Published online Dec 9, 2024. doi: 10.5492/wjccm.v13.i4.99587
Revised: September 24, 2024
Accepted: October 10, 2024
Published online: December 9, 2024
Processing time: 97 Days and 22.2 Hours
Most trauma occurs among young male subjects in Qatar. We examined the predictive values of the delta shock index (DSI), defined as the change in the shock index (SI) value from the scene to the initial reading in the emergency unit
To explore whether high DSI is associated with severe injuries, more interven
A retrospective analysis was conducted after data were extracted from the Na
This analysis included 13212 patients with a mean age of 33 ± 14 years, and 24% had a high DSI. Males accounted for 91% of the study population. The trauma activation level was higher in patients with a high DSI (38% vs 15%, P = 0.001). DSI correlated with RTS (r = -0.30), TRISS (r = -0.30), NTBU (r = 0.20), GCS (r = -0.24), ISS (r = 0.22), and HLOS (r = 0.14) (P = 0.001 for all). High DSI was associated with significantly higher rates of intubation, la
In addition to sex-biased observations, almost one-quarter of the study cohort had a higher DSI and were mostly young. High DSI correlated significantly with the other injury severity scores, which require more time and imaging to be ready to use. Therefore, DSI is a practical, simple bedside tool for triaging and prognosis in young patients with trauma.
Core Tip: The delta shock index (DSI) is defined as the change of SI value from the scene to the initial reading in the emergency unit (i.e., subtracting calculated SI at admission from SI at the scene). Among young trauma patients, high DSI is associated with severe injuries, more interventions, and worse outcomes (i.e., blood transfusion, exploratory laparotomy, ventilator-associated pneumonia, hospital length of stay, and in-hospital mortality). Apart from gender-biased observation, almost one-quarter of the study cohort had a higher DSI and were mostly young. High DSI correlated significantly with the other injury severity scores that need more time and imaging to be ready to use. Therefore, DSI is a practical, simple bedside tool for triaging and prognosis in young, injured patients.
- Citation: Asim M, El-Menyar A, Ahmed K, Al-Ani M, Mathradikkal S, Alaieb A, Hammo AA, Taha I, Kloub A, Al-Thani H. Delta shock index predicts injury severity, interventions, and outcomes in trauma patients: A 10-year retrospective observational study. World J Crit Care Med 2024; 13(4): 99587
- URL: https://www.wjgnet.com/2220-3141/full/v13/i4/99587.htm
- DOI: https://dx.doi.org/10.5492/wjccm.v13.i4.99587
Traumatic injuries have a substantial impact on morbidity and mortality rates worldwide, particularly in younger patients[1]. The initial severity of injury and quality of care significantly influence the outcomes of trauma patients in emergency settings[2-4]. Furthermore, bleeding remains the primary preventable factor leading to mortality among trauma victims[5,6]. Therefore, to improve survival based on an early goal-directed resuscitation approach, prompt identification of physiological derangement and efficient hemorrhage control are paramount[7].
Uncontrolled bleeding in trauma patients results in hypovolemic shock, which may be further worsened by the lethal triad of coagulopathy, lactic acidosis, and hypothermia[8]. Therefore, early restoration of hemostasis with exploratory laparotomy or interventional radiology is crucial for treating shock, in addition to massive blood transfusion[9]. Fur
Notably, the assessment of initial vital signs offers a simple and practical approach to the early determination of physiological derangement in trauma patients; nevertheless, relying only on individual vital signs for prognosis is often inaccurate[1]. As a result, various shock indices (SI) have been suggested for predicting outcomes based on vital signs obtained at the scene and in the emergency department (ED)[2]. The delta SI (DSI), which is the difference between the SI obtained at the accident scene and that in the ED (DSI = ED SI – Scene SI), has shown a better predictive power for out
A retrospective cohort analysis was conducted to include trauma patients admitted to a national level I trauma center, Hamad General Hospital (HGH), Doha, Qatar, between January 2011 and June 2021. The study included all trauma patients who required hospital admission and had initial vital signs taken at the scene and repeated in the ED. Patients with missing vital signs, either at the scene or in the ED, and those who died before arrival at the hospital were excluded from the study. Data were retrieved from the Qatar National Trauma Registry (QNTR) database at HGH and from electronic medical records [Cerner Corporation (North Kansas City, Missouri, United States)].
Data variables extracted for the study included demographics (age and sex), emergency medical services (EMS) time, scene time, team level activation, vital signs at the scene and in the ED (pulse, systolic blood pressure, diastolic blood pressure, respiratory rate), Glasgow coma scale (GCS) at the scene and in the ED, ethanol levels, cardio-pulmonary resuscitation, ED disposition, revised trauma score (RTS), trauma score and injury severity score (TRISS), injury severity score (ISS), abbreviated injury scale (AIS), focused assessment with sonography in trauma (FAST), and interventions [intubation, exploratory laparotomy, extracorporeal membrane oxygenation (ECMO), and resuscitative endovascular balloon occlusion of the aorta (REBOA)]. Information regarding in-hospital complications (sepsis, VAP, acute respiratory distress syndrome, thromboembolic events, abdominal compartment syndrome, multiorgan failure, and disseminated intravascular coagulation), discharge disposition, need for prehospital fluid administration, overall blood transfusion, massive blood transfusion, length of hospital and intensive care unit (ICU) stay, ventilatory days, and mortality was also collected. Based on the vital signs seen at the scene and during ED triage, we computed the SI as the ratio of heart rate to systolic blood pressure[14]. DSI was calculated by subtracting the SI at the scene from the SI in the ED[10,11]. The Medical Research Center (Institutional Review Board, MRC-01-21-990) approved the study protocol, with a waiver of informed consent for the retrospective chart review of anonymous data from the QNTR database. This study follows the reco
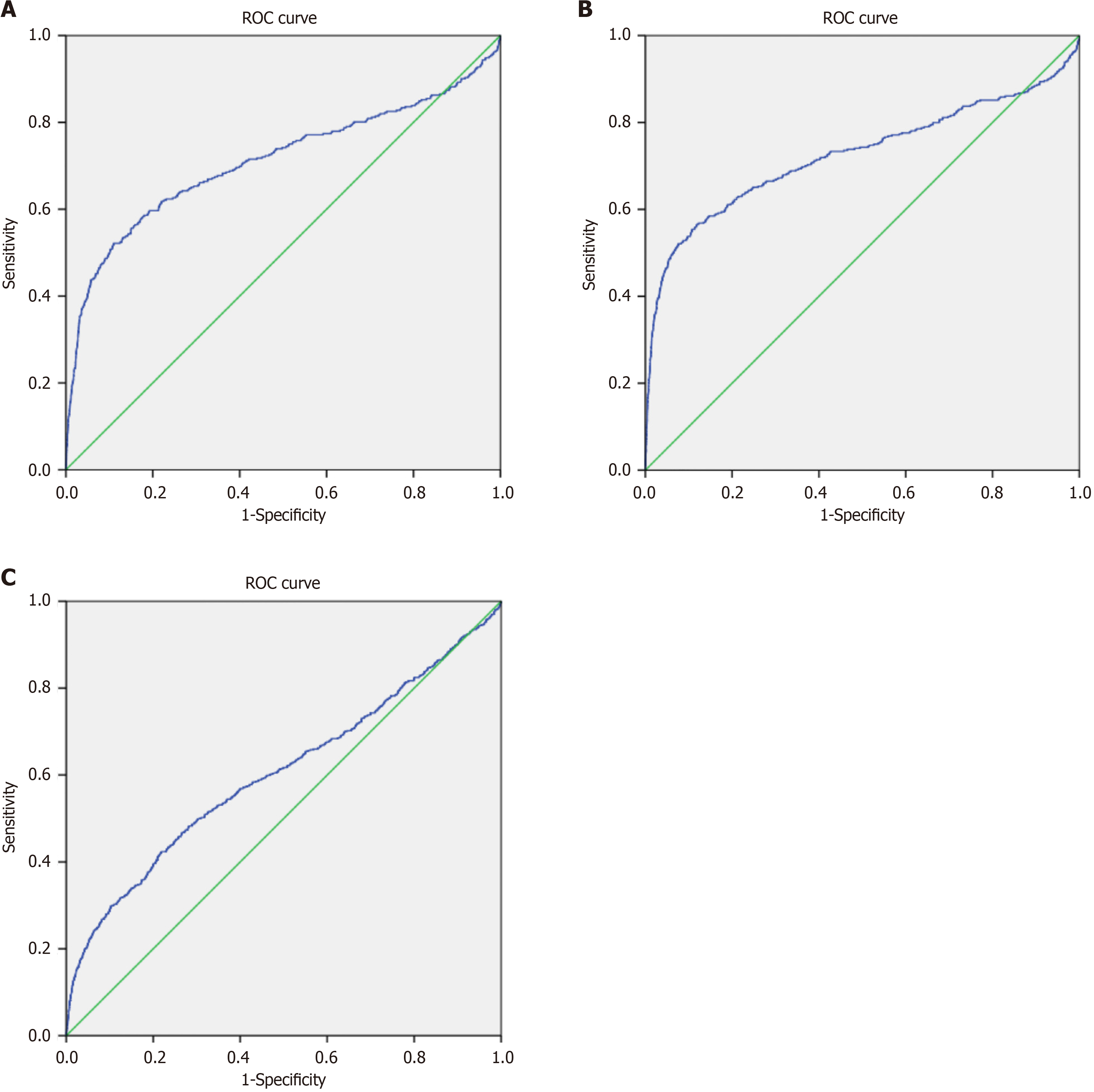
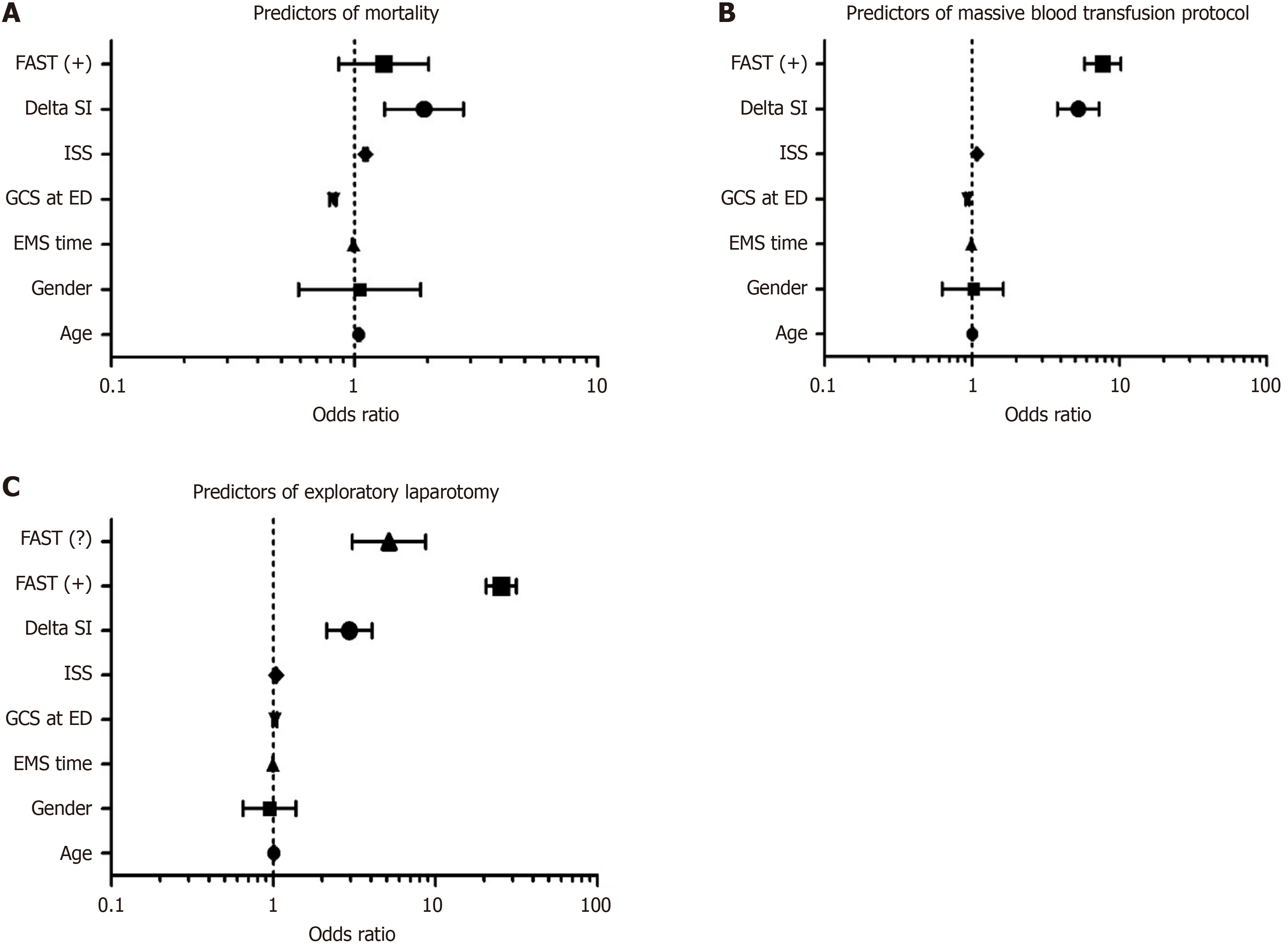
Data are presented as proportions, median, or the mean ± SD, as appropriate. Differences in categorical and continuous variables were analyzed using the χ2 test and Student’s t-test, as appropriate. The Yates corrected χ2 test was used for categorical variables if the expected cell frequencies were less than 5. Patients were grouped based on DSI as low (≤ 0.1) or high (> 0.1). Correlations between DSI and ISS, RTS, AIS, Glasgow coma scale (GCS), TRISS, HLOS, and NTBU were assessed using Pearson correlation coefficient (r) analysis. Receiver operating characteristic curves and area under the curve were used to identify the predictive power of DSI for mortality and need for massive transfusion protocol activation (MTP) and exploratory laparotomy. Furthermore, the diagnostic testing accuracy of DSI for predicting mortality and need for MTP and exploratory laparotomy was identified in terms of sensitivity, specificity, negative predictive value, and negative likelihood ratio. Multivariable regression analyses were performed to determine the predictors of mortality, massive transfusion, and exploratory laparotomy, using the most relevant covariates (age, sex, ISS, GCS ED, DSI, EMS time, and FAST). Data were expressed as odds ratios (OR) and 95% confidence intervals (CIs). A two-tailed P value of < 0.05 was considered statistically significant. All data analyses were performed using Statistical Package for the Social Sciences version 21 (SPSS, Inc., Chicago, IL, United States).
During the study period, a total of 13212 trauma patients with a mean age of 33 ± 15 years were included in this study, of which 91% were male and 24% had a high DSI. The overall injury severity score was 12.4 ± 9.3, and GCS at ED was 15 (3-15), 18% required blood transfusion, and massive transfusion protocol was activated in 3.2% of cases. Table 1 compares the demographic and clinical characteristics based on DSI. Patients with a high DSI had prolonged scene time (P = 0.001) and markedly impaired vital signs at the accident scene (P = 0.001) and upon arrival at the hospital (P = 0.001), including the mean GCS score (P = 0.001 for both), as compared to the low-DSI group. The need for cardio-pulmonary resuscitation (5.8% vs 1.3%, P = 0.001) and trauma activation level (TT1) was also higher in patients with a high DSI (38% vs 15%, P = 0.001). Moreover, patients with a high DSI were more likely to be transferred from the ED to the operating room (P = 0.001) and intensive care unit (P = 0.001) than those in the low-DSI group.
| DSI ≤ 0.1 (n = 10039; 76%) | DSI > 0.1 (n = 3173; 24%) | P value | |
| Age (years) | 33.6 ± 14.5 | 32.2 ± 15.1 | 0.001 |
| Males | 9113 (90.8) | 2860 (90.1) | 0.28 |
| EMS time (min) | 70.6 ± 27.9 | 70.8 ± 28.3 | 0.67 |
| Scene time (min) | 24.2 ± 15.8 | 26.9 ± 18.1 | 0.001 |
| Level 1 trauma activation code | 1350 (15.4) | 1058 (37.6) | 0.001 |
| Level 2 trauma activation code | 7177 (82.0) | 1712 (60.9) | 0.001 |
| Vital signs at scene | |||
| Pulse rate | 94.4 ± 19.8 | 88.1 ± 21.5 | 0.001 |
| Systolic blood pressure | 128.7 ± 21.9 | 138.1 ± 25.2 | 0.001 |
| Diastolic blood pressure | 80.1 ± 16.7 | 86.7 ± 21.8 | 0.001 |
| Respiratory rate | 19.3 ± 4.3 | 19.7 ± 5.4 | 0.001 |
| GCS (mean, 95%CI) | 14.30 (14.26-14.34) | 13.03 (12.90-13.15) | 0.001 |
| Vitals at TRU | |||
| Pulse rate | 87.3 ± 16.8 | 103.4 ± 22.4 | 0.001 |
| Systolic blood pressure | 131.2 ± 18.9 | 115.4 ± 21.6 | 0.001 |
| Diastolic blood pressure | 79.4 ± 13.4 | 72.5 ± 16.6 | 0.001 |
| Respiratory rate | 19.4 ± 3.2 | 20.3 ± 4.3 | 0.001 |
| GCS (mean, 95%CI) | 14.08 (14.03-14.14) | 12.22 (12.05-12.38) | 0.001 |
| Cardio-pulmonary resuscitation | 131 (1.3) | 184 (5.8) | 0.001 |
| ED disposition | |||
| Operating room | 1698 (16.9) | 720 (22.7) | 0.001 |
| Intensive care unit | 1917 (19.1) | 1065 (33.6) | 0.001 |
| Step-down unit | 107 (1.1) | 21 (0.7) | 0.001 |
| Floor | 5735 (57.1) | 1261 (39.7) | 0.001 |
| High dependency unit | 214 (2.1) | 45 (1.4) | 0.001 |
| Transfer to another facility | 54 (0.5) | 6 (0.2) | 0.001 |
| Home | 305 (3.0) | 41 (1.3) | 0.001 |
| Died | 9 (0.1) | 14 (0.4) | 0.001 |
| Revised trauma score | 7.6 ± 0.8 | 6.9 ± 1.5 | 0.001 |
| TRISS | 0.97 ± 0.08 | 0.90 ± 0.19 | 0.001 |
| Injury severity score | 11.3 ± 8.2 | 15.9 ± 11.3 | 0.001 |
| Head AIS | 3.3 ± 0.9 | 3.6 ± 1.0 | 0.001 |
| Chest AIS | 2.6 ± 0.7 | 2.7 ± 0.7 | 0.001 |
| Abdomen AIS | 2.5 ± 1.2 | 2.6 ± 1.0 | 0.04 |
| Pelvis AIS | 2.1 ± 0.5 | 2.3 ± 0.7 | 0.001 |
Patients with a high DSI sustained significant injuries, as indicated by higher mean ISS (P = 0.001), greater head AIS (P = 0.001), chest AIS (P = 0.001), abdominal AIS (P = 0.04), and pelvis AIS (P = 0.001), and lower TRISS (P = 0.001) and RTS
Table 2 compares the management and outcomes of the patients with trauma. The need for intubation (P = 0.001), exploratory laparotomy (P = 0.001), ECMO (P = 0.001), REBOA (P = 0.001), prehospital fluid administration (P = 0.001), and blood transfusion (P = 0.001) was significantly associated with high DSI compared to low DSI. Moreover, patients with a high DSI frequently required intubation at the scene, whereas those with a low DSI were more likely to be intubated in the ED (P = 0.001). In addition, the rates of FAST positivity (P = 0.001) and in-hospital complications, such as VAP (P = 0.001), acute respiratory distress syndrome (P = 0.001), thromboembolic events (P = 0.001), abdominal compartment syndrome (P = 0.002), multiorgan failure (P = 0.001), and disseminated intravascular coagulation (P = 0.01), were significantly higher in the high-DSI group. Furthermore, patients with a high DSI were found to have a longer hospital stay (P = 0.001) and critical care unit stay (P = 0.001) and required prolonged mechanical ventilation (P = 0.001). The overall in-hospital mortality rate was 2.8%, and patients with a high DSI (7.3% vs 1.4%, P = 0.001) had a 5-fold higher risk of mortality than those with a low DSI. Patients with a low DSI were more likely to be discharged home (88.3% vs 75.1%; P = 0.001), whereas those with a high DSI frequently required rehabilitation (8.0% vs 4.6%; P = 0.001).
| DSI ≤ 0.1 (n = 10039; 76%) | DSI > 0.1 (n = 3173; 24%) | P value | |
| Intubation | 1315 (13.1) | 1108 (34.9) | 0.001 |
| Intubation location | |||
| Scene | 433 (33.0) | 539 (49.0) | 0.001 |
| Trauma resuscitation unit | 550 (42.0) | 397 (36.1) | 0.001 |
| Operating room | 226 (17.2) | 128 (11.6) | 0.001 |
| Intensive care unit | 72 (5.5) | 27 (2.5) | 0.001 |
| Floor | 12 (0.9) | 3 (0.3) | 0.001 |
| Referring facility | 18 (1.4) | 6 (0.5) | 0.001 |
| FAST done | 9570 (95.3) | 3047 (96.0) | 0.09 |
| Negative | 8786 (93.9) | 2638 (88.5) | 0.001 |
| Positive | 445 (4.8) | 304 (10.2) | 0.001 |
| Undetermined | 125 (1.3) | 39 (1.3) | 0.001 |
| Exploratory laparotomy | 380 (3.8) | 281 (8.9) | 0.001 |
| ECMO | 8 (0.1) | 11 (0.3) | 0.001 |
| REBOA | 1 (0.0) | 3 (0.1) | 0.01 |
| Prehospital fluid administered | 3626 (36.1) | 1392 (43.9) | 0.001 |
| Prehospital fluid (mL) | 466 ± 399 | 585 ± 472 | 0.001 |
| Blood transfusion | 1358 (13.5) | 1039 (32.7) | 0.001 |
| Total blood units transfused | 3 (1-73) | 4 (1-68) | 0.001 |
| Massive transfusion protocol | 155 (1.5) | 269 (8.5) | 0.001 |
| In-hospital complications | |||
| Sepsis | 98 (1.0) | 87 (2.7) | 0.001 |
| Ventilator-associated pneumonia | 263 (2.6) | 226 (7.1) | 0.001 |
| Acute respiratory distress syndrome | 56 (0.6) | 51 (1.6) | 0.001 |
| Thromboembolic events | 46 (0.5) | 39 (1.2) | 0.001 |
| Abdominal compartment syndrome | 3 (0.05) | 7 (0.2) | 0.002 |
| Multiorgan failure | 6 (0.1) | 12 (0.4) | 0.001 |
| Disseminated intravascular coagulation | 1 (0.01) | 4 (0.1) | 0.01 |
| Hospital length of stay | 5 (1-505) | 7 (1-360) | 0.001 |
| ICU length of stay | 3 (1-155) | 5 (1-161) | 0.001 |
| Ventilatory days | 3 (1-180) | 5 (1-115) | 0.001 |
| Mortality | 141 (1.4) | 231 (7.3) | 0.001 |
| Death on arrival | 1 (0.02) | 6 (0.2) | 0.001 |
| Discharge disposition | |||
| Home | 8840 (88.3) | 2376 (75.1) | 0.001 |
| Rehabilitation | 461 (4.6) | 254 (8.0) | 0.001 |
| Long-term care | 72 (0.7) | 61 (1.9) | 0.001 |
| Transfer to another hospital | 499 (5.0) | 242 (7.6) | 0.001 |
| Died | 141 (1.4) | 231 (7.3) | 0.001 |
Table 3 shows the univariate correlation between the DSI and the other relevant covariates. DSI was significantly correlated with ISS (r = 0.223), GCS (r = -0.239), TRISS (r = -0.297), RTS (r = -0.301), head AIS (r = 0.166), chest AIS (r = 0.065), blood transfusion (r = 0.20), and HLOS (r = 0.14) (P = 0.001 for all).
| Variable | Pearson correlation (r) | P value |
| Age | 0.002 | 0.79 |
| Injury severity score | 0.223 | 0.001 |
| Glasgow coma scale | -0.239 | 0.001 |
| TRISS | -0.297 | 0.001 |
| Revised trauma score | -0.301 | 0.001 |
| Blood transfusion units | 0.205 | 0.001 |
| Head AIS | 0.166 | 0.001 |
| Chest AIS | 0.065 | 0.001 |
| Hospital length of stay | 0.142 | 0.001 |
| ICU length of stay | 0.109 | 0.001 |
Figure 1A shows the receiver operating characteristic curve analysis. For mortality prediction, high DSI had better specificity, negative predictive value, and negative likelihood ratio (77%, 99%, and 0.49, respectively). Similarly, high DSI had better specificity, negative predictive value, and negative likelihood ratio (77.3%, 98.5%, and 0.47%, respectively) for predicting the need for MTP (Figure 1B) and exploratory laparotomy (Figure 1C). Figure 2 shows the multivariate reg
This study highlighted that DSI based on a nationally representative population could accurately predict the need for massive blood transfusion and exploratory laparotomy in severely injured patients. Therefore, a great difference between the SI in the ED and at the accident scene in trauma patients indicates the likelihood of the need for blood transfusion and surgical intervention. Additionally, a high DSI is associated with an increased risk of mortality in patients with injuries. Our findings suggest that an increase in heart rate at the same systolic blood pressure level in trauma patients signifies an increased risk of poor outcomes. In line with our observations, recent literature has highlighted the accuracy of DSI in predicting mortality and hemodynamic instability in adult[11,12,15] and pediatric[10] trauma patients. We also demon
Numerous adjusted scoring systems have been proposed to improve the accuracy of outcome predictions in patients[7,16-18]. However, only a limited number of studies in trauma patients[1,2,11,12] have explored the prognostic implications of DSI, which could be an effective early triage tool to identify minimal bleeding compared to conventional vital signs as well as SI at the scene and in the ED. Shock measurement that accounts for temporal variation is anticipated to be better than shock measures obtained at a single time point post-injury[19].
In our study, patients with a high DSI had prolonged scene times and markedly impaired vital signs, including a lower GCS score. Such an association between DSI and initial physiological parameters was foreseeable as severely injured patients at the accident scene require more time to stabilize before being transported to the ED for definitive resuscitation and urgent lifesaving interventions[20]. Similarly, an earlier retrospective observational study by Funabiki et al[21] of 139242 elderly trauma patients demonstrated an association between high DSI and emergency hemostatic resuscitation, especially among patients presenting with hypertension and a low GCS score on hospital arrival. Furthermore, in our study, the proportion of TT1 was higher in patients with a high DSI, and these patients had a greater chance of being transferred to the operating room and ICU directly from the ED. The high TT1 in patients with elevated DSI suggests greater urgency and severity of trauma. This would prompt a quicker decision-making to initiate massive blood tran
Furthermore, our research demonstrated that patients with a high DSI were more likely to sustain severe injuries, as evidenced by frequent anatomical injuries, greater ISS, and lower TRISS and RTS scores. Therefore, the degree of physiological derangement is associated with the severity of the injury, which mainly depends on the anatomical injury location[1,23]. Consistent with our findings, a previous study by Funabiki et al[21] reported a significantly higher rate of severe injuries (ISS > 15) in patients with high DSI than in those with low DSI. This indicates that DSI can serve as an indicator of evolving trauma severity, with an increase in DSI suggesting hypovolemic shock, continued bleeding, and inadequate resuscitation in the field[11,15,24]. Bardes et al[25] conducted a retrospective study including 549 adults with blunt chest or abdominal trauma who were transferred from the scene and 127 referred from other facilities. This study revealed a positive correlation between ISS and SI, with no observed correlation between ISS and DSI. Notably, variability in prehospital care, resuscitation approaches, existing health conditions, and the timing of interventions can affect the initial physiological condition of patients, injury severity, and outcomes.
As shown in Table 2, a high DSI was associated with a higher rate of interventions (exploratory laparotomy, intubation, ECMO, and REBOA), hemostatic resuscitation (prehospital fluid administration and blood transfusion), and in-hospital complications than a low DSI. Our results are consistent with a previous study involving adult trauma patients con
Kin et al[15] conducted a retrospective observational analysis of 628 adult patients with trauma who were presented to the ED. The study revealed no notable differences in length of hospital and ICU stay, amount of blood transfused, or duration of mechanical ventilation associated with DSI. In contrast, in our study, DSI significantly correlated with hospital and ICU stay, ventilatory days, and number of blood units transfused. This variability could arise because the previous study used different cutoff values for defining high DSI (≥ 0.3), as opposed to the present study (DSI > 0.1), leading to discrepancies in the observed associations.
Previous studies have shown that DSI is associated with the worst clinical outcomes in trauma patients[1,2,21,29]. Consistent with these observations, the overall in-hospital mortality rate was 2.8% in our study, and a high DSI was significantly associated with the risk of mortality. Funabiki et al[21] reported a significantly higher rate of in-hospital mortality in elderly trauma patients with a high DSI (OR = 1.27). Huang et al[2] demonstrated that a high DSI upon ED admission is associated with increased in-hospital and early mortality among critically ill trauma patients who were transferred to the ICU. Kim et al[1] reported a significantly higher rate of in-hospital mortality in the high DSI (> 0.1) group than in the low DSI (≤ 0.1) (2.0% vs 0.8%, P < 0.01). Similarly, a previous study involving trauma patients with moderate injury severity identified a correlation between DSI and 48-h mortality[29].
In this study, we performed multivariate regression analysis to identify predictors of mortality and the need for ma
Another study reported that in-hospital mortality (aOR = 2.82), the need for massive transfusion (aOR = 5.24), embolization (aOR = 3.15), and surgery (aOR = 1.29) were independently associated with a high DSI (> 0.1)[1]. These results imply that high DSI levels could serve as an indicator for identifying patients in shock and those at a higher risk of mortality, necessitating prompt intervention[30].
Early identification of such patients based on DSI levels could enable emergency physicians to intervene promptly and implement appropriate treatments and interventions[31,32] to improve patient outcomes and increase the chances of survival following trauma.
Based on the sensitivity analysis for mortality and the need for massive transfusion and exploratory laparotomy, the present study determined a threshold value of 0.1. Consequently, a DSI > 0.1 is deemed clinically relevant for detecting minor physiological changes and identifying patients at risk of mortality and those requiring massive transfusion and emergency surgery. Our findings align with those of previous investigations[1,11,13,21], which also identified > 0.1 as the cutoff value for high DSI in trauma patients. Based on our findings, DSI > 0.1 appears to have moderate or modest predictive value for mortality and the need for massive transfusion in trauma patients; however, its predictive value for determining the necessity of exploratory laparotomy seems to be limited. Therefore, clinicians should consider additional factors and clinical assessments when making decisions regarding surgical intervention in patients with trauma.
This observational study has limitations, primarily owing to its retrospective and single-institution design. Second, the cutoff values for DSI may vary across different trauma systems; therefore, the generalizability of our findings may be limited to other regional trauma centers in rural settings. Third, we could not address the possible difficulty of recording prehospital vital signs by EMS providers, particularly in severely injured patients. Fourth, we could not ascertain the causal relationship between high DSI and the increased mortality rate observed within the cohort. Fifth, we lacked data on resuscitation involving interventions and drugs administered in the prehospital setting, which could influence heart rate and, subsequently, the DSI. Therefore, it was challenging to determine whether a high DSI resulted from physio
In conclusion, in addition to sex-biased observations, almost one-quarter of the study cohort had a higher DSI among young trauma patients. DSI was an independent predictor of mortality, massive blood transfusion, and exploratory laparotomy in patients with trauma. Therefore, it could potentially serve as a tool for predicting unfavorable outcomes and the necessity for hemostatic intervention. In addition, a high DSI correlated significantly with the other injury severity scores, which require more time and imaging to be ready to use. Therefore, it is imperative to use the DSI and devise a treatment plan that considers the anatomical location and severity of the injury. Overall, the DSI is a practical, simple bedside tool for triaging and prognosis in young patients with trauma. Further research is necessary to validate these findings and to establish a more accurate cutoff point for DSI that correlates with the indications for exploratory laparotomy in patients with trauma.
The authors thank all the staff of the trauma registry database at the Trauma Surgery Section, Department of Surgery, Hamad General Hospital, Doha, Qatar.
| 1. | Kim DK, Jeong J, Shin SD, Song KJ, Hong KJ, Ro YS, Kim TH, Jamaluddin SF; PATOS Clinical Research Network. Association between prehospital field to emergency department delta shock index and in-hospital mortality in patients with torso and extremity trauma: A multinational, observational study. PLoS One. 2021;16:e0258811. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 13] [Reference Citation Analysis (0)] |
| 2. | Huang YS, Chiu IM, Tsai MT, Lin CF, Lin CF. Delta Shock Index During Emergency Department Stay Is Associated With in Hospital Mortality in Critically Ill Patients. Front Med (Lausanne). 2021;8:648375. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 12] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 3. | Fite RO, Mesele M, Wake M, Assefa M, Tilahun A. Severity of Injury and Associated Factors among Injured Patients Who Visited the Emergency Department at Wolaita Sodo Teaching and Referral Hospital, Ethiopia. Ethiop J Health Sci. 2020;30:189-198. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 4. | Mitchell RJ, Cameron CM, McClure R. Higher mortality risk among injured individuals in a population-based matched cohort study. BMC Public Health. 2017;17:150. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 13] [Cited by in RCA: 11] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 5. | Rossaint R, Bouillon B, Cerny V, Coats TJ, Duranteau J, Fernández-Mondéjar E, Hunt BJ, Komadina R, Nardi G, Neugebauer E, Ozier Y, Riddez L, Schultz A, Stahel PF, Vincent JL, Spahn DR; Task Force for Advanced Bleeding Care in Trauma. Management of bleeding following major trauma: an updated European guideline. Crit Care. 2010;14:R52. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 551] [Cited by in RCA: 480] [Article Influence: 32.0] [Reference Citation Analysis (0)] |
| 6. | Latif RK, Clifford SP, Baker JA, Lenhardt R, Haq MZ, Huang J, Farah I, Businger JR. Traumatic hemorrhage and chain of survival. Scand J Trauma Resusc Emerg Med. 2023;31:25. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 44] [Reference Citation Analysis (0)] |
| 7. | El-Menyar A, Asim M, Ramzee AF, Nabir S, Ahmed MN, Al-Thani A, Al-Abdulmalek A, Al-Thani H. Bio-Shock Index: Proposal and Rationale for a New Predictive Tool for In-Hospital Mortality in Patients with Traumatic Brain Injury. World Neurosurg. 2019;132:e169-e177. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 8. | van Veelen MJ, Brodmann Maeder M. Hypothermia in Trauma. Int J Environ Res Public Health. 2021;18. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 25] [Cited by in RCA: 37] [Article Influence: 9.3] [Reference Citation Analysis (0)] |
| 9. | Moore FA, Nelson T, McKinley BA, Moore EE, Nathens AB, Rhee P, Puyana JC, Beilman GJ, Cohn SM; StO2 Study Group. Massive transfusion in trauma patients: tissue hemoglobin oxygen saturation predicts poor outcome. J Trauma. 2008;64:1010-1023. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 68] [Cited by in RCA: 72] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 10. | Asmar S, Zeeshan M, Khurrum M, Con J, Chehab M, Bible L, Latifi R, Joseph B. Delta Shock Index Predicts Outcomes in Pediatric Trauma Patients Regardless of Age. J Surg Res. 2021;259:182-191. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 11. | Joseph B, Haider A, Ibraheem K, Kulvatunyou N, Tang A, Azim A, O'Keeffe T, Gries L, Vercruysse G, Rhee P. Revitalizing Vital Signs: The Role of Delta Shock Index. Shock. 2016;46:50-54. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 24] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 12. | Schellenberg M, Strumwasser A, Grabo D, Clark D, Matsushima K, Inaba K, Demetriades D. Delta Shock Index in the Emergency Department Predicts Mortality and Need for Blood Transfusion in Trauma Patients. Am Surg. 2017;83:1059-1062. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 21] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 13. | Hosseinpour H, Anand T, Bhogadi SK, Colosimo C, El-Qawaqzeh K, Spencer AL, Castanon L, Ditillo M, Magnotti LJ, Joseph B. Emergency Department Shock Index Outperforms Prehospital and Delta Shock Indices in Predicting Outcomes of Trauma Patients. J Surg Res. 2023;291:204-212. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 6] [Reference Citation Analysis (0)] |
| 14. | El-Menyar A, Goyal P, Tilley E, Latifi R. The clinical utility of shock index to predict the need for blood transfusion and outcomes in trauma. J Surg Res. 2018;227:52-59. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 40] [Article Influence: 5.7] [Reference Citation Analysis (0)] |
| 15. | Kim MJ, Park JY, Kim MK, Lee JG. Usefulness of Shock Index to Predict Outcomes of Trauma Patient: A Retrospective Cohort Study. J Trauma Inj. 2019;32:17-25. [RCA] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 16. | Wu SC, Chou SE, Liu HT, Hsieh TM, Su WT, Chien PC, Hsieh CH. Performance of Prognostic Scoring Systems in Trauma Patients in the Intensive Care Unit of a Trauma Center. Int J Environ Res Public Health. 2020;17. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 20] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 17. | Carsetti A, Antolini R, Casarotta E, Damiani E, Gasparri F, Marini B, Adrario E, Donati A. Shock index as predictor of massive transfusion and mortality in patients with trauma: a systematic review and meta-analysis. Crit Care. 2023;27:85. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 27] [Reference Citation Analysis (0)] |
| 18. | Lee YT, Bae BK, Cho YM, Park SC, Jeon CH, Huh U, Lee DS, Ko SH, Ryu DM, Wang IJ. Reverse shock index multiplied by Glasgow coma scale as a predictor of massive transfusion in trauma. Am J Emerg Med. 2021;46:404-409. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 20] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 19. | Rau CS, Wu SC, Kuo SC, Pao-Jen K, Shiun-Yuan H, Chen YC, Hsieh HY, Hsieh CH, Liu HT. Prediction of Massive Transfusion in Trauma Patients with Shock Index, Modified Shock Index, and Age Shock Index. Int J Environ Res Public Health. 2016;13. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 34] [Cited by in RCA: 53] [Article Influence: 5.9] [Reference Citation Analysis (0)] |
| 20. | Yuksen C, Angkoontassaneeyarat C, Thananupappaisal S, Laksanamapune T, Phontabtim M, Namsanor P. Accuracy of Trauma on Scene Triage Screening Tool (Shock Index, Reverse Shock Index Glasgow Coma Scale and National Early Warning Score) to Predict the Severity of Emergency Department Triage: A Retrospective Cross-Sectional Study. Open Access Emerg Med. 2023;15:79-91. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 21. | Funabiki S, Yamamoto R, Homma K, Yoshizawa J, Jia S, Takanashi Y, Kahara R, Sasaki J. Delta Shock Index and higher incidence of emergency surgery in older adults with blunt trauma. Eur J Trauma Emerg Surg. 2024;50:561-566. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 22. | Cooper MC, Srivastava G. Correlation of Level of Trauma Activation With Emergency Department Intervention. Pediatr Emerg Care. 2018;34:369-375. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 23. | van Wessem KJP, Leenen LPH, Hietbrink F. Physiology dictated treatment after severe trauma: timing is everything. Eur J Trauma Emerg Surg. 2022;48:3969-3979. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 7] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 24. | Cannon CM, Braxton CC, Kling-Smith M, Mahnken JD, Carlton E, Moncure M. Utility of the shock index in predicting mortality in traumatically injured patients. J Trauma. 2009;67:1426-1430. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 167] [Cited by in RCA: 192] [Article Influence: 12.0] [Reference Citation Analysis (0)] |
| 25. | Bardes JM, Price BS, Adjeroh DA, Doretto G, Wilson A. Emergency medical services shock index is the most accurate predictor of patient outcomes after blunt torso trauma. J Trauma Acute Care Surg. 2022;92:499-503. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 5] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 26. | Asim M, El-Menyar A, Chughtai T, Al-Hassani A, Abdelrahman H, Rizoli S, Al-Thani H. Shock Index for the Prediction of Interventions and Mortality in Patients With Blunt Thoracic Trauma. J Surg Res. 2023;283:438-448. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 27. | El-menyar A, Peralta R, Latifi R, Consunji RJ, Al-thani H. Shock Index: A Simple Predictor of Exploratory Laparotomy and Massive Blood Transfusion Protocol in Patients with Abdominal Trauma. J Am Coll Surg. 2018;227:e64. [RCA] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 28. | El-Menyar A, Jabbour G, Asim M, Abdelrahman H, Mahmood I, Al-Thani H. Shock index in patients with traumatic solid organ injury as a predictor of massive blood transfusion protocol activation. Inj Epidemiol. 2019;6:41. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 12] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 29. | Bruijns SR, Guly HR, Bouamra O, Lecky F, Wallis LA. The value of the difference between ED and prehospital vital signs in predicting outcome in trauma. Emerg Med J. 2014;31:579-582. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 28] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 30. | Kawai Y, Yamamoto K, Miyazaki K, Asai H, Fukushima H. Explainable Prediction Model of the Need for Emergency Hemostasis Using Field Information During Physician-Staffed Helicopter Emergency Medical Service Interventions: A Single-Center, Retrospective, Observational Pilot Study. Air Med J. 2023;42:336-342. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 4] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 31. | Haider AA, Azim A, Rhee P, Kulvatunyou N, Ibraheem K, Tang A, O'Keeffe T, Iftikhar H, Vercruysse G, Joseph B. Substituting systolic blood pressure with shock index in the National Trauma Triage Protocol. J Trauma Acute Care Surg. 2016;81:1136-1141. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 25] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 32. | Tran A, Taljaard M, Abdulaziz KE, Matar M, Lampron J, Steyerberg EW, Vaillancourt C. Early identification of the need for major intervention in patients with traumatic hemorrhage: development and internal validation of a simple bleeding score. Can J Surg. 2020;63:E422-E430. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 8] [Article Influence: 1.6] [Reference Citation Analysis (0)] |