Published online Mar 24, 2017. doi: 10.5410/wjcu.v6.i1.27
Peer-review started: August 18, 2016
First decision: September 6, 2016
Revised: December 8, 2016
Accepted: December 27, 2016
Article in press: December 29, 2016
Published online: March 24, 2017
Processing time: 197 Days and 8.2 Hours
Seminoma is a germ cell tumour which primarily affects the testes. Seminomas are treated by orchidectomy with usually excellent outcomes. We report the occurrence of a classical seminoma in a 92-year-old man, who is currently the oldest patient with this histology reported in literature. He presented with a painful, swollen testis. Scrotal ultrasound scan revealed a testicular mass. A left inguinal orchidectomy was carried out and histological examination confirmed the diagnosis of a classical seminoma. Further staging by computerised tomography revealed pulmonary lesions suspicious of metastases. The patient declined further treatment in view of his age and co-morbidities.
Core tip: This is the first case in the literature which describes the occurrence of such a tumour in patients over the age of 90 and should raise the index of suspicion for malignant testicular tumours in elderly patients where infectious causes of testicular swellings are by far the most common.
- Citation: Denning C, Tay LJ, Carton J, Attar KH. Classical seminoma in a 92-year-old patient. World J Clin Urol 2017; 6(1): 27-29
- URL: https://www.wjgnet.com/2219-2816/full/v6/i1/27.htm
- DOI: https://dx.doi.org/10.5410/wjcu.v6.i1.27
We would like to introduce the first case in the literature which describes the occurrence of a testicular seminoma in patients over the age of 90 and we hope that this presentation will educate the future doctors to raise the index of suspicion for malignant testicular tumours in elderly patients where infectious causes of testicular swellings are by far the most common.
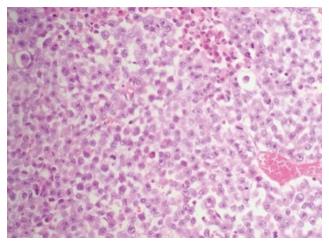
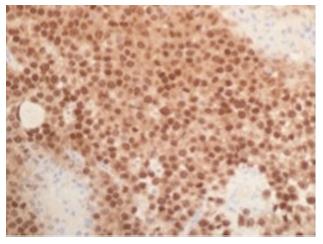
A 92-year-old man presented with a 4 wk history of a left painful swollen scrotal mass, initially to his General Practitioner (GP), and subsequently to the emergency department. His medical history included alcoholic liver disease, oesophageal varices, chronic obstructive airway disease, and a cardiac pacemaker. Scrotal ultrasound scan showed a 4cm heterogeneous vascular testicular mass. Laboratory tests revealed normal levels of serum alpha feta protein (AFP) (2 kU/L) βhCG (< 2 iU/L) and lactate dehydrodgense (LDH) (59 iU/L). Left inguinal orchidectomy was performed in view of the suspicious findings. Macroscopic histopathological examination revealed a well-circumscribed pale grey mass measuring 6.5 cm with central necrosis. Histological sectioning showed sheets of large polygonal cells (Figure 1) which stained positively for Oct-3/4 (Figure 2) and placental alkaline phosphatase (PLAP). These findings were consistent with a diagnosis of classical seminoma with no evidence of intratubular germ cell neoplasia. The tumour had not breached the tunica vaginalis nor involved the spermatic cord. A staging computerised tomography (CT) scan revealed diffuse pulmonary metastases, a collapse fracture of the 12th thoracic vertebra and severe ascites (secondary to chronic liver disease). The patient declined further intervention including oncological input in view of his age and co-morbidities. He died 6 wk later but a post mortem was not carried out.
Testicular cancer is the 16th most common cancer in men in the United Kingdom. It accounts for 1% of all new cases of male cancer. Between 2009 and 2011, 84% of testicular cancer cases were diagnosed in men aged 15-49 years in the United Kingdom; only 6% occurred in patients aged over 60[1]. The incidence of testicular cancer in patients older than 85 is only 2.4 per 100000. Ninety-five percent of testicular tumours are germ cell tumours (GCTs), which includes seminomas (40%-45%) and non-seminomas (55%-60%). GCTs develop from a non-invasive lesion called carcinoma in situ (CIS) of the testis (ITGCN), whose malignant transformation is likely to be influenced by hormones at or after puberty[2]. Seminoma rarely occurs in the adolescent or infant population and the peak age of incidence is between aged 35-39 years with less than 10% being diagnosed after the age of 50[3]. A large study in 2008 revealed an 86-year-old patient with spermatocytic seminoma[4] while a recent case report describes spermatocytic seminoma in a 92-year-old.
Malignant testicular lumps are usually painless, and hence the presentation of seminoma as a painful, swollen testis is unusual[5]. Differential diagnosis in a 92-year-old patient with a painful lump in the testicle would include orchitis, epididymitis, or an abscess, especially if accompanied by symptoms of systemic infection. Testicular torsion is also possible, but this is most common in the second and third decades of life and presents acutely. A persistent processus vaginalis may lead to a hydrocele or an indirect inguinal hernia, and a painful strangulated hernia or hydrocele can present at any age[6]. This is often accompanied by abdominal pain, nausea, and vomiting all of which were absent in this patient.
Serum tumour markers may detect the presence of a testicular seminoma. Serum AFP is not raised in classical seminoma and serum β human Chorionic Gonadotrophin is elevated in only 10%-20%. PLAP is positive in 50% of cases, but has a low sensitivity in smokers, and on its own, has a limited use in the diagnosis of testicular cancer[7]. LDH may be elevated in seminomas and usually has some prognostic value in later stages[8].
It remains uncertain as to why this gentleman only presented to his GP after four weeks. Perhaps a limited awareness of sinister causes of testicular lumps or apprehension to accessing care may have led to this delay. Patient education is of key importance, not only to highlight symptoms to be aware of but also to reiterate the importance of early presentation.
This is a rare case of classical seminoma in a 92-year-old, which we believe is the oldest patient in the literature. Testicular cancer should remain within the differential diagnoses of an elderly patient presenting with a testicular swelling, even if their symptoms are atypical. Education of the general public should highlight the importance of urgent access to medical care when faced with symptoms of a testicular swelling.
Elderly gentleman with a painful, swelling in his left testicle.
Four centimeter tender, scrotal mass in left testicle.
A combination of ultrasound, blood markers and histopathology following orchidectomy allowed us to exclude orchitis, epididymitis, abscess testicular torsion persistent and processus vaginalis to conclude that the cause of these symptoms was a seminoma.
Laboratory tests revealed normal levels of serum alpha feta protein (2 kU/L) βhCG (< 2 iU/L) and lactate dehydrodgense (59 iU/L).
Scrotal ultrasound scan showed a 4 cm heterogeneous vascular testicular mass alongside a staging computerised tomography scan which revealed diffuse pulmonary metastases, a collapse fracture of the 12th thoracic vertebra and severe.
Histological sectioning of the mass showed sheets of large polygonal cells which stained positively for Oct-3/4 and placental alkaline phosphatase which was consistent with seminoma.
The patient declined treatment following orchidectomy.
Please provide other contents related to the case report to help readers better understand the present case.
Testicular cancer should remain within the differential diagnoses of an elderly patient presenting with a testicular swelling, even if their symptoms are atypical. Education of the general public should highlight the importance of urgent access to medical care when faced with symptoms of a testicular swelling.
This is a well written case report on a seminoma in a 92-year-old patient. It is an interesting report, since the vast majority of seminomas occur at a much earlier age.
Manuscript source: Invited manuscript
Specialty Type: Urology and Nephrology
Country of Origin: United Kingdom
Peer-Review Report Classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): B, B, B
Grade D (Fair): 0
Grade E (Poor): 0
P- Reviewer: Crea F, Mehdi I, Romani A S- Editor: Ji FF L- Editor: A E- Editor: Lu YJ
| 1. | Office for National Statistics. Testicular incidence by age. [accessed 2014 Oct 10]. Available from: http://www.ons.gov.uk/ons/search/index.html?newquery=cancer registrations. |
| 2. | Rajpert-De Meyts E, Bartkova J, Samson M, Hoei-Hansen CE, Frydelund-Larsen L, Bartek J, Skakkebaek NE. The emerging phenotype of the testicular carcinoma in situ germ cell. APMIS. 2003;111:267-278; discussion 278-279. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 64] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 3. | Townsend JS, Richardson LC, German RR. Incidence of testicular cancer in the United States, 1999-2004. Am J Mens Health. 2010;4:353-360. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 24] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 4. | Berney DM, Warren AY, Verma M, Kudahetti S, Robson JM, Williams MW, Neal DE, Powles T, Shamash J, Oliver RT. Malignant germ cell tumours in the elderly: a histopathological review of 50 cases in men aged 60 years or over. Mod Pathol. 2008;21:54-59. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 32] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 5. | Horwich A, Shipley J, Huddart R. Testicular germ-cell cancer. Lancet. 2006;367:754-765. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 298] [Cited by in RCA: 272] [Article Influence: 14.3] [Reference Citation Analysis (0)] |
| 6. | Kraft BM, Kolb H, Kuckuk B, Haaga S, Leibl BJ, Kraft K, Bittner R. Diagnosis and classification of inguinal hernias. Surg Endosc. 2003;17:2021-2024. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 34] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 7. | Doherty AP, Bower M, Christmas TJ. The role of tumour markers in the diagnosis and treatment of testicular germ cell cancers. Br J Urol. 1997;79:247-252. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 24] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 8. | Mencel PJ, Motzer RJ, Mazumdar M, Vlamis V, Bajorin DF, Bosl GJ. Advanced seminoma: treatment results, survival, and prognostic factors in 142 patients. J Clin Oncol. 1994;12:120-126. [PubMed] |