Published online Mar 24, 2016. doi: 10.5410/wjcu.v5.i1.72
Peer-review started: June 10, 2015
First decision: August 18, 2015
Revised: November 13, 2015
Accepted: December 17, 2015
Article in press: December 18, 2015
Published online: March 24, 2016
Processing time: 286 Days and 5.6 Hours
Intramedullary spinal cord tumors are rare. The improved survival resulting from more effective treatments for many cancers has led to an increased number of publications concerning intramedullary spinal cord metastasis (ISCM), including case reports and literature reviews; however, ISCM remains extremely rare in renal cancer. A 69-year-old man with a medical history of renal cell carcinoma (RCC) presented with urinary retention and bilateral paralysis of the lower extremities. A neurological examination revealed bilateral paraparesis below L1. Although brain magnetic resonance imaging (MRI), bone scintigraphy, and abdominal contrast-enhanced computed tomography revealed no abdominal findings, the thracolumbar MRI indicated a spot on the spinal cord at the Th12 level that exhibited hyperintensity on T2-weighted imaging and gadolinium diethylenetriaminepentaacetic acid enhancement on T1-weighted imaging. Accordingly, an ISCM of RCC was diagnosed. The patient rejected all treatments for these metastases except the steroid therapy. The patient’s condition deteriorated owing to metastatic progression, and he died 3 mo after the appearance of ISCM symptoms. The prognosis of this condition was poor. The mean survival durations were 8 mo with surgical treatment, 4 mo with irradiation, and 2 mo with palliative treatments. In cases involving neurological features and if brain or bone metastasis or spinal cord compression is not clearly observed, gadolinium-enhanced MRI should be performed to determine the existence of ISCM. Recently, some authors have reported the efficacy of ISCM resection. Surgical treatment could potentially yield improvements in the nervous symptoms or a longer survival after treatment. Although the prognosis was poor in most cases of ISCM, surgical treatment may improve the patient’s quality of life.
Core tip: Intramedullary spinal cord metastasis (ISCM) is extremely rare in renal cancer. A 69-year-old man with a medical history of renal cell carcinoma presented with urinary retention and bilateral paralysis of the lower extremities. A neurological examination revealed bilateral paraparesis below L1. ISCM of renal cell carcinoma was diagnosed via thracolumbar gadolinium-enhanced magnetic resonance imaging (MRI). In a case involving neurological features and if brain or bone metastasis or spinal cord compression is not clearly observed, gadolinium-enhanced MRI should be performed to reveal the existence of ISCM.
- Citation: Soga H, Imanishi O. Case of intramedullary spinal cord metastasis of renal cell carcinoma. World J Clin Urol 2016; 5(1): 72-74
- URL: https://www.wjgnet.com/2219-2816/full/v5/i1/72.htm
- DOI: https://dx.doi.org/10.5410/wjcu.v5.i1.72
Intramedullary spinal cord tumors are rare. The improved survival resulting from more effective treatments for many cancers has led to an increased number of publications concerning intramedullary spinal cord metastasis (ISCM), including case reports and literature reviews; however, it is still extremely rare in renal cancer. Lung cancer and breast cancer are the most common primary tumors associated with ISCM[1,2]. In the present case, a 69-year-old man with a medical history of renal cell carcinoma (RCC) presented with urinary retention and bilateral paralysis of lower extremities. Magnetic resonance imaging (MRI) revealed an ISCM of RCC.
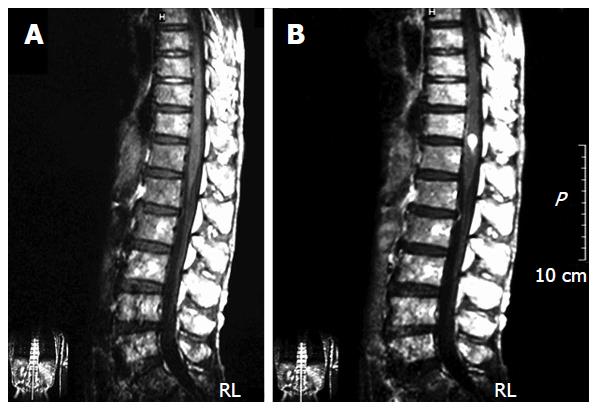
A 69-year-old man presented with cough since the previous month. The patient was diagnosed with stage IV renal cancer and multiple pulmonary metastases following a radical left nephrectomy and right segmental lung resection. A histopathological examination confirmed clear cell carcinoma, grade 2, pT1b, pM1-pul. Immunotherapy was initiated, with interferon alpha as an adjuvant therapy. Three months after adjuvant therapy initiation, the patient observed urinary retention after experiencing gait unsteadiness. The results of serum biochemical and hematological evaluations were normal. A neurological examination revealed bilateral paraparesis below L1. Deep tendon reflexes were absent in both legs. Brain MRI and bone scintigraphy revealed no abnormal findings. An abdominal contrast-enhanced computed tomography did not reveal a lymphatic mass or liver metastasis; however thracolumbar MRI indicated a spot on the spinal cord at the level of the Th12 level that exhibited hyperintensity on T2-weighted imaging and gadolinium diethylenetriaminepentaacetic acid enhancement on T1-weighted imaging (Figure 1). According to the radiographic findings and clinical history, the patient was diagnosed with an ISCM of RCC. The patient rejected all treatment for these metastases except steroid therapy. His condition deteriorated due to metastatic progression, and he died 3 mo after the appearance of ISCM symptoms.
Intramedullary spinal cord tumor is rare. Clinically, intramedullary metastatic disease affects only 0.1%-0.4% of all cancer patients and comprises only 1%-3% of all intramedullary spinal cord neoplasms[3]. Furthermore, intramedullary metastatic disease clinically affects only 4%-8.5% of all cancer patients with central nervous system metastases[4,5]. In a study of 1096 autopsy cases with neoplasms, 200 cases (18%) were found to harbor central nerves system metastases, and ISCMs were found in 10 cases (0.9%) of those cases. In that report, 199 of the 200 metastatic cases had lung tumors. ISCM might result from venous dissemination via the Batson’s plexus or direct nerve root invasion[6]. Most cases of ISCM might have additional metastases with various clinical features that cause unique symptoms such as gait disturbance or leg weakness; however, Rykken et al[1] reported that the clinical presentation of the ISCM preceded the primary tumor diagnosis in 20% of patients. Those authors suggested that the lack of a known primary malignancy should not dissuade clinicians from considering an ISCM when faced with a spinal cord mass[1]. MRI is generally a useful modality for the diagnosis of ISCM; furthermore, gadolinium-enhanced MRI is recommended as the most efficient diagnostic method, because unenhanced MRI dose not routinely yield critical findings.
Based on an understanding of the mechanism underlying RCC initiation and progression, several clinical trials evaluated the molecular targeting of RCC and observed efficacy against metastatic RCC[7]. However, no reports described the efficacy of the molecular targeting therapies against ISCM, possibly because some metastases already existed at the time of ISCM diagnosis. Several therapies, such as laminectomy, tumor reduction surgery, irradiation therapy, or steroid therapy, are used for ISCM treatment. The mean survival durations were 8 mo with surgical treatment, 4 mo with irradiation, and 2 mo with palliative treatment. Recently, some authors reported the efficacy of surgical ISCM removal[2,8]. Despite the poor prognosis of most cases, surgical treatment could potentially yield improvements in the nervous symptoms or survival duration one of more than 1 year after treatment[8]. Therefore, surgical treatment might be considered to effectively improve the patient’s quality of life. In the present case, we selected palliative steroid treatment because of the rapid lung metastasis growth and patient’s wishes. Steroid therapy significantly reduced the edematous infiltration observed on MRI, but did not improve the patient’s symptoms in our case.
In a case involving neurological features and if brain or bone metastasis or spinal cord compression is not evident, gadolinium-enhanced MRI should be performed to reveal the existence of ISCM. Depending on the patient’s condition, surgical treatment may be selected to improve the patient’s quality of life.
A 69-year-old man with a medical history of renal cell carcinoma presented with urinary retention and paralysis of bilateral lower extremities.
Neurological examination revealed bilateral paraparesis below L1.
Bone metastasis, brain metastasis, and pathological compression fracture.
The results of serum biochemical and hematological evaluations were normal.
The thracolumbar magnetic resonance imaging (MRI) indicated a spot on the spinal cord at the Th12 level that exhibited gadolinium diethylenetriaminepentaacetic acid (DTPA) enhancement on T1-weighted imaging.
Although histopathological examination of renal tumor confirmed renal cell carcinoma (clear cell carcinoma, grade 2, pT1b), pathologic examination of tumor in spinal cord was not performed.
The patient rejected all treatments for metastases except the steroid therapy.
According to some reviews concerning intramedullary spinal cord metastasis (ISCM), lung cancer was the most frequent primary malignant disease, followed by brain and breast cancers.
ISCM is rare, which comprises only 1%-3% of all intramedullary spinal cord neoplasms.
The gadolinium DTPA enhanced MRI is the most efficient diagnostic method, and early diagnosis and surgical treatment might improve the patient’s quality of life.
The paper describes an unusual metastasis in renal carcinoma and also provides information concerning the frequency of this rare spinal cord metastasis by other neoplasm.
P- Reviewer: Eirini G, Hakenberg OW, Papatsoris AG S- Editor: Gong XM L- Editor: A E- Editor: Li D
| 1. | Rykken JB, Diehn FE, Hunt CH, Schwartz KM, Eckel LJ, Wood CP, Kaufmann TJ, Lingineni RK, Carter RE, Wald JT. Intramedullary spinal cord metastases: MRI and relevant clinical features from a 13-year institutional case series. AJNR Am J Neuroradiol. 2013;34:2043-2049. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 45] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 2. | Payer S, Mende KC, Westphal M, Eicker SO. Intramedullary spinal cord metastases: an increasingly common diagnosis. Neurosurg Focus. 2015;39:E15. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 62] [Article Influence: 6.9] [Reference Citation Analysis (0)] |
| 3. | Ateaque A, Martin JL, O’Brien C. Intramedullary spinal cord metastases from a hypernephroma 11 years following the diagnosis and treatment of the primary lesion. Br J Neurosurg. 2000;14:474-476. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 19] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 4. | Chason JL, Walker FB, Landers JW. Metastatic carcinoma in the central nervous system and dorsal root ganglia. A prospective autopsy study. Cancer. 1963;16:781-787. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 5. | Schiff D, O’Neill BP. Intramedullary spinal cord metastases: clinical features and treatment outcome. Neurology. 1996;47:906-912. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 182] [Cited by in RCA: 146] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 6. | Edelson RN, Deck MD, Posner JB. Intramedullary spinal cord metastases. Clinical and radiographic findings in nine cases. Neurology. 1972;22:1222-1231. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 141] [Cited by in RCA: 121] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 7. | Skolarikos AA, Papatsoris AG, Alivizatos G, Deliveliotis C. Molecular pathogenetics of renal cancer. Am J Nephrol. 2006;26:218-231. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 13] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 8. | Park J, Chung SW, Kim KT, Cho DC, Hwang JH, Sung JK, Lee D. Intramedullary spinal cord metastasis in renal cell carcinoma: a case report of the surgical experience. J Korean Med Sci. 2013;28:1253-1256. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 12] [Cited by in RCA: 13] [Article Influence: 1.1] [Reference Citation Analysis (0)] |