Published online Jul 24, 2014. doi: 10.5410/wjcu.v3.i2.119
Revised: March 5, 2014
Accepted: March 13, 2014
Published online: July 24, 2014
Processing time: 212 Days and 17.2 Hours
Laparoendoscopic single-site surgery (LESS) has been developed to benefit patients by enabling surgeons to perform scarless surgery. In this review we aimed to summarize and critically analyze the available evidence on the current status and future prospects for LESS in pediatric urology, with special emphasis on our experience with LESS in children. The clinical data available clearly demonstrate that LESS can safely and effectively be performed in a variety of pediatric urology settings. As clinical experience increases, expanding indications are expected to be documented and the efficacy of the procedure to improve. So far, the quality of evidence of all available studies remains low; mostly being small case series or case-control studies from selected centers. Thus, the only objective benefit of LESS remains improved cosmetic outcome. Prospective randomized studies are awaited to determine which LESS procedures will be established and which are unlikely to stand the test of time. Technological advances hold promise to minimize the challenging technical nature of scarless surgery. In this respect, robotics may be a driving force in the development of LESS.
Core tip: Laparoendoscopic single-site surgery (LESS) has been developed to benefit patients by enabling surgeons to perform scarless surgery. Clinical data demonstrate that LESS is safe and effective in many pediatric urology settings. As clinical experience increases, expanding indications are expected, along with improved efficacy. Prospective randomized studies are awaited to determine whether LESS procedures will be established as routine and will be able to stand the test of time. Technological advances hold promise to minimize the challenging technical nature of scarless surgery. In this respect, robotics is likely to drive a major paradigm shift in the development of LESS.
- Citation: Wagmaister J, Kocherov S, Chertin B. Laparoscopic single site surgery: Experience in pediatric urology. World J Clin Urol 2014; 3(2): 119-126
- URL: https://www.wjgnet.com/2219-2816/full/v3/i2/119.htm
- DOI: https://dx.doi.org/10.5410/wjcu.v3.i2.119
Laparoscopic surgery is beginning to gain acceptance as a standard of care in many intra-abdominal procedures in adult and pediatric urology[1]. Today, laparoscopic procedures are commonly performed and have become widely accepted as alternatives to open surgery, if not the gold standard in some procedures, such as radical or partial nephrectomy[2]. Even the more technically demanding procedures, such as laparoscopic pyeloplasty, laparoscopic-assisted bladder reconstruction, and laparoscopic ureteral reimplantation, have achieved widespread acceptance and are now routinely performed at many centers worldwide. With increasing experience in the laparoscopic environment, efforts are now directed at further minimizing morbidity and improving cosmetic outcomes. This has led to the development of techniques, multichannel single-access ports, and novel bent/articulating instruments that allow the laparoscopic procedure to be performed through a single skin incision, often hidden within the umbilicus or utilizing the nature orifices of the human body in order to seal surgical incisions completely. Following this concept natural orifice transluminal endoscopic surgery (NOTES) and laparoendoscopic single-site surgery (LESS) have been developed in an attempt to reduce further the morbidity and scaring associated with surgical intervention[3-5]. Conceptually, these techniques share a common underlying hypothesis that has driven their development-namely, that a reduction in the number of transcutaneous points of access may benefit patients in terms of port-related complications, recovery time, pain, and cosmesis by potentially performing scarless surgery. The first documented one-port single-incision laparoscopy was cholecystectomy in 1997. Ten years later, the first single-port nephrectomy was done. Since then urologists have successfully performed various procedures with LESS, including partial nephrectomy, pyeloplasty, orchiectomy, orchiopexy, varicocelectomy, ureterolithotomy, sacrocolpopexy, renal biopsy, renal cryotherapy, and adrenalectomy[6,7].
In this review, we describe the rationale of the technique, the current clinical applications, the advantages and disadvantages compared to standard laparoscopy, and the results of LESS in pediatric urological surgery, with some attention in robotic surgery.
LESS is a minimally invasive surgical procedure in which the surgeon operates almost exclusively through a single entry point, typically the patient’s navel. Unlike a traditional multiport laparoscopic approach, LESS leaves only a single small umbilical scar, usually not larger than 2 cm. This particular access can be achieved through a single fascial incision site with a single trocar with multiple ports, or through a single skin incision site with multiple fascial incisions with individual trocars. The most popular technique is the first mentioned above: a single port with multiple channels. Like conventional laparoscopy, there are two principal approaches for renal, adrenal and ureteral surgery: transperitoneal and retroperitoneal[8]. Although the first mentioned above is the best known and usually performed, today sufficient clinical studies have shown the effectiveness and safety of LESS through a retroperitoneal approach, especially in nephrectomy for nonfunctioning kidney and in other extirpative retroperitoneal procedures[9].
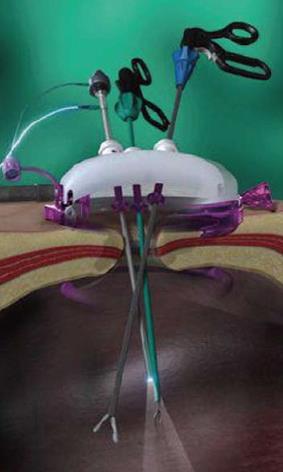
With the time and development of the technique, the concept of LESS was diversified and the surgeons proposed different acronyms for LESS and associated procedures. They include: single port access, single incision laparoscopic surgery (SILS), natural orifice transumbilical surgery, transumbilical endoscopic surgery, single-access site laparoscopic surgery, single-site access, one-port umbilical surgery, transumbilical laparoendoscopic single-site surgery, transumbilical laparoscopic assisted surgery, and embryonic natural orifice transluminal endoscopic surgery[10-14]. The common factor is a single small skin incision, usually at the umbilicus (Figure 1).
Robotic LESS (R-LESS) uses the Da Vinci Surgery System via a one single-port approach to improve ergonomics that limit conventional single-port laparoscopy[15].
Minimally invasive surgery is a changing and evolving field. Since the first documented laparoscopic procedure in humans performed by Hans Christian Jacobaeus in 1910, there has been great progress that has expanded throughout the surgical specialties. In 1918, Goetze developed the first automatic pneumoperitoneum needle. In 1929, Kalk introduced the forward oblique (135 degrees) view lens systems, and in 1938, Veress developed a specially designed spring-loaded needle. Veress did not promote the use of his needle for laparoscopic purposes. He used the Veress Needle for the induction of pneumothorax. To date, the Veress Needle is the most important instrument to create pneumoperitoneum. The real credit for videoscopic surgery goes to Hopkins, who discovered in 1953 the rigid rod lens system that revolutionized the field of laparoscopic surgery. As a result of this development, in 1970, gynecologists started to embrace laparoscopy and thoroughly incorporated the technique into their practice. General surgeons, despite their exposure to laparoscopy remained confined to traditional open surgery until 1977, when the first laparoscopic assisted appendectomy was performed by Dekok. In that setup, the appendix was exteriorized and ligated outside. In the same year, Semm first demonstrated the endoloop suturing technique in laparoscopic surgery. The first documented laparoscopic cholecystectomy was performed by Mühe in Germany in 1985. In 1994, the first robotic arm was designed to hold the telescope, and in 1996, a live telecast of laparoscopic surgery was performed remotely via the internet (robotic telesurgery)[16]. As part of the natural development of minimally invasive surgery, in the late 1990s, LESS emerged[3]. The reason for the development of this type of procedure rests on the premise ”LESS pain, LESS scar”, but the practical advantages in the field are many more than those. As already mentioned, the first urological use of LESS was reported in 2007 with the completion of single-port nephrectomy for a small nonfunctioning kidney, as well as transperitoneal ureterolithotomy[3,6]. To date, there is extensive experience with LESS in adult and pediatric urology in extirpative and nonextirpative procedures such as pyeloplasty, varicocelectomy and orchidopexy[3]. In other specialties such as gynecology, LESS has been used for several years, making single incision laparoscopic tubal ligation one of the most popular procedures in that field[17-19].
Multichannel ports can be used during LESS as one access approach. These devices allow for the insertion of instruments and a camera and involve a single fascial incision. TriPort (Advanced Surgical Concepts, Bray, Ireland) is the best-known FDA-approved access system. The size of the TriPort is fully adjustable, and allows a series of instruments to be introduced into any sized abdominal incision, from a 5 mm incision up to a hand-assisted laparoscopic surgery incision. Each device consists of a retractor component and a valve component, where the instruments are inserted. The valve component of TriPort is made of a unique elastomeric material that allows the passage of standard laparoscopic instruments and scopes simultaneously. The TriPort has three inlet valves: one for a 12-mm instrument and two for 5-mm instruments. QuadPort (Olympus, Advanced Surgical Concepts) is also available, and has four ports: two inlets for 12-mm instruments and two for 5-mm instruments. A separate insufflation port is provided through the valve housing in both devices. The high elasticity of the gel valve allows the removal of small specimens, whereas larger specimens are withdrawn into the distal end of the port and removed simultaneously with the device at the end of the procedure (Figure 2).
The Uni-X Single Port Access Laparoscopic System (Pnavel Systems, Cleveland, OH, United States) is a single port with three working channels, which all accommodate specialized 5-mm laparoscopic instruments. The device is placed through an open access technique and requires a 2-cm fascial incision. Once passed into the abdomen, the port is anchored in place using fascial sutures that are placed before attaching the device to the patient. As with TriPort, Uni-X has a separate valve port for insufflation. Once the procedure is complete, the port is untied and the specimen is removed through the initial incision[6]. The GelPOINT system from Applied Medical Technology (Brecksville, OH, United States) accommodates varying abdominal walls and incision sizes, provides continuous access, and ensures improved articulation of 5-12-mm instruments. The Alexis wound protector/retractor offers atraumatic retraction and protection, maintains moisture at the incision site, while providing convenient extracorporeal resection and specimen retrieval. The SILS Port designed by Covidien Tyco Health Care (Mansfield, MA, United States) consists of a blue flexible soft-foam port, with access channels for three cannulae. The 5-mm cannula may be interchanged at any time during the procedure with a 5-12-mm cannula. The SILS Port adapts its configuration to the size of the cannulae while maintaining pneumoperitoneum (Figure 3). We have utilized in all our patients the SILS Port (Covidien, Tyco Health Care). It is our preferential access devise for all LESS procedures. It has a foam port that expands after insertion to prevent air leakage. It is significantly cheaper compared with the others at least on the Israeli market. The access port is easy inserted via a 2-cm incision that is performed within the umbilicus. During the procedure the 5-mm trocars can be easily replaced by 10-12-mm trocars during surgery when needed.
A basic tenet of laparoscopic surgery involves triangulation of instruments so as to produce adequate intracorporeal working space for anatomical dissection and manipulation of tissues. The parallel and close proximity of the right-hand and left-hand instrument shafts of standard laparoscopic instruments through a solitary port results in crowding of the laparoscope and the instruments, preventing appropriate triangulation. Articulated instruments were designed to overcome these challenges. Some of articulated instruments include the SILS Multiple Instrument Access Port manufactured by Covidien and the Laparo-Angle Articulating Instruments made by Cambridge Endoscopic Devices (Cambridge, MA, United States), articulating laparoscopic graspers (e.g., Real Hand; Novare Surgical Systems, Cupertino, CA, United States and Autonomy Laparo-angle; Cambridge Endo, Framingham, MA, United States), endoshears (Cambridge Endo), and laparoscopic needle drivers (Cambridge Endo). A combination of conventional and flexible (articulating) instruments provides improved intraoperative ergonomics and further facilitates dissection during surgery.
There are two types of telescope for LESS: 30° and 0°. Pelvic procedures require the use of a 30° lens directed upwards, whereas upper tract procedures need either a 30° lens facing downward or a 0° lens[20] (Figure 4).
We have utilized a 60-cm, 5-mm, 0° telescope (Karl Storz, Germany) for all LESS intra-abdominal or renal surgery, and a 30° telescope with a right-angle light cord adapter in order to move the camera further from the operating surgeon, minimizing incidental collision of instruments during pelvic surgery. We think that it is crucial to use a long 60-cm telescope with an adaptor that allows receiving a fair laparoscopic picture without interfering with the surgeons within the limited operative field (Figure 5).
The key problem with conventional laparoscopes is that they have a large extracorporeal profile, with a light cable exiting at 90°. This configuration leads to clashing of the instruments and camera during LESS. Thus, the ideal telescope for LESS should remove the light cord and camera head from the operative field. Low-profile camera systems have been introduced for this purpose.
Park and colleagues have developed a transabdominal magnetic anchoring and guidance system (MAGS), which can be used to control an intra-abdominal laparoscope and multiple working instruments introduced through a single 1.5-cm port[21]. Once passed into the abdomen, instruments are affixed to the abdominal wall using external magnetic anchors. Currently, the MAGS incorporates an internal camera system, two types of passive tissue retractors, and a robotic arm cauterizer. By fixing internal instruments to external magnetic anchors, this platform allows for unrestricted intra-abdominal movement of surgical instruments, creating the potential benefits of LESS while maintaining an operative perspective similar to that of standard laparoscopy. This system has the added benefit of allowing the surgeon to reposition instruments intraoperatively without additional incisions.
LESS is performed through a single abdominal incision, usually at the umbilicus. We and others have modified routine laparoscopic procedures in order to overcome the limitations of LESS. In general, a single port with multiple channels is used through which the laparoscope and the operative instruments are passed. The procedure usually involves two surgeons. As we have mentioned, pelvic procedures require the use of a 30° lens directed upwards, whereas upper tract procedures need either a 30° lens facing downward or a 0° lens[20].
We have performed LESS nephrectomy by a transperitoneal approach while the patient is in a flank position, utilizing the usual technique. In this setting, the retroperitoneal space is entered through the Told line utilizing Ligasure 5 mm-37 cm (Covidien). An articulating grasper (Covidien) and an articulating dissector (Cambridge Endo) are used in order to develop an operative space. Using both articulating instruments at this stage avoids extracorporeal hand cross and intracorporeal instrument collision. However, we have found particularly useful the use of both articulating instruments only at the initial stage of the surgery. After the initial dissection and the formation of an operative space, the articulating dissector can be easily replaced by a straight instrument such as Ligasure, allowing not only the dissection, but also rapid hemostasis, which shortens the time of the operation. After dissection of the colon away from the kidney, the ureter is identified and transected. Ligation of the hilum vessels is performed utilizing large Auto Suture hemostatic clips (Covidien). The specimen is retrieved into a laparoscopic bag and removed through one of the ports or together with the LESS port. No drain is needed for these cases. In the cases of large hydronephrosis and right-sided kidney, trans-flank holding stitches through the renal pelvis, in the same manner as used in laparoscopic pyeloplasty, can be used in order to facilitate renal dissection.
For single site laparoscopic gonadectomy, the LESS port is inserted in the same manner as for nephrectomy. Vascular control is achieved solely by utilizing the Ligasure system. In the case of varicocelectomy, laparoscopic dissection of the spermatic vein is performed sparing the spermatic artery and dissecting away the lymphatic vessels. Ligation of the spermatic vein is performed utilizing Auto Suture hemostatic clips (Endo Clip; Covidien Tyco Health Care) or using sealing devices such as the Ligasure system only without hemostatic clips.
R-LESS is performed through the same umbilical incision as for conventional LESS. When the SILS port (Covidien Tyco Health Care) is used, a finger is placed to guide introduction of two robotic trocars adjacent to the fascial incision through two separate fascial stab incisions. If using a GelPort (Applied Medical Technology), the access device is placed through the fascial incision and the robot is subsequently docked. The robotic cannulae utilized vary from 8 to 5 mm to accommodate the Endowrist (Intuitive Surgical, Sunnyvale, CA, United States) monopolar shears and the Endowrist Schertel Grasper, depending on the procedure to be performed.
Beyond the obvious better cosmetic results, advantages of LESS include reduced postoperative pain, reduced operative complications related to trocar insertion (e.g. wound infections, epigastric vessel injury and organ herniation), and easier specimen removal through a larger incision (specimens may be fragmented in the laparoscopic bag)[22,23]. Those benefits are especially relevant in pediatric and young populations in whom the esthetic outcome is crucial (Figure 6).
Not all patients will be candidates for single-site surgery[24]. As with any other minimally invasive surgical technique (laparoscopy or robotics), patient selection is a composite of clinical judgment, risk, benefits, alternatives and a well-informed patient. Other limitations of this technique are the added cost and the technical challenges of the procedure. The major limitation is the lack of working space. The surgeon and the assistant must maneuver in a small space, resulting in hand and instrument collisions. The laparoscopic surgery concept of triangulation is challenged with the single-port procedure, and the ability to move the scope is significantly limited by other instruments[25].
Specialized equipment for single-port procedures can be used to help overcome these technical challenges, including the use of articulating instruments, a flexible laparoscope or a 30° laparoscope, and instruments of varying lengths. Articulating instruments can help with triangulation because the operator is able to work with two instruments in a similar location inside the abdomen while his or her hands are separated on the outside of the abdomen. Other disadvantages of LESS are related to operative time and learning curve.
Almost all body cavities can be entered through a small skin incision, therefore, the theoretical applications of LESS seem to be unlimited. However in a practical way, this statement is not entirely correct. Although LESS has successfully been proved for almost all diagnostic, extirpative and reconstructive surgery, there are limitations inherent to patient selection, surgical skills of the team, operative time, setup of the operating room, and availability of devices. In urology, LESS has been principally described for renal, ureteral, and prostatic surgery. In the most specialized centers it is now used for adrenal, bladder and testicular minimally invasive surgery as well. Despite the slower introduction of LESS in the pediatric population, today various LESS procedures have been described in pediatric urology with apparently good results.
Nephrectomy for nonfunctioning kidney is a good example. In 2010 Koh et al[26] reported outcome in 11 LESS nephrectomies in pediatric patients (age range: 0.1-16.2 years, with a mean age of 5.7 years) using an umbilical incision. None of the patients required conversion to conventional laparoscopy or open surgery. However, an accessory port was used in five of 11 cases. Of the 11 patients, two were infants, aged 39 d and 3.5 mo. The mean operative time was 139 min (range: 85-205 min), and the mean hospital stay was 1.5 d (range: 1.0-2.1 d)[26]. Ham et al[27] reported their results in four LESS nephrectomies and two nephroureterectomies through a homemade transumbilical port in children, without intraoperative or postoperative complications. The median operation time was 112 min (range: 90-148 min), and the median blood loss was 30 mL (range: 0-50 mL). All patients were discharged on postoperative day 2. As the surgeon had gained experience, the length of the umbilical incision was decreased from 2.0 to 1.0 cm[27]. In another recent study, Ganpule et al[28] reported on 10 patients who underwent different LESS procedures through the umbilicus. Seven patients underwent nephrectomy and three pyeloplasty. Mean age of the nephrectomized patients was 3.14 ± 1.7 years; the mean operating room time was 97.5 ± 12.54 min. All procedures were technically successful[28].
Another usual application of LESS in pediatric urology is varicocelectomy. Kaouk et al[29] reported three consecutive adolescent patients who underwent transumbilical varicocelectomy without placement of any additional ports or conversion to open surgery. The mean operative duration was < 1 h and all patients were discharged on the same day as their surgery and none required rehospitalization. There was no varicocele recurrence, or intraoperative or postoperative complications including wound infection, hydrocele, or incision site herniation[29].
LESS pyeloplasty is another popular but technically demanding procedure. Desai et al[30] performed 17 pyeloplasties; two with robotic assistance. The mean operative time and blood loss were 236 min and 79 mL, respectively. There were no complications, but all cases required an additional 2-mm port to aid suturing. One case was converted to conventional laparoscopy. All patients were symptom-free post-procedure and postoperative imaging showed unobstructed drainage in 15 of the 16 patients for whom data were available[30]. White et al[7] performed eight pyeloplasties; one with the aid of the Da Vinci robotic platform. The mean operative time and blood loss were 233 min and 62.5 mL, respectively. Renographic follow-up was documented as within normal limits and there were no complications apart from a wound site hernia[7]. One of the most recent studies was done at the Bayi Children’s Hospital and included 24 pediatric patients with ureteropelvic junction obstruction who underwent transumbilical LESS pyeloplasty. All operations were successful. None was converted to open surgery and no additional sheath tube or incision besides umbilicus was needed. No intraoperative complications occurred. The mean operative time was 145 min, and the average blood loss -10 mL. Two patients had postoperative urinary fistula, which naturally disappeared at 4 and 7 d postoperatively, respectively. In follow-up, 23 of 24 patients demonstrated a significant decrease in renal pelvis diameter[31].
Orchidopexy has been performed with LESS as well. Noh et al[32] published the results of LESS orchidopexy in 17 patients with a median age of 11 mo (range: 3-43 mo). The study included two bilateral procedures and five primary Fowler-Stephens (FS) procedures. One patient underwent a staged FS orchidopexy, with the LESS technique utilized during the second stage. Median laparoscopic dissection time for each testis was 35 min (range: 22-40 min). There was no blood loss or intraoperative complications. In follow-up, all testes were noted to be in the scrotum without testicular atrophy[32].
Other LESS procedures have also been performed in pediatric urology, such as ureteral reimplantation and bladder augmentation. The data for this type of surgery is limited to case reports and small series[33,34] (Table 1).
| Ref. | Type of study | Procedure | Nopts | Operating time | Need for conversion | Complications/events | Blood loss |
| Koh et al[26] | Retrospective | Nephrectomy | 11 | 139 min | No | Acc. port in 5 | 20 mL |
| Kocherov et al[35] | Case Control | Nephrectomy | 8 | 65 min | No | None | None |
| Ganpule et al[28] | Retrospective | Nephrectomy | 7 | 97.5 min | No | None | None |
| Ham et al[27] | Prospective | Nephrectomy | 4 | 112 min | No | None | 0-50 mL |
| Ham et al[27] | Prospective | Nephro-UBil | 2 | 112 min | No | None | 0-50 mL |
| Kocherov et al[35] | Case Control | Gonadectomy | 4 | 37.5 min | No | None | None |
| Kocherov et al[35] | Case Control | Varicocelectomy | 6 | 26 min | No | None | None |
| Kaouk et al[29] | Retrospective | Varicocelectomy | 3 | < 1 h | No | None | None |
| Noh et al[32] | Retrospective | Orchidopexy | 17 | 35 min | No | None | None |
| Desai et al[30] | Retrospective | Pyeloplasty | 17 | 236 min | No | Acc. port in all | 79 mL |
| White et al[7] | Prospective | Pyeloplasty | 8 | 233 min | No | None | 136 mL |
| Zhou et al[31] | Prospective | Pyeloplasty | 24 | 145 min | No | Two urinary fistulas | 10 mL |
Since 2011 a total of 18 patients underwent 23 procedures at our department: eight patients underwent nephrectomy due to nonfunctioning kidneys; four had removal of bilateral intra-abdominal gonads; four had high ligation of spermatic vein (HLSV); one underwent hysterectomy; and the remaining one had bilateral HLSV. A 1-year-old child who required hysterectomy was diagnosed with 46 XY ovotestis disorder of sexual differentiation and was raised as a boy. He required the removal of ovary and hypoplastic uterus. In all the patients a multichannel single laparoscopic port (Covidien) inserted through a 2-cm skin incision was used in order to obtain access into the abdominal cavity. All the patients underwent LESS without complications within a reasonable operating time. No one required conversion to open or conventional laparoscopic surgery. In two patients with large hydronephrosis we utilized a transcutaneous holding stitch, which was introduced through the renal pelvis and allowed additional manipulation of the severely hydronephrotic kidney, facilitating dissection and avoiding a need for additional trocar insertion. All but one patient were discharged on the day of surgery or on the day after[35] (Table 1).
Thus far, LESS is no longer an experimental technique; however, there are only a few retrospective studies with a significant number of cases that can prove the efficacy and safety of this technique for different indications. The advantages of LESS still exist at a theoretical level, because no clear benefit on postoperative course and patient convalescence has been definitively proven. The only potential benefit of LESS remains the claimed cosmetic outcome. Another obvious limitation is the lack of comparative studies between LESS and standard laparoscopy in terms of clinical outcome. Only a few retrospective case-control studies have compared LESS with standard laparoscopic techniques. In one such study, LESS nephrectomy (11 procedures) demonstrated no difference in median operating room time (122 min vs 125 min), change in hemoglobin levels, analgesic use, length of hospital stay, or complication rate compared to standard laparoscopic nephrectomy (22 procedures)[22]. A limitation of this study, in addition to it being retrospective, was that patients had their nephrectomy specimens removed through an extension of the umbilical incision up to 4-6 cm, thus obscuring the possible benefits of LESS, such as shorter convalescence and reduced postoperative pain, compared with standard laparoscopy. These results might not indicate any advantages of LESS over standard laparoscopy[36]. We have also identified a similar historic group of patients from our database who underwent conventional laparoscopy and have compared their outcome to those patients undergoing the LESS technique[35]. This group included two patients with androgen insensitivity that underwent gonadectomy; four with nonfunctioning kidneys who underwent nephrectomy; and four who underwent HLSV. All patients in this group had similar parameters in terms of age and indications for surgery as the LESS group. Outcome data regarding operative time, narcotic requirements, length of hospitalization, and complication rate were obtained following chart review. In spite of the fact that in those patients who underwent LESS the operating time seemed to be longer, there was no difference in the length of surgery and intraoperative narcotic requirements between conventional laparoscopy and LESS. None of the patients in the LESS group required narcotic administration compared with three patients from the conventional laparoscopy group (one gonadectomy and two nephrectomies) who required postoperative narcotic treatment. LESS patients had shorter hospitalization compared with the conventional laparoscopy group, but only in the nephrectomy group.
LESS has proved to be immediately applicable in the clinical field of pediatric urology, being safe and feasible in the hands of experienced laparoscopic surgeons in well-selected patients. We believe that one of the future challenges for LESS in the pediatric population may be the treatment of nephrolithiasis. Despite promising early outcomes, the benefits of LESS are not obvious at present, with the only claimed advantage being cosmetic. Prospective randomized studies are required to define the benefits of this technique for patients as well as to elucidate the cost-effectiveness of the approach.
P- Reviewers: Liatsikos E, Papatsoris AG, Sofikerim M, Venkatachalam RV S- Editor: Song XX L- Editor: Kerr C E- Editor: Lu YJ
| 1. | Smaldone MC, Sweeney DD, Ost MC, Docimo SG. Laparoscopy in paediatric urology: present status. BJU Int. 2007;100:143-150. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 32] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 2. | Eskicorapci SY, Teber D, Schulze M, Ates M, Stock C, Rassweiler JJ. Laparoscopic radical nephrectomy: the new gold standard surgical treatment for localized renal cell carcinoma. ScientificWorldJournal. 2007;7:825-836. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 52] [Cited by in RCA: 47] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 3. | Raman JD, Bensalah K, Bagrodia A, Stern JM, Cadeddu JA. Laboratory and clinical development of single keyhole umbilical nephrectomy. Urology. 2007;70:1039-1042. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 275] [Cited by in RCA: 232] [Article Influence: 13.6] [Reference Citation Analysis (0)] |
| 4. | Gettman MT, Lotan Y, Napper CA, Cadeddu JA. Transvaginal laparoscopic nephrectomy: development and feasibility in the porcine model. Urology. 2002;59:446-450. [PubMed] |
| 5. | Kaouk JH, Haber GP, Goel RK, Crouzet S, Brethauer S, Firoozi F, Goldman HB, White WM. Pure natural orifice translumenal endoscopic surgery (NOTES) transvaginal nephrectomy. Eur Urol. 2010;57:723-726. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 98] [Cited by in RCA: 109] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 6. | Tracy CR, Raman JD, Cadeddu JA, Rane A. Laparoendoscopic single-site surgery in urology: where have we been and where are we heading? Nat Clin Pract Urol. 2008;5:561-568. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 164] [Cited by in RCA: 137] [Article Influence: 8.6] [Reference Citation Analysis (0)] |
| 7. | White WM, Haber GP, Goel RK, Crouzet S, Stein RJ, Kaouk JH. Single-port urological surgery: single-center experience with the first 100 cases. Urology. 2009;74:801-804. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 232] [Cited by in RCA: 216] [Article Influence: 13.5] [Reference Citation Analysis (0)] |
| 8. | Gill IS, Advincula AP, Aron M, Caddedu J, Canes D, Curcillo PG 2nd, Desai MM, Evanko JC, Falcone T, Fazio V. Consensus statement of the consortium for laparoendoscopic single-site surgery. Surg Endosc. 2010;24:762-768. [PubMed] |
| 9. | Wang L, Cai C, Liu B, Yang Q, Wu Z, Xiao L, Yang B, Chen W, Xu Z, Song S. Perioperative outcomes and cosmesis analysis of patients undergoing laparoendoscopic single-site adrenalectomy: a comparison of transumbilical, transperitoneal subcostal, and retroperitoneal subcostal approaches. Urology. 2013;82:358-364. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 12] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 10. | Cuesta MA, Berends F, Veenhof AA. The “invisible cholecystectomy”: A transumbilical laparoscopic operation without a scar. Surg Endosc. 2008;22:1211-1213. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 203] [Cited by in RCA: 185] [Article Influence: 10.3] [Reference Citation Analysis (0)] |
| 11. | Zhu JF. Scarless endoscopic surgery: NOTES or TUES. Surg Endosc. 2007;21:1898-1899. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 54] [Cited by in RCA: 54] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 12. | Pappalepore N, Tursini S, Marino N, Lisi G, Lelli Chiesa P. Transumbilical laparoscopic-assisted appendectomy (TULAA): a safe and useful alternative for uncomplicated appendicitis. Eur J Pediatr Surg. 2002;12:383-386. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 43] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 13. | Rao P, Desai MM, Gill IS, Rane A, Rao PP, Dombivli E. India: E-NOTES. A new paradigm: experience in 33 cases. J Urol. 2008;179:238. [RCA] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 14. | Michalik M, Frask A. Natural Orifice Transluminal Endoscopic Surgery. Polish J Surgery. 2008;80:51-53. |
| 15. | Kaouk JH, Goel RK. Single-port laparoscopic and robotic partial nephrectomy. Eur Urol. 2009;55:1163-1169. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 141] [Cited by in RCA: 129] [Article Influence: 8.1] [Reference Citation Analysis (0)] |
| 16. | Mishra RK. History of Minimal Access Surgery: World Laparoscopy Hospital. History of Minimal Access Surgery, October 7th. India, Cyber City, DLF Phase II, Gurgaon: NCR Delhi 2011; . |
| 17. | Wheeless CR Jr, Thompson BH. Laparoscopic sterilization: review of 3, 600 cases. Obstet Gynecol. 1973;42:303-306. |
| 18. | Singh KB. Tubal sterilization by laparoscopy: simplified technique. N Y State J Med. 1977;77:194-196. |
| 19. | Wheeless CR. A rapid, inexpensive, and effective method of surgical sterilization by laparoscopy. J Reprod Med. 1969;5:255. |
| 20. | White MA, Haber GP, Autorino R, Khanna R, Altunrende F, Yang B, Stein RJ, Kaouk JH. Robotic laparoendoscopic single-site surgery. BJU Int. 2010;106:923-927. [PubMed] |
| 21. | Park S, Bergs RA, Eberhart R, Baker L, Fernandez R, Cadeddu JA. Trocar-less instrumentation for laparoscopy: magnetic positioning of intra-abdominal camera and retractor. Ann Surg. 2007;245:379-384. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 155] [Cited by in RCA: 125] [Article Influence: 6.9] [Reference Citation Analysis (0)] |
| 22. | Raman JD, Bagrodia A, Cadeddu JA. Single-incision, umbilical laparoscopic versus conventional laparoscopic nephrectomy: a comparison of perioperative outcomes and short-term measures of convalescence. Eur Urol. 2009;55:1198-1204. [PubMed] |
| 23. | Pak CH, Baik S, Kim CS. Initial experience with retroperitoneal laparoendoscopic single-site surgery for upper urinary tract surgery. Korean J Urol. 2011;52:842-846. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 8] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 24. | Irwin BH, Cadeddu JA, Tracy CR, Kim FJ, Molina WR, Rane A, Sundaram CP, Raybourn III JH, Stein RJ, Gill IS. Complications and conversions of upper tract urological laparoendoscopic single-site surgery (LESS): multicentre experience: results from the NOTES Working Group. BJU. 2011;107:1284-1289. |
| 25. | Romanelli JR, Earle DB. Single-port laparoscopic surgery: an overview. Surg Endosc. 2009;23:1419-1427. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 281] [Cited by in RCA: 248] [Article Influence: 15.5] [Reference Citation Analysis (2)] |
| 26. | Koh CJ, De Filippo RE, Chang AY, Hardy BE, Berger A, Eisenberg M, Patil M, Aron A, Gill IS, and Mihir M. Desai. Laparoendoscopic Single-site Nephrectomy in Pediatric Patients: Initial Clinical Series of Infants to Adolescents. UROLOGY. 2010;76:1461. |
| 27. | Ham WS, Im YJ, Jung HJ, Hong CH, Han WK, Han SW. Initial experience with laparoendoscopic single-site nephrectomy and nephroureterectomy in children. Urology. 2011;77:1204-1208. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 21] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 28. | Ganpule A, Sheladiya C, Mishra S, Sabnis R, Desai M. Laparoendoscopic single-site urologic surgery in children less than 5 years of age. Korean J Urol. 2013;54:541-546. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 29. | Kaouk JH, Palmer JS. Single-port laparoscopic surgery: initial experience in children for varicocelectomy. BJU Int. 2008;102:97-99. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 159] [Cited by in RCA: 154] [Article Influence: 9.1] [Reference Citation Analysis (0)] |
| 30. | Desai MM, Berger AK, Brandina R, Aron M, Irwin BH, Canes D, Desai MR, Rao PP, Sotelo R, Stein R. Laparoendoscopic single-site surgery: initial hundred patients. Urology. 2009;74:805-812. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 258] [Cited by in RCA: 240] [Article Influence: 15.0] [Reference Citation Analysis (0)] |
| 31. | Zhou H, Sun N, Zhang X, Xie H, Ma L, Shen Z, Zhou X, Tao T. Transumbilical laparoendoscopic single-site pyeloplasty in infants and children: initial experience and short-term outcome. Pediatr Surg Int. 2012;28:321-325. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 16] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 32. | Noh PH, Vinson MA, Bansal D. LaparoEndoscopic Single Site orchidopexy for intra-abdominal testes in the pediatric population with a multichannel single port and flexible tip laparoscope. J Endourol. 2013;27:1381-1383. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 7] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 33. | Permpongkosol S, Ungbhakorn P, Leenanupunth C. Laparoendoscopic Single-Site Ureteral Reimplantation as a Treatment of the Single Ectopic Ureter. USA: Mary Ann Liebert, Inc 2011; . |
| 34. | Noguera RJS, Astigueta JC, Carmona O, De Andrade RJ, Luis S, Cuomo B, Manrique J, Gill IS, Desai MM. Laparoscopic Augmentation Enterocystoplasty Through a Single Trocar. Urology. 2009;73:1371-1374. |
| 35. | Kocherov S, Lev G, Shenfeld OZ, Chertin B. Laparoscopic single site surgery: initial experience and description of techniques in the pediatric population. J Urol. 2011;186:1653-1657. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 19] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 36. | Raman JD, Bagrodia A, Cadeddu JA. Single-Incision, Umbilical Laparoscopic versus Conventional Laparoscopic Nephrectomy: A Comparison of Perioperative Outcomes and Short-Term Measures of Convalescence. European Urology. 2009;55:1198-1206. |