Published online Sep 9, 2021. doi: 10.5492/wjccm.v10.i5.163
Peer-review started: March 16, 2021
First decision: May 13, 2021
Revised: May 25, 2021
Accepted: August 19, 2021
Article in press: August 19, 2021
Published online: September 9, 2021
Processing time: 177 Days and 1.3 Hours
Disasters resulting in mass casualty incidents can rapidly overwhelm the Emergency Department (ED). To address critical manpower needs in the ED’s disaster response, medical student involvement has been advocated. Duke-National University of Singapore Medical School is in proximity to Singapore General Hospital and represents an untapped manpower resource. With appropriate training and integration into ED disaster workflows, medical students can be leveraged upon as qualified manpower. This review provides a snapshot of the conceptualization and setting up of the Disaster Volunteer Corps – a programme where medical students were recruited to receive regular training and assessment from emergency physicians on disaster response principles to fulfil specific roles during a crisis, while working as part of a team under supervision. We discuss overall strategy and benefits to stakeholders, emphasizing the close symbiotic relationship between academia and healthcare services.
Core Tip: The Disaster Volunteer Corps provides a unique way of teaching medical students disaster medicine principles in a hands-on experiential format, while simultaneously enhancing operational readiness of the hospital in times of disaster. This model of collaboration between university education and healthcare services provides a feasible model of structured volunteerism.
- Citation: Ponampalam R, Pong JZ, Wong XY. Medical students as disaster volunteers: A strategy for improving emergency department surge response in times of crisis. World J Crit Care Med 2021; 10(5): 163-169
- URL: https://www.wjgnet.com/2220-3141/full/v10/i5/163.htm
- DOI: https://dx.doi.org/10.5492/wjccm.v10.i5.163
Disasters can occur with little warning and produce mass casualties that quickly overwhelm an Emergency Department’s (ED) capacity. In many parts of the world, EDs operate at close to maximum capacity daily, and strategies are thus needed to cope with a sudden increase in patient load. Disaster contingency plans of many hospitals involve the shunting of existing non emergent operations staff and heal
In the literature, there have been a multitude of recommendations made for the improvement of ED surge capacity[1,2]. These range from strategies to recognise an impending surge, resource utilisation during a surge, new workflows and processes, and of note to this review, the role of additional staff in the form of medical students to augment ED surge capacity. As many medical schools are built beside hospitals, the EDs of these hospitals thus have a ready and available manpower resource that can be quickly activated in an emergency. Due to the flexible nature of day-to-day responsibilities for medical students as compared to physicians and nurses working on the wards, medical students could potentially respond rapidly to the ED within minutes of activation. They can be task trained to fulfil specific roles, working under supervision and as part of a team. It is notable from previous disasters that medical students were eager and enthusiastic to contribute in times of crisis, but were often held back by their perceived lack of experience and feelings of inadequacy[3-6]. Indeed, a recent study noted that medical students were capable of carrying out disaster triage with equal parity to emergency physicians[7,8]. Students were also made ‘runners’ within the hospital during a crisis, a role they could play well due their familiarity with the hospital layout and equipment location[9]. With proper training, coordination, and integration with ED workflow, medical students can thus be a huge asset in disaster management at the ED.
Several disaster training programmes aimed at medical students have been published in literature, with varying training approaches. Duration of the courses ranges from one day to four weeks, comprising both didactic lectures and practical training[10]. To the best of our knowledge, there has been no reported studies where medical students were formally inducted as volunteers attached to an Emergency Department, with staggered training over the entire duration of their medical school career.
This review provides a snapshot of the conceptualization and setting up of the Disaster Volunteer Corps (DVC) program at Duke-National University of Singapore (Duke-NUS) Medical School, a novel approach of formally engaging medical students as disaster volunteers while supplementing the medical curriculum. We discuss overall strategy and benefits to stakeholders, emphasizing the close symbiotic relationship between academia and healthcare services.
The overall objective of the DVC is to recruit, train, and retain keen medical students in different areas of disaster management, who can be reliably activated in the event of an emergency to serve as skilled manpower support.
The specific aims of the DVC are threefold: (1) Educational aim: The educational aim is for the training of medical students in the core competencies needed to support disaster operations in the ED; (2) Institutional aim: To strengthen the surge capacity of the ED, by having a pool of trained, competent, and trusted volunteers that can be rapidly mobilized; and (3) National aim: The national aim of the DVC is achieved through the training of medical students, to improve the community response to terror and crisis. This is in line with the Singapore government’s strategy of a robust community response to threats and disasters[11].
Singapore General Hospital (SGH) is the largest tertiary care hospital in Singapore, with approximately 350 patients presenting each day to the ED. Duke-NUS Medical School, SGH’s affiliated medical university, is located in proximity to the ED (400 meters away) and has a cohort of approximately 250 students. For most days of the week, medical students undertake their clinical rotations in the wards, clinics, and operating theatres of SGH.
The DVC represents a tripartite partnership between major stakeholders of SGH, Duke-NUS Medical School, and the Students’ Council of Duke-NUS Medical School. The proposal to involve medical students as disaster volunteers in a formal capacity involved ensuring that the goals of the DVC aligned with each stakeholder’s agenda.
In keeping with Duke-NUS Medical School’s agenda for student education, the DVC curriculum was designed to complement traditional medical education. As most medical schools do not teach much in the way of disaster medicine, the DVC seeks to plug this gap, enhancing medical education in a practical and hands-on approach. Duke-NUS Medical School was thus supportive of the DVC as it was in keeping with its objective of education and service to the community. The emergency planning committee and senior management of SGH recognized and appreciated the potential contributions of student volunteers and supported training by providing manpower and resources for the DVC. From the medical student perspective, the program offered an opportunity for formal disaster training to be equipped with skill sets which would allow them to contribute practically and productively in a real-world crisis. They would also be integrated into ED disaster planning and operations as an asset. The proposal for the DVC was thus warmly received among the medical student population.
A formal agreement between SGH and Duke-NUS Medical School for the participation of its students was achieved. Students of the DVC could take their leave amidst their clinical duties (e.g., ward round, clinic) if they were activated in a true disaster. Medical liability and insurance were also extended by Duke-NUS Medical School to students participating in official DVC activities. Tasks in which students could participate in were agreed upon, and for which they were trained for as per the curriculum (Table 1).
| Module | Duration | Workshop |
| 1 | 7 h | Introduction and disaster medicine principles; HAZMAT decontamination course |
| 2 | 7 h | Disaster field responder course; Disaster first aid course |
| 3 | 7 h | Bioterrorism and pandemic responder course; Radiation responder course |
| 4 | 7 h | Psychological first aider course; Introduction to hospital disaster operations |
The DVC pilot program was officially launched in 2019 with ten medical student volunteers. Scheduled training sessions were held once every three months, with students task trained for specific disaster roles (Table 1). Core faculty involved in training were emergency physicians with subspecialty fellowships in disaster medicine, prehospital medicine, and toxicology, and who were actively involved in the hospital’s disaster planning and response committee. This allowed for added realism in the DVC trainings. Contributions were made also from other specialities including nursing, security, and allied health.
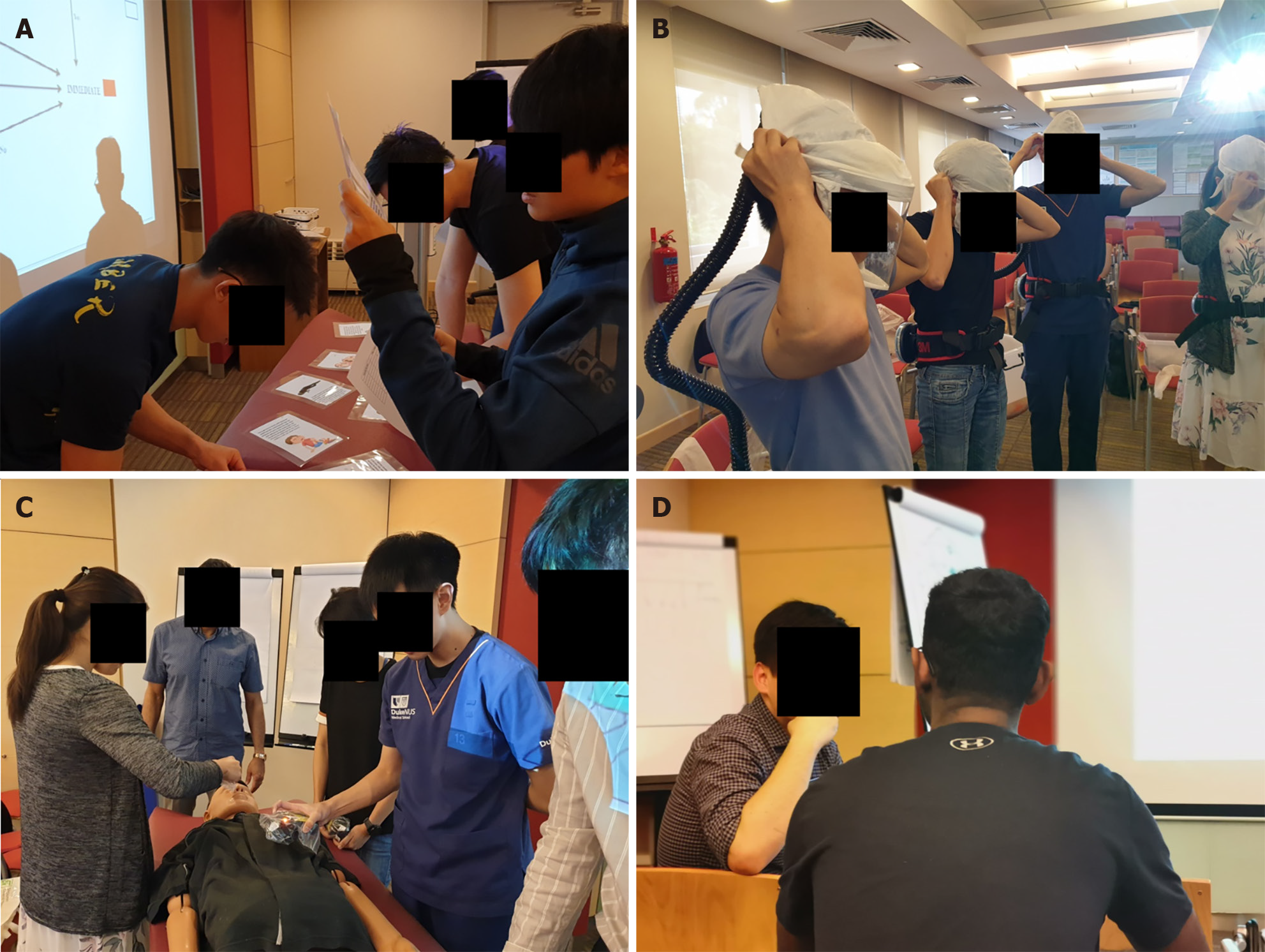
The DVC curriculum was composed of modular courses (Figures 1-3), with assessment to ensure competency of volunteers[12]. The modular concept for training was adopted as it allowed better flexibility for medical students to acquire specific skillsets and competencies over time while giving better control to hospital emergency response planners to achieve a targeted readiness level and facilitating deployment decisions for students in specific roles as part of the hospitals’ disaster response team. Each module consisted of a didactic lecture giving broad overview of disaster response plans followed by specific task training based on unique assigned roles and culminated in a summary disaster simulation exercise for better appreciation of coordination and workflow as part of the hospital’s disaster response team. Assessments to ensure competency for the specific task included multiple choice questions, quizzes, and objective structured clinical examinations. Feedback on each training session was sought so as to improve training for subsequent batches of students. A train-the-trainer approach was adopted, where medical students who had completed a module would assist ED faculty in the training of subsequent batches of students. This leverages on peer learning and teaching pedagogy, promotes ownership of knowledge, and allows for program scalability. On a practical level, records of students who have underwent training are kept which would allow trainers to tap on these students to assist them and subsequently carry out training sessions independently. A call-tree activation process synchronized with the hospital’s disaster activation plans was implemented for DVC activation in times of crisis.
In addition to the scheduled training sessions, the DVC was also invited to participate in a hospital wide disaster simulation exercise as an observer, with plans for enhanced participation as the DVC matures. Through the DVC program and with exposure to disaster simulation exercises, we aim to enable the deployment of student volunteers during crisis situations in defined roles according to their competency, working under general supervision of team leaders.
The critical shortage of skilled manpower during a disaster is to be anticipated. Although there may be large numbers of good Samaritans who would volunteer their services during a crisis, the specific skills required in these individuals are often lacking and at best questionable, making deployment decisions difficult. There is also difficulty in ensuring ED security in the context of accepting help from individuals whose motives may not be apparent at the outset. Considering these issues, medical students who are often already in the hospital on clinical attachment and can be trained to fulfil specific roles in times of disaster[13], represent an untapped man
The involvement of medical students in disaster operation, however, is not without its challenges. Although the practical hands-on approach adopted by the DVC gives medical students an advantage in appreciating the complexities of dealing with disasters, there are several contentious issues related to their actual deployment in times of disaster. Concerns include exposure to psychological trauma, medical student safety, and the medicolegal aspects of caring for patients in such situations[14-16]. It is therefore important for the level of involvement and specific roles of students to be agreed upon by all stakeholders to prevent misunderstanding, ensure safety of the students, and maximise their assistance in times of disaster. The decision making and actions required in crisis situations are made even more difficult with the limited resources available[17]. These are challenges faced by healthcare workers with extensive experience and training and would be compounded for medical students with limited experience and knowledge. Critical decisions on the need for performing interventions such as field amputations and surgical procedures should thus be left to qualified physicians, with medical students best placed to render aid under supervision on predetermined tasks. Discussions should also be had about the psychological impact of working in disaster environments, with possible exposure to grievous injuries and suffering, the ethics of providing care in extreme situations, reasons for withholding treatment in certain conditions, triage intentions with the aim of benefiting the majority, and palliative care for the unsalvageable[18-20].
The potential contribution of medical students in crisis conditions are manifold[21], and training of students to fulfil specific roles with clearly defined objectives would be beneficial for ED surge capacity. The participation of well trained, motivated, and readily available volunteers would be invaluable in ED disaster management.
The DVC provides a unique way of teaching medical students disaster medicine principles in a hands-on experiential format, while simultaneously enhancing the operational readiness of the hospital and ED in times of disaster. This model of close collaboration between university education and healthcare services provides a feasible model of structured volunteerism that could be replicated in other similar settings.
Dr. Kenneth Tan Boon Kiat, Head, Department of Emergency Medicine, Singapore General Hospital, who provided logistics and manpower support and the multidisciplinary team of experts including emergency physicians, psychiatrists, palliative care doctors, nurses, radiation physicists and medical social workers who contributed to the workshops and training activities of the Disaster Volunteer Corps program.
Manuscript source: Invited manuscript
Specialty type: Emergency medicine
Country/Territory of origin: Singapore
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Pandya A S-Editor: Wang LL L-Editor: A P-Editor: Li X
| 1. | Bradt DA, Aitken P, FitzGerald G, Swift R, O'Reilly G, Bartley B. Emergency department surge capacity: recommendations of the Australasian Surge Strategy Working Group. Acad Emerg Med. 2009;16:1350-1358. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 22] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 2. | American Medical Association and American Public Health Association. Improving health system preparedness for terrorism and mass casualty events - recommendations for action. 2007. [cited 20 April 2021]. Available from: https://stacks.cdc.gov/view/cdc/6891. |
| 3. | Kaiser HE, Barnett DJ, Hsu EB, Kirsch TD, James JJ, Subbarao I. Perspectives of future physicians on disaster medicine and public health preparedness: challenges of building a capable and sustainable auxiliary medical workforce. Disaster Med Public Health Prep. 2009;3:210-216. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 63] [Cited by in RCA: 67] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 4. | Katz CL, Gluck N, Maurizio A, DeLisi LE. The medical student experience with disasters and disaster response. CNS Spectr. 2002;7:604-610. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 18] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 5. | Avashia YJ, Thaller SR. Postearthquake plastic surgery mission trip to Port-au-Prince, Haiti: a medical student's perspective. J Craniofac Surg. 2011;22:1549-1551. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 6. | Reyes H. Students' response to disaster: a lesson for health care professional schools. Ann Intern Med. 2010;153:658-660. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 10] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 7. | Merin O, Ash N, Levy G, Schwaber MJ, Kreiss Y. The Israeli field hospital in Haiti--ethical dilemmas in early disaster response. N Engl J Med. 2010;362:e38. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 97] [Cited by in RCA: 68] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 8. | Sapp RF, Brice JH, Myers JB, Hinchey P. Triage performance of first-year medical students using a multiple-casualty scenario, paper exercise. Prehosp Disaster Med. 2010;25:239-245. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 36] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 9. | Roccaforte JD. The World Trade Center attack. Observations from New York's Bellevue Hospital. Crit Care. 2001;5:307-309. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 28] [Cited by in RCA: 30] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 10. | Ashcroft J, Byrne MHV, Brennan PA, Davies RJ. Preparing medical students for a pandemic: a systematic review of student disaster training programmes. Postgrad Med J. 2021;97:368-379. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 37] [Cited by in RCA: 57] [Article Influence: 11.4] [Reference Citation Analysis (0)] |
| 11. | Government of Singapore. Be prepared, our response matters. 2019. [cited 20 April 2021]. Available from: https://www.sgsecure.sg. |
| 12. | Hsu EB, Thomas TL, Bass EB, Whyne D, Kelen GD, Green GB. Healthcare worker competencies for disaster training. BMC Med Educ. 2006;6:19. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 136] [Cited by in RCA: 126] [Article Influence: 6.6] [Reference Citation Analysis (0)] |
| 13. | Verson J, Dyga N, Agbayani N, Serafin F, Hondros L. Design and implementation of a medical student hazardous materials response team: the Medical Student HazMat Team. Int J Emerg Med. 2018;11:38. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 14. | Silver-Isenstadt A, Ubel PA. Erosion in medical students' attitudes about telling patients they are students. J Gen Intern Med. 1999;14:481-487. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 30] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 15. | Kessler CS, McGuinn M, Spec A, Christensen J, Baragi R, Hershow RC. Underreporting of blood and body fluid exposures among health care students and trainees in the acute care setting: a 2007 survey. Am J Infect Control. 2011;39:129-134. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 50] [Cited by in RCA: 56] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 16. | Wynia MK. Ethics and public health emergencies: encouraging responsibility. Am J Bioeth. 2007;7:1-4. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 13] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 17. | Kirsch TD, Moon MR. A piece of my mind. The line. JAMA. 2010;303:921-922. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 10] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 18. | Carney JK, Schilling LM, Frank SH, Biddinger PD, Bertsch TF, Grace CJ, Finkelstein JA. Planning and incorporating public health preparedness into the medical curriculum. Am J Prev Med. 2011;41:S193-S199. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 24] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 19. | Kinlaw K, Barrett DH, Levine RJ. Ethical guidelines in pandemic influenza: recommendations of the Ethics Subcommittee of the Advisory Committee of the Director, Centers for Disease Control and Prevention. Disaster Med Public Health Prep. 2009;3 Suppl 2:S185-S192. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 44] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 20. | Lo B, Katz MH. Clinical decision making during public health emergencies: ethical considerations. Ann Intern Med. 2005;143:493-498. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 29] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 21. | Kaiser HE, Barnett DJ, Hayanga AJ, Brown ME, Filak AT. Medical students' participation in the 2009 Novel H1N1 influenza vaccination administration: policy alternatives for effective student utilization to enhance surge capacity in disasters. Disaster Med Public Health Prep. 2011;5:150-153. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 9] [Article Influence: 0.6] [Reference Citation Analysis (0)] |