Published online Jun 9, 2024. doi: 10.5492/wjccm.v13.i2.91794
Revised: April 23, 2024
Accepted: April 26, 2024
Published online: June 9, 2024
Processing time: 149 Days and 21.7 Hours
Quality indicators in healthcare refer to measurable and quantifiable parameters used to assess and monitor the performance, effectiveness, and safety of healthcare services. These indicators provide a systematic way to evaluate the quality of care offered, and thereby to identify areas for improvement and to ensure that patient care meets established standards and best practices. Respiratory therapists play a vital role in areas of clinical administration such as infection control practices and quality improvement initiatives. Quality indicators serve as essential metrics for respiratory therapy departments to assess and enhance the overall quality of care. By systematically tracking and analyzing indicators related to infection control, treatment effectiveness, and adherence to protocols, respiratory care practitioners can identify areas to improve and implement evidence-based changes. This article reviewed how to identify, implement, and monitor quality indicators specific to the respiratory therapy departments to set benchmarks and enhance patient outcomes.
Core Tip: Quality management is indispensable in hospitals and healthcare settings, with a primary emphasis on enhancing patient outcomes. Given the pivotal role they play, training a core team of respiratory therapists in quality management and identifying relevant quality indicators in their specialty can significantly enhance their practices that ultimately benefit patient outcomes on a broader scale.
- Citation: Karthika M, Vanajakshy Kumaran S, Beekanahaali Mokshanatha P. Quality indicators in respiratory therapy. World J Crit Care Med 2024; 13(2): 91794
- URL: https://www.wjgnet.com/2220-3141/full/v13/i2/91794.htm
- DOI: https://dx.doi.org/10.5492/wjccm.v13.i2.91794
Quality management is an essential aspect of all hospital and healthcare settings as it primarily focusses on the overall patient outcome. The incorporation of quality control in healthcare is a part of the transformation of healthcare systems with diverse organizational structures[1]. Various definitions are available on quality in healthcare. The Institute of Medicine defines healthcare quality as “the degree to which healthcare services for individuals and populations increase the likelihood of desired health outcomes and are consistent with current professional knowledge”[2]. Meanwhile, the Agency for Healthcare Research and Quality defines healthcare quality “as doing the right thing for the right patient, at the right time, in the right way to achieve the best possible results”[3].
Accurate, appropriate, and continuous assessment of quality is an important factor for efficient patient care[4,5]. Several reports in the literature have emphasized the above statement from an organizational and departmental perspectives[6-8] as well as from the healthcare professionals’ perspectives including physicians and nurses[9-12]. Nevertheless, there remains a paucity of literature that supports the bidirectional involvement of quality management professionals and allied healthcare professionals with the importance of quality improvement and the need for quality indicators in allied health[13,14].
The respiratory therapy department is an integral part of any healthcare system due to the diverse scope of practice of these professionals. Due to their multidisciplinary areas of practice and years of experience, respiratory therapists at the leadership level assume administrative roles in process improvement areas such as infection control practices and quality management[15]. Hence, it would be ideal if a core team of respiratory therapists were trained in quality management and to establish quality indicators related to their areas of practice that would have a global impact at the patient outcome. This article broadly aimed to propose a framework to develop, implement, and assess the quality indicators related to respiratory care practices.
It is well known that any unit/service/division or department of healthcare must provide proof that it practices evidence-based, high-quality healthcare that is based on the latest standard treatment guidelines and validated clinical care pathways[16]. It is important for the healthcare system that the care delivered is “Safe, Effective, Efficient, Equitable, Timely and Patient Oriented”[17]. The healthcare delivery must incorporate “Patient Reported Outcome Measures (PROMs)” to assess the health status of patients at a particular point in time.
PROM tools can be used during an illness or due course of the treatment, and in some cases pre-PROMs and post-PROMs are used to assess the impact of the therapeutic intervention[18]. The clinical outcomes must be accompanied by acceptable feedback from the recipients of healthcare. The feedback shall include measures that document “Patient Reported Experience Measures” as it provides valuable information for achieving the goals of the healthcare system[19]. Both PROMs and Patient Reported Experience Measures are measured from the perspectives of patients and are utilized in the assessment of quality of healthcare.
Finally, the unit should demonstrate that it follows the principles of value-based healthcare delivery, which is the measurable improvement of the patient’s health status against the cost of attaining that improvement. The ability to provide proof that the unit delivers highly reliable healthcare that is of high quality and leads to desired outcomes is vital to the survival, growth, and scaling up of the unit.
An understanding of the characteristics of quality indicators is necessary for the quality improvement team of the respiratory therapy department to utilize the right indicator for the best outcome. There are various descriptions of “indicators” in healthcare. Quality indicators in healthcare can be described as measurement tools used to monitor, evaluate, and improve the quality of patient care, clinical support services, and organizational functions that aim to improve the patient outcome[20,21]. These indicators are expected to align the requirements of clinical departments including respiratory therapy[15] (Table 1).
| Characteristics | Description |
| Measurement objective | Statistical performance is measured over time |
| Structure | About the structure of the department |
| Process | About the processes in department |
| Outcomes | About the outcomes in department |
| Characteristic measured | |
| Quality | Effectiveness, efficiency, equity, patient orientation are the measures of quality |
| Safety | Timeliness and other aspects of safety are measures of safety |
| Numerical expression used | |
| Sentinel | When occurrence is rare and can be captured as numbers against time |
| Percentage | When occurrence is more common and can be easily understood as percentages |
| Rate | When occurrence needs to be understood and compared to a benchmark |
| Numerator used | |
| Sentinel | Occurrence in numbers |
| Percentage | Occurrence in numbers |
| Rate | Occurrence in numbers |
| Denominator used | |
| Sentinel | Generally, time in days, weeks, months, or years |
| Percentage | Total number studied |
| Rate | Usually, number of patient days |
| Multiplication factor used | |
| Sentinel | None |
| Percentage | 100 |
| Rate | 1000 |
| Formula used | |
| Sentinel | Numerator/Denominator |
| Percentage | Numerator/Denominator × 100 |
| Rate | Numerator /Denominator × 1000 |
| Definition | Precise definition of numerator and denominator must be made and accepted by all stakeholders |
| Start and end times | If the indicator measures start or end times, either in numerator or denominator, then these must be precisely defined |
| Continuous or intermittent monitoring | Some indicators must be monitored continuously without any interruption and others may need intermittent monitoring |
| Sample size | Sample size must be scientifically planned based on the sample volume. The sampling methodology must be scientifically validated |
Considering the paucity of available literature on quality indicators specific to respiratory therapy, we recommend applying the indicators used in acute care and other related settings aligned to respiratory care practices to develop the framework for the respiratory therapy department[22-24].
According to the guidelines set forth by the UNAIDS monitoring and evaluation fundamentals, the essential components of an ideal indicator are as follows[25]: Clearly stated title and definition; clearly stated purpose and rationale; clearly defined methods for measurement, including the description of the numerator, denominator, and calculation, as applicable; clearly stated data collection methodology and tools; frequency of data collection to be clearly defined; clearly defined data disaggregation; availability of guidelines to interpret and use data from the indicator; strengths and weaknesses of the indicator and the challenges in its use; and relevant sources of additional information on the indicator to be cited.
It is of paramount importance that the development and selection of these indicators be based on validity, reliability, feasibility, relevance, pertinence, applicability, and data availability with minimum bias and based on the best evidence available[26-28]. Hence respiratory therapy departments embarking on this process must comb the literature from other related specialties to create suitable indicators. When doing so, it is important to adhere to the principles.
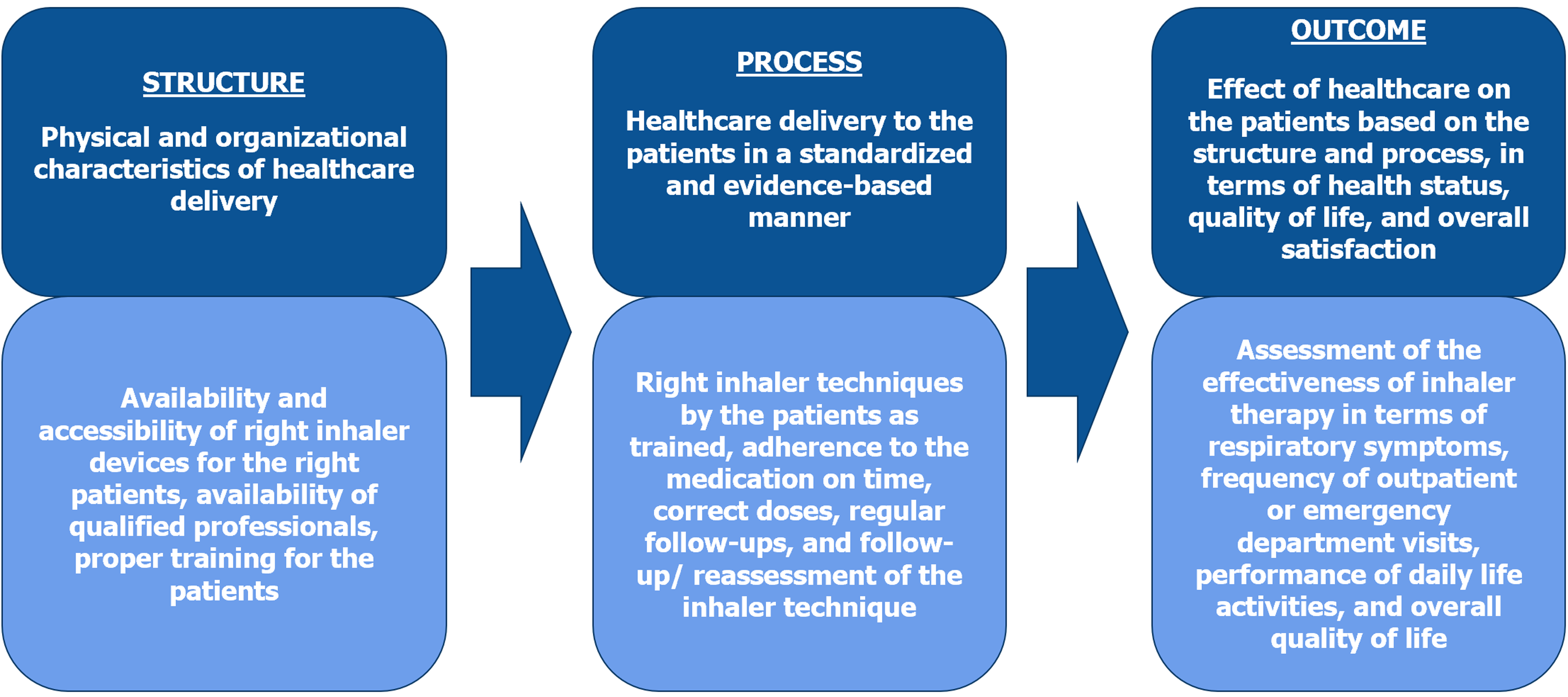
In healthcare settings, the most used framework to distinguish between various types of quality indicators is Donabedian’s triad of structure, process, and outcome indicators[29]. Now, let’s understand how Donabedian’s indicators can be useful in reducing inhaler errors where respiratory therapists play a vital role (Figure 1). The first component of the triad is structure, which refers to the needful resources and infrastructure to offer healthcare, inclusive of physical facilities, resources and equipment, appropriate staffing levels, and training and education programs. It is applied by the availability of user-friendly inhaler devices, availability of qualified respiratory therapists or healthcare professionals, proper training for healthcare professionals and patients on how to use the inhaler correctly, infection control, and the accessibility of the inhaler for patients with limited mobility or other special needs.
The second component of the triad is process, which refers to the delivery of healthcare services, including the procedures, hospital protocols, and practices used for both diagnostic and therapeutic purposes. This component emphasizes the magnitude of delivering healthcare services in a consistent, standardized, and evidence-based manner. It is applied by teaching the proper technique to the patients, adherence to the time, adherence to the medication, correct doses, regular follow-ups, and reassessment of the inhaler technique.
The third and most important component of the triad is outcome, which refers to the impact of the structure and process on the patients in relation to their health status, quality of life, and overall satisfaction with care, emphasizing the assessment of patient outcomes. This part of the triad assesses the effectiveness of inhaler therapy (i.e. reduction in respiratory symptoms, reduction of frequent outpatient or emergency department visits, improvements in performing daily life activities and overall quality of life through the usage of measurement scales such as Asthma Control Tests, Chronic Obstructive Pulmonary Disease Assessment Test, St. George’s Respiratory Questionnaire, Modified Medical Research Council Dyspnea scale, etc.).
The key message from the above example is the link between the three indicators, namely how the structural indicator influences process of care, which in turn will reflect on the patient’s outcome. Table 2 offers a few more examples of independent indicators related to the respiratory therapy department[15].
| Structural indicators | Process indicators | Outcome indicators |
| Average number of respiratory therapists in areas like ICU, emergency department, wards, etc. | Patient assessment | Morbidity and mortality related to care |
| Average number of routine and urgent respiratory visits in the wards | Application of specific oxygen therapy device | Ventilator-associated events |
| Knowledge regarding departmental clinical practice guidelines | Application of disease-specific ventilation, based on the patients | Ulcers related to artificial airways, non-invasive ventilation masks, etc. |
| Knowledge regarding airway management and mechanical ventilation | Performing/assisting intubation | Success and failure rates related to care: Successful weaning and extubation, accidental extubation, reintubation rates, etc. |
| Knowledge on the rights and responsibilities of patients and staff | Performing/assisting arterial line insertion | Equipment utilization indices |
| Interpretation of blood gas reports | Equipment down time | |
| Documented patient feedback |
The current article utilized these essential characteristics and components to draft a framework to identify, implement, monitor, review, and analyze these quality indicators to provide a basis for continuous quality improvement in a respiratory therapy unit.
Identifying quality indicators in respiratory therapy is a dynamic multifaceted process that considers a combination of clinical guidelines, literature review, and adherence to evidence-based practices. The first step at an institutional level in this process is to develop a Respiratory Therapy Quality Committee. Various steps are involved in developing a new committee, from team engagement, resource acquisition, and program organization.
As mentioned in one of the steps in the framework developed by Professor John Kotter[30], the committee that includes champions and departmental and support staff, shall have a chairman, a secretary, and a leadership team from the respiratory therapy department, a physician representative from pulmonology or critical care, and representatives from the quality department, infection control, information technology, and medical records department. The committee shall be empowered to invite non-members who might be expected to contribute to a particular aspect of the agenda, as and when needed.
The most important function of the committee is to develop, document, and implement a quality improvement program for the unit. It is necessary for the committee to examine the existing outcomes to identify high-priority goals that can lead to the development of specific, measurable, achievable, realistic, and time bound objectives[31]. The committee also chooses the best practices that apply to the identified goals and objectives of the department, develops plans to implement best practices, creates mandates for change, implements the quality improvement plan with iterative modifications, identifies the resistance to changes and addresses them, monitors and analyzes outcomes, reports results to all stakeholders, and maintains the gains.
To do this, the committee must identify: (1) Areas where one-time quality improvement projects would suffice; and (2) Areas where a continuous quality improvement program would be needed. A one-time quality improvement project in healthcare involves a focused and time-bound initiative aimed at addressing a specific issue or an area of improvement within a department or clinical setting. These projects are designed to bring about measurable enhancements in the quality of care, patient outcomes, or operational efficiency. An example is to orient the new staff on bedside and departmental documentation. Such an initiative will aim to offer proper orientation and training to the new staff on electronic health records (EHRs) and timely follow-up, thereby initiating an accurate and thorough recording of patient assessments, interventions, and outcomes[32].
On the other hand, a continuous quality improvement (CQI) program is a systematic and ongoing process aimed at improving the quality of services, patient outcomes, and overall performance within the hospital or healthcare setting. CQI involves the identification of areas for improvement, the implementation of changes, and the continuous monitoring and evaluation of these changes to ensure sustained excellence. An example of CQI is identification of Key Performance Indicators relevant to respiratory therapy practices, such as patient satisfaction, adherence to clinical protocols, and outcomes like reduced hospital and intensive care unit (ICU) readmissions[17]. Table 3 summarizes some of the specific quality and safety indicators proposed for respiratory therapy based on closely aligned professions like critical care medicine and nursing and knowledge from the relevant literature[22,33-37].
| No. | Name of indicator | Type | Dimension measured | Frequency of data collection |
| 1 | Availability of respiratory therapists in: (1) Acute care settings (ICUs and emergency departments); (2) Wards and outpatient departments; and (3) Pulmonary diagnostics department | Quality | Structure | Monthly |
| 2 | Inventory check/availability of calibrated equipment in: (1) Acute care settings (ICUs and emergency departments); and (2) Respiratory therapy departments | Quality | Structure | Monthly |
| 3 | Percentage of ventilator circuits changed as per guidelines | Quality | Process | Monthly |
| 4 | Percentage of heat and moisture exchange filters that were changed as per guidelines | Quality | Process | Monthly |
| 5 | Percentage of patients in adherence to VAP prevention bundle | Safety | Process | Monthly |
| 6 | Percentage of patients on semirecumbent posture during MV | Safety | Process | Monthly |
| 7 | Average number of routine and urgent respiratory therapy visits | Quality | Process | Monthly |
| 8 | Knowledge regarding clinical practice guidelines | Safety | Process | Monthly |
| 9 | Infection control practices | Safety | Process | Monthly |
| 10 | Patient and staff rights and responsibilities | Quality | Process | Monthly |
| 11 | Care plan indicators: (1) Assessment by respiratory therapists; (2) Reassessment by respiratory therapists; and (3) Respiratory care plan | Quality | Process | Monthly |
| 12 | Carrying out procedures related to: (1) Oxygen therapy; (2) Nebulization; (3) Humidification; (4) Bronchial hygiene; (5) Artificial airway; (6) Vascular access; (7) Noninvasive or invasive ventilation, and (8) Assistance in invasive procedures such as an arterial line, central line, and chest tube insertion, bronchoscopy, etc. | Safety | Process | Monthly |
| 13 | Percentage of patients successfully weaned off from invasive ventilation | Quality | Outcome | Monthly |
| 14 | Percentage of patients successfully weaned off from noninvasive ventilation | Quality | Outcome | Monthly |
| 15 | Successful spontaneous breathing trials leading to successful extubation | Quality | Outcome | Monthly |
| 16 | Percentage of patients intubated on first attempt | Safety | Outcome | Monthly |
| 17 | Percentage of patients who could not be intubated after multiple attempts | Safety | Outcome | Monthly |
| 18 | Percentage of patients who developed cardiac arrest during intubation | Safety | Outcome | Monthly |
| 19 | Percentage of accidental extubation | Safety | Outcome | Monthly |
| 20 | Rate of ventilator-associated events | Safety | Outcome | Monthly |
| 21 | Morbidity and mortality related to care infection indices (ventilator-associated infections) | Safety | Outcome | Monthly |
| 22 | Success and failure rates related to care (e.g., successful extubation, accidental extubation, reintubation rates) | Safety | Outcome | Monthly |
| 23 | Equipment and time utilization indices | Safety | Outcome | Monthly |
| 24 | Equipment down time | Safety | Outcome | Monthly |
| 25 | Patient safety incidents | Safety | Outcome | Monthly |
The implementation of identified indicators requires a well thought out strategy that encompasses the following key components to ensure success: (1) Establish standardized protocols and procedures. The team should construct standardized protocols and procedures for implementing and measuring the selected quality indicators. Clearly outline the steps involved and ensure that all the members of a respiratory therapy quality improvement team are trained on these standardized processes[38]; (2) Establish data collection mechanisms. Implementation of reliable data collection mechanisms, utilizing EHRs and other technology-driven solutions play an important role in the process. Ensure the accuracy and completeness of collected data to facilitate meaningful analysis of the selected quality indicators[39]; (3) Implement continuous monitoring systems. Establishment of continuous monitoring systems to track the performance of quality indicators over time is a must in the process. The use of statistical process control charts and run charts will aid in the effective analysis. Regular evaluation of trends and any deviation from established benchmarks need to be promptly addressed[40]; and (4) Ongoing education and training. The quality improvement team must develop a culture of continuous learning by providing ongoing education and training to respiratory therapy staff. It is important to keep them informed about changes in protocols, new evidence-based practices, and the rationale behind the selected quality indicators[41].
The following is an example of assessing the ventilation-associated event (VAE) rate as a quality indicator related to respiratory therapy practices.
The VAE rate measures the occurrence of complications associated with mechanical ventilation, including ventilator-associated conditions (VACs), infection-related VACs, and possible ventilator-associated pneumonia.
The following implementation process should be undertaken: (1) Data collection. Respiratory therapists collect data on ventilator parameters, patient symptoms, and laboratory results; (2) Monitoring. Regularly monitor ventilator settings and patient response to identify any deviation from the norm; (3) Documentation. Document any signs of respiratory distress, changes in chest X-rays, and laboratory results indicating possible infections; and (4) Analysis. Analyze collected data to calculate the VAE rate, distinguishing between a VAC, infection-related VAC, and possible ventilator-associated pneumonia.
The following outcomes can be assessed: (1) A lower VAE rate indicates effective ventilator management, reduced risk of complications, and improved patient safety; and (2) Implementation of evidence-based practices, such as daily spontaneous breathing trials and oral care protocols, to reduce the risk of ventilator-associated complications.
The monitoring of implemented indicators is crucial for identifying the areas of improvement, ensuring adherence to evidence-based practices, and ultimately improving patient outcomes.
EHRs are a foundation in monitoring quality indicators. The adoption of EHRs allows for seamless data collection, storage, and analysis, providing respiratory therapy departments with the ability to promptly capture critical information about patient care. The utility of real-time data in healthcare is vital in improving the quality of patient care and outcomes[42].
Monitoring adherence to clinical pathways (documentation of clinical rounds and therapy, timely dispatch of devices, missed alerts, etc.) ensures that respiratory therapists follow established care plans and protocols. This approach helps to maintain consistency in care delivery, streamline the processes, and support evidence-based practices[43].
In the healthcare system, incident reporting is crucial for capturing events related to ventilator management, oxygen administration, or any deviation from established protocols. Root cause analysis helps uncover the factors contributing to incidents and guides the development of preventive strategies[44]. Incident reporting fosters a culture of learning from mistakes rather than blaming individuals. Hence incident reporting and root cause analysis are integral to quality monitoring in the respiratory therapy department.
Statistical process control charts offer a visual representation of trends over time, aiding in the identification of variations and enabling timely interventions. They are a versatile tool for monitoring quality indicators with substantial benefits[45]. This method shall be utilized by respiratory therapy departments to track and analyze key performance indicators such as VAE, ensuring that care delivery remains consistent and aligned with established benchmarks.
Audits and quality assurance checks contribute to the ongoing evaluation of respiratory therapy practices. By implementing regular assessments, departments can proactively identify areas for improvement and reinforce adherence to established protocols. The American Association for Respiratory Care provides comprehensive clinical practice guidelines that serve as a valuable resource for ensuring quality assurance in respiratory therapy[46].
Patient/family feedback through surveys or reports from focus groups provide valuable insights into the patient experience and satisfaction. It is emphasized that patient satisfaction and healthcare outcomes are directly related, making patient feedback an integral part of the monitoring process[47]. This approach ensures that respiratory therapy remains patient-centered, aligning with the broader goal of enhancing overall patient well-being.
Benchmarking of practices to those set by the American Thoracic Society and the National Quality Forum allows respiratory therapy departments to assess their performance against industry benchmarks. This comparative framework assists in identifying areas of excellence and areas that may require improvement. The American Thoracic Society provides documents that outline comparative effectiveness research in lung diseases, serving as a guide for bench
In conclusion, monitoring quality indicators in respiratory therapy is a multifaceted approach, and these strategies, grounded in evidence-based practices, contribute to the ongoing improvement of respiratory therapy services, ensuring patient-centered care and fostering positive patient outcomes.
In the evolving landscape of healthcare, it is understood that quality indicators guide the respiratory therapy profession toward excellence, safety, and patient-centered care. Quality indicators, ranging from VAE rates to oxygen saturation maintenance, serve as crucial benchmarks for evaluating the effectiveness and safety of respiratory interventions. These indicators are not isolated metrics; rather, they intertwine evidence-based practices, patient outcomes, and continuous improvement efforts.
Moreover, quality indicators act as sentinels for patient safety. For instance, as in VAE, diligent monitoring and analysis become keystones in the prevention of complications. The reduction of adverse events not only safeguards patient well-being but also testifies to the commitment of respiratory therapists to the highest standards of care. As we conclude this exploration, it is essential to recognize the collaborative nature of respiratory care professionals in the overall process of quality improvement, with the engagement of diverse stakeholders, including physicians, nurses, other healthcare professionals, administrators, regulatory bodies, and patients. Quality indicators, in this sense, become a common language spoken by all involved in the delivery of respiratory care, fostering a culture where everyone contributes to the symphony of improvement.
Provenance and peer review: Invited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Critical care medicine
Country of origin: India
Peer-review report’s classification
Scientific Quality: Grade C
Novelty: Grade B
Creativity or Innovation: Grade B
Scientific Significance: Grade B
P-Reviewer: Luo W, China S-Editor: Liu JH L-Editor: A P-Editor: Cai YX
| 1. | Mito M, Kusano M, Kawaura Y. Hepatocyte transplantation in man. Transplant Proc. 1992;24:3052-3053. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 607] [Cited by in RCA: 656] [Article Influence: 31.2] [Reference Citation Analysis (0)] |
| 2. | Medicare: A Strategy for Quality Assurance: Volume 1. Washington (DC): National Academies Press (US); 1990– . [PubMed] |
| 3. | Agency for Healthcare Research and Quality. Understanding quality management: child health care quality toolbox. 2012. Accessed October 18, 2023. Available from: http://www.ahrq.gov/profressionals/quality-safety/quality-resources/tools/chtoolbx/understand/index.html. |
| 4. | Berwick DM. Toward an applied technology for quality measurement in health care. Med Decis Making. 1988;8:253-258. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 20] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 5. | Williamson P, Altman D, Blazeby J, Clarke M, Gargon E. Driving up the quality and relevance of research through the use of agreed core outcomes. J Health Serv Res Policy. 2012;17:1-2. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 187] [Cited by in RCA: 232] [Article Influence: 17.8] [Reference Citation Analysis (0)] |
| 6. | Young RA, Roberts RG, Holden RJ. The Challenges of Measuring, Improving, and Reporting Quality in Primary Care. Ann Fam Med. 2017;15:175-182. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53] [Cited by in RCA: 60] [Article Influence: 7.5] [Reference Citation Analysis (1)] |
| 7. | Kazandjian VA, Wicker KG, Matthes N, Ogunbo S. Safety is part of quality: a proposal for a continuum in performance measurement. J Eval Clin Pract. 2008;14:354-359. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 9] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 8. | Schull MJ, Guttmann A, Leaver CA, Vermeulen M, Hatcher CM, Rowe BH, Zwarenstein M, Anderson GM. Prioritizing performance measurement for emergency department care: consensus on evidence-based quality of care indicators. CJEM. 2011;13:300-309, E28. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 59] [Cited by in RCA: 76] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 9. | Scholle SH, Roski J, Adams JL, Dunn DL, Kerr EA, Dugan DP, Jensen RE. Benchmarking physician performance: reliability of individual and composite measures. Am J Manag Care. 2008;14:833-838. [PubMed] |
| 10. | Scholle SH, Roski J, Dunn DL, Adams JL, Dugan DP, Pawlson LG, Kerr EA. Availability of data for measuring physician quality performance. Am J Manag Care. 2009;15:67-72. [PubMed] |
| 11. | Izumi S. Quality improvement in nursing: administrative mandate or professional responsibility? Nurs Forum. 2012;47:260-267. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 15] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 12. | Robinson J, Gelling L. Nurses+QI=better hospital performance? A critical review of the literature. Nurs Manag (Harrow). 2019;26:22-28. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 5] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 13. | Grimmer K, Lizarondo L, Kumar S, Bell E, Buist M, Weinstein P. An evidence-based framework to measure quality of allied health care. Health Res Policy Syst. 2014;12:10. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 17] [Cited by in RCA: 14] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 14. | Lizarondo L, Grimmer K, Kumar S. Assisting allied health in performance evaluation: a systematic review. BMC Health Serv Res. 2014;14:572. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 19] [Cited by in RCA: 16] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 15. | Karthika M, Sureshkumar VK, Bennett A, Noorshe AH, Mallat J, Praveen BM. Quality Management in Respiratory Care. Respir Care. 2021;66:1485-1494. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Reference Citation Analysis (0)] |
| 16. | NABH 5th edition. Accessed October 20, 2023. Available from: https://www.nabh.co/images/Standards/1.%205th%20Edition%20Hospital%20Std%20April%202020.pdf. |
| 17. | Crossing the Quality Chasm: A New Health System for the 21st Century. Washington (DC): National Academies Press (US); 2001 . [PubMed] |
| 18. | Ahern S, Ruseckaite R, Ackerman IN. Collecting patient-reported outcome measures. Intern Med J. 2017;47:1454-1457. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 37] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 19. | Weldring T, Smith SM. Patient-Reported Outcomes (PROs) and Patient-Reported Outcome Measures (PROMs). Health Serv Insights. 2013;6:61-68. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 343] [Cited by in RCA: 599] [Article Influence: 49.9] [Reference Citation Analysis (1)] |
| 20. | Panteli D, Quentin W, Busse R. Understanding healthcare quality strategies: a five-lens framework. In: Busse R, Klazinga N, Panteli D, et al editors. Improving healthcare quality in Europe: Characteristics, effectiveness, and implementation of different strategies [Internet]. Copenhagen (Denmark): European Observatory on Health Systems and Policies; 2019. (Health Policy Series, No. 53.) 2. Accessed October 26, 2023. Available from: https:// www.ncbi.nlm.nih.gov/books/NBK549261/. |
| 21. | Characteristics of clinical indicators. QRB Qual Rev Bull. 1989;15:330-339. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 42] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 22. | Ray B, Samaddar DP, Todi SK, Ramakrishnan N, John G, Ramasubban S. Quality indicators for ICU: ISCCM guidelines for ICUs in India. Indian J Crit Care Med. 2009;13:173-206. [PubMed] |
| 23. | Flaatten H. The present use of quality indicators in the intensive care unit. Acta Anaesthesiol Scand. 2012;56:1078-1083. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 52] [Cited by in RCA: 57] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 24. | Braun JP, Kumpf O, Deja M, Brinkmann A, Marx G, Bloos F, Kaltwasser A, Dubb R, Muhl E, Greim C, Bause H, Weiler N, Chop I, Waydhas C, Spies C. The German quality indicators in intensive care medicine 2013--second edition. Ger Med Sci. 2013;11:Doc09. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 19] [Reference Citation Analysis (0)] |
| 25. | An introduction to indicators. UNAIDS monitoring and evaluation fundamentals. Geneva: United Nations Joint Programme on HIV/AIDS; 2010. Accessed October 29, 2023. Available from: https://www.unaids.org/sites/default/files/sub_landing/files/8_2-Intro-to-IndicatorsFMEF.pdf. |
| 26. | Wollersheim H, Hermens R, Hulscher M, Braspenning J, Ouwens M, Schouten J, Marres H, Dijkstra R, Grol R. Clinical indicators: development and applications. Neth J Med. 2007;65:15-22. [PubMed] |
| 27. | Guide to Inpatient Quality Indicators: Quality of Care in Hospitals–Volume, Mortality, and Utilization. AHRQ Quality Indicators; 2007. Accessed November 02, 2023. Available from: https://www.ahrq.gov/downloads/pub/inpatqi/iqi_guide.pdf. |
| 28. | Curtis JR, Cook DJ, Wall RJ, Angus DC, Bion J, Kacmarek R, Kane-Gill SL, Kirchhoff KT, Levy M, Mitchell PH, Moreno R, Pronovost P, Puntillo K. Intensive care unit quality improvement: a "how-to" guide for the interdisciplinary team. Crit Care Med. 2006;34:211-218. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 252] [Cited by in RCA: 230] [Article Influence: 12.1] [Reference Citation Analysis (0)] |
| 29. | Donabedian A. The Definition of Quality and Approaches to Its Assessment. Vol 1. Explorations in Quality Assessment and Monitoring. Ann Arbor, Michigan, USA: Health Administration Press; 1980. |
| 30. | Kotter JP. Leading change: why transformation efforts fail. IEEE Eng Manag Rev. 2009;37:42-48. [RCA] [DOI] [Full Text] [Cited by in Crossref: 87] [Cited by in RCA: 88] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 31. | Hooper JE, Richardson H, Maters AW, Carroll KC, Pronovost PJ. The Association of Departmental Quality Infrastructure and Positive Change: A Pathology Department Illustration. Acad Pathol. 2018;5:2374289517744753. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 32. | O'Connor M. Pain management: improving documentation of assessment and intensity. J Healthc Qual. 2003;25:17-21; quiz 22. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 7] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 33. | Al-dorzi HM, Arabi YM. Quality Indicators in Adult Critical Care Medicine. JQSH. 2023;. [RCA] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 34. | Evangelou E, Middleton N, Kyprianou T, Kouta C, Merkouris A, Raftopoulos V, Palazis L, Lambrinou E. Nursing quality indicators for adult intensive care: A consensus study. Nurs Crit Care. 2021;26:234-243. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 8] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 35. | Carini E, Gabutti I, Frisicale EM, Di Pilla A, Pezzullo AM, de Waure C, Cicchetti A, Boccia S, Specchia ML. Assessing hospital performance indicators. What dimensions? Evidence from an umbrella review. BMC Health Serv Res. 2020;20:1038. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 39] [Cited by in RCA: 25] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 36. | Schang L, Blotenberg I, Boywitt D. What makes a good quality indicator set? A systematic review of criteria. Int J Qual Health Care. 2021;33. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 26] [Cited by in RCA: 41] [Article Influence: 10.3] [Reference Citation Analysis (0)] |
| 37. | Zhou H, Bai G, Gao J, Zhou Y, Ma E, Hu L, Hu G, Zhao P, Jiang F, Luo L, Liu Y. The development of indicator measure for monitoring the quality of patient-centered care in China's tertiary hospitals. PLoS One. 2018;13:e0205489. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 11] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 38. | Kaplan HC, Brady PW, Dritz MC, Hooper DK, Linam WM, Froehle CM, Margolis P. The influence of context on quality improvement success in health care: a systematic review of the literature. Milbank Q. 2010;88:500-559. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 515] [Cited by in RCA: 479] [Article Influence: 31.9] [Reference Citation Analysis (0)] |
| 39. | Sydnor ER, Perl TM. Hospital epidemiology and infection control in acute-care settings. Clin Microbiol Rev. 2011;24:141-173. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 381] [Cited by in RCA: 358] [Article Influence: 25.6] [Reference Citation Analysis (0)] |
| 40. | Benneyan JC, Lloyd RC, Plsek PE. Statistical process control as a tool for research and healthcare improvement. Qual Saf Health Care. 2003;12:458-464. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 643] [Cited by in RCA: 740] [Article Influence: 35.2] [Reference Citation Analysis (0)] |
| 41. | Grol R, Grimshaw J. From best evidence to best practice: effective implementation of change in patients' care. Lancet. 2003;362:1225-1230. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2963] [Cited by in RCA: 2983] [Article Influence: 135.6] [Reference Citation Analysis (0)] |
| 42. | Blumenthal D, Tavenner M. The "meaningful use" regulation for electronic health records. N Engl J Med. 2010;363:501-504. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1345] [Cited by in RCA: 1210] [Article Influence: 80.7] [Reference Citation Analysis (0)] |
| 43. | Ogrinc G, Mooney SE, Estrada C, Foster T, Goldmann D, Hall LW, Huizinga MM, Liu SK, Mills P, Neily J, Nelson W, Pronovost PJ, Provost L, Rubenstein LV, Speroff T, Splaine M, Thomson R, Tomolo AM, Watts B. The SQUIRE (Standards for QUality Improvement Reporting Excellence) guidelines for quality improvement reporting: explanation and elaboration. Qual Saf Health Care. 2008;17 Suppl 1:i13-i32. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 255] [Cited by in RCA: 301] [Article Influence: 17.7] [Reference Citation Analysis (0)] |
| 44. | Martin-Delgado J, Martínez-García A, Aranaz JM, Valencia-Martín JL, Mira JJ. How Much of Root Cause Analysis Translates into Improved Patient Safety: A Systematic Review. Med Princ Pract. 2020;29:524-531. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 38] [Article Influence: 7.6] [Reference Citation Analysis (0)] |
| 45. | Thor J, Lundberg J, Ask J, Olsson J, Carli C, Härenstam KP, Brommels M. Application of statistical process control in healthcare improvement: systematic review. Qual Saf Health Care. 2007;16:387-399. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 255] [Cited by in RCA: 245] [Article Influence: 13.6] [Reference Citation Analysis (0)] |
| 46. | American Association for Respiratory Care (AARC). (2015). Clinical Practice Guidelines. Accessed November 12, 2023. Available from: https://www.aarc.org/resources/clinical-resources. |
| 47. | Boulding W, Glickman SW, Manary MP, Schulman KA, Staelin R. Relationship between patient satisfaction with inpatient care and hospital readmission within 30 days. Am J Manag Care. 2011;17:41-48. [PubMed] |