Published online Nov 9, 2021. doi: 10.5492/wjccm.v10.i6.377
Peer-review started: February 1, 2021
First decision: March 17, 2021
Revised: March 19, 2021
Accepted: August 20, 2021
Article in press: August 20, 2021
Published online: November 9, 2021
Processing time: 276 Days and 14.8 Hours
Trauma is a major cause of morbidity globally and the sixth leading cause of death, accounting for 10% of all mortalities. The genitourinary trauma is estimated for approximately 10% of all patients presenting with trauma, and the kidney is the most injured genitourinary organ globally. However, there is a paucity of data on genitourinary injury from the Sub-Saharan, and there may be variations from common genitourinary organs injured in developed nations.
To provide insight on the epidemiology and management of genitourinary trauma in Sub-Saharan Africa with recommendations based on international guidelines.
A thorough literature search of genitourinary trauma was conducted using PubMed, Google Scholar and African Journal Online.
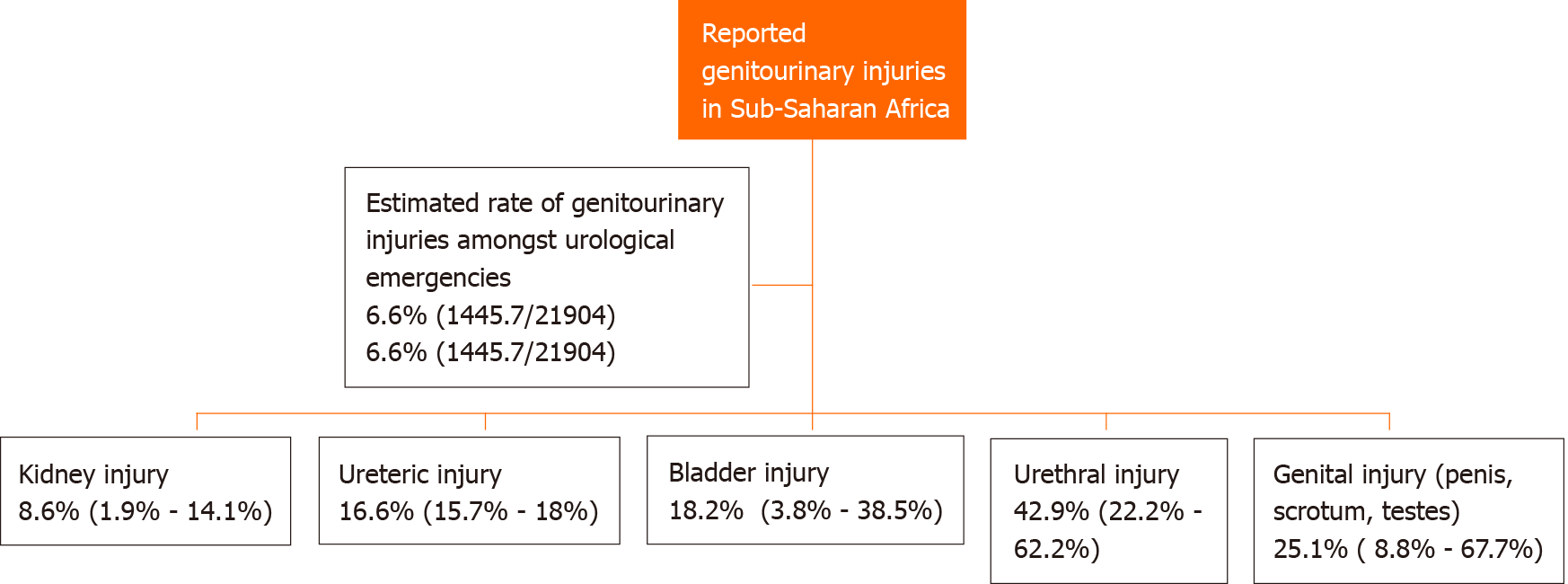
A total of 30 studies from the Sub-Saharan region were eligible for the study and reviewed for epidemiology, biodata, types of injury, mechanisms of injury, treatment and follow-up. After evaluating 21904 patients presenting with urological emergencies, approximately 6.6% of cases were due to genitourinary trauma. The commonest injury was urethral 42.9% (22.2-62.2%) followed by injury to the external genitalia (penis, scrotum, testes) 25.1% (8.8-67.7%).
Genitourinary injury in Sub-Saharan Africa is underreported, and the presence of more trauma registries, trained urologists and trauma facilities could improve the overall standard of care as well as providing data for research and development in the field.
Core Tip: The genitourinary trauma accounts for about 10% of all patients presenting with trauma, and the kidney is the most injured genitourinary organ globally. In Sub-Saharan Africa, after evaluating 21904 patients presenting with urological emer
- Citation: Cassell III AK, Manobah B. Management of genitourinary trauma – current evaluation from the Sub-Saharan region: A systematic review. World J Crit Care Med 2021; 10(6): 377-389
- URL: https://www.wjgnet.com/2220-3141/full/v10/i6/377.htm
- DOI: https://dx.doi.org/10.5492/wjccm.v10.i6.377
Trauma is a major cause of morbidity globally and the sixth leading cause of death, approximately 10% of all mortalities[1]. Trauma is most common in the ages between 15-45 years with a male predominance[2,3]. A global trauma morbidity and mortality study by James et al[4] reported that in 1990, there were about 4260493 injury deaths, which subsequently increased to 4484722 deaths in 2017. The increasing trauma burden is now of global concern making it a component of the Sustainable Develo
The genitourinary tract has continually been injured in about 10% of patients presenting with trauma[5]. Renal trauma is the most frequent injury occurring in about 5% of all traumatic injury and 10% of abdominal injuries[1]. A registry of 43000 trauma victims in France by Paparel et al[6] showed that the rate of genitourinary injury was 0.5%, with the kidney (43%) and testes (24%) most affected. Motor vehicle accidents account for more than 70% of blunt renal injuries.
Ureteral trauma is rare and occurs in less than 1% of all urological trauma[5]. A review of the National Trauma Data Bank in the United States revealed that ureteral injury is more common amongst the younger population usually due to penetrating trauma than blunt trauma[7]. About 88% of the penetrating trauma was due to gunshot wounds, while most blunt injuries were associated with motor vehicle accidents (50%)[5]. Nearly 91% of patients with ureteral injuries have associated injuries usually in the colon, appendix and small bowel[7,8]. The rate of iatrogenic injuries following gynecological procedures range from 0.2-7.3 per 1000 surgeries[9] with 80% involving the pelvic ureters.
The majority of bladder ruptures are extraperitoneal (70%) and associated with blunt trauma in 51%-86% of cases[5]. The rate of intraperitoneal bladder rupture is much lower at 17%-39%. Patients with bladder rupture are frequently diagnosed with pelvic fracture ranging from 35%-90%, which denotes a strong association between these injuries[10]. Penetrating bladder injuries are less common (14%-49%) and caused by gunshot wounds in about 88% of injuries[11].
Urethral injuries are rare and represent 4% of genitourinary trauma. Urethral injury is about 5 times more likely to occur in males than females[12]. Blunt trauma especially straddle type injury is more frequently associated with the anterior urethra, mainly the bulbar portion. Perhaps urethral catheterization could be the commonest cause of anterior urethral injury, but data is lacking to establish the exact incidence. Posterior urethral injuries associated with pelvic injury are the most common non-iatrogenic urethral injury in developed and industrialized countries[13].
Traumatic injury to the external genitalia is found in about 27%-68% of all patients with genitourinary trauma[5]. Blunt trauma accounts for 85% of scrotal and testicular injuries, and nearly 40%-60% of penetrating genitourinary injuries involves the penis, scrotum and testes. The rate of penile trauma ranges from 10%-16% of genitourinary injuries with penile fracture being even more underreported[14].
The epidemiology of genitourinary trauma is not well established in most parts of Sub-Saharan Africa due to the lack of trauma registries. Most reports are extrapolated from hospital-based data and does not reflect the true incidence. The rate of traumatic injuries to the genitourinary tract is expected to rise in Africa with the increase in motor vehicle accidents and gunshot wounds from civil or domestic conflicts.
This review has provided insight on the epidemiology and management of genitourinary trauma in Sub-Saharan Africa. Moreover, the standard management guidelines of genitourinary trauma have been summarized to identify the gaps in the standard of care.
A thorough literature search of genitourinary trauma was conducted from 2000 to 2020 using the various search engines and databases (PubMed, Google Scholar, African Journal Online AJOL). The key search terms were “genitourinary trauma” and “traumatisme génito-urinaire.” Each keyword was appended with the following indexes: guideline, Sub-Saharan Africa, Africa, Senegal, Mali, Cote d’Ivoire, Ghana, Nigeria, Kenya, Liberia, Tanzania and Burkina Faso.
Duplicated articles on genitourinary trauma during the search were also excluded from the study. Other publications on genitourinary trauma from Europe, United States and Asia were excluded from the analysis and used for discussion in the background and main text. The American Urological Association guideline on urological trauma and the European Association of Urologists guideline on geni
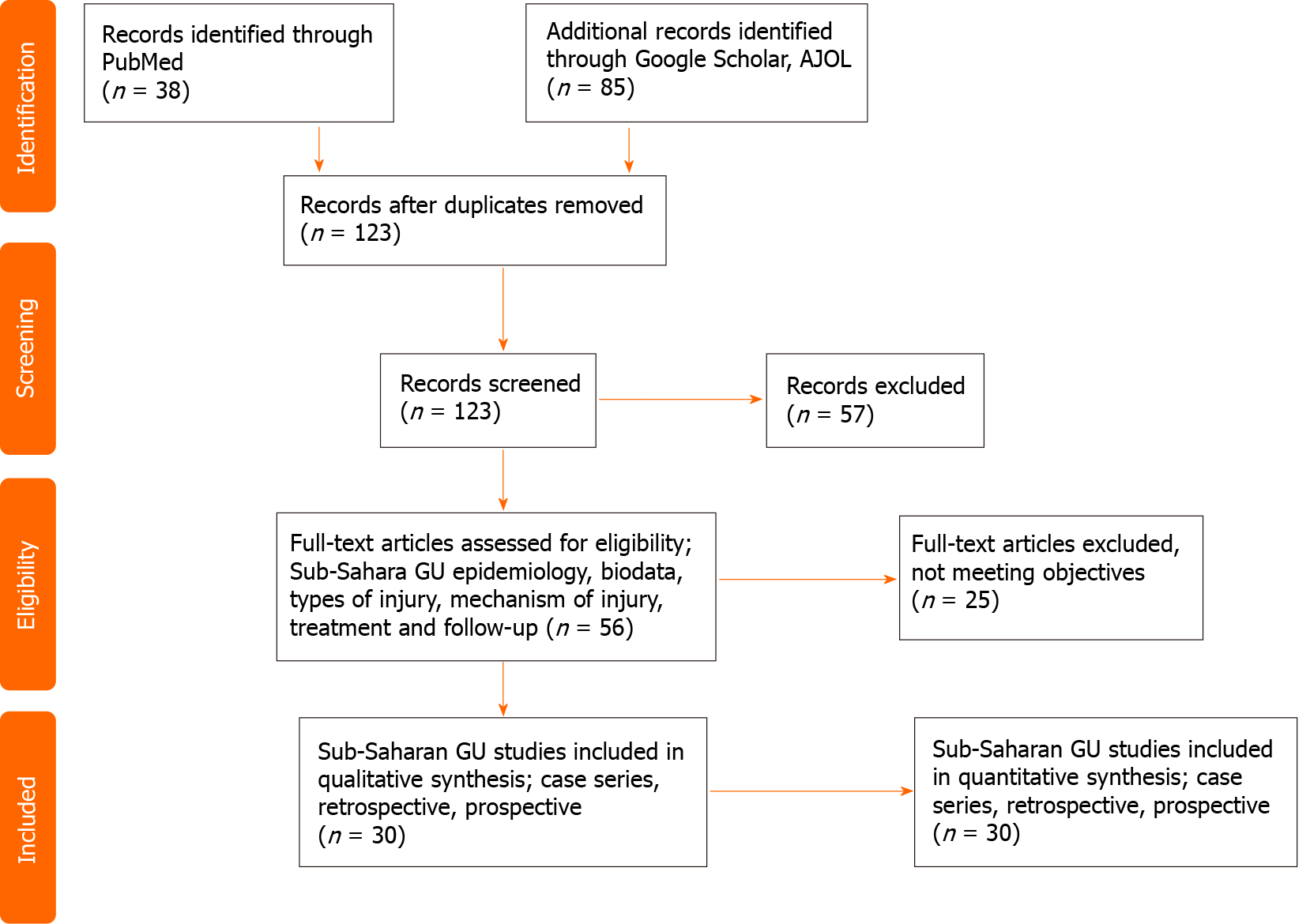
The title, abstract and full text of the retrieved literature were screened for eligibility. About 30 publications on genitourinary trauma from the Sub-Saharan region met the desired objective for synthesis. Published articles on genitourinary trauma, urological emergencies as well as urological complication from obstetric and gynecological surgeries were assessed for epidemiology, biodata, types of injury, mechanisms of injury, treatment and follow-up. A PRISMA flow chart is used to summarize the selection criteria as shown in Figure 1.
A pool analysis of eight retrospective studies (Figure 2) from Senegal[15-17], Burkina Faso[18], Benin[19,20], Guinea[21], Nigeria[22-24] and Ivory Coast[25,26] evaluating 21904 patients presenting with urological emergencies revealed that approximately 6.6% of cases were due to genitourinary trauma. Further analysis of genitourinary trauma in the Sub-Saharan region showed that the rate of urethral injury[16,19,21,27,28] was the highest 42.9% (22.2%-62.2%) followed by injury to the external genitalia (penis, scrotum, testes) [15,16,19-21,24-28] at a rate of 25.1% (8.8%-67.7%). The results showed the incidence rate bladder injury[16,19-22,24-28] to be 18.2% (3.8%-38.5%), ureteric injury[19,20,27] 16.6% (15.7%-18%) and kidney injury[16,19,20-22,24-28] 8.6% (1.9%-14.1%).
A pool analysis of six publications (Table 1) from the Sub-Saharan[29-34] region involving 98 patients with penile trauma showed that about 75.2% of penile trauma presented fracture of the tunica albuginea with or without concomitant urethral injury. The mean age was 36.5 years with range of 0.003-73 years. Other penile injuries included rupture of the penile dorsal vein[29], penile contusion[30], genital mutilation, post-circumcision injury and penile gunshot injury[32]. Patients presenting with genital mutilation were either self-inflicted or due to assault. In 2012, Orakwe et al[35] also reported three cases of genital mutilation caused by ritualistic attacks in Nigeria.
| Ref. | Country/Territory | No. of patients | Age range in yr | Mean age in yr | Penile injury | Causes of penile injury | Treatment | Complications |
| Sow et al[29] | Senegal | 23 | 19-47 | 32.4 | Fracture of tunica albuginea-82.6%; Fracture of tunica albuginea + partial urethral injury; Rupture of the penile dorsal vein | Sexual intercourse, masturbation, firearm, self-circumcision attempt | Evacuation of hematoma and repair of the albuginea | ED, coital penile pain, penile chordee |
| Paré et al[30] | Burkina | 6 | 30-43 | 38.3 | Fracture of tunica albuginea - 83.3%; Penile Contusion | Sexual intercourse | Evacuation of hematoma and repair of the albuginea | No ED |
| Odzébé et al[31] | Congo Brazzaville | 09 | 25-73 | 46.3 | Fracture of tunica albuginea | Sexual intercourse; Masturbation | Evacuation of hematoma and repair of the albuginea | ED; Penile chordee |
| Oranusi et al[32] | Nigeria | 23 | 0.003-43 | 28.9 | Penile fracture (34.8%) - (Sexual intercourse); Genital mutilation 26% (self-inflicted/assault); Post circumcision 13% (untrained nurses), Penile gunshot injury | Repair of albuginea, refashioning of residual penile stump, repair of albuginea | Not specified | |
| Omisanjo et al[33] | Nigeria | 15 | 23-56 | 35.2 | Penile fracture 100% + concomitant urethral injury 26.7% | Sexual intercourse 66.7%; Rolling over erect penis 20% Masturbation 13% | Evacuation of hematoma and repair of the albuginea | ED 6.7%; Penile chordee 13.3% |
| Barry et al[34] | Guinea | 22 | 22-51 | 37.8 | Penile fracture 100% | Sexual intercourse 59.1%; Masturbation 31.8%; Rolling over erect penis 9.1% | Evacuation of hematoma and repair of the albuginea | No ED |
The commonest cause of penile fracture was sexual intercourse[29-34]. Other causes of penile fracture were masturbation[29,31-34] and rolling over an erect penis[33,34].
The management approach to the penile fracture was evacuation of the hematoma and repair of the tunica albuginea[29-34]. Few studies from Senegal, Congo and Nigeria reported a complications such as erectile dysfunction and abnormal penile curvature after albuginea repair for penile fracture[29-31,33,34].
A retrospective study of 23 patients by Oranusi et al[32] showed that post circumcision injury was seen in 13% of patients with penile trauma most of which was performed by untrained nurses. Another study by Appiah et al[36] in Ghana reviewing 72 patients with circumcision related injuries showed that urethrocutaneous fistula was the commonest injury (77.8%) followed by glans amputation (6.9%). The majority of these cases were operated during the neonatal period (94.7%), mostly by nurse practitioners (77.8%).
A total of seven studies[37-43] were reviewed for urological complications of obstetric and gynecological operations involving 233 patients (Table 2). The mean age was 39.6 years with a range of 16-74 years. The ureters were the commonest urological organ injured (17.2%-87%)[37-43] followed by bladder injury (3.8%-28.6%)[37,39,41-43]. The ureters were frequently injured by either ligation, laceration or transection. The laterality of ureteric injury revealed left ureteric injury 34.1%, right ureteric injury 18.5% and bilateral ureteric injury 20.6%. Most of these injuries occurred following total abdominal hysterectomy 17.9% to 92.9% and to a lesser extent myomectomy, cesarean section and ovariectomy[37-43]. The distal ureters were the most commonly injured segment, as such a ureteroneocystostomy was performed more frequently (36.0%-81.3%). Other interventions included laceration repair, psoas hitch, Boari’s flap, nephroureterectomy in patient with right colonic tumor and nephrectomy for non-functioning kidney.
| Series | Country/territory | Patient population | Age range in yr | Mean age in yr | Urological injury | Causes of injury | Intervention |
| Papoola et al[37] | Nigeria | 11 | 28-65 | 43.8 | Ureteric injury (45.5%); Bladder injury (18.2%) | TAH-60%; Ovariectomy | UNC: 36%; Uretero-ureterostomy; Bladder repair; Catheter drainage |
| Kingsley et al[38] | Nigeria | 20 | N/A | 34.5 ± 3.8 | L. ureteric injury (50%); R. ureteric injury (21.4%); Bilateral (28.6%) | TAH-55%; Myomectomy, CS, excision of right colonic tumor | UNC: 67.8%; Psoas hitch, Boari’s flap, TUU, R. Nephroureterectomy |
| Ekeke et al[39] | Nigeria | 25/8270 | 24-62 | 38.4 | L. ureteric injury (37.5%); R. ureteric injury (33.3%); Bilateral (29.2%); Bladder injury (28%) | TAH-48%, Subtotal H-16%, CS:12%, ovariectomy, VVF repair. | Ureteric laceration repair- 40%, UNC: 44%, Boari’s flap, bladder repair |
| Mensah et al[40] | Ghana | 14 | 18-74 | N/A | Bilateral ureteral injury | TAH-92.9%; VVF repair-7.1% | Dialysis-36%; UNC, deligation, psoas hitch, TUU |
| Sebukoto et al[41] | Tanzania | 105/11219 | N/A | N/A | Ureteral injury 17.2%; R. ureter 6.7%; L. ureter 4.8%; Bilateral 5.7%; Bladder injury 3.8% | C-Section 34.3%; TAH- 17.1% | |
| Chianakwana et al[42] | Nigeria | 32 | N/A | N/A | Ureteric injury 87%; Bladder injury 9.4%; Urethral Injury 2.1% | TAH, Myomectomy | UNC 81.3%; Bladder repair; Tube ureterostomy |
| Obarisiagbon et al[43] | Nigeria | 16 | 16-50 | 41.5 | Left ureter 44%;Right ureter 12.5%; Bilateral 18.8%; Bladder injury 25% | TAH 75%; C-section 31% | UNC 68.8%; Bladder repair; Conservative; Nephrectomy |
To date, some urological or surgical institutions have formulated guideline statements for the management of urogenital trauma including the American Urological Association, European Association of Urologists, World Society of Emergency Surgery and the American Association for the Surgery of Trauma[1-3]. The contemporary management of genitourinary trauma in Sub-Saharan Africa is extrapolated from these guidelines. It is therefore essential that insight into the diagnostic and management algorithm of genitourinary trauma is available to all urologists in the region.
Patients with genitourinary injuries should be approached systematically like all other trauma patients. The hemodynamic status, the mechanism of injury and associated injuries must be fully assessed to guide decision making[3]. The presence of hematuria, flank pain and lower ribs fracture should raise the index of renal trauma. Male patients with pelvic fracture associated with blood at the urethral meatus and high riding prostate may denote an associated urethral injury.
The exact incidence of urological injury in the Sub-Saharan region remains vague due to the lack of reporting and availability of trauma registry. Nevertheless, trauma represent a significant proportion of disease burden in the region. A pool analysis of 21904 patients presenting with urological emergencies from Senegal[15-17], Burkina Faso[18], Benin[19,20], Guinea[21], Nigeria[22-24] and Ivory Coast[25,26] revealed that approximately 6.6% of cases were due to genitourinary trauma. This finding is however lower than the global estimate of genitourinary injury at 10%. A 5-year audit of 527 deaths at a teaching hospital in Nigeria showed that trauma was the commonest cause of mortality (41.8%), and urological causes accounted for 6% of mortality[44].
Adult and pediatric trauma patients presenting with gross or microscopic hematuria and decreasing systolic blood pressure require an enhanced intravenous contrast computed tomography (CT) scan with immediate and delayed images[1-3]. Imaging will also be required for patients with significant blunt force to the flank, rib fracture, rapid deceleration and penetrating injury to the abdomen, flank or lower chest.
In stable patients with grade I-III renal injury (Table 3), expectant management is indicated. These include intensive care admission, bed rest, serial hematocrit and blood transfusion. These interventions lower the rate of nephrectomies and preserves renal function.
| Grade | Type | Description |
| Grade (I) | Contusion | Gross or microscopic hematuria |
| Hematoma | Non-expanding subcapsular hematoma, parenchyma spared | |
| Grade (II) | Hematoma | Confined non-expanding perirenal hematoma |
| Laceration | < 1 cm parenchymal tear without urine extravasation | |
| Grade (III) | Laceration | > 1 cm parenchymal tear without urine leakage |
| Grade (IV) | Laceration | Parenchymal tear across the renal cortex, medulla and collecting system |
| Vascular | Injury to major branch of renal artery or vein with contained hemorrhage | |
| Grade (V) | Laceration | Kidney is completely shattered |
| Vascular | Devascularized kidney from renal hilum avulsion |
Patients who are hemodynamically unstable despite ongoing resuscitation suggest ongoing bleeding and will require immediate intervention. These patients can either benefit from surgery or angioembolization. The goal of surgery is to arrest further bleeding and repair the kidney if feasible. An on-table intravenous pyelogram is required to assess the function of the contralateral kidney as the possibility of nephre
In centers with interventional radiologists, minimally invasive treatment like angioembolization of bleeding segment vessels is possible in selected patients.
A follow-up CT scan should be performed in patients with deep renal lacerations (American Association for the Surgery of Trauma Grade IV-V) (Table 3) undergoing observation who present with fever, worsening flank pain, falling hematocrit and abdominal distension. The risk of urinoma and hemorrhage is high in grade IV-V injury; as such, the rate of intervention is likely after 48 h[1]. Urinary drainage can be done using ureteral stent along with a percutaneous urinoma drain or percutaneous nephrostomy.
The rate of renal trauma in the Sub-Saharan Africa was approximately 8.6% with a range of 1.9%-14.1% from the review. A prospective study from Ofoha et al[28] in Nigeria evaluating 104 patients with genitourinary trauma showed that renal trauma accounted for 13.5% of urogenital trauma, and grade V renal injury was the comm
In polytraumatized patients especially with visceral injuries, vascular injuries and complex pelvis or vertebral fractures, ureteral injury should be suspected[2]. The absence of hematuria does not rule out injury to the ureters. Therefore, stable patients not requiring exploratory laparotomy should undergo an intravenous contrast enhanced abdomino-pelvic CT scan with 10-min delayed images to assess for ureteral injury[1-3]. Contrast extravasation, absence of contrast distal to the suspected zone of injury and ipsilateral hydronephrosis are suggestive of ureteral injury.
Patients who proceed to laparotomy without preoperative imaging should have their ureters mobilized and inspected. Intra-ureteral dye using methylene blue can aid detection of the injured segment. Ureteral laceration discovered during laparotomy should be repaired in stable patients. Contused ureters should be managed with ureteral stenting or resection and primary repair in selected patients, particularly gunshot wounds[1,2]. Percutaneous nephrostomy and distal ligation of the injured ureter is a viable alternative following inability to stent especially for damage control in polytraumatized patients. Definitive repair is delayed until the patient is hemodynamically stable.
Females with ureterovaginal fistula from gynecological surgery or pelvic trauma can be initially managed with ureteral stent with a reported success rate of 64%[1,2]. Nevertheless, a ureteral reimplantation is necessary in the presence of stent failure. Ureteral reimplantation can be performed along with a Boari’s flap, psoas hitch or a transureteroureterostomy with good outcome.
Ureteral injuries occurring proximal to the iliac vessels are best repaired using a tension free spatulated end to end ureteral anastomosis over a ureteral stent. If primary repair is not feasible, a ureteroneocystostomy is another option. A simple ureteroneocystostomy is a viable procedure for ureteral injury distal to the iliac vessels[1-3]. To allow tension free repair, other maneuvers to mobilize the bladder should be performed when necessary. When the ureter is injured during an endoscopic proce
After analysis of the seven studies in the review, findings showed the ureters are commonly injured following gynecological procedures especially abdominal hysterectomy at a rate of 17.9% to 92.9%[37-43]. Retrospective analyses by Kingsley et al[38] and Ekeke et al[39] evaluating ureteral injuries after gynecological surgeries in Nigeria revealed that leakage of fluid per vagina or surgical site was the commonest presen
Gross hematuria is a common sign of bladder injury. Patients presenting with gross hematuria and pelvic fracture is an absolute indication for bladder imaging using retrograde cystography to evaluate the presence of bladder injury[1-3]. Suprapubic pain, inability to void or low urine output are other indicators of a potential bladder rupture. Plain film cystography has similar sensitivity to CT cystography for assessing bladder rupture.
In the setting of blunt or penetrating trauma, intraperitoneal rupture must be repaired because it is unlikely to heal with catheter drainage alone[1-3]. Bacterial translocation leading to sepsis and peritonitis is the end result if intraperitoneal bladder rupture is left untreated. A follow-up cystography is required to assess for healing in complex repair.
Uncomplicated extraperitoneal rupture are drained using a urethral catheter for 2-3 wk to allow bladder healing. A follow-up cystography is essential to assess for bladder healing. Complicated extraperitoneal bladder injury with bony spicules, concurrent rectal/vaginal injury or bladder neck injury are best managed with primary repair during the repair of other injuries[1,2].
A quantitative analysis of 13 studies evaluating genitourinary trauma[16,19-22,24-28] in the Sub-Saharan region showed the incidence rate of bladder injury to be 18.2% (3.8%-38.5%). Another report from the Sub-Saharan region revealed blunt trauma from motor vehicle accidents was the most frequent mechanism of injury causing more intraperitoneal bladder rupture (26.1%) than extraperitoneal bladder rupture (21.7%)[22]. The presence of hematuria, abdominal distension, cystography and/or cystoscopy were used to diagnose bladder injury in the study[22].
A prospective study by Ofoha et al[28] in evaluating 104 patients with genitourinary trauma in Nigeria showed that 24% of patient had bladder injury. Intraperitoneal bladder rupture was more common at 64% compared to extraperitoneal rupture at 24%. The fact that gunshot and motor vehicle accident were the commonest mechanism of injury in this study explains the predominance of intraperitoneal rupture.
Trauma patients presenting with blood at the urethral meatus should be offered prompt retrograde urethrogram to assess for partial or complete urethral disruption[1-3]. Blind catherization should be avoided in this setting or limited to single attempt by an experienced practitioner. In the presence of pelvic fracture urethral injury, a suprapubic catheter should be placed to establish proper drainage[1-3]. A good communication should be maintained between the urologist and orthopedics desiring open reduction and internal fixation to reduce the risk of plate infection from adjacent suprapubic tube. In patients who are hemodynamically stable, an endoscopic realignment can be attempted. However, prolonged attempts at realignment in the emergency setting only aggravate the risk of developing urethral stricture. Pelvic fracture urethral injury is associate with a high rate of urethral stricture, erectile dysfunction and urinary incontinence[1,2]. Therefore, these patients have to be followed over a year as most will require urethroplasty or endoscopic treatment with direct vision urethrotomy. Stable patients presenting with uncomplicated penetrating injury of the anterior urethra can undergo spatulated primary urethral repair. In the setting of extensive tissue destruction, a delayed repair should be offered. Patients with blunt trauma to the bulbar urethral from straddle injury should receive suprapubic catheter for urinary diversion. The rate of subsequent urethral stricture is high after straddle injury. Therefore, close monitoring using cystoscopy, uroflowmetry and retrograde urethrogram is essential for management[1-3].
The analyzed data from this review[16,19,21,27,28] showed that urethral trauma was the most frequent injury of the genitourinary system in the Sub-Saharan region at a rate of 42.9% (22.2%-62.2%). A report from a teaching hospital in Cotonou Benin assessing 32 patients with genitourinary trauma by Ouattara et al[20] showed that urethral rupture accounted for 50% of external genital injury. As such, acute urinary retention (42.1%) and urethrorrhagia (13.2%) were common presentations. Data from a teaching hospital in Nigeria assessing 104 patients with genitourinary trauma reported a high rate of urethral injury with 92% of patients receiving suprapubic urinary diversion and deferred urethroplasty[28].
Penile fracture should be suspected when a patient presents with a history of penile snapping, swelling and ecchymosis during a sexual intercourse/manipulation followed by immediate detumescence[1-3]. Penile fracture can be diagnosed by history and physical exam alone. However, in equivocal cases, ultrasound can be done to evaluate penile fracture, which is cheaper and readily available. Magnetic resonance imaging should be reserved for cases with ambiguous sonographic findings[1,2]. Patients with penile fracture, blood at the urethral meatus and inability to void should be assessed for concomitant urethral injury using either urethroscopy or retrograde urethrogram. All cases of penile fracture should be repaired at presentation. The injured corpus cavernous should be properly exposed, and the tunica is repaired using absorbable sutures[1]. Early repair is associated with better outcome.
Patients presenting with scrotal swelling, scrotal ecchymosis and inability to identify the testicular contour on physical exam following a blunt or penetrating trauma should undergo scrotal exploration. Moderate debridement of devitalized tissues and tunica closure or orchidectomy for non-salvageable testes are options based on intraoperative findings[1,2]. Reconstructive techniques for extensive genital wounds include advancement flaps, pedicle flaps or skin graft.
Individuals with traumatic penile amputation will require urgent penile replan
Genital injuries often leave patients with scarred or poorly functional genitalia. The social and emotional intimacy of these patients are too frequently deterred by these injuries. It is always prudent to involve psychological and reproductive counseling for affected individuals.
The rate of external genital injury (penis, scrotum, testes) in the Sub-Saharan region[15,16,19-21,24-28] was also found to be relatively high at a rate of 25.1% (8.8%-67.7%). Data from a pool analysis of penile trauma in Sub-Saharan Africa[29-34] showed that about 75.2% of penile trauma were penile fracture (fracture of the tunica albuginea) with or without concomitant urethral injury. Most of these injuries had optimal outcomes with early repair. The review has also shown that post-circumcision injury is currently rising especially when these procedures are being performed in the neonatal period by untrained nurses. Circumcision is a delicate procedure that is mistaken by most health practitioners as minor. The anatomy of the genitals in neonates is delicate and as such should be handled by trained health practitioners preferably urologists. The lack of specialists in most Sub-Saharan settings compels mid-level health workers to assume major operative roles.
The management of genitourinary injury is challenging. The choice of conservative or operative management for genitourinary trauma is crucial for optimal outcome especially in renal injury. Prompt repair of external genital injuries can produce satisfactory results. However, patients should be counseled about the possibility of sexual dysfunction. Genitourinary injury in Sub-Saharan Africa is underreported. The presence of more trauma registries, trained urologists and trauma facilities can improve the overall standard of care and provide data for research and development in the field.
The research tends to highlight the burden of genitourinary injury in the Sub-Saharan region and the differences in the injury pattern from developed nations.
Due to paucity of information and publication on urological injuries in the Sub-Saharan nations, it was essential to review and synthesize the available data in the region.
The manuscript has provided insight into management challenges of genitourinary trauma in developing nations of Africa and summarized the available international guidelines to identify progress and gaps in the region.
This research is a systematic review in accordance with the PRISMA guideline.
Amongst urological emergencies, genitourinary trauma accounted for 6.6% of cases. Urethral injury and injury to the external genitalia accounted for most of the trauma burden as compared to renal injury in developed nations.
A trauma registry is necessary to promote research and improvement in trauma care. Prompt repair of injuries to the external genitalia has shown satisfactory results.
The manuscript has highlighted the paucity of data on genitourinary trauma in Sub-Saharan Africa. The research intends to project the need for investment in trauma care and to establish trauma registries around the continent.
Special thanks to the Department of Surgery of the John F. Kennedy Medical Center, Monrovia, Liberia.
Manuscript source: Invited manuscript
Specialty type: Urology and nephrology
Country/Territory of origin: Liberia
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Wang H S-Editor: Wu YXJ L-Editor: Filipodia P-Editor: Wu RR
| 1. | Kitrey ND, Djakovic N, Gonsalves M, Kuehhas FE, Lumen N, Serafetinidis E, Sharma DM, Summerton DJ, Veskimäe E. EAU Guidelines on Urological trauma. European Association of Urology, 2018. [cited 1 February 2021]. Available from: https://uroweb.org/wp-content/uploads/EAU-Guidelines-on-Urological-Trauma-2018-large-text.pdf. |
| 2. | Morey AF, Brandes S, Dugi DD 3rd, Armstrong JH, Breyer BN, Broghammer JA, Erickson BA, Holzbeierlein J, Hudak SJ, Pruitt JH, Reston JT, Santucci RA, Smith TG 3rd, Wessells H; American Urological Assocation. Urotrauma: AUA guideline. J Urol. 2014;192:327-335. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 291] [Cited by in RCA: 311] [Article Influence: 28.3] [Reference Citation Analysis (0)] |
| 3. | Coccolini F, Moore EE, Kluger Y, Biffl W, Leppaniemi A, Matsumura Y, Kim F, Peitzman AB, Fraga GP, Sartelli M, Ansaloni L, Augustin G, Kirkpatrick A, Abu-Zidan F, Wani I, Weber D, Pikoulis E, Larrea M, Arvieux C, Manchev V, Reva V, Coimbra R, Khokha V, Mefire AC, Ordonez C, Chiarugi M, Machado F, Sakakushev B, Matsumoto J, Maier R, di Carlo I, Catena F; WSES-AAST Expert Panel. Kidney and uro-trauma: WSES-AAST guidelines. World J Emerg Surg. 2019;14:54. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 152] [Cited by in RCA: 114] [Article Influence: 19.0] [Reference Citation Analysis (0)] |
| 4. | James SL, Castle CD, Dingels ZV, Fox JT, Hamilton EB, Liu Z, S Roberts NL, Sylte DO, Henry NJ, LeGrand KE, Abdelalim A, Abdoli A, Abdollahpour I, Abdulkader RS, Abedi A, Abosetugn AE, Abushouk AI, Adebayo OM, Agudelo-Botero M, Ahmad T, Ahmed R, Ahmed MB, Eddine Aichour MT, Alahdab F, Alamene GM, Alanezi FM, Alebel A, Alema NM, Alghnam SA, Al-Hajj S, Ali BA, Ali S, Alikhani M, Alinia C, Alipour V, Aljunid SM, Almasi-Hashiani A, Almasri NA, Altirkawi K, Abdeldayem Amer YS, Amini S, Loreche Amit AM, Andrei CL, Ansari-Moghaddam A, T Antonio CA, Yaw Appiah SC, Arabloo J, Arab-Zozani M, Arefi Z, Aremu O, Ariani F, Arora A, Asaad M, Asghari B, Awoke N, Ayala Quintanilla BP, Ayano G, Ayanore MA, Azari S, Azarian G, Badawi A, Badiye AD, Bagli E, Baig AA, Bairwa M, Bakhtiari A, Balachandran A, Banach M, Banerjee SK, Banik PC, Banstola A, Barker-Collo SL, Bärnighausen TW, Barrero LH, Barzegar A, Bayati M, Baye BA, Bedi N, Behzadifar M, Bekuma TT, Belete H, Benjet C, Bennett DA, Bensenor IM, Berhe K, Bhardwaj P, Bhat AG, Bhattacharyya K, Bibi S, Bijani A, Bin Sayeed MS, Borges G, Borzì AM, Boufous S, Brazinova A, Briko NI, Budhathoki SS, Car J, Cárdenas R, Carvalho F, Castaldelli-Maia JM, Castañeda-Orjuela CA, Castelpietra G, Catalá-López F, Cerin E, Chandan JS, Chanie WF, Chattu SK, Chattu VK, Chatziralli I, Chaudhary N, Cho DY, Kabir Chowdhury MA, Chu DT, Colquhoun SM, Constantin MM, Costa VM, Damiani G, Daryani A, Dávila-Cervantes CA, Demeke FM, Demis AB, Demoz GT, Demsie DG, Derakhshani A, Deribe K, Desai R, Nasab MD, da Silva DD, Dibaji Forooshani ZS, Doyle KE, Driscoll TR, Dubljanin E, Adema BD, Eagan AW, Eftekhari A, Ehsani-Chimeh E, Sayed Zaki ME, Elemineh DA, El-Jaafary SI, El-Khatib Z, Ellingsen CL, Emamian MH, Endalew DA, Eskandarieh S, Faris PS, Faro A, Farzadfar F, Fatahi Y, Fekadu W, Ferede TY, Fereshtehnejad SM, Fernandes E, Ferrara P, Feyissa GT, Filip I, Fischer F, Folayan MO, Foroutan M, Francis JM, Franklin RC, Fukumoto T, Geberemariyam BS, Gebre AK, Gebremedhin KB, Gebremeskel GG, Gebremichael B, Gedefaw GA, Geta B, Ghafourifard M, Ghamari F, Ghashghaee A, Gholamian A, Gill TK, Goulart AC, Grada A, Grivna M, Mohialdeen Gubari MI, Guimarães RA, Guo Y, Gupta G, Haagsma JA, Hafezi-Nejad N, Bidgoli HH, Hall BJ, Hamadeh RR, Hamidi S, Haro JM, Hasan MM, Hasanzadeh A, Hassanipour S, Hassankhani H, Hassen HY, Havmoeller R, Hayat K, Hendrie D, Heydarpour F, Híjar M, Ho HC, Hoang CL, Hole MK, Holla R, Hossain N, Hosseinzadeh M, Hostiuc S, Hu G, Ibitoye SE, Ilesanmi OS, Ilic I, Ilic MD, Inbaraj LR, Indriasih E, Naghibi Irvani SS, Shariful Islam SM, Islam MM, Ivers RQ, Jacobsen KH, Jahani MA, Jahanmehr N, Jakovljevic M, Jalilian F, Jayaraman S, Jayatilleke AU, Jha RP, John-Akinola YO, Jonas JB, Joseph N, Joukar F, Jozwiak JJ, Jungari SB, Jürisson M, Kabir A, Kadel R, Kahsay A, Kalankesh LR, Kalhor R, Kamil TA, Kanchan T, Kapoor N, Karami M, Kasaeian A, Kassaye HG, Kavetskyy T, Kebede HK, Keiyoro PN, Kelbore AG, Kelkay B, Khader YS, Khafaie MA, Khalid N, Khalil IA, Khalilov R, Khammarnia M, Khan EA, Khan M, Khanna T, Khazaie H, Shadmani FK, Khundkar R, Kiirithio DN, Kim YE, Kim D, Kim YJ, Kisa A, Kisa S, Komaki H, M Kondlahalli SK, Korshunov VA, Koyanagi A, G Kraemer MU, Krishan K, Bicer BK, Kugbey N, Kumar V, Kumar N, Kumar GA, Kumar M, Kumaresh G, Kurmi OP, Kuti O, Vecchia C, Lami FH, Lamichhane P, Lang JJ, Lansingh VC, Laryea DO, Lasrado S, Latifi A, Lauriola P, Leasher JL, Huey Lee SW, Lenjebo TL, Levi M, Li S, Linn S, Liu X, Lopez AD, Lotufo PA, Lunevicius R, Lyons RA, Madadin M, El Razek MMA, Mahotra NB, Majdan M, Majeed A, Malagon-Rojas JN, Maled V, Malekzadeh R, Malta DC, Manafi N, Manafi A, Manda AL, Manjunatha N, Mansour-Ghanaei F, Mansouri B, Mansournia MA, Maravilla JC, March LM, Mason-Jones AJ, Masoumi SZ, Massenburg BB, Maulik PK, Meles GG, Melese A, Melketsedik ZA, N Memiah PT, Mendoza W, Menezes RG, Mengesha MB, Mengesha MM, Meretoja TJ, Meretoja A, Merie HE, Mestrovic T, Miazgowski B, Miazgowski T, Miller TR, Mini GK, Mirica A, Mirrakhimov EM, Mirzaei-Alavijeh M, Mithra P, Moazen B, Moghadaszadeh M, Mohamadi E, Mohammad Y, Mohammad KA, Darwesh AM, Gholi Mezerji NM, Mohammadian-Hafshejani A, Mohammadoo-Khorasani M, Mohammadpourhodki R, Mohammed S, Mohammed JA, Mohebi F, Molokhia M, Monasta L, Moodley Y, Moosazadeh M, Moradi M, Moradi G, Moradi-Lakeh M, Moradpour F, Morawska L, Velásquez IM, Morisaki N, Morrison SD, Mossie TB, Muluneh AG, Murthy S, Musa KI, Mustafa G, Nabhan AF, Nagarajan AJ, Naik G, Naimzada MD, Najafi F, Nangia V, Nascimento BR, Naserbakht M, Nayak V, Ndwandwe DE, Negoi I, Ngunjiri JW, Nguyen CT, Thi Nguyen HL, Nikbakhsh R, Anggraini Ningrum DN, Nnaji CA, Nyasulu PS, Ogbo FA, Oghenetega OB, Oh IH, Okunga EW, Olagunju AT, Olagunju TO, Bali AO, Onwujekwe OE, Asante KO, Orpana HM, Ota E, Otstavnov N, Otstavnov SS, A MP, Padubidri JR, Pakhale S, Pakshir K, Panda-Jonas S, Park EK, Patel SK, Pathak A, Pati S, Patton GC, Paulos K, Peden AE, Filipino Pepito VC, Pereira J, Pham HQ, Phillips MR, Pinheiro M, Polibin RV, Polinder S, Poustchi H, Prakash S, Angga Pribadi DR, Puri P, Syed ZQ, Rabiee M, Rabiee N, Radfar A, Rafay A, Rafiee A, Rafiei A, Rahim F, Rahimi S, Rahimi-Movaghar V, Rahman MA, Rajabpour-Sanati A, Rajati F, Rakovac I, Ranganathan K, Rao SJ, Rashedi V, Rastogi P, Rathi P, Rawaf S, Rawal L, Rawassizadeh R, Renjith V, N Renzaho AM, Resnikoff S, Rezapour A, Ribeiro AI, Rickard J, Rios González CM, Ronfani L, Roshandel G, Saad AM, Sabde YD, Sabour S, Saddik B, Safari S, Safari-Faramani R, Safarpour H, Safdarian M, Sajadi SM, Salamati P, Salehi F, Zahabi SS, Rashad Salem MR, Salem H, Salman O, Salz I, Samy AM, Sanabria J, Riera LS, Santric Milicevic MM, Sarker AR, Sarveazad A, Sathian B, Sawhney M, Sawyer SM, Saxena S, Sayyah M, Schwebel DC, Seedat S, Senthilkumaran S, Sepanlou SG, Seyedmousavi S, Sha F, Shaahmadi F, Shahabi S, Shaikh MA, Shams-Beyranvand M, Shamsizadeh M, Sharif-Alhoseini M, Sharifi H, Sheikh A, Shigematsu M, Shin JI, Shiri R, Siabani S, Sigfusdottir ID, Singh PK, Singh JA, Sinha DN, Smarandache CG, R Smith EU, Soheili A, Soleymani B, Soltanian AR, Soriano JB, Sorrie MB, Soyiri IN, Stein DJ, Stokes MA, Sufiyan MB, Rasul Suleria HA, Sykes BL, Tabarés-Seisdedos R, Tabb KM, Taddele BW, Tadesse DB, Tamiru AT, Tarigan IU, Tefera YM, Tehrani-Banihashemi A, Tekle MG, Tekulu GH, Tesema AK, Tesfay BE, Thapar R, Tilahune AB, Tlaye KG, Tohidinik HR, Topor-Madry R, Tran BX, Tran KB, Tripathy JP, Tsai AC, Car LT, Ullah S, Ullah I, Umar M, Unnikrishnan B, Upadhyay E, Uthman OA, Valdez PR, Vasankari TJ, Venketasubramanian N, Violante FS, Vlassov V, Waheed Y, Weldesamuel GT, Werdecker A, Wiangkham T, Wolde HF, Woldeyes DH, Wondafrash DZ, Wondmeneh TG, Wondmieneh AB, Wu AM, Yadav R, Yadollahpour A, Yano Y, Yaya S, Yazdi-Feyzabadi V, Yip P, Yisma E, Yonemoto N, Yoon SJ, Youm Y, Younis MZ, Yousefi Z, Yu Y, Yu C, Yusefzadeh H, Moghadam TZ, Zaidi Z, Zaman SB, Zamani M, Zamanian M, Zandian H, Zarei A, Zare F, Zhang ZJ, Zhang Y, Zodpey S, Dandona L, Dandona R, Degenhardt L, Dharmaratne SD, Hay SI, Mokdad AH, Reiner RC Jr, Sartorius B, Vos T. Global injury morbidity and mortality from 1990 to 2017: results from the Global Burden of Disease Study 2017. Inj Prev. 2020;26:i96-i114. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 111] [Cited by in RCA: 103] [Article Influence: 20.6] [Reference Citation Analysis (0)] |
| 5. | McGeady JB, Breyer BN. Current epidemiology of genitourinary trauma. Urol Clin North Am. 2013;40:323-334. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 58] [Cited by in RCA: 59] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 6. | Paparel P, N'Diaye A, Laumon B, Caillot JL, Perrin P, Ruffion A. The epidemiology of trauma of the genitourinary system after traffic accidents: analysis of a register of over 43,000 victims. BJU Int. 2006;97:338-341. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 59] [Cited by in RCA: 50] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 7. | Siram SM, Gerald SZ, Greene WR, Hughes K, Oyetunji TA, Chrouser K, Cornwell EE 3rd, Chang DC. Ureteral trauma: patterns and mechanisms of injury of an uncommon condition. Am J Surg. 2010;199:566-570. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 59] [Cited by in RCA: 60] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 8. | Pereira BM, Ogilvie MP, Gomez-Rodriguez JC, Ryan ML, Peña D, Marttos AC, Pizano LR, McKenney MG. A review of ureteral injuries after external trauma. Scand J Trauma Resusc Emerg Med. 2010;18:6. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 91] [Cited by in RCA: 58] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 9. | Gilmour DT, Das S, Flowerdew G. Rates of urinary tract injury from gynecologic surgery and the role of intraoperative cystoscopy. Obstet Gynecol. 2006;107:1366-1372. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 140] [Cited by in RCA: 120] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 10. | Deibert CM, Spencer BA. The association between operative repair of bladder injury and improved survival: results from the National Trauma Data Bank. J Urol. 2011;186:151-155. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 35] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 11. | Pereira BM, de Campos CC, Calderan TR, Reis LO, Fraga GP. Bladder injuries after external trauma: 20 years experience report in a population-based cross-sectional view. World J Urol. 2013;31:913-917. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 67] [Cited by in RCA: 54] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 12. | Bariol SV, Stewart GD, Smith RD, McKeown DW, Tolley DA. An analysis of urinary tract trauma in Scotland: imnpact on management and resource needs. Surgeon. 2005;3:27-30. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 20] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 13. | Mundy AR, Andrich DE. Urethral trauma. Part I: introduction, history, anatomy, pathology, assessment and emergency management. BJU Int. 2011;108:310-327. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 44] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 14. | Cerwinka WH, Block NL. Civilian gunshot injuries of the penis: the Miami experience. Urology. 2009;73:877-880. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 22] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 15. | Diabaté I, Ouédraogo B, Thiam M. [Acute scrotal swellings at Louga Regional Hospital, Senegal: epidemiologic, etiologic and therapeutic aspects]. Pan Afr Med J. 2016;24:214. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 16. | Fall B, Diao B, Fall PA, Diallo Y, Sow Y, Ondongo AA, Diagana M, Ndoye AK, Ba M, Diagne BA. [Urological emergencies at the Dakar university teaching hospital: epidemiological, clinical and therapeutic features]. Prog Urol. 2008;18:650-653. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 26] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 17. | Diabaté I, Ondo CZ, Sow I, Ba A, MBoup C. Les urgences urologiques au centre hospitalier de Louga, Sénégal: aspects épidémiologiques et évaluation de la prise en charge. Afr J Urol. 2015;21:181-186. [RCA] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 18. | Traore MT, Yameogo CA, Kabore M, Ouedraogo S. Epidemiology of Urological Emergencies at the Regional University Hospital Center of Ouahigouya, Burkina Faso. Open J Urol. 2020;10:177-183. [DOI] [Full Text] |
| 19. | Dejinnin Avakoudjo JG, Natchagande G, Soumanou FK, Oliyide AR, Yevi MI. Genitourinary Emergencies at University Hospital in Cotonou: About 437 Patients. Med Sur Urol. 2018;7:1-5. [DOI] [Full Text] |
| 20. | Ouattara A, Avakoudjo JG, Hounnasso P, Ciss D, Hodonou F, Gandaho I. Les urgences urologiques traumatiques au CHNU-HKM de Cotonou: aspects épidémiologiques, diagnostiques et thérapeutiques. Médecine d’Afrique Noire. 2013;60:396-401. [RCA] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 19] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 21. | Bobo Diallo A, Bah I, Diallo TM, Bah OR, Amougou B, Bah MD, Guirassy S, Bobo Diallo M. [The profile urological emergencies at the Conakry University Teaching Hospital, Guinea]. Prog Urol. 2010;20:214-218. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 15] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 22. | Salako AA, Adisa AO, Eziyi AK, Banjo OO, Badmus TA. Traumatic urologic injuries in Ile-Ife, Nigeria. J Emerg Trauma Shock. 2010;3:311-313. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 23. | Eke N, Sapira MK, Echem RC. Spectrum of urological procedures in University of Port Harcourt Teaching Hospital, Port Harcourt, Nigeria. Niger J Clin Pract. 2007;10:74-78. [PubMed] |
| 24. | Osuigwe AN, Ekwunife CN. Paediatric day-case surgery at NAUTH, Nnewi, Nigeria. Trop Doct. 2004;34:41-42. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.0] [Reference Citation Analysis (0)] |
| 25. | Dekou A, Konan PG, Kouame B. Les traumatismes de l’appareil génito-urinaire: Aspects épidémiologiques et lésionnels. Afr J Urol. 2008;14:105-113. [RCA] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 26. | Djè K, Yao B, Sanou B, Kokoua A, Gnananzan KG. Genitourinary complications of pelvic trauma Les complications uro-génitales des traumatismes du bassin: a propos de 41 cas. Afr J Urol. 2006;12:37-43. [RCA] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 27. | Ekeke ON, Anyadike CC. Changing Pattern of Genitourinary Injuries in the Niger Delta Region of Nigeria. J Advances Med Med Research. 2018;25:1-10. [DOI] [Full Text] |
| 28. | Ofoha CG, Shu'aibu SI, Onowa VE, Galam ZZ. Contemporary management of genitourinary injuries in a tertiary trauma centre in Nigeria. Inter J Research Med Sci. 2018;6:1134-1138. [DOI] [Full Text] |
| 29. | Sow Y, Fall PA, Diao B, Fall B, Ndoye AK, Diagne BA. Les traumatismes de la verge: à propos de 23 cas. Andrologie. 2008;18:210-215. [DOI] [Full Text] |
| 30. | Paré AK, Ouattara A, Botcho G, Kirakoya B, Kaboré FA, Bako A, Yé D, Bayané D, Konaté M, Kambou T. [Penile fracture: about six cases observed at the Souro Sanou University Hospital of Bobo-Dioulasso, Burkina Faso]. Pan Afr Med J. 2019;33:257. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 31. | Odzébé AW, Mouss RB, Opara AS, Damba JJ, Ondongo AM, Mouzenzo A, Bouya PA. Penile Fracture at the Department of Urology and Andrology, University Hospital, Brazzaville. Open J Urol. 2019;9:195-200. [DOI] [Full Text] |
| 32. | Oranusi CK, Nwofor A. Traumatic penile injuries: Mechanisms and problems of treatment in a tertiary institution in Nigeria. Niger J Clin Pract. 2014;17:763-766. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 33. | Omisanjo OA, Bioku MJ, Ikuerowo SO, Sule GA, Esho JO. A prospective analysis of the presentation and management of penile fracture at the Lagos State University Teaching Hospital (LASUTH), Ikeja, Lagos, Nigeria. Afr J Urol. 2015;21:52-56. [RCA] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 34. | Barry Mi, Kanté D, Diallo T. Les diverticules de la vessie au service d'urologie du CHU Ignace Deen de Conakry. Étude rétrospective de 28 cas. Annales d'Urologie. 2001;35:111-116. [RCA] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 35. | Orakwe JC, Undie CU. Male genital injuries caused by ritual attacks in Nigeria: problems of management. Afr J Urol. 2012;18:75-77. [RCA] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 36. | Appiah KA, Gyasi-Sarpong CK, Azorliade R, Aboah K, Laryea DO, Otu-Boateng K, Baah-Nyamekye K, Maison PO, Arthur D, Antwi IO, Frimpong-Twumasi B, Yenli EM, Togbe SK, Amoah G. Circumcision-related tragedies seen in children at the Komfo Anokye Teaching Hospital, Kumasi, Ghana. BMC Urol. 2016;16:65. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 10] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 37. | Popoola AA, Ezeoke GG, Olarinoye A. Urological complications from obstetrics & gynaecological procedures in ilorin, Nigeria - case series. J West Afr Coll Surg. 2013;3:99-109. [PubMed] |
| 38. | Kingsley OC. Pattern of iatrogenic ureteral injuries in a tertiary health center in Nigeria. Trop J Med Research. 2016;19:47-51. [RCA] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 39. | Ekeke ON, Amusan EO, Eke N. Urological Complications of Obstetrics and Gynaecology Surgeries in a Developing Country. J Urol Nephrol. 2015;2:1-6. [DOI] [Full Text] |
| 40. | Mensah J, Klufio G, Ahiaku F, Osafo C, Gepi-Attee S. Delayed recognition of bilateral ureteral injury after gyneacological surgery. Ghana Med J. 2008;42:133-136. [PubMed] |
| 41. | Sebukoto HR, Semwaga E, Rugakingila RA. Urological injuries following obstetrical and gynecological surgeries. East Cen Afr J Surg. 2016;21:148-155. [DOI] [Full Text] |
| 42. | Chianakwana GU, Okafor PI, Ikechebelu JI, Mbonu OO. Urological injuries following gynecological operations--our experience in a teaching hospital in Nigeria. West Afr J Med. 2006;25:153-156. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 43. | Obarisiagbon EO, Olagbuji BN, Onuora VC, Oguike TC, Ande AB. Iatrogenic urological injuries complicating obstetric and gynaecological procedures. Singapore Med J. 2011;52:738-741. [PubMed] |
| 44. | Ekeke ON, Okonta KE, Igwe PO. Surgical inpatient mortality in a Nigerian Tertiary Hospital. Niger J Clin Pract. 2016;19:308-312. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 9] [Article Influence: 1.3] [Reference Citation Analysis (0)] |