Published online May 9, 2022. doi: 10.5492/wjccm.v11.i3.169
Peer-review started: September 3, 2021
First decision: December 2, 2021
Revised: December 11, 2021
Accepted: March 6, 2022
Article in press: March 6, 2022
Published online: May 9, 2022
Processing time: 245 Days and 10.3 Hours
There is variability in intensive care unit (ICU) resources and staffing worldwide. This may reflect variation in practice and outcomes across all health systems.
To improve research and quality improvement measures administrative leaders can create long-term strategies by understanding the nature of ICU practices on a global scale.
The Global ICU Needs Assessment Research Group was formed on the basis of diversified skill sets. We aimed to survey sites regarding ICU type, availability of staffing, and adherence to critical care protocols. An international survey ‘Global ICU Needs Assessment’ was created using Google Forms, and this was distributed from February 17th, 2020 till September 23rd, 2020. The survey was shared with ICU providers in 34 countries. Various approaches to motivating healthcare providers were implemented in securing submissions, including use of emails, phone calls, social media applications, and WhatsApp™. By completing this survey, providers gave their consent for research purposes. This study was deemed eligible for category-2 Institutional Review Board exempt status.
There were a total 121 adult/adult-pediatrics ICU responses from 34 countries in 76 cities. A majority of the ICUs were mixed medical-surgical [92 (76%)]. 108 (89%) were adult-only ICUs. Total 36 respondents (29.8%) were 31-40 years of age, with 79 (65%) male and 41 (35%) female participants. 89 were consultants (74%). A total of 71 (59%) respondents reported having a 24-h in-house intensivist. A total of 87 (72%) ICUs were reported to have either a 2:1 or ≥ 2:1 patient/nurse ratio. About 44% of the ICUs were open and 76% were mixed type (medical-surgical). Protocols followed regularly by the ICUs included sepsis care (82%), ventilator-associated pneumonia (79%); nutrition (76%), deep vein thrombosis prophylaxis (84%), stress ulcer prophylaxis (84%), and glycemic control (89%).
Based on the findings of this international, multi-dimensional, needs-assessment survey, there is a need for increased recruitment and staffing in critical care facilities, along with improved patient-to-nurse ratios. Future research is warranted in this field with focus on implementing appropriate health standards, protocols and resources for optimal efficiency in critical care worldwide.
Core Tip: Intensive care unit (ICU) practices are variable across the world. Most common admitting diagnoses for ICUs worldwide are similar to Western reporting in literature. We aimed to survey sites regarding ICU type, availability of staffing, and adherence to critical care protocols. There is variable protocol penetration for processes of care in ICUs. Future research is warranted in this field with focus on implementing appropriate health standards, protocols and resources for optimal efficiency in critical care worldwide.
- Citation: Nawaz FA, Deo N, Surani S, Maynard W, Gibbs ML, Kashyap R. Critical care practices in the world: Results of the global intensive care unit need assessment survey 2020. World J Crit Care Med 2022; 11(3): 169-177
- URL: https://www.wjgnet.com/2220-3141/full/v11/i3/169.htm
- DOI: https://dx.doi.org/10.5492/wjccm.v11.i3.169
Critical care is defined by varying practices across countries worldwide. This is affected by multi-factorial trends in epidemiology, finance, and cultural and human resources that in turn influence patient outcomes[1].
Intensive care units (ICUs) are at the center of diverse practices in health systems around the world. Their needs are dictated by hierarchical arrangements, resource designation, patient demographics, and health practices, including the allied goals of health providers[2]. With a necessity for standardization deemed essential for efficiency and high-quality patient care, it is vital to understand the context of epidemiological variability, resource accessibility, and local health practices[3] in such sophisticated settings. Moreover, the current understanding and comparison of clinical practices, guidelines, equipment, and facilities available in different countries can help identify potential areas of quality improvement via protocol development and enhancement of unified care delivery. Current literature on this topic can be found in developed countries[4,5]; however, it is significantly limited in multinational settings[6-8] on a global level.
We aimed to delineate the critical care practices that are found worldwide and their characteristics, including staffing, ICU resources, and adherence to protocols. This study sets a novel benchmark in sharing insights on key areas of critical care by highlighting the state of ICUs across different countries and understanding the trends in contemporary health systems. By defining gaps in knowledge, resources, and protocols, this study can facilitate the development of best practice strategies and thereby lay a strong foundation for critical care provision worldwide[9].
This was a cross-sectional, multinational, survey-based study. We proposed the formation of a multidisciplinary, diverse team of skilled researchers who established the “Global ICU Needs Assessment Research Group”.
A questionnaire was developed under the guidance of this research group with the goal of evaluating most common patient presentations, and resource needs in terms of ICU equipment and assisting technology.
Furthermore, we asked about other variables, such as the availability of intensivists, residents, fellows, 12-h in-house intensivists, and patient/nurse ratio, along with other demographics of those surveyed, such as their level of qualification, duration of clinical experience, and overall expertise in this field. It was also deemed crucial to include outcome variables, such as mechanical ventilation (MV) duration, MV mortality, ICU length of stay, ICU mortality, and sepsis mortality as well. Using a pilot study approach, we implemented this strategy within a randomized group of ICU clinicians before proceeding with the main study phase. This was done for internal validation purposes in the form of a survey shown in the digital supplement.
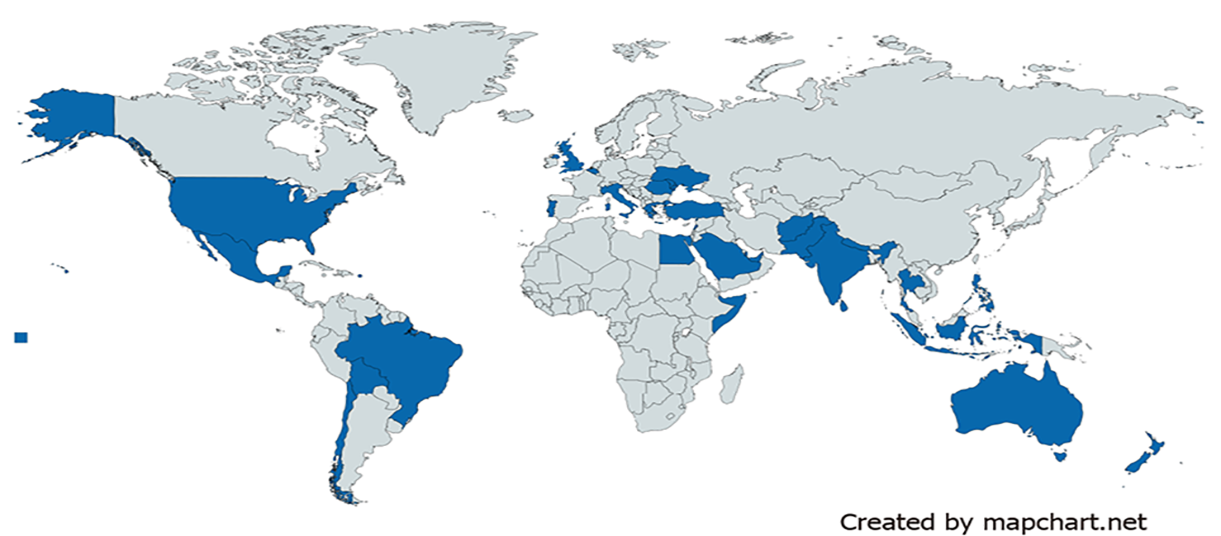
Sample of convenience was done. Intensivists were contacted using social media platforms and personal networking and via critical care societies. The survey was designed using Google™ forms online and sent out from February 17th, 2020 to 23rd September, 2020, to critical care professionals in 34 countries worldwide (Figure 1). The need for regular follow-ups and motivation within critical care professionals was a vital factor to this study. This was achieved by leveraging various online platforms, such as e-mail and social media applications including WhatsApp™[20].
Using a diverse set of researchers, critical care physicians, and digital platforms, a sample of 122 ICUs was acquired through this questionnaire.
The responses were presented as stratified data in the form of mean, with standard deviation, or median with interquartile range. It was also deemed necessary to include relevant pictographic presentation of this data.
Descriptive statistical analysis was used after obtaining eligibility for category-2 Institutional Review Board exempt status.
ICU practices at a given healthcare facility, including details about the respondents and demographics of the facility. The survey asked about the state of the ICU being open or closed, type of patients receiving care, number of ICU beds, protocols implemented for efficient practice.
The respondents of this survey primarily reflected a young adult population, with the respondents of this survey primarily reflected a young adult population with the greatest proportion 31-40 years old and males representing the majority, n = 79 (65%) with an average ICU experience of 3 years. Moreover, consultants were the main constituents of the survey respondents at n = 89 (74%), followed by residents from post-graduate year 3 and above (18, 15%). The ICU settings were mostly designed as a mixed medical-surgical environment (92, 76%) in academic teaching hospitals (38, 32%) with an average of 16 (interquartile range 11-20) beds. Furthermore, the ICUs were commonly open type, (53, 44%) (Table 1).
| Demographic variables | Responses in % (n = 121) |
| Age (yr) | |
| 31-40 | 29.8 |
| 41-50 | 23.1 |
| 20-30 | 23.1 |
| > 50 | 24.0 |
| Gender | |
| Male | 65.3 |
| Female | 34.7 |
| Intensive care unit experience (yr) | |
| < 10 | 50.4 |
| 10-20 | 35.5 |
| 21-30 | 9.9 |
| > 30 | 4.1 |
| Designation | |
| Consultant staff | 73.6 |
| Resident-PGY-3 and above | 14.9 |
| Resident-PGY-1 | 5.0 |
| Resident-PGY-2 | 6.6 |
| Intensive care unit specialty wise distribution | |
| Mixed medical-surgical | 76.0 |
| Medical | 7.4 |
| Others | 16.6 |
| Institution type | |
| Private/non-academic | 16.5 |
| Government hospital (tertiary care) | 19.8 |
| Academic teaching hospital | 31.5 |
| Corporate teaching hospital | 8.2 |
| Other | 0.9 |
| Number of intensive care unit beds | |
| < 11 | 28.1 |
| 11-20 | 31.4 |
| 21-30 | 23.1 |
| > 30 | 17.4 |
| Intensive care unit type | |
| Open | 43.8 |
| Closed | 56.2 |
The need for intensivists and nurses to lead critical care is noted worldwide[1]. The analysis showed a patient/nurse ratio of 2:1 being implemented in the majority (55%) of the ICU units, and only (10%) of responders were following a 1:1 nursing care approach. Moreover, 34% of ICUs, which typically functioned at 2:1 patient/nurse ratios, transferred to 1:1 for complicated cases. There was also a significant number of ICUs (20, 16.5%) working with more than a 2:1 patient/nurse ratio. It is also noteworthy that a vast majority of the ICUs (101, 84%) were led by certified intensivists with 24-h intensivists deployed in 71 (59%) of the ICUs for optimal patient care. Other notable providers were residents/fellows/medical students active in 101 (84%) ICU units (Table 2).
| Clinical resource parameters | Responses in % (n = 121) |
| Patient/nurse ratio (n) | |
| Usually 2:1 (for complicated patients 1:1) (n = 41) | 33.9 |
| 2:1 (n = 26) | 21.5 |
| > 2:1 (n = 20) | 16.5 |
| 1:1 (n = 31) | 25.6 |
| No fixed patient/nurse (n = 3) | 2.5 |
| 24 h in-house intensivist (n = 71) | 58.7 |
| Certified intensivist (n = 101) | 83.5 |
| Residents/fellows/medical students rotate through or cover intensive care units along with staff intensivists (n = 101) | 83.5 |
Critical care was driven by protocols that were followed within all ICU facilities. There was a strong predominance of protocols for Advanced Cardiac Life Support (93%), glucose control (89%), stress ulcer prophylaxis (84%), deep vein thrombosis (DVT) prophylaxis (84%) and sepsis care (82%). The protocols least reported included palliative care/end of life (44%), acute lung injury (55%), transfusion restriction (59%), hypothermia after cardiac arrest (61%), and delirium (67%) (Table 3).
| High (%) | Medium (%) | Low (%) | |||
| Glucose control | 89.3 | Daily interruption of sedation | 69.4 | Palliative care/end of Life | 43.8 |
| Advanced cardiac life support | 93.4 | Acute coronary syndrome | 81.0 | Delirium | 66.9 |
| Deep vein thrombosis prophylaxis | 83.5 | Acute lung injury | 54.5 | Early mobility | 68.6 |
| Stress ulcer prophylaxis | 83.5 | Transfusion restriction | 58.7 | Hypothermia after cardiac arrest | 61.2 |
| Severe sepsis | 81.7 | ||||
| Ventilator-associated pneumonia bundle | 78.5 | ||||
| Nutrition | 76.0 | ||||
The sample population was analyzed across a total 121 adult/adult-pediatrics ICU responses from 34 countries in 76 cities. Distribution of the respondents was spread amongst North America (41.3%), Asia (30.5%), Europe (18.2%), Africa (5.8%), South Africa (2.6%) and Oceania (1.6%) (Figure 1).
The most common diagnoses for patients admitted into the ICU settings in this study included sepsis (88%), respiratory failure (88%) and heart failure (55%), as shown in Table 4.
| Common diagnoses | No | % of intensive care unit |
| Sepsis or septic shock | 106 | 87.6 |
| Respiratory failure | 106 | 87.6 |
| Heart failure | 67 | 55.4 |
| Post-operative observation | 68 | 56.2 |
| Poisoning | 15 | 12.4 |
| Head trauma | 37 | 30.6 |
| Renal failure | 46 | 38.0 |
| Alcohol withdrawal | 13 | 10.7 |
| Epilepsy or uncontrolled seizures | 18 | 14.9 |
| Chronic obstructive pulmonary disease exacerbation | 37 | 30.6 |
| Hypertension | 15 | 12.4 |
| Cardiogenic shock | 37 | 30.6 |
| Electrolyte imbalance | 20 | 16.5 |
| Hypotension or hypovolemic shock | 44 | 36.4 |
| Heat stroke | 4 | 3.3 |
The average ICU mortality (n = 36) assessed in this survey was 14% (interquartile range 2-40); ICU length of stay (n = 41) was 5.2 d (interquartile range 2-21); mechanical ventilation (MV) duration (n = 34) was 4.3 d (1-15); MV patient mortality (n = 27) was 20% (1-64) and sepsis mortality (n = 27) was at 21% (5-70) across the survey respondents (Table 5).
| Variables | Outcome |
| Intensive care unit mortality (response n =36) | 14% |
| Intensive care unit length of stay, in days (response n = 41) | 5.2 |
| Mechanical ventilation mortality (response n = 27) | 19.5% |
| Mechanical ventilation duration, in days (response n = 34) | 4.3 |
| Sepsis mortality (response n = 27) | 21.2% |
In a multi-national study that evaluates the critical care practices of 121 ICUs in 34 countries, the majority of the centers were from mixed medical-surgical or medical practices, with consultants comprising the majority of respondents. The most common diagnoses included sepsis/septic shock and respiratory failure. The largest proportion of responders were young adult males who identified as intensivists, suggesting that this field is expanding to include more learners who are early in their training.
Considering that this was a multinational study, it is important to note that local practices and resources may vary between different regions. A lack of resources may limit the total number of beds available, or even result in a lower number of monthly admissions[10] in a given center relative to other regions. Because financial resources may influence how patients are triaged or how the healthcare organization is structured[11], it is important to keep this in mind when evaluating multi-center data from different countries.
The predominant diagnosis in the ICU was sepsis. Studies show that sepsis has a mortality rate varying from 13% to 39%[12]. The second most common diagnosis was respiratory failure, with studies indicating a mortality rate of 26.2%[13]. Both sepsis and respiratory failure followed the same trend that is observed in country-specific ICU studies[14]. Considering that the mortality rates of both diseases are so high, it is imperative that ICUs are equipped with the resources and training to achieve best practice guidelines[15].
Many of the reported surveys were from individuals in mixed medical-surgical ICUs that were closed in nature and had 24-h intensivists. Additionally, the greatest number of the respondents reported having 11-20 beds in the ward. Most of these centers were within academic or privately-owned hospitals. Although it is believed that ICUs with more beds will achieve better optimal care, it is important to consider that more money shifted towards ICUs will limit funding to other departments[16]. This predominantly impacts areas of low-resource settings, which is why the median ICU beds in low-income countries is 8[7]. Closed ICUs are associated with better outcomes, such as shorter ICU stay and decreased ICU costs[17]. North America is reported to have the lowest amount of closed ICUs (63%), with Western Europe having the highest (89%) (17). Since closed ICUs require an intensivist working on site, more and more ICUs are now including a 24-h intensivist, which can lead to decreased risk of in-hospital death and rate of complications[1].
Respondents most often reported a patient/nurse ratio of 2:1, which flexed to 1:1 for complicated patients. In a study by Sakr et al[1] it was reported that a patient/nurse ratio of more than 1.5:1 was associated with a higher risk of in-hospital death. Adequate care in ICUs requires proper staffing of nurses. This can greatly impact patient outcomes, especially if there are limited nurses available to provide care[1]. A high patient/nurse ratio can result in more mistakes being made due to a stressful work environment and fatigue[18]. It is imperative that adequate staffing is provided to ICUs to best provide patient care in an optimized environment.
Kredo et al[19] noted that evidence-informed best practice guidelines are imperative to optimizing patient care. A multifaceted, team-based approach in the ICU is the best way of reinforcing these guidelines and developing strategies that can better manage the patient or prevent complications[15]. In our survey, we found that a majority of centers are able to follow best practice guidelines related to glucose control, advanced cardiac life support, DVT prophylaxis, and stress ulcer prophylaxis. However, challenges exist with protocols related to palliative care, acute lung injury, and transfusion restriction. It is important to address barriers to guideline adherence, which can differ from region to region. Some commonly reported barriers include lack of knowledge[20] or needing effective leadership to promote adoption of guidelines[21].
The strengths of this study include being one of the first multinational surveys to collect data from 34 countries during the pandemic of the century[22]. Having more regions participate in a survey like this is beneficial because it provides a snapshot of the ICU statistics in that area. A multi-center design allows for a broader range of data representing the resources of each area vs a single center study. These data can be used to evaluate current ICU resources and limitations worldwide and can therefore help administration create designs to optimize care for patients who are in the critical care unit. Such multi-national collaborations would lead to robust data collection during pandemic and peace times[23-25].
Our study has several limitations. First, since our primary recruitment method was through social media and networking at critical care societies, we may be missing out on data from remote areas or sites that did not see our recruitment invitation online. Second, as we had only 34 countries represented, a larger sample size from different geographical locations would allow us to understand the needs of the ICU in those regions better. Recall bias is also a factor in survey studies, as participants may not be able to fill in all the information as accurately as possible. Additionally, since this survey was filled out during the year of the coronavirus disease 2019 pandemic, ICUs may have been impacted or changed very drastically to meet the needs of their community. Therefore, the reported results may not accurately reflect ICU data prior to the pandemic. A final limitation to our study is that we did not stratify our data into geographical regions to evaluate differences from region to region. Further research could aim to delineate this data.
This international, multi-dimensional, needs-assessment survey reflects a need for increased recruitment and staffing in critical care facilities, along with improved patient-to-nurse ratios. Multi-center ICU data are imperative in designing future critical care delivery models that reflect the needs of the patient and address barriers to their care. Understanding current trends in health systems helps us develop quality improvement interventions that can lead to better outcomes in patients.
There is variability in intensive care unit (ICU) resources and staffing worldwide. This may reflect variation in practice and outcomes across all health systems.
By understanding the nature of ICU practices on a global scale, administrative leaders can create long-term strategies for improved research and quality improvement measures.
We aimed to delineate the critical care practices that are found worldwide and their characteristics, including staffing, ICU resources, and adherence to protocols.
An international survey ‘Global ICU Needs Assessment 2020’ was created using Google Forms, and this was distributed from February 17th, 2020 till September 23rd, 2020. The survey was shared with ICU providers in 34 countries.
There were a total 121 adult/adult-pediatrics ICU responses from 34 countries in 76 cities. A majority of the ICUs were mixed medical-surgical (92, 76%). 108 (89%) were adult-only ICUs. Total 36 respondents (29.8%) were 31-40 years of age, with 79 (65%) male and 41 (35%) female participants. 89 were consultants (74%). A total of 71 (59%) respondents reported having a 24-h in-house intensivist.
Based on the findings of this international, multi-dimensional, needs-assessment survey, there is a need for increased recruitment and staffing in critical care facilities, along with improved patient-to-nurse ratios.
Future research is warranted in this field with focus on implementing appropriate health standards, protocols and resources for optimal efficiency in critical care worldwide.
Provenance and peer review: Invited article; Externally peer reviewed.
Peer-review model: Single blind
Corresponding Author's Membership in Professional Societies: American College of Chest Physician; Society of Critical Care Medicine.
Specialty type: Critical care medicine
Country/Territory of origin: United States
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B, B, B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Lopes-Junior LC, Brazil; Sánchez JIA, Colombia S-Editor: Wang JJ L-Editor: A P-Editor: Wang JJ
| 1. | Sakr Y, Moreira CL, Rhodes A, Ferguson ND, Kleinpell R, Pickkers P, Kuiper MA, Lipman J, Vincent JL; Extended Prevalence of Infection in Intensive Care Study Investigators. The impact of hospital and ICU organizational factors on outcome in critically ill patients: results from the Extended Prevalence of Infection in Intensive Care study. Crit Care Med. 2015;43:519-526. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 126] [Cited by in RCA: 148] [Article Influence: 14.8] [Reference Citation Analysis (0)] |
| 2. | Kartik M, Gopal PBN, Amte R. Quality Indicators Compliance Survey in Indian Intensive Care Units. Indian J Crit Care Med. 2017;21:187-191. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 6] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 3. | Smith GR Jr, Ma M, Hansen LO, Christensen N, O'Leary KJ. Association of hospital admission service structure with early transfer to critical care, hospital readmission, and length of stay. J Hosp Med. 2016;11:669-674. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 4. | Fowler RA, Abdelmalik P, Wood G, Foster D, Gibney N, Bandrauk N, Turgeon AF, Lamontagne F, Kumar A, Zarychanski R, Green R, Bagshaw SM, Stelfox HT, Foster R, Dodek P, Shaw S, Granton J, Lawless B, Hill A, Rose L, Adhikari NK, Scales DC, Cook DJ, Marshall JC, Martin C, Jouvet P; Canadian Critical Care Trials Group; Canadian ICU Capacity Group. Critical care capacity in Canada: results of a national cross-sectional study. Crit Care. 2015;19:133. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 40] [Cited by in RCA: 53] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 5. | Juneja D, Nasa P, Singh O. Physician staffing pattern in intensive care units: Have we cracked the code? World J Crit Care Med. 2012;1:10-14. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 13] [Cited by in RCA: 9] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 6. | Chittawatanarat K, Sataworn D, Thongchai C; Thai Society of Critical Care Medicine Study Group. Effects of ICU characters, human resources and workload to outcome indicators in Thai ICUs: the results of ICU-RESOURCE I study. J Med Assoc Thai. 2014;97 Suppl 1:S22-S30. [PubMed] |
| 7. | Murthy S, Leligdowicz A, Adhikari NK. Intensive care unit capacity in low-income countries: a systematic review. PLoS One. 2015;10:e0116949. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 176] [Cited by in RCA: 227] [Article Influence: 22.7] [Reference Citation Analysis (0)] |
| 8. | Vukoja M, Riviello E, Gavrilovic S, Adhikari NK, Kashyap R, Bhagwanjee S, Gajic O, Kilickaya O; CERTAIN Investigators. A survey on critical care resources and practices in low- and middle-income countries. Glob Heart. 2014;9:337-42.e1. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 68] [Article Influence: 6.2] [Reference Citation Analysis (0)] |
| 9. | Kashyap R, Nawaz F, Deo N, Surani SR, Global ICU Need Assessment (GINA) study group. Critical Care Practice in the World: Results of the Global ICU Need Assessment Survey (GINA 2020). Am J Respir Crit Care Med. 2021;203:A1699. [DOI] [Full Text] |
| 10. | Singer DE, Carr PL, Mulley AG, Thibault GE. Rationing intensive care--physician responses to a resource shortage. N Engl J Med. 1983;309:1155-1160. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 158] [Cited by in RCA: 141] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 11. | Vestergaard AH, Christiansen CF, Nielsen H, Christensen S, Johnsen SP. Geographical variation in use of intensive care: a nationwide study. Intensive Care Med. 2015;41:1895-1902. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 9] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 12. | Sakr Y, Jaschinski U, Wittebole X, Szakmany T, Lipman J, Ñamendys-Silva SA, Martin-Loeches I, Leone M, Lupu MN, Vincent JL; ICON Investigators. Sepsis in Intensive Care Unit Patients: Worldwide Data From the Intensive Care over Nations Audit. Open Forum Infect Dis. 2018;5:ofy313. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 141] [Cited by in RCA: 278] [Article Influence: 39.7] [Reference Citation Analysis (0)] |
| 13. | Zahar JR, Azoulay E, Klement E, De Lassence A, Lucet JC, Regnier B, Schlemmer B, Bedos JP. Delayed treatment contributes to mortality in ICU patients with severe active pulmonary tuberculosis and acute respiratory failure. Intensive Care Med. 2001;27:513-520. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 82] [Cited by in RCA: 84] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 14. | Kashyap R, Vashistha K, Saini C, Dutt T, Raman D, Bansal V, Singh H, Bhandari G, Ramakrishnan N, Seth H, Sharma D, Seshadri P, Daga MK, Gurjar M, Javeri Y, Surani S, Varon J; ININ-2018 Investigators Team. Critical care practice in India: Results of the intensive care unit need assessment survey (ININ2018). World J Crit Care Med. 2020;9:31-42. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 4] [Cited by in RCA: 9] [Article Influence: 1.8] [Reference Citation Analysis (2)] |
| 15. | Aragon D, Sole ML. Implementing best practice strategies to prevent infection in the ICU. Crit Care Nurs Clin North Am. 2006;18:441-452. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 16] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 16. | Valley TS, Noritomi DT. ICU beds: less is more? Intensive Care Med. 2020;46:1594-1596. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 10] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 17. | Vincent JL. Evidence supports the superiority of closed ICUs for patients and families: Yes. Intensive Care Med. 2017;43:122-123. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 13] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 18. | Sasichay-Akkadechanunt T, Scalzi CC, Jawad AF. The relationship between nurse staffing and patient outcomes. J Nurs Adm. 2003;33:478-485. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 97] [Cited by in RCA: 96] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 19. | Kredo T, Bernhardsson S, Machingaidze S, Young T, Louw Q, Ochodo E, Grimmer K. Guide to clinical practice guidelines: the current state of play. Int J Qual Health Care. 2016;28:122-128. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 202] [Cited by in RCA: 280] [Article Influence: 31.1] [Reference Citation Analysis (0)] |
| 20. | Jansson M, Ala-Kokko T, Ylipalosaari P, Syrjälä H, Kyngäs H. Critical care nurses' knowledge of, adherence to and barriers towards evidence-based guidelines for the prevention of ventilator-associated pneumonia--a survey study. Intensive Crit Care Nurs. 2013;29:216-227. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 48] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 21. | Sinuff T, Cook D, Giacomini M, Heyland D, Dodek P. Facilitating clinician adherence to guidelines in the intensive care unit: A multicenter, qualitative study. Crit Care Med. 2007;35:2083-2089. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 114] [Cited by in RCA: 112] [Article Influence: 6.2] [Reference Citation Analysis (0)] |
| 22. | Shah A, Kashyap R, Tosh P, Sampathkumar P, O'Horo JC. Guide to Understanding the 2019 Novel Coronavirus. Mayo Clin Proc. 2020;95:646-652. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 64] [Cited by in RCA: 64] [Article Influence: 12.8] [Reference Citation Analysis (0)] |
| 23. | Walkey AJ, Kumar VK, Harhay MO, Bolesta S, Bansal V, Gajic O, Kashyap R. The Viral Infection and Respiratory Illness Universal Study (VIRUS): An International Registry of Coronavirus 2019-Related Critical Illness. Crit Care Explor. 2020;2:e0113. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 72] [Cited by in RCA: 71] [Article Influence: 14.2] [Reference Citation Analysis (0)] |
| 24. | Walkey AJ, Sheldrick RC, Kashyap R, Kumar VK, Boman K, Bolesta S, Zampieri FG, Bansal V, Harhay MO, Gajic O. Guiding Principles for the Conduct of Observational Critical Care Research for Coronavirus Disease 2019 Pandemics and Beyond: The Society of Critical Care Medicine Discovery Viral Infection and Respiratory Illness Universal Study Registry. Crit Care Med. 2020;48:e1038-e1044. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 26] [Cited by in RCA: 44] [Article Influence: 8.8] [Reference Citation Analysis (0)] |
| 25. | Domecq JP, Lal A, Sheldrick CR, Kumar VK, Boman K, Bolesta S, Bansal V, Harhay MO, Garcia MA, Kaufman M, Danesh V, Cheruku S, Banner-Goodspeed VM, Anderson HL 3rd, Milligan PS, Denson JL, St Hill CA, Dodd KW, Martin GS, Gajic O, Walkey AJ, Kashyap R; Society of Critical Care Medicine Discovery Viral Infection and Respiratory Illness Universal Study (VIRUS): COVID-19 Registry Investigator Group. Outcomes of Patients With Coronavirus Disease 2019 Receiving Organ Support Therapies: The International Viral Infection and Respiratory Illness Universal Study Registry. Crit Care Med. 2021;49:437-448. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 102] [Cited by in RCA: 97] [Article Influence: 24.3] [Reference Citation Analysis (0)] |