Copyright
©The Author(s) 2021.
World J Crit Care Med. Jan 9, 2021; 10(1): 1-11
Published online Jan 9, 2021. doi: 10.5492/wjccm.v10.i1.1
Published online Jan 9, 2021. doi: 10.5492/wjccm.v10.i1.1
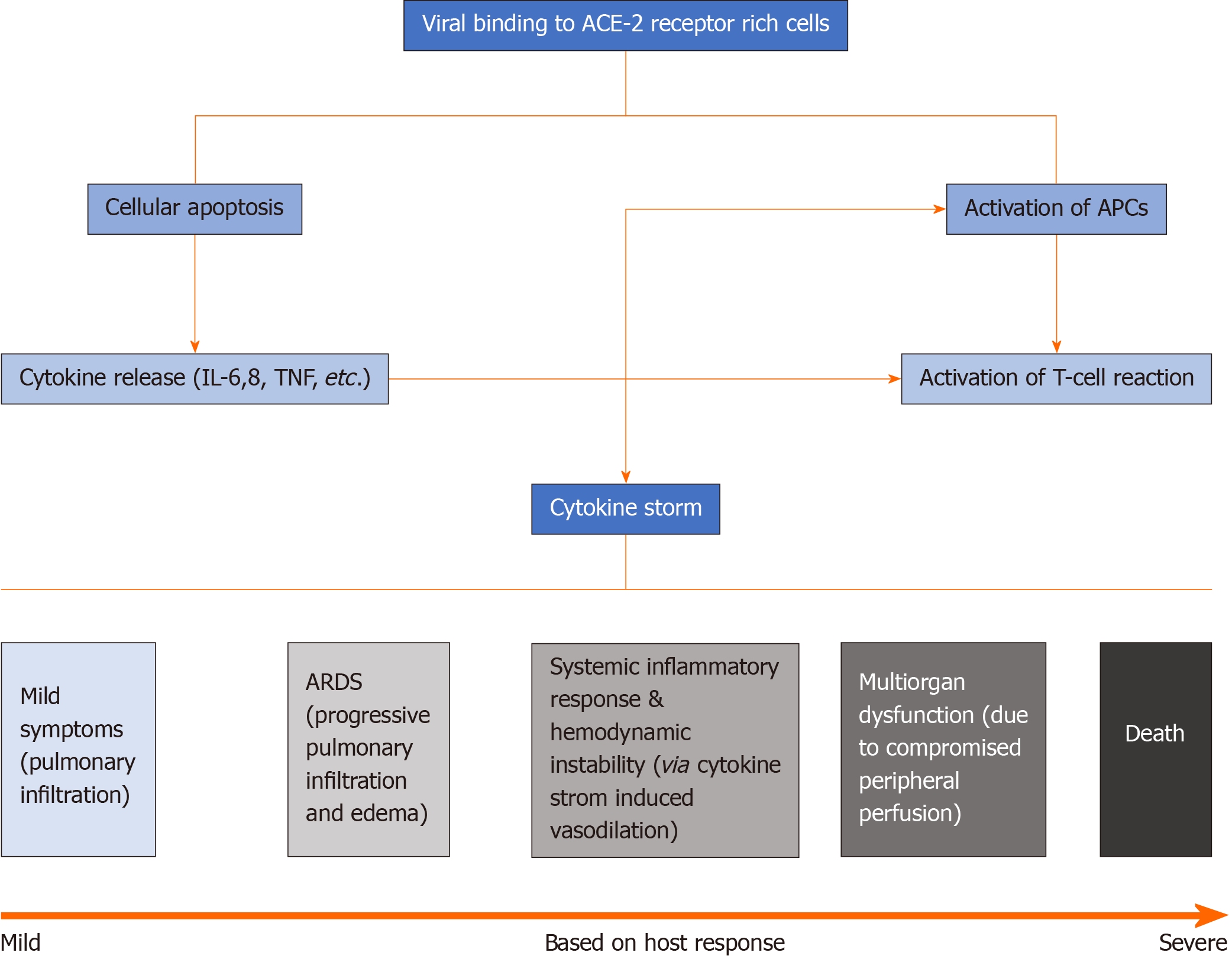
Figure 1 Pathophysiology of coronavirus disease 2019 infection.
Viral binding and invasion of angiotensin converting enzyme 2 receptor-rich cells triggers destruction of infected cells with release of cytokines (mainly interleukin-6, interleukin-8 and tumor necrosis factor) and chemo-attractants, as well as activation of neighboring antigen presenting cells (APCs). Cytokine surge and APC activation triggers a T-cell mediated response and further release of cytokines. Activation of T-cells along with ongoing destruction of infected cells leads to cytokine storm. Symptoms developed range from mild respiratory symptoms to multiorgan failure and death based upon host response. ACE-2: Angiotensin converting enzyme 2; APCs: Antigen presenting cells; IL: Interleukin; TNF: Tumor necrosis factor; ARDS: Acute respiratory distress syndrome.
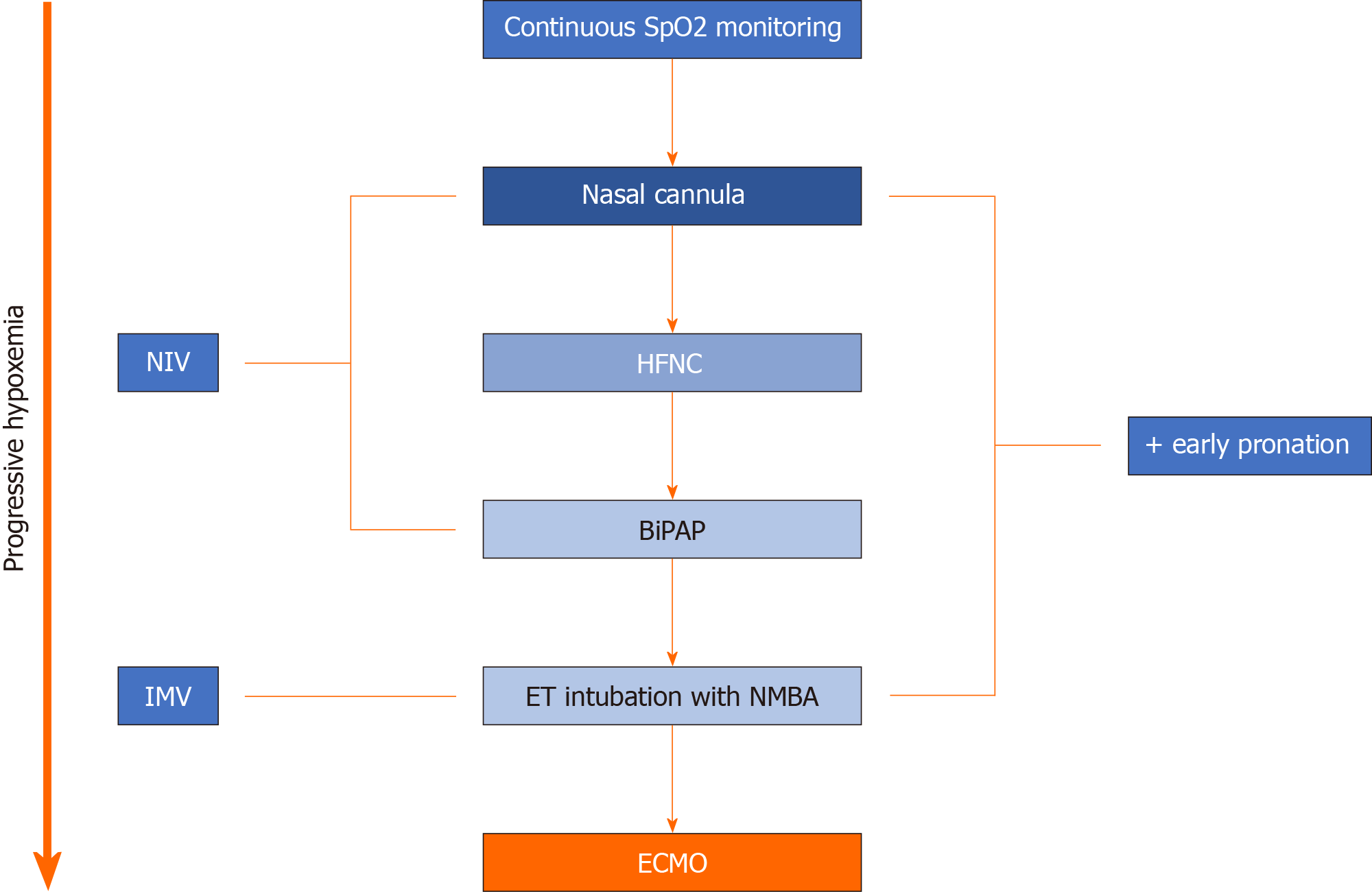
Figure 2 Respiratory management in coronavirus disease patients with pulmonary compromise.
Extracorporeal membrane oxygenation is reserved as a final resort when all other noninvasive and invasive ventilation options fail. SpO2: Saturation of oxygen via pulse oximetry; HFNC: High flow nasal cannula; BiPAP: Bilevel positive airway pressure; ET: Endotracheal; NMBA: Neuromuscular blockade agent; NIV: Noninvasive ventilation; IMV: Invasive mechanical ventilation; ECMO: Extracorporeal membrane oxygenation.
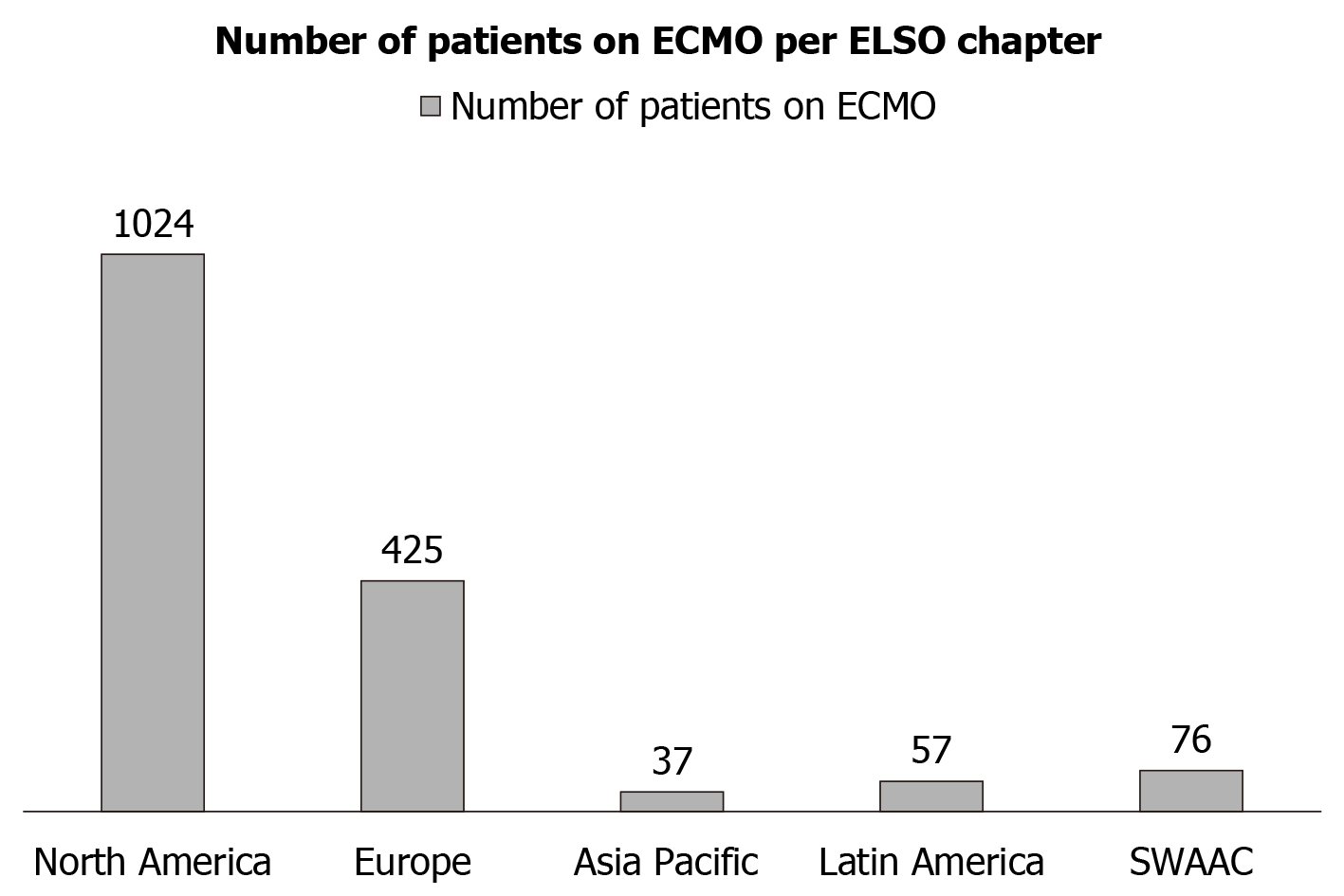
Figure 3 Utilization of extracorporeal membrane oxygenation.
Various Extracorporeal Life Support Organization chapter uses were reported. Data reported was based on reports from June 26, 2020. ECMO: Extracorporeal membrane oxygenation; ELSO: Extracorporeal Life Support Organization.
- Citation: Kichloo A, Kumar A, Amir R, Aljadah M, Farooqi N, Albosta M, Singh J, Jamal S, El-Amir Z, Kichloo A, Lone N. Utilization of extracorporeal membrane oxygenation during the COVID-19 pandemic. World J Crit Care Med 2021; 10(1): 1-11
- URL: https://www.wjgnet.com/2220-3141/full/v10/i1/1.htm
- DOI: https://dx.doi.org/10.5492/wjccm.v10.i1.1