Published online Mar 28, 2015. doi: 10.5412/wjsp.v5.i1.137
Peer-review started: September 28, 2014
First decision: December 17, 2014
Revised: December 29, 2014
Accepted: January 15, 2015
Article in press: January 19, 2015
Published online: March 28, 2015
Processing time: 187 Days and 7.4 Hours
Accumulation of experiences and technological advances after the first report of laparoscopic liver resection (LLR) are now revealing the characteristics and specific advantages of this approach, especially for hepatocellular carcinoma (HCC) patients with chronic liver diseases (CLD). In laparoscopic approach, there are minimum needs for: (1) laparotomy and dissection of the attachments and adhesion which may cause destructions in the collateral blood and lymphatic flows; and (2) compression of the liver which may cause parenchymal damage for the liver resection (LR). These are especially beneficial for the patients with CLD. LLR results in minimal postoperative ascites and the other complications, which could potentially lead to lowering the risk of fatal liver failure. These characteristics of LLR facilitate surgical treatment application to the patients of HCC with background CLD. Laparoscopic approach also results in improved vision and manipulation in a small operative field under several conditions, including the cases where it is necessary to perform repeat LR between adhesions. These characteristics make LLR safer and more accessible to the repeat treatment, such as multicentric and metachronous lesions in the cirrhotic liver. These advantages of LLR indicate it is a superior method than open LR under certain conditions in patients of HCC with background CLD.
Core tip: In laparoscopic approach, there are minimum needs for: (1) laparotomy and dissection of the attachments/adhesion which may cause destructions in the collateral blood/lymphatic flows; and (2) compression of the liver which may cause parenchymal damage for liver resection (LR). Therefore, laparoscopic LR (LLR) results in minimal postoperative ascites and following fatal complications in the patients with hepatocellular carcinoma and chronic liver disease. Laparoscopic approach also results in improved vision and manipulation in a small operative field in the case of repeat LR between adhesions. These characteristics make LLR safer and more accessible to the repeat treatment, such as multicentric/metachronous lesions in cirrhotic liver.
- Citation: Kawabe N, Morise Z, Tomishige H, Nagata H, Kawase J, Arakawa S, Isetani M. Laparoscopic liver resection for the treatment of hepatocellular carcinoma. World J Surg Proced 2015; 5(1): 137-141
- URL: https://www.wjgnet.com/2219-2832/full/v5/i1/137.htm
- DOI: https://dx.doi.org/10.5412/wjsp.v5.i1.137
Hepatocellular carcinoma (HCC) is the fifth most common cancer and the third most common cause of cancer-related deaths[1,2]. Treatment options for HCC include liver resection (LR)[3], liver transplantation[4], transarterial chemoembolization (TACE), and local ablation therapy[5]. Most experts think LR and liver transplantation are the best hopes for cure. However, patients with HCC usually have underlying chronic liver disease (CLD), and hence are at high risk of developing significant postoperative complications and also multicentric/metachronous lesions. Although liver transplantation should be considered in patients with deteriorating liver function according to the Milan criteria[6], LR should be considered as a primary therapy in patients with well-preserved liver function[7,8]. When considering the treatment of HCC in patients with CLD, the degree of invasive surgical stress[9], especially to the background liver, should be considered in addition to the oncological effects. Patients with CLD have high rates of morbidity and mortality at surgery[10], which increase according to Child-Pugh class of the patients[11]. Even limited open LR often develops refractory ascites, which leads to fatal liver failure in severe CLD patients[12,13].
In Japan, criteria is based on three parameters for selecting patient eligibility for LR: (1) the presence or absence of ascites; (2) total serum bilirubin level; and (3) indocyanine green retention rate at 15 min (ICG R15)[14]. Although there are other treatment options for HCC, local ablation therapy and TACE, depending on the tumor condition and the liver function, a large number of patients with severe CLD are still not able to undergo those treatment modalities. This is especially true in the condition of patients that need repeat treatments for multicentric metachronous lesions occurring in chronic impaired liver. For those patients, “less invasive” laparoscopic LR (LLR) may provide a good option.
Since the first successful report of laparoscopic liver wedge resection in 1992[15], LLR is thought to be a “less invasive” procedure than open LR (OLR)[16]. In a comprehensive meta-analysis study, LLR was compared to OLR in 1678 patients across 26 studies. While it is associated with longer operating times and no differences in oncological outcomes, it is advantageous in several aspects, such as reduced amount of bleeding, decreased time of application of Pringle’s maneuver, decreases in morbidity rate, and shorter hospital stay[17]. Recent technological development of devices and accumulation of experiences have facilitated the expansion of LLR indication[18,19]. In addition to common advantages of laparoscopic surgery[20], accumulation of experiences is now revealing specific advantages of LLR, especially for HCC and CLD patients.
The characteristics and advantages of LLR for HCC patients are discussed in this review.
LLR may be particularly advantageous for cirrhotic patients, given the potential for lower levels of parietal and hepatic injury, which leads to the preservation of venous/lymphatic collateral circulation. Several studies have shown the safety and feasibility and its short-term benefits of LLR for HCC patients[21-28]. To date, several studies[29-33], in which the groups of laparoscopic and open LR in comparison had comparable background liver condition, have investigated the major differences between the groups (Table 1)[29,34-41]. Favorable short-term results, including fewer incidences of ascites and liver failure, and shorter hospital stays, correlate with the laparoscopic procedure without the compromise of overall survival (Table 1). In addition to usual advantages of laparoscopic surgery, LLR has the advantage of minimal ascites, due to lower damage on venous/lymphatic collateral circulation, which leads to lower risk of fatal liver failure. This feature of LLR could be one of the most remarkable specific advantage.
| Ref. | % of LC patients | Ascites | Liver failure | Hospital stay (d, mean ± SD) | Mortality | Overall survival (5-yr, %) | ||||||
| LLR | OLR | LLR | OLR | LLR | OLR | LLR | OLR | LLR | OLR | LLR | OLR | |
| Lai et al[34] | 92 | 93.94 | NA | NA | NA | NA | NA | NA | 0/25 | 1/33 | 60 (3-yr) | NA |
| Aldrighetti et al[35] | 56.25 | 56.25 | 0/16 | 1/6 | NA | NA | 6.3 ± 1.7 | 9 ± 3.8 | 0/16 | 0/16 | (No significant difference ) | |
| Tranchart et al[36] | 73.81 | 80.95 | 3/42 | 11/42 | 0/36 | 4/53 | 6.7 ± 5.9 | 9.6 ± 3.4 | 1/42 | 1/42 | 59.5 | 47.4 |
| Kim et al[37] | 92.31 | 86.21 | 0/26 | 1/29 | NA | NA | 11.08 ± 4.96 | 16.1 ± 10.7 | 0/26 | 0/29 | 84.6 (2-yr RFS) | 82.8 (2-yr RFS) |
| Lee et al[38] | 84.85 | 64 | 0/33 | 2/50 | NA | NA | NA | NA | 0/33 | 0/50 | 76 | 76.1 |
| Truant et al[39] | 100 | 100 | 5/36 | 12/53 | NA | NA | 6.5 ± 2.7 | 9.5 ± 4.8 | 0/36 | 4/53 | 70 | 46 |
| Ker et al[29] | NA | NA | 2/116 | 26/208 | NA | NA | 6.2 ± 3 | 12.4 ± 6.8 | 0/116 | 6/208 | 62.2 | 71.8 |
| Kanazawa et al[40] | 100 | 100 | 3/28 | 18/28 | 0/28 | 0/28 | 10 (6-25)1 | 19 (8-49)1 | 0/28 | 0/28 | NA | NA |
| Cheung et al[41] | 87.5 | 71.9 | 0/32 | 1/64 | NA | NA | 4 (2-16)1 | 7 (4-42)1 | 2/32 | 12/64 | 76.6 | 57 |
When patients undergo LR, they are exposed three types of stresses: (1) general, whole-body surgical stress; (2) reduced liver function due to resected liver volume; and (3) surgery-induced injury to the environment around the liver caused by laparotomy and mobilization of the liver and to the liver parenchyma caused by compression of the liver. Reduction of the third injury with LLR lowers the risk of fatal complications for patients with severe CLD.
We also experienced that HCC patients with severe CLD (Child-Pugh class B/C and ICG R15 of ≥ 40%) who underwent LLR had favorable and comparable perioperative outcomes to patients with mild/moderate CLD[42]. As of June 2014, 53 patients with HCC and CLD underwent LLR in our hospital. Nine out of 53 patients had severe CLD (Child-Pugh class B/C and ICG R15 of ≥ 40%). These nine and 41 patients (Child-Pugh class A and ICG R15 of 10.1%-27.4%; three patients were excluded from analysis because of concomitant combined surgery) were compared in short-tem outcomes. The results, such as operative bleeding, day of oral intake restored, postoperative drain discharge, morbidity and mortality, were comparable in the groups. Among these nine patients, one underwent living-related liver transplantation 20 mo after hepatectomy.
This extensive review of the literature in combination with our experiences indicates that LLR is the better therapeutic option for severe CLD patients with tumors on the surface of the liver, especially after repeat treatments. LLR for severe CLD patients may also prove to be an advantageous option in bridging therapy to liver transplantation.
At the introduction of LLR in 1997, we selected the patients who could undergo adequate oncological LLR for cancers. The indication of LLR had been gradually extended from liver surface partial resection to large anatomical resection (right/left hepatectomy and posterior/anterior/median sectionectomy). The inclusion criteria are now a tumor size less than 15 cm without severe adhesion, invasion to major vessels, or a need for reconstruction of vessels or biliary tract.
As of June 2014, we have performed 53 of LLR for HCC and CLD patients, including 17 cases of anatomical resections and 9 cases of repeat hepatectomy (including 1 patient of 4th laparoscopic hepatectomy). There was no operative-mortality and the rate of morbidity (Clavien-Dindo Grade II or above) was 17.0%. Tumor numbers are 1-4 and sizes are 0.8-14.5 cm. The median of their operating time and blood loss was 315 min and 100 mL. From these and the other experiences, we propose advantages and disadvantages of LLR in technical aspects, listed in Table 2.
| Advantages |
| Good view and manipulation in a small operative field-minimum damages on the environment around the liver |
| Meticulous manipulation under magnified view |
| Less adhesion after surgery |
| Good view in the dorsal area of the liver around inferior vena cava |
| Dissection and handling organs/tumors using postural change and the gravity with the maintenance of similar view by the laparoscopic adjustments[43,44] |
| Less venous bleeding under the pneumo-peritoneal pressure |
| Disadvantages |
| Restrictions on the movements of forceps |
| Difficulties of handling large-sized/volume organs and tumors |
| These should be conquered with port arrangements and dissection and handling organs/tumors using postural change and the gravity |
| Lack of tactile sensation |
| Lack of overview of whole operative field |
| These easily lead to disorientation during surgery and should be conquered with preoperative (MDCT) simulation plus intraoperative US navigation |
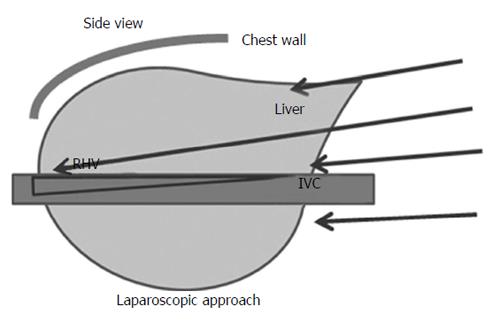
The subphrenic space is the cage with the liver inside. In the laparoscopic approach of LR, a laparoscope and forceps are entering into the cage directly from caudal direction and obtain a good vision/manipulation for resection in the small field (Figure 1). On the other hand in open approach, the cage is opened with the big subcostal incision and the liver is picked up with the dissection of retroperitoneal attachments before resection. Therefore, in the laparoscopic approach, there are minimum needs for: (1) dissection of the attachments/adhesions which may cause destructions of the collateral blood and lymphatic flows; and (2) compression of the liver which may cause parenchymal damage, in addition to the minimum abdominal wall incision. These characteristics lead to two advantages especially beneficial for HCC patients with CLD: (1) Advantageous for repeat procedures: Repeat LLR for patients with CLD and repeat lesions was feasible and safe. The procedure resulted in less adhesion and good vision/manipulation in the small area between adhesions; and (2) Minimal invasion due to good vision and manipulation in small operative fields (a minimum need for extended dissection of attachments and adhesions): With adequate port arrangement and positioning of patients[41,42], the manipulation in the small operative field is facilitated by good vision of the peri-inferior vena cava area, subphrenic space, the area next to the attachment of retro-peritoneum, and the area between the adhesions. Therefore, there is a minimum need for dissection/adhesiolysis that could cause destructions of the collateral blood and lymphatic flows.
There are minimum needs in laparoscopic approach for: (1) laparotomy and dissection of the attachments/adhesion which may cause destructions in the collateral blood/lymphatic flows; and (2) compression of the liver which may cause parenchymal damage in laparoscopic approach. These are especially beneficial for CLD patients. LLR results in minimal postoperative ascites, which could potentially lead to lower risk of fatal complications. These characteristics of LLR facilitate the surgical treatments for HCC/CLD patients.
LLR also results in improved vision and manipulation in a small operative field under several conditions, including the cases where it is necessary to perform repeat hepatectomy between adhesions, such as multicentric/metachronous lesions in the cirrhotic liver. These characteristics could make LLR a safer and more accessible approach for patients with repeat treatments.
These advantages of LLR indicate it is a superior method when compared to OLR under certain conditions in patients with HCC and CLD.
P- Reviewer: Pan Q S- Editor: Ji FF L- Editor: A E- Editor: Liu SQ
| 1. | El-Serag HB, Rudolph KL. Hepatocellular carcinoma: epidemiology and molecular carcinogenesis. Gastroenterology. 2007;132:2557-2576. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3846] [Cited by in RCA: 4265] [Article Influence: 236.9] [Reference Citation Analysis (2)] |
| 2. | Schütte K, Bornschein J, Malfertheiner P. Hepatocellular carcinoma--epidemiological trends and risk factors. Dig Dis. 2009;27:80-92. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 239] [Cited by in RCA: 309] [Article Influence: 19.3] [Reference Citation Analysis (0)] |
| 3. | Capussotti L, Ferrero A, Viganò L, Polastri R, Tabone M. Liver resection for HCC with cirrhosis: surgical perspectives out of EASL/AASLD guidelines. Eur J Surg Oncol. 2009;35:11-15. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 45] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 4. | Hwang S, Lee SG, Belghiti J. Liver transplantation for HCC: its role: Eastern and Western perspectives. J Hepatobiliary Pancreat Sci. 2010;17:443-448. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 55] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 5. | Lau WY, Leung TW, Yu SC, Ho SK. Percutaneous local ablative therapy for hepatocellular carcinoma: a review and look into the future. Ann Surg. 2003;237:171-179. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 148] [Cited by in RCA: 179] [Article Influence: 8.1] [Reference Citation Analysis (0)] |
| 6. | Mazzaferro V, Regalia E, Doci R, Andreola S, Pulvirenti A, Bozzetti F, Montalto F, Ammatuna M, Morabito A, Gennari L. Liver transplantation for the treatment of small hepatocellular carcinomas in patients with cirrhosis. N Engl J Med. 1996;334:693-699. [PubMed] |
| 7. | Ryder SD. Guidelines for the diagnosis and treatment of hepatocellular carcinoma (HCC) in adults. Gut. 2003;52 Suppl 3:iii1-iii8. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 150] [Cited by in RCA: 220] [Article Influence: 10.0] [Reference Citation Analysis (0)] |
| 8. | Cha CH, Ruo L, Fong Y, Jarnagin WR, Shia J, Blumgart LH, DeMatteo RP. Resection of hepatocellular carcinoma in patients otherwise eligible for transplantation. Ann Surg. 2003;238:315-321; discussion 321-323. [PubMed] |
| 9. | Hoeper MM, Krowka MJ, Strassburg CP. Portopulmonary hypertension and hepatopulmonary syndrome. Lancet. 2004;363:1461-1468. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 344] [Cited by in RCA: 282] [Article Influence: 13.4] [Reference Citation Analysis (0)] |
| 10. | Ziser A, Plevak DJ, Wiesner RH, Rakela J, Offord KP, Brown DL. Morbidity and mortality in cirrhotic patients undergoing anesthesia and surgery. Anesthesiology. 1999;90:42-53. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 261] [Cited by in RCA: 224] [Article Influence: 8.6] [Reference Citation Analysis (0)] |
| 11. | Mansour A, Watson W, Shayani V, Pickleman J. Abdominal operations in patients with cirrhosis: still a major surgical challenge. Surgery. 1997;122:730-735; discussion 735-736. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 308] [Cited by in RCA: 250] [Article Influence: 8.9] [Reference Citation Analysis (0)] |
| 12. | Belghiti J, Hiramatsu K, Benoist S, Massault P, Sauvanet A, Farges O. Seven hundred forty-seven hepatectomies in the 1990s: an update to evaluate the actual risk of liver resection. J Am Coll Surg. 2000;191:38-46. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 800] [Cited by in RCA: 798] [Article Influence: 31.9] [Reference Citation Analysis (0)] |
| 13. | Lai EC, Fan ST, Lo CM, Chu KM, Liu CL, Wong J. Hepatic resection for hepatocellular carcinoma. An audit of 343 patients. Ann Surg. 1995;221:291-298. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 302] [Cited by in RCA: 319] [Article Influence: 10.6] [Reference Citation Analysis (0)] |
| 14. | Torzilli G, Makuuchi M, Inoue K, Takayama T, Sakamoto Y, Sugawara Y, Kubota K, Zucchi A. No-mortality liver resection for hepatocellular carcinoma in cirrhotic and noncirrhotic patients: is there a way? A prospective analysis of our approach. Arch Surg. 1999;134:984-992. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 344] [Cited by in RCA: 352] [Article Influence: 13.5] [Reference Citation Analysis (0)] |
| 15. | Gagner M, Rheault M, Dubuc J. Laparoscopic partial hepatectomy for liver tumor. Surg Endosc. 1992;6:97-98. |
| 16. | Kaneko H, Tsuchiya M, Otsuka Y, Yajima S, Minagawa T, Watanabe M, Tamura A. Laparoscopic hepatectomy for hepatocellular carcinoma in cirrhotic patients. J Hepatobiliary Pancreat Surg. 2009;16:433-438. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 58] [Cited by in RCA: 59] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 17. | Mirnezami R, Mirnezami AH, Chandrakumaran K, Abu Hilal M, Pearce NW, Primrose JN, Sutcliffe RP. Short- and long-term outcomes after laparoscopic and open hepatic resection: systematic review and meta-analysis. HPB (Oxford). 2011;13:295-308. [PubMed] |
| 18. | Buell JF, Cherqui D, Geller DA, O’Rourke N, Iannitti D, Dagher I, Koffron AJ, Thomas M, Gayet B, Han HS. The international position on laparoscopic liver surgery: The Louisville Statement, 2008. Ann Surg. 2009;250:825-830. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1249] [Cited by in RCA: 1155] [Article Influence: 72.2] [Reference Citation Analysis (0)] |
| 19. | Tsuchiya M, Otsuka Y, Tamura A, Nitta H, Sasaki A, Wakabayashi G, Kaneko H. Status of endoscopic liver surgery in Japan: a questionnaire survey conducted by the Japanese Endoscopic Liver Surgery Study Group. J Hepatobiliary Pancreat Surg. 2009;16:405-409. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 27] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 20. | Viganò L, Tayar C, Laurent A, Cherqui D. Laparoscopic liver resection: a systematic review. J Hepatobiliary Pancreat Surg. 2009;16:410-421. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 135] [Cited by in RCA: 135] [Article Influence: 8.4] [Reference Citation Analysis (0)] |
| 21. | Morise Z. Pure laparoscopic hepatectomy for HCC patients. Hepatocellular Carcinoma - Clinical Research. Zagreb, Croatia: InTech 2012; 183-196. [DOI] [Full Text] |
| 22. | Chen HY, Juan CC, Ker CG. Laparoscopic liver surgery for patients with hepatocellular carcinoma. Ann Surg Oncol. 2008;15:800-806. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 118] [Cited by in RCA: 110] [Article Influence: 6.5] [Reference Citation Analysis (0)] |
| 23. | Dagher I, Lainas P, Carloni A, Caillard C, Champault A, Smadja C, Franco D. Laparoscopic liver resection for hepatocellular carcinoma. Surg Endosc. 2008;22:372-378. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 75] [Cited by in RCA: 69] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 24. | Kaneko H, Takagi S, Otsuka Y, Tsuchiya M, Tamura A, Katagiri T, Maeda T, Shiba T. Laparoscopic liver resection of hepatocellular carcinoma. Am J Surg. 2005;189:190-194. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 248] [Cited by in RCA: 243] [Article Influence: 12.2] [Reference Citation Analysis (0)] |
| 25. | Cherqui D, Laurent A, Tayar C, Chang S, Van Nhieu JT, Loriau J, Karoui M, Duvoux C, Dhumeaux D, Fagniez PL. Laparoscopic liver resection for peripheral hepatocellular carcinoma in patients with chronic liver disease: midterm results and perspectives. Ann Surg. 2006;243:499-506. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 236] [Cited by in RCA: 233] [Article Influence: 12.3] [Reference Citation Analysis (0)] |
| 26. | Shimada M, Hashizume M, Maehara S, Tsujita E, Rikimaru T, Yamashita Y, Tanaka S, Adachi E, Sugimachi K. Laparoscopic hepatectomy for hepatocellular carcinoma. Surg Endosc. 2001;15:541-544. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 146] [Cited by in RCA: 145] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 27. | Sarpel U, Hefti MM, Wisnievsky JP, Roayaie S, Schwartz ME, Labow DM. Outcome for patients treated with laparoscopic versus open resection of hepatocellular carcinoma: case-matched analysis. Ann Surg Oncol. 2009;16:1572-1577. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 107] [Cited by in RCA: 107] [Article Influence: 6.7] [Reference Citation Analysis (0)] |
| 28. | Hu BS, Chen K, Tan HM, Ding XM, Tan JW. Comparison of laparoscopic vs open liver lobectomy (segmentectomy) for hepatocellular carcinoma. World J Gastroenterol. 2011;17:4725-4728. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 56] [Cited by in RCA: 66] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 29. | Ker CG, Chen JS, Kuo KK, Chuang SC, Wang SJ, Chang WC, Lee KT, Chen HY, Juan CC. Liver Surgery for Hepatocellular Carcinoma: Laparoscopic versus Open Approach. Int J Hepatol. 2011;2011:596792. [PubMed] |
| 30. | Endo Y, Ohta M, Sasaki A, Kai S, Eguchi H, Iwaki K, Shibata K, Kitano S. A comparative study of the long-term outcomes after laparoscopy-assisted and open left lateral hepatectomy for hepatocellular carcinoma. Surg Laparosc Endosc Percutan Tech. 2009;19:e171-e174. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 70] [Cited by in RCA: 77] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 31. | Nguyen KT, Marsh JW, Tsung A, Steel JJ, Gamblin TC, Geller DA. Comparative benefits of laparoscopic vs open hepatic resection: a critical appraisal. Arch Surg. 2011;146:348-356. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 272] [Cited by in RCA: 293] [Article Influence: 19.5] [Reference Citation Analysis (0)] |
| 32. | Laurent A, Cherqui D, Lesurtel M, Brunetti F, Tayar C, Fagniez PL. Laparoscopic liver resection for subcapsular hepatocellular carcinoma complicating chronic liver disease. Arch Surg. 2003;138:763-769; discussion 769. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 234] [Cited by in RCA: 219] [Article Influence: 10.0] [Reference Citation Analysis (0)] |
| 33. | Belli G, Fantini C, D’Agostino A, Cioffi L, Langella S, Russolillo N, Belli A. Laparoscopic versus open liver resection for hepatocellular carcinoma in patients with histologically proven cirrhosis: short- and middle-term results. Surg Endosc. 2007;21:2004-2011. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 189] [Cited by in RCA: 186] [Article Influence: 10.3] [Reference Citation Analysis (0)] |
| 34. | Lai EC, Tang CN, Ha JP, Li MK. Laparoscopic liver resection for hepatocellular carcinoma: ten-year experience in a single center. Arch Surg. 2009;144:143-147; discussion 148. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 89] [Cited by in RCA: 94] [Article Influence: 5.9] [Reference Citation Analysis (0)] |
| 35. | Aldrighetti L, Guzzetti E, Pulitanò C, Cipriani F, Catena M, Paganelli M, Ferla G. Case-matched analysis of totally laparoscopic versus open liver resection for HCC: short and middle term results. J Surg Oncol. 2010;102:82-86. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 109] [Cited by in RCA: 117] [Article Influence: 7.8] [Reference Citation Analysis (0)] |
| 36. | Tranchart H, Di Giuro G, Lainas P, Roudie J, Agostini H, Franco D, Dagher I. Laparoscopic resection for hepatocellular carcinoma: a matched-pair comparative study. Surg Endosc. 2010;24:1170-1176. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 182] [Cited by in RCA: 188] [Article Influence: 11.8] [Reference Citation Analysis (0)] |
| 37. | Kim HH, Park EK, Seoung JS, Hur YH, Koh YS, Kim JC, Cho CK, Kim HJ. Liver resection for hepatocellular carcinoma: case-matched analysis of laparoscopic versus open resection. J Korean Surg Soc. 2011;80:412-419. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 31] [Cited by in RCA: 41] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 38. | Lee KF, Chong CN, Wong J, Cheung YS, Wong J, Lai P. Long-term results of laparoscopic hepatectomy versus open hepatectomy for hepatocellular carcinoma: a case-matched analysis. World J Surg. 2011;35:2268-2274. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 83] [Cited by in RCA: 95] [Article Influence: 7.3] [Reference Citation Analysis (0)] |
| 39. | Truant S, Bouras AF, Hebbar M, Boleslawski E, Fromont G, Dharancy S, Leteurtre E, Zerbib P, Pruvot FR. Laparoscopic resection vs open liver resection for peripheral hepatocellular carcinoma in patients with chronic liver disease: a case-matched study. Surg Endosc. 2011;25:3668-3677. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 90] [Cited by in RCA: 106] [Article Influence: 7.6] [Reference Citation Analysis (0)] |
| 40. | Kanazawa A, Tsukamoto T, Shimizu S, Kodai S, Yamazoe S, Yamamoto S, Kubo S. Impact of laparoscopic liver resection for hepatocellular carcinoma with F4-liver cirrhosis. Surg Endosc. 2013;27:2592-2597. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 81] [Cited by in RCA: 95] [Article Influence: 7.9] [Reference Citation Analysis (0)] |
| 41. | Cheung TT, Poon RT, Yuen WK, Chok KS, Jenkins CR, Chan SC, Fan ST, Lo CM. Long-term survival analysis of pure laparoscopic versus open hepatectomy for hepatocellular carcinoma in patients with cirrhosis: a single-center experience. Ann Surg. 2013;257:506-511. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 181] [Cited by in RCA: 200] [Article Influence: 16.7] [Reference Citation Analysis (0)] |
| 42. | Morise Z, Sugioka A, Kawabe N, Umemoto S, Nagata H, Ohshima H, Kawase J, Arakawa S, Yoshida R. Pure laparoscopic hepatectomy for hepatocellular carcinoma patients with severe liver cirrhosis. Asian J Endosc Surg. 2011;4:143-146. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 37] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 43. | Tomishige H, Morise Z, Kawabe N, Nagata H, Ohshima H, Kawase J, Arakawa S, Yoshida R, Isetani M. Caudal approach to pure laparoscopic posterior sectionectomy under the laparoscopy-specific view. World J Gastrointest Surg. 2013;5:173-177. [PubMed] |
| 44. | Ikeda T, Yonemura Y, Ueda N, Kabashima A, Shirabe K, Taketomi A, Yoshizumi T, Uchiyama H, Harada N, Ijichi H. Pure laparoscopic right hepatectomy in the semi-prone position using the intrahepatic Glissonian approach and a modified hanging maneuver to minimize intraoperative bleeding. Surg Today. 2011;41:1592-1598. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 35] [Article Influence: 2.5] [Reference Citation Analysis (0)] |