Published online Dec 9, 2024. doi: 10.5492/wjccm.v13.i4.98579
Revised: September 4, 2024
Accepted: September 9, 2024
Published online: December 9, 2024
Processing time: 123 Days and 12.6 Hours
Clavicle fractures are frequent orthopedic injuries, often resulting from direct trauma or a fall. Most clavicle fractures are treated conservatively without any complications or adverse effects. Concomitant injuries of the subclavian vein or artery are rarely encountered and most commonly associated with high-energy trauma or comminuted clavicle fractures. They are potentially life-threatening conditions leading to hemorrhage, hematoma, pseudoaneurysm or upper limb ischemia. However, the clinical presentation might be obscure and easily missed, particularly in closed and minimally displaced clavicular fractures, and timely diagnosis relies on early clinical suspicion. Currently, computed tomography angiography has largely replaced conventional angiography for the assessment of subclavian vessel patency, as it demonstrates high accuracy and temporal reso
Core Tip: Clavicle fractures complicated by vascular injuries are rare and potentially life-threatening conditions. Diagnosis of subclavian vessel injuries might be substantially delayed due to the overshadowing presence of the more obvious fracture symptoms and pain. Sound knowledge of the anatomy, better understanding of the severity of injury and fracture pattern and thorough clinical examination are important to raise the suspicion of a vascular injury and optimize medical care. Clavicle fractures combined with subclavian vessel injuries that are associated with serious hemorrhage or limb ischemia should be addressed operatively to restore vascular continuity and upper limb function. Future research should aim at optimizing diagnostic protocols and exploring advanced therapeutic techniques to enhance patient care in these complex cases.
- Citation: Chalidis B, Davitis V, Papadopoulos P, Pitsilos C. Subclavian vessels injury: An underestimated complication of clavicular fractures. World J Crit Care Med 2024; 13(4): 98579
- URL: https://www.wjgnet.com/2220-3141/full/v13/i4/98579.htm
- DOI: https://dx.doi.org/10.5492/wjccm.v13.i4.98579
Clavicular fractures are common injuries, particularly among young and active individuals, often resulting from falls, sports activities and traffic accidents[1]. They show the highest incidence of all shoulder girdle fractures and account for up to 4% of all adult fractures[2,3]. The majority of clavicle fractures occur at the midshaft region of the clavicle, which is the weakest point of the bone[4].
Although most clavicular fractures heal uneventfully without significant complications, the proximity of fracture location to major neurovascular structures, such as the subclavian vessels and brachial plexus, carries the risk of serious and potentially life-threatening conditions[5]. Subclavian vessels are more susceptible to injury in trauma patients with spiral or oblique clavicle fracture where sharp bone fragments may lacerate and damage the surrounding soft tissues[6]. Injury of the subclavian vessels can lead to hematoma formation, pseudoaneurysm, compromised blood flow to the arm and major bleeding, necessitating early medical attention and often urgent surgical intervention[7]. However, the clinical presentation might be obscure and easily missed, particularly in closed and minimally displaced clavicular fractures, and timely diagnosis relies on early clinical suspicion[6,8]. Therefore, understanding of bone and neurovascular anatomy of the clavicular region is essential for the effective management of complex injuries with simultaneous involvement of the clavicle and subclavian artery or vein[9].
This review aims to highlight the significance of prompt diagnosis of subclavian vessel injuries associated with clavicular fractures as a key factor to optimize medical care, improve recovery and minimize complications. Furthermore, the current evidence regarding the available treatment options for the treatment of these complex injuries and the expected functional outcome is thoroughly discussed.
The clavicle is a s-shaped long bone that functions as a strut between the sternum and the scapula, thereby playing a crucial role in shoulder biomechanics[10]. It is divided into three parts: (1) The medial (sternal) end; (2) The shaft; and (3) The lateral (acromial) end[11]. The medial clavicle articulates with the manubrium of the sternum at the sternoclavicular joint, while the lateral part of the bone articulates with the acromion of the scapula forming the acromioclavicular joint[6]. The clavicle also serves as an attachment site for several muscular structures, including the deltoid, trapezius, subclavius, pectoralis major, and sternocleidomastoid muscles[12].
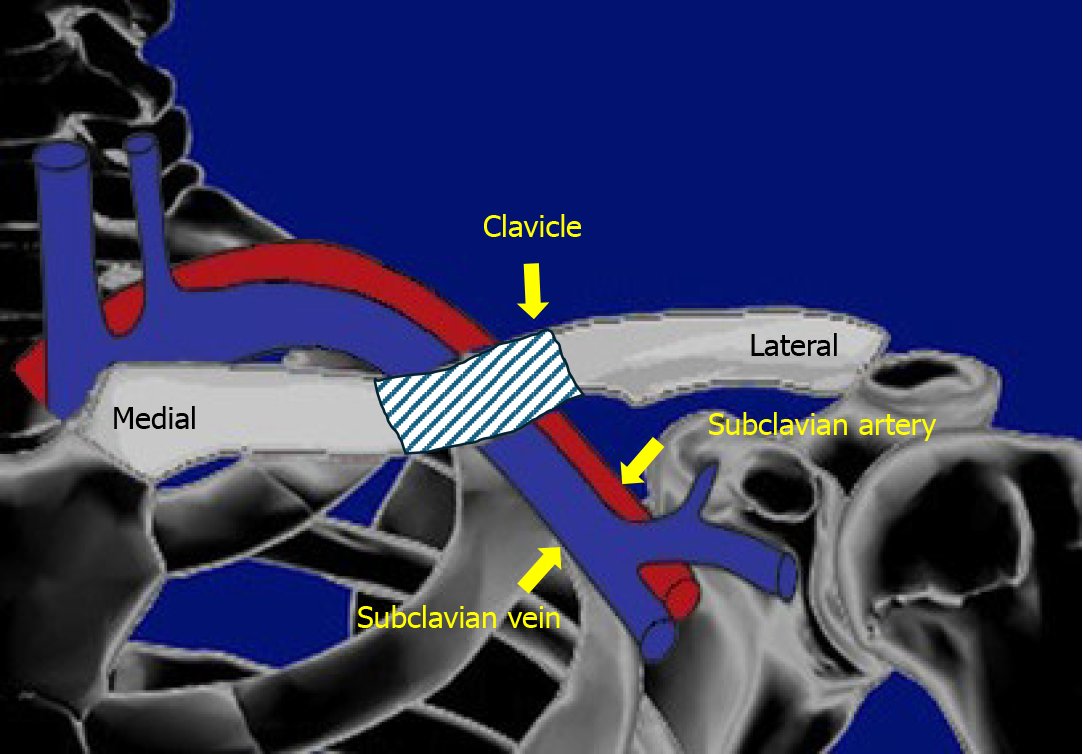
The subclavian artery and vein are located adjacent to the clavicle and facilitate blood supply and drainage of upper limb, respectively[13].
The subclavian artery originates from the brachiocephalic trunk on the right side and directly from the arch of the aorta on the left side[14]. It travels laterally and passes posterior to the clavicle and over the first rib, before becoming the axillary artery at the lateral border of the first rib[12]. In relation to the clavicle, the artery is located postero-superiorly at the medial edge of the bone but gradually becomes postero-inferior at the midshaft and inferior laterally[15]. A mean bone to vessel distance of beyond 10 mm has been found along its entire course[16].
The subclavian vein is formed by the union of the axillary and cephalic veins and runs parallel and anterior to the subclavian artery[9,13]. It travels behind the clavicle and merges with the internal jugular vein to form the brachiocephalic vein[17]. At the medial half of the clavicle, the mean bone to vein distance is less than 10 mm, and this close proximity between the two structures predisposes to vessel rupture and hemorrhage during injury or at the time of fracture fixation with plates and screws (Figure 1)[16].
Clavicular fractures are a common musculoskeletal injury, accounting for approximately 2.6% to 5% of all adult fractures and 35% to 44% of acute shoulder girdle injuries[2]. The midshaft portion of the clavicle is the most frequently affected location, constituting about 62% to 81% of all clavicular fractures[18,19]. The subclavian vessels may be damaged at the time of the initial injury or during fracture fixation or even in the course of conservative management of clavicle fractures[19]. The overall incidence of subclavian vessel injury after clavicular fractures is relatively low and estimated at around 0.3% to 3%[2,20]. Despite the rarity of the complication, the implications of such injuries are severe and potentially catastrophic as subclavian vessels are the main conduits responsible for the blood supply of upper limbs[21]. Studies have shown that subclavian vessel injuries are more likely to occur in clavicle fracture patterns with significant displacement and comminution or after high-energy trauma, such as motor vehicle accidents and falls from height[22,23]. Additionally, clavicular fractures combined with penetrating upper extremity and chest trauma have a higher incidence of vascular injuries compared to blunt trauma[24]. These conditions can lead to life-threatening complications including hemorrhage, ischemia and nerve damage, requiring urgent diagnosis and accurate intervention[25]. A comprehensive review by Katras et al[26], which included patients suffering from clavicular fractures complicated by vascular injuries, showed that the majority of those conditions needed immediate surgical intervention, highlighting the importance of early detection and management. Moreover, another study by Smith and Gupta[21] emphasized that the diagnosis of subclavian vessel injury might be substantially delayed due to the overshadowing presence of the more obvious fracture symptoms and pain.
The underlying mechanism of subclavian vessels injury at the time of clavicular fractures is multifaceted and involves both direct and indirect trauma[27,28]. Sound knowledge of the anatomy of the area and better understanding of the severity of injury and fracture characteristics would raise early the suspicion of a vascular injury and would prevent a life-threatening hemorrhagic complication (Table 1)[29].
| Direct trauma | Indirect trauma |
| Laceration or puncture from sharp fracture fragments | Crush between clavicle and adjacent bones |
| Penetration from comminuted fragments after high energy mechanism | Acute external compression after hematoma formation |
| Perforation from fixation implants | Stretch after distraction injury |
| Chronic compression from hypertrophic callus |
Direct laceration or puncture of the subclavian vessels may be encountered directly by the sharp edges of fractured clavicle fragments[30]. This could be more common in comminuted midshaft clavicular fractures, where the displaced fracture ends may impinge and damage the subclavian artery or vein[28]. In high-energy trauma, such as motor vehicle accidents or falls from height, the fracture fragments can also penetrate the subclavian vessels, leading to severe vascular damage and hemorrhage[31]. On the other hand, iatrogenic injury of subclavian vessels may occur during surgical treatment with open reduction and internal fixation. Vessel perforation by the drill bit or screws is likely to result in acute intraoperative bleeding or late vascular and neurological complications[32,33].
At the time of injury, subclavian artery and vein can be crushed against the first rib or displaced clavicular bone fragments causing vessel occlusion, thrombosis or pseudoaneurysm formation[27,34-36]. Moreover, traction forces during fall or vehicle accidents could stretch subclavian vessels beyond their capacity and lead to intimal tears or vessel spasm and secondary restriction of blood flow[37]. On some occasions, excessive bleeding from the medullary cavity of the fractured clavicle results in hematoma formation in the surrounding space and subsequent subclavian vessel compression and obstruction[26,38,39]. Similarly, external compression from callus formation in the setting of hypertrophic nonunion may predispose to late vascular insufficiency[40].
Subclavian vessel injury following clavicular fractures may be presented with many different clinical features, depending on the type of vascular lesion (Table 2)[26,28,41]. This heterogeneity of symptoms and clinical course underlines the importance of meticulous clinical examination and proper laboratory screening for confirmation of the arterial or vein injury[42].
| Subclavian artery | Subclavian vein |
| Laceration and tear | Laceration and tear |
| Occlusion, stenosis, and external compression | Thrombosis |
| Aneurysm, pseudoaneurysm, pseudoaneurysm rupture or thrombosis | Aneurysm |
| Arteriovenous fistula | |
Post-traumatic subclavian artery laceration following a clavicle fracture can cause hypovolemic shock, anemia, co
Occlusion or severe compression of the subclavian artery can result in limb ischemia and decreased perfusion of upper extremity[27,42,44]. Pallor, coldness and delayed capillary refill are strong indications for immediate arteriography to evaluate the blood flow to the extremity and the location of the lesion[42]. Sodhi et al[28] described a case of a young man who admitted with shock and decreased level of consciousness in the emergency department after a motor vehicle accident. The patient had no palpable left upper extremity pulses and emergent angiogram revealed a complete occlusion of his left subclavian artery as a result of a displaced medial midshaft clavicle fracture. Similarly, Katras et al[26], reported a 52-year-old man who presented to the hospital with left arm ischemia due to distal subclavian artery obstruction after a posteriorly displaced distal clavicle fracture. Apart from acute subclavian artery involvement, delayed external vascular compression during shoulder abduction and development of thoracic outlet syndrome have been also described due to hypertrophic callus formation after clavicular fracture union or more often non-union[40,45].
Acute or late arterial thrombosis is another rare complication of clavicle fractures[41,46]. Lyons et al[47] reported a 12-year-old girl with absent right radial pulse after a fall while cheerleading. Chest and shoulder x-rays illustrated a closed right clavicle fracture, while angiogram and Doppler ultrasound confirmed an acute incomplete subclavian arterial thrombosis. On the other hand, Van Schaik et al[41] described a middle-aged man who presented with ipsilateral upper extremity numbness and claudication, five years after a conservatively treated clavicular fracture. Imaging studies revealed subclavian and brachial artery thrombosis, which were attributed to fracture nonunion and mobility of bone fragments.
Secondary formation of subclavian artery aneurysm or pseudoaneurysm has been also reported after a clavicular fracture. A pseudoaneurysm (or false aneurysm) is determined by a tear in the arterial wall and collection of blood around the vessel and it is much more common than a true aneurysm after clavicular fractures[48-50]. It may remain asymptomatic for a long time exhibiting a tumor-like lesion appearance or it may be thrombosed or ruptured[42,51]. Delayed onset of paresthesia and development of brachial plexopathy could be also symptoms of subclavian artery pseudoaneurysm formation[52]. In the case reported by Rodriguez-Merchan and Gomez-Cardero[53], an arterial pseudoaneurysm was presented as a supraclavicular mass at 3 months after a closed clavicle fracture. As the fracture was not healed, a correlation between fracture delayed union and development of pseudoaneurysm was established. In another published case report, Pallet et al[54] diagnosed a subclavian artery pseudoaneurysm 5 years after open reduction and internal fixation of a midshaft clavicle fracture. The patient complained of ipsilateral hand numbness, the radial pulse was absent and the Allen test demonstrated significantly reduced patency of the radial artery and mildly reduced patency of the ulnar artery. Imaging studies did not reveal any contact of a screw tip with the vessel and the authors related artery pseudoaneurysm development to chronic abrasion of the vessel against the metalware and fracture callus during shoulder movements. Lawson et al[55] reported a case of a young woman who presented with acute axillary and supraclavicular swelling after a sports massage session due to rupture of subclavian artery pseudoaneurysm. The patient had a history of a clavicular fracture nonunion for 16 years and was diagnosed with a small subclavian artery pseudoaneurysm 6 years ago. Both vascular defect and clavicle non-union were addressed surgically with radiological-guided stenting and fracture internal fixation, respectively.
Arteriovenous fistula is another uncommon complication of clavicular fractures[56]. This direct connection between the subclavian artery and vein was previously reported after an open clavicle fracture or as sequelae of a conservatively treatment clavicular fracture[56,57].
Subclavian vein thrombosis is a distinct vascular disorder that has been correlated with clavicle fractures[58,59]. Claes et al[60] presented a case of a 20-year-old man who underwent open reduction and internal fixation of an isolated clavicle fracture after a motocross accident. Two weeks postoperatively, patient’s arm appeared swollen, red-colored, warm and tender with clearly expanded veins. Imaging studies revealed vein thrombosis, which was treated conservatively with administration of low molecular-weight heparin. Subclavian vein thrombosis has been also reported in conservatively treated clavicle fractures, as a result of displaced bone fragments or malunion[35,38].
Laceration of subclavian vein and subsequent bleeding or hematoma formation have been described at the time of clavicular injury and fracture or during surgical intervention and fracture fixation[37]. Bain et al[32] reported the fatal case of a 34-year old man who received open reduction and internal fixation of a displaced midshaft clavicle fracture. During the operative procedure, the most medial screw penetrated the subclavian vein causing laceration of the vessel and consecutive air embolism. Although bleeding was controlled, patient experienced a sudden hemodynamic collapse and died despite resuscitation efforts. Subclavian vein aneurysm formation as a result of clavicle fracture pseudarthrosis and subsequent development of thoracic outlet syndrome have been also reported in the literature[45].
Patient symptoms and clinical presentation along with early clinical awareness are fundamental for the timely diagnosis of subclavian vessel injury[58,61]. However, imaging studies are necessary to confirm clinical suspicion and guide appropriate treatment decisions. Ultrasonography and Echo-Doppler are non-invasive tools that can be initially applied for the evaluation of subclavian artery and vein integrity[41,56]. However, angiography remains the gold standard for the confirmation of subclavian vascular lesions[62,63]. The classic angiography, including arteriography and venography, has been widely used in both emergent and chronic cases[33,37]. Most recently, computed tomography (CT) angiography has replaced classic angiography for the assessment of vessels patency, as it demonstrates high accuracy and temporal resolution, acute turnaround time and capability of multiplanar reconstruction[39,61,64]. The injection of contrast medium during angiography facilitates detection of vessel disruption or extravasation[64]. Moreover, CT angiography has the additional advantage of 3-dimentional reconstruction of the vessels network providing a more detailed description of the vascular lesion[49].
Depending on the hemodynamic stability of the patient and the severity of the injury, subclavian vessel lesions can be treated conservatively or interventionally.
Conservative treatment of subclavian vessel injuries after clavicle fractures include observation and drug administration. Costa et al[43] described a case of a young man suffering from clavicle and multiple rib fractures. Even though the ipsilateral radial pulse was absent and a distal subclavian artery tear was identified, no vascular intervention was performed and full recovery of vessel patency was confirmed after a 12-month follow-up period. Cooney and Kloss[38] presented a male patient with subclavian vein hematoma formation secondary to clavicle fracture nonunion. As there was no active bleeding or other concomitant neurovascular injuries, the hematoma was successfully treated conservatively with observation and frequent follow-ups, and no further management was required. In another case published by Conant and Hickerson[56], an arteriovenous fistula between the subclavian artery and vein was detected four months after a non-united medial third closed clavicle fracture. The authors commented that the elevated venous pressure due to hypertrophic callus formation resulted in venous dilation and subsequent fistula development. Both bone and vessel lesions were managed with observation alone, as no pain and functional impairment existed.
Anticoagulation therapy is the primary treatment of subclavian vein thrombosis[59,65]. Thrombolysis has been associated with favorable results if administered within the first 14 days from the onset of symptoms[65]. The pharmacologic anticoagulation includes the use of direct oral anticoagulants, vitamin K antagonists or low molecular weight heparin for 3 months to 6 months after the event, without any established advantage of one agent over the others[66]. Among all the available anticoagulants and according to the literature data, the low molecular weight heparin has been most extensively used for the treatment of subclavian vein thrombosis following clavicle fractures with proven effectiveness and safety[35,47,60].
Clavicle fractures combined with subclavian vessel injuries that are associated with serious hemorrhage or limb ischemia should be addressed operatively[67]. In this scenario, the clavicle fracture can be fixed simultaneously through the same approach and after re-establishment of the blood flow[26,34]. Autologous or synthetic vascular grafts are necessary for the restoration of subclavian vein and artery continuity in case of irreparable tears[28]. These can be used as interposition grafts to restore the vascular continuity in situ or as vascular bypass to reroute the blood flow around the lesion[28,43]. However, acute and sharp lacerations of the subclavian artery may be amenable to direct repair with good to excellent outcomes[26].
On the other hand, chronic subclavian artery stenosis can be managed effectively with intravascular intervention and stent placement[46]. Percutaneous vascular stent implantation is the suggested treatment option also for subclavian pseudoaneurysms, as it minimizes the risks of open surgery[33,53,68]. However, development of symptomatic pseudoaneurysms after clavicle fractures may require open surgery if extensive bone overgrowth or prominent metalware are apparent. In this case, repair of pseudoaneurysms should be combined with partial claviculectomy and hardware removal[69,70].
Clavicle fractures associated with traumatic subclavian vessel injuries are infrequent clinical conditions. The symptoms may vary from simple hematoma and soft-tissue swelling to severe limb ischemia and life-threatening hemorrhage[67]. Mortality from such injuries ranges from 5% to 30% but these numbers do not represent the true rate, as some patients do not survive to reach medical care[71]. Regardless the selected treatment choice, early diagnosis and proper assessment of bone fracture and vascular lesion have been associated with full recovery and at least satisfactory functional outcome in the vast majority of cases[72]. However, the paucity of data due to the rarity of injury does not allow the extraction of secure conclusions.
While subclavian vessel injury in the context of clavicular fractures is quite uncommon, its potential severity warrants a high index of suspicion, especially when high-energy trauma and significantly displaced fractures are apparent. Arterial and venous complications may develop immediately at the time of injury or up to years later. Clinical awareness and timely intervention are the key points to achieve good outcome and low mortality rate.
| 1. | Robinson CM. Fractures of the clavicle in the adult. Epidemiology and classification. J Bone Joint Surg Br. 1998;80:476-484. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 377] [Cited by in RCA: 401] [Article Influence: 14.9] [Reference Citation Analysis (0)] |
| 2. | Postacchini F, Gumina S, De Santis P, Albo F. Epidemiology of clavicle fractures. J Shoulder Elbow Surg. 2002;11:452-456. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 588] [Cited by in RCA: 585] [Article Influence: 25.4] [Reference Citation Analysis (0)] |
| 3. | Nowak J, Mallmin H, Larsson S. The aetiology and epidemiology of clavicular fractures. A prospective study during a two-year period in Uppsala, Sweden. Injury. 2000;31:353-358. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 179] [Cited by in RCA: 160] [Article Influence: 6.4] [Reference Citation Analysis (0)] |
| 4. | Nordqvist A, Petersson C. The incidence of fractures of the clavicle. Clin Orthop Relat Res. 1994;127-132. [PubMed] |
| 5. | Degiannis E, Velmahos G, Krawczykowski D, Levy RD, Souter I, Saadia R. Penetrating injuries of the subclavian vessels. Br J Surg. 1994;81:524-526. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 31] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 6. | Parson SH. Clinically Oriented Anatomy, 6th edn. J Anat. 2009;215:474-474. [RCA] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 7. | Raviraja A, Chandrashekar C, Roshan S, Srinivas J. Subclavian artery and vein injury following clavicle fracture due to blunt trauma. Injury Extra. 2009;40:36-38. [DOI] [Full Text] |
| 8. | Rich NM, Hobson RW, Jarstfer BS, Geer TM. Subclavian artery trauma. J Trauma. 1973;13:485-496. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 69] [Cited by in RCA: 50] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 9. | Vatansever A, Demiryürek D, Erçakmak B, Özsoy H, Hazirolan T, Şentürk YE. Redefining the morphometry of subclavian vessels for clavicle fracture treatments. Surg Radiol Anat. 2019;41:365-372. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 10. | Huang JI, Toogood P, Chen MR, Wilber JH, Cooperman DR. Clavicular anatomy and the applicability of precontoured plates. J Bone Joint Surg Am. 2007;89:2260-2265. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 50] [Cited by in RCA: 50] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 11. | von Rüden C, Rehme-Röhrl J, Augat P, Friederichs J, Hackl S, Stuby F, Trapp O. Evidence on treatment of clavicle fractures. Injury. 2023;54 Suppl 5:110818. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Reference Citation Analysis (0)] |
| 12. | Driscoll P. Gray's Anatomy, 39th Edition. Emerg Med J. 2006;23:492-492. [RCA] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 7] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 13. | Lavallée C, Ayoub C, Mansour A, Lambert J, Lebon JS, Lalu MM, Denault A. Subclavian and axillary vessel anatomy: a prospective observational ultrasound study. Can J Anaesth. 2018;65:350-359. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 19] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 14. | Rahimi O, Geiger Z. Anatomy, Thorax, Subclavian Arteries. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing, 2024. [PubMed] |
| 15. | Sinha A, Edwin J, Sreeharsha B, Bhalaik V, Brownson P. A radiological study to define safe zones for drilling during plating of clavicle fractures. J Bone Joint Surg Br. 2011;93:1247-1252. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53] [Cited by in RCA: 47] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 16. | Steinmetz G, Conant S, Bowlin B, Hamilton J, Allen J, Stoner J, White C. The Anatomy of the Clavicle and Its In Vivo Relationship to the Vascular Structures: A 2D and 3D Reconstructive Study Using CT Scans. J Orthop Trauma. 2020;34:e14-e19. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 7] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 17. | Capobianco SM, Fahmy MW, Sicari V. Anatomy, Thorax, Subclavian Veins. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing, 2024. [PubMed] |
| 18. | Herteleer M, Winckelmans T, Hoekstra H, Nijs S. Epidemiology of clavicle fractures in a level 1 trauma center in Belgium. Eur J Trauma Emerg Surg. 2018;44:717-726. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 25] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 19. | Hill JM, McGuire MH, Crosby LA. Closed treatment of displaced middle-third fractures of the clavicle gives poor results. J Bone Joint Surg Br. 1997;79:537-539. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 341] [Cited by in RCA: 344] [Article Influence: 12.3] [Reference Citation Analysis (0)] |
| 20. | Leroux T, Wasserstein D, Henry P, Khoshbin A, Dwyer T, Ogilvie-Harris D, Mahomed N, Veillette C. Rate of and Risk Factors for Reoperations After Open Reduction and Internal Fixation of Midshaft Clavicle Fractures: A Population-Based Study in Ontario, Canada. J Bone Joint Surg Am. 2014;96:1119-1125. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 100] [Cited by in RCA: 106] [Article Influence: 9.6] [Reference Citation Analysis (0)] |
| 21. | Smith AA, Gupta N. Subclavian Artery Trauma. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing, 2024. [PubMed] |
| 22. | Tanmit P, Angkasith P, Teeratakulpisarn P, Thanapaisal C, Wongkonkitsin N, Prasertcharoensuk S, Panich C. Treatment Outcome of Traumatic Subclavian Artery Injuries. Vasc Health Risk Manag. 2021;17:481-487. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 4] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 23. | Cox CS Jr, Allen GS, Fischer RP, Conklin LD, Duke JH, Cocanour CS, Moore FA. Blunt versus penetrating subclavian artery injury: presentation, injury pattern, and outcome. J Trauma. 1999;46:445-449. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 36] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 24. | Gottschalk HP, Dumont G, Khanani S, Browne RH, Starr AJ. Open clavicle fractures: patterns of trauma and associated injuries. J Orthop Trauma. 2012;26:107-109. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 11] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 25. | Zlowodzki M, Zelle BA, Cole PA, Jeray K, McKee MD; Evidence-Based Orthopaedic Trauma Working Group. Treatment of acute midshaft clavicle fractures: systematic review of 2144 fractures: on behalf of the Evidence-Based Orthopaedic Trauma Working Group. J Orthop Trauma. 2005;19:504-507. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 452] [Cited by in RCA: 405] [Article Influence: 20.3] [Reference Citation Analysis (0)] |
| 26. | Katras T, Baltazar U, Rush DS, Davis D, Bell TD, Browder IW, Compton RP, Stanton PE Jr. Subclavian arterial injury associated with blunt trauma. Vasc Surg. 2001;35:43-50. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 39] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 27. | Gill I, Quayle J, Fox M. A low energy paediatric clavicle fracture associated with acute brachial plexus injury and subclavian artery compression. Ann R Coll Surg Engl. 2013;95:e30-e33. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 28. | Sodhi KS, Arora J, Khandelwal N. Post-traumatic occlusion of subclavian artery with clavicle fracture. J Emerg Med. 2007;33:419-420. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 10] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 29. | Franga DL, Hawkins ML, Mondy JS. Management of subclavian and axillary artery injuries: spanning the range of current therapy. Am Surg. 2005;71:303-307. [PubMed] |
| 30. | Kendall KM, Burton JH, Cushing B. Fatal subclavian artery transection from isolated clavicle fracture. J Trauma. 2000;48:316-318. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 37] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 31. | Arnold S, Gilroy D, Laws P, Kempthorne J. Subclavian artery laceration following clavicle fracture, successfully treated with a combined endovascular and open surgical approach. BMJ Case Rep. 2021;14:e241382. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 32. | Bain GI, Eng K, Zumstein MA. Fatal Air Embolus During Internal Fixation of the Clavicle: A Case Report. JBJS Case Connect. 2013;3:e24. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 6] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 33. | Bain GI, Galley IJ, Keogh AR, Durrant AW. Axillary artery pseudoaneurysm after plate osteosynthesis for a clavicle nonunion: A case report and literature review. Int J Shoulder Surg. 2010;4:79-82. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 13] [Cited by in RCA: 15] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 34. | Demir D, Borger van der Burg B, Stollenwerck G, Hoencamp R. Subclavian artery occlusion after a clavicle fracture. BMJ Case Rep. 2019;12:e229314. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 35. | Wright SW. Subclavian vein thrombosis following clavicular fracture. Emerg Med J. 2009;26:840. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 36. | Serrano JA, Rodríguez P, Castro L, Serrano P, Carpintero P. Acute subclavian artery pseudoaneurysm after closed fracture of the clavicle. Acta Orthop Belg. 2003;69:555-557. [PubMed] |
| 37. | Faisham WI, Mohammad P, Juhara H, Munirah NM, Shamsulkamaruljan H, Ziyadi GM. Clavicle fracture and subclavian vessels disruption with massive haemothorax mimic intrathoracic injury. Malays J Med Sci. 2011;18:74-77. [PubMed] |
| 38. | Cooney DR, Kloss B. Case report: Delayed subclavian vein injury secondary to clavicular malunion. J Emerg Med. 2012;43:648-650. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 39. | Belmir H, Chagou A, Tijani Y, Azghari A. Pseudoaneurysm of the subclavian artery following clavicle fracture due to blunt traumatism: a case report. Pan Afr Med J. 2020;36:262. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 40. | Nicholson JA, Stirling PHC, Strelzow J, Robinson CM. Dynamic Compression of the Subclavian Artery Secondary to Clavicle Nonunion: A Report of 2 Cases. JBJS Case Connect. 2019;9:e4. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 41. | van Schaik PM, de Borst GJ, Moll FL, Toorop RJ. Late onset acute occlusion of the subclavian artery after clavicle fracture. Vascular. 2015;23:661-662. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 42. | Malekpour F, Hebeler K, Kirkwood ML. Open Surgical Approach for Type II Endoleak in Subclavian Artery Pseudoaneurysm Presented With Neurological Symptoms After Endovascular Repair. Vasc Endovascular Surg. 2020;54:467-470. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 4] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 43. | Costa MC, Robbs JV. Nonpenetrating subclavian artery trauma. J Vasc Surg. 1988;8:71-75. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 10] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 44. | Kluemper C, Koestner T, Cowart J, Higgins M. Intercostal Entrapment of Clavicle Fracture Causing a Pulseless, Flaccid Upper Extremity. J Hand Surg Am. 2018;43:1143-1143. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 45. | Casbas L, Chauffour X, Cau J, Bossavy JP, Midy D, Baste JC, Barret A. Post-traumatic thoracic outlet syndromes. Ann Vasc Surg. 2005;19:25-28. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 15] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 46. | Mandal AK, Jordaan J, Missouris CG. Fractured clavicle and vascular complications. Emerg Med J. 2004;21:648. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 9] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 47. | Lyons MM, Holzmeister AM, Cappello T. Nonoperative Management of Subclavian Artery Thrombosis in Pediatric Clavicle Fractures: A Case Report. JBJS Case Connect. 2021;11. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 48. | Gullo J, Singletary EM, Larese S. Emergency bedside sonographic diagnosis of subclavian artery pseudoaneurysm with brachial plexopathy after clavicle fracture. Ann Emerg Med. 2013;61:204-206. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 18] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 49. | Mirza WR, Shiraev TP. Endovascular Management of a Left Subclavian Artery Pseudoaneurysm Secondary to Clavicular Fracture. Eur J Vasc Endovasc Surg. 2018;55:624. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 50. | Heffernan EJ, Keaveny TV. Pathological fracture of the clavicle causing subclavian pseudoaneurysm formation. Ir Med J. 2008;101:184-185. [PubMed] |
| 51. | Tachtsi MD, Pitoulias GA, Fycatas P, Kalogirou T, Papadimitriou DK. Subclavian artery aneurysm due to clavicle fracture. Ann Vasc Surg. 2011;25:984. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 11] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 52. | Makida K, Iwase T, Tanaka K, Kobayashi M. Hybrid surgery for a pseudoaneurysm caused by a clavicle fracture. J Orthop Sci. 2019;24:1130-1132. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 53. | Rodriguez-Merchan EC, Gomez-Cardero P. Delayed union of a fracture of the middle third of the clavicle presenting with a late subclavian pseudoaneurysm. Musculoskelet Surg. 2010;94:89-92. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 10] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 54. | Pallett SJC, Singh I, Rady N, Goshai H. Delayed Subclavian Artery Aneurysm Following Fixation of a Clavicular Fracture. Vasc Endovascular Surg. 2018;52:459-462. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 55. | Lawson J, Crockett S, Griffiths D, Riga C, Sabharwal S, Thomas R, Das R. Ruptured subclavian artery pseudoaneurysm following a shoulder massage on a background of clavicle non-union. BMJ Case Rep. 2023;16:e253826. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 56. | Conant SH, Hickerson LE. Arteriovenous Fistula Development After Nonoperative Treatment of a Clavicular Fracture: A Case Report. JBJS Case Connect. 2018;8:e65. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 5] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 57. | Ding M, Hu J, Ni J, Lv H, Song D, Shu C. Iatrogenic subclavian arteriovenous fistula: rare complication of plate osteosynthesis of clavicle fracture. Orthopedics. 2012;35:e287-e289. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 16] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 58. | Kitsis CK, Marino AJ, Krikler SJ, Birch R. Late complications following clavicular fractures and their operative management. Injury. 2003;34:69-74. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 68] [Cited by in RCA: 52] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 59. | Ranke H, Märdian S, Haas NP, Baecker H. [Thrombosis of the subclavian vein after conservative treatment of a clavicular fracture: A rare complication]. Unfallchirurg. 2016;119:255-258. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 60. | Claes T, Debeer P, Bellemans J, Claes T. Deep venous thrombosis of the axillary and subclavian vein after osteosynthesis of a midshaft clavicular fracture: a case report. Am J Sports Med. 2010;38:1255-1258. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 11] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 61. | Kou HW, Liao CH, Huang JF, Hsu CP, Wang SY, Ou Yang CH, Kang SC, Hsu YP, Hsieh CH, Kuo IM. Eighteen years' experience of traumatic subclavian vascular injury in a tertiary referral trauma center. Eur J Trauma Emerg Surg. 2019;45:973-978. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 12] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 62. | Liu JL, Li JY, Jiang P, Jia W, Tian X, Cheng ZY, Zhang YX. Literature review of peripheral vascular trauma: Is the era of intervention coming? Chin J Traumatol. 2020;23:5-9. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 16] [Cited by in RCA: 20] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 63. | Assenza M, Centonze L, Valesini L, Campana G, Corona M, Modini C. Traumatic subclavian arterial rupture: a case report and review of literature. World J Emerg Surg. 2012;7:18. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 27] [Cited by in RCA: 19] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 64. | Rajiah P. Updates in Vascular Computed Tomography. Radiol Clin North Am. 2020;58:671-691. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 15] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 65. | Jalota Sahota R, Lotfollahzadeh S, Soos MP. Subclavian Vein Thrombosis. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing, 2024. [PubMed] |
| 66. | Kearon C, Akl EA, Comerota AJ, Prandoni P, Bounameaux H, Goldhaber SZ, Nelson ME, Wells PS, Gould MK, Dentali F, Crowther M, Kahn SR. Antithrombotic therapy for VTE disease: Antithrombotic Therapy and Prevention of Thrombosis, 9th ed: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines. Chest. 2012;141:e419S-e496S. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2565] [Cited by in RCA: 2569] [Article Influence: 197.6] [Reference Citation Analysis (0)] |
| 67. | McCready RA, Procter CD, Hyde GL. Subclavian-axillary vascular trauma. J Vasc Surg. 1986;3:24-31. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 7] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 68. | Francis D, Kumar M, Singh M, Okafor TL, Reddy MMRK, Inban P, Singh P, Sirekulam V, Akuma O, Akuma CM, Thakkar K. Endovascular management of traumatic pseudoaneurysm of left subclavian artery: A case report. Radiol Case Rep. 2023;18:4066-4070. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 69. | Casselman F, Vanslembroek K, Verougstraete L. An unusual cause of thoracic outlet syndrome. J Trauma. 1997;43:142-143. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 29] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 70. | Shackford SR, Connolly JF. Taming of the screw: a case report and literature review of limb-threatening complications after plate osteosynthesis of a clavicular nonunion. J Trauma. 2003;55:840-843. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 50] [Cited by in RCA: 46] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 71. | Demetriades D, Rabinowitz B, Pezikis A, Franklin J, Palexas G. Subclavian vascular injuries. Br J Surg. 1987;74:1001-1003. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 51] [Cited by in RCA: 53] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 72. | Buchanan DAS, Owen D, Angliss R, McClure DN. Acute subclavian artery occlusion with associated clavicle fracture managed with bypass graft alone. BMJ Case Rep. 2018;2018:bcr2018224719. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |