Published online Mar 9, 2025. doi: 10.5492/wjccm.v14.i1.98938
Revised: November 4, 2024
Accepted: November 22, 2024
Published online: March 9, 2025
Processing time: 154 Days and 21.6 Hours
Airway management plays a crucial role in providing adequate oxygenation and ventilation to patients during various medical procedures and emergencies. When patients have a limited mouth opening due to factors such as trauma, inflammation, or anatomical abnormalities airway management becomes challenging. A commonly utilized method to overcome this challenge is the use of video laryngoscopy (VL), which employs a specialized device equipped with a camera and a light source to allow a clear view of the larynx and vocal cords. VL over
Core Tip: Airway management in patients with a limited mouth opening is difficult with the currently available video laryngoscopes. We devised an affordable flangeless video laryngoscope and successfully tested it on a manikin.
- Citation: Mustahsin M, Singh H. Novel flangeless video laryngoscope for limited mouth opening. World J Crit Care Med 2025; 14(1): 98938
- URL: https://www.wjgnet.com/2220-3141/full/v14/i1/98938.htm
- DOI: https://dx.doi.org/10.5492/wjccm.v14.i1.98938
Airway management plays a crucial role in providing adequate oxygenation and ventilation to patients during various medical procedures and emergencies[1]. However, when patients have a limited mouth opening due to trauma, inflammation, or anatomical abnormalities airway management is challenging. Video laryngoscopy (VL) is commonly utilized to overcome this challenge[2,3]. VL employs a specialized device equipped with a camera and a light source to provide a clear view of the larynx and vocal cords. VL overcomes the limitations of direct laryngoscopy in patients with limited mouth opening, enabling better visualization and successful intubation[4]. Various types of video laryngoscope blades are available. We devised a novel flangeless video laryngoscope for use in patients with a limited mouth opening and tested it on a manikin. Further testing of this device on patients is required, but this novel device may be useful in the management of patients with a limited mouth opening.
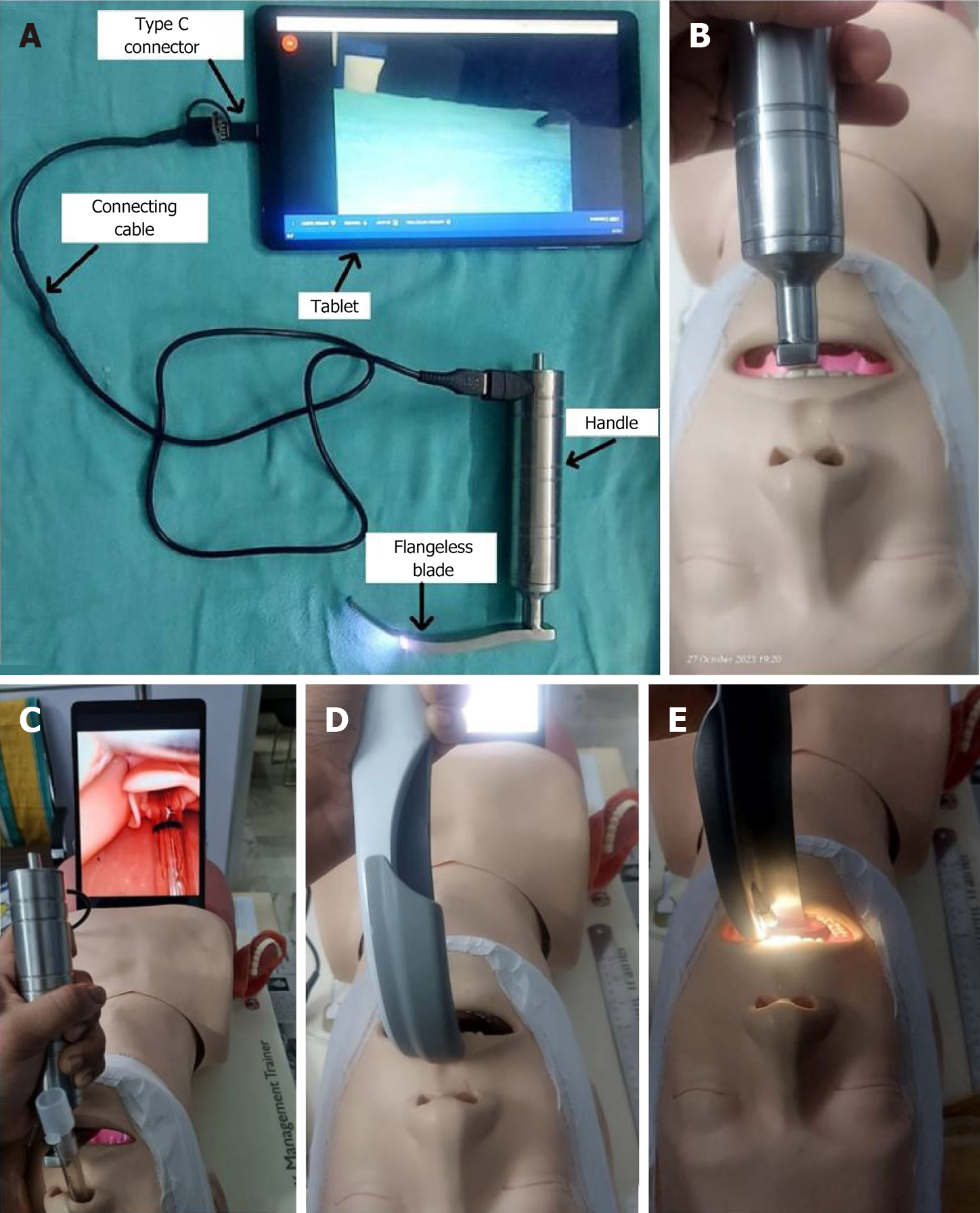
With the help of a biomedical engineering team from Era University (Uttar Pradesh, India) we modified a Macintosh laryngoscope into a flangeless video laryngoscope by attaching a waterproof wireless borescope examination camera (4 mm in diameter) with six light-emitting diodes. It was attached 40 mm proximal to the tip of the laryngoscope (Figure 1A). This flangeless video laryngoscope is utilized similarly to conventional and video laryngoscopes with the exception of the mode of insertion. Conventional or video laryngoscope is inserted along the angle of the mouth, whereas the flangeless video laryngoscope is inserted directly over the tongue. The image captured from the camera can be seen on a smartphone or tablet connected via a universal serial bus type C cable (Figure 1B) and using the Inskam application (freely downloaded from the Google Play store). During our testing, the high definition image seen on the smartphone was clear and had no connection issues. The real-time video can also be transmitted to a control room where an experienced airway operator can monitor and guide junior staff performing the procedure.
To test this flangeless video laryngoscope, we performed a manikin study. Ten certified anaesthesiologists with 3 years of anaesthesiology training and experience with video laryngoscope performed the intubation with the Macintosh laryngoscope, our flangeless laryngoscope, and a traditional video laryngoscope. The number of attempts, the time of intubation, the percentage of glottic opening (POGO) scores, and Cormack-Lehane grading (CL) were recorded in a manikin with a normal mouth opening. Data were analyzed using statistical product and service solutions statistics (IBM Corp., Armonk, NY, United States) version 21.0. Intergroup comparison was performed by repeat measures analysis of variance for parametric data and the Friedman test for non-parametric data. Between group comparisons were performed using the paired t-test for parametric data and Wilcoxon signed rank test for non-parametric ranked data.
Statistically, there was no significant intergroup or between group difference for attempts among the different types of laryngoscopes (P > 0.5). Mean intubation time was the quickest for the Macintosh (10.14 seconds ± 3.55 seconds) followed by the flangeless laryngoscope (10.66 seconds ± 5.68 seconds) and finally the traditional video laryngoscope (16.82 seconds ± 9.69 seconds). However, there was no significant difference in intubation times between the Macintosh and the flangeless nor the traditional and the flangeless (P > 0.05). The mean POGO scores were 54.00 ± 9.66 for the Macintosh, 79.00 ± 20.20 for the traditional, and 89.00 ± 5.68 for the flangeless. The traditional laryngoscope and flangeless laryngoscope both had a significantly higher POGO score compared to the Macintosh laryngoscope (P < 0.05), but there was no significant difference between the traditional and flangeless devices (P = 0.158).
The median CL scores (interquartile range) were 2 (1, 2) for the Macintosh, 2 (1, 2) for the traditional, and 1 (1, 1) for the flangeless laryngoscope. The flangeless laryngoscope had a significantly lower CL score compared to the Macintosh laryngoscope (P = 0.046). There were no other significant differences when comparing the three devices (P > 0.05) (Table 1).
| Observer | Macintosh | Traditional | Flangeless | |||||||||
| A | TOI | POGO | CL | A | TOI | POGO | CL | A | TOI | POGO | CL | |
| 1 | 1 | 10.47 | 60 | 2 | 1 | 14.19 | 70 | 2 | 1 | 4.58 | 80 | 1 |
| 2 | 1 | 11.98 | 50 | 2 | 1 | 15.12 | 90 | 1 | 1 | 11.80 | 80 | 2 |
| 3 | 1 | 9.87 | 60 | 2 | 3 | 19.93 | 50 | 2 | 1 | 15.80 | 90 | 1 |
| 4 | 1 | 10.11 | 70 | 1 | 1 | 9.53 | 100 | 1 | 1 | 11.10 | 90 | 1 |
| 5 | 1 | 10.45 | 40 | 1 | 1 | 8.76 | 90 | 1 | 1 | 17.12 | 90 | 1 |
| 6 | 1 | 7.92 | 50 | 2 | 1 | 8.87 | 40 | 1 | 1 | 17.19 | 90 | 1 |
| 7 | 1 | 18.51 | 60 | 1 | 2 | 38.91 | 100 | 1 | 1 | 5.15 | 90 | 1 |
| 8 | 1 | 8.79 | 60 | 1 | 1 | 15.36 | 80 | 2 | 1 | 12.23 | 90 | 1 |
| 9 | 1 | 4.54 | 40 | 1 | 2 | 27.30 | 90 | 1 | 1 | 8.95 | 100 | 1 |
| 10 | 1 | 8.80 | 50 | 2 | 1 | 10.20 | 80 | 2 | 1 | 2.64 | 90 | 1 |
| Central tendency (IQR) | 1 (1, 1) | 10.14 ± 3.55 | 54.00 ± 9.66 | 2 (1, 2) | 1 (1, 2) | 16.82 ± 9.69 | 79.00 ± 20.20 | 2 (1, 2) | 1 (1, 1) | 10.66 ± 5.26 | 89.00 ± 5.68 | 1 (1, 1) |
| 95%CI | 7.60-12.70 | 47.09-60.91 | 1.12-1.88 | 0.90-1.90 | 9.89-23.75 | 64.52-93.48 | 1.03-1.77 | 1.00-1.00 | 6.89-14.42 | 84.94-93.06 | 1.00-1.00 | |
After successfully testing the flangeless video laryngoscope in a manikin, we limited the mouth opening of the manikin to 1 cm (interincisor gap) with micropore paper tape. We were unable to insert the blades of the Macintosh laryngoscope and video laryngoscope (Figure 1D and E). However, the flangeless video laryngoscope was inserted and nasal intubation was performed with a 7 mm internal diameter endotracheal tube (Figure 1C).
The improvised flangeless video laryngoscope offers several advantages. Most importantly, it can be inserted into the mouths of patients with a limited opening, which resolves the challenge of using other commercially available video laryngoscopes that cannot be inserted in these cases. The flangeless video laryngoscope offers incredible ease-of-use and accessibility because it is a plug-and-play smartphone device. Furthermore, it is reusable and significantly more affordable than other options, costing only 150 dollars compared to 1500 dollars.
However, it is important to note that the device has only been tested on a manikin. While a manikin is useful for practicing and testing, it may not always accurately reflect the performance of a device on real patients with limited mouth openings. Despite this limitation, the advantages of this flangeless video laryngoscope make it an intriguing option for intubating patients with a limited mouth opening.
In conclusion, this novel flangeless video laryngoscope offers the combined benefits of excellent glottis view similar to a video laryngoscope and easy insertion and successful intubation in patients with a limited mouth opening (up to 1 cm), thus overcoming the challenge of inserting other video laryngoscopes on the market currently. Further research on real patients with limited mouth openings is required to bring this device into the clinic.
| 1. | Szarpak L. Laryngoscopes for difficult airway scenarios: a comparison of the available devices. Expert Rev Med Devices. 2018;15:631-643. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 11] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 2. | Shruthi AH, Dinakara D, Chandrika YR. Role of videolaryngoscope in the management of difficult airway in adults: A survey. Indian J Anaesth. 2020;64:855-862. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 10] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 3. | Gordon JK, Bertram VE, Cavallin F, Parotto M, Cooper RM. Direct versus indirect laryngoscopy using a Macintosh video laryngoscope: a mannequin study comparing applied forces. Can J Anaesth. 2020;67:515-520. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 4] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 4. | Lewis SR, Butler AR, Parker J, Cook TM, Schofield-Robinson OJ, Smith AF. Videolaryngoscopy versus direct laryngoscopy for adult patients requiring tracheal intubation: a Cochrane Systematic Review. Br J Anaesth. 2017;119:369-383. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 190] [Cited by in RCA: 224] [Article Influence: 37.3] [Reference Citation Analysis (0)] |