Peer-review started: December 2, 2023
First decision: December 19, 2023
Revised: December 28, 2023
Accepted: January 22, 2024
Article in press: January 22, 2024
Published online: February 2, 2024
Processing time: 61 Days and 21.2 Hours
Upper tract urothelial carcinoma (UTUC) representing only a small fraction of all urothelial tumors. It predominantly affects the renal pelvis in men, often coexisting with bladder carcinoma. UTUC displays a more aggressive genetic profile compared to bladder neoplasms, with the majority of patients presenting with advanced disease. Histologically, about a quarter of UTUC cases exhibit high-grade subtypes, associated with a worse prognosis. Tobacco use and past exposure to aromatic amines are significant risk factors for UTUC. Imaging mo
We present a case of an 84-year-old woman who underwent percutaneous endoscopic excision of a renal pelvis neoplasm using the Tullio laser. Despite successful tumor removal, the patient experienced a postoperative complication with abdominal fluid leakage. Conservative management effectively resolved the complication. Given the patient's age and refusal for radical surgery, the conservative approach proved to be a valid therapeutic choice.
Overall, UTUC remains a diagnostic and therapeutic challenge due to its rarity. However, advances in endoscopic and percutaneous techniques provide valuable alternatives for selected patients, warranting further exploration in this evolving field.
Core Tip: Upper tract urothelial carcinoma remains a diagnostic and therapeutic challenge due to its rarity. Advances in endoscopic and percutaneous techniques provide valuable alternatives for selected patients, warranting further exploration in this evolving field. However, complications from these new procedures are still infrequent, and their treatment or management poses a new challenge for the doctor. With this case, we aim to propose a damage management approach to handle future complications.
- Citation: Bernabei M, Fabbri N, Romeo D, Paiolo E, Bandi M, Simone M. Conservative management of an early abdominal complication during a Tullio percutaneous endoscopic excision of renal pelvis urothelial carcinoma: A case report. World J Clin Urol 2024; 13(1): 1-6
- URL: https://www.wjgnet.com/2219-2816/full/v13/i1/1.htm
- DOI: https://dx.doi.org/10.5410/wjcu.v13.i1.1
Urothelial carcinoma is the fourth most common malignancy worldwide, ranking after breast (or prostate), lung, and colorectal cancer[1,2]. Among urothelial cell carcinomas, localized upper tract urothelial carcinoma (UTUC) is rare, representing only 5%-10% of all urothelial tumors[3]. Bilateral synchronous disease occurs in only 1%-5% of cases[4]. It is more prevalent in men, with a mean age of diagnosis at 65 years, and primarily affects the renal pelvis rather than the ureter, often coexisting with bladder carcinoma in 20% of cases[1]. UTUC presents a more aggressive genetic phenotype compared to bladder neoplasms (TCC-B), with 60% of patients presenting with advanced disease[5]. Approximately 25% of UTUC cases exhibit different histological subtypes, which are high-grade and have a worse prognosis compared to pure urothelial carcinomas. Rare subtypes include sarcomatoid and 'inverted growth pattern' types[6,7]. The most significant risk factor is tobacco use, which increases the relative risk from 2.5 to 7[2]. Occupational exposure to aromatic amines such as benzidine and beta-naphthylamine, though these substances have been banned from industrial production since 1960, is another risk factor[1]. Uro-computed tomography (CT) is the preferred imaging modality, while MRI is a valid alternative in cases of iodine-based contrast media contraindication[1]. Ureterorenoscopy, both semi-rigid and flexible, is essential for direct visualization of the lesion[8], allowing for biopsy sampling. The obtained grading is often used for approximate staging, given the small size of the biopsy samples and difficulty in obtaining depth due to the risk of perforation and neoplastic dissemination[2,8]. For decades, the "gold-standard" treatment for all cases of UTUC has been nephroureterectomy with excision of the bladder cuff. However, in 2018, a recommendation for a conservative approach in all "low-risk" cases emerged[1,5].
In the latest European guidelines, the conservative surgical approach has taken on an increasingly prominent role, with strong recommendations in "low-risk" pathology[6]. The "endoscopic" conservative treatment, particularly in selected patients, has shown oncological results equivalent to radical surgery[7].
In a large cohort of "high-risk" patients treated with conservative surgery, relatively high and comparable overall survival (OS) and cancer-specific survival (CSS) have been documented, consistent with previous studies even after 10 years of follow-up[6].
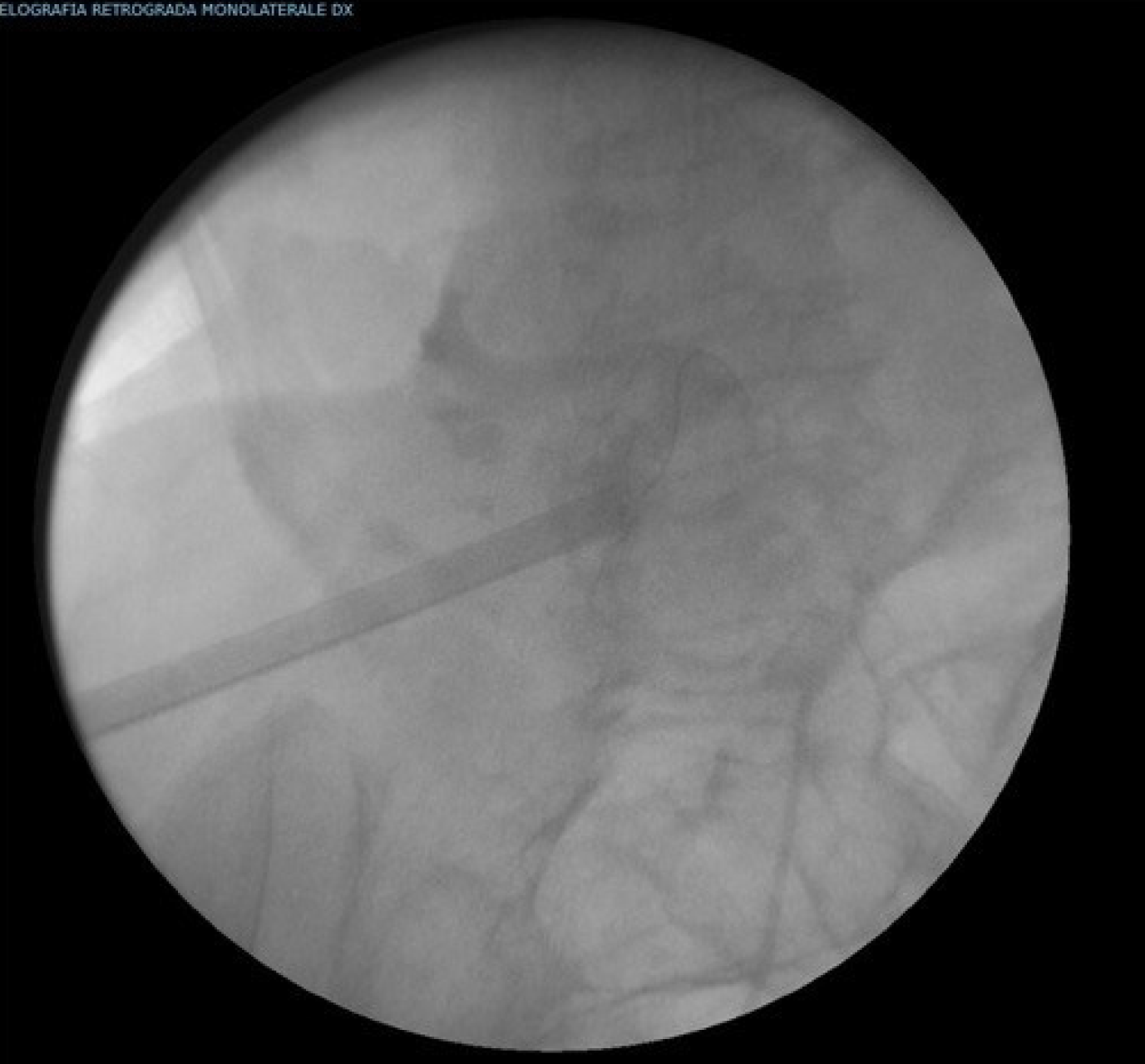
Retrograde approach is indicated for smaller malignancies of the distal ureter[8], utilizing lasers for improved visualization and ablative capacity, although staging limitations and the risk of neoplastic dissemination persist[4]. Percu
The novelty of this clinical case lies in the unique presentation of the complication, unprecedented in the literature, and our proposed treatment approach, which did not rely on previous guidelines or suggestions.
The novelty of this clinical case lies in the unique presentation of the complication, unprecedented in the literature, and our proposed treatment approach, which did not rely on previous guidelines or suggestions.
An 84-year-old woman was admitted to our Urology Department at the Lagosanto Hospital in Ferrara for percutaneous resection of a neoformation in the right renal pelvis (approximately 15 mm diameter). The diagnosis was made through contrast-enhanced CT, performed as part of a follow-up for intermediate-risk non-muscle invasive bladder cancer (TCC-B).
On December 14, 2022, the patient underwent a combined retrograde endoscopic approach using digital flexible ureterorenoscopy and antegrade percutaneous approach to the renal pelvis (using a Dresden nephroscope with a 24 Ch Nephromax balloon) with "endovision" technique for "en bloc" laser ablation of the pelvis neoformation using the Tullio Revolix 200 Laser (Figure 1).
At the end of the procedure, an 8 cm percutaneous nephrostomy tube (PCN) and an "open end" 6 cm ureteral catheter were left in place, anchored to an 18 cm Foley catheter.
The patient had previously undergone multiple endoscopic resections at another facility. Her medical history included atrial fibrillation, hypertension, and two previous abdominal surgeries (appendectomy and left colon resection for neoplasia in 2011).
Her medical history included atrial fibrillation, hypertension, and two previous abdominal surgeries (appendectomy and left colon resection for neoplasia in 2011).
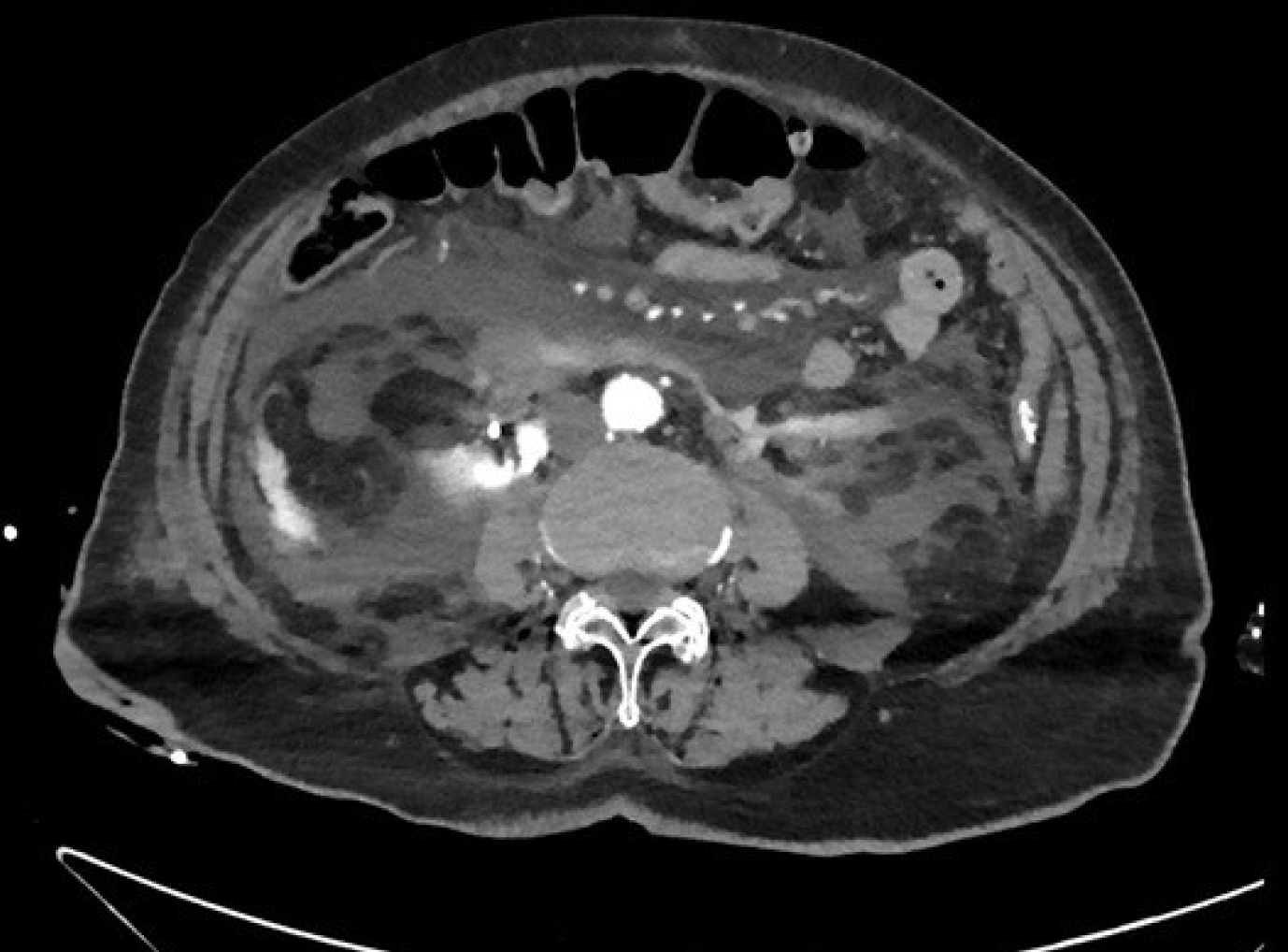
In the immediate postoperative period, due to the presence in the immediate postoperative period of abdominal distension without hemodynamic instability, a CT urogram (Figure 2) was performed, revealing the presence of irrigation fluid leakage in the intra and extra-peritoneal spaces, extending to all quadrants, including the periepatic region. However, there was no evidence of active radiopaque urine leakage during the urographic phase or active bleeding foci.
Laboratory examinations were regular, without signs of anemia or systemic infection.
A CT urogram (Figure 2) was performed, revealing the presence of irrigation fluid leakage in the intra- and extra-peritoneal spaces, extending to all quadrants, including the periepatic region. However, there was no evidence of active radiopaque urine leakage during the urographic phase or active bleeding foci.
The patient was transferred to our Intensive Care Unit for the next 48 h, where the hemodynamic parameters remained consistently stable. According to General Surgeons, it was decided not to proceed with surgical intervention.
A follow-up abdominal CT was performed on the 5th postoperative day, documenting complete absorption of the intra/retroperitoneal fluid collection, without evidence of late extravesical contrast extravasation (at 7 min), but with the presence of blood clots in the renal pelvis and mid-proximal ureter.
Therefore, due to the persistent evacuation of small clots from the renal pelvis during daily PCN flushes, it was decided to replace the ureteral stent with a mono-J catheter (8 cm) retrogradely on the 6th postoperative day to allow for more effective nephrolusosis.
After an additional 3 d, with the patient's clinical condition remaining stable, the mono-J catheter was replaced with a JJ stent (7 cm × 24 cm) to enable the patient's discharge. The discharge took place after another 4 d (13th postoperative day) with the PCN tube (open) and JJ stent in place. On the 21st postoperative day, the PCN tube was closed and removed the following day. Currently, the patient is in excellent general condition, and histological examination revealed low-grade urothelial carcinoma.
UTUC often remains asymptomatic for a prolonged period before presenting with micro or macrohematuria in 70%-80% of cases. Less commonly, patients may experience lumbar pain or, occasionally, detect a lumbar mass. Systemic manifestations, such as asthenia, unexplained weight loss, or night sweats, suggest advanced or metastatic disease[1,9]. According to the latest guidelines from the European Association of Urology (2023), UTUC can be classified into "low-risk" disease if specific criteria are met: unifocality, size less than 2 cm, negative high-grade cytology, low-grade histology after biopsy, and no invasive features on CT. On the other hand, "high-risk" disease is defined if at least one of the following criteria is present: hydronephrosis, size equal to or greater than 2 cm, high-grade cytology or histology after biopsy, multifocality, local invasion on CT, previous radical cystectomy for high-grade urothelial carcinoma of the bladder, or histological subtypes[8]. In general, UTUC exhibits a worse prognostic course compared to TCC-B, with inferior oncological outcomes for single ureteral lesions in comparison to those located in the intrarenal collecting system[1]. The two most significant prognostic factors are the T stage and grade, rather than tumor size and multifocality[2]. The rate of ipsilateral recurrence is 37% for low-grade tumors and 63% for high-grade tumors[4]. For many years, the "gold standard" treatment for all UTUC cases has been nephroureterectomy with bladder cuff excision. However, there is still a high recurrence rate necessitating salvage surgery, particularly for high-grade tumors[9]. Nevertheless, in some cases, several years may elapse before disease progression occurs, thereby preserving patients from potential dialysis initiation[2,7]. Renal-sparing surgery, such as distal ureterectomy with ureterocystoneostomy for distal tract neoplasms or segmental resection with ureteroureterostomy for mid or proximal ureter tumors, is a valid alternative not only for "low-risk" cases but also for patients with chronic renal insufficiency, solitary kidneys, or bilateral neoplasms[1]. Conservative "endoscopic" treatment is a viable option for selected patients, offering oncological outcomes equivalent to radical surgery[7], as documented by overlapping OS and CSS, even after a follow-up of more than 10 years[6]. Percutaneous access is also a feasible approach for larger tumors within the intrarenal collecting system, as demonstrated in our case. However, due to the relative rarity of urothelial carcinoma in the UTUC, there is limited substantial literature supporting the best treatment options beyond nephroureterectomy, and guidelines regarding the ideal follow-up schedule for UTUC are still evolving. According to the latest European guidelines, a ureterorenoscopy as a second-look should be performed within 6-8 wk after the initial procedure, especially in "low-risk" pathology. For "high-risk" patients, endoscopic follow-up is recommended at 3 and 6 months after the initial treatment. Extending the follow-up regimen to these patients could increase the detection rate of clinically significant recurrences and potentially improve Overall Survival[10].
In our case, considering the patient's age, comorbidities, tumor characteristics, and the patient's refusal to provide consent for radical surgery, we opted for percutaneous endoscopic excision of the renal pelvis neoplasm using the Tullio laser. Despite the successful eradication of the lesion, the patient experienced an early postoperative complication, which was effectively managed conservatively in collaboration with the General Surgeons. This conservative approach was based on 4 main aspects: (1) The presence of a non-infected abdominal fluid collection primarily composed of physio
In conclusion, given the occurrence of a complication like this, a conservative approach can be a valid therapeutic choice.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Urology and nephrology
Country/Territory of origin: Italy
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): 0
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Figaroa OJA, Netherlands S-Editor: Liu JH L-Editor: A P-Editor: Zheng XM
| 1. | Lucca I, Leow JJ, Shariat SF, Chang SL. Diagnosis and management of upper tract urothelial carcinoma. Hematol Oncol Clin North Am. 2015;29:271-288, ix. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 14] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 2. | Hasan MN, Rouprêt M, Keeley F, Cracco C, Jones R, Straub M, Traxer O, Osther PJS, Brehmer M. Consultation on UTUC, Stockholm 2018 aspects of risk stratification: long-term results and follow-up. World J Urol. 2019;37:2289-2296. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 12] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 3. | Yakoubi R, Colin P, Seisen T, Léon P, Nison L, Bozzini G, Shariat SF, Rouprêt M. Radical nephroureterectomy versus endoscopic procedures for the treatment of localised upper tract urothelial carcinoma: a meta-analysis and a systematic review of current evidence from comparative studies. Eur J Surg Oncol. 2014;40:1629-1634. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 88] [Cited by in RCA: 77] [Article Influence: 7.0] [Reference Citation Analysis (0)] |
| 4. | Raman JD, Park R. Endoscopic management of upper-tract urothelial carcinoma. Expert Rev Anticancer Ther. 2017;17:545-554. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 6] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 5. | Porta C, Giannatempo P, Rizzo M, Lucarelli G, Ditonno P, Battaglia M. An evaluation of UGN-101, a sustained-release hydrogel polymer-based formulation containing mitomycin-C, for the treatment of upper urothelial carcinomas. Expert Opin Pharmacother. 2020;21:2199-2204. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 6. | Hendriks N, Baard J, Beerlage HP, Schout BMA, Doherty KSG, Pelger RCM, Kamphuis GM. Survival and Long-term Effects of Kidney-sparing Surgery Versus Radical Nephroureterectomy on Kidney Function in Patients with Upper Urinary Tract Urothelial Carcinoma. Eur Urol Open Sci. 2022;40:104-111. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 21] [Reference Citation Analysis (0)] |
| 7. | Motamedinia P, Hoenig D, Okeke Z, Smith A. A Case for Nephron Sparing Surgery in the Management of Upper Tract Urothelial Carcinoma. J Endourol. 2016;30 Suppl 1:S18-S22. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 3] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 8. | Upper Urinary Tract Urothelial Cell Carcinoma. EAU Oncology guidelines, 2023. |
| 9. | Farrow JM, Kern SQ, Gryzinski GM, Sundaram CP. Nephron-sparing management of upper tract urothelial carcinoma. Investig Clin Urol. 2021;62:389-398. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 10. | Figaroa OJA, Hendriks N, Kamphuis GM, Beerlage HP, van Moorselaar RJA, Bins AD, Baard J. Longer is Better for Endoscopic Follow-up of Upper Tract Urothelial Carcinoma After Ureteroscopic Treatment: An Evaluation Spanning 10 Years of Data. Eur Urol Oncol. 2023;. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Reference Citation Analysis (0)] |