Peer-review started: April 8, 2016
First decision: July 14, 2016
Revised: November 7, 2016
Accepted: December 27, 2016
Article in press: December 29, 2016
Published online: March 24, 2017
Processing time: 330 Days and 14.7 Hours
Upper tract urothelial cell carcinoma (UTUCC), formerly known as transitional cell carcinoma of the upper urinary tract, is a rare oncologic disease in Western countries. Thus its disease process and its management are not as well defined as other urologic cancers. We are reviewing the current evidence based literature available to develop a plan for the treatment of UTUCC. A PubMed search was completed using the key words “upper tract urothelial cell carcinoma”, “epidemiology”, “risk factor”, “treatment” and “prognosis”. Six hundred fifty two articles were found. We narrowed our search to articles published between January 2004 and June 2016 for a more contemporary review of the topic. Four hundred seventy articles were then available for review. Further detailed search was performed for relevance on the topic and hundred one articles were selected for the review. Many risk factors have been found to be associated with the development of UTUCC, including tobacco use. Patients are often asymptomatic and may only present with microscopic or gross hematuria. Tumor grade and stage are pivotal in determining the treatment options for UTUCC. Advancements in endoscopic techniques have aided in the diagnosis, grading and treatment of this disease. Treatment options include topical therapy, with combinations of methotrexate, vinblastine, doxorubicin and cisplatin or gemcitibine or cisplatin, endoscopic resection, segmental ureterectomy and ureteral implantation, and nephroureterectomy, including bladder cuff. Treatment recommendations depend on tumor grade and stage, renal function, tumor location and the patient’s prognosis. There are currently no tissue or blood-based biomarkers available to accurately monitor the disease. Further studies of gene expression and biomarkers may hopefully improve the management of this disease. Although rare in many countries, UTUCC is becoming more prevalent due to exposure to carcinogenic herbal remedies and other identifiable risk factors. Numerous treatment modalities, both surgical and chemotherapeutic, have been utilized to treat both low and high grade UTUCC tumors. Additional clinical trials are necessary to further develop methods for screening, treatment, and surveillance to improve management.
Core tip: To review the current literature on upper tract urothelial cell carcinoma (UTUCC) and provide a contemporary management plan for treatment based on best available evidence. Large randomized controlled trials are lacking in UTUCC due to the fortunately rare occurrence of the disease. Treatment recommendations for the primary lesion, imaging, and follow-up in this review are based on the stage and grade of the tumor. Early diagnosis and aggressive treatment remains the mainstay of therapy for UTUCC.
- Citation: Choi K, McCafferty R, Deem S. Contemporary management of upper tract urothelial cell carcinoma. World J Clin Urol 2017; 6(1): 1-9
- URL: https://www.wjgnet.com/2219-2816/full/v6/i1/1.htm
- DOI: https://dx.doi.org/10.5410/wjcu.v6.i1.1
Upper tract urothelial cell carcinoma (UTUCC) accounts for 95% of upper tract carcinoma, with the remaining types being squamous cell carcinoma and adenocarcinoma[1]. Although UTUCC is a rare disease in the West, with an incidence of approximately 40000 cases per year, the incidence has risen in recent years. It is more common and the incidence has risen quickly in Asian countries, especially Taiwan, along with the Balkan regions[2].
UTUCC shares a similar embryologic origin as the bladder, both being derived from the urothelium. But due to anatomic, biological, and molecular differences between upper tract urothelial carcinoma and bladder cancer, they have been referred to as “disparate twin” diseases[2,3]. Accurate local surgical staging and subsequent clinical staging (TNM) is important to help standardize treatment planning. Modern management of UTUCC includes chemotherapy, endoscopic procedures, and nephroureterectomy. We will review the epidemiology, risk factors, classification, diagnosis, staging and medical and surgical treatments of UTUCC.
Upper tract urothelial cell cancer can be found with higher incidence in Balkan regions, and most recently in certain Asian countries especially in Taiwan[2,4,5].
Upper tract urothelial cell cancers are most commonly diagnosed later in life, mostly in the eighth decade[6]. However, it should also be considered in younger populations, especially in patients with exposure to aristolochic acid (AA) plants, which is commonly used for weight loss in Asian countries. It is a very uncommon disease, with an incidence of less than 1 case per 40000[2]. It makes up 5% of all urothelial tumors and 5% to 7% of all renal tumors[6]. Men are twice as likely to have UTUCC, compared to women[7]. Although low in incidence, UTUCC is very aggressive, as many patients are asymptomatic and tend to present later with advanced stage disease, often with metastasis. A thorough understanding of this disease is pivotal in successful diagnosis and treatment[8].
The most well known risk factor for UTUCC is aristolochic acid plants, more commonly used in Balkan regions and in Asian countries, especially in Taiwan[4,9-12]. Balkan endemic nephropathy, associated with ingesting the aristolochic acid plants, can lead to renal failure and increased risk of UTUCC. In addition to increased exposure to aristolochic acid, Balkan populations are also known to have genetic and hereditary predisposition to UTUCC. Other risk factors are microsatellite instability and lynch syndrome type II[13-16].
Other risk factors for UTUCC are similar to bladder urothelial cell carcinoma, with the most common risk factor being cigarette smoking[7,17,18]. Tobacco use is found to increase the relative risk exposure from 2.5 to 7[19]. Occupational exposures to chemicals such as petrochemical and plastic industries, ink solvents, coals, asphalt and aniline dye products are shared risk factors between UTUCC and bladder UCC[20,21]. Newly identified risk factors associated with UTUCC include inverted papilloma which are found in the bladder[22].
UTUCC can be associated with bladder urothelial cell carcinoma but occurs in less than 5%, although nearly 25% in patients with carcinoma in situ (CIS). Environmental exposures unique to upper tract tumors include Blackfoot disease, Artesian well water, weight-reducing pills, well water, arsenic, organic chlorides, and Ergot alkaloids[5,23]. Phenacetin-based analgesics and cyclophosphamide have also been found to be causative agents in UTUCC.
UTUCC has been associated with significant delays in presentation, as many cases are asymptomatic. However, these cancers tend to be very aggressive once they present. Typically, it presents with microscopic or gross hematuria. Flank pain can be present in up to 30% of patients. This is often attributed to urinary tract obstruction by the tumor.
The most common locations for this tumor are the renal pelvis and less often the ureter. Ureteral tumors are located most commonly in the lower ureter and least commonly in the upper ureter. Incidence based on location is as follows: distal ureter in 70%, mid ureter in 25% and then proximal ureter in 5%[24-26].
Contrasted imaging of the collecting systems and ureters with CT urogram or retropyelogram is necessary along with cystoscopy to diagnose UTUCC. UTUCC is most frequently identified as an obstruction or filling defect, often known as the “goblet sign” when found in the ureter (Figure 1). CT urogram is the gold standard for both staging and diagnosis, with the sensitivity of 0.67-1 and specificity of 0.93[19,27-31]. If the patient has renal failure or another reason to avoid intravenous contrast, a retrograde pyelogram can be performed. Suspect UTUCC if a central renal tumor is seen, as the mass grows into the renal sinus (Figure 2).
Physicians must have a high index of suspicion for UTUCC when faced with a positive cytology despite having a negative cystoscopy, especially high grade UCC and CIS[32,33]. In this scenario, ureteral barbotage, also known as selective ureteral catherization is performed[34]. Ureteral washing has 80% sensitivity and ureteral brushing has 90% sensitivity. Of note, such selective collection of urine samples should occur prior to retrograde pyelography, as high-osmolar contrast agents may alter the cytologic features of the urine sample.
Once UTUCC is suspected, ureteropyeloscopy and biopsy is indicated[35-37]. Coupled with biopsy, ureteropyeloscopy is the method of choice for diagnosis of UTUCC[38-40]. However, due to the small size of the ureteral scopes, thin walled ureter and small biopsy forceps, staging is limited. Nevertheless, concordance between biopsy and final pathology is as high as 90% to 92%.
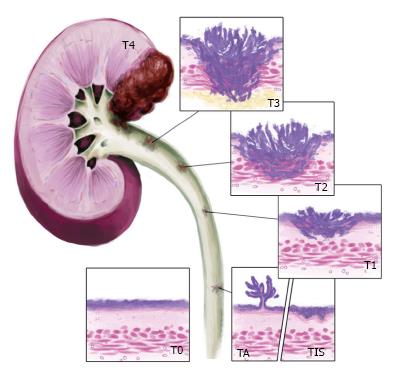
The TNM Staging System for UTUCC provided in Figure 3 and Table 1 defines the locations and extent of disease. The staging system begins at T0, which is no evidence of primary tumor and progresses to T4, where the tumor invades adjacent organs or through the kidney into the perinephric fat. Of note, tumor stage was identified as the most important determinant in predicting recurrence and survival. There for all efforts to obtain an accurately staged tissue is crucial[41].
| T - primary tumor | |
| TX | Primary tumor cannot be assessed |
| T0 | No evidence of primary tumor |
| Ta | Papillary noninvasive carcinoma |
| Tis | Carcinoma in situ |
| T1 | Tumor invades subepithelial connective tissue |
| T2 | Tumor invades the muscularis |
| T3 | (For renal pelvis only) tumor invades beyond muscularis into peripelvic fat or the renal parenchyma T3 (For ureter only) tumor invades beyond muscularis into periureteric fat |
| T4 | Tumor invades adjacent organs, or through the kidney into the perinephric fat |
| N - regional lymph nodes | |
| NX | Regional lymph nodes cannot be assessed |
| N0 | No regional lymph node metastasis |
| N1 | Metastasis in a single lymph node, ≤ 2 cm in greatest dimension |
| N2 | Metastasis in a single lymph node, > 2 cm but not > 5 cm in greatest dimension; or multiple lymph nodes, none > 5 cm in greatest dimension |
| N3 | Metastasis in a lymph node, > 5 cm in greatest dimension |
| M - distant metastasis | |
| M0 | No distant metastasis |
| M1 | Distant metastasis |
Lymph node involvement for renal pelvis tumors may include renal hilar, paracaval, aortic, and retroperitoneal nodes. For ureteral lymph node involvement, renal hilar, iliac, paracaval, periureteral, and pelvic nodes are commonly involved.
The most pivotal factors in determining prognosis are tumor stage and grade[42-46]. Invasion of the vascular, lymphatic, renal hilum and parenchyma, and perineural tissue surrounding the kidney has been shown to indicate more aggressive tumor behavior[47-52]. Multifocal disease, including areas such as the bladder, have been found to indicate a higher likelihood of recurrence and a worse overall prognosis[53]. Tumor necrosis greater than 10% is another independent risk factor indicating worse prognosis[54,55]. Age, gender and tumor location have been found to offer little information on disease course and predicting overall prognosis[56-61]. Numerous molecular markers including E-cadherin, Telomerase RNA component, hypoxia-inducible factor (HIF) 1-α, epithelial membrane protein 3, and C-erb-B2 have been investigated as possible diagnostic and prognostic tools[62-66]. More data is needed before applying the markers in a clinical setting.
Stage and grade of the tumor is instrumental in deciding treatment plans. Nephroureteretomy (NU) with bladder cuff has been the gold standard, and remains the treatment of choice for high grade (TA/T1, HG or CIS), invasive, or multifocal tumors, along with regional lymph node dissection[42,67].
Segmental resection or distal ureterectomy may be indicated in select cases to preserve renal function[68-70]. Tumors located in the distal third of the ureter can utilize a Psoas Hitch[71,72] which was popularized by Turner-Warwick. This method is an effective means to bridge the resultant defect of the lower third of the ureter. However, a small contracted bladder is a contraindication due to insufficient bladder capacity.
Ureteral defects proximal to the pelvic brim require more than a Psoas hitch. A lengthy ureteral tumor or diseased ureter in a patient with a need to preserve renal function can utilize an ileal ureteral substitution. Relative contraindications for ileal ureteral substitution include renal insufficiency, bladder outlet obstruction, and inflammatory bowel disease.
Endoscopic resection or ablation can be considered in patients with a solitary kidney or poor surgical candidates, especially for low grade and low stage tumors[73-78]. Holmium or Nd: Yag may be used for tumor ablation, as well as ureteral resection via an ureteroscope (Figures 4 and 5)[79].
A percutaneous approach may be considered in large (> 1.5 cm) renal pelvis UCC that are grade 1 and possibly grade 2[80,81]. The advantage for the percutaneous approach is that after 2-3 wk and with a normal nephrogram, BCG or mitomycin may be administered into the collecting system through the nephrostomy tube, as opposed to retrograde administration via reflux up a ureteral stent which is more challenging[82-85]. The disadvantage for a percutaneous approach is that 1/3 will recur and it is more invasive than other treatment options.
There is a lack of prospective studies that use of chemotherapy, whether neoadjuvant or adjuvant, due to the low incidence of this disease. The National Comprehensive Cancer Network® (NCCN®) Clinical Practice Guidelines in Oncology (NCCN Guidelines®) suggest the use of both with patient discretion (Table 2). For muscle invasive UCC, MVAC (methotrexate, vinblastine, doxorubicin, and cisplatin) or gemcitabine and cisplatin chemotherapy are both treatment options[85-91]. Of note, BCG and mitomycin treatment for upper tract UCC is extrapolated from bladder cancer and retrospective studies. There are currently no prospective studies showing improved survival and these are difficult to construct since it is such a rare disease. A role for BCG in the management of upper tract CIS has been demonstrated in retrospective studies, although a definitive efficacy of adjuvant topical therapy after endoscopic resection of Ta/T1 tumors has not yet been proven[84,92]. Of note, immunotherapy and chemotherapy in the upper tract has limitations due to difficulty delivering them to the system, unlike bladder instillations with such agents. Currently NCCN Guidelines® support using postsurgical intrapelvic chemotherapy or BCG for low grade UTUCC of the renal pelvis after endoscopic resection[91].
| Pathologic staging | Adjuvant treatment | Follow-up |
| pT0, pT1 | None | Cystoscopy every 3 mo for 1 yr, then at increasing intervals Imaging of upper tract collecting system at 3- to 12-mo intervals, if endoscopic resection ± CT scan or MRI ± Chest X-ray |
| pT2, pT3 pT4, pN+ | Consider adjuvant chemotherapy | Cystoscopy every 3 mo for 1 yr, then at increasing intervals Imaging of upper tract collecting system at 3- to 12-mo intervals ± CT scan or MRI ± Chest X-ray |
Chemotherapy for metastatic disease was studied using MVAC (methotrexate, vinblastine, doxorubicin, and cisplatin) in 184 patients from 1986 to 2004 at M.D. Anderson Center. Median recurrence-free survival was 2.4 years[75]. Patients with advanced disease should receive chemotherapy, preferably in a neoadjuvant setting. Enlarged lymph nodes should be biopsied prior to surgery, and if positive then intravenous chemotherapy should be administered, followed by surgery if no progression, as with bladder UCC.
Radiation plays a very small role in the treatment of UTUCC. Adjuvant radiotherapy may help limit local disease in a palliative setting. Although its role is limited, when combined with chemotherapy it may improve survival and disease-free survival[93,94].
Management principles of UTUCC are similar to that of bladder cancer. Low grade/low stage tumors may recur, but have a low likelihood of progression and high grade/high stage tumors are more aggressive and have a higher chance to metastasize. The challenge is identifying tumors as Ta low grade and ruling out CIS and more aggressive tumors[95,96] as obtaining adequate tissue for diagnosis can be challenging. Surveillance after treatment of UTUCC comes with many options. Per the European Association of Urology guidelines, low grade/stage tumors follow up should include cystoscopy every 3 mo for 1-2 years with periodic urine cytology, then every 6 mo for 2 years[41]. If renal sparing surgery was performed, an ureteroscopy would also be required. If the tumor was high grade/stage the management would be similar to that of the low grade/stage. In addition you would recommend imaging of the pelvis and abdomen and a chest X-ray.
Upper tract urothelial cell carcinoma is a rare disease with an incidence of less than 40000 cases per year. The most common presenting symptoms of UTUCC include hematuria and ureteral obstructive symptoms such as flank pain. The work up would then include cystoscopy, urine cytology, BUN, Creatinine and a CT Urogram. Tumor stage and grade are the most important prognostic factors to help the physician determine the best treatment options for the patient. Nephroureterectomy continues to be the gold standard for treatment in high grade, high stage tumors. In patients with low grade/stage disease, an absent contralateral kidney, poor renal function, or bilateral disease, renal sparing therapies including endoscopic resection, intravesical therapy with BCG or mitomycin C, and ureteral resection with ureteroureterostomy or re-implantation should be considered as an option for treatment. With appropriate treatment, the 5 year recurrence free survival rate for low grade/stage disease can be as high as 92%. However if the disease is not caught early and the patient has high grade/stage disease the 5 year recurrence free survival can be as low as 5%-48%. Factors such as high pathological stage, lymph node metastasis and vascular invasion increase the risk of recurrence and lead to decreased overall survival. Due to the aggressive nature of this disease, and lack of large prospective studies on this topic, large multi-institutional clinical trials are necessary to further investigate options for diagnosis, treatment, and surveillance to help those diagnosed with UTUCC.
Special thanks to Mike Tran MD, who drew illustrations for this topic.
Manuscript source: Invited manuscript
Specialty Type: Urology and Nephrology
Country of Origin: United States
Peer-Review Report Classification
Grade A (Excellent): 0
Grade B (Very good): B, B, B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P- Reviewer: Ali-El-Dein B, Creta M, Papatsoris AG, Soria F S- Editor: Kong JX L- Editor: A E- Editor: Lu YJ
| 1. | Ploeg M, Aben KK, Kiemeney LA. The present and future burden of urinary bladder cancer in the world. World J Urol. 2009;27:289-293. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 580] [Cited by in RCA: 645] [Article Influence: 40.3] [Reference Citation Analysis (1)] |
| 2. | Matin SF, Shariat SF, Milowsky MI, Hansel DE, Kassouf W, Koppie T, Bajorin D, Grollman AP. Highlights from the first symposium on upper tract urothelial carcinoma. Urol Oncol. 2014;32:309-316. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 10] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 3. | Wang Y, Lang MR, Pin CL, Izawa JI. Comparison of the clonality of urothelial carcinoma developing in the upper urinary tract and those developing in the bladder. Springerplus. 2013;2:412. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 13] [Cited by in RCA: 16] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 4. | Chen CH, Dickman KG, Moriya M, Zavadil J, Sidorenko VS, Edwards KL, Gnatenko DV, Wu L, Turesky RJ, Wu XR. Aristolochic acid-associated urothelial cancer in Taiwan. Proc Natl Acad Sci USA. 2012;109:8241-8246. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 279] [Cited by in RCA: 298] [Article Influence: 22.9] [Reference Citation Analysis (0)] |
| 5. | Tan LB, Chen KT, Guo HR. Clinical and epidemiological features of patients with genitourinary tract tumour in a blackfoot disease endemic area of Taiwan. BJU Int. 2008;102:48-54. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 50] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 6. | Munoz JJ, Ellison LM. Upper tract urothelial neoplasms: incidence and survival during the last 2 decades. J Urol. 2000;164:1523-1525. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 385] [Cited by in RCA: 371] [Article Influence: 14.8] [Reference Citation Analysis (0)] |
| 7. | Rink M, Xylinas E, Trinh QD, Lotan Y, Margulis V, Raman JD, Fisch M, Lee RK, Chun FK, Abdennabi J. Gender-specific effect of smoking on upper tract urothelial carcinoma outcomes. BJU Int. 2013;112:623-637. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 31] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 8. | Raman JD, Shariat SF, Karakiewicz PI, Lotan Y, Sagalowsky AI, Roscigno M, Montorsi F, Bolenz C, Weizer AZ, Wheat JC. Does preoperative symptom classification impact prognosis in patients with clinically localized upper-tract urothelial carcinoma managed by radical nephroureterectomy? Urol Oncol. 2011;29:716-723. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 51] [Cited by in RCA: 49] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 9. | Grollman AP, Shibutani S, Moriya M, Miller F, Wu L, Moll U, Suzuki N, Fernandes A, Rosenquist T, Medverec Z. Aristolochic acid and the etiology of endemic (Balkan) nephropathy. Proc Natl Acad Sci USA. 2007;104:12129-12134. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 463] [Cited by in RCA: 433] [Article Influence: 24.1] [Reference Citation Analysis (0)] |
| 10. | Arlt VM, Stiborová M, vom Brocke J, Simões ML, Lord GM, Nortier JL, Hollstein M, Phillips DH, Schmeiser HH. Aristolochic acid mutagenesis: molecular clues to the aetiology of Balkan endemic nephropathy-associated urothelial cancer. Carcinogenesis. 2007;28:2253-2261. [PubMed] |
| 11. | Laing C, Hamour S, Sheaff M, Miller R, Woolfson R. Chinese herbal uropathy and nephropathy. Lancet. 2006;368:338. [PubMed] |
| 12. | Lord GM, Cook T, Arlt VM, Schmeiser HH, Williams G, Pusey CD. Urothelial malignant disease and Chinese herbal nephropathy. Lancet. 2001;358:1515-1516. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 150] [Cited by in RCA: 127] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 13. | Roupret M, Catto J, Coulet F, Azzouzi AR, Amira N, Karmouni T, Fromont G, Sibony M, Vallancien G, Gattegno B. Microsatellite instability as indicator of MSH2 gene mutation in patients with upper urinary tract transitional cell carcinoma. J Med Genet. 2004;41:e91. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 50] [Cited by in RCA: 52] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 14. | Acher P, Kiela G, Thomas K, O’Brien T. Towards a rational strategy for the surveillance of patients with Lynch syndrome (hereditary non-polyposis colon cancer) for upper tract transitional cell carcinoma. BJU Int. 2010;106:300-302. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 28] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 15. | Rouprêt M, Yates DR, Comperat E, Cussenot O. Upper urinary tract urothelial cell carcinomas and other urological malignancies involved in the hereditary nonpolyposis colorectal cancer (lynch syndrome) tumor spectrum. Eur Urol. 2008;54:1226-1236. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 130] [Cited by in RCA: 142] [Article Influence: 8.4] [Reference Citation Analysis (0)] |
| 16. | Rouprêt M, Cancel-Tassin G, Comperat E, Fromont G, Sibony M, Molinié V, Allory Y, Triau S, Champigneulle J, Gaffory C. Phenol sulfotransferase SULT1A1*2 allele and enhanced risk of upper urinary tract urothelial cell carcinoma. Cancer Epidemiol Biomarkers Prev. 2007;16:2500-2503. [PubMed] |
| 17. | Pommer W, Bronder E, Klimpel A, Helmert U, Greiser E, Molzahn M. Urothelial cancer at different tumour sites: role of smoking and habitual intake of analgesics and laxatives. Results of the Berlin Urothelial Cancer Study. Nephrol Dial Transplant. 1999;14:2892-2897. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 62] [Cited by in RCA: 55] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 18. | Hagiwara M, Kikuchi E, Tanaka N, Matsumoto K, Ide H, Miyajima A, Masuda T, Nakamura S, Oya M. Impact of smoking status on bladder tumor recurrence after radical nephroureterectomy for upper tract urothelial carcinoma. J Urol. 2013;189:2062-2068. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 37] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 19. | NCCN Clinical Practice Guidelines in Oncology (NCCN Guidelines®). Bladder cancer. Version 2.2015. [accessed 2016 Feb 3]. Available from: https://www.nccn.org/professionals/physician_gls/PDF/bladder.pdf. |
| 20. | Colin P, Koenig P, Ouzzane A, Berthon N, Villers A, Biserte J, Rouprêt M. Environmental factors involved in carcinogenesis of urothelial cell carcinomas of the upper urinary tract. BJU Int. 2009;104:1436-1440. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 179] [Cited by in RCA: 201] [Article Influence: 12.6] [Reference Citation Analysis (0)] |
| 21. | Shinka T, Miyai M, Sawada Y, Inagaki T, Okawa T. Factors affecting the occurrence of urothelial tumors in dye workers exposed to aromatic amines. Int J Urol. 1995;2:243-248. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 31] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 22. | Furihata M, Yamasaki I, Ohtsuki Y, Sonobe H, Morioka M, Yamamoto A, Terao N, Kuwahara M, Fujisaki N. p53 and human papillomavirus DNA in renal pelvic and ureteral carcinoma including dysplastic lesions. Int J Cancer. 1995;64:298-303. [PubMed] |
| 23. | Palvio DH, Andersen JC, Falk E. Transitional cell tumors of the renal pelvis and ureter associated with capillarosclerosis indicating analgesic abuse. Cancer. 1987;59:972-976. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 24. | Azémar MD, Comperat E, Richard F, Cussenot O, Rouprêt M. Bladder recurrence after surgery for upper urinary tract urothelial cell carcinoma: frequency, risk factors, and surveillance. Urol Oncol. 2011;29:130-136. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 109] [Cited by in RCA: 108] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 25. | Raman JD, Ng CK, Scherr DS, Margulis V, Lotan Y, Bensalah K, Patard JJ, Kikuchi E, Montorsi F, Zigeuner R. Impact of tumor location on prognosis for patients with upper tract urothelial carcinoma managed by radical nephroureterectomy. Eur Urol. 2010;57:1072-1079. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 137] [Cited by in RCA: 138] [Article Influence: 8.6] [Reference Citation Analysis (0)] |
| 26. | Melamed MR, Reuter VE. Pathology and staging of urothelial tumors of the kidney and ureter. Urol Clin North Am. 1993;20:333-347. [PubMed] |
| 27. | Dillman JR, Caoili EM, Cohan RH, Ellis JH, Francis IR, Schipper MJ. Detection of upper tract urothelial neoplasms: sensitivity of axial, coronal reformatted, and curved-planar reformatted image-types utilizing 16-row multi-detector CT urography. Abdom Imaging. 2008;33:707-716. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 51] [Cited by in RCA: 30] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 28. | Van Der Molen AJ, Cowan NC, Mueller-Lisse UG, Nolte-Ernsting CC, Takahashi S, Cohan RH. CT urography: definition, indications and techniques. A guideline for clinical practice. Eur Radiol. 2008;18:4-17. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 243] [Cited by in RCA: 214] [Article Influence: 11.9] [Reference Citation Analysis (0)] |
| 29. | Wang LJ, Wong YC, Chuang CK, Huang CC, Pang ST. Diagnostic accuracy of transitional cell carcinoma on multidetector computerized tomography urography in patients with gross hematuria. J Urol. 2009;181:524-531; discussion 531. [PubMed] |
| 30. | Wang LJ, Wong YC, Huang CC, Wu CH, Hung SC, Chen HW. Multidetector computerized tomography urography is more accurate than excretory urography for diagnosing transitional cell carcinoma of the upper urinary tract in adults with hematuria. J Urol. 2010;183:48-55. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 85] [Cited by in RCA: 73] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 31. | Ng CK, Shariat SF, Lucas SM, Bagrodia A, Lotan Y, Scherr DS, Raman JD. Does the presence of hydronephrosis on preoperative axial CT imaging predict worse outcomes for patients undergoing nephroureterectomy for upper-tract urothelial carcinoma? Urol Oncol. 2011;29:27-32. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 66] [Cited by in RCA: 57] [Article Influence: 3.4] [Reference Citation Analysis (1)] |
| 32. | Zincke H, Aguilo JJ, Farrow GM, Utz DC, Khan AU. Significance of urinary cytology in the early detection of transitional cell cancer of the upper urinary tract. J Urol. 1976;116:781-783. [PubMed] |
| 33. | Highman WJ. Transitional carcinoma of the upper urinary tract: a histological and cytopathological study. J Clin Pathol. 1986;39:297-305. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 31] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 34. | Konety BR, Metro MJ, Melham MF, Salup RR. Diagnostic value of voided urine and bladder barbotage cytology in detecting transitional cell carcinoma of the urinary tract. Urol Int. 1999;62:26-30. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 15] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 35. | Abdel-Razzak OM, Ehya H, Cubler-Goodman A, Bagley DH. Ureteroscopic biopsy in the upper urinary tract. Urology. 1994;44:451-457. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 30] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 36. | Guarnizo E, Pavlovich CP, Seiba M, Carlson DL, Vaughan ED, Sosa RE. Ureteroscopic biopsy of upper tract urothelial carcinoma: improved diagnostic accuracy and histopathological considerations using a multi-biopsy approach. J Urol. 2000;163:52-55. [PubMed] |
| 37. | Keeley FX, Kulp DA, Bibbo M, McCue PA, Bagley DH. Diagnostic accuracy of ureteroscopic biopsy in upper tract transitional cell carcinoma. J Urol. 1997;157:33-37. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 206] [Cited by in RCA: 158] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 38. | Brien JC, Shariat SF, Herman MP, Ng CK, Scherr DS, Scoll B, Uzzo RG, Wille M, Eggener SE, Terrell JD. Preoperative hydronephrosis, ureteroscopic biopsy grade and urinary cytology can improve prediction of advanced upper tract urothelial carcinoma. J Urol. 2010;184:69-73. [PubMed] |
| 39. | Lee KS, Zeikus E, DeWolf WC, Rofsky NM, Pedrosa I. MR urography versus retrograde pyelography/ureteroscopy for the exclusion of upper urinary tract malignancy. Clin Radiol. 2010;65:185-192. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 28] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 40. | Ishikawa S, Abe T, Shinohara N, Harabayashi T, Sazawa A, Maruyama S, Kubota K, Matsuno Y, Osawa T, Shinno Y. Impact of diagnostic ureteroscopy on intravesical recurrence and survival in patients with urothelial carcinoma of the upper urinary tract. J Urol. 2010;184:883-887. [PubMed] |
| 41. | Rouprêt M, Babjuk M, Compérat E, Zigeuner R, Sylvester RJ, Burger M, Cowan NC, Böhle A, Van Rhijn BW, Kaasinen E. European Association of Urology Guidelines on Upper Urinary Tract Urothelial Cell Carcinoma: 2015 Update. Eur Urol. 2015;68:868-879. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 372] [Cited by in RCA: 405] [Article Influence: 40.5] [Reference Citation Analysis (0)] |
| 42. | Margulis V, Shariat SF, Matin SF, Kamat AM, Zigeuner R, Kikuchi E, Lotan Y, Weizer A, Raman JD, Wood CG. Outcomes of radical nephroureterectomy: a series from the Upper Tract Urothelial Carcinoma Collaboration. Cancer. 2009;115:1224-1233. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 731] [Cited by in RCA: 848] [Article Influence: 53.0] [Reference Citation Analysis (0)] |
| 43. | Sobin L, Gospodarowicz M, Wittekind C. TNM Classification of Malignant Tumours. Urological Tumours. Renal Pelvis and Ureter. 7th revised edition. USA: Wiley-Blackwell, UICC 2009; 258-261. |
| 44. | Langner C, Hutterer G, Chromecki T, Winkelmayer I, Rehak P, Zigeuner R. pT classification, grade, and vascular invasion as prognostic indicators in urothelial carcinoma of the upper urinary tract. Mod Pathol. 2006;19:272-279. [PubMed] |
| 45. | Lehmann J, Suttmann H, Kovac I, Hack M, Kamradt J, Siemer S, Wullich B, Zwergel U, Stöckle M. Transitional cell carcinoma of the ureter: prognostic factors influencing progression and survival. Eur Urol. 2007;51:1281-1288. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 83] [Cited by in RCA: 72] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 46. | Li CC, Chang TH, Wu WJ, Ke HL, Huang SP, Tsai PC, Chang SJ, Shen JT, Chou YH, Huang CH. Significant predictive factors for prognosis of primary upper urinary tract cancer after radical nephroureterectomy in Taiwanese patients. Eur Urol. 2008;54:1127-1134. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 154] [Cited by in RCA: 165] [Article Influence: 9.7] [Reference Citation Analysis (0)] |
| 47. | Kikuchi E, Margulis V, Karakiewicz PI, Roscigno M, Mikami S, Lotan Y, Remzi M, Bolenz C, Langner C, Weizer A. Lymphovascular invasion predicts clinical outcomes in patients with node-negative upper tract urothelial carcinoma. J Clin Oncol. 2009;27:612-618. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 219] [Cited by in RCA: 237] [Article Influence: 13.9] [Reference Citation Analysis (0)] |
| 48. | Kim DS, Lee YH, Cho KS, Cho NH, Chung BH, Hong SJ. Lymphovascular invasion and pT stage are prognostic factors in patients treated with radical nephroureterectomy for localized upper urinary tract transitional cell carcinoma. Urology. 2010;75:328-332. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 43] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 49. | Novara G, Matsumoto K, Kassouf W, Walton TJ, Fritsche HM, Bastian PJ, Martínez-Salamanca JI, Seitz C, Lemberger RJ, Burger M. Prognostic role of lymphovascular invasion in patients with urothelial carcinoma of the upper urinary tract: an international validation study. Eur Urol. 2010;57:1064-1071. [PubMed] |
| 50. | Fujimoto H, Tobisu K, Sakamoto M, Kamiya M, Kakizoe T. Intraductal tumor involvement and renal parenchymal invasion of transitional cell carcinoma in the renal pelvis. J Urol. 1995;153:57-60. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 16] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 51. | Davis BW, Hough AJ, Gardner WA. Renal pelvic carcinoma: morphological correlates of metastatic behavior. J Urol. 1987;137:857-861. [PubMed] |
| 52. | Rey A, Lara PC, Redondo E, Valdés E, Apolinario R. Overexpression of p53 in transitional cell carcinoma of the renal pelvis and ureter. Relation to tumor proliferation and survival. Cancer. 1997;79:2178-2185. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 53. | Corrado F, Ferri C, Mannini D, Corrado G, Bertoni F, Bacchini P, Lelli G, Lieber MM, Song JM. Transitional cell carcinoma of the upper urinary tract: evaluation of prognostic factors by histopathology and flow cytometric analysis. J Urol. 1991;145:1159-1163. [PubMed] |
| 54. | Zigeuner R, Shariat SF, Margulis V, Karakiewicz PI, Roscigno M, Weizer A, Kikuchi E, Remzi M, Raman JD, Bolenz C. Tumour necrosis is an indicator of aggressive biology in patients with urothelial carcinoma of the upper urinary tract. Eur Urol. 2010;57:575-581. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 135] [Cited by in RCA: 133] [Article Influence: 8.3] [Reference Citation Analysis (0)] |
| 55. | Seitz C, Gupta A, Shariat SF, Matsumoto K, Kassouf W, Walton TJ, Fritsche HM, Otto W, Tritschler S, Bastian PJ. Association of tumor necrosis with pathological features and clinical outcome in 754 patients undergoing radical nephroureterectomy for upper tract urothelial carcinoma: an international validation study. J Urol. 2010;184:1895-1900. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 44] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 56. | Fernández MI, Shariat SF, Margulis V, Bolenz C, Montorsi F, Suardi N, Remzi M, Wood CG, Roscigno M, Kikuchi E. Evidence-based sex-related outcomes after radical nephroureterectomy for upper tract urothelial carcinoma: results of large multicenter study. Urology. 2009;73:142-146. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 63] [Cited by in RCA: 61] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 57. | Lughezzani G, Sun M, Perrotte P, Shariat SF, Jeldres C, Budäus L, Latour M, Widmer H, Duclos A, Bénard F. Gender-related differences in patients with stage I to III upper tract urothelial carcinoma: results from the Surveillance, Epidemiology, and End Results database. Urology. 2010;75:321-327. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 88] [Cited by in RCA: 89] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 58. | Shariat SF, Favaretto RL, Gupta A, Fritsche HM, Matsumoto K, Kassouf W, Walton TJ, Tritschler S, Baba S, Matsushita K. Gender differences in radical nephroureterectomy for upper tract urothelial carcinoma. World J Urol. 2011;29:481-486. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 100] [Cited by in RCA: 127] [Article Influence: 8.5] [Reference Citation Analysis (0)] |
| 59. | Shariat SF, Godoy G, Lotan Y, Droller M, Karakiewicz PI, Raman JD, Isbarn H, Weizer A, Remzi M, Roscigno M. Advanced patient age is associated with inferior cancer-specific survival after radical nephroureterectomy. BJU Int. 2010;105:1672-1677. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 93] [Cited by in RCA: 94] [Article Influence: 5.9] [Reference Citation Analysis (0)] |
| 60. | Favaretto RL, Shariat SF, Chade DC, Godoy G, Adamy A, Kaag M, Bochner BH, Coleman J, Dalbagni G. The effect of tumor location on prognosis in patients treated with radical nephroureterectomy at Memorial Sloan-Kettering Cancer Center. Eur Urol. 2010;58:574-580. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 127] [Cited by in RCA: 153] [Article Influence: 10.2] [Reference Citation Analysis (0)] |
| 61. | Isbarn H, Jeldres C, Shariat SF, Liberman D, Sun M, Lughezzani G, Widmer H, Arjane P, Pharand D, Fisch M. Location of the primary tumor is not an independent predictor of cancer specific mortality in patients with upper urinary tract urothelial carcinoma. J Urol. 2009;182:2177-2181. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 86] [Cited by in RCA: 90] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 62. | Eltz S, Comperat E, Cussenot O, Rouprêt M. Molecular and histological markers in urothelial carcinomas of the upper urinary tract. BJU Int. 2008;102:532-535. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 51] [Cited by in RCA: 43] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 63. | Nakanishi K, Kawai T, Suzuki M, Torikata C. Growth factors and oncogene products in transitional cell carcinoma. Mod Pathol. 1996;9:292-297. [PubMed] |
| 64. | Nakanishi K, Kawai T, Torikata C, Aurues T, Ikeda T. E-cadherin expression in upper-urinary-tract carcinoma. Int J Cancer. 1997;74:446-449. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 65. | Nakanishi K, Kawai T, Hiroi S, Kumaki F, Torikata C, Aurues T, Ikeda T. Expression of telomerase mRNA component (hTR) in transitional cell carcinoma of the upper urinary tract. Cancer. 1999;86:2109-2116. [PubMed] |
| 66. | Remzi M, Haitel A, Margulis V, Karakiewicz P, Montorsi F, Kikuchi E, Zigeuner R, Weizer A, Bolenz C, Bensalah K. Tumour architecture is an independent predictor of outcomes after nephroureterectomy: a multi-institutional analysis of 1363 patients. BJU Int. 2009;103:307-311. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 136] [Cited by in RCA: 133] [Article Influence: 7.8] [Reference Citation Analysis (0)] |
| 67. | Remzi M, Haitel A, Margulis V, Karakiewicz P, Montorsi F, Kikuchi E, Zigeuner R, Weizer A, Bolenz C, Bensalah K. Tumour architecture is an independent predictor of outcomes after nephroureterectomy: a multi-institutional analysis of 1363 patients. BJU Int. 2009;103:307-311. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 136] [Cited by in RCA: 133] [Article Influence: 7.8] [Reference Citation Analysis (0)] |
| 68. | Lughezzani G, Sun M, Perrotte P, Shariat SF, Jeldres C, Budaus L, Alasker A, Duclos A, Widmer H, Latour M. Should bladder cuff excision remain the standard of care at nephroureterectomy in patients with urothelial carcinoma of the renal pelvis? A population-based study. Eur Urol. 2010;57:956-962. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 69] [Cited by in RCA: 76] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 69. | Phé V, Cussenot O, Bitker MO, Rouprêt M. Does the surgical technique for management of the distal ureter influence the outcome after nephroureterectomy? BJU Int. 2011;108:130-138. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 55] [Cited by in RCA: 58] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 70. | Zigeuner R, Pummer K. Urothelial carcinoma of the upper urinary tract: surgical approach and prognostic factors. Eur Urol. 2008;53:720-731. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 128] [Cited by in RCA: 128] [Article Influence: 7.5] [Reference Citation Analysis (0)] |
| 71. | Ahn M, Loughlin KR. Psoas hitch ureteral reimplantation in adults--analysis of a modified technique and timing of repair. Urology. 2001;58:184-187. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 56] [Cited by in RCA: 48] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 72. | Manassero F, Mogorovich A, Fiorini G, Di Paola G, De Maria M, Selli C. Ureteral reimplantation with psoas bladder hitch in adults: a contemporary series with long-term followup. ScientificWorldJournal. 2012;2012:379316. [PubMed] |
| 73. | Chen GL, Bagley DH. Ureteroscopic management of upper tract transitional cell carcinoma in patients with normal contralateral kidneys. J Urol. 2000;164:1173-1176. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 17] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 74. | Gadzinski AJ, Roberts WW, Faerber GJ, Wolf JS. Long-term outcomes of nephroureterectomy versus endoscopic management for upper tract urothelial carcinoma. J Urol. 2010;183:2148-2153. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 95] [Cited by in RCA: 97] [Article Influence: 6.5] [Reference Citation Analysis (0)] |
| 75. | Brown GA, Busby JE, Wood CG, Pisters LL, Dinney CP, Swanson DA, Grossman HB, Pettaway CA, Munsell MF, Kamat AM. Nephroureterectomy for treating upper urinary tract transitional cell carcinoma: Time to change the treatment paradigm? BJU Int. 2006;98:1176-1180. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 76. | Bagley DH, Grasso M. Ureteroscopic laser treatment of upper urinary tract neoplasms. World J Urol. 2010;28:143-149. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 41] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 77. | Rouprêt M, Hupertan V, Traxer O, Loison G, Chartier-Kastler E, Conort P, Bitker MO, Gattegno B, Richard F, Cussenot O. Comparison of open nephroureterectomy and ureteroscopic and percutaneous management of upper urinary tract transitional cell carcinoma. Urology. 2006;67:1181-1187. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 105] [Cited by in RCA: 97] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 78. | Cornu JN, Rouprêt M, Carpentier X, Geavlete B, de Medina SG, Cussenot O, Traxer O. Oncologic control obtained after exclusive flexible ureteroscopic management of upper urinary tract urothelial cell carcinoma. World J Urol. 2010;28:151-156. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 75] [Cited by in RCA: 74] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 79. | Abad PG, Del Peso AC, Arjona MF. Holmium: YAG laser ablation of upper urinary tract transitional cell carcinoma with new Olympus digital flexible ureteroscope. Urol Ann. 2013;5:212-214. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 80. | Palou J, Piovesan LF, Huguet J, Salvador J, Vicente J, Villavicencio H. Percutaneous nephroscopic management of upper urinary tract transitional cell carcinoma: recurrence and long-term followup. J Urol. 2004;172:66-69. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 93] [Cited by in RCA: 80] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 81. | Rouprêt M, Traxer O, Tligui M, Conort P, Chartier-Kastler E, Richard F, Cussenot O. Upper urinary tract transitional cell carcinoma: recurrence rate after percutaneous endoscopic resection. Eur Urol. 2007;51:709-713; discussion 714. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 83] [Cited by in RCA: 78] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 82. | Irie A, Iwamura M, Kadowaki K, Ohkawa A, Uchida T, Baba S. Intravesical instillation of bacille Calmette-Guérin for carcinoma in situ of the urothelium involving the upper urinary tract using vesicoureteral reflux created by a double-pigtail catheter. Urology. 2002;59:53-57. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 74] [Cited by in RCA: 55] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 83. | Nonomura N, Ono Y, Nozawa M, Fukui T, Harada Y, Nishimura K, Takaha N, Takahara S, Okuyama A. Bacillus Calmette-Guérin perfusion therapy for the treatment of transitional cell carcinoma in situ of the upper urinary tract. Eur Urol. 2000;38:701-704; discussion 705. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 69] [Cited by in RCA: 52] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 84. | Thalmann GN, Markwalder R, Walter B, Studer UE. Long-term experience with bacillus Calmette-Guerin therapy of upper urinary tract transitional cell carcinoma in patients not eligible for surgery. J Urol. 2002;168:1381-1385. [PubMed] |
| 85. | Audenet F, Yates DR, Cussenot O, Rouprêt M. The role of chemotherapy in the treatment of urothelial cell carcinoma of the upper urinary tract (UUT-UCC). Urol Oncol. 2013;31:407-413. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 62] [Cited by in RCA: 64] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 86. | Hellenthal NJ, Shariat SF, Margulis V, Karakiewicz PI, Roscigno M, Bolenz C, Remzi M, Weizer A, Zigeuner R, Bensalah K. Adjuvant chemotherapy for high risk upper tract urothelial carcinoma: results from the Upper Tract Urothelial Carcinoma Collaboration. J Urol. 2009;182:900-906. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 167] [Cited by in RCA: 159] [Article Influence: 9.9] [Reference Citation Analysis (0)] |
| 87. | Kaag MG, O’Malley RL, O’Malley P, Godoy G, Chen M, Smaldone MC, Hrebinko RL, Raman JD, Bochner B, Dalbagni G. Changes in renal function following nephroureterectomy may affect the use of perioperative chemotherapy. Eur Urol. 2010;58:581-587. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 169] [Cited by in RCA: 220] [Article Influence: 14.7] [Reference Citation Analysis (0)] |
| 88. | Lane BR, Smith AK, Larson BT, Gong MC, Campbell SC, Raghavan D, Dreicer R, Hansel DE, Stephenson AJ. Chronic kidney disease after nephroureterectomy for upper tract urothelial carcinoma and implications for the administration of perioperative chemotherapy. Cancer. 2010;116:2967-2973. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 138] [Cited by in RCA: 163] [Article Influence: 10.9] [Reference Citation Analysis (0)] |
| 89. | Matin SF, Margulis V, Kamat A, Wood CG, Grossman HB, Brown GA, Dinney CP, Millikan R, Siefker-Radtke AO. Incidence of downstaging and complete remission after neoadjuvant chemotherapy for high-risk upper tract transitional cell carcinoma. Cancer. 2010;116:3127-3134. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 175] [Cited by in RCA: 176] [Article Influence: 11.7] [Reference Citation Analysis (0)] |
| 90. | Kim TS, Oh JH, Rhew HY. The efficacy of adjuvant chemotherapy for locally advanced upper tract urothelial cell carcinoma. J Cancer. 2013;4:686-690. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 28] [Cited by in RCA: 35] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 91. | Papatsoris AG, Chrisofos M, Skolarikos A, Varkarakis I, Lekas A, Dellis A, Koritsiadis S, Deliveliotis C. Upper urinary tract transitional cell carcinoma. A 10-year experience. Tumori. 2008;94:75-78. [PubMed] |
| 92. | Shapiro EY, Lipsky MJ, Cha DY, McKiernan JM, Benson MC, Gupta M. Outcomes of intrarenal Bacillus Calmette-Guérin/interferon-α2B for biopsy-proven upper-tract carcinoma in situ. J Endourol. 2012;26:1645-1650. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 19] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 93. | Hall MC, Womack JS, Roehrborn CG, Carmody T, Sagalowsky AI. Advanced transitional cell carcinoma of the upper urinary tract: patterns of failure, survival and impact of postoperative adjuvant radiotherapy. J Urol. 1998;160:703-706. [PubMed] |
| 94. | Czito B, Zietman A, Kaufman D, Skowronski U, Shipley W. Adjuvant radiotherapy with and without concurrent chemotherapy for locally advanced transitional cell carcinoma of the renal pelvis and ureter. J Urol. 2004;172:1271-1275. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 73] [Cited by in RCA: 65] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 95. | Wheat JC, Weizer AZ, Wolf JS, Lotan Y, Remzi M, Margulis V, Wood CG, Montorsi F, Roscigno M, Kikuchi E. Concomitant carcinoma in situ is a feature of aggressive disease in patients with organ confined urothelial carcinoma following radical nephroureterectomy. Urol Oncol. 2012;30:252-258. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 62] [Cited by in RCA: 67] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 96. | Pieras E, Frontera G, Ruiz X, Vicens A, Ozonas M, Pizá P. Concomitant carcinoma in situ and tumour size are prognostic factors for bladder recurrence after nephroureterectomy for upper tract transitional cell carcinoma. BJU Int. 2010;106:1319-1323. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 63] [Cited by in RCA: 62] [Article Influence: 4.1] [Reference Citation Analysis (0)] |