Copyright
©2014 Baishideng Publishing Group Inc.
World J Clin Urol. Nov 24, 2014; 3(3): 310-319
Published online Nov 24, 2014. doi: 10.5410/wjcu.v3.i3.310
Published online Nov 24, 2014. doi: 10.5410/wjcu.v3.i3.310
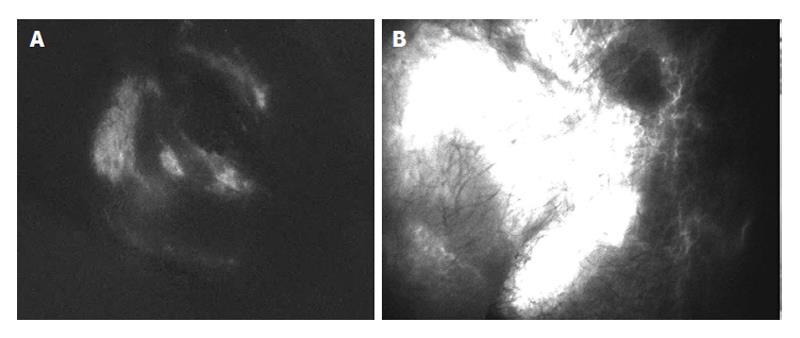
Figure 1 Photodynamic eye lymphography.
A: Photodynamic eye (PDE) lymphography of normal testis. The injected indocyanine is canalized into the local lymphatic network and is rapidly drained out of the subcutaneous scrotal tissue; B: PDE lymphography of lymphedematous testis. Indocyanine diffusively accumulates in the scrotal subcutaneous tissue as a consequence of the impaired lymphatic drainage.
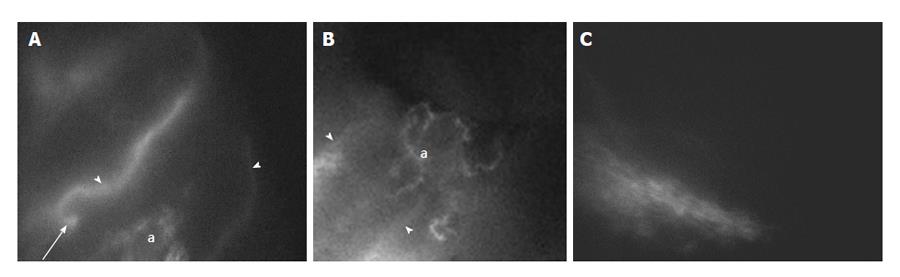
Figure 2 Photodynamic eye lymphography of lymphatic meshes.
A and B: Photodynamic eye (PDE) lymphographies of the complex mesh of small lymphatic vessels (a) developed between lymphatic collectors (arrowheads) at 3 mo from surgery in responder patients. Arrow: lympho-venous anastomosis; C: PDE lymphography showing, in a non responder patient, the complete absence of lymphatic network at 3 mo from surgery.
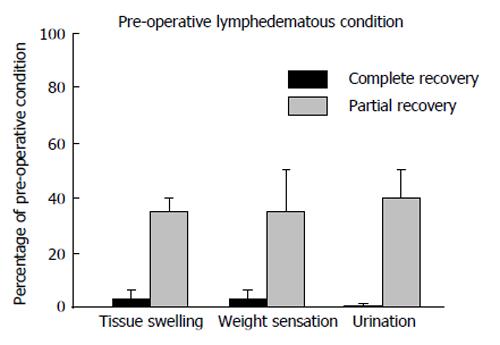
Figure 3 Post surgical self-evaluation of tissue swelling, weight sensation and urination expressed as percentage of the pre-operative lymphedematous condition in patients showing a complete or only partial recovery at three months after surgery.
Based on patients evaluation, even partial recovery represented a significant improvement with respect to pre-operative condition. In responding patients the objective clinical outcome was accompanied by a subjective evaluation of almost complete recovery of the normal tissue swelling, weight sensation and urination. Zero percentage on the Y axis corresponds to the normal condition. Histograms presents mean values ± SD of the mean.
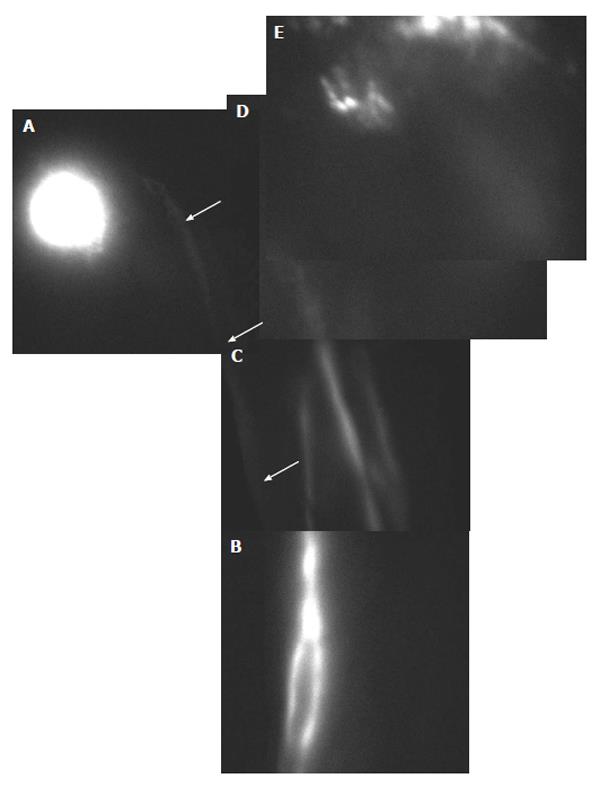
Figure 4 Photodynamic eye lymphography performed at three months after lympho-venous shunt of the the spermatic cord in a patient affected by lymphedema of the lower limb and of the external genitals secondary to radical prostatectomy and lymphadenectomy of the pelvic-inguinal lymph-nodes chain.
After injection (bright spot, A) in the scrotum, fluorescent indocyanine travels along a lymphatic vessel (arrows) in the thigh to connect with the lymphatic network of the lower limb (B). After injection in the foot, indocyanine flows along the lower limb lymphatics vessels (B and C) to be shunted directly into the external genitals lymphatic plexus (D and E) bypassing the excised pelvic-inguinal lymph-nodes chain.
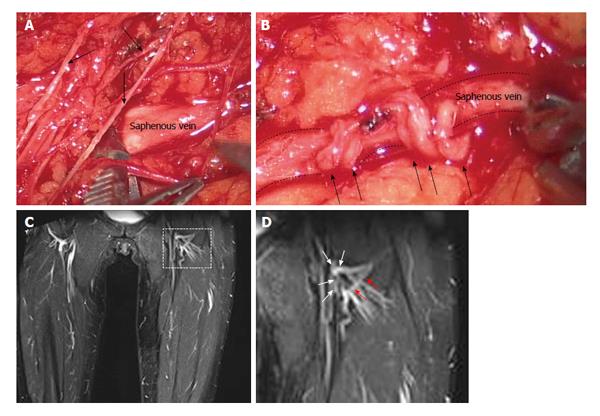
Figure 5 Lymphatic meshes were observed not only in patients who underwent spermatic funicular microsurgery, but also in patients who positively responded to the treatment of the lower limb swelling.
A: Microsurgical identification of the saphenous vein and of lymphatic vessels (arrows) in the crural area; B: Latero-terminal lympho-venous anastomosis, confectioned with interrupted stitches, between lymphatic vessels (arrows) and the saphenous vein (dashed line) in proximity of the femoral-saphenous cross; C: Magnetic resonance image of the lower limb obtained in the same patient of A, B at 8 years after microsurgery. Details of the left limb crural area (delimited by the dashed line) are presented in D; D: White arrows identify the sites were latero-terminal lympho-venous anastomosis were confectioned, while red arrows focus on a new developed lymphatic collector.
- Citation: Mukenge SM, Negrini D, Catena M, Ferla G. Innovative microsurgical treatment of male external genitals lymphedema. World J Clin Urol 2014; 3(3): 310-319
- URL: https://www.wjgnet.com/2219-2816/full/v3/i3/310.htm
- DOI: https://dx.doi.org/10.5410/wjcu.v3.i3.310