Published online Nov 9, 2021. doi: 10.5492/wjccm.v10.i6.345
Peer-review started: June 28, 2021
First decision: July 29, 2021
Revised: August 9, 2021
Accepted: October 27, 2021
Article in press: October 27, 2021
Published online: November 9, 2021
Processing time: 129 Days and 17.9 Hours
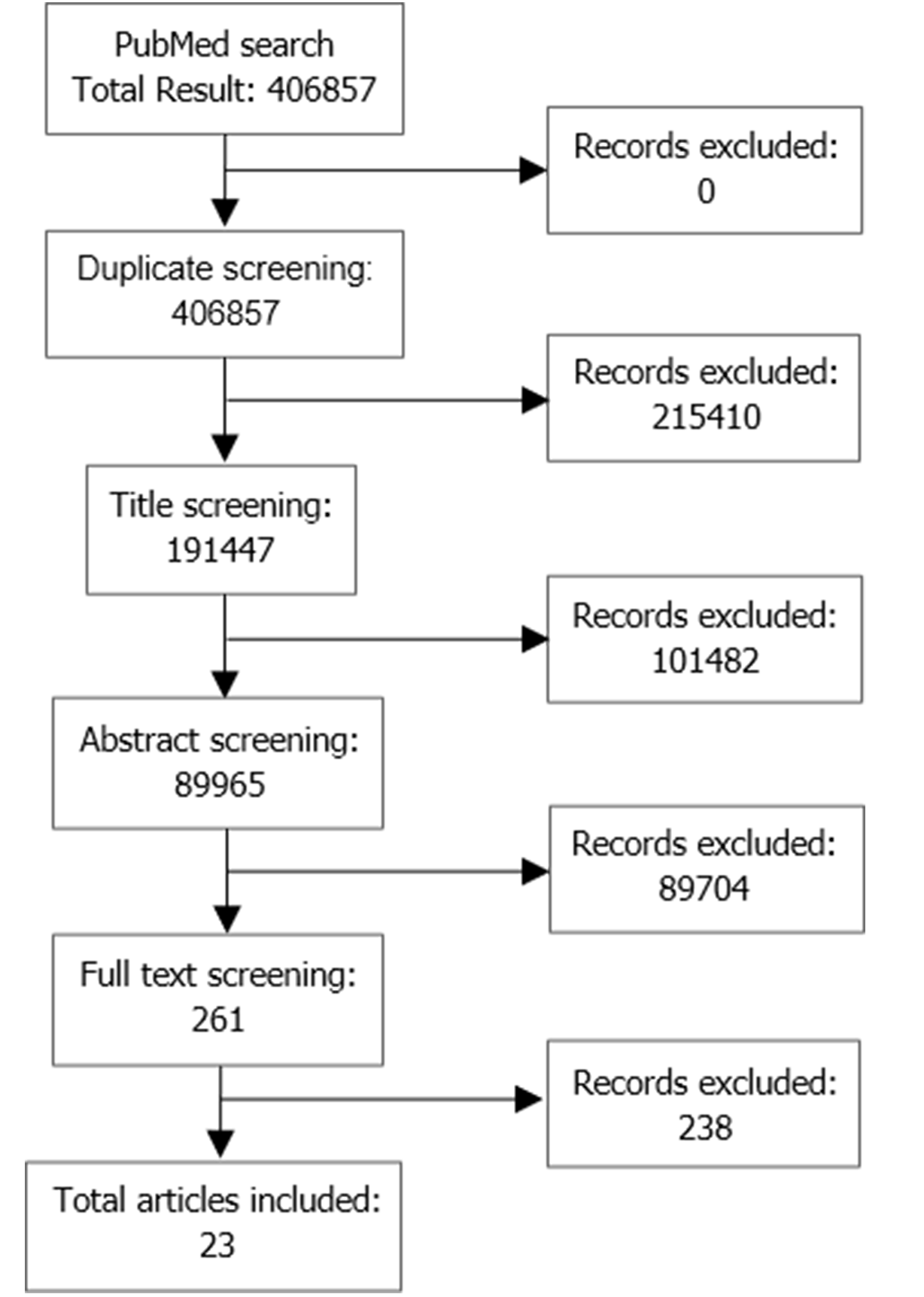
According to the World Health Organization as of September 16, 2021, there have been over 226 million documented cases of coronavirus disease 2019 (COVID-19), which has resulted in more than 4.6 million deaths and approximately 14% develop a more severe disease that requires respiratory assistance such as intubation. Early tracheostomy is recommended for patients that are expected to be on prolonged mechanical ventilation; however, supporting data has not yet been provided for early tracheostomies in COVID-19 patients. The aim of this study was to explore established guidelines for performing tracheostomies in patients diagnosed with COVID-19. Factors considered were patient outcomes such as mortality, ventilator-associated pneumonia, intensive care unit length of stay, complications associated with procedures, and risks to healthcare providers that performed tracheostomies. Various observational studies, meta-analyses, and systematic reviews were collected through a PubMed Database search. Additional sources were found through Google. The search was refined to publications in English and between the years of 2003 and 2021. The keywords used were “Coronavirus” and/or “guidelines'' and/or “tracheostomy” and/or “intensive care”. Twenty-three studies were retained. Due to the complex presentation of the respiratory virus COVID-19, previously established guidelines for tracheostomies had to be reevaluated to determine if these guidelines were still applicable to these critically ill ventilated patients. More specifically, medical guidelines state benefits to early tracheostomies in critically ill ventilated non-COVID-19 patients. However, after having conducted this review, the assumptions about the benefits of early tracheostomies in critically ill ventilated patients may not be appropriate for COVID-19 patients.
Core Tip: With the sudden onset coronavirus disease 2019 (COVID-19), guidelines for patient care were rapidly evolving to protect both providers and patients. However, it has yet to be determined if performing tracheostomies earlier or later was more beneficial for outcomes in patients infected with COVID-19. This review assesses studies that discuss the timing of tracheostomies in COVID-19 patients to establish appropriate guidelines for best patient outcomes.
- Citation: Amadi N, Trivedi R, Ahmed N. Timing of tracheostomy in mechanically ventilated COVID-19 patients. World J Crit Care Med 2021; 10(6): 345-354
- URL: https://www.wjgnet.com/2220-3141/full/v10/i6/345.htm
- DOI: https://dx.doi.org/10.5492/wjccm.v10.i6.345
After the first case of severe acute respiratory syndrome coronavirus 2 [coronavirus disease 2019 (COVID-19)] was documented in China in December 2019, the novel respiratory illness quickly turned into a pandemic and brought about a crisis to the current healthcare system. COVID-19 has played a large role in the number of diagnoses and hospitalizations not just in the United States, but worldwide. According to the World Health Organization (WHO) as of September 16, 2021, there have been over 226 million documented cases of COVID-19, which has resulted in more than 4.6 million deaths[1]. Likewise, hospital and intensive care unit (ICU) admissions have seen a drastic uptick as well. According to WHO, approximately 14% of patients develop a more severe disease, many of whom may require respiratory assistance[2,3]. Initially, supplemental oxygen is given to patients with non-invasive means such as a nasal cannula, high flow oxygen, continuous positive airway pressure machines, or bilevel positive airway pressure machines. These patients may require a more invasive form of ventilation such as endotracheal intubation with mechanical ventilation. A tracheostomy is a common surgical procedure that is done when patients require prolonged mechanical ventilation[4].
The use of tracheostomies dates as far back to 3600 B.C. The open tracheostomy used to be the procedure of choice, however, over the last few decades, the percu
This review aims to examine the timing of tracheostomy procedures performed in COVID-19 patients and their impact on outcomes.
A total of 23 studies were identified and selected for the review, Figure 1.
For COVID-19 patients, the AAO-HNS recommends that tracheostomies should not be performed in the first 2-3 wk of endotracheal intubation in hospitalized patients. They add that patients should be stable and preferably have a negative COVID-19 test[9,14]. Similar recommendations have been expressed by The British Association of Otorhinolaryngology, that a tracheostomy should not be performed within the first 14 d of intubation and COVID-19 status should be checked prior to performing the procedure[15]. The Infectious Disease Control Committee at Hospital Italiano de Buenos Aires followed guidelines that were also similar to those of the United States. Guidelines for tracheostomies in India vary slightly from other countries[13]. Because of a shortage of available tests, confirming COVID-19 status was not necessarily required before performing tracheostomy. Guidelines also suggest a more conservative approach where if there are any contradictions to intervention or unclear prognosis then tracheostomy should be delayed beyond the 14-d period.
Systematic reviews, meta-analyses and case report: Bier-Laning et al[16] conducted a study to review 59 institutions treating COVID-19 patients globally. The authors identified variability in the timing of performing tracheostomies in COVID-19 patients. However, while 91% of institutions recommended waiting a minimum of 14 days before performing the tracheostomy, only 78% of centers waited 14 d in order to pass the infectious period and retested patients before performing the procedure.
Another review stated that patients diagnosed with COVID-19 who required mechanical ventilation very rapidly deteriorate. The authors mentioned two studies: one from the United States and one from China- both of which showed very high mortality in ventilated patients. Therefore, suggesting that performing a tracheostomy early may not be very helpful[12].
Mandal et al[17] performed a review of papers that took into consideration COVID-19 patients that required tracheostomies. This study examined guidelines for timing, staff safety, procedure, technique, and post-operative care. The authors gathered recommended guidelines for tracheostomies from the United States, Canada, and India and assessed the measures concluding that guidelines were very similar. The authors concluded that a tracheostomy can be performed at or after the 2-wk waiting period as long as the patient’s prognosis is good and the ventilator setting is at 50% oxygen. However, while the waiting period is strongly recommended, it is not necessary and can be bypassed for a tracheostomy to be performed sooner if the patient is still infectious given that the endotracheal tube is not proving to be sufficient.
A study published by Hiramatsu et al[18] included a case study of a patient that received a tracheostomy on the 28th day of having COVID-19 symptoms. The patient was elderly with many underlying conditions. After the tracheostomy, the patient’s condition improved and was then eligible for transfer to another hospital. This study reflects back to the severe acute respiratory syndrome (SARS) pandemic of 2002. Tracheostomy studies conducted during this time reported that the timing from tracheal intubation to tracheostomy averaged 14 d to 25 d. In COVID-19 patients with acute respiratory failure, it is suggested that ETs (before 10 d) should be avoided.
A case report by Holmen et al[19] presented a case of a COVID-19 patient that required an extensive ICU stay due to prolonged endotracheal intubation. The patient tested negative for COVID-19 on the 37th day and a tracheostomy was later performed. Using this case, the authors raised questions about the guidelines regarding the infectivity period in COVID-19 patients[20].
An additional case report was assessed for this study. Two cases were presented, each in which the patients on mechanical ventilation underwent percutaneous tracheostomy within the two weeks of observing infectivity. Despite patients testing positive for COVID-19, the procedure can be performed safely with minimal infectivity and danger to the patients[21].
Observational Studies: A study conducted in China analyzed data from 80 patients who underwent elective tracheostomies. An ET was defined as the tracheostomy that was performed before 14 d and a late tracheostomy was defined as the procedure that was performed after 14 d. From this cohort, the median duration from endotracheal intubation to tracheostomy was 17.5 d. At the 60-d follow-up, 31 (38.8%) patients had been successfully weaned from the ventilator, 17 (21.2%) patients had been discharged from the ICU and a total of 43 (53.8%) patients had died. Late tracheostomy was associated with a lower death rate compared to ET, the hazard ratio of late tracheostomy was 0.34 (95% confidence interval: 0.17–0.70). Tracheostoma bleeding was a complication that occurred in 4 (13.3%) of ET patients and 10 (20.0%) of late tracheostomy patients. Subcutaneous emphysema occurred in one patient in each group. There was one incidence of both tracheostoma infection and mediastinal emphysema in the late tracheostomy group[22].
In a study from Italy, 50 patients were admitted in the ICU and were put on mechanical ventilation. The study cohort consisted of 23 patients who underwent a tracheostomy. ET was defined as if the procedure was performed before 10 d and late tracheostomy was defined as the tracheostomy was performed after 10 d. The average time between the initial intubation and tracheostomy was 13 d. The mean time that the patients were mechanically ventilated was 29 d and the mean length of stay in the ICU was 27 d. Nine tracheostomies were performed early, and 14 tracheostomies were performed late. After a median follow-up of 50 d, 9 (39.0 %) patients died, 5 (22.0%) were still receiving invasive mechanical ventilation (IMV) in the ICU, 3 (13.0%) were discharged from the ICU to be moved to the sub-intensive unit, and 6 (26.0%) were decannulated and discharged. Among the patients that were alive, the mean time from tracheostomy and decannulation was 26.8 d. Among deceased mean time from tracheostomy and death was 13.7 d. In this study, an ET was associated with a higher risk of mortality[23].
A study conducted in the United States of ten hospitals in the Chicagoland metropolitan area collected data from 486 hospitalized patients. Of the 138 patients that required IMV, only 19 (13.8%) intubated patients required tracheostomies. From the 138 IMV patients, 78 (56.5%) were eventually extubated and 21 had died making the mortality rate 15.2%. The timing of tracheostomy was not mentioned therefore information about the relationship of timing of tracheostomy to successful weaning or overall mortality was not provided. Thirty-nine patients remained intubated at the last follow-up. The mean length of stay for hospitalized patients was 19 d. Of the 78 patients that were extubated, 30 (38.5%) were extubated within 1-7 d, 42 (53.8%) were extubated within 7-14 d, and 6 (7.7%) were extubated after 14 d. In this study, most deaths occurred within the 14-d incubation period[10].
Schuler et al[23] conducted a study consisting of 18 patients. Tracheostomies were performed between 2 d and 16 d after intubation. The authors state that while delaying tracheostomies minimizes risk to healthcare providers, complications such as myopathy, ventilator-associated respiratory muscle atrophy, neuropathy, and inability to wean, as well as other concerns such as over-occupation of ICU beds, lengthier sedation, and inability to communicate. In this study, ETs also reduced the number of patients requiring prone positioning which often leads to accidental decannulation of the ventilation tube. The authors state that taking into consideration the clinical state of the patient, performing an earlier tracheostomy may be beneficial.
An additional study observed 29 patients with COVID-19 that were admitted to the ICU and underwent a tracheostomy. Outcomes were mortality, ICU stay, and time on mechanical ventilation. Although the average time to tracheostomy was 15.2 d, which is considered a delayed procedure. The authors found that for each day of delay in performing the procedure, the number of days on mechanical ventilation increased by 0.6 d. Delayed tracheostomies did not impact ICU stay or mortality[24].
A study conducted in the United States at the University of Pennsylvania, tracheostomies were performed in 53 COVID-19 patients with acute respiratory failure. In these patients, the average (range) time from intubation to tracheostomy was 19.7 (8-42) d. At the time of follow-up, 30 (56.6%) patients had been removed from ventilator support, 16 (30.2%) had been discharged, 7 (13.2%) had been decannulated, and 6 (11.3%) had died. There was a weak positive correlation of ET to weaning the patients from the ventilator[25].
Botti et al[26] conducted a retrospective study on 44 COVID-19 ICU patients in Italy that underwent tracheostomies. This retrospective cohort study was focused on patients over 18 years of age with severe COVID-19 pneumonia that required mechanical ventilation. Average time from intubation to tracheostomy was 7 d. Of the 44 patients, 25 (56.8%) had reported complications at follow-up such as subcutaneous emphysema, infection, or mild hemorrhage. A total of 15 (34.1%) patients had died at follow-up but there was no correlation between the timing of tracheostomy and mortality (P = 0.82). ETs were performed at this center in order to increase ICU capacity but not necessarily because of the success of performing the procedure earlier.
A study conducted in Japan included 16 patients that received tracheal intubation but nearly a third (31.0%) required tracheostomies. The average time from intubation to tracheostomy was 20 d (14-27 d) which followed the study guidelines for performing a tracheostomy after 2-3 wk of intubation. There were no reported infections amongst providers[27].
Editorials and letters to the editor: In a letter to the editor, Ferri et al[28] analyzed a sample of 8 patients that underwent tracheostomies. Tracheostomies were performed on patients that were intubated for at least 14 days. Of these 8 patients, 2 (25%) patients died after the procedure and the median time from tracheostomy to death was 3 days. This mortality rate was lower than that of COVID-19 patients admitted to the ICU at the time. In this study cohort, an intubation period of less than 20 d was associated with an increased risk of death.
An editorial by Mesolella[29] discusses if the timing of tracheostomies is a factor that influences the clinical outcome of patients. In this editorial, the author states that even while early procedures have shown better outcomes such as mortality, pneumonia, and time of mechanical ventilation, there are many complications to performing a tracheostomy that outweighs the benefits. The author suggests that by the end of the waiting period of 21 d, the viral load would have decreased, minimizing the risk to health care providers and giving providers a more accurate prognosis for the patient.
A letter to the editor by Kwak et al[30] reviewed articles as well as data from NYU Langone Health for the accuracy and efficacy of proposed guidelines for performing tracheostomies on COVID-19 patients. At this center, researchers found that the mean time from endotracheal intubation to tracheostomy was 12.2 d and the onset of symptoms to tracheostomy was 22.8 d. The authors suggest that by day 12 from intubation or day 22 from the onset of symptoms, the viral load should be greatly decreased therefore not causing any more risk than a routine tracheostomy. ETs also showed decreased time on mechanical ventilation by an average of 6.7 d and overall length of hospital stay by an average of 6.9 d. Finally, the authors stated that despite performing ETs, none of the surgeons performing the procedures were infected with COVID-19.
McGrath et al[31] discussed the changes that had been implemented for tracheostomies with the onset of COVID-19. The authors gathered that 30-d survival improved significantly with tracheostomy in general, and ICU length of stay was reported to be shorter with ETs. The authors concluded that the recommendation to postpone tracheostomies to minimize infectivity is second to the physiological status of the individual patient.
Due to the complicated presentation of COVID-19, the best practice for patient care and disease management has yet to be established. Case by case management, risk-benefit analysis, and justified medical judgement seems to provide the optimum course of action when presented with the role of providing care to these unique cases. Also, based on how critically ill COVID-19 patients are managed, guidelines will need to be established on appropriate landmarks for patients.
Various studies mention the complications associated with delaying tracheostomies[17,21,29]. Complications can be related to early or late procedure, severity of disease, comorbidities, type of tracheostomy performed, where the procedure was performed, and individual patient demographics. Many sources discussed the risk to providers performing tracheostomies on patients. The waiting period of a minimum of 14 d was mostly implemented to wait for the infectious period to pass in order to protect healthcare providers. However, in the studies that allowed ETs, there was no presentation of COVID-19 infection in providers from performing the procedure[30].
Studies on the timing of tracheostomies are still very scarce considering the novelty of the virus. However, using the limited data that is available and reflecting on studies from the 1918 H1N1 pandemic and the 2002 SARS pandemic, researchers and providers can attempt to predict how tracheostomies will define outcomes for COVID-19 patients. Other limitations of this study included varying qualities of studies gathered. Due to the novelty of the virus, researchers were limited in the number of participants that were able to be included in the study prior to publication. All eligible studies were included in this review regardless of quality due to a lack of available content. Further studies by authors aim to address these limitations.
Considering that tracheostomies are an aerosol-generating procedure, waiting to perform this procedure after the infectious period of 2-3 wk, may prevent or reduce the transmission of disease creating a safer environment for healthcare providers[18]. It was also mentioned that tracheostomies in general may not be beneficial in COVID-19 patients who are suffering from rapidly progressing disease[12]. The majority of studies showed a waiting period of 2 wk from the timing of intubation to performing a tracheostomy, Table 1.
| Ref. | Title | Country | Following Guidelines for COVID-19 in the United States? | Timing of Tracheostomy | Type of Tracheostomy | Where was the Tracheostomy Done | Patient Outcome |
| Parker et al[9] | AAO Position Statement: Tracheotomy Recommendations During the COVID-19 Pandemic | United States | Yes | Can be considered after 2-3 weeks from intubation with negative COVID test | Unknown | ICU or operating room | Inconclusive |
| Hur et al[10] | Factors Associated with Intubation and Prolonged Intubation in Hospitalized Patients with Covid-19 | United States | Yes | Assessed after ICU admission and intubation | Open | Operating Room | Unknown |
| Meng et al[11] | Early vs Late Tracheostomy in Critically Ill Patients: A Systematic Review and Meta-analysis | China | No | Various Timings | Open and Percutaneous | ICU or CCU | Early trach does not significantly alter the mortality, incidence of VAP duration of MV or length of ICU stay |
| Shiba et al[12] | Tracheostomy Considerations During the COVID-19 Pandemic | Global | Yes | Avoided if the patient is still infectious | Open and Percutaneous | Operating Room and ICU bedside | If the patient cannot be intubated, a laryngeal mask airway may be preferred over an emergent trach |
| Smith et al[13] | Tracheostomy in the intensive care unit: Guidelines during COVID-19worldwide pandemic | Argentina | No | After 21 days, negative COVID-19 test | Percutaneous | ICU | No benefits to early trach, but benefits to trach may be the possibility of decreasing sedation and delirium, increasing patient comfort, and reducing the incidence of laryngotracheal stenosis, ICU stay, and pneumonia |
| Heyd et al[14] | Tracheostomy Protocols During COVID-19 Pandemic | Global | Yes | >21 days depending on vent settings; patient shouldn’t be infectious | Open | ICU or operating room | Inconclusive |
| Takhar, et al[15] | Recommendation of a Practical Guideline for Safe Tracheostomy During the COVID-19 Pandemic | Global | Yes | At least 14 days | Open and Percutaneous | Operating Room and ICU bedside | Tracheostomy should be avoided if the prognosis is not deemed favorable since the mortality is ~50% |
| Bier-Laning et al[16] | Tracheostomy During the COVID-19Pandemic: Comparison of International Perioperative Care Protocols and Practices in 26 Countries | Global | Yes | 2-3 weeks from intubation preferably with negative COVID-19 test and falling inflammatory markers | Open and Percutaneous | Negative pressure room in ICU or Operating Room | Should reduce risk of virus exposure to providers and increase patient stability |
| Mandal et al[17] | A Systematic Review on Tracheostomy in COVID-19 Patients: Current Guidelines and Safety Measures | Global | Yes | At least 14 days; Patient should no longer be infectious | Open and Percutaneous | Operating Room and ICU bedside | Inconclusive |
| Hiramatsu et al[18] | Anesthetic and Surgical Management of Tracheostomy in a Patient With COVID-19 | Japan | Yes | Day 28 of hospitalization | Open | Negative-pressure room in ICU | Patient improved by day 35 and transferred to another hospital |
| Holmenet al[19] | Delayed Tracheostomy in a Patient With Prolonged Invasive Mechanical Ventilation due to COVID-19 | United States | Yes | Day 41 of intubation | Unknown | Unknown | Patient status improved and was discharged to rehab facility on day 58 of hospitalization |
| Marzban-Rad et al[20] | Early percutaneous dilational tracheostomy in COVID-19 patients: A case report | Iran | No | <10 days | Percutaneous | ICU | Early tracheostomy can be safely performed and improve patients’ condition when necessary |
| Tang et al[21] | Tracheostomy in 80 COVID-9 Patients: A Multicenter, Retrospective, Observational Study | China | Yes | Before 14 days or after 14 days | Open and Percutaneous | ICU or Operating room | Trachs within 14 days were associated with an increased mortality rate |
| Volo et al[22] | Elective Tracheostomy During COVID-19 Outbreak: To Whom, When, How? Early Experience from Venice, Italy | Italy | No | Median timing was 13 days- 10 days was the cut off for early to late | Open and Percutaneous | ICU | Early tracheostomy was associated with a greater risk of mortality. This conclusion was combined with SOFA scores greater than 6 and D-dimer greater than 4 |
| Schuler et al[23] | Surgical tracheostomy in a cohort of COVID-19 patients | Germany | No | Between 2-16 days | Open | ICU | No infection to staff, decreased sedatives, decrease the risk of myopathy, neuropathy, shortened ICU stay |
| Mata-Castro et al[24] | Tracheostomy in patients with SARS-CoV-2 reduces time on mechanical ventilation but not intensive care unit stay | Spain | No | 15.2 days | Unknown | Operating theatre in ICU | Delay in trach increased days of mechanical ventilation |
| Chao et al[25] | Outcomes After Tracheostomy in COVID-19 Patients | United States | Yes | 8-30 days, average 17.5 days | Open and percutaneous | Negative pressure room in ICU | Patients who underwent earlier trachs achieved ventilator liberation sooner than late trach, patients with ARDS on vents should be delayed |
| Botti et al[26] | The Role of Tracheotomy and Timing of Weaning and Decannulation in Patients Affected by Severe COVID-19 | Italy | No | 2-17 days, average 7 days | Open or percutaneous | Negative pressure room in ICU | Tracheostomies proved to be an easier approach for patients with blockages |
| Nishio et al[27] | Surgical strategy and optimal timing of tracheostomy in patients with COVID-19: Early experiences in Japan | Japan | Yes | 14-27 days, average 20 days | Open | ICU | No differences in blood loss or infection from pre to post-procedure |
| Ferri et al[28] | Indications and Times for Tracheostomy in Patients With SARS CoV2-related | Italy | No | Intubated 14 days or more | Open | ICU | The mortality rate amongst trached patients was 25% compared to 26% |
| Mesolella et al[29] | Is Timing of Tracheotomy a Factor Influencing the Clinical Course in COVID-19 Patients? | Italy | Yes | After 18 days | Unknown | ICU | Decreased pneumonia, MV rates, ability to oral feed, avoid injury to the larynx |
| Kwak et al[30] | Tracheostomy in COVID-19 Patients: Why Delay or Avoid? | United States | No | 12.8 Days | Unknown | Unknown | Decreased LOS, decreased MV, no infection to providers |
| McGrath et al[31] | Tracheostomy for COVID-19: business as usual? | Untied Kingdom | No | Case-specific | Open, percutaneous or hybrid | ICU or operating theatre | Safe for providers and patients, prevents prolonged ventilation, physiological status of patient is more important than the viral load |
In summary, the timing of tracheostomy in COVID-19 patients varied from institution to institution. However, the majority of data support delaying tracheostomies for after the first two weeks of intubation. Furthermore, the patient’s overall health condition, physiological parameters, hemodynamics status and disease burden must be considered prior to proceeding with a tracheostomy.
Manuscript source: Unsolicited manuscript
Corresponding Author's Membership in Professional Societies: ACS, 03027897.
Specialty type: Critical care medicine
Country/Territory of origin: United States
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Arumugam VA, Li L, Tsoulfas G S-Editor: Liu M L-Editor: A P-Editor: Liu M
| 1. | World Health Organization. WHO Coronavirus (COVID-19) Dashboard. 2021. [cited 7 April 2021]. Available from: https://covid19.who.int/. |
| 2. | Botta M, Tsonas AM, Pillay J, Boers LS, Algera AG, Bos LDJ, Dongelmans DA, Hollmann MW, Horn J, Vlaar APJ, Schultz MJ, Neto AS, Paulus F; PRoVENT-COVID Collaborative Group. Ventilation management and clinical outcomes in invasively ventilated patients with COVID-19 (PRoVENT-COVID): a national, multicentre, observational cohort study. Lancet Respir Med. 2021;9:139-148. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 117] [Cited by in RCA: 199] [Article Influence: 39.8] [Reference Citation Analysis (0)] |
| 3. | World Health Organization. Clinical management of severe acute respiratory infection (SARI) when COVID-19 disease is suspected. [cited 7 April 2021]. Available from: https://www.who.int/docs/default-source/coronaviruse/clinical-management-of-novel-cov.pdf. |
| 4. | Cooper JD. Tracheal Injuries Complicating Prolonged Intubation and Tracheostomy. Thorac Surg Clin. 2018;28:139-144. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 30] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 5. | Rajesh O, Meher R. Historical Review of Tracheostomy. Inter J Otolaryngol. 2005;4. |
| 6. | Borman J, Davidson JT. A history of tracheostomy: si spiritum ducit vivit (Cicero). Br J Anaesth. 1963;35:388-390. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 34] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 7. | Heffner JE. Timing of tracheotomy in ventilator-dependent patients. Clin Chest Med. 1991;12:611-625. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 30] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 8. | Hsu CL, Chen KY, Chang CH, Jerng JS, Yu CJ, Yang PC. Timing of tracheostomy as a determinant of weaning success in critically ill patients: a retrospective study. Crit Care. 2005;9:R46-R52. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 59] [Cited by in RCA: 71] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 9. | Parker N, Schiff B, Fritz M, Rapoport S, Schild S, Altman K, Merati A, Kuhn M. AAO Position Statement: Tracheotomy Recommendations During the COVID-19 Pandemic. 2021. [cited 7 April 2021]. Available from: https://www.entnet.org/content/aao-position-statement-tracheotomy-recommendations-during-covid-19-pandemic. |
| 10. | Hur K, Price CPE, Gray EL, Gulati RK, Maksimoski M, Racette SD, Schneider AL, Khanwalkar AR. Factors Associated With Intubation and Prolonged Intubation in Hospitalized Patients With COVID-19. Otolaryngol Head Neck Surg. 2020;163:170-178. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 113] [Cited by in RCA: 136] [Article Influence: 27.2] [Reference Citation Analysis (1)] |
| 11. | Meng L, Wang C, Li J, Zhang J. Early vs late tracheostomy in critically ill patients: a systematic review and meta-analysis. Clin Respir J. 2016;10:684-692. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 93] [Cited by in RCA: 79] [Article Influence: 8.8] [Reference Citation Analysis (0)] |
| 12. | Shiba T, Ghazizadeh S, Chhetri D, St John M, Long J. Tracheostomy Considerations during the COVID-19 Pandemic. OTO Open. 2020;4:2473974X20922528. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 40] [Cited by in RCA: 44] [Article Influence: 8.8] [Reference Citation Analysis (0)] |
| 13. | Smith D, Montagne J, Raices M, Dietrich A, Bisso IC, Las Heras M, San Román JE, García Fornari G, Figari M. Tracheostomy in the intensive care unit: Guidelines during COVID-19 worldwide pandemic. Am J Otolaryngol. 2020;41:102578. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 24] [Cited by in RCA: 27] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 14. | Heyd CP, Desiato VM, Nguyen SA, O'Rourke AK, Clemmens CS, Awad MI, Worley ML, Day TA. Tracheostomy protocols during COVID-19 pandemic. Head Neck. 2020;42:1297-1302. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 60] [Cited by in RCA: 57] [Article Influence: 11.4] [Reference Citation Analysis (0)] |
| 15. | Takhar A, Walker A, Tricklebank S, Wyncoll D, Hart N, Jacob T, Arora A, Skilbeck C, Simo R, Surda P. Recommendation of a practical guideline for safe tracheostomy during the COVID-19 pandemic. Eur Arch Otorhinolaryngol. 2020;277:2173-2184. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 98] [Cited by in RCA: 113] [Article Influence: 22.6] [Reference Citation Analysis (0)] |
| 16. | Bier-Laning C, Cramer JD, Roy S, Palmieri PA, Amin A, Añon JM, Bonilla-Asalde CA, Bradley PJ, Chaturvedi P, Cognetti DM, Dias F, Di Stadio A, Fagan JJ, Feller-Kopman DJ, Hao SP, Kim KH, Koivunen P, Loh WS, Mansour J, Naunheim MR, Schultz MJ, Shang Y, Sirjani DB, St John MA, Tay JK, Vergez S, Weinreich HM, Wong EWY, Zenk J, Rassekh CH, Brenner MJ. Tracheostomy During the COVID-19 Pandemic: Comparison of International Perioperative Care Protocols and Practices in 26 Countries. Otolaryngol Head Neck Surg. 2021;164:1136-1147. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 53] [Article Influence: 10.6] [Reference Citation Analysis (0)] |
| 17. | Mandal A, Nandi S, Chhebbi M, Basu A, Ray M. A Systematic Review on Tracheostomy in COVID-19 Patients: Current Guidelines and Safety Measures. Indian J Otolaryngol Head Neck Surg. 2020;1-5. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 2] [Article Influence: 0.7] [Reference Citation Analysis (1)] |
| 18. | Hiramatsu M, Nishio N, Ozaki M, Shindo Y, Suzuki K, Yamamoto T, Fujimoto Y, Sone M. Anesthetic and surgical management of tracheostomy in a patient with COVID-19. Auris Nasus Larynx. 2020;47:472-476. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 19] [Cited by in RCA: 15] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 19. | Holmen IC, Kent A, Lakritz S, Brickson C, Mastalerz K. Delayed Tracheostomy in a Patient With Prolonged Invasive Mechanical Ventilation due to COVID-19. Cureus. 2020;12:e8644. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 20. | Marzban-Rad S, Sattari P, Heidarian Moghadam M, Azimi G. Early percutaneous dilational tracheostomy in COVID-19 patients: A case report. Clin Case Rep. 2021;9:1014-1017. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 8] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 21. | Tang Y, Wu Y, Zhu F, Yang X, Huang C, Hou G, Xu W, Hu M, Zhang L, Cheng A, Xu Z, Liu B, Hu S, Zhu G, Fan X, Zhang X, Yang Y, Feng H, Yu L, Wang B, Li Z, Peng Y, Shen Z, Fu S, Ouyang Y, Xu J, Zou X, Fang M, Yu Z, Hu B, Shang Y. Tracheostomy in 80 COVID-19 Patients: A Multicenter, Retrospective, Observational Study. Front Med (Lausanne). 2020;7:615845. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 30] [Cited by in RCA: 33] [Article Influence: 6.6] [Reference Citation Analysis (0)] |
| 22. | Volo T, Stritoni P, Battel I, Zennaro B, Lazzari F, Bellin M, Michieletto L, Spinato G, Busatto C, Politi D, Spinato R. Elective tracheostomy during COVID-19 outbreak: to whom, when, how? Eur Arch Otorhinolaryngol. 2021;278:781-789. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 31] [Cited by in RCA: 40] [Article Influence: 10.0] [Reference Citation Analysis (0)] |
| 23. | Schuler PJ, Greve J, Hoffmann TK, Hahn J, Boehm F, Bock B, Reins J, Ehrmann U, Barth E, Traeger K, Jungwirth B, Wepler M. Surgical tracheostomy in a cohort of COVID-19 patients. HNO. 2021;69:303-311. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 1] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 24. | Mata-Castro N, Sanz-López L, Pinacho-Martínez P, Varillas-Delgado D, Miró-Murillo M, Martín-Delgado MC. Tracheostomy in patients with SARS-CoV-2 reduces time on mechanical ventilation but not intensive care unit stay. Am J Otolaryngol. 2021;42:102867. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 14] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 25. | Chao TN, Harbison SP, Braslow BM, Hutchinson CT, Rajasekaran K, Go BC, Paul EA, Lambe LD, Kearney JJ, Chalian AA, Cereda MF, Martin ND, Haas AR, Atkins JH, Rassekh CH. Outcomes After Tracheostomy in COVID-19 Patients. Ann Surg. 2020;272:e181-e186. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 85] [Cited by in RCA: 89] [Article Influence: 17.8] [Reference Citation Analysis (0)] |
| 26. | Botti C, Lusetti F, Peroni S, Neri T, Castellucci A, Salsi P, Ghidini A. The Role of Tracheotomy and Timing of Weaning and Decannulation in Patients Affected by Severe COVID-19. Ear Nose Throat J. 2021;100:116S-119S. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 19] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 27. | Nishio N, Hiramatsu M, Goto Y, Shindo Y, Yamamoto T, Jingushi N, Wakahara K, Sone M. Surgical strategy and optimal timing of tracheostomy in patients with COVID-19: Early experiences in Japan. Auris Nasus Larynx. 2021;48:518-524. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 8] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 28. | Ferri E, Boscolo Nata F, Pedruzzi B, Campolieti G, Scotto di Clemente F, Baratto F, Cristalli G. Indications and timing for tracheostomy in patients with SARS CoV2-related. Eur Arch Otorhinolaryngol. 2020;277:2403-2404. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 20] [Cited by in RCA: 27] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 29. | Mesolella M. Is Timing of Tracheotomy a Factor Influencing the Clinical Course in COVID-19 Patients? Ear Nose Throat J. 2021;100:120S-121S. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 4] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 30. | Kwak PE, Persky MJ, Angel L, Rafeq S, Amin MR. Tracheostomy in COVID-19 Patients: Why Delay or Avoid? Otolaryngol Head Neck Surg. 2021;164:683-684. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 31. | McGrath BA, Brenner MJ, Warrillow SJ. Tracheostomy for COVID-19: business as usual? Br J Anaesth. 2020;125:867-871. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 20] [Cited by in RCA: 18] [Article Influence: 3.6] [Reference Citation Analysis (0)] |