Published online Jul 28, 2013. doi: 10.5412/wjsp.v3.i2.8
Revised: April 25, 2013
Accepted: June 5, 2013
Published online: July 28, 2013
Processing time: 146 Days and 3.7 Hours
AIM: To evaluate our experience and surgical technique of laparoscopic appendectomy via reduced port surgery (LARPS).
METHODS: Sixteen patients (8 men and 8 women; median age: 31.0 years) who underwent LARPS between November 2009 and May 2012 were included in the present study. We performed LARPS, in which access devices were inserted through an umbilical skin incision with 1 additional skin incision in the left lower abdomen. After setting access devices, pneumoperitoneum was maintained at 10 mmHg using CO2 and a 3 mm trocar was positioned (or direct puncture was performed by the Endo Relief system) under laparoscopic guidance. The mesoappendix was dissected using an ultrasonically activated device. After mesoappendix dissection, ligation was performed near the appendix base and the appendix was dissected using an ultrasonically activated device. The appendix was then removed. At the end of surgery, we administered local anesthesia with ropivacaine 1% (10 mL) for the skin incisions. The outcomes were evaluated in terms of operation time, intraoperative blood loss, length of postoperative hospital stay and surgical complications.
RESULTS: Our surgical procedure allowed operators to use instruments as in conventional laparoscopic appendectomy. The basic principle of triangulation of instrumentation was maintained to some degree. LARPS was performed in 9 patients with catarrhal appendicitis, 5 with phlegmonous appendicitis, and 2 with gangrenous appendicitis. The median surgery time was 60 min and the median intraoperative blood loss was 1.2 mL. The median length of postoperative hospitalization was 4 d. There were no conversions to open surgery, no operation-related complications or mortality.
CONCLUSION: Our experience and surgical technique suggest that LARPS is a safe and feasible procedure for patients with appendicitis.
Core tip: Our experience and surgical technique suggest that laparoscopic appendectomy via reduced port surgery is a safe and feasible procedure for patients with appendicitis. Although the present study showed that this procedure offers cosmetic advantages and technical simplicity, the effectiveness and feasibility of this method should be assessed in randomized trials.
- Citation: Mori S, Baba K, Yanagita S, Kita Y, Maemura K, Mataki Y, Uchikado Y, Okumura H, Nakajyo A, Natsugoe S, Takao S, Aridome K. Reduced port surgery for appendectomy: Early experience and surgical technique. World J Surg Proced 2013; 3(2): 8-12
- URL: https://www.wjgnet.com/2219-2832/full/v3/i2/8.htm
- DOI: https://dx.doi.org/10.5412/wjsp.v3.i2.8
Laparoscopic appendectomy has become a commonly performed surgical procedure worldwide. It is safe, effective and minimally invasive. Compared with open appendectomy, laparoscopic appendectomy is associated with less overall morbidity, an acceptable operation time, a lower incidence of superficial surgical site infection, and a shorter hospital stay[1-5]. Single-incision laparoscopic surgery is a novel technique that may be performed when considering minimally invasive surgery and desiring a cosmetic benefit. Recently, single-incision laparoscopic appendectomy (SILA) has become a major focus of study[6-12] and prospective randomized studies were performed to compare the outcome of SILA and conventional laparoscopic appendectomy (CLA)[13-16]. The results showed the SILA approach to be similar in terms of perioperative outcomes. In the SILA group, wound cosmesis and satisfaction scores were better; however, the operative time was longer and worse pain scores were demonstrated upon exertion.
In the present study, we describe our experience and surgical technique in patients who underwent laparoscopic appendectomy via reduced port surgery (LARPS).
Sixteen patients (male, n = 8; female, n = 8; mean age: 31.0 years; range, 16-49 years) who were admitted to our hospital from November 2009 to May 2012 were included in this study. Patients were excluded if they had high dense adhesions, perforated appendicitis, acute appendicitis with abscess, or American Society Anesthesiologist scores (ASA) of 4 or 5. All patients had appendicitis and underwent LARPS. Nine patients had catarrhal appendicitis, 5 had phlegmonous appendicitis, and 2 had gangrenous appendicitis.
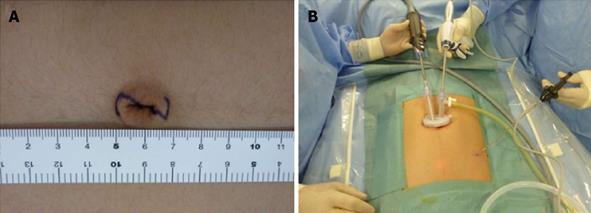
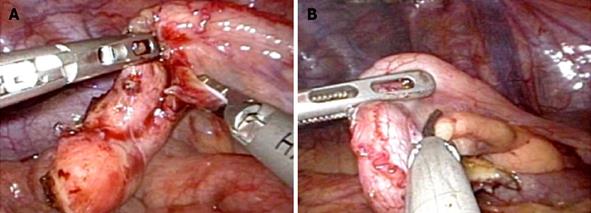
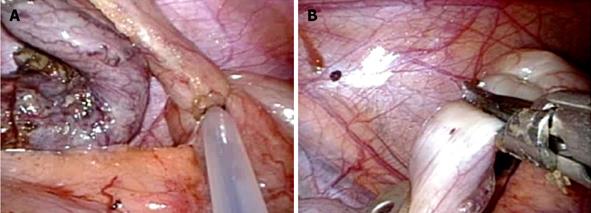
All patients underwent general anesthesia and were placed in the supine position. The operator and assistant stood on the left side of the patient. The skin was cut along a Z-line marked in the umbilical region (Figure 1A). We used an EZ-access with a Lap-Protector (Hakko Medical Inc., Chikuma, Japan) for the umbilical access device and an Endo Relief (Hope Denshi Co., Kamagaya, Japan) which has a 2.4 mm shaft with a 5 mm diameter head. Two 5 mm trocars were placed through the EZ-access for a 5 mm laparoscope and 5 mm instrument (Figure 1B). After setting the EZ-access with the Lap-Protector, pneumoperitoneum was maintained at 10 mmHg using CO2 and a 3 mm trocar was positioned (or direct puncture was performed by the Endo Relief system) under laparoscopic guidance into the left lower abdomen (Figure 1B). Laparoscopic instruments were inserted and the mesoappendix was dissected using an ultrasonically activated device (Figure 2). After mesoappendix dissection, ligation was performed near the appendix base using 1 endoloop (Figure 3A) (Ethicon, PDS 0)[17] and the appendix was dissected using an ultrasonically activated device (Figure 3B). The appendix was then removed through the Lap-Protector without contacting the abdominal wall. We administered local anesthesia with ropivacaine 1% (10 mL) for the skin incisions at the end of surgery.
Intraoperative information about the surgical duration, complications and blood loss was collected. Postoperative data comprised of complications, length of postoperative hospital stay, and pathological findings. We also conducted the interview post operatively about whether the operative scars were excellent, not bad or bad.
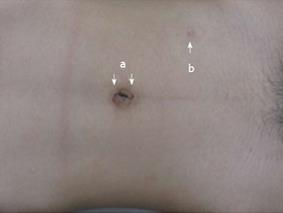
Our surgical procedure allowed operators to use instruments as in conventional laparoscopic appendectomy and the basic principle of triangulation of instrumentation was maintained to some degree. The umbilical and another skin incision positioned on the left lower abdomen shrunk in the wrinkle (Figure 4). The mean surgical duration was 60 min (range, 35-150 min) and the mean amount of blood loss was 1 mL (range, 0-20 mL). The median hospital stay after surgery was 4 d (range, 3-7 d). No intraoperative complications developed in this series. One patient received 1 additional port because of dense adhesions; however, there were no conversions to open surgery. All patients were free of complications such as leakage of the appendix stump, bleeding, intra-abdominal abscesses and small bowel obstruction. There was no intraoperative or postoperative mortality. Additionally, 9, 5 and 2 patients had catarrhal, phlegmonous and gangrenous appendicitis, respectively. For our interview about the operative scars, all patients answered that the scars were excellent.
Recently, SILA has been reported to demonstrate perioperative outcomes and safety similar to that shown by CLA[15,16] as a result of innovation and technological advances. It has been suggested that SILA results in better cosmetic outcomes than CLA[9-11]. However, SILA resulted in worse pain scores upon exertion, required a higher dosage of intravenous analgesics, and involved a longer operative time compared with CLA[15,16]. We performed LARPS to treat appendicitis by cutting the skin over the umbilicus with a 2 cm long Z-incision, inserting 2 trocars into the incision and placing another 3 mm trocar (or performing direct puncture by the Endo Relief system) into the left lower abdomen to assist the surgeon. The assisting surgeon usually operates the camera on left side of the patients. Because the appendix was adherent near the lower peritoneal midline, the assisting surgeon stood opposite the operator at the beginning of operation (Figure 1B). The skin incisions were almost hidden after surgery and most patients expressed satisfaction with the virtually scarless outcome. The potential advantages of our procedure are a well-balanced cosmetic outcome and technical simplicity for laparoscopic appendectomy.
We performed LARPS, a novel surgical procedure, to treat appendicitis. This method yielded good short-term outcomes, including good cosmetic results and a technically simplified SILA. Generally speaking, single-incision laparoscopic surgery is somewhat ergonomically challenging to the operator because the basic principle of triangulation of instrumentation, which is applicable to conventional laparoscopic surgery, is lost to some degree and instruments often interfere with one another. Our surgical procedure allows operators to use instruments as in CLA. Both the triangulation of instrumentation and eye-hand and hand-hand coordination are improved, resulting in less interference among instruments compared with SILA. We needed to insert an additional trocar into 1 patient with gangrenous acute appendicitis because of dense adhesions. The duration of surgery and volume of blood lost were 150 min and 20 mL, respectively. This patient did not develop any intraoperative or postoperative complications.
In our procedure, another 3 mm skin incision to assist the surgeon was positioned on the left lower abdomen. The skin incision shrunk in the wrinkle, resulting in a virtually scarless outcome. Positioning one instrument upon the left lower abdomen allowed the operator to maintain eye-hand and hand-hand coordination, maintain the basic principle of triangulation of instrumentation, and avoid interference of instruments. If drain placement was required, the drain could be inserted into the skin incision on the left lower abdomen. In this series, 2 patients required drain placement in the pouch of Douglas because of gangrenous acute appendicitis.
The specimens could be removed through the umbilical skin incision protected by the Lap-Protector. After removing the specimens, pneumoperitoneum was easily maintained using the EZ-access. After washing the intraperitoneal cavity, we removed the Endo Relief or trocar under laparoscopic guidance, closed the peritoneum and fascia at the umbilicus, and administered local anesthesia with ropivacaine 1% (10 mL) for the skin incisions. No patients required a higher dosage of intravenous analgesics postoperatively; the only additional analgesia comprised of oral non-steroidal anti-inflammatory drugs (NSAIDs).
Although our experience was limited to 16 patients, none experienced any intraoperative or postoperative complications, the operative time and length of postoperative hospital stay were acceptable, and the postoperative pain upon exertion was controlled with occasional NSAIDs.
In conclusion, our experience and surgical technique suggest that LARPS is a safe and feasible procedure for patients with appendicitis. Although the present study showed that this procedure offers cosmetic advantages and technical simplicity, the effectiveness and feasibility of this method should be assessed in randomized trials.
The authors deeply appreciate the contributions of all colleagues and patients who participated in this study and thank the editors and reviewers for their help with this manuscript.
Laparoscopic appendectomy has become a commonly performed surgical procedure worldwide. It is safe, effective and minimally invasive. Compared with open appendectomy, laparoscopic appendectomy is associated with less overall morbidity, an acceptable operation time, a lower incidence of superficial surgical site infection, and a shorter hospital stay.
It has been suggested that SILA results in better cosmetic outcomes than conventional laparoscopic appendectomy (CLA). However, SILA resulted in worse pain scores upon exertion, required a higher dosage of intravenous analgesics, and involved a longer operative time compared with CLA.
The authors’ experience and surgical technique suggest that laparoscopic appendectomy via reduced port surgery (LARPS) is a safe and feasible procedure for patients with appendicitis.
The authors performed LARPS, a novel surgical procedure, to treat appendicitis. This method yielded good short-term outcomes, including good cosmetic results and a technically simplified SILA.
The paper flows straight through and the authors present their experience well. Although the number of subjects is very small, they present the data as safe and feasible, recommending randomized trials to show any benefit. This is appropriate.
P- Reviewers Mintz Y, Snyder B S- Editor Zhai HH L- Editor Roemmele A E- Editor Lu YJ
| 1. | Moazzez A, Mason RJ, Katkhouda N. Thirty-day outcomes of laparoscopic versus open appendectomy in elderly using ACS/NSQIP database. Surg Endosc. 2013;27:1061-1071. [PubMed] |
| 2. | Mason RJ, Moazzez A, Moroney JR, Katkhouda N. Laparoscopic vs open appendectomy in obese patients: outcomes using the American College of Surgeons National Surgical Quality Improvement Program database. J Am Coll Surg. 2012;215:88-99; discussion 99-100. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 32] [Article Influence: 2.5] [Reference Citation Analysis (2)] |
| 3. | Yeh CC, Hsieh CH, Liao CC, Su LT, Wang YC, Li TC. Diabetes mellitus and cerebrovascular disease as independent determinants for increased hospital costs and length of stay in open appendectomy in comparison with laparoscopic appendectomy: a nationwide cohort study. Am Surg. 2012;78:329-334. [PubMed] |
| 4. | Yaghoubian A, Kaji AH, Lee SL. Laparoscopic versus open appendectomy: outcomes analysis. Am Surg. 2012;78:1083-1086. [PubMed] |
| 5. | Katsuno G, Nagakari K, Yoshikawa S, Sugiyama K, Fukunaga M. Laparoscopic appendectomy for complicated appendicitis: a comparison with open appendectomy. World J Surg. 2009;33:208-214. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 55] [Cited by in RCA: 52] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 6. | Feinberg EJ, O’Connor DJ, Feinberg ML, Vemulapalli P, Camacho D. Single-incision laparoscopic appendectomy: an early experience. Am Surg. 2011;77:286-289. [PubMed] |
| 7. | Chouillard E, Dache A, Torcivia A, Helmy N, Ruseykin I, Gumbs A. Single-incision laparoscopic appendectomy for acute appendicitis: a preliminary experience. Surg Endosc. 2010;24:1861-1865. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 40] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 8. | Chow A, Purkayastha S, Nehme J, Darzi LA, Paraskeva P. Single incision laparoscopic surgery for appendicectomy: a retrospective comparative analysis. Surg Endosc. 2010;24:2567-2574. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 59] [Cited by in RCA: 58] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 9. | Kim HJ, Lee JI, Lee YS, Lee IK, Park JH, Lee SK, Kang WK, Cho HM, You YK, Oh ST. Single-port transumbilical laparoscopic appendectomy: 43 consecutive cases. Surg Endosc. 2010;24:2765-2769. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53] [Cited by in RCA: 50] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 10. | Chiu CG, Nguyen NH, Bloom SW. Single-incision laparoscopic appendectomy using conventional instruments: an initial experience using a novel technique. Surg Endosc. 2011;25:1153-1159. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 25] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 11. | Cho MS, Min BS, Hong YK, Lee WJ. Single-site versus conventional laparoscopic appendectomy: comparison of short-term operative outcomes. Surg Endosc. 2011;25:36-40. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 50] [Cited by in RCA: 48] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 12. | Amos SE, Shuo-Dong W, Fan Y, Tian Y, Chen CC. Single-incision versus conventional three-incision laparoscopic appendectomy: a single centre experience. Surg Today. 2012;42:542-546. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 21] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 13. | Perez EA, Piper H, Burkhalter LS, Fischer AC. Single-incision laparoscopic surgery in children: a randomized control trial of acute appendicitis. Surg Endosc. 2013;27:1367-1371. [PubMed] |
| 14. | St Peter SD, Adibe OO, Juang D, Sharp SW, Garey CL, Laituri CA, Murphy JP, Andrews WS, Sharp RJ, Snyder CL. Single incision versus standard 3-port laparoscopic appendectomy: a prospective randomized trial. Ann Surg. 2011;254:586-590. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 173] [Cited by in RCA: 166] [Article Influence: 11.9] [Reference Citation Analysis (0)] |
| 15. | Teoh AY, Chiu PW, Wong TC, Poon MC, Wong SK, Leong HT, Lai PB, Ng EK. A double-blinded randomized controlled trial of laparoendoscopic single-site access versus conventional 3-port appendectomy. Ann Surg. 2012;256:909-914. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 76] [Cited by in RCA: 84] [Article Influence: 7.0] [Reference Citation Analysis (0)] |
| 16. | Lee WS, Choi ST, Lee JN, Kim KK, Park YH, Lee WK, Baek JH, Lee TH. Single-port laparoscopic appendectomy versus conventional laparoscopic appendectomy: a prospective randomized controlled study. Ann Surg. 2013;257:214-218. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 77] [Cited by in RCA: 82] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 17. | Beldi G, Muggli K, Helbling C, Schlumpf R. Laparoscopic appendectomy using endoloops: a prospective, randomized clinical trial. Surg Endosc. 2004;18:749-750. [PubMed] |