Published online Mar 24, 2016. doi: 10.5410/wjcu.v5.i1.24
Peer-review started: September 5, 2015
First decision: November 24, 2015
Revised: December 24, 2015
Accepted: January 5, 2016
Article in press: January 7, 2016
Published online: March 24, 2016
Processing time: 202 Days and 20.2 Hours
Urology has been on the forefront of technological advances in minimally invasive surgery, from laparoscopy to robot-assisted surgeries. As with all new technological advances in medicine, the results of new advances are compared to previously established gold standards. When it comes to robot-assisted urology, morbidity, oncological outcomes, and cost between the same surgeries performed in an open fashion vs with robot-assistance should be assessed. Because healthcare spending is increasingly under more scrutiny, there is debate on the cost effectiveness of robot-assisted surgeries given the high acquisition and maintenance cost of robotic systems. This articles aims to critically evaluate the cost effectiveness of robot-assisted surgeries for prostatectomies, cystectomies, and partial nephrectomies in the United States.
Core tip: Robot-assisted urologic oncologic surgeries offers significant amounts of benefit, with shorter length of stay, less blood loss and improved peri-operative quality of life. The high fixed cost of robot acquisition and maintenance is offset by increasing the number of robot cases per year, narrowing the gap in cost between robot-assisted surgeries and open surgeries. Cost effective analysis and cost benefit analysis of robot-assisted surgeries are difficult to assess given the difficulties with evaluating indirect costs. However, the measurable differences favor robot-assisted surgeries.
- Citation: Chen CJ, Humphreys MR. Cost effectiveness of robot-assisted urologic oncological surgery in the United States. World J Clin Urol 2016; 5(1): 24-28
- URL: https://www.wjgnet.com/2219-2816/full/v5/i1/24.htm
- DOI: https://dx.doi.org/10.5410/wjcu.v5.i1.24
Healthcare spending is an important topic as current practices are under heavy scrutiny and affected by changes in healthcare policy. The cost of medical care has come to the forefront in both the medical and political community. This places pressure on the scientific community to develop technological advances that will not only improve health outcomes but that are also more cost effective. Robot-assisted surgery is a recent technology targeted in the debate regarding cost effectiveness and added value of healthcare.
Since the approval of the Da Vinci Surgical System (Intuitive Surgical, Inc., Sunnyvale, CA) by the Food and Drug Administration (FDA) in 2000, robotic assisted surgery has been rapidly adopted, with more than 1400 systems installed in the United States by 2009, growing by 85% from 2007 to 2009[1]. As of March 2015, Intuitive has reported that 3317 base units have been installed worldwide, with 2254 units in the United States, 556 in Europe, 194 in Japan and 313 in the rest of the world[2].
The urologic community has been quick to adopt robotic assisted laparoscopic surgery especially in urologic oncology, first through embracing robotic assisted prostatectomy and more recently increasing utilization to partial nephrectomies and cystectomies. Currently, the majority of radical prostatectomies are performed robotically in the United States, with estimate in 2009 being 69% performed robotically[3].
Robotic assisted laparoscopic surgery offers several advantages. From the surgeon’s perspective, robotic assisted surgery offers improved visual field, including 3-dimentional view, improved freedom of movement through “wristed” instruments, elimination of surgeon tremor and ergonomic benefits[4]. For the patient, benefits include improved cosmetics with smaller incision sites, decrease loss of blood, decreased post-procedure pain, shorter length of stay and faster recovery[4]. However, some reported disadvantages include longer operative time, lack of tactile sensation, and instrument collision resulting in injury to surrounding organs.
Currently in the United States, most patients pay for their healthcare through insurance, and ultimately only pay a small portion directly leading to poor understanding of medical costs. Many studies have demonstrated that robotic surgery can be more expensive due to the high acquisition cost[5-7].
There are three types of models to assess the economics of medical care (Table 1): Cost-identification analysis, cost effective analysis, and cost-benefit analysis[8]. Cost-identification analysis simply identifies the cost without addressing outcomes. Cost effectiveness analysis is a method used to assess cost and outcomes[9]. It is often presented as an incremental cost effectiveness ratio, where the numerator is the difference of cost between two different interventions and the denominator is the difference between the health outcomes[10]. Health outcomes can be measured in several different ways (i.e., quality of life, disease free survival, life years gained). Cost-benefit analysis evaluates whether the benefit is worth the cost done by measuring cost and outcomes in the same unit[8].
| Economic models of medical care | Definition |
| Cost identification analysis | Identifies cost without evaluating outcomes |
| Cost effectiveness analysis | Assess cost and outcomes; represented as an incremental cost effectiveness ratio (difference of cost between two different interventions/the difference between the health outcomes) |
| Cost-benefit analysis | Evaluates whether the benefit is worth the cost done by measuring cost and outcomes in the same unit |
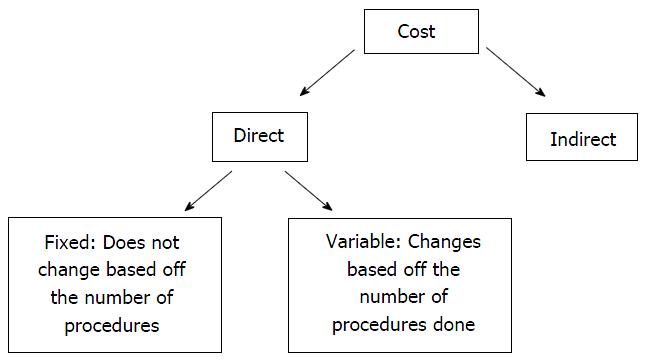
Direct costs are divided into two categories (Figure 1), fixed cost which would not change based off of the number of procedures and variable cost which does change based on the number of procedures done[8]. Indirect costs are measured by cost incurred by loss of livelihood or life due to morbidity or mortality such as lost wages or disability[8]. Given the difficulties in evaluating indirect costs, there has not been any study to evaluate this. Most published literature focus on the direct cost of robotic surgery.
Some of the draw backs to economic analysis are due to bias and uncertainties. It is difficult to obtain precise values for many of the components for necessary cost analysis. Insurance reimbursement also differs compared to actual cost. Currently, Medicare uses cost effective analysis for preventative services but not for treatment.
The direct costs in robotic surgery tend to be higher than open procedures predominantly due to the high acquisition cost of a robotic surgical system as well as cost of disposable instruments and terms of maintenance agreements. Currently, Intuitive Surgical is the only company on the market producing a FDA approved robotic surgical system, thus, holding a monopoly on the market. It is estimated that robotic acquisition is typically around 1.5 million dollars with an annual $150000 service contract. Per the American Hospital Association’s 2008 asset life assessment guidelines, most studies amortize this cost over 7 years, dividing the total cost over the total number of robotic cases to determine the cost per case[11-14]. Thus, the cost of robotic utilization per case is lower at a large volume practice compared to a low volume practice. Other direct cost consists of cost for robotic instruments. With programmed obsolesce, robotic instruments are limited to 10 uses per instrument compared to laparoscopic and open instruments, which tend to have unlimited uses.
Out of the limited literature published on the cost of robotic assisted urologic surgery, the literature is most robust for radical prostatectomy. Bolenz et al[5] published their data on cost from the hospital billing department. They obtained disposable laparoscopic cost, including cost of trocars, specimen entrapment sac, suction irrigator, clip appliers, and use of adjuvant hemostatic agents. Cost specific for the robot included robotic instruments per use. They evaluated operative time to determine OR cost, including cost for anesthesia and OR overhead. The rate for room and board was included, based on length of stay. They concluded that the median direct cost for robotic assisted radical prostatectomy (RARP) was $6752, laparoscopic prostatectomy was $5687 and $4437 for open radical retropubic prostatectomy (RRP)[5]. However, they did not include acquisition cost and maintenance cost in these values, which would only raise the cost of RARP.
Bolenz et al[15] subsequently published a systematic review on the cost of prostatectomy using different methods, including 11 studies that reported the direct cost of the procedure in their final analysis. Out of the 11 studies included, 6 studies compared open RRP with minimally invasive prostatectomy. For minimal invasive prostatectomy, which included both laparoscopic and robotic prostatectomy, the cost ranged from $5058-$11806. For open RRP, the cost ranged from $4075-$6296. The direct cost in minimally invasive prostatectomy was higher than open in 5 out of the 6 studies.
Hyams et al[16] specifically evaluated the impact of surgical volume on the cost of radical prostatectomy. They used a statewide database to identify all open and robotic prostatectomies between 2008-2011 in Maryland. They found that in both the open RRP and the RARP groups, the larger the surgical volume, the lower the cost per case. However, they still note that open RRP had lower direct costs even at high volume. This study did not take into account acquisition and maintenance costs; thus, possibly increasing the difference between the cost for RARP and open RRP more.
In a retrospective study of 882 patients (294 in the robot-assisted group and 588 in the open group), Krambeck et al[17] demonstrated that there was significant difference in median operation time between the RARP and open RRP groups; however, by the last 100 RARP cases, there was no difference in median operation time. They included docking time of the robot in their analysis. Through their study, they demonstrated that with increased experience, the cost of OR time could be equivalent between the two groups.
There are no studies that have directly analyzed and calculated a value for the indirect cost of robotic assisted prostatectomies. However, there have been studies that indirectly address this through evaluating cancer control and side effects.
In a retrospective study of 400 patients, the overall incidence of positive surgical margin was 15% in the RARP arm compared to 35% in the open RRP arm (P < 0.001)[18]. When sub-stratified based on pathological stage, the positive surgical margin was lower in the RARP groups for both pT2 and pT3 disease[18].
Tewari et al[19] demonstrated in a prospective comparison between open RRP and RARP that patients in the RARP group had faster return of continence (44 d vs 160 d) and erections (180 d vs 440 d) compared to those in the open RRP group. They also report that positive margins were more frequent in the open RRP group compared to the RARP group (23% vs 9%).
There has only been one study published evaluating and comparing quality of life in men undergoing RARP vs open RRP in the peri-operative period. In a prospective study, Miller et al[20] had patients complete the SF-12 version 2 Physical and Mental Health Survey Acute Form preoperatively and weekly postoperatively for 6 wk. This questionnaire assesses physical functioning, role limitations due to physical health, pain, general health perceptions, vitality, social functioning, role limitations due to emotional problems, and mental health. This was broken down into a mental component score and a physical component score, which higher scores indicating better functioning. The physical component score was consistently higher in the RARP group starting from week 1 to week 6. There was no statistically difference in the mental component score except on the preoperative survey, where the RARP group scored higher than the open RRP group. Studies that have looked at long term quality of life notice no difference between different methods of RARP and open RRP[21,22].
The direct cost comparison between robot-assisted radical cystectomy (RARC) and open radical cystectomy (ORC) is less clear compared to that analysis for prostatectomies. There are significantly fewer studies published for cystectomies and as a whole, the urologic community is at an earlier stage in the learning process for cystectomies compared to prostatectomies.
Yu et al[23] reported that RARC costs is greater than ORC cost by $3797; however, they did not elaborate on how these numbers were obtained. They report in their retrospective study using the United States Nationwide Inpatient sample no difference in length of hospital stay or transfusion rates between the RARC and ORC groups. The RARC group had lower parenteral nutrition use and lower inpatient complications, but they were not able to classify or grade these complications.
In a retrospective study on 20 RARC and 20 ORC at a single institute, Smith et al[7] demonstrated that the cost of the RARC group was overall higher than the ORC by $1640. They included fixed cost, variable cost, as well as hospital cost. Fixed cost included base cost and disposable equipment cost for ORC. Robotic fixed cost included amortization of the robot as well as maintenance fees. Variable operating room cost depended on the duration of the case, which was higher in the RARC group. Hospital cost was actually higher in the ORC group because of increased transfusion rates and length of stay.
On the other hand, Martin et al[14] demonstrate when evaluating actual patient costs there is a 38% cost advantage favoring RARC when combining both operating room and hospital costs. The absolute cost was not given. The costs relating to the operating room was more in the RARC group because of longer procedure time and fixed cost of robot acquisition and maintenance. However, there was a significant difference in the length of stay (LOS), with the mean LOS of 5 d in the RARC group and 10 d in the ORC group. This was a relatively small study with 19 patients in the RARC group and 14 patients in the ORC group.
Lee et al[11] also demonstrated similar findings. In a retrospective study on 186 patients, they subdivided the patients based of the type of urinary diversion used. The cost of RARC with orthotopic neobladder was less than the cost ORC with orthotopic neobladder. They conclude that the difference in LOS is able to offset the higher cost of robotic surgery. Furthermore, the overall complication rate within the 90-d global surgery period was lower in the RARC group (49.4%) than the ORC group (61.2%).
The main limitation of cost evaluation of RARC vs ORC is the lack of published data on effectiveness as well as comparison of side effects. There is limited data on oncologic outcome, with the longest follow-up of 3.5 years in RARC[24].
There are limited studies evaluating the cost of robotic-assisted partial nephrectomy (RAPN), open partial nephrectomy (OPN) and laparoscopic partial nephrectomy (LPN). The studies that have been published are small, with the largest only evaluating 89 patients[12].
Hyams et al[25] evaluated 20 consecutive RAPN and OPN from 2009-2010. They calculated that RAPN was $1066.09 more than LPN. This was attributed to the high capital cost for robotic surgery specific to their center. Capital cost was estimated for the purchase and amortization of 2 robotic systems as well as maintenance cost divided by the total number of robotic cases between 2001 and 2009. They concluded that when the fixed robotic cost was calculated based off 1 robotic system with “ideal” utilization of 300 cases per year, the cost difference is only $333.85 per case.
In another study that compared RALN to OLN, Alemozaffar et al[13] also conclude that RALN can be cost equivalent to OPN by minimizing OR time and LOS. However, RALN was most expensive when fixed costs were factored.
Overall, robotic assisted surgery has offered significant amounts of benefit to urologic surgery, with shorter LOS, less blood loss, and improved peri-operative quality of life. Given the high fixed cost of robotic acquisition and maintenance, robotic assisted surgery is more often than not, more expensive than open procedure when evaluating direct costs. However, the gap in cost between robotic assisted and open surgery can be narrowed in high volume centers where the fixed cost can be divided between a larger number of cases. Also, if the LOS is substantially different between robotic and open groups, such as in cystectomies, the cost of robotic surgery can actually be even lower than an open procedure. Due to the difficulty of identifying indirect costs and health outcomes, it is very difficult to assess cost-benefit of robotic assisted surgery. Furthermore, these cost evaluations do not factor in patient preference and requests for procedures to be done robotically. Ultimately, more data is needed in evaluating and comparing long term surgical outcomes between robotic assisted and open surgery.
P- Reviewer: Donkov I, Ilie CP, Pignot G S- Editor: Qi Y L- Editor: A E- Editor: Li D
| 1. | Barbash GI, Glied SA. New technology and health care costs--the case of robot-assisted surgery. N Engl J Med. 2010;363:701-704. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 672] [Cited by in RCA: 622] [Article Influence: 41.5] [Reference Citation Analysis (0)] |
| 2. | Intuitive surgical/investor FAQ. Available from: http://phx.corporate-ir.net/phoenix.zhtml?c=122359&p=irol-faq. |
| 3. | Lowrance WT, Eastham JA, Savage C, Maschino AC, Laudone VP, Dechet CB, Stephenson RA, Scardino PT, Sandhu JS. Contemporary open and robotic radical prostatectomy practice patterns among urologists in the United States. J Urol. 2012;187:2087-2092. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 146] [Cited by in RCA: 175] [Article Influence: 13.5] [Reference Citation Analysis (0)] |
| 4. | Yu HY, Hevelone ND, Lipsitz SR, Kowalczyk KJ, Nguyen PL, Choueiri TK, Kibel AS, Hu JC. Comparative analysis of outcomes and costs following open radical cystectomy versus robot-assisted laparoscopic radical cystectomy: results from the US Nationwide Inpatient Sample. Eur Urol. 2012;61:1239-1244. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 135] [Cited by in RCA: 135] [Article Influence: 10.4] [Reference Citation Analysis (0)] |
| 5. | Bolenz C, Gupta A, Hotze T, Ho R, Cadeddu JA, Roehrborn CG, Lotan Y. Cost comparison of robotic, laparoscopic, and open radical prostatectomy for prostate cancer. Eur Urol. 2010;57:453-458. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 196] [Cited by in RCA: 195] [Article Influence: 12.2] [Reference Citation Analysis (0)] |
| 6. | Mir SA, Cadeddu JA, Sleeper JP, Lotan Y. Cost comparison of robotic, laparoscopic, and open partial nephrectomy. J Endourol. 2011;25:447-453. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 88] [Cited by in RCA: 91] [Article Influence: 6.5] [Reference Citation Analysis (0)] |
| 7. | Smith A, Kurpad R, Lal A, Nielsen M, Wallen EM, Pruthi RS. Cost analysis of robotic versus open radical cystectomy for bladder cancer. J Urol. 2010;183:505-509. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 80] [Cited by in RCA: 77] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 8. | Eisenberg JM. Clinical economics. A guide to the economic analysis of clinical practices. JAMA. 1989;262:2879-2886. [PubMed] |
| 9. | Russell LB, Gold MR, Siegel JE, Daniels N, Weinstein MC. The role of cost-effectiveness analysis in health and medicine. Panel on Cost-Effectiveness in Health and Medicine. JAMA. 1996;276:1172-1177. [PubMed] |
| 10. | Detsky AS, Naglie IG. A clinician’s guide to cost-effectiveness analysis. Ann Intern Med. 1990;113:147-154. [PubMed] |
| 11. | Lee R, Ng CK, Shariat SF, Borkina A, Guimento R, Brumit KF, Scherr DS. The economics of robotic cystectomy: cost comparison of open versus robotic cystectomy. BJU Int. 2011;108:1886-1892. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 65] [Cited by in RCA: 66] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 12. | Ferguson JE, Goyal RK, Raynor MC, Nielsen ME, Pruthi RS, Brown PM, Wallen EM. Cost analysis of robot-assisted laparoscopic versus hand-assisted laparoscopic partial nephrectomy. J Endourol. 2012;26:1030-1037. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 18] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 13. | Alemozaffar M, Chang SL, Kacker R, Sun M, DeWolf WC, Wagner AA. Comparing costs of robotic, laparoscopic, and open partial nephrectomy. J Endourol. 2013;27:560-565. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 44] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 14. | Martin AD, Nunez RN, Castle EP. Robot-assisted radical cystectomy versus open radical cystectomy: a complete cost analysis. Urology. 2011;77:621-625. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 90] [Cited by in RCA: 89] [Article Influence: 5.9] [Reference Citation Analysis (0)] |
| 15. | Bolenz C, Freedland SJ, Hollenbeck BK, Lotan Y, Lowrance WT, Nelson JB, Hu JC. Costs of radical prostatectomy for prostate cancer: a systematic review. Eur Urol. 2014;65:316-324. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 77] [Cited by in RCA: 74] [Article Influence: 6.7] [Reference Citation Analysis (0)] |
| 16. | Hyams ES, Mullins JK, Pierorazio PM, Partin AW, Allaf ME, Matlaga BR. Impact of robotic technique and surgical volume on the cost of radical prostatectomy. J Endourol. 2013;27:298-303. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 24] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 17. | Krambeck AE, DiMarco DS, Rangel LJ, Bergstralh EJ, Myers RP, Blute ML, Gettman MT. Radical prostatectomy for prostatic adenocarcinoma: a matched comparison of open retropubic and robot-assisted techniques. BJU Int. 2009;103:448-453. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 206] [Cited by in RCA: 191] [Article Influence: 11.2] [Reference Citation Analysis (0)] |
| 18. | Smith JA, Chan RC, Chang SS, Herrell SD, Clark PE, Baumgartner R, Cookson MS. A comparison of the incidence and location of positive surgical margins in robotic assisted laparoscopic radical prostatectomy and open retropubic radical prostatectomy. J Urol. 2007;178:2385-2389; discussion 2389-2390. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 218] [Cited by in RCA: 205] [Article Influence: 11.4] [Reference Citation Analysis (0)] |
| 19. | Tewari A, Srivasatava A, Menon M. A prospective comparison of radical retropubic and robot-assisted prostatectomy: experience in one institution. BJU Int. 2003;92:205-210. [PubMed] |
| 20. | Miller J, Smith A, Kouba E, Wallen E, Pruthi RS. Prospective evaluation of short-term impact and recovery of health related quality of life in men undergoing robotic assisted laparoscopic radical prostatectomy versus open radical prostatectomy. J Urol. 2007;178:854-858; discussion 859. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 58] [Cited by in RCA: 54] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 21. | Ball AJ, Gambill B, Fabrizio MD, Davis JW, Given RW, Lynch DF, Shaves M, Schellhammer PF. Prospective longitudinal comparative study of early health-related quality-of-life outcomes in patients undergoing surgical treatment for localized prostate cancer: a short-term evaluation of five approaches from a single institution. J Endourol. 2006;20:723-731. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 43] [Cited by in RCA: 35] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 22. | Namiki S, Egawa S, Terachi T, Matsubara A, Igawa M, Terai A, Tochigi T, Ioritani N, Saito S, Arai Y. Changes in quality of life in first year after radical prostatectomy by retropubic, laparoscopic, and perineal approach: Multi-institutional longitudinal study in Japan. Urology. 2006;67:321-327. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 20] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 23. | Yu HY, Hevelone ND, Lipsitz SR, Kowalczyk KJ, Hu JC. Use, costs and comparative effectiveness of robotic assisted, laparoscopic and open urological surgery. J Urol. 2012;187:1392-1398. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 182] [Cited by in RCA: 200] [Article Influence: 15.4] [Reference Citation Analysis (0)] |
| 24. | Mmeje CO, Nunez-Nateras R, Nielsen ME, Pruthi RS, Smith A, Wallen EM, Humphreys MR, Woods ME, Castle EP. Oncologic outcomes for lymph node-positive urothelial carcinoma patients treated with robot assisted radical cystectomy: with mean follow-up of 3.5 years. Urol Oncol. 2013;31:1621-1627. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 16] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 25. | Hyams E, Pierorazio P, Mullins JK, Ward M, Allaf M. A comparative cost analysis of robot-assisted versus traditional laparoscopic partial nephrectomy. J Endourol. 2012;26:843-847. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 36] [Article Influence: 2.8] [Reference Citation Analysis (0)] |