Published online Mar 28, 2013. doi: 10.5412/wjsp.v3.i1.1
Revised: September 24, 2012
Accepted: November 17, 2012
Published online: March 28, 2013
We report a rare case of malignant schwannoma of the brachial plexus treated during a surgical campaign aimed at the poorest communities in the Cuzco region of Peru. A Peruvian 40-year-old-female from a mountain community presented with a mass on the lateral side of her left supraclavicular space. No imaging tools were available during this surgical campaign and so a biopsy of the tumor was carried out. Histopathological examination revealed it to be a low grade malignant schwannoma. A nerve enucleation of the tumor was chosen as neither chemotherapy nor radiotherapy was available. The tumour was a firm mass 4 cm x 3 cm x 2 cm in size. After excision of the lesion the patient presented neurological sequelae (deltoid, bicep, and tricep weakness) but her condition improved over the next 3 years. We report this case of malignant schwannoma of the brachial plexus as its incidence is very rare (the reported incidence is 0.001%) and because of its challenging treatment in poor healthcare conditions.
- Citation: Benevello C, Sommacale D, Palladino E, Bildea A, Tres I, Volpin E. A rare case of malignant schwannoma of the brachial plexus. World J Surg Proced 2013; 3(1): 1-3
- URL: https://www.wjgnet.com/2219-2832/full/v3/i1/1.htm
- DOI: https://dx.doi.org/10.5412/wjsp.v3.i1.1
Peripheral nerve sheath tumors (PNST) include the schwannoma, the most common tumor arising from peripheral nerves, and neurofibromas. Malignant PNST (MPNST), also known as neurogenic sarcomas, include schwannomas and neurofibrosarcomas which are indistinguishable when viewed with histological techniques. MPNST account for 5% to 10%[1] of soft tissue sarcomas, and have an incidence of 0.001% in the general population[2]. MPNST develop 4% to 10% in neurofibromatosis type 1 (NF1), an autosomical dominant neurocutaneous disorder with an estimated incidence of 1 in 2500 births.
Peripheral nerve tumors of the upper limb are very rare; they represent less than 5% of all tumors in this region[2]. Solitary benign peripheral nerve schwannomas are the most common. These can cause nerves to exhibit different clinical features depending on type, site of lesion and their histopatologic pattern. Benign schwannomas are generally solitary, oval, capsulated and elastic. Malignant tumors are very rare with rapid growth, invasion of the nerve and neurological deficit[3].
Magnetic resonance imaging and ultrasound can localize the tumor but definitive diagnosis is possible only with a histopatological exam.
Although rare, MPNST is one of the most aggressive tumors of the head and neck area. Complete surgical removal is the main treatment and most important prognostic factor. Adjuvant radiotherapy should be used to assist surgical excision in local control[4]. The role of adjuvant chemotherapy remains controversial[4].
Schwannomas originating from the brachial plexus are extremely rare and to our knowledge those manifesting preoperatively as a large lesion have rarely been reported. We report a case of malignant schwannoma of brachial plexus manifesting as an enlarging mass in the supraclavicular space, treated during a surgical campaign in difficult healthcare conditions.
A 40-year-old woman presenting a mass of the left supraclavicular fossa, was referred to us during a surgical campaign in October 2008 aimed at the poorest communities in the Cuzco region of Peru. She showed no signs of any neurological disturbances to the left upper limb. In her past history there was no significant disease and physical examination showed no abnormalities. Radiology was unavailable in our hospital so we performed a surgical biopsy. The excised section was gray-white to gray-yellow, soft and fleshy in appearance. Pathologically it was diagnosed as a low-grade malignant schwannoma composed of two types of regions known as Antoni A and B regions; we decided to remove the mass completely.
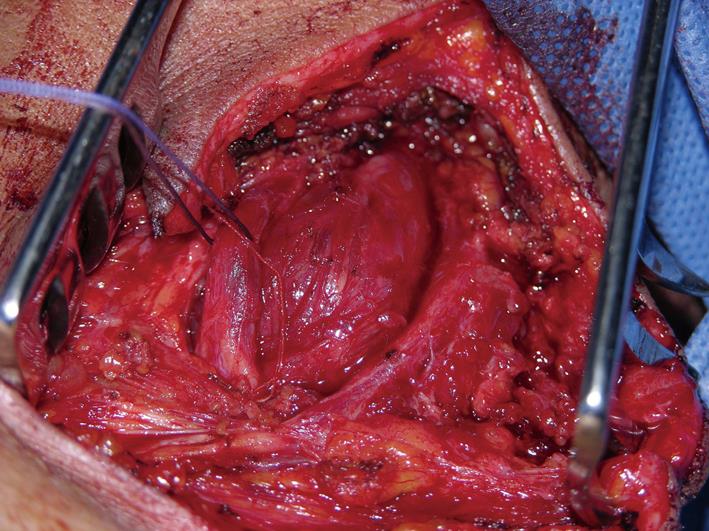
An anterior supraclavicular approach was used. After the small skin incision, we displaced the sternocleidomastoideus muscle and proceeded with the complete dissection of this solid vascularised mass arising from the medial cord (Figure 1). The nerves were enlarged by the tumour. Finally, while trying to preserve the nervous structures, the mass was removed (Figure 2).
The histopathology of the tumour was consistent with a low grade malignant schwannoma.
After surgery the patient had motor disturbances on the left upper limb, particularly on the biceps muscle, she kept deltoid and distal finger movements and she retained sensation. Radiotherapy and chemotherapy weren’t available in this clinical centre and we couldn’t follow the patient for a possible period of rehabilitation. When she returned to the medical centre, 3 years later, she was improved, without any further symptoms and, at physical examination, showed no sign of relapse.
The aetiology of PNST is usually unknown. However, several hereditary disorders are known to predispose to benign and MPNSTs, notably NF1 and NF2[5], both of which are inherited in an autosomal dominant fashion.
All ages and both sexes may be affected by PNSTs. Sporadic MPNSTs are most common between 40 and 50 years of age, while those occurring in the setting of NF1 are diagnosed some 10 years earlier. In total, MPNSTs account for 5%-10% of all soft tissue sarcomas.
Schwannomas are encapsulated spindle cell tumors with distinct Antoni A and B components, hyaline vessel walls, and nuclear palisading[6].
Neurofibromas are unencapsulated tumors composed of spindle cells dispersed in fibromyxoid stroma.
Perineuriomas may arise in soft tissues or within nerves, and are composed of cells with elongated bipolar cytoplasmic processes frequently arranged in whorls or a storiform pattern.
MPNSTs typically are characterized by the presence of pale spindle cells often arranged in fascicles with alternating cellular and more myxoid areas. Most MPNSTs arise from Schwann cells, but the possibility remains that some arise from nerve sheath cells other than the Schwann cells. Approximately two-thirds of all MPNSTs are associated with neurofibromas[3].
In the literature survival rate is estimated to be 48% at 5 years and prognostic factors are: tumour localization, size, grade of malignancy and radical surgical treatment[7].
Benign PNSTs rarely recur after surgery. MPNST, on the other hand, are often highly aggressive tumors, and more than 60% of patients die of the disease[8].
In the treatment of malignant schwannoma, surgical removal is the first choice[9]; however the resecting margin of the tumor is always difficult and controversial[10]. Sometimes, in the case of malignant lesions, only the sacrifice of involved nerves allows complete resection. Aggressive surgical intervention and radiotherapy can result in good survival[11]. In our case the pathology result reported a low grade malignant lesion and for this reason we decided to resect the tumor, even if we couldn’t perform any additional necessary treatment, principally radiotherapy. Our patient showed signs of neurological disorder postoperatively as she presented deltoid, bicep, and tricep weakness. Unfortunately we couldn’t follow her with further therapy, but she came back to the medical centre after 3 years and was improved.
In conclusion we experienced an unusual case of malignant schwannoma involving nervous structures of the brachial plexus. We report its difficult treatment in a poor social and cultural context during a surgical campaign and the particular importance of its complete surgical removal in these complicated conditions, even thought no adjuvant treatment was available.
P- Reviewer Bassetto F S- Editor Jiang L L- Editor Hughes D E- Editor Zheng XM
| 1. | Yang T, Rockhill J, Born DE, Sekhar LN. A case of high-grade undifferentiated sarcoma after surgical resection and stereotactic radiosurgery of a vestibular schwannoma. Skull Base. 2010;20:179-183. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 40] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 2. | Puataweepong P, Janwityanujit T, Larbcharoensub N, Dhanachai M. Radiation-induced peripheral malignant nerve sheath tumor arising from vestibular schwannoma after linac-based stereotactic radiation therapy: a case report and review of literatures. Case Rep Med. 2012;2012:648191. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 14] [Cited by in RCA: 23] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 3. | Clarke SE, Kaufmann RA. Nerve tumors. J Hand Surg Am. 2010;35:1520-1522; quiz 1522. [PubMed] |
| 4. | Minovi A, Basten O, Hunter B, Draf W, Bockmühl U. Malignant peripheral nerve sheath tumors of the head and neck: management of 10 cases and literature review. Head Neck. 2007;29:439-445. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 80] [Cited by in RCA: 73] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 5. | Guerrissi JO. Solitary benign schwannomas in major nerve systems of the head and neck. J Craniofac Surg. 2009;20:957-961. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 19] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 6. | Kumar A, Akhtar S. Schwannoma of brachial plexus. Indian J Surg. 2011;73:80-81. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 15] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 7. | Bojsen-Møller M, Myhre-Jensen O. A consecutive series of 30 malignant schwannomas. Survival in relation to clinico-pathological parameters and treatment. Acta Pathol Microbiol Immunol Scand A. 1984;92:147-155. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.0] [Reference Citation Analysis (0)] |
| 8. | Guo A, Liu A, Wei L, Song X. Malignant peripheral nerve sheath tumors: differentiation patterns and immunohistochemical features - a mini-review and our new findings. J Cancer. 2012;3:303-309. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 40] [Cited by in RCA: 57] [Article Influence: 4.4] [Reference Citation Analysis (1)] |
| 9. | Saito S, Suzuki Y. Schwannomatosis affecting all three major nerves in the same upper extremity. J Hand Surg Eur Vol. 2010;35:592-594. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 6] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 10. | Langner E, Del Negro A, Akashi HK, Araújo PP, Tincani AJ, Martins AS. Schwannomas in the head and neck: retrospective analysis of 21 patients and review of the literature. Sao Paulo Med J. 2007;125:220-222. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 49] [Cited by in RCA: 51] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 11. | Lin CT, Huang TW, Nieh S, Lee SC. Treatment of a malignant peripheral nerve sheath tumor. Onkologie. 2009;32:503-505. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 13] [Article Influence: 0.8] [Reference Citation Analysis (0)] |