INTRODUCTION
Gastric bypass was first described in the literature by Mason et al[1] in 1967 and soon replaced jejuno-ileal bypass as the surgical procedure of choice for severe obesity. Roux-en-Y gastric bypass survives to this day as the gold standard bariatric operation for individuals with body mass index (BMI) > 40 or BMI > 35 in the presence of significant comorbidities, despite challenges from vertical banded gastroplasty in the 1970s and 80s, laparoscopic adjustable banding in the 1990s, and laparoscopic sleeve gastrectomy in the last five years. Its superiority in terms of degree and reliability of weight loss and durability of weight loss has been well documented[2-6]. However, Roux-en-Y gastric bypass does not describe a single operation, but rather a family of operations. There are many variants, and each one is probably performed a little differently by each and every surgeon who carries it out. The same is also true of other types of bariatric surgery, and distinguishes these operations from most other abdominal procedures. Unlike so much of abdominal surgery, where resection is undertaken to remove tumours or other offending organs, bariatric surgery aims to achieve weight loss and metabolic benefits, through anatomical changes undertaken to alter physiology or function. There is a real need to standardise the key features of the gastric bypass. Concepts regarding how these operations achieve their goal are changing, and will continue to change as our understanding of the drivers of obesity and metabolic disease also changes.
Gastric bypass, gastroplasty, gastric banding and sleeve gastrectomy have all been primarily regarded as restrictive operations, meaning the operation achieves weight loss, through restriction to eating resulting in an enforced reduction in energy intake. But as we have learned more over the years, we begin to appreciate other less obvious mechanisms by which each or some of these operations may achieve their goal[7,8]. In the 1980s Gastric bypass was recognised as having a greater impact on food choice than gastroplasty (or the subsequent variant of adjustable gastric banding), because of its propensity to induce dumping following the intake of sugar and fat[9]. This distinction remains and certainly contributes to the superior results of gastric bypass over the other restrictive operations. More recently, following intense interest in the metabolic benefits of bariatric surgery, there is compelling, though not yet conclusive evidence that duodenal bypass confers its own benefit, distinct from that brought about by reduction in the size of the gastric reservoir, and the slowing of gastric emptying[7,8].
Notwithstanding our knowledge of subtle mechanisms by which gastric bypass may achieve major weight loss, the restrictive component remains an essential feature of a successful gastric bypass operation. Significant weight regain after gastric bypass is invariably related to increased energy intake, which may come about through one or more of the following: (1) diminished restriction; (2) increased intake of energy dense foods; or (3) increased frequency of eating (“grazing”). While the latter two of these are largely beyond the control of the surgeon, the first can be minimised by attention to technical detail in the performance of gastric bypass. Variation in weight loss following gastric bypass does occur and is to be expected. One of the major factors accounting for such variation is the degree of restriction imposed by the surgery and the degree to which that restriction is permanent. It is the purpose of this paper to outline the authors’ view on those features of a gastric bypass which may optimise weight loss and enhance the prospect of that loss being durable. These opinions have been developed through a 28 year experience of around 1500 gastric bypass operations, and review of such literature as can provide a basis to the recommendations. As many of the recommendations have never been subjected to rigorous testing, they might best, at this time, be considered opinion or “hypothesis”.
BACKGROUND TO THE RECOMMENDATIONS
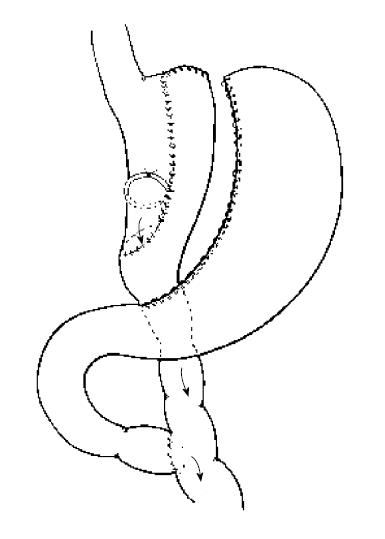
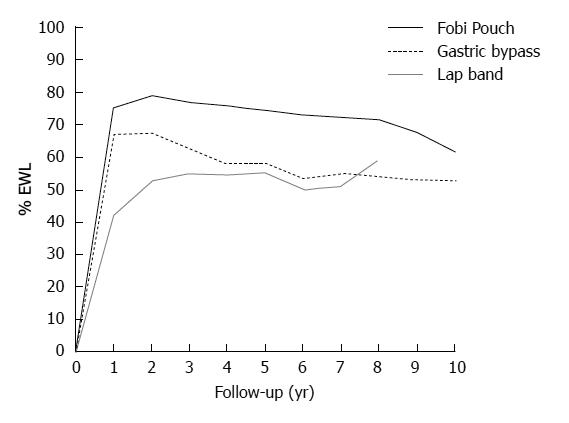
The weakness and disappointments of all bariatric operations rest largely with long-term weight regain. Reports of long-term weight loss outcomes are rare in the literature, and there exist no randomised trials comparing weight loss beyond around 5 years for any of the commonly and currently performed operations. Yet it is well recognised that the differences between operations may not become apparent for at least 5 years. At the present time the most mature and useful comparative data on various operations comes from the systematic review conducted by O’Brien et al[10] and reported in Obesity Surgery in 2006. In this report comparative data was presented for laparoscopic adjustable banding, BPD procedures, gastric bypass and banded gastric bypass. To be included in the systematic review, individual series had to have at least 100 patients with minimum 3-year follow-up. A total of over 1500 gastric bypasses were reported on and over 700 banded gastric bypasses. The former were a mix of open and laparoscopic bypasses and included the experience of a number of leading gastric bypass surgeons at the time, including the large experiences of Wittgrove et al[11] and Higa et al[12]. The Banded bypasses were all open procedures coming from three groups around the World reported by Fobi et al[13], Capella et al[14] and my own group[15]. In essence, all three groups performed a very similar procedure shown schematically in Figure 1, and referred to in this paper as the Fobi Pouch gastric bypass. The summary weight loss data, taken from the systematic review of O’Brien et al[10] is shown in Figure 2. The best early and late results were achieved by the banded gastric bypass and BPD procedures, which both yielded very similar results, and which were both clearly superior to those of the non banded gastric bypass group. Although the early results of the gastric bypass group were superior to those of the adjustable gastric banding group, there was significant weight regain in the standard gastric bypass group with time, meaning much of the advantage over the gastric banding group was subsequently lost.
Figure 1 Schematic diagram of Fobi Pouch Gastric Bypass.
Figure 2 Medium - long-term weight loss data for banded gastric bypass (Fobi Pouch), standard gastric bypass and Laparoscopic adjustable banding.
Data from systematic review by O’Brien et al[10] 2006. (%EWL on the x axis refers to the percentage of pre-operative weight in excess of ideal body weight, which has been lost at any one point in time, shown on the y axis.
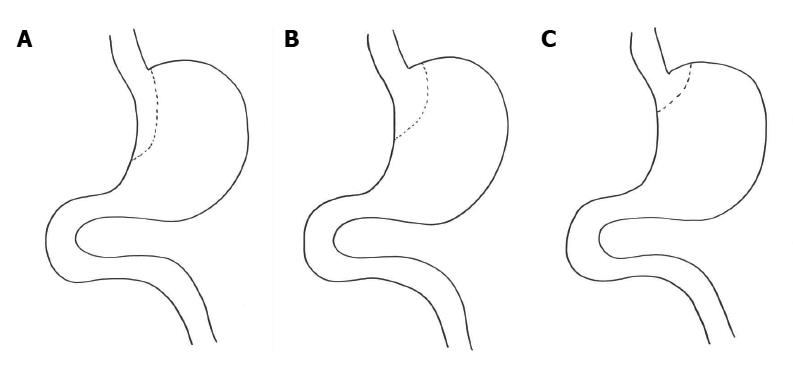
Having contributed 342 of the 779 patients to the banded gastric bypass group reported by O’Brien et al[10], we feel justified in proposing possible explanations for the superiority of this operation over the standard gastric bypass, performed by acknowledged expert surgeons, whether by open or laparoscopic surgery. In essence the difference rests with the size and shape of the pouch which possibilities are shown diagrammatically in Figure 3 and the presence of a silastic ring to define the size of the outlet[16]. These issues underpin the basis of our recommendations.
Figure 3 Schematic representations of possible configurations of gastric pouch.
A: Shows a long narrow pouch based on the lesser curve; B: Shows a rather wider and shorter pouch based on the lesser curve; C: Shows a very small pouch formed by stapling just beyond the oesophago-gastric junction.
FOOD RESTRICTION AND GASTRIC BYPASS
Restriction to eating is achieved through the size and integrity of the gastric pouch and the size of the gastric outlet. We learned many years ago that simple stapling to create the pouch was unreliable, and the integrity of the pouch could be lost, and weight regained through so-called, “staple-line” disruption[17,18]. The problem persisted despite the development of better staplers. Gastric transection was required and over time became an integral part of all modern gastric bypass operations[19]. However, despite gastric transection, gastro-gastric fistulae may develop as staple lines adhere to one another and recanalisation occurs. This occurrence has been described in up to 6% of cases[20]. The consequence will depend on the size of the gastro-gastric fistula and may include gastric ulceration[17,21], bleeding and weight regain[22,23]. Prevention of this occurrence can be achieved by interposition of small bowel as described and proposed by Capella et al[23] and Fobi[22] and is to be recommended. We have never seen a gastro-gastric fistula develop following Fobi Pouch gastric bypass in over 1000 such operations performed by us since 1997.
POUCH SIZE
Much time and effort has been given to thinking about the optimal size of the gastric pouch. In the 1980s this was thought to be about 30 mL. Today, we believe it should be rather smaller. We learned through the 1980s that horizontal pouches, made across the upper portion of the greater curve of the stomach, as originally proposed, were very prone to dilatation. The recognition that vertical pouches based on the lesser curve of the stomach were much less prone to dilatation than the horizontal pouches based on the greater curve was an important one[24]. In addition to being less liable to dilatation, such vertically oriented pouches preserved a more reliable blood supply for the gastro-enteric anastomosis. Regardless of size, gastric pouches that include even a little of the greater curve of the stomach are more likely to dilate over time, and lead to weight regain, than those which begin at the angle of His. This is an important point, particularly in the age of laparoscopic gastric bypass. Gastric pouches should begin close to the angle of His rather than include any portion of greater curve and should be oriented down the lesser curve for a variable distance. The one caveat here is that the stapling should be carried out through stomach wall not lower oesophagus, to ensure more reliable healing.
POUCH LENGTH
It is both of interest and instructive to note empirically that weight loss after a Roux-en-Y gastric bypass operation is considerably greater than would be expected following total gastrectomy. There are likely two reasons for this. The pattern of motility in the oesophagus and jejunum are quite different from that of the stomach. Both propel food forward relatively quickly. The stomach does not, acting rather to churn its content. Inclusion in the food stream of a portion of stomach therefore acts to slow the passage of food from the oesophagus to the jejunum and hence contribute to the restriction imposed by the operation. If this tube (or lesser curve pouch) is too short (as shown in Figure 3C), strong peristalsis in the oesophagus may allow food to pass quickly to the jejunum and hence lead to reduced “restriction”. For this reason small pouches based immediately below the gastro-oesophageal junction are not likely to function optimally, and weight loss may be disappointing. Ideally, the pouch should incorporate a length of lesser curve of the stomach (as shown in Figure 3A). Poiseuille’s Law tells us that the flow rate through a tube is inversely proportional to its length. Slow flow or emptying of the pouch is desirable after gastric bypass and contributes to the restriction. In the Fobi pouch variant of gastric bypass the length of the gastric pouch is typically up to 8-10 cm[14,15] which is rather more than would commonly be achieved in the construction of a laparoscopic Roux-en-Y gastric bypass.
SHAPE OF THE POUCH
Much has been written and discussed over the years concerning the optimal size of the gastric pouch. Much less has ever been said or written regarding its shape. Yet it is likely that the shape (length and diameter) may be rather more important than the size itself[16]. LaPlace Law tells us that the pressure required to distend a structure (tube) is inversely proportional to its radius. Poiseuille’s Law, mentioned above, tells us that resistance to flow through a tube is proportional to the length of the tube and inversely proportional to the 4th power of the radius. These two laws of physics suggest that for optimum function (viz. no dilatation with time, and slow emptying) the gastric pouch should be made long and narrow, as is the case with Fobi Pouch gastric bypass(as demonstrated in Figure 3). There is a tendency in the creation of a laparoscopic gastric bypass for the pouch to be made wider and therefore shorter (to accomplish the small volume) in order to allow the anastomosis to be performed using stapling devices, which will not fit into a long and narrow gastric pouch (such as is schematically shown in Figure 3B). The weight regain not uncommonly seen 3-5 years following laparoscopic gastric bypass[25] is certainly often explained by enlargement of the pouch. For durable restriction and therefore weight loss, a long narrow pouch is required.
GASTRIC OUTLET
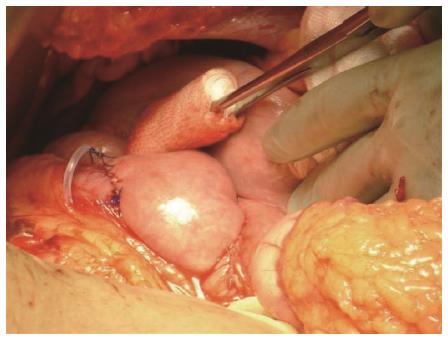
For many years there has been general agreement that diameter of the gastric outlet should be around 1cm. This was the recommended size for gastric bypass operations when these became popular in the 1980s, and seemed confirmed by the 5.0 or 5.5 cm circumference size of the ring or band placed around the vertical banded gastroplasty[26,27]. However, from the early days of gastric bypass, it became clear that one of the reasons for late weight regain was enlargement of the gastric outlet, or gastro-jejunal anastomosis and more rapid emptying of the pouch as a result. This led Linner et al[28] and later Fobi[22] to describe the importance of placement of a ring around the gastric pouch to define the outlet size, once and for all. Unfortunately restrictive rings and bands gained a very bad reputation during the time of vertical banded gastroplasty, and most surgeons were disinclined to use such a device in the context of gastric bypass because of concern regarding possible ring/band erosion. Our experience and that of Fobi was however quite different. Ring erosion is a very infrequent occurrence and in our experience of over 1400 operations has never been seen except in the context of gastric ulceration. Further, again in our experience, gastric ulceration is largely related to staple-line disruption (gastro-gastric fistula)[17,21] or NSAID usage. As practiced in the setting of Fobi Pouch gastric bypass we have never seen a ring erosion in over 1000 operations carried out since 1997. Recent reports from others concur with this experience[29]. We however do emphasise that the ring should fit loosely around the gastric pouch rather than create a constriction around the pouch. This is likely to be the defining difference between the ring of the Fobi Pouch and the ring/band placed on a gastroplasty, which undoubtedly was more prone to erosion. Placement of a ring/band around the gastric pouch certainly contributes to the restriction and the nature of food that can be tolerated. The recommended ring size in the Fobi Pouch gastric bypass setting is 6.5 cm length[30] which gives an outside maximum diameter of the pouch of 1.9 cm. That such a ring should sit loosely around the gastric pouch as shown in Figure 4 demonstrates the narrow nature of the pouch formed.
Figure 4 Operative photo showing the loose placement of a 6.
5 cm silastic ring proximal to the gastro-jejunal anastomosis.
There is now a growing recognition of the role played by the ring in weight loss maintenance[29-33], and surgeons undertaking gastric bypass are being encouraged to place a ring for this reason. In a non randomised study recently reported by Awad et al[29] they compared the weight loss in their hands of 260 patients who underwent gastric bypass with a band and 218 patients who underwent the same gastric bypass but without a band. Percentage excess weight loss was equivalent for the first 24-36 mo and thereafter the %EWL was superior in the banded group. Weight loss was maintained through to 10 years in the banded group and by 7 years there was almost a 20% EWL difference between the banded and non banded groups, which difference was them maintained.
LENGTH OF ROUX LOOP
There remains a view held by some that the length of the biliary and alimentary limbs of the Roux loop are of importance. There is little evidence that this is the case. It is true that the length of the alimentary limb may determine the degree of malabsorption that occurs following the operation, however, unless this is extreme the degree to which this augments weight loss, and the degree to which such a contribution is durable is highly variable and unpredictable[34,35] because of adaptation occurring within the common channel of small bowel. In our opinion the length of the biliary limb should simply be determined by the convenience of the point for mesenteric division, such that the loop passes without tension to be anastomosed to the stomach. This is commonly in the vicinity of 50-60 cm from the duodeno-jejunal flexure. There is little reason to extend the length of the alimentary limb beyond 75 cm, which is quite sufficient to prevent bilio-pancreatic secretion reflux into the gastric pouch. Lengths in excess of half the small bowel, risk conferring troublesome diarrhoea, and should not be necessary in the vast majority of circumstances.
COMMENTARY ON LAPAROSCOPIC GASTRIC BYPASS
The ability to undertake gastric bypass laparoscopically, as opposed to by open surgery, clearly confers advantage in terms of hospital stay and recovery time. This has been well shown in a number of comparative studies which have only ever examined short-medium term weight loss, recovery time and complications. While rates of serious complications are similar, the specifics of the complications are different and weight loss in the first 1-5 years has been comparable[36-38]. However, the more important and meaningful comparison needs to be between standard gastric bypass (laparoscopic or open) and Fobi Pouch gastric bypass, as was made in the systematic review of O’Brien et al[10]. While randomised data on this point is scant, both this[39] and non-randomised data certainly point to the advantage of including a ring[29].
We believe that the majority of surgeons performing laparoscopic gastric bypass make the gastric pouch too short, too wide and without a ring to dictate the size of the gastric outlet. This lends itself perfectly to pouch dilatation, outlet enlargement and enhanced gastric emptying. The way in which laparoscopic staplers are used to create the pouch and particularly the way in which the anastomosis is performed using staplers (circular or linear)[25] is in large measure to blame. A long narrow pouch can certainly be performed with existing staplers, but an anastomosis between the Roux loop and a gastric pouch of no more than 1cm diameter dictates that a hand-sewn anastomosis be performed. This is a challenge for many surgeons, but should be regarded as the goal. A ring can undoubtedly be added with relative ease, particularly using the now commercially available devices such as the GaBP Ring®[33].
SUMMARY OF RECOMMENDATIONS
The superiority of the medium and long-term weight loss of the Fobi Pouch gastric bypass over more standard forms of gastric bypass, whether performed open or laparoscopically, provides the basis for the opinion and hypothesis expressed in this paper. We propose that for optimum reliability and sustainability in terms of weight loss a gastric bypass should include the following: (1) a vertical pouch of approximately 1 cm diameter, approximately 7-8 cm in length, originating close to the angle of His; (2) a transected stomach with interposition of a small bowel loop between staple lines; (3) a loose fitting silastic rubber ring of 6.5 cm circumference placed approximately 1cm proximal to the gastro-jejunal anastomosis; and (4) an alimentary limb length to the Roux loop of 75-100 cm.
At the present time, few if any of these suggestions have been reliably settled through thorough randomised prospective study. However, support for the comments from uncontrolled clinical experience and the systematic review reported by O’Brien et al[10] in 2006 does exist. It is common to see significant late weight regain after standard gastric bypass as demonstrated in the systematic review of O’Brien et al[10] and unfortunately some individuals regain all the weight they lost. This is most often attributable to pouch enlargement or rapid gastric pouch emptying, neither of which seem to occur after Fobi Pouch Gastric bypass. In my own experience of over 1000 Fobi Pouch gastric bypass operations, performed since 1997, we have never seen significant weight regain from technical failure due to pouch enlargement, gastro-gastric fistula or gastric outlet enlargement. We have never seen a single individual regain all of the weight lost, and we have never performed a revision procedure because of inadequate weight loss. The only individuals who have regained significant weight (usually no more than 50% of expected weight loss), have done so because of poor food choices or grazing throughout the day. This number represents 5%-10% of those who have undergone the surgery. With the 6.5 cm circumference silastic ring, we have reported removal of the ring in 1.8% of instances, because of severe intolerance to food with very frequent and troublesome regurgitation[30]. When this has been done, some weight regain has been universal, and longer term control of weight has been compromised.
CONCLUSION
A great deal has been learned by those practicing bariatric surgery from the early days of gastric bypass. The challenge for today’s surgeons is to embrace these lessons and test them, if they feel so inclined. There need not be such a thing as a technical failure following gastric bypass - but there will continue to be, if we ignore the lessons learned from the past. Gastric bypass is a thoroughly reliable procedure, when performed well. The success and durability of the weight loss achieved depends on the details of the operation performed. Not all gastric bypasses are the same - make your next one, a good one!
P- Reviewer: Aoyagi K, Baba H, Chello M S- Editor: Wen LL L- Editor: A E- Editor: Wang CH