site registry of IHCA | Randomised controlled simulation trial | Randomised controlled simulation trial | Randomised controlled simulation trial | Randomised clinical simulation | Retrospective cohort | Prospective randomized pilot | Randomized controlled study | ||||||||
| Sample size | 90 | 14373 | 30212 | 93 | 43 | 45 | 43 | 14 | 14 | 36 | 36 | 231 | 1489 | 54 venues with realistic full-scale CPR mannequin | 43 | 53 | |
| Participants | Bystander | Adult patients | Paramedics and emergency physicians | Bystander | Adult volunteers | Nurse | Emergency medical technicians | Bystander | Volunteers (bystander) | ||||||||
| Inclusion criteria | The training included simulation-based scenarios with unconscious patients and cardiac arrest cases with a focus on high-quality CPR with simultaneously real-time guidance (video-instructed DA-CPR) | We identified 70881 patients 18 years or older with an index pulseless IHCA between July 1, 2017, and December 31, 2019. We excluded arrests at hospitals that did not respond to the AHA surveys or had missing information on TCC availability; at hospitals with less than 10 cardiac arrests over the study period; that occurred outside of an ICU or hospital ward (e.g., emergency room and operating room); and in patients with an implantable cardioverterdefibrillator. Additionally, we excluded patients with missing information related to arrest time or survival | No specefic criteria | Volunteers aged 18 years or older were recruited for the simulation trial from October 2019 to July 2020. Healthcare providers, and participants with chronic lung diseases, cardiovascular diseases, visual disabilities, or hearing disabilities were excluded during initial enrollment. Written consent was obtained from all participants | Inclusion criteria were no theoretical or practical training on BLS in the previous 2 years | Training in BLS in the last 2 years and a minimum of 2 years of professional experience in emergency services as well as familiarity with the use of AED and the ALS | OHCA patients with a presumed cardiacetiology who were more than 18 years of age between January and December 2017 | NR | Ninety-six adults without CPR training within 5 years were recruited | ||||||||
| Age (years) | 21.25 (11.17) | 65.5 (15.4) | 65.6 (15.1) | NR | 30.5 (12.0) | 29.1 (10.2) | 30.8 (12.1) | 23 | 23 | 33 ± 8 | 32 ± 7 | NR | NR | NR | NR | 50.1 ± 11.5 | 50.4 ± 12.7 |
| BMI (kg/m2) | NR | NR | NR | NR | NR | NR | NR | 22.5 | 22.1 | NR | NR | NR | NR | NR | NR | NR | NR |
| Male | 50 | 8500 (59.1) | 17724 (58.7) | NR | 10 | 11 | 9 | 14 | 14 | 39% | 28% | NR | NR | NR | NR | NR | NR |
| Female | 40 | 5873 (40.9) | 12488 (41.3) | NR | 33 | 34 | 34 | 0 | 0 | 61% | 72% | NR | NR | NR | NR | NR | NR |
| Has provided CPR | 52 | NR | NR | 93 | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | 4 (70) | 1 (90) |
| Witnessed an emergency | 29 | NR | NR | 93 | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | - | - |
| Had first aid course | 48 | NR | NR | 93 | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | 18 (60) | 18 (90) |
| Ref. | Morand et al[30], 2023 | You et al[31], 2008 | Barcala et al[17], 2023 | Bolle et al[7], 2011 | Bang et al[32], 2020 | Bolle et al[33], 2009 | Kim et al[8], 2021 | Yuksen et al[23], 2016 | Lee et al[34], 2018 | |||||||||
| Comparators | Video | Video telephony-directed | Video calls | Video | Audio | Video | Audio | Non-guide | Video | Audio | Video | Voice | Physicians | EMT | Video | |||
| Country | Switzerland | South Korea | Spain | Norway | South Korea | Norway | South Korea | Thailand | South Korea | |||||||||
| Study period | 2021 | 2008 | 2021 | 2011 | Jun-19 | December 2006 and January 2007 | 2020 | 2014 | July to November 2015 | |||||||||
| Study design | NR | A prospective observational study | Descriptive and comparative design | Randomized controlled trial | Prospective randomized simulation | Clinical trial | Mixed method design | Retrospective study | Randomized trial | |||||||||
| Sample size | 28 | 52 public officers | 16 | 90 | 90 | 30 | 30 | 30 | 180 | 12 | 12 | 14 | 14 | 28 | 48 | 48 | ||
| Participants | Bystander | Public officers | Coastal fshermen | High school students | Laypersons | High school students | NR | Physicians, nurses and EMT | Paramedics | |||||||||
| Inclusion criteria | NR | No previous experience with the use of a defibrillator participated in the study | Professional fishermen with at least 10 years of experience (to ensure fully familiar with the boat and with performing tasks while sailing) who had not undergone BLS training in the previous 6 months | High school students from Tromso were recruited as lay bystanders during regular school hours | Adult college students (age ≥ 18 years) and selected 90 participants who did not have formal training, such as the AHA BLS course, in CPR and AED | The study population was selected during regular school hours without prior warning | NR | NR | NR | |||||||||
| Age (years) | NR | NR | 32.7 ± 6.8 | 46 ± 4 | 17.3 | 17.9 | 22.5 (22.0-26.25) | 22.0 (22.0-23.0) | 26 (23.0-25.0) | 17.3 | 17.9 | 22.33 ± 1.67 | 22.42 ± 1.98 | 27.64 ± 2.56 | 30.64 ± 4.29 | 29.68 ± 7.013 | 33 (27-42) | 32 (25-43) |
| BMI (kg/m2) | NR | NR | - | - | - | - | - | - | - | 23.4 ± 5.1 | 23.9 ± 4.8 | |||||||
| Male | NR | NR | 69 (20) | 100% | 27% | 34% | 43 (30) | 36 (70) | 40% | 27% | 34% | 58 (30) | 33 (30) | 50% | 42 (90) | 82% | 70 (80) | 67 (40) |
| Female | NR | NR | 30 (80) | 0% | 73% | 66% | 56 (70) | 63 (30) | 60% | 73% | 66% | 41 (70) | 66 (70) | 50% | 57 (10) | 18% | 29 (20) | 32 (60) |
| Has provided CPR | NR | NR | - | - | - | 83 (30) | 70% | 76 (70) | - | - | 28 (60) | 7 (10) | 14 (30) | - | ||||
| Witnessed an emergency | NR | NR | - | - | - | - | - | - | - | - | ||||||||
| Had first aid course | NR | NR | - | - | 73% | 71% | - | - | - | - | - | |||||||
| Ref. | Design | Intervention | Results | Conclusion |
| Ecker et al[20], 2020 | Randomized controlled simulation trial | The participants received a smartphone to call emergency services, with emergency eye video-call in V-CPR group and normal telephone functionality in the other. Groups: T-CPR and V-CPR groups received standardized CPR assistance via phone | Mean compression frequency of V-CPR group was 106.4, 11.7 minutes, T-CPR group 98.9, 12.3 minutes (NS), Unassisted group 71.6, 32.3 minutes (P < 0.001). Mean compression depth was 55.4, 12.3 mm in V-CPR, 52.1, 13.3 mm in T-CPR (P < 0.001) and 52.9, 15.5 mm. In unassisted (P < 0.001). Total percentage of correct chest. Compressions were significantly higher (P < 0.001) in V-CPR (82.6%), than T-CPR (75.4%) and unassisted (77.3%) groups | CPR was shown to be superior to unassisted CPR and was comparable to T-CPR. However, V-CPR leads to a significantly better hand position than other methods. With the other study groups. V-CPR assistance resulted in Volunteers performing chest compressions with more accurate compression depth. Despite reaching statistical significance, this may be of little clinical relevance |
| Perry et al[19], 2020 | A simulation study | A simulation study was conducted comparing CPR effectiveness under three conditions: Telephone-instructed, video-instructed, and video-instructed with the filming protocol | Compared with telephone-instructed CPR, the filming protocol improved the proportion of time in which the bystander’s hands were in the correct position during chest compressions. Compared with video-instructed CPR, the filming protocol improved the proportion of time in which the chest was fully released after each compression and the proportion. Of time in which the compressions were conducted with an appropriate rhythm. The depth and rate of compressions did not. Improve the filming protocol condition | Video-instructed CPR with the filming protocol improves CPR effectiveness compared to telephone- and Video-instructed CPR. Detailed implementation can improve new technology introduction |
| Johnsen et al[24], 2008 | A simulation study | They used video calls and traditional phone calls for the rest | Video calls influenced the information base and understanding of the dispatchers. The dispatchers experienced that (1) Video calls help obtain information and provide, adequate functionality to support CPR assistance; (2) Their CPR assistance becomes easier; (3) The CPR might be of better quality; but (4) There is a risk of ‘‘noise’’ | Video communication can improve the dispatchers’ understanding of the rescuers situation, and the assistance they provide |
| Lee et al[11], 2011 | Randomized controlled simulation trial | Adult volunteers were randomized to receive audio-assisted instructions (audio group = 39), or video-demonstrated instructions (video group = 39) | For the video group, the chest compression rate was more optimal (99.5 minutes vs 77.4 minutes, P < 0.01), and the time from the initial phone call to the first compressions was shorter (184 seconds vs 211 seconds, P < 0.01). The depth of compressions was deeper in the audio group (31.3 mm vs 27.5 mm, P = 0.21), but neither group performed the recommended compression depth. The hand positions for compression were more appropriate in the video group (71.8% vs 43.6%, P = 0.01). As many as 71.8% of the video group had no ‘hands-off’ events when performing compression (vs 46.2% for the audio group, P = 0.02) | Instructions from the dispatcher, along with a video demonstration of CPR, improved the time to initiate compression, the compression rate and the correct hand positioning. It also reduced the ‘hands-off’ events during CPR. However, emphasized instructions by video may be needed to increase. The depth of compressions |
| Peltan et al[15], 2022 | Multicenter randomized controlled trial | The telemedical consultant for intervention-group | No-flow fraction did not differ between the 36 intervention groups (0.22-0.13) and the 35 control group (0.19-0.10) resuscitation simulations were included in the intention-to-treat analysis (P ¼, 41). The etiology of the simulated cardiac arrest was identified more often during evaluable resuscitations supported by a telemedical intensivist consultant (22/32, 69%) compared with control resuscitations [10/34 (29%); P ¼, .001], but other measures of resuscitation quality, resuscitation team performance, and participant experience did not differ between intervention groups. Problems with audio quality or telemedicine. Connection affected 14 intervention group resuscitations (39%) | Consultation by a telemedical intensivist physician did not improve. Resuscitation quality during simulated ward-based IHCA |
| Lee et al[9], 2021 | Retrospective cohort study | Audio-instructed DA-CPR | Favorable neurologic outcome was observed more in patients who received video-instructed DA-CPR (n = 75, 19.4%) than in patients who received audio-instructed DA-CPR (n = 117, 6.8%). The survival to discharge rate was also higher in video-instructed DA-CPR (n = 105, 27.1%) than audio-instructed DA-CPR (n = 211, 12.3%) | Video-instructed DA-CPR was significant. Associated with neurologic recovery (aOR = 2.11, 95%CI: 1.48-3.01) and survival to discharge (aOR = 1.81, 95%CI: 1.33-2.46) compared to audio-instructed DA-CPR in adult OHCA patients after adjusting for age, gender, underlying diseases and CPR location. Video-instructed DA-CPR was associated with favorable outcomes in adult patients with OHCA in a metropolitan city equipped with sufficient experience and facilities |
| Sonkin et al[21], 2022 | A simulation study | Participants communicated with the experimenter, presenting video clips showing patients that simulated three emergency scenarios: Trauma, an unresponsive patient with cardiac arrest, and an opiate overdose | The trauma scenario was assessed most promptly, with instructions to handle the bleeding provided by all. Paramedics. In the unresponsive patient with cardiac arrest scenario, most of the participants achieved a correct initial. Diagnosis, and in the opiate overdose scenario, over half of the paramedics sought visual clinical clues for the differential. Diagnoses of loss of consciousness and their causes. Additional results show the type of assessment, treatment, and Diagnosis participants were provided in each scenario and their confidence about the situation. In the cardiac arrest scenario, the participants were assessed. the LOC in 41 (98%) sessions within a median of 1minute and 24 seconds (IQR: 00:41-02:33), evaluated breathing in 37 (88%) sessions within a median of 1 minute and 39 seconds (IQR: 00:54-03:14). The participants instructed the bystander to check central pulse in 10 (24%) sessions within a median of 3 minutes and 58 seconds (IQR: 03:06-05:20) - these participants were asked to measure the pulse only after the patient collapsed. Skin tone and sweating were assessed in 19 (45%) sessions within a median of 1 minute and 45 seconds (IQR: 01:06-02:28) and a list of the patient’s current Medications were requested in 10 (24%) sessions within a median of 2 minutes and 38 seconds (IQR: 01:25-03:17) | The findings show that direct video communication between paramedics and the scene may facilitate correct diagnosis, provision of instructions for treatment, and early preparation of medications or equipment. These may decrease time to correct diagnosis and lifesaving treatment, and impact patient morbidity and mortality. Moreover, the findings highlight the differences between incidents with higher visual clarity, such as trauma and conditions. Require an extended diagnosis to reveal, such as unresponsive patients. This may also increase the paramedics’ mental preparedness for what is expected at the scene |
| Meinich-Bache et al[25], 2018 | A simulation study | Smartphone video analysis in real-time is feasible for a range of conditions. With the use of a web-connected smartphone application which utilises the smartphone camera | Four experiments were performed to test the accuracy of the calculated chest compression rate. Under different conditions, a fifth experiment was done to test the accuracy of the CPR summary parameters TFSCR, TC, TWC, ACR, and NC. The average compression rate detection error was 2.7 compressions per minute (± 5.0 cpm), the calculated chest. The compression rate was within ± 10 cpm at 98% (± 5.5) of the time, and the average error of the summary CPR parameters was 4.5% (± 3.6) | Real-time chest compression quality measurement by smartphone cameras are feasible for a range of bystanders, compression rates, camera positions, and noise conditions. (Is technology may be used to measure and improve the quality of telephone CPR and minimising hands-off times) |
| Kim et al[8], 2021 | Retrospective cohort study | SALS | A total of 616 consecutive out-of-hospital cardiopulmonary resuscitation cases in NHs were recorded, and 199 (32.3%) underwent SALS. Among the NH arrest patients, the survival discharge rate was a little higher in the SALS group than in the BLS group (4.0% vs 1.7%), but the difference was not significant (P = 0.078). Survival discharge with good neurologic outcome rates was 0.5% in the SALS group and 1.0% in the BLS group (P = 0.119). On the other hand, in the non-NH group, all outcome measures significantly improved when SALS was performed compared to BLS alone (survival discharge rate: 10.0% vs 7.3%, P = 0.001; good neurologic outcome: 6.8% vs 3.3%, Pb 0001) | As a result of providing prehospital ACLS with direct medical intervention through remote video calls to paramedics, the survival to discharge rate and the good neurologic outcome (CPC 1, 2) of non-NH patients significantly improved; however, those of NH patients were not significantly increased |
| Linderoth et al[22], 2021 | Retrospective study | Live video of dispatcher-assisted CPR | CPR was provided with live video streaming in 52 OHCA calls, with 90 bystanders who performed chest compressions. Hand position was incorrect for 38 bystanders (42.2%) and improved for 23 bystanders (60.5%) after video-instructed DA-CPR. The compression rate was incorrect for thirty-six bystanders (40.0%) and improved for 27 bystanders (75.0%). Compression depth was incorrect for 57 bystanders (63.3%) and enhanced for 33 bystanders (57.9%). The adjusted odds ratios for improved CPR after video-instructed DA-CPR were hand position 5.8 (95%CI: 2.8-12.1), compression rate 77 (95%CI: 3.4-17.3), and compression depth 7.1 (95%CI: 3.9-12.9). Hands-o time was reduced for 34 | Live video streaming from the scene of a cardiac arrest to medical dispatchers is feasible. It allowed an opportunity for dispatchers to coach those providing CPR, which was associated with a subjectively evaluated improvement in CPR performance |
| Ofoma et al[26], 2022 | A prospective, voluntary, multi-site registry of IHCA | Telemedicine critical care | 14373 (32.2%) participants suffered IHCA at hospitals with TCC, and 27032 (60.6%) occurred in an ICU. There was no difference between TCC and non-TCC hospitals in acute resuscitation survival rate or survival to discharge rates for either IHCA occurring in the ICU (acute survival OR = 1.02; 95%CI: 0.92-1.15; survival to discharge OR = 0.94; 95%CI: 0.83-1.07) or outside of the ICU (acute survival OR = 1.03; 95%CI: 0.91-1.17); survival to discharge (OR = 0.99; 95%CI: 0.86-1.12). Timing of cardiac arrest did not modify the association between TCC availability and acute resuscitation survival (P = 0.37 for interaction) or survival to discharge (P = 0.39 for interaction) | Hospital availability of TCC was not associated with improved outcomes for in-hospital cardiac arrest |
| Plata et al[18], 2021 | Randomised controlled simulation trial | Telemedicine | No-flow fraction did not differ between the 36 intervention group (0.22-0.13) and the 35 control group (0.19-0.10) resuscitation simulations included in the intention-to treat analysis (P ¼ .41). The etiology of the simulated cardiac arrest was identified more often during evaluable resuscitations supported by a telemedical intensivist consultant (22/32, 69%) compared with control resuscitations [10/34 (29%); P ¼ .001], but other measures of resuscitation quality, resuscitation team performance, and participant experience did not differ between intervention groups. Problems with audio quality or the telemedicine connection affected 14 intervention group resuscitations (39%) | Consultation by a telemedical intensivist physician did not improve resuscitation quality during simulated ward-based IHCA |
| Lee et al[27], 2021 | Randomised controlled simulation trial | Video call-based DACPR (V-DACPR) compared to conventional DACPR | The simulation results of 131 volunteers were analysed. The mean proportion of adequate hand positioning was highest in V-DACPR with rapid transition (V-DACPR with rapid transition vs C-DACPR: 92.7% vs 82.4%, P = 0.03). The mean chest compression depth was deeper in both V-DACPR groups than in the C-DACPR group (V-DACPR with rapid transition vs C-DACPR: 40.7 mm vs 35.9 mm, P = 0.01, V-DACPR with delayed transition vs C- DACPR: 40.9 mm vs 35.9 mm, P = 0.01). Improvement in the proportion of adequate hand positioning was observed in the V-DACPR groups (r = 0.25, P < 0.01 for rapid transition and r = 0.19, P < 0.01 for delayed transition) | Participants in the V-DACPR groups performed higher quality chest compression with higher appropriate hand positioning and deeper compression depth than the C-DACPR group |
| Aranda-García et al[16], 2023 | Randomised controlled simulation trial | A SG-VA intervention group or a SP-AA control group | Nine of the 14 SG-VA rescuers correctly completed the BLS protocol compared with none of the SP-AA rescuers (P = 0.01). A significantly higher number of SG-VA rescuers successfully opened the airway (13 vs 5, P = 0.002), checked breathing (13 vs 8, P = 0.03), correctly positioned the automatic external defibrillator pads (14 vs 6, P = 0.001), and warned bystanders to stay clear before delivering the shock (12 vs 0, P < 0.001). No significant differences were observed for performance times or chest compression quality. The mean compression rate was 104 compressions per minute in the SG-VA group and 98 in the SP-AA group (P = 0.46); the mean compression depth was 4.5 cm and 4.4 cm (P = 0.49), respectively | Smart glasses could significantly improve dispatcher-assisted bystander performance in an OHCA event. Their potential in real-life situations should be evaluated |
| Pérez Alonso et al[14], 2017 | Randomised clinical simulation | GG/control | Thirty-six nurses were enrolled in each study group. Statistically significant differences were found in the percentages of successful defibrillation (100% GG vs 78% control; P = 0005) and CPR completion times: 213.91 seconds for GG and 250.31 seconds for control (average difference = 36.39 seconds (95%CI: 12.03-60.75), P = 0.004) | Telematics support by an expert through GG improves success rates and completion times while performing CPR in simulated clinical situations for nurses in simulated scenarios |
| Lee et al[28], 2020 | Retrospective cohort | Audio-instructed DA-CPR vs video-instructed DA-CPR | A total of 1720 eligible OHCA patients (1489 and 231 in the audio and video groups, respectively) were evaluated. The median ITI was 136 seconds in the audio group and 122 seconds in the video group (P = 0.12). The survival to discharge rates were 89% in the audio group and 14.3% in the video group (P < 0.01). Good neurological outcomes occurred in 5.8% and 10.4% of the audio and video groups, respectively (P < 0.01). Compared to the audio group, the AORs (95%CIs) for survival to discharge, good neurological outcome, and early ITI of the video group were 120 (0.741, 94), 1.28 (0.732, 26) and 1.00 (0.701, 43), respectively. The PSM population showed results similar to those of the original cohort | Compared to audio-instructed DA-CPR, video-instructed DA-CPR was not associated with survival improvement in this observational study conducted in one metropolitan city. Randomised controlled trials are needed to compare the effects of video- and audio-instructed DA-CPR |
| Ecker et al[35], 2021 | Prospective randomised pilot | A video live stream from the caller’s smartphone to the EMS dispatch centre | - | This study shows that V-CPR is feasible using a video livestream from a smartphone and that typical resuscitation mistakes (which would lead to low-quality CPR) can be detected and corrected by the EMS dispatcher. Moreover, specific training of dispatchers could become necessary to achieve the best results in V-CPR |
| Yang et al[29], 2009 | Randomised controlled study | Video cell phone with both voice and video modes | The quality of CPR was evaluated by reviewing the videos and mannequin reports. Chest compressions among the video group were faster (median rate 955 vs 63.0 minutes, P < 0.01), deeper (median depth 36.0 vs 25.0 mm, P < 0.01), and of more appropriate depth (20.0% vs 0%, P < 0.01). The video group had more “hands-off” time (5.0 vs 0 seconds, P < 0.01), longer time to first chest compression (145.0 vs 116.0 seconds, P < 0.01) and total instruction time (150.0 vs 121.0 seconds, P < 0.01) | The quality of CPR was evaluated by reviewing the videos and mannequin reports. Chest compressions among the video group were faster (median rate 955 vs 63.0 minutes, P < 0.01), deeper (median depth 36.0 mm vs 25.0 mm, P < 0.01), and of more appropriate depth (20.0% vs 0%, P < 0.01). The video group had more “hands-off” time (5.0 seconds vs 0 seconds, P < 0.01), longer time to first chest compression (145.0 seconds vs 116.0 seconds, P < 0.01) and total instruction time (150.0 seconds vs 121.0 seconds, P < 0.01) |
| Morand et al[30], 2023 | NR | Live video tools | The first study’s results show that dispatchers are interested in visualising the scene with live video and broadcasting a live demonstration video when possible. The initial results also show that collaboration within the community is enhanced by the shared simulation and debriefing experiences, clarifying regulation procedures, and improving communication. Finally, an iterative development based on the lessons learned, expectations, and constraints of each previous study promotes the existence of a living lab that aims to determine the place of live video tools in the sequence of care performed by dispatchers | Living labs offer the opportunity to grasp previously undetected insights and redefine the use of the applications while potentially developing a sense of community among the stakeholders |
| You et al[31], 2008 | A prospective observational study | Video telephony | Placement of the electrode pads was performed correctly by all 52 participants, and 51 (98%) delivered an accurate shock. The mean (SD) time to correct shock delivery was 131.8 (20.6) seconds (range: 101-202) | Correct pad placement and shock delivery can be performed using an AED when instructions are provided via video telephone because a dispatcher can monitor every step and provide correct information |
| Barcala et al[17], 2023 | Descriptive and comparative design | SGs | Reliability was analysed by comparing the assessment of variables performed by the dispatcher through SGs with those registered by an on-scene instructor. Assistance through SGs was needed in 72% of the BLS steps, which enabled all participants to perform the ABC approach and use AED correctly. Feasibility was proven that the dispatcher’s feedback through SGs helped to improve bystanders’ performance, as after the dispatcher gave feedback via SGs, only 3% of skills were incorrect. Comparison of on-scene instructor vs SGs assessment by dispatcher differ in 8% of the analysed skills: Most significant difference in the “incorrect hand position during CPR” (on-scene: 33% vs dispatcher: 0%). When comparing the 1st minute with the 2nd minute, there were only significant differences in the percentage of compressions with correct depth (1st: 48 ± 42%, 2nd: 70 ± 31, P = 0.02) | Using SGs in aquatic settings seems feasible if the right wireless connectivity conditions are available. Communication between the emergency dispatcher and the witness is seamless and is especially helpful during the dispatch of the ABC approach and AED use. The small sample size did not allow us to investigate significant differences in CPR-quality markers. We consider that these devices have great potential for communication between dispatchers and laypersons but need improvement to be used in real emergencies |
| Bolle et al[7], 2011 | Randomised controlled trial | Video calls or via ordinary mobile phone calls | Each student answered a questionnaire to assess the technology’s understanding, confidence and usefulness. The mean age was 17.3 years in the video group and 17.9 years in the audio group. There were 27% male participants in the video group and 34% male participants in the audio group. Seventy-three per cent of the students in the video group and 71% in the audio group reported previous cardiopulmonary resuscitation training | Audio-visual communication during dispatch-assisted cardiopulmonary resuscitation improved rescuers’ confidence in this study of simulated cardiac arrest. The sound quality may be a problem with current video mobile calls, but users prefer video communication despite low-quality images. The use of audio-visual communication between lay bystanders and dispatchers has the potential to improve the quality of human interaction and, thus, the quality of pre-hospital resuscitation |
| Bang et al[32], 2020 | Prospective randomised simulation | Videocall assist laypersons | There was no significant difference among the three groups regarding baseline characteristics. Performance scores in the checklist for using AED were higher in the mobile video call-guided group, especially in the “power on AED” and “correctly attaches pads” categories, than in the other groups. However, the time interval to defibrillation was significantly longer in the mobile video call-guided group. Conclusions. Mobile video call guidance might be an alternative method to facilitate AED use by laypersons. Therefore, further well-designed research is needed to evaluate the feasibility of this approach in OHCA | In summary, this simulation evaluation confirmed that the AED performance of the laypersons improved in the video call-guided group than in the control or voice call-guided group. When using an AED alone, the AED could not be turned on quickly, and the pad could not be appropriately placed; therefore, a video call could be considered a feasible alternative in layperson CPR for OHCA |
| Bolle et al[33], 2009 | Clinical trial | The median CPR time without chest compression (“hands-off time”) was shorter in the video-call group vs the audio-call group (303 vs 331 seconds; P 5 0.048), but the median time to first compression was not shorter (104 vs 102 seconds; P 5 0.29). The median time to first ventilation was insignificantly shorter in the video-call group (176 vs 205 seconds; P 5 0.16). This group also had a slightly higher proportion of ventilation without error (0.11 vs 0.06; P 5 0.30) | Video calls or audio calls with experienced nurse dispatchers | Video communication is unlikely to improve T-CPR significantly without proper training of dispatchers and when using dispatch protocols written for audio-only calls. Improved dispatch procedures and training for handling video calls require further investigation |
| Kim et al[8], 2021 | Mixed method design | Video instructions vs audio instruction | Video-based instruction was found to be more effective in the number of chest compressions (P < 0.01), chest compression rate (P < 0.01), and chest compression interruptions (P < 0.01). The accuracy of the video group for the chest compression region was high (P = 0.05). Participants’ experiences were divided into three categories: ‘‘unfamiliar but beneficial experience’’, ‘‘met helper during a desperate and embarrassing situation’’, and ‘‘diverse views on drone use” | This study examined the impact of audio and video CPR instructions provided by dispatchers when an automatic defibrillator is delivered via drone during a cardiac arrest scenario outside a hospital. The research revealed significant differences between the audio and video instruction groups in various aspects of CPR performance, including chest compressions, compression rate, and hands-off time. Additionally, differences were observed in factors such as compression location, hand shape, and posture, indicating variations in CPR accuracy. Participants reported three main categories of experiences: Finding unfamiliar but helpful drone assistance, encountering assistance in a challenging situation, and having diverse opinions on drone use. These findings offer valuable insights for developing emergency medical services utilising drones and formulating video-instruction guidelines for dispatchers |
| Yuksen et al[23], 2016 | Retrospective study | Video instruction vs on-scene medical instruction | Fourteen representative teams, 14 physicians, 14 nurses, and 28 emergency medicine technicians, participated in the study. The average ages of participants in all three occupations were between the second and third decade of life. The percentages of participants with more than three years of ambulance experience were 71%, 64.3%, and 53.6% in the physicians, nurses, and EMTs groups. The median times of all outcomes were significantly longer in the online group than the on-scene group, including times from start to chest compression (total 102 seconds vs 36 seconds), full times from the beginning to VT/VF detection (187 seconds vs 99 seconds); times from VT/VF detection to the first defibrillation (57 seconds vs 28 seconds); and times from the start of adrenaline injection (282 seconds vs 165 seconds). The percentages of using amiodarone (21.43% vs 57.14%; P value < 0.001), establishment of a definitive airway (35.71% vs 100%; P value = 0.003), and correct detections of PEA (28.57% vs 100%; P value < 0.001) were significantly lower in the online group than the on-scene group. The high-quality CPR outcomes between the online and on-scene groups were comparable | Online medical instruction may have worse CPR outcomes compared with on-scene medical instruction in shockable, simulated CPR scenarios. Further studies are needed to confirm these results |
| Lee et al[34], 2018 | Randomised trial | Video call guidance | The median value of the time to the first defibrillation was significantly shorter in the video call guidance group (56 seconds) than in the conventional group. Group (73 seconds) (P < 0.001). The median value of the total hands-of time was also significantly shorter (228 seconds vs 285.5 seconds) | Physician-guided CPR with a video call enabled prompt manual defibrillation and significantly shortened the time required for first defibrillation, hands-of-time, and hands-of ratio in simulated cases of prehospital cardiac arrest |
The use of video calls in healthcare has experienced significant growth, particularly in critical situations like cardiac arrest, where time is of the essence. Video calls have the potential to bridge the gap between patients and healthcare providers, facilitating timely assessment, instructions, and potentially life-saving interventions. This article explores the benefits and challenges of incorporating video calls during cardiac arrest, highlighting the changing landscape of emergency response. In cardiac emergencies, swift assessment is crucial. Video calls enable real-time visual evaluation of the patient’s condition, empowering healthcare professionals to gather essential information about signs, symptoms, and the environment. This, in turn, promptly facilitates informed decision-making.
The integration of cutting-edge technology in healthcare has led to innovative approaches to delivering medical care. One such development is using GG for telematics support during CPR. Through GG, expert physicians can visually identify and promptly correct technique errors[36,37]. Studies have shown that real-time guidance in CPR, facilitated by wearable technology like GG, leads to more accurate and effective chest compressions, ultimately improving the chances of survival. Incorporating GG into standard CPR training programs can enhance the preparedness of healthcare pro
In an observational study, the feasibility of using GG for recording inpatient cardiac arrests was explored. Simulated cardiac arrest events were recorded using in-room physician observation, stationary video camera (SVC), and GG[36]. The results demonstrated that GG successfully recorded most events and was judged superior to SVC regarding global visibility and audibility. Additionally, GG showed better interpretability compared to SVC recordings. Respondents found GG easy to use, although some expressed concerns about potential distractions during resuscitations. The study suggests that GG is a viable and acceptable method for capturing simulated inpatient resuscitation events.
In a randomized controlled study developed in a tertiary care academic medical center, forty-two first-year pediatric residents were assessed during simulated pediatric cardiopulmonary arrests using a high-fidelity manikin. The study aimed to evaluate the impact of real-time video communication via GG between the first responder and a remote intensivist on the management of in-hospital pediatric cardiac emergencies before the arrival of the intensive care unit team. During the second evaluation, residents in the GG group could communicate with a remote intensivist in real-time video, while the control group provided standard care. Results indicated that, initially, both groups exhibited high proportions of time without ventilation (no-blow fraction) at 74% and without compression (no-flow fraction) at 95%. However, in the second evaluation, while there was no significant reduction in no-blow and no-flow fractions with the introduction of GG, the technique and rate of chest compressions were notably more appropriate (P < 0.001), and insufflations were significantly more effective (P = 0.04) compared to the control group[38]. The findings suggest that real-time video communication via GG may not reduce the initial no-blow and no-flow fractions within the first 5 minutes of simulated pediatric cardiopulmonary arrests. Still, it notably enhances the quality of insufflations and chest com
Another randomized clinical trial to assess whether utilizing augmented reality (AR) glasses, adapted to American Heart Association (AHA) guidelines, would enhance adherence to crucial life-saving procedures during pediatric CPR compared to using pediatric advanced life support pocket reference cards. The primary outcome measured the time it took, in seconds, from the onset of a specific cardiac arrest scenario to the first attempt at defibrillation. Secondary outcomes included the time taken for chest compressions, subsequent defibrillation attempts, drug administration, and intervals between various procedures, all evaluated against AHA guidelines. The trial included twenty residents divided into two groups. Surprisingly, the use of AR glasses did not significantly improve the time taken for the first defibrillation attempt (with an average of 146 seconds) or adherence to AHA guidelines in terms of other critical resuscitation actions and drug dosages. However, notable improvements were observed in accuracy and adherence when administering defibrillation doses compared to using pediatric advanced life support pocket reference cards. Notably, without AR glasses, residents administered incorrect doses in 65% of cases, including 21 instances of shock overdoses exceeding 100 Joules, resulting in a cumulative defibrillation dose of 18.7 Joules per kilogram. The use of AR glasses led to a significant reduction in these errors by 53% and a 37% decrease in the cumulative defibrillation dose[39].
Smart glasses have emerged as a potentially transformative technology in various fields, including healthcare. In the context of CPR, these innovative devices have the potential to enhance the evaluation of CPR quality significantly. One of the most significant advantages of using smart glasses during CPR is their ability to provide real-time feedback to the rescuer[40]. Equipped with AR displays, smart glasses can overlay essential metrics such as compression depth, rate, and recoil quality directly in the rescuer’s field of vision. This immediate feedback enables rescuers to make timely ad
Another significant emergency response and CPR advancement is T-CPR. It plays a critical role in enhancing guided bystander CPR. T-CPR plays a pivotal role in OHCA scenarios. It enables dispatchers to guide bystanders through life-saving interventions, potentially bridging the critical time gap before professional medical help arrives. The concept of T-CPR emerged in the late 20th century[42], coinciding with the widespread availability of telecommunication networks. One study focused on T-CPR, which involved emergency dispatchers guiding bystanders in performing CPR during OHCA[43]. While T-CPR instructions had been shown to boost bystander CPR rates, there was a lack of standardized evaluation methods. The researchers analyzed audio recordings of OHCA calls from a large regional dispatch center over one year. The results showed high agreement among evaluators in most reporting metrics. Recognizing the need for CPR, dispatchers initiated T-CPR instructions in nearly one-third of cases, resulting in bystander CPR in about 14%. The study emphasized the importance of a standardized methodology for evaluating TCPR to enhance quality, establish performance benchmarks, and guide future research on improving bystander CPR rates and OHCA survival.
Subsequent research has consistently affirmed the efficacy of T-CPR in enhancing survival rates. For instance, Culley et al[5] aimed to evaluate the impact of a T-CPR program in King County, explicitly focusing on bystander CPR rates and dispatcher-related delays in providing CPR instructions over the phone. The research spans from 1976 to 1988, incorporating a cardiac arrest surveillance system and the review of 267 recorded calls reporting cardiac emergencies in 1988. Following the implementation of the dispatcher-assisted telephone CPR program, the rate of bystander CPR increased significantly from 32% (1976-1981) to 54% (1982-1988), although a direct increase in survival rates was not demonstrated. Dispatcher response times were assessed, showing that it took a median of 75 seconds to identify the issue, with subsequent delivery of early protocols, ventilation, and compression instructions taking 19 seconds, 25 seconds, and 30 seconds, respectively - the total time to convey the entire CPR message they have averaged 2.3 minutes. Notably, the most common cause of delay was unnecessary questions, accounting for 57% of delays, with inquiries about the patient’s age being the most frequent (32%).
While T-CPR has proven invaluable in many situations, it is essential to acknowledge its limitations. Understanding these constraints allows for better refinement and optimization of T-CPR programs. One of the primary limitations of T-CPR is the absence of physical presence. Unlike professional first responders, dispatchers cannot assess the victim’s condition directly, which can sometimes lead to challenges in accurately gauging the severity of the situation. This absence of visual cues may result in delays or errors in providing instructions. Effective communication is crucial during a cardiac emergency. However, language barriers, technical issues, or the caller’s emotional state can impede clear and concise communication between the dispatcher and the bystander. This challenge is particularly pronounced in diverse or multilingual communities[44]. T-CPR primarily focuses on guiding bystanders verbally through the CPR process. While this is highly effective for chest compressions, it does not allow for direct guidance on other interventions that may be necessary, such as airway management or defibrillation. This limitation can impact the overall quality of care provided. Dispatchers cannot directly observe the effects of bystander-initiated CPR. They rely on the caller’s descriptions, which may not always be accurate or detailed enough. This inability to assess the effectiveness of interventions in real time can hinder decision-making and potentially delay critical actions. The quality of T-CPR instructions depends heavily on the training and experience of the dispatcher. While many dispatch centers provide rigorous training, there can be variability in the level of expertise among individual dispatchers. This can lead to inconsistencies in the quality of T-CPR provided across different emergency call centers. Dispatchers need to manage caller anxiety and maintain focus on providing clear guidance. Some cardiac emergencies may involve unique or complex circumstances that require specialized interventions beyond standard CPR protocols. Providing CPR to pediatric patients requires technical knowledge and techniques. Dispatchers may face added challenges in guiding bystanders through pediatric CPR, especially if the caller is unfamiliar with pediatric resuscitation procedures[45].
The main focus of this study is the video calls for DA-CPR. This innovative approach leverages video communication technology to enhance the quality and effectiveness of CPR interventions guided by dispatchers. This discussion will explore the various aspects, benefits, challenges, and future potential of using video calls in DA-CPR. Video calls empower bystanders with limited medical training to perform CPR effectively. Through live guidance from healthcare providers, bystanders can receive step-by-step instructions to ensure proper chest compressions and rescue breathing techniques. Healthcare providers can prepare the receiving hospital by providing critical patient information obtained through video calls. This includes vital signs, rhythm analysis, and any specific patient history or medications, enabling the hospital team to mobilize resources and plan interventions.
Video calls serve as an invaluable tool for education and training. Dispatchers can use live video feeds to demonstrate CPR techniques, ensuring callers understand the required actions[46]. This can be particularly beneficial for individuals who may not have prior CPR training. Video calls can help calm the rescuer by directly connecting with a professional dispatcher. Seeing and hearing the dispatcher can instill confidence and reduce panic, especially in high-stress situations like cardiac arrests. In complex cases, video calls can facilitate consultation with medical experts who can provide additional guidance and recommendations. This is particularly valuable when specialized knowledge or interventions are required[11].
Bolle et al[7] conducted a study to determine if video calls on mobile phones could enhance the confidence of lay rescuers during simulated cardiac arrest scenarios. They involved 180 high school students who were randomly divided into three groups. Some communicated through video calls, while others used regular mobile phone calls, all receiving guidance from experienced nurse dispatchers. After the scenarios, each student completed a questionnaire to evaluate their comprehension, confidence, and perception of the technology. On average, participants in the video call group were around 17.3 years old, slightly younger than those in the audio call group (average age of 17.9 years). Most rescuers in both groups believed video calls were more effective than audio calls in medical emergencies. This preference was significantly more robust in the video call group (P = 0.0002). The study concluded that visual contact through video calls increased rescuers’ confidence in stressful emergencies.
Lee et al[9] investigated whether video-instructed DA-CPR provided better neurologic recovery and survival to-discharge outcomes compared to audio-instructed DA-CPR in adult OHCA cases in a well-equipped metropolitan city. The research in Seoul, South Korea, analyzed data from adult bystander-witnessed OHCA cases between January 2018 and October 2019. The study included 2019 adult OHCA patients who received DA-CPR. Video instruction was more commonly given to elderly patients and those outside a home or medical facility. Patients who received video-instructed DA-CPR demonstrated higher rates of favorable neurologic outcomes (19.4%) and survival to discharge (27.1%) compared to those who received audio-instructed DA-CPR (6.8% and 12.3%, respectively). After adjusting for factors like age, gender, underlying diseases, and CPR location, video-instructed DA-CPR was found to be significantly associated with improved neurologic recovery (2.11 times higher) and survival to discharge (1.81 times higher) compared to audio-instructed DA-CPR.
A previous meta-analysis by Lin et al[47] aimed to compare the effectiveness of video-assisted and audio-assisted DI-CPR on bystander CPR quality. The subsequent analysis involved a meticulous examination of the disparities in DI-CPR quality under both video and audio guidance. The outcomes revealed noteworthy distinctions between the two groups. Notably, the initiation of chest compressions displayed a slower response in the video-assisted group compared to their audio-assisted counterparts, showcasing a median delay of 31.5 seconds. Additionally, the video-guided group exhibited a significantly higher chest compression rate, surpassing the audio-guided group by 19.9 compressions per minute. There was a slight preference for the audio-guided group regarding correct hand positioning, though this distinction did not reach statistical significance. Similarly, chest compression depth and time to first ventilation exhibited minimal di
Another meta-analysis by Bielski et al[4] aimed to assess the effectiveness of video-guided dispatcher-assisted bystander CPR (V-DACPR) in contrast to the traditional method of audio-guided dispatcher-assisted bystander CPR (C-DACPR). Compared to the C-DACPR, the V-DACPR significantly enhanced the chances of prehospital return of spon
In this article, we conducted a thorough assessment of existing literature on the enhancement of DA-CPR quality through video instruction. Nevertheless, we encountered certain constraints. For instance, we incorporated studies with various methodologies, populations, and interventions. This diversity challenges arriving at unequivocal conclusions, particularly when endeavoring to amalgamate data from studies employing fundamentally different approaches. Fur
Also, through this systematic review, we identified infrastructure and technological barriers that limit the adoption of audio and video communication. For instance, a vast majority of people lack access to high-speed internet. Despite its effectiveness, audio-instructed dispatcher-assisted CPR is not without challenges. Variability in dispatcher training and experience can influence the quality of instructions provided. Additionally, factors such as caller anxiety, language barriers, and environmental noise levels can hinder effective communication, highlighting the need for ongoing dis
However, satellite solutions such as the Satisfaction with Medicines platform can provide telemedical services to remote areas, but these initiatives require significant investment and coordination between governments and technology providers. Moreover, the coronavirus disease 2019 pandemic highlighted the challenges people faced in adapting to new technological tools. This technological transition had significant implications for patient safety, health equity, and quality of care. Patients with low digital literacy struggled to adapt to the sudden shift toward telehealth, leading to varying health outcomes. As technology advances, future research should focus on optimizing the integration of video calls into dispatcher-assisted CPR protocols. This may involve the development of user-friendly interfaces, addressing privacy concerns, and exploring the potential for augmented reality or other emerging technologies to enhance real-time guidance.
DA-CPR is a critical link in the chain of survival for OHCA patients. Extensive research has demonstrated its effectiveness in increasing bystander-initiated CPR and improving patient outcomes. Advances in technology, such as video calls and AED integration, continue to refine and enhance the delivery of DA-CPR. However, ongoing efforts are needed to standardize dispatcher training and improve communication strategies to ensure the highest quality of care for cardiac arrest victims.
| 1. | Bobrow BJ, Spaite DW, Berg RA, Stolz U, Sanders AB, Kern KB, Vadeboncoeur TF, Clark LL, Gallagher JV, Stapczynski JS, LoVecchio F, Mullins TJ, Humble WO, Ewy GA. Chest compression-only CPR by lay rescuers and survival from out-of-hospital cardiac arrest. JAMA. 2010;304:1447-1454. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 341] [Cited by in RCA: 337] [Article Influence: 22.5] [Reference Citation Analysis (1)] |
| 2. | Kienbacher CL, Schreiber W, Herkner H, Holzhacker C, Chwojka CC, Tscherny K, Egger A, Fuhrmann V, Niederer M, Neymayer M, Bernert L, Gamsjäger A, Grünbeck I, Heitger MB, Saleh L, Schmidt S, Schönecker S, Wirth D, Williams KA, Roth D. Drone-Facilitated Real-Time Video-Guided Feedback Helps to Improve the Quality of Lay Bystander Basic Life Support. A Randomized Controlled Simulation Trial. Prehosp Emerg Care. 2025;29:46-52. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 3. | Eberhard KE, Linderoth G, Gregers MCT, Lippert F, Folke F. Impact of dispatcher-assisted cardiopulmonary resuscitation on neurologically intact survival in out-of-hospital cardiac arrest: a systematic review. Scand J Trauma Resusc Emerg Med. 2021;29:70. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 33] [Article Influence: 8.3] [Reference Citation Analysis (0)] |
| 4. | Bielski K, Böttiger BW, Pruc M, Gasecka A, Sieminski M, Jaguszewski MJ, Smereka J, Gilis-Malinowska N, Peacock FW, Szarpak L. Outcomes of audio-instructed and video-instructed dispatcher-assisted cardiopulmonary resuscitation: a systematic review and meta-analysis. Ann Med. 2022;54:464-471. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 27] [Article Influence: 9.0] [Reference Citation Analysis (0)] |
| 5. | Culley LL, Clark JJ, Eisenberg MS, Larsen MP. Dispatcher-assisted telephone CPR: common delays and time standards for delivery. Ann Emerg Med. 1991;20:362-366. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 146] [Cited by in RCA: 142] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 6. | Vaillancourt C, Charette ML, Bohm K, Dunford J, Castrén M. In out-of-hospital cardiac arrest patients, does the description of any specific symptoms to the emergency medical dispatcher improve the accuracy of the diagnosis of cardiac arrest: a systematic review of the literature. Resuscitation. 2011;82:1483-1489. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 55] [Cited by in RCA: 50] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 7. | Bolle SR, Johnsen E, Gilbert M. Video calls for dispatcher-assisted cardiopulmonary resuscitation can improve the confidence of lay rescuers--surveys after simulated cardiac arrest. J Telemed Telecare. 2011;17:88-92. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 32] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 8. | Kim HJ, Kim JH, Park D. Comparing audio- and video-delivered instructions in dispatcher-assisted cardiopulmonary resuscitation with drone-delivered automatic external defibrillator: a mixed methods simulation study. PeerJ. 2021;9:e11761. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 17] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 9. | Lee HS, You K, Jeon JP, Kim C, Kim S. The effect of video-instructed versus audio-instructed dispatcher-assisted cardiopulmonary resuscitation on patient outcomes following out of hospital cardiac arrest in Seoul. Sci Rep. 2021;11:15555. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 24] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 10. | Aranda-García S, Otero-Agra M, Fernández-Méndez F, Herrera-Pedroviejo E, Darné M, Barcala-Furelos R, Rodríguez-Núñez A. Augmented reality training in basic life support with the help of smart glasses. A pilot study. Resusc Plus. 2023;14:100391. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 7] [Reference Citation Analysis (0)] |
| 11. | Lee JS, Jeon WC, Ahn JH, Cho YJ, Jung YS, Kim GW. The effect of a cellular-phone video demonstration to improve the quality of dispatcher-assisted chest compression-only cardiopulmonary resuscitation as compared with audio coaching. Resuscitation. 2011;82:64-68. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 40] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 12. | Moher D, Liberati A, Tetzlaff J, Altman DG; PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Int J Surg. 2010;8:336-341. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9207] [Cited by in RCA: 8041] [Article Influence: 536.1] [Reference Citation Analysis (2)] |
| 13. | Cochrane Methods Bias. RoB 2: A revised Cochrane risk-of-bias tool for randomized trials. [cited 17 November 2021]. Available from: https://methods.cochrane.org/bias/resources/rob-2-revised-cochrane-risk-bias-tool-randomized-trials. |
| 14. | Pérez Alonso N, Pardo Rios M, Juguera Rodriguez L, Vera Catalan T, Segura Melgarejo F, Lopez Ayuso B, Martí Nez Riquelme C, Lasheras Velasco J. Randomised clinical simulation designed to evaluate the effect of telemedicine using Google Glass on cardiopulmonary resuscitation (CPR). Emerg Med J. 2017;34:734-738. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 13] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 15. | Peltan ID, Guidry D, Brown K, Kumar N, Beninati W, Brown SM. Telemedical Intensivist Consultation During In-Hospital Cardiac Arrest Resuscitation: A Simulation-Based, Randomized Controlled Trial. Chest. 2022;162:111-119. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 6] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 16. | Aranda-García S, Barrio-Cortes J, Fernández-Méndez F, Otero-Agra M, Darné M, Herrera-Pedroviejo E, Barcala-Furelos R, Rodríguez-Núñez A. Dispatcher-assisted BLS for lay bystanders: A pilot study comparing video streaming via smart glasses and telephone instructions. Am J Emerg Med. 2023;71:163-168. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
| 17. | Barcala-Furelos R, Aranda-García S, Otero-Agra M, Fernández-Méndez F, Alonso-Calvete A, Martínez-Isasi S, Greif R, Rodríguez-Núñez A. Are smart glasses feasible for dispatch prehospital assistance during on-boat cardiac arrest? A pilot simulation study with fishermen. Intern Emerg Med. 2023;18:1551-1559. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 8] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 18. | Plata C, Nellessen M, Roth R, Ecker H, Böttiger BW, Löser J, Wetsch WA. Impact of video quality when evaluating video-assisted cardiopulmonary resuscitation: a randomized, controlled simulation trial. BMC Emerg Med. 2021;21:96. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 6] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 19. | Perry O, Wacht O, Jaffe E, Sinuany-Stern Z, Bitan Y. Using a filming protocol to improve video-instructed cardiopulmonary resuscitation. Technol Health Care. 2020;28:213-220. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 8] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 20. | Ecker H, Lindacher F, Adams N, Hamacher S, Wingen S, Schier R, Böttiger BW, Wetsch WA. Video-assisted cardiopulmonary resuscitation via smartphone improves quality of resuscitation: A randomised controlled simulation trial. Eur J Anaesthesiol. 2020;37:294-302. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 26] [Article Influence: 6.5] [Reference Citation Analysis (0)] |
| 21. | Sonkin R, Jaffe E, Wacht O, Morse H, Bitan Y. Real-time video communication between ambulance paramedic and scene - a simulation-based study. BMC Health Serv Res. 2022;22:1049. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 22. | Linderoth G, Rosenkrantz O, Lippert F, Østergaard D, Ersbøll AK, Meyhoff CS, Folke F, Christensen HC. Live video from bystanders' smartphones to improve cardiopulmonary resuscitation. Resuscitation. 2021;168:35-43. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 35] [Article Influence: 8.8] [Reference Citation Analysis (0)] |
| 23. | Yuksen C, Sawatmongkornkul S, Tuangsirisup J, Sawanyawisuth K, Sittichanbuncha Y. The CPR outcomes of online medical video instruction versus on-scene medical instruction using simulated cardiac arrest stations. BMC Emerg Med. 2016;16:25. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 5] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 24. | Johnsen E, Bolle SR. To see or not to see--better dispatcher-assisted CPR with video-calls? A qualitative study based on simulated trials. Resuscitation. 2008;78:320-326. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 48] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 25. | Meinich-Bache Ø, Engan K, Birkenes TS, Myklebust H. Real-Time Chest Compression Quality Measurements by Smartphone Camera. J Healthc Eng. 2018;2018:6241856. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 9] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 26. | Ofoma UR, Drewry AM, Maddox TM, Boyle W, Deych E, Kollef M, Girotra S, Joynt Maddox KE; American Heart Association's Get With The Guidelines®- Resuscitation Investigators. Outcomes of in-hospital cardiac arrest among hospitals with and without telemedicine critical care. Resuscitation. 2022;177:7-15. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 27. | Lee SGW, Kim TH, Lee HS, Shin SD, Song KJ, Hong KJ, Kim JH, Park YJ. Efficacy of a new dispatcher-assisted cardiopulmonary resuscitation protocol with audio call-to-video call transition. Am J Emerg Med. 2021;44:26-32. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 10] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 28. | Lee SY, Song KJ, Shin SD, Hong KJ, Kim TH. Comparison of the effects of audio-instructed and video-instructed dispatcher-assisted cardiopulmonary resuscitation on resuscitation outcomes after out-of-hospital cardiac arrest. Resuscitation. 2020;147:12-20. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 41] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 29. | Yang CW, Wang HC, Chiang WC, Hsu CW, Chang WT, Yen ZS, Ko PC, Ma MH, Chen SC, Chang SC. Interactive video instruction improves the quality of dispatcher-assisted chest compression-only cardiopulmonary resuscitation in simulated cardiac arrests. Crit Care Med. 2009;37:490-495. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 51] [Cited by in RCA: 60] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 30. | Morand O, Larribau R, Safin S, Pages R, Soichet H, Rizza C. The Integration of Live Video Tools to Help Bystanders During an Emergency Call: Protocol for a Mixed Methods Simulation Study. JMIR Res Protoc. 2023;12:e40699. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 31. | You JS, Park S, Chung SP, Park JW. Performance of cellular phones with video telephony in the use of automated external defibrillators by untrained laypersons. Emerg Med J. 2008;25:597-600. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 14] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 32. | Bang JY, Cho Y, Cho GC, Lee J, Kim IY. Can Mobile Videocall Assist Laypersons' Use of Automated External Defibrillators? A Randomized Simulation Study and Qualitative Analysis. Biomed Res Int. 2020;2020:4069749. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 10] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 33. | Bolle SR, Scholl J, Gilbert M. Can video mobile phones improve CPR quality when used for dispatcher assistance during simulated cardiac arrest? Acta Anaesthesiol Scand. 2009;53:116-120. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 38] [Cited by in RCA: 51] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 34. | Lee DK, Park SM, Kim YJ, Lee CA, Jeong WJ, Kim GW, Shin DH, Lee YH. CPR Guidance by an Emergency Physician via Video Call: A Simulation Study. Emerg Med Int. 2018;2018:1480726. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 4] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 35. | Ecker H, Wingen S, Hamacher S, Lindacher F, Böttiger BW, Wetsch WA. Evaluation Of CPR Quality Via Smartphone With A Video Livestream - A Study In A Metropolitan Area. Prehosp Emerg Care. 2021;25:76-81. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 18] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 36. | Kassutto SM, Kayser JB, Kerlin MP, Upton M, Lipschik G, Epstein AJ, Dine CJ, Schweickert W. Google Glass Video Capture of Cardiopulmonary Resuscitation Events: A Pilot Simulation Study. J Grad Med Educ. 2017;9:748-754. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 6] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 37. | Albrecht UV, von Jan U, Kuebler J, Zoeller C, Lacher M, Muensterer OJ, Ettinger M, Klintschar M, Hagemeier L. Google Glass for documentation of medical findings: evaluation in forensic medicine. J Med Internet Res. 2014;16:e53. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 70] [Cited by in RCA: 37] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 38. | Imbriaco G, Canova GS, Righi L, Tararan S, Di Mario G, Ramacciati N. Dispatcher-Assisted CPR in Italy: A Nationwide Survey of Current Practices and Future Challenges in Emergency Medical Communication Centers. J Clin Med. 2025;14:637. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 39. | Siebert JN, Ehrler F, Gervaix A, Haddad K, Lacroix L, Schrurs P, Sahin A, Lovis C, Manzano S. Adherence to AHA Guidelines When Adapted for Augmented Reality Glasses for Assisted Pediatric Cardiopulmonary Resuscitation: A Randomized Controlled Trial. J Med Internet Res. 2017;19:e183. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 43] [Cited by in RCA: 32] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 40. | Aranda-García S, Santos-Folgar M, Fernández-Méndez F, Barcala-Furelos R, Pardo Ríos M, Hernández Sánchez E, Varela-Varela L, San Román-Mata S, Rodríguez-Núñez A. "Dispatcher, Can You Help Me? A Woman Is Giving Birth". A Pilot Study of Remote Video Assistance with Smart Glasses. Sensors (Basel). 2022;23:409. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 11] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 41. | Kebapci A, Ozkaynak M, Bowler F, Ponicsan H, Zhang Z, Bai E. A Pilot Randomized Controlled Study to Determine the Effect of Real-Time Videos With Smart Glass on the Performance of the Cardiopulmonary Resuscitation. Comput Inform Nurs. 2025;43:e01211. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 42. | Eisenberg MS, Hallstrom AP, Carter WB, Cummins RO, Bergner L, Pierce J. Emergency CPR instruction via telephone. Am J Public Health. 1985;75:47-50. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 131] [Cited by in RCA: 125] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 43. | Dameff C, Vadeboncoeur T, Tully J, Panczyk M, Dunham A, Murphy R, Stolz U, Chikani V, Spaite D, Bobrow B. A standardized template for measuring and reporting telephone pre-arrival cardiopulmonary resuscitation instructions. Resuscitation. 2014;85:869-873. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 39] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 44. | Ahmed F, Khan UR, Soomar SM, Raheem A, Naeem R, Naveed A, Razzak JA, Khan NU. Acceptability of telephone-cardiopulmonary resuscitation (T-CPR) practice in a resource-limited country- a cross-sectional study. BMC Emerg Med. 2022;22:139. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 45. | Berger S. Survival From Out-of-Hospital Cardiac Arrest: Are We Beginning to See Progress? J Am Heart Assoc. 2017;6:e007469. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 13] [Cited by in RCA: 23] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 46. | Gruenerbl A, Javaheri H, Monger E, Gobbi M, Lukowicz P. Training CPR with a wearable real time feedback system. Proceedings of the 2018 ACM International Symposium on Wearable Computers; 2018 Oct 8-12; Singapore. New York: Association for Computing Machinery, 2018: 44-47. |
| 47. | Lin YY, Chiang WC, Hsieh MJ, Sun JT, Chang YC, Ma MH. Quality of audio-assisted versus video-assisted dispatcher-instructed bystander cardiopulmonary resuscitation: A systematic review and meta-analysis. Resuscitation. 2018;123:77-85. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 43] [Cited by in RCA: 63] [Article Influence: 9.0] [Reference Citation Analysis (0)] |