Published online Jun 9, 2024. doi: 10.5492/wjccm.v13.i2.91558
Peer-review started: December 30, 2023
First decision: January 16, 2024
Revised: January 28, 2024
Accepted: March 4, 2024
Article in press: March 4, 2024
Published online: June 9, 2024
Processing time: 155 Days and 20.6 Hours
Vascular injuries of the upper extremities are considered relatively rare injuries affecting mostly the young population. They often are complex injuries accom
To analyze data about the mechanism of injury, the management algorithm and functional outcomes of vascular injuries of the upper extremity.
One hundred and fifteen patients (96 males and 19 females) with arterial injuries of the upper extremity treated in a tertiary trauma center from January 2003 to December 2022 was conducted. Mean patients’ age was 33.7 years and the mean follow up time was 7.4 years. Patients with Mangled Extremity Severity Score ≥ 7 and Injury Severity Score ≥ 20, previous upper limb surgery or major trauma and any neuromuscular or psychiatric disease were excluded, from the study.
A penetrating trauma was the most common cause of injury. The radial artery was the artery injured in most of the cases (37.4%) followed by the ulnar (29.5%), the brachial (12.1%) and the axillary (6%). A simultaneous injury of both of the forearm’s arteries was in 15.6% of the cases. In 93% of the cases there were other concomitant musculoskeletal injuries of the extremity. Tendon lacerations were the most common, followed by nerve injuries. The postoperative functional scores (full Disabilities of the Arm, Shoulder, and Hand and VAS) had very satisfactory values.
Although vascular injuries of the upper extremity are rare, they may occur in the context of major combined musculoskeletal trauma. Although a multidisciplinary approach is essential to optimize outcome, the ability of trained hand surgeons to repair all injuries in combined vascular and musculoskeletal upper extremity trauma, excluding isolated vascular injuries, ensures shorter operative times and better functional outcomes.
Core Tip: Vascular injuries of the upper extremities are considered relatively rare injuries affecting mostly the young population. They often are complex injuries accompanied by other musculoskeletal trauma or trauma from other anatomic locations. Although a multidisciplinary approach is essential to optimize outcome, the ability of trained orthopaedic hand surgeons to repair all injuries in combined vascular and musculoskeletal upper extremity trauma, excluding isolated vascular injuries, ensures shorter operative times and better functional outcomes.
- Citation: Stefanou N, Mylonas T, Angelis FA, Arnaoutoglou C, Varitimidis SE, Dailiana ZH. Upper extremity vascular injuries: Etiology, management and outcome. World J Crit Care Med 2024; 13(2): 91558
- URL: https://www.wjgnet.com/2220-3141/full/v13/i2/91558.htm
- DOI: https://dx.doi.org/10.5492/wjccm.v13.i2.91558
Vascular injuries of the upper extremity in civilians are a rare entity, and comprise 30% to 40% of all arterial trauma in the upper extremities which account up to 1% of all traumatic injuries, having devastating consequences for limb function and the life of the patient[1,2]. Such injuries are either isolated or are present in the setting of complex musculoskeletal trauma. They can occur as well with additional trauma to head, chest, abdomen and other extremities affecting the therapeutic decision, treatment, length of stay and costs. Sometimes they lead to permanent disabilities for the patient or even amputation[3]. It is common for these injuries to occur in younger males, under the age of 35 years, resulting in serious social and economic implications because of the morbidity caused by the poor functional outcomes and amputations[4]. High level of suspicion, early recognition and prompt treatment can have excellent results for the patient and for the limb and function[5]. We therefore present our experience from a general university hospital, a level I trauma hospital, contributing to the current knowledge for upper-extremity vascular injuries by retrospectively analyzing data about the mechanism of injury, the management algorithm and functional outcomes. Our goal is to contribute further to the understanding of the mechanisms that cause these injuries and to the improvement of management protocols and thus the reduction of their dramatic consequences in some cases.
After the approval of the institutional review board a retrospective study was conducted from January 2003 until December 2022 for patients admitted at our department having suffered an isolated arterial injury or in the setting of complex orthopaedic trauma. Sex, age, location and type of vascular injury, concomitant injuries, mechanism of trauma, treatment, additional procedures, length of stay, postoperative course, functional assessment, and long-term follow-up were recorded. The patients were usually first evaluated at the emergency department or referred from the five hospitals of our health district, with a population of approximately one million people. The diagnosis was based on our department’s diagnostic algorithm for the management of vascular injuries in musculoskeletal trauma (Figure 1 in the study by Stefanou et al[6] Combined musculoskeletal and vascular injuries of the extremities) starting with clinical examination at first and the use of a doppler device. In the presence of hard signs for vascular injury no further imaging was needed, apart from few cases in which was necessary for medicolegal reasons, and the patient was taken to the operation room as soon as possible[7]. At the presence of soft signs consultation from vascular surgeons was asked and ultrasonography was performed and in most cases a computed tomography (CT) angiography confirmed the diagnosis[8,9].
In some cases, the diagnosis was made intraoperatively or the arterial damage was a result of iatrogenic trauma. Arterial repair was done by orthopaedic hand surgeons addressing all other concomitant injuries in the setting of complex trauma and vascular surgeons treated the arterial injuries at the level of the elbow and proximal. Major associated venous injuries were repaired whenever possible, in order to prevent postoperative venous hypertension or development of a compartment syndrome.
All patients were treated within 16 h from the injury and underwent primary repair of all injured structures. Broad-spectrum antibiotics were administered to all patients on arrival at the hospital and continued for 5 d postoperatively, while receiving aspirin 100 mg/d for 3 wk postoperatively. Co-administration of low molecular weight heparin was held for the first 3 d postoperatively in patients older than 14 years.
Fracture fixation was performed first when there was no evidence of cold or prolonged warm ischemia, especially in concomitant presence of unstable, comminuted fracture pattern. Injured structures identified from superficial to deep layer, based on the knowledge of the cross-sectional anatomy, and reconstruction started from the deeper layer. Nerves are repaired after bone and vascular structures followed by muscle and tendons, which are the last to be reapproximated. Fasciotomies performed concomitantly in all cases with limb revascularization. Second look for surgical site infection, soft-tissue viability and confirmation of vascular perfusion was routinely performed 24-48 h after initial surgery. The fasciotomy incision closure or split-thickness skin graft placement performed after 7-10 d in case of optimal postoperative findings.
Postsurgical functional outcome evaluation was based on the parameters calculating the Disabilities of the Arm, Shoulder, and Hand (DASH) score. The questionnaire was filled out by the patient directly or indirectly over the telephone at his/her most recent follow-up. The result of the score is a number from 0 to 100, where 0 reflects minimum and 100 maximum disability of the patient to accomplish everyday activities. Also, the VAS score was used, evaluating the degree of pain that those patients still experience. Patients with Mangled Extremity Severity Score (MESS) ≥ 7 and Injury Severity Score (ISS) ≥ 20, previous upper limb surgery or major trauma and any neuromuscular or psychiatric disease were excluded, from the study. All patients had baseline follow-up visits at 1, 3, and 6 wk, 3, 6, 12 months, unless there were specific complications necessitating closer observation.
The tests used to obtain p-values were the Pearson χ2 and Fisher’s Exact. Logistic regression analysis was used to study the significant correlations. All P values were based on two-tailed tests and the level of statistical significance was set at P < 0.05 and the SPSS v21.0 was used for the analysis of the data.
During the twenty years period of the study, one hundred and fifteen patients were treated at our hospital suffering from 134 arterial injuries. The mean age was 33.7 years, (range: 2-71 years) and thirteen patients (11.3%) were under the age of 16 years. The majority of the patients were men (96/115, 83.5%). Eighteen patients (15.6%) had more than one upper-extremity arterial injury. The most common mechanism of injury was penetrating trauma (83/115, 72.1%), followed by high energy trauma in 17/115 patients (15.7%), injuries caused by industrial or heavy machinery resulting in amputations, (14/115, 12%), and one iatrogenic arterial lesion while fixing a fracture which was referred from another hospital (Table 1).
| Patients, n = 115 | Penetrating, n = 83 | High energy, n = 17 | Heavy machinery, n = 14 | Iatrogenic, n = 1 |
| Mean age: 33.7 (yr) | 35 | 33 | 32 | 40 |
| Male: 96 (83.5%) | 71 | 13 | 11 | 1 |
| Female: 19 (16.5%) | 12 | 4 | 3 | - |
| Mean length of hospitalization (days): 6 | 3 | 9 | 8 | 3 |
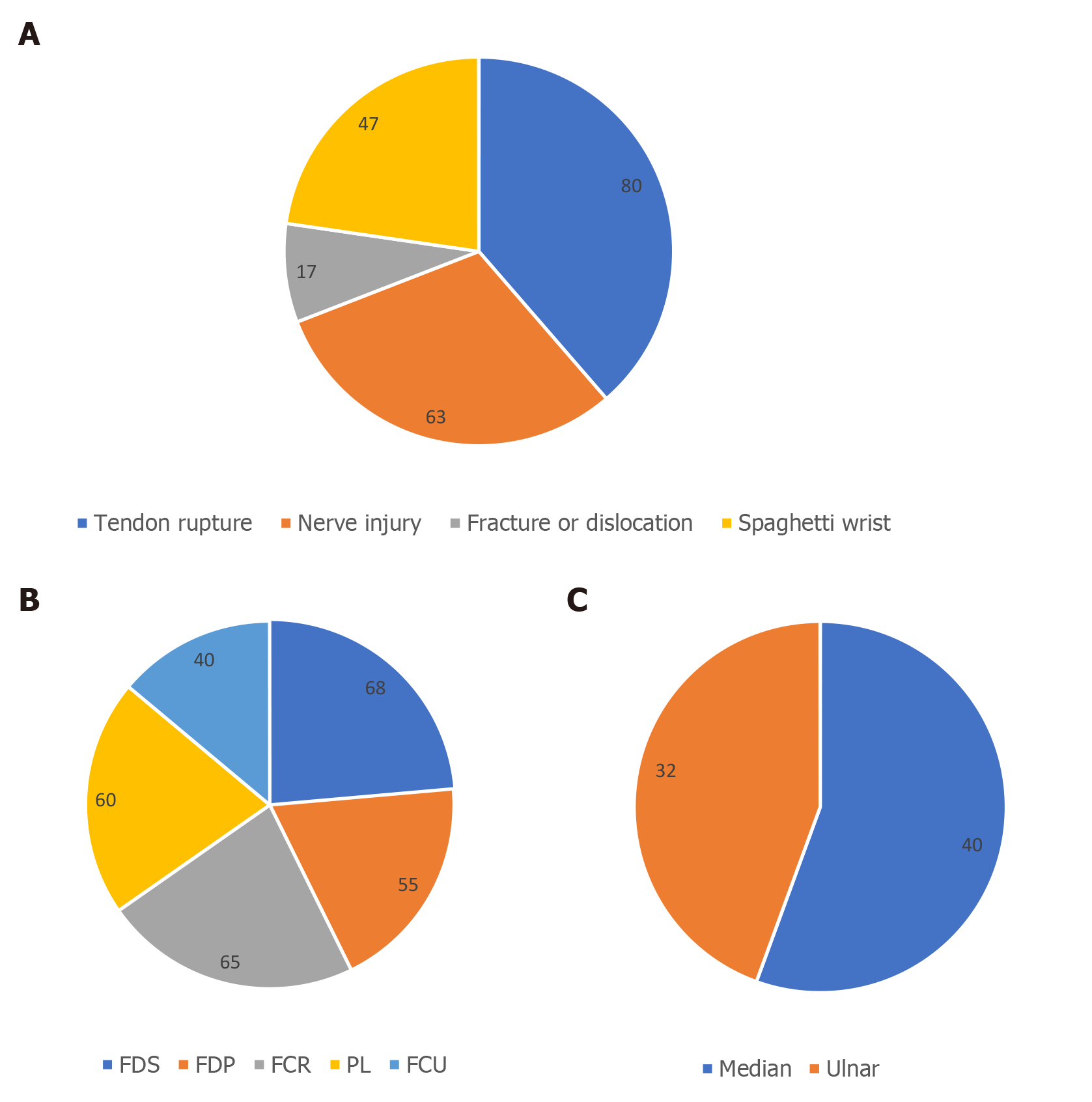
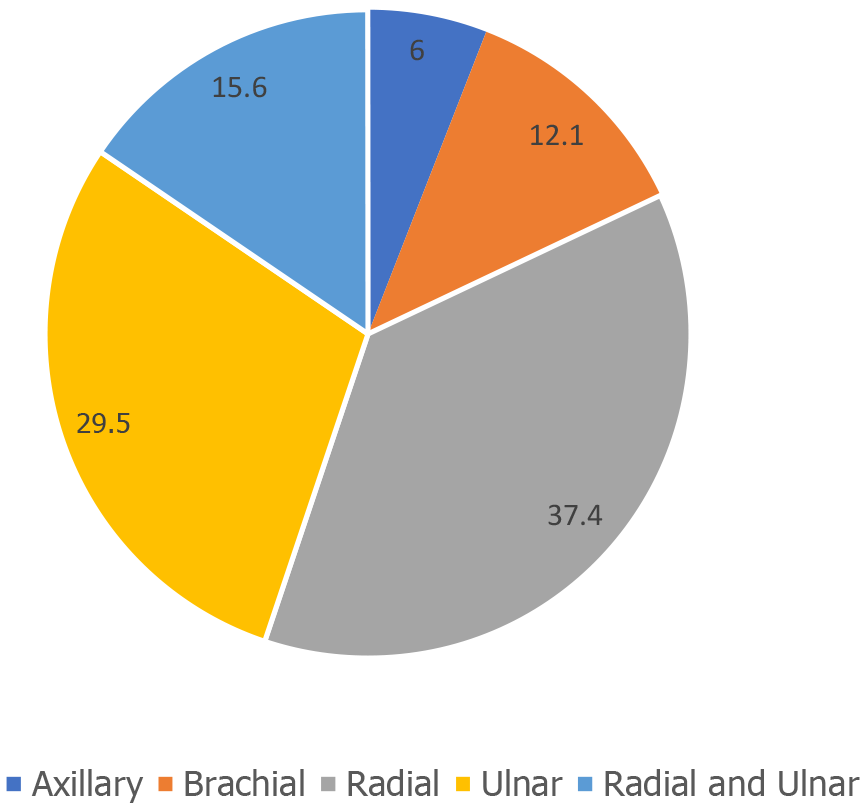
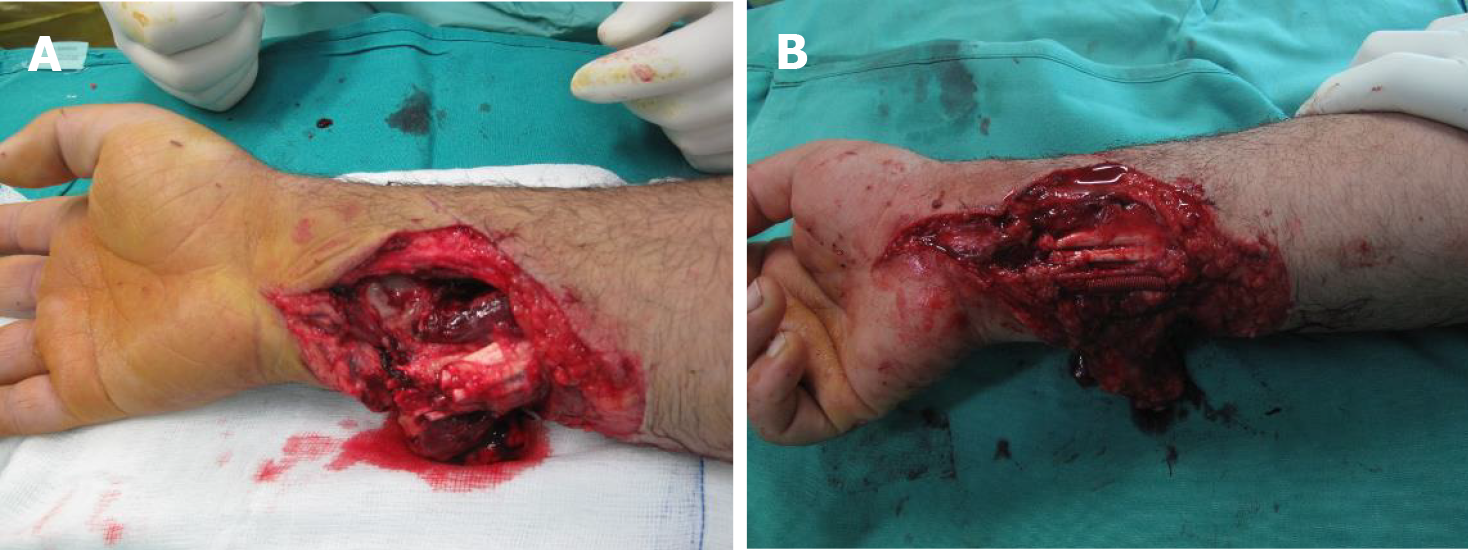
There were identified 7 patients (6%) with lesions to the axillary artery, 14 patients (12.1%) with the brachial artery to be affected and the rest 82% of the patients were injured at the radial, ulnar or even both arteries (Figure 2). Concomitant injuries were reported at 107/115 patients (93%) with more common among them tendon ruptures, nerve lesions, fracture or dislocation and injuries other than the musculoskeletal system (Figure 1A). The tendon of flexor digitorum superficialis was injured in 68% of the cases, the flexor carpi radialis at 65%, the palmaris longus at 60%, the flexor carpi ulnaris at 40% and the flexor digitorum profundus at 55% (Figure 1B). Among the nerves affected, the median nerve was injured at 40% of the cases and the ulnar nerve at 32% (Figure 1C). Nerve autografts (sural nerve) were used for nerve reconstruction when needed (7 cases). Almost half of the patients (54/115, 47%) presented with a spaghetti wrist type of injury (Figure 3). For this type of injury, we set the threshold of the structures involved at 3, including at least one major nerve (median/ulnar) and often one major artery (median/ulnar), according to most accepted definition in literature proposed by Puckett and Meyer in 1985[10]. There were also recorded fractures and soft tissue injuries in patients suffering higher energy trauma treated with open reduction and internal fixation and skin grafts respectively. A CT angiography was used preoperatively at 45 (39%) cases to confirm the diagnosis.
The treatment used most frequently was end-to-end suturing of the injured artery (98/134, 73.1%), followed at 11.2% (15/134) by ligation due to extensive trauma and good collateral circulation. Bypass venous grafting was used in 12.6% (17/134) of the arterial injuries using saphenous vein as a graft and in 10% of the cases limb salvage procedures were performed. Prophylactic fasciotomies were carried out simultaneously with the revascularization surgery in cases of high risk of compartment syndrome since there seems to be a four-times decrease in the rates of eventual amputation (Table 2). Secondary procedures and revisits at the operating theatre were necessary for 28 patients (24%). The reasons for that were closing of the fasciotomies, debridement, tendon transfers, neurolysis, tenolysis or revascularization failure resulting in 5 secondary amputations (Figure 4). Surgical time ranged between 2.1 and 4 h. The mean length of stay was 6 days, range 2 to 43, the shortest a patient who died in the intensive care unit due to head and chest trauma and the longest a patient suffering a forearm amputation with infection requiring stump revision.
| Patients (with 134 arterial injuries), n = 115 | Axillary | Brachial | Radial | Ulnar | Radial and ulnar |
| End to end anastomoses (fasciotomies) | 4 (3) | 8 (5) | 35 | 27 | 24 (of both) (10) |
| Ligation | - | - | 7 | 4 | 4 (1 of 2) |
| By pass venous grafting (fasciotomies) | 3 (1) | 6 (3) | 1 | 3 | 4 (1 of 2) |
| Total (%) | 7 (6) | 14 (12.1) | 43 (37.4) | 34 (29.5) | 18 (15.6) |
At a mean follow up of 7.4 years (from 2 to 14 years), the functional scores had an acceptable value, compared to the severity of the studied injuries. The mean full dash value was 12.8 (from 5 to 68.3) and the mean VAS score, estimating the intensity of posttraumatic pain that these patients live with, was 1.6 (from 1 to 4) (Table 3). There was no significant correlation between anatomic distribution of vascular injury, sex, age, concomitant injuries (nerve, tendons, compartment syndrome, head/neck, abdominal, or lower extremity), mechanism of trauma, MESS-ISS scores, additional operations, post-operative complications, length of stay and postoperative functional assessment.
| Mean values (range) | |
| Full DASH | 12.8 (5-68.3) |
| VAS | 1.6 (1-4) |
Management of injuries of the upper limb including arterial lesions is primarily performed by orthopaedic hand surgeons at our institution with the aid of vascular surgeons for the axillary and brachial arteries. Initial evaluation of the patients was done at the emergency department addressing also concomitant injuries according to the ATLS principles for polytrauma patients. After initial resuscitation and secondary survey many of these injuries were identified due to the presence of hard signs for vascular injury and the patients were admitted as fast as possible for vascular exploration and damage control or definitive treatment in the operating theatre. In the presence of soft signs further imaging studies were needed either to rule out or confirm the diagnosis and proceed with treatment. For simple penetrating wounds and stable patients, diagnostic modalities including, doppler sonography, ultrasonography, CT angiography, were used accordingly per case[11-13].
The most challenging concept of upper extremity vascular trauma, which commonly demands a multidisciplinary approach, is in the setting of complex injuries affecting soft tissue, bones and nerves[14,15]. These injuries require specialties from a field of experts and is time consuming and sometimes difficult to address all lesions at once. Experienced hand orthopaedic surgeons able to treat the whole range of upper extremity trauma and all its consequences, requiring help from vascular surgeons only for complex arterial lesions proximal of the antecubital crease leads to shorter operational times, shorter time to revascularization and low rates of complications and secondary procedures. Also, during initial treatment fasciotomies were performed as deemed necessary lowering in that fashion the return to the OR for that reason[16,17]. For the cases also that primary amputation was the treatment of choice (these patients were excluded from the study), the full extent of the injury was evaluated more accurately and an appropriate and a functional, stump was created[18-20].
Review of the literature regarding upper extremity vascular injuries showed scarce evidence[2,4,5]. All previous studies were conducted at a level I trauma center as in our institution and there are some retrospective series covering periods from 2 to 7 years. To our knowledge, this 20-years series is the longest and one of the largest in the literature with 115 patients[14,21,22]. Also, quality of the data regarding patients’ demographics, mechanism of injury and outcomes offer a deeper insight to understand the crucial parameters affecting the management of that type of injuries. The overall rate of vascular trauma presenting to our department seems to be lower than the average estimated in other series, somewhat lower 1%, and that is explained due to lack of primary health care in the region of the hospital for many of the past years. The study population was in line with that reported in literature, affecting young males in 83.5%. Our case series had a much higher rate of complex upper limb injuries with vascular involvement than found in the literature due to the specific features of the region, agricultural works all year long and the base of many industrial sites, thus presenting many patients with complete and incomplete amputations, high energy and crushing injuries. Therefore, some patients required complex limb salvage procedures but in almost of 10% of the cases primary amputation was performed (MESS ≥ 7), which is a higher percentage comparing to the literature[14].
In the present study the most common treatment was primary repair of the involved artery by end-to-end suturing, whereas ligation was chosen in cases with good collateral circulation and complex injuries. Bypass venous grafting was used in 13.4% of the cases. The rates mentioned above are in accordance with the existent literature describing similar results[5]. This high success rate of treatment, low amputation rate concerning the penetrating and combined trauma and the need for secondary procedures was the result of prompt diagnosis and early treatment as result of the high suspicion rate of our on-call doctors at our emergency department, deep knowledge and expertise of our hand orthopaedic surgeons and the assistance of the anesthesiology department. Parameters mentioned above led to minimizing ischemia time and giving the best possible results treating these patients. For that reason, we suggest that management of such cases should be done in organized centers with such resources.
By searching the literature, we found another retrospective study conducted by Joshi et al[21] in 2007, where the number of patients participated is much smaller but a 5 year follow up is recorded. The interesting point in that study, is the fact that patients suffering from blunt trauma had not only greater motor and sensory deficit postoperatively but also worse DASH scores compared to those who had a penetrating trauma. The explanation to this finding is the concomitant injuries resulting from blunt trauma, that are more common compared to cases with penetrating trauma, and this is a keynote conclusion which we should keep in mind when managing such injuries.
We also noticed in an older retrospective study by Cikrit et al[22] the fact that many of the patients who had a major vessel injury (axillary or brachial artery) presented in the ER with palpable peripheral pulses and most of the patients suffering from an arterial injury had a normal Allen test. This indicates that our suspicion for an arterial damage in cases of laceration injuries, blunt trauma or complex injuries should be strong and we should use all the modern means we have available for a prompt diagnosis. These are principles that we have established in our department in collaboration with the other specialties. Also, a second point we should keep in mind, is the fact that patients with isolated arterial injury had perfect postoperative function. On the other hand, patients with concomitant nerve injuries could have serious functional deficits, indicating that one should be very careful when evaluating such types of injuries. There is a consensus in the literature that the most important prognostic factor for the degree and time of functional recovery is nerve involvement. In our study there was no significant statistical correlation between the functional impairment and the presence of nerve injury. The explanation for this is that the majority of nerve injuries involved peripheral injuries distally from zone 5 of the flexors as well as the absence of explosive injuries such as those from gunshots. Moreover, in all cases the primary repair of nerve injuries was our main goal, with or without the use of nerve grafts.
In the cases of combined vascular and bone injuries the location of trauma dictates the order of fixation. In general, when the vascular injury is located above the elbow, it is the first to be addressed since the time of limb ischemia is critical. Exception to this surgical sequence is when external fixation is required immediately to stabilize the limb after massive musculoskeletal trauma[6]. On the other hand, for forearm arterial injuries, orthopedic stabilization of associated bony injuries typically is performed before vascular reconstruction. As far as the forearm is concerned, it is known that in cases of a single arterial injury, ligation of the radial or ulnar artery can be performed if the presence of collateral blood supply is confirmed. However, we believe that it is better to fix an arterial injury whenever this is possible, in order to avoid possible impairment in musculoskeletal structures, hand grip strength, and hand functionality. There are some older studies supporting that ligation of one out of the two arteries of the forearm leads to cold sensitivity of the hand and wound healing issues but we also rely for this primarily on the experience of our department in the management of these injuries[23,24]. Nevertheless, we must emphasize the fact that most studies were conducted over twenty years ago and a more recent review of outcomes in single-vessel trauma is lacking. Moreover, it is worth to mention a recent meta-analysis which concludes that there is no difference in outcomes after repair or ligation of a single vessel[25]. Finally, if both arteries are injured, ulnar repair is preferred because it is commonly the dominant and larger vessel[26].
In an ischemic upper extremity, revascularization must be performed as soon as possible within the warm ischemia period of 4-6 h to prevent infection and tissue necrosis and minimize the possibility of reperfusion syndrome, although areas with fewer and smaller muscle bellies (e.g. distal to wrist level) can afford longer period of decreased arterial flow prolonging available time for reconstruction up to 24 h[27]. Nayar et al[28] had a systematic review aiming to make clear the rationale behind the decision making for either a primary amputation or a limb salvage procedure after a severe upper limb injury. They concluded that the decision on such matter is multifactorial. Current scoring systems are predominantly based on lower limb trauma, with lack of robust evidence to guide management of the upper extremity. Even though there are some scores showing the way, e.g. MESS (MESSI) introduced by Johansen et al[29] in 1990, in our department we try to give a chance to salvage procedures except for cases of prolonged ischemia or inability to save the limb because of extreme abuse[6,29]. We strongly believe that the good results of our study are due to our adherence to clear diagnostic protocols for combined vascular and musculoskeletal injuries as well as the establishment of an algorithm for the sequential anatomical restoration of injured structures in these types of major and complex injuries of the upper extremity[6,29].
Although vascular injuries of the upper extremity are rare, they may occur in the context of major combined musculoskeletal trauma. Τhe use of distinct diagnostic and therapeutic algorithms for the management of these injuries and the timely referral of these patients to organized trauma centers ensure firstly the survival of the patient and the extremity and secondarily the best functional outcome. Considering soft-tissue damage, the duration of limb ischemia and the patients’ general medical status primary arterial repair is indicated in stable patients if both radial and ulnar arteries are damaged or in the presence of an axillary or brachial arteries injury. Although a multidisciplinary approach is essential to optimize outcome, the ability of trained orthopaedic hand surgeons to repair all injuries in combined vascular and musculoskeletal upper extremity trauma, excluding individual vascular injuries, ensures shorter operative times and better functional outcomes.
Vascular injuries of the upper extremity are rare but complex injuries affecting mostly the young population and causing chronic dysfunction.
The management of this type of injuries is challenging often leading to unpredictable outcomes and dissatisfied patients.
The objectives of this study were to analyze data about the mechanism of injury, the management algorithm and functional outcomes of vascular injuries of the upper extremity.
This retrospective study included 115 patients that suffered an arterial injury between 2003 and 2022 and treated in a tertiary orthopaedic department. Patients with Mangled Extremity Severity Score ≥ 7 and Injury Severity Score ≥ 20, previous upper limb surgery or major trauma and any neuromuscular or psychiatric disease were excluded, from the study. The study analyzed the demographics data of the included patients, the anatomic structures mostly involved, the management and the postoperative outcomes at a mean follow up of 7.4 years.
A penetrating trauma was the most common cause of injury. The radial artery was the artery injured in most of the cases (37.4%) followed by the ulnar (29.5%), the brachial (12.1%) and the axillary (6%). A simultaneous injury of both of the forearm’s arteries was in 15.6% of the cases. In 93% of the cases there were other concomitant musculoskeletal injuries of the extremity. Tendon lacerations were the most common followed by nerve injuries. The postoperative functional scores (full Disabilities of the Arm, Shoulder, and Hand and VAS) had very satisfactory values.
In cases of complex injuries of the upper extremity, primary arterial repair is indicated in stable patients if both radial and ulnar arteries are damaged or in the presence of an axillary or brachial arteries injury. A multidisciplinary approach is essential to optimize postoperative outcome. The ability of trained orthopaedic hand surgeons to repair all injuries in combined vascular and musculoskeletal upper extremity trauma, excluding isolated vascular injuries, ensures better functional outcomes.
The different methods for the diagnosis and management of severe, vascular injuries of the upper extremity were studied.
Provenance and peer review: Invited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Orthopedics
Country/Territory of origin: Greece
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Bassetto F, Italy S-Editor: Liu JH L-Editor: A P-Editor: Che XX
| 1. | Lebowitz C, Matzon JL. Arterial Injury in the Upper Extremity: Evaluation, Strategies, and Anticoagulation Management. Hand Clin. 2018;34:85-95. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 16] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 2. | Fields CE, Latifi R, Ivatury RR. Brachial and forearm vessel injuries. Surg Clin North Am. 2002;82:105-114. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 32] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 3. | Inkellis E, Low EE, Langhammer C, Morshed S. Incidence and Characterization of Major Upper-Extremity Amputations in the National Trauma Data Bank. JB JS Open Access. 2018;3:e0038. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 21] [Cited by in RCA: 33] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 4. | Andrew Koman L. Management of upper extremity arterial penetrating vascular trauma. Injury. 2021;52:3573-3579. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 5. | Kakkos SK, Tyllianakis M, Panagopoulos A, Kokkalis Z, Lianou I, Koletsis E, Tsolakis I, Papadoulas S, Gliatis J, Maroulis I, Kitrou P. Outcome Predictors in Civilian and Iatrogenic Arterial Trauma. World J Surg. 2021;45:160-167. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 6. | Stefanou N, Arnaoutoglou C, Papageorgiou F, Matsagkas M, Varitimidis SE, Dailiana ZH. Update in combined musculoskeletal and vascular injuries of the extremities. World J Orthop. 2022;13:411-426. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 3] [Reference Citation Analysis (0)] |
| 7. | Gonzalez RP, Falimirski ME. The utility of physical examination in proximity penetrating extremity trauma. Am Surg. 1999;65:784-789. [PubMed] |
| 8. | Fox N, Rajani RR, Bokhari F, Chiu WC, Kerwin A, Seamon MJ, Skarupa D, Frykberg E; Eastern Association for the Surgery of Trauma. Evaluation and management of penetrating lower extremity arterial trauma: an Eastern Association for the Surgery of Trauma practice management guideline. J Trauma Acute Care Surg. 2012;73:S315-S320. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 121] [Cited by in RCA: 131] [Article Influence: 10.9] [Reference Citation Analysis (0)] |
| 9. | Hood DB, Weaver FA, Yellin AE. Changing perspectives in the diagnosis of peripheral vascular trauma. Semin Vasc Surg. 1998;11:255-260. [PubMed] |
| 10. | Puckett CL, Meyer VH. Results of treatment of extensive volar wrist lacerations: the spaghetti wrist. Plast Reconstr Surg. 1985;75:714-721. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 43] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 11. | Miller-Thomas MM, West OC, Cohen AM. Diagnosing traumatic arterial injury in the extremities with CT angiography: pearls and pitfalls. Radiographics. 2005;25 Suppl 1:S133-S142. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 115] [Cited by in RCA: 104] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 12. | Montorfano MA, Pla F, Vera L, Cardillo O, Nigra SG, Montorfano LM. Point-of-care ultrasound and Doppler ultrasound evaluation of vascular injuries in penetrating and blunt trauma. Crit Ultrasound J. 2017;9:5. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 29] [Cited by in RCA: 32] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 13. | Fleiter TR, Mervis S. The role of 3D-CTA in the assessment of peripheral vascular lesions in trauma patients. Eur J Radiol. 2007;64:92-102. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 30] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 14. | Myers SI, Harward TR, Maher DP, Melissinos EG, Lowry PA. Complex upper extremity vascular trauma in an urban population. J Vasc Surg. 1990;12:305-309. [PubMed] |
| 15. | Cakir O, Subasi M, Erdem K, Eren N. Treatment of vascular injuries associated with limb fractures. Ann R Coll Surg Engl. 2005;87:348-352. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 34] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 16. | Branco BC, Inaba K, Barmparas G, Schnüriger B, Lustenberger T, Talving P, Lam L, Demetriades D. Incidence and predictors for the need for fasciotomy after extremity trauma: a 10-year review in a mature level I trauma centre. Injury. 2011;42:1157-1163. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 55] [Cited by in RCA: 52] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 17. | Mahajan RK, Srinivasan K, Jain A, Bhamre A, Narayan U, Sharma M. Management of Complex Upper Extremity Trauma with Associated Vascular Injury. Indian J Plast Surg. 2022;55:224-233. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 18. | Peng YP, Lahiri A. Spare-part surgery. Semin Plast Surg. 2013;27:190-197. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 32] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 19. | MacKenzie EJ, Jones AS, Bosse MJ, Castillo RC, Pollak AN, Webb LX, Swiontkowski MF, Kellam JF, Smith DG, Sanders RW, Jones AL, Starr AJ, McAndrew MP, Patterson BM, Burgess AR. Health-care costs associated with amputation or reconstruction of a limb-threatening injury. J Bone Joint Surg Am. 2007;89:1685-1692. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 150] [Cited by in RCA: 167] [Article Influence: 9.3] [Reference Citation Analysis (0)] |
| 20. | Korompilias AV, Beris AE, Lykissas MG, Vekris MD, Kontogeorgakos VA, Soucacos PN. The mangled extremity and attempt for limb salvage. J Orthop Surg Res. 2009;4:4. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 29] [Cited by in RCA: 29] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 21. | Joshi V, Harding GE, Bottoni DA, Lovell MB, Forbes TL. Determination of functional outcome following upper extremity arterial trauma. Vasc Endovascular Surg. 2007;41:111-114. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 30] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 22. | Cikrit DF, Dalsing MC, Bryant BJ, Lalka SG, Sawchuk AP, Schulz JE. An experience with upper-extremity vascular trauma. Am J Surg. 1990;160:229-233. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 38] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 23. | Aftabuddin M, Islam N, Jafar MA, Haque E, Alimuzzaman M. Management of isolated radial or ulnar arteries at the forearm. J Trauma. 1995;38:149-151. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 23] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 24. | Lee RE, Obeid FN, Horst HM, Bivins BA. Acute penetrating arterial injuries of the forearm. Ligation or repair? Am Surg. 1985;51:318-324. [PubMed] |
| 25. | Schippers SM, Hajewski C, Glass NA, Caldwell L. Single Forearm Vessel Injury in a Perfused Hand: Repair or Ligate? A Systematic Review. Iowa Orthop J. 2018;38:159. [PubMed] |
| 26. | Franz RW, Goodwin RB, Hartman JF, Wright ML. Management of upper extremity arterial injuries at an urban level I trauma center. Ann Vasc Surg. 2009;23:8-16. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 36] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 27. | Chipman AM, Ottochian M, Ricaurte D, Gunter G, DuBose JJ, Stonko DP, Feliciano DV, Scalea TM, Morrison J. Contemporary management and time to revascularization in upper extremity arterial injury. Vascular. 2023;31:284-291. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 6] [Reference Citation Analysis (0)] |
| 28. | Nayar SK, Alcock HMF, Edwards DS. Primary amputation versus limb salvage in upper limb major trauma: a systematic review. Eur J Orthop Surg Traumatol. 2022;32:395-403. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 13] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 29. | Johansen K, Daines M, Howey T, Helfet D, Hansen ST Jr. Objective criteria accurately predict amputation following lower extremity trauma. J Trauma. 1990;30:568-72; discussion 572. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 474] [Cited by in RCA: 374] [Article Influence: 10.7] [Reference Citation Analysis (0)] |