Published online Nov 24, 2013. doi: 10.5410/wjcu.v2.i3.46
Revised: September 18, 2013
Accepted: November 1, 2013
Published online: November 24, 2013
Processing time: 170 Days and 16.5 Hours
AIM: To investigate and improve our out-patients department patient satisfaction, provide minimum consultation delay and appropriate consultation duration to meet with targets.
METHODS: We distributed the modified satisfaction with outpatient service (SWOPS) questionnaires developed for use in Irish hospitals by the Health Services Research between August and December 2012. The patient disclosed their age and sex and completed the modified SWOPS questionnaire anonymously. Every patient was eligible to participate in the study who attended any of the Urology Outpatient Clinics. Patients lacking capacity to consent were excluded. Additionally, each patient was only permitted to complete one questionnaire regardless of repeat attendances within the 4 mo study period. The answers to every question were presented as percentages. One-way ANOVA was used to establish whether there was a significant difference in appointment delay and “Overall Satisfaction” on the different clinic days. The unpaired t-test was applied to establish whether “Overall Satisfaction” was affected by diagnosis (benign or malignant). Paired t-test was used to establish whether “Overall Satisfaction” was affected by appointment delay and appointment length.
RESULTS: Three hundred and forty-eight questionnaires were completed with an overall > 65% participation rate. Eighty-one point six percent were male and 18.4% female with a mean age of 65 ± 21 years. Mean delay time was 32 min, which 30.6% stated should be an improvement priority. The delay times for Wednesday (mean 13 min) were significantly (P < 0.05) lower than for other days (mean 36 min). Generally 12-15 min outpatient appointment length is acceptable and adequate for patients as 97.70% suggested, however 31.60% of patients would favour longer duration. Eleven point four nine percent do not want to see different doctors each time, and 31.60% of the patient feel that no change is required. Average satisfaction was 84.65%. There was no significant relationship between satisfaction and clinic day, diagnosis and consultation length, whether the patient was reviewed by a registrar or consultant. Satisfaction was universally high and independent of consultation delay/length and diagnosis. Dissatisfaction in delay times with a significant improvement on Wednesday suggests necessary and achievable improvements. Notably, the Wednesday clinic has less patients per doctor per hour and enforces a 1 patient per 15 min slot with a no over-booking policy.
CONCLUSION: Surveying our patient dissatisfaction would require more frequent audits by clinicians to improve patient satisfaction and to achieve better quality of care.
Core tip: With our survey we would like to emphasize the need of regular audit activity at the outpatient clinic to improve patient satisfaction and to identify potential pitfalls of the outpatient pathway. Ideally every outpatient clinic or medical practice should conduct a survey yearly for quality improvement purposes to improve patient care and outcomes through systematic review of care against explicit criteria and implement changes if necessary.
- Citation: Lukacs S, Tschobotko B, Mukerji G, Vale J, Mazaris E. How to improve a urology outpatient service? A survey of patient satisfaction. World J Clin Urol 2013; 2(3): 46-52
- URL: https://www.wjgnet.com/2219-2816/full/v2/i3/46.htm
- DOI: https://dx.doi.org/10.5410/wjcu.v2.i3.46
The National Health Service (NHS) in the United Kingdom and the health system in the United States of America seek to develop so called “patient centred care”[1,2], as patient perception of their healthcare experience has gained increasing attention over the past 20 years[3]. Researching patients’ healthcare experience is an important method of creating effective action plans for quality improvement in health care organisations[4].
Currently, there is a drive for reducing patient waiting times for the benefit of patients, healthcare providers, managers, and Department of Health. Consequently, Out-patient clinics have also been subject to new targets. The Department of Health’s Operating Framework for 2012/13[5] confirmed the NHS Constitution guarantees that patients should expect to receive treatment for non-urgent conditions at an inpatient or outpatient basis within 18 wk. In addition all GP referrals with suspected malignancy should receive specialist review within 2 wk.
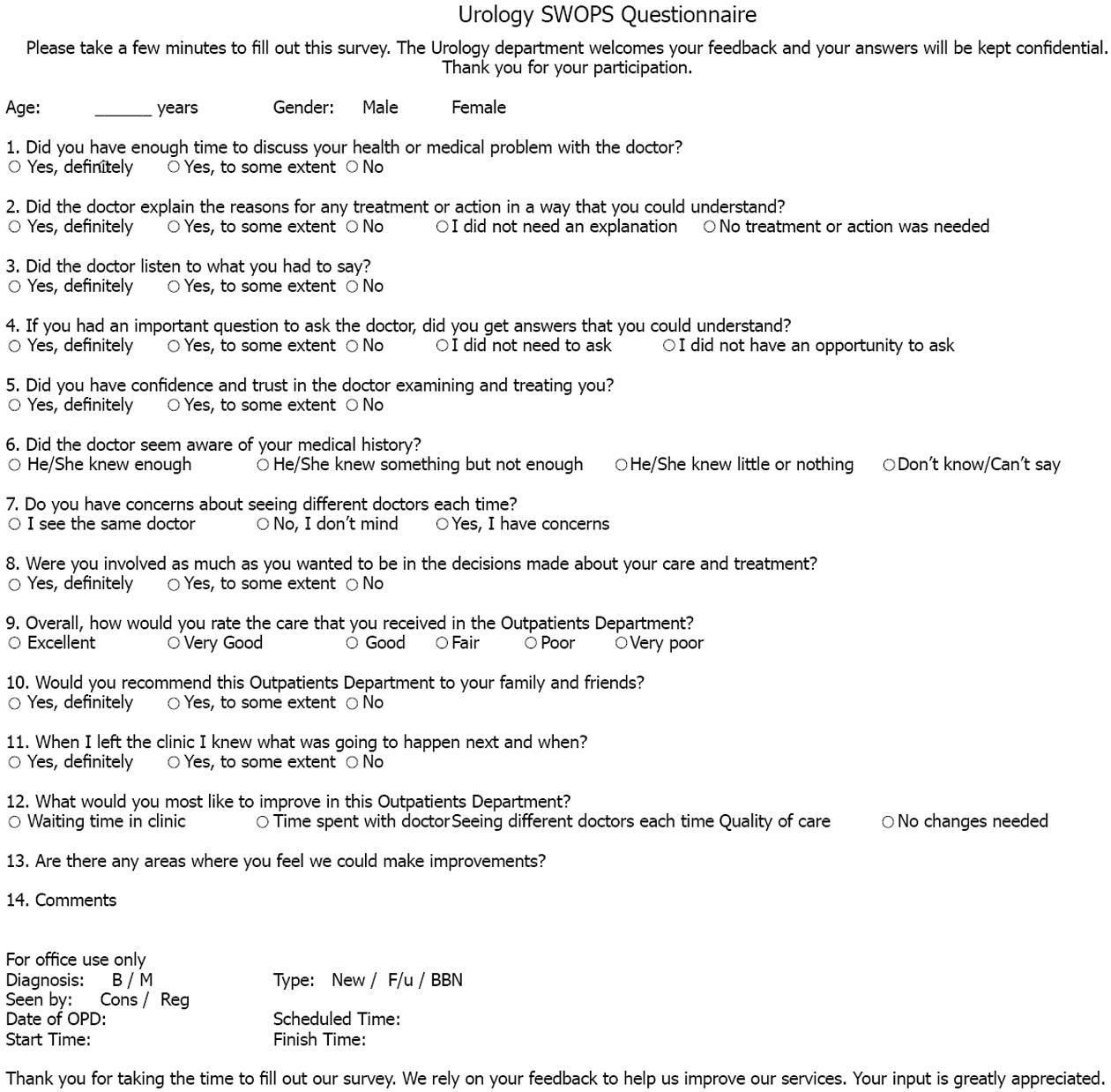
As we are searching for ways to make our Outpatient’s Department service more responsive to the general public and in order to improve the patient experience at our Urology Out-Patient’s Department, we conducted a prospective study of patient satisfaction among patients attending between August 2012 and December 2012. Our modified satisfaction with outpatient service (SWOPS) questionnaires (Figure 1) were used. St Mary’s Urology out-patients department targets maximum patient satisfaction as it is one of the key criteria by which the quality of health care service is evaluated[6,7]. This survey aimed to develop a framework for identifying factors affecting patient satisfaction, and to identify potential, and correctable causes in order to improve overall satisfaction and healthcare quality improvement. Therefore we focused on patient dissatisfaction in order to identify reasons which make patients disappointed with the service provided.
The survey was performed in four Outpatient Urology Clinics held weekly (Monday, Wednesday, Thursday and Friday) at St Mary’s Hospital, Imperial Healthcare NHS Trust, London. These are led by the same 2 consultants and 2 registrars. Patients were seen, reviewed and consulted randomly; the next patient was seen by the next available doctor. It is of note, that Wednesday clinic has less patients per doctor per hour and enforces a 1 patient per 15 min slot with a no over-booking policy, which results into a smooth continuously flowing clinic without significant delays.
Data was collected prospectively between August 2012 and December 2012 using our modified SWOPS questionnaires (Figure 1). The SWOPS questionnaire is multi-dimensional outpatient instrument, which was developed for use in Irish hospitals by the Health Services Research Centre at the Department of Psychology, Royal College of Surgeons in Ireland (RCSI). The generic items of the questionnaire make up an overall dimension with an α co-efficient of 0.84. The high reliability co-efficient of each of these dimensions allows users to “select” questions whilst maintaining validity. Therefore the modified SWOPS questionnaire is valid[8], Every patient who attended our four Urology clinics was asked to complete the modified SWOPS questionnaires, the doctor completed sections including consultation length and delay, diagnosis (benign or proven malignant), whether the consultation was Registrar or Consultant led and whether the patient was new or follow-up. The patients disclosed their age and sex and completed 12 of the questions of the modified SWOPS questionnaire anonymously. At the end of the questionnaire 2 open questions were provided for the patients to express their personal view, impression and recommendations. Every patient was eligible to participate in the survey who attended the Urology Outpatient Clinic. Patients with diagnosed mental health disorder and patients lacking capacity to consent to completing the questionnaire were excluded. Additionally, each patient was only permitted to complete one questionnaire regardless of repeat attendances within the 4 mo study period. Doctors were unaware of the collected data and feedback until the end of the survey. The Questionnaire was completed at the end of the consultation by the patient in the waiting area and were collected at the Outpatient Department Reception in a sealed container.
The responses to each question by each patient were recorded onto Microsoft Excel spreadsheet 2010. The number of answers were recorded as percentages. The responses to the “scalable” questions (Questions 1-6 and Questions 8-11) were recorded as a percentage of the maximum score for that question. In order to ensure that these questions were consistently “scalable” for the calculation of “Overall Satisfaction” the following rules were applied: (1) For Question 2, response options 4 and 5 were not taken into account (for the calculation of overall satisfaction); (2) For Question 4, response options 4 and 5 were not taken into account; (3) For Question 6, response option “Don’t Know” was excluded.
The average percentage score, i.e., “Overall Satisfaction” was then calculated.
The unpaired t-test was applied to establish whether “Overall Satisfaction” was affected by diagnosis (benign or malignant).
The paired t-test was used to establish whether “Overall Satisfaction” was affected by appointment delay and appointment length.
Furthermore one-way ANOVA was used to establish whether there was a significant difference in appointment delay and “Overall Satisfaction” on the different clinic days.
The survey had an overall > 65% participation rate. A total of 348 patients completed and returned the questionnaire. The demographic characteristics of the survey consisted of 284 males (81.6%) and 64 females (18.4%) with an average age of 61 years and a mean age 65 ± 21 years. 29.88% of patients (n = 104) were new referrals to the clinic with no previous experience with the Department and 244 (70.12%) were at least seen once previously so called follow up patient. All clinics were a mixture of patients diagnosed with benign and malignant urological diseases. Overall 214 (61.49%) patients attended clinic for benign urological problems and 134 (38.51%) for a histologically proven malignancy either as a new diagnosis or follow up. One hundred and fifty-six (44.82%) patients were seen by the Consultant and 192 (55.17%) patients by the registrars. Groups seen by Consultant and registrar were identical demographically (age, sex), in terms of medical condition (new or follow up) and histological diagnosis (benign or malignant) as a result of random outpatient consultation. Overall statistical analysis did not reveal any significant difference between consultant and registrar led consultation in duration time, delay of consultation, and patient satisfaction (Table 1).
| Consultant led clinic | Registrar led clinic | |||
| Mean | SD | Mean | SD | |
| Consultation time (min) | 13.61 | 10.58 | 13.81 | 10.19 |
| Delay of consultation (min) | 33.71 | 18.84 | 36.48 | 20.22 |
| Patient satisfaction | 0.90 | 0.14 | 0.89 | 0.12 |
The number of patients who completed the questionnaire for every clinic were respectively for the Monday clinic 98 (28.16%), Wednesday clinic 52 (14.94%), Thursday clinic 74 (21.26%), Friday clinic 124 (35.63%).
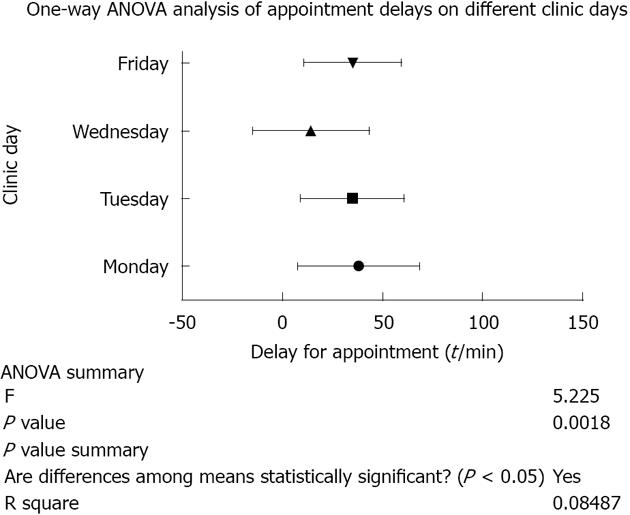
Analysis of the Appointment Length and Appointment Delay Times (Table 2), clearly showed similarities in appointment or consultation length by average of 13 min per consultation. On Question 12, only 16.66% (n = 58) of the patients found this consultation length inadequate. Further analysis of Appointment Delay time to patient schedule showed that notably Wednesday appointment delay length was only 14 min far less compared with other clinics, where patients have nearly 35-min delay to see the doctor. One-way ANOVA Analysis of Appointment Delays on Different Clinic Days (Figure 2) is statistically significantly different with a P value of less than 0.0018. On Question 12, 31.60% (n = 110) of patients stated the waiting time in clinic needs to improve.
| Clinic day | Appointment delayed length mean(min) | Appointment delayed ± SD(min) | Appointment length mean(min) | Appointment length ± SD |
| Monday | 38 | 30 | 13 | 7 |
| Wednesday | 14 | 28 | 12 | 9 |
| Thursday | 35 | 25 | 14 | 12 |
| Friday | 35 | 23 | 14 | 11 |
Analysis of the individual Clinic days (Table 3), showed no statistically significant difference between the clinic days or whether the visit was a result of a benign or malignant diagnosis. However, the Wednesday clinic had the highest overall satisfaction rate with 87.7% of the attending patients with the lowest standard deviation compared with any other clinic days.
| Factor | Satisfaction (%) | SD |
| Monday clinic | 83.4 | 16 |
| Wednesday clinic | 87.7 | 15.7 |
| Thursday clinic | 83.2 | 17.7 |
| Friday clinic | 84.3 | 18.9 |
| Benign diagnosis | 83 | 18.6 |
| Malignant diagnosis | 86 | 15.3 |
The individual answers to the questions of the questionnaire are presented in percentages in Table 4.
| Question | Total responses | Response | Responses |
| Question 1 Did you have enough time to discuss your health or medical problem with the doctor? | 348 | Yes, definitely | 242 (69.54) |
| Yes, to some extent | 98 (28.16) | ||
| No | 8 (2.29) | ||
| Yes, definitely | 252 (72.41) | ||
| Yes, to some extent | 72 (20.68) | ||
| Question 2 Did the doctor explain the reasons for any treatment or action in a way that you could understand? | 348 | No | 8 (2.29) |
| I did not need an explanation | 6 (1.72) | ||
| No treatment or action was needed | 10 (2.87) | ||
| Yes, definitely | 268 (77.01) | ||
| Question 3 Did the doctor listen to what you had to say? | 348 | Yes, to some extent | 80 (22.98) |
| No | 0 (0) | ||
| Yes, definitely | 202 (58.04) | ||
| Yes, to some extent | 94 (27.01) | ||
| Question 4 If you had an important question to ask the doctor, did you get the answers that you could understand? | 348 | No | 14 (4.02) |
| I did not need to ask | 30 (8.62) | ||
| I did not have an opportunity to ask | 8 (2.29) | ||
| Yes, definitely | 260 (74.71) | ||
| Question 5 Did you have the confidence and trust in the doctor examining treating you? | 348 | Yes, to some extent | 82 (23.56) |
| No | 6 (1.72) | ||
| He/she new enough | 234 (67.24) | ||
| Question 6 Did the doctor seem aware of yor medical history? | 348 | He/she knew something but not enough | 88 (25.28) |
| He/she knew little or nothing | 16 (4.59) | ||
| Don’t know/Can’t say | 10 (2.87) | ||
| I see the same doctor | 74 (21.26) | ||
| Question 7 Do you have concerns about seeing different doctors each time? | 348 | No, I don’t mind | 214 (61.49) |
| Yes, I have concerns | 60 (17.24) | ||
| Yes, definitely | 204 (58.62) | ||
| Question 8 Were you involved as much as you wanted to be in the decisions made about your care and treatment? | 348 | Yes, to some extent | 136 (39.08) |
| No | 8 (2.29) | ||
| Excellent | 120 (34.48) | ||
| Very good | 100 (28.73) | ||
| Question 9 Overall, how would you rate the care that you received in the Outpatients Department? | 348 | Good | 80 (22.98) |
| Fair | 30 (8.62) | ||
| Poor | 14 (4.02) | ||
| Very poor | 4 (1.11) | ||
| Yes, definitely | 212 (60.91) | ||
| Question 10 Would you recommend this Outpatients Department to your family and friends? | 348 | Yes, to some extent | 124 (35.63) |
| No | 12 (3.44) | ||
| Yes, definitely | 246 (70.68) | ||
| Question 11 When I left the clinic I knew what was going to happen next and when? | 348 | Yes, to some extent | 94 (27.01) |
| No | 8 (2.29) | ||
| Waiting time in clinic | 110 (30.60) | ||
| Time spent with doctor | 58 (16.66) | ||
| Question 12 What would you most like to improve in this Outpatients Department? | 348 | Seeing different doctors each time | 40 (11.49) |
| Quality of care | 30 (8.62) | ||
| No changes needed | 110 (31.60) |
A prospectively administered exit survey questionnaire is a reasonably effective way of eliciting the view of members of the public but it is important to be aware of the limitation of this method. Firstly response rate can be often quite low and depends on the quality of the questionnaire, the clinical set up, the selling point of the questionnaire and also the willingness of those approached in this way to respond truly. Patients who are extremely satisfied or dissatisfied will more commonly be willing to express their feelings, and fill the questionnaire which can result in a significant bias for the study. Our survey participation rate after excluding the ineligible patients was 65%.
For better understanding of the large amount of data collected, we divided the questionnaires into 3 major areas. First was the sufficient appointment length surveyed by the first question. Generally a 12-15 min outpatient appointment length is acceptable and adequate for patients as 97.70% were not dissatisfied, however, when patients answered the last question 16.66% of them would like to spend more time with their doctor. We concluded that an average of 20 min consultation time (3 patients/h) would be satisfactory for both doctors and patients. This would result at an average of 12 patients over a half day clinical session. The second part is focus on doctor-patient interaction and communication (Q 2, 3, 4, 5, 6, 7, 8, 11). Good communication between patients and healthcare professionals has long been seen as the bedrock of quality from the patient’s perspective[9]. Generally doctors and healthcare professionals are appreciated more when they are genuinely interested in what patients have to say or ask, when they provide clear explanation and examples about the possible treatment options, as well as offer sufficient time for patient interaction. Direct patient involvement by having the opportunity to choose treatment options or decision how to manage their condition is becoming more common[10]. A shared decision approach may be the preferred way, however the extent of patient involvement in their decision making process is dependent upon the background knowledge and education. Our survey results showed that generally patients were happy, however, in some cases the lack of notes resulted in lack of confidence and dissatisfaction for the doctor and the Department. Therefore this group of questions focused on the received care, expectations and area of improvement (Q9, 10, 12).
Furthermore we concluded the following from the patient answers (Table 3): Question two highlights the importance of good patient/doctor interaction and involvement in the decision making process to improve patient understanding of their disease and medical management plan, resulting in improvement of patient compliance to treatment. Question three indicates the importance of doctor/patient interaction, especially underlining the importance of active listening to the patient. Question four demonstrated that answering patient questions about their problem is extremely important, however, that should be explained in a way that the patient understands. In question five 1.72% of the patients have no confidence in their doctor, a fact probably difficult to correct, however 74.71% answered “Yes, definitely” and 23.56% answered “Yes, to some extent” being confident in their doctor. Patient perception of the delivered quality of care is commonly measured by the doctors’ knowledge of patient’s disease and past medical history. Question six supported that most patients were generally satisfied (92.52%) with our service, however, improvement was required to satisfy the remaining 7.5%. Question seven surprisingly revealed, that patients not necessarily wanted to see the same doctor, providing that their medical records were updated and the presently treating medical doctor were made aware of their condition. Question eight suggested that 97.70% of patients feel that the consultation was adequately managed, and they were involved in the decision making process fully in 58.62%. Question nine revealed that an overall 86.20% had excellent or good opinion about the care that they received, 8.62% found it fair, however 6.32% of the patients were dissatisfied (18 patients in total). Both the 14 questionnaires which found our service poor and the remaining 4 that found it very poor were analysed independently. Overall from the group of these 18 patients, 17 would probably have been satisfied with the department, however their average delay to be seen was more than 65 min, which resulted to major disappointment. The remaining patient was dissatisfied as he was delayed by 45 min, his notes were missing and the doctor was unaware of his history. Question ten confirmed however, when it is about recommending the department to family members only 3.44% of the patients would not make such a recommendation, which might suggest individual or personal issues, and was independent from the quality of care which they received. Question eleven underlines the importance of sharing future management plan with patients to improve patient compliance. At last but not least question twelve highlights the expectation of the patient and suggestion for further improvement. Thirty-one point six percent of patients seemed happy with the present status quo, however that does not necessarily mean a happy customer. Moreover there is plenty of room for improvement as 76.43% would favour changes to improve service delivery. By far more than 31.6% of patients would like to reduce the waiting time in the clinic (time spent in the department waiting for consultation), which turned out one of the independent factors influencing patient satisfaction.
Some outpatient urology clinics are performing minimal invasive procedures as well during their outpatient consultation, such as flexible cystoscopies, prostatic biopsies or even ureteric stenting[11]. In these circumstances a sufficient pain management is mandatory and could result in further improvement in patient satisfaction[12] and outpatient service.
Alternatively for the measurement of patient satisfaction the Patient Satisfaction Questionnaire Short Form (PSQ-18) can also be used, which is an adaptable, reliable, and validated tool that may be applied to various settings, as well as comparing interventions[13,14].
It seems that in the era of financial constraints, hospital managers focus more on the number of patients seen in clinic in order to reduce waiting times, satisfy targets and earn more financially for their hospitals. However, quantity is not only what matters, quality in the delivery of care has to be a priority for every physician. Therefore it is very important to evaluate patient satisfaction and implement new strategies to provide quality care to our patients.
Patient satisfaction gained increasing attention over the past 20 years as one of the primary factors to measure quality of care. The findings of this study are important because, to our knowledge, such specific outpatient survey and feedback is rarely undertaken in the hospital setting. Satisfaction surveys are mainly used by hospital managers who evaluate their staff in their working environment.
In an era when reductions in patient waiting times (and to meet the increasing demand) is the main priority of all parties (patient, healthcare provider, managers, and ministry), organizing and running an effective outpatient clinic could face a major challenge. On this ground more and more clinicians are trying to come up with a solution to improve patient satisfaction by not compromising managerial and financial targets at the same time.
Satisfaction with outpatient service (SWOPS) questionnaire is multi-dimensional outpatient instrument, was developed by the Health Services Research Centre at the Department of Psychology, Royal College of Surgeons in Ireland for use in Irish hospitals. The generic items of the questionnaire make up an overall dimension with an α co-efficient of 0.84. The high reliability co-efficient of each of these dimensions allows users to “select” questions whilst maintaining validity, providing a valid questionnaire for researchers and clinicians to audit their patient satisfaction and outcomes.
SWOPS questionnaire can be used in any clinical setting from outpatient to inpatient and ward setting. Also it is a useful tool in the primary care to monitor quality of care.
Patient satisfaction is the perception of the patient of one or more aspects of the received care, thus a tool for measuring quality of care.
This is an interesting topic as outpatient department service is very important in the diagnostic, therapeutic and follow-up process of many urological pathologies.
P- Reviewers: Hakenberg OW, Mazaris E, Papatsoris AG, Soria F S- Editor: Song XX L- Editor: A E- Editor: Liu XM
| 1. | Department of Health. The NHS plan. London: Department of Health 2000; 88-95 Available from: http://webarchive.nationalarchives.gov.uk/20130107105354/http://www.dh.gov.uk/prod_consum_dh/groups/dh_digitalassets/@dh/@en/@ps/documents/digitalasset/dh_118522.pdf. |
| 2. | Institute of Medicine. Crossing the quality chasm: a new health system for the 21st century. Washington D.C. : National Academy Press 2001; . |
| 3. | Coulter A. The Autonomous Patient: Ending Paternalism in Medical Care. London: Stationery Office (for the Nuffield Trust) 2002; 128. |
| 4. | Levine AS, Plume SK, Nelson EC. Transforming patient feedback into strategic action plans. Qual Manag Health Care. 1997;5:28-40. [PubMed] |
| 5. | Available from: https://www.gov.uk/government/publications/the-operating-framework-for-the-nhs-in-england-2012-13. |
| 6. | Young GJ, Meterko M, Desai KR. Patient satisfaction with hospital care: effects of demographic and institutional characteristics. Med Care. 2000;38:325-334. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 280] [Cited by in RCA: 271] [Article Influence: 10.8] [Reference Citation Analysis (0)] |
| 7. | Goldwag R, Berg A, Yuval D, Benbassat J. Predictors of patient dissatisfaction with emergency care. Isr Med Assoc J. 2002;4:603-606. [PubMed] |
| 8. | Keegan O, McGee H. A guide to hospital outpatient satisfaction survey: practical recommendations and the Satisfaction with Outpatient’ (SWOP) Questionnaire. Dublin: Royal College of Surgeons in Ireland 2003; . |
| 9. | Grol R, Wensing M, Mainz J, Jung HP, Ferreira P, Hearnshaw H, Hjortdahl P, Olesen F, Reis S, Ribacke M. Patients in Europe evaluate general practice care: an international comparison. Br J Gen Pract. 2000;50:882-887. [PubMed] |
| 10. | Sitzia J, Wood N. Patient satisfaction: a review of issues and concepts. Soc Sci Med. 1997;45:1829-1843. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 956] [Cited by in RCA: 938] [Article Influence: 33.5] [Reference Citation Analysis (0)] |
| 11. | Masood J, Ismail M, El-Husseiny T, Moraitis K, Albanis S, Papatsoris A, Buchholz N. ‘An interventional urology list’ - a novel concept for UK urological services. Ann R Coll Surg Engl. 2011;93:27-30. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 6] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 12. | Young A, Ismail M, Papatsoris AG, Barua JM, Calleary JG, Masood J. Entonox® inhalation to reduce pain in common diagnostic and therapeutic outpatient urological procedures: a review of the evidence. Ann R Coll Surg Engl. 2012;94:8-11. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 23] [Cited by in RCA: 26] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 13. | Dawn AG, Lee PP, Hall-Stone T, Gable W. Development of a patient satisfaction survey for outpatient care: a brief report. J Med Pract Manage. 2003;19:166-169. [PubMed] |
| 14. | Marshall GN, Hays RD, Santa Monica. The patient satisfaction questionnaire short form (PSQ-18). CA: RAND Corporation 1994; 7865. |