Published online May 8, 2016. doi: 10.5409/wjcp.v5.i2.212
Peer-review started: July 31, 2015
First decision: December 4, 2015
Revised: December 17, 2015
Accepted: January 16, 2016
Article in press: January 19, 2016
Published online: May 8, 2016
Processing time: 278 Days and 13.1 Hours
AIM: To determine if dopamine is effective in treating neonatal hypotension and safe to use comparing to other inotropes.
METHODS: This is a review of evidence on inotropic treatment of neonatal hypotension. Databases searched were MEDLINE and the Cochrane Library, a total of 134 studies were identified. Only studies with high quality evidence (level 1a and b and 2a) were included. After review, only eight studies were included in the final analysis. Pooled risk ratios derived for each outcome [Mantel-Haenzel (M-H) fixed effect] with CI, as reported in the Cochrane reviews were plotted in forest plot form.
RESULTS: Eight articles met inclusion criteria, which all included treatment in preterm infants. Dopamine increased mean arterial blood pressure (BP) (n = 163; r = 0.88, 95%CI: 0.76 to 0.94) and systolic BP (n = 142; r = 0.81, 95%CI: 0.42 to 0.94) comparing to placebo. Dopamine has been shown overall to be statistically more effective in increasing BP than dobutamine (n = 251, r = 0.26, 95%CI: 0.20-0.32). However there were no differences in short term outcomes (periventricular leucomalacia, periventricular haemorrhage) and mortality between both drugs. There is no statistical evidence of dopamine being more effective than adrenaline or corticosteroids. There was no difference in morbidity and mortality outcomes when dopamine was compared to hydrocortisone (RR 1.81, 95%CI: 0.18 to 18.39) or adrenaline.
CONCLUSION: In preterms, dopamine is the most studied drug, and we suggest it could be used as first line treatment in hypotension.
Core tip: Hypotension is a common feature in the preterm infant. The aim of this systematic review was to determine, after review of evidence, if dopamine would make a good first line drug therapy for hypotension in the neonatal population. Dopamine was shown across trials to increase blood pressure more effectively than dobutamine. There was no difference in morbidity and mortality outcomes when dopamine was compared to hydrocortisone or adrenaline. In preterm infants, dopamine is the most studied drug, and in general safer than others to use, we therefore cautiously suggest it could be used as first line treatment in hypotension.
- Citation: Bhayat SI, Gowda HMS, Eisenhut M. Should dopamine be the first line inotrope in the treatment of neonatal hypotension? Review of the evidence. World J Clin Pediatr 2016; 5(2): 212-222
- URL: https://www.wjgnet.com/2219-2808/full/v5/i2/212.htm
- DOI: https://dx.doi.org/10.5409/wjcp.v5.i2.212
Hypotension is a problem frequently encountered on the neonatal intensive care unit. It is more common in preterm infants. The prevalence is said to be up to 45% in infants with a birth weight < 1500 g[1]. Indeed, in preterm infants, organ development is still in process, and imposes challenges with fluid homeostasis[2]. Low blood pressure (BP) is also frequent in the sick term infant.
The main purpose of treating hypotension is to prevent end organ damage. Statistically, low BP is associated with short and long term adverse effects. In the extreme preterm, hypotension is associated with increased mortality, cerebral lesions[3], intraventricular haemorrhage[4], periventricular leucomalacia and neurodevelopmental morbidity[5].
BP equals flow multiplied by resistance, hence depends on the cardiac output and the vascular resistance[6,7]. In very low birth weight infants (VLBW), the aetiology of hypotension is unclear: Variable left ventricular output (LVO), a large patent ductus arteriosus (PDA), and myocardial dysfunction may contribute to low BP in this population. Volume depletion is not a common cause in preterm hypotension[8].
The normal physiological BP of a newborn infant remains unknown[9]. It is believed to vary with postnatal age and gestation[10]. Thus, the definition of hypotension is variable, but it seems like the most common one used by clinicians is the following: The mean arterial BP should be maintained at, or greater than the gestational age in weeks; this definition is based on statistics rather than physiology[9], and has been recommended by the British Association of Perinatal Medicine. This definition has also been used in numerous randomised control trials[11]. A borderline low BP below the number arrived at by using the gestational age does not necessarily require treatment, and it is up to the clinician’s discretion to also evaluate end organ perfusion and decide on treatment. Furthermore, low mean arterial BP in sick preterm infants could compromise cerebral autoregulation. Cerebral autoregulation is essential because it ensures appropriate cerebral blood flow, which is one of the major determinants of oxygen delivery to the brain. The minimal BP required to maintain cerebral perfusion is unknown[8].
The choice of first line inotropic support has been dependent on clinicians. A homogeneous evidence-based treatment will benefit clinicians. This would allow health professionals to assess the problem further and consider next steps, whilst effectively treating hypotension in a safe way. By definition, a first line therapy should be effective, safe, and available. Dopamine is a precursor of noradrenaline, it is a hormone and neurotransmitter of the catecholamine and phenethylamine families. To increase BP, dopamine has a vasoconstrictive effect and may cause decreased blood supply and oxygen to certain organs. Dopamine effect is dose dependent[6] and acts on dopamine, alpha, and beta receptors; it also has a serotoninergic action[12].
The aim of this review is to determine, after appraisal of available evidence, if dopamine is effective in treating hypotension and safe to use compared to other inotropes, and therefore if dopamine would make a suitable first line drug therapy for hypotension in the neonatal population. Objective of this systematic review was to summarise all available high-level evidence comparing dopamine with other inotropes regarding effectiveness on hypotension, mortality, neurological outcome and adverse effects in the neonatal population.
For the purpose of this article, the definition of hypotension stated by the authors of reported studies included in this review has been used.
Medline via Healthcare Database Advanced Search and the Cochrane Library were searched. Reference lists of articles identified were checked resulting in further articles retrieved. Articles from the personal libraries of the investigators were also included. Only published studies were included.
The search was done in February 2015. The following MeSH terms were used: “Hypotension” (major), “Dopamine” (explode), “Dobutamine” (explode), “Hydrocortisone” (explode), “epinephrine” (explode), “norepinephrine” (explode). Results were limited to “Human” and “Age Group Newborn Infant birth to 1 mo”.
The following results were obtained with Medline search:
Hypotension (Major) AND Dopamine (explode) - 56 results
Hypotension (Major) AND Dobutamine (explode) - 23 results
Hypotension (Major) AND Epinephrine (explode) - 16 results
Hypotension (Major) AND Norepinephrine (explode) - 3 results
Hypotension (Major) AND Hydrocortisone (explode) - 36 results
The search gave us a total of 134 articles. After the duplicates were removed, there were a total of 86 articles.
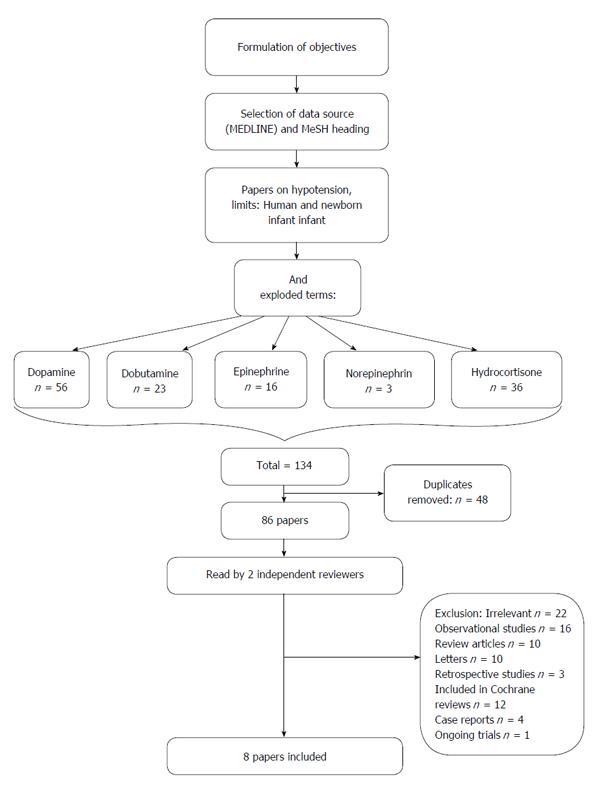
All titles and abstracts were read by 2 independent reviewers. Inclusion criteria applied were: Levels of evidence 1a, 1b and 2a (Table 1). All abstracts were read and screened, and only the ones with a high level of evidence were kept. After this screening process, 22 studies were noted to be irrelevant to our question, and 56 did not qualify as level 1 or 2 evidence (16 observational studies, 10 review articles, 10 letters, 3 retrospective studies, 12 already included in Cochrane reviews, 4 case reports, 1 on-going randomised control trial) (For PRISMA flow chart of study selection, Figure 1).
| Level of evidence | Type of study |
| 1a | Systematic review (with homogeneity) of RCTs |
| 1b | Individual RCT (with narrow confidence interval) |
| 1c | All or none (when patients died before the treatment became available, and now some survive) |
| 2a | Systematic review (with homogeneity) of cohort studies |
| 2b | Individual cohort study (including low quality RCT) |
| 2c | “Outcomes” research, ecological studies |
| 3a | SR (with homogeneity) of case-control studies |
| 3b | Individual case-control study |
| 4 | Case-series (and poor quality cohort and case-control studies) |
| 5 | Expert opinion without explicit critical appraisal, or based on physiology, bench research or “first principles” |
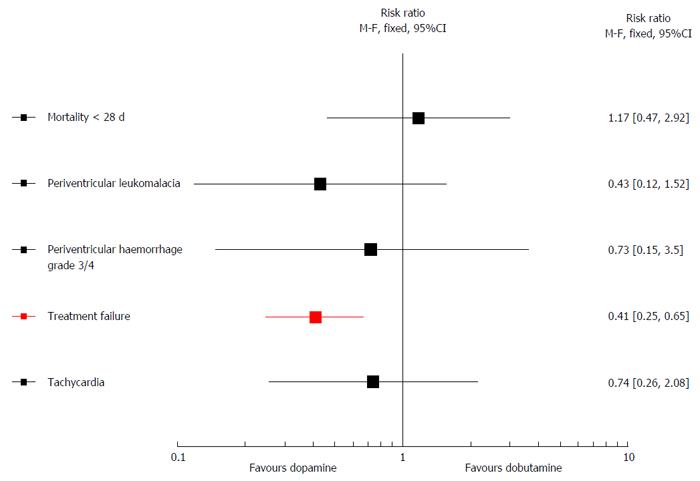
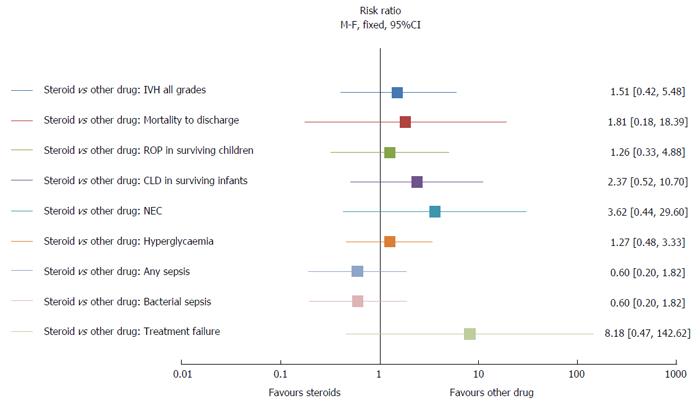
Figures 2 and 3 were made using Excel version 14.0 (Microsoft Office 2011 for Mac). Pooled risk ratios derived for each outcome [Mantel-Haenzel (M-H) fixed effect] with CI, as reported in the Cochrane reviews were plotted in forest plot form. Straight mark scatter charts were used to make these figures. The aim was to give a good visual representation of key outcomes of the Cochrane reviews regarding hypotension.
A recent meta-analysis by Sassano-Higgins et al[13] showed that dopamine increases BP significantly in the hypotensive preterm infant and that it has a greater efficacy than other forms of therapy. In this review, after looking at 26 studies, whether random or fixed effect meta-analysis, it was found that there was a significant association between administrating dopamine and treatment success. Dopamine increased mean arterial BP (12 studies; n = 163; r = 0.88, 95%CI: 0.76 to 0.94) and systolic BP (8 studies; n = 142; r = 0.81, 95%CI: 0.42 to 0.94). All the 12 studies were prospective case series without any controls examining the treatment success of dopamine.
Dobutamine is a synthetic catecholamine which acts essentially on beta receptors, creating an adrenergic effect[14]. Dobutamine is the second most commonly used inotrope to treat hypotension in the preterm infant[15]; it is thought to have the same benefits as dopamine but without the peripheral vasoconstrictive effect[16].
Three articles containing trial data on a comparison of dopamine and dobutamine were identified.
The Cochrane review by Subhedar et al[16] compared dopamine and dobutamine. The main aims of this review were: Comparing the effectiveness of the treatment in reducing mortality and long-term outcomes (neurodevelopmental outcome at 2 years), in reducing the incidence of adverse neuroradiological sequelae (severe periventricular haemorrhage and/or periventricular leucomalacia), increasing systemic arterial BP and/or cardiac output, and to compare the frequency of adverse effects between both drugs. A total of 5 randomised control trials were included, with a total of 209 infants. Comparing dopamine vs dobutamine, there was neither a difference in mortality (RR 1.17, 95%CI: 0.47 to 2.92; RD 0.02, 95%CI: -0.12 to 0.16), nor in the incidence of periventricular leucomalacia (RR 0.43, 95%CI: 0.12 to 1.52; RD -0.08, 95%CI: -0.19 to 0.04), or in the incidence of grade 3 or 4 periventricular haemorrhages (RR 0.73, 95%CI: 0.15 to 3.50; RD - 0.02, 95%CI: -0.13 to 0.09), or in the incidence of tachycardia (RD -0.06, 95%CI: -0.25 to 0.14) (Figure 2). No studies looked at the long-term neurodevelopmental outcome. In treating hypotension, dopamine was more successful than dobutamine as evident from a significantly reduced risk of treatment failure (RR 0.41, 95%CI: 0.25 to 0.65). LVO was analysed in one paper[17] in the Cochrane review. Initially the raw numbers showed a drop in LVO with dopamine, compared to a rise in LVO with dobutamine. However the Cochrane review excluded this outcome from the analysis as the calculation of absolute changes was not possible. The authors concluded that dopamine was more effective than dobutamine in the short-term treatment of hypotension. As there were no statistical differences in long term outcomes and safety, no firm recommendations could be made.
The meta-analysis by Sassano-Higgins et al[13] mentioned in the above paragraph on dopamine and its effects on BP, contained a subgroup analysis where dopamine was compared with dobutamine. Dopamine administration was associated with a significantly greater overall efficacy for increase in BP than dobutamine (7 studies; n = 251; r = 0.26; 95%CI: 0.20 to 0.32). There were no statistically significant differences in adverse neurological outcomes between dopamine and dobutamine. This meta-analysis contained two additional studies in addition to the five studies included in the Cochrane review by Subhedar et al[16] (2003). The latter excluded the study by Miall-Allen et al[18] (1989) because it was a non-randomised study reporting the effect of addition of dobutamine in hypotensive preterm infants who did not respond to dopamine. Furthermore, it was a prospective case control study. Filippi et al[19]’s primary objective was endocrine effects of dopamine and dobutamine. This study did not meet the inclusion criteria for a Cochrane review. Short-term improvement in BP was analysed in the Cochrane review, looking at 4 articles with successful treatment of hypotension. Each article looked at individually, concluded in an increase of BP. A pooled estimate was not done regarding short-term effect on BP with both drugs in view of the variation in measuring and reporting BP in the included studies. However, in the meta-analysis[13], pooled analysis of the 7 studies (n = 251, r = 0.26, 95%CI: 0.20-0.32) showed that dopamine had a greater efficacy in increasing the BP compared to dobutamine.
However, dopamine is also thought to have endocrine adverse effects. Indeed exogenous dopamine infusion suppresses PRL, thyroid stimulating hormone (TSH) and T4 secretion by acting on specific dopamine D2 receptors[20]. It is believed that in preterm infants, unlike in adults, dopamine crosses the blood brain barrier and exerts its effects directly at the hypothalamic level as well as on the dopamine receptor trophic cells[21]. Filippi et al[19]’s study, which was not included in the Cochrane review, compared the endocrine effects between dopamine and dobutamine in VLBW, in a randomised prospective trial published in 2007. Thirty-five hypotensive infants were randomised into 2 groups, whether they received dopamine or dobutamine for hypotension after 2 boluses of crystalloid. In the group of infants treated with dopamine, levels of TSH, total thyroxine (T4), prolactine (PRL), and growth hormone (GH) were significantly reduced after 12 h, comparing to the dobutamine group (P < 0.01). However after stopping dopamine, from the first day onwards, levels of TSH, T4 and PRL increased briskly. There was also a mild but non-significant increase in GH. Dobutamine did not affect hormone levels. The authors conclude that dopamine induces suppression of pituitary function, but it is a transient effect.
Adrenaline [= Epinephrine (EP)] is a potent inotrope, and chronotrope, which acts on alpha and beta-receptors. It acts as a systemic and pulmonary vasodilator in low doses, and when doses are increased, it increases systemic pressure more than pulmonary pressure[22].
Three articles were identified comparing adrenaline and dopamine: Two randomised controlled trials and one Cochrane review.
In 2005, the randomised control trial by Valverde et al[23] compared 2 groups of preterm infants < 32 wk < 1501 g with low BP receiving either dopamine (DP) or adrenaline at increasing doses. Fifty-nine infants were included. The study was ongoing at the time of the Cochrane review; therefore it hasn’t been completely included. Treatment success by obtaining an optimal BP was present in 96.3% of patients with dopamine and 93.7% with adrenaline; there was no statistical significance between these 2 groups. Amongst the primary outcomes, the only one that varied between the 2 groups was the heart rate. Indeed, the heart rate was increased in both dopamine and adrenaline groups [at time of obtaining optimal BP: 157 beats per minute (bpm) vs 169 bpm respectively], but was significantly higher in the adrenaline group (P = 0.03). There was no other statistically significant difference in the primary outcomes (systemic and cerebral haemodynamic variables) or secondary outcomes (acid-base status, blood lactate concentration, glycaemia, haematocrit) between both treatment groups. Cerebral blood volume (CBV), measured by near infrared spectroscopy (NIRS), was analysed in both groups, and it was noted that drug-induced changes varied with gestational age. In very preterm infants < 28 wk, the EP- induced increase in CBV was greater than with dopamine. However, DP-induced increase in CBV was greater in less preterm infants (> 28 wk).
A randomised control trial in 2006 by Valverde et al[23] compared 2 groups of preterm infants < 1501 g and < 32 wk gestation, receiving either dopamine or adrenaline, and short and medium term outcomes were measured. This trial was not included in the Cochrane review from Paradisis et al[24]. The study was mentioned in the Cochrane review, but had only been published as an abstract for a meeting as the above study by Pellicer et al[25]. Looking into details of the study by Pellicer et al[25] and Valverde et al[23], the list of authors are identical but the order of the authors differs; the included cohort of infants is the same (period of inclusion, inclusion and exclusion criteria), however the primary outcomes are different as Pellicer looks more at cerebral haemodynamics, whereas Valverde analysed systemic effects and clinical outcomes. In Valverde’s article, both groups were comparable, although randomisation technique was not explained. There was no difference in treatment failure in both groups (dopamine: 36%; epinephrine: 37%). Withdrawal occurred later in the dopamine group. Infants in the adrenaline group had higher lactates, higher blood sugars and lower base excesses (P < 0.05). There was no difference in medium term comorbidities (enteral nutrition tolerance, gastrointestinal complications, severity of lung disease, PDA, cerebral ultrasound diagnoses, retinopathy of prematurity) and mortality. Authors conclusion was that compared to dopamine, adrenaline had the same effect on BP, but also had transitory effects on lactate metabolism. As there is no further evidence to explain or confirm these side effects it is difficult to recommend adrenaline over dopamine as a first line therapy in treatment of hypotension for the preterm infant.
A Cochrane review in 2004[24], updated in 2009 but with no changes made to the conclusion, looked at the effectiveness and safety of adrenaline in comparison with no treatment and other inotropes (dopamine, dobutamine, noradrenaline, or isoprenaline). Only one study published in an abstract form comparing dopamine and adrenaline was included. It was a very selective group with infants only above 1750 grams. There was a significant increase in the BP in the adrenaline and the dopamine group, however the significance of the difference was not reported. Outcomes like mortality, neurodevelopment, and peri or intra ventricular haemorrhage were not reported. This Cochrane review concluded that there was not enough evidence to show an effect of adrenaline in preterm infants with cardiovascular compromise.
Glucocorticoids increase vascular tone and myocardial contractility by increasing responsiveness to circulating catecholamines. In preterm infants, immaturity may also lead to limited adrenal reserves, being one the causes of low BP[26], therefore the use of steroids as treatment for hypotension is logical. In daily clinical practice, steroids are usually used for refractory hypotension. One Cochrane review analysed the effect of steroids in neonatal hypotension.
The population targeted is the preterm infant. Hydrocortisone is the most common steroid used in the treatment of neonatal hypotension.
The Cochrane review by Ibrahim et al[27] included, in addition to the comparison of corticosteroids vs placebo, also a comparison of steroids with dopamine. The primary objective was to investigate the effect of corticosteroids as a primary treatment of hypotension, and the secondary outcome was to look at benefits or adverse effects of steroid therapy (mortality, IVH grade 3 or 4, periventricular leukomalacia, chronic lung disease in surviving infants, necrotizing enterocolitis, bacterial sepsis). The population studied was all preterm infants < 37 wk and less than 28 d old with hypotension. A total of 4 studies were included. In this article, as the main focus is dopamine, therefore only the comparison of steroids and dopamine has been reviewed, which is based on one randomised controlled trial by Bourchier et al[28]. There was no statistically significant difference in effect of hydrocortisone on mortality comparing to dopamine (RR 1.81, 95%CI: 0.18 to 18.39; RD 0.04, 95%CI: -0.12 to 0.20), or on morbidities like infection comparing to dopamine (RR 0.60, 95%CI: 0.20 to 1.82; RD -0.13, 95%CI: -0.39 to 0.14), and hyperglycaemia comparing to dopamine (RR 1.27, 95%CI: 0.48 to 3.33; RD 0.07, 95%CI: -0.21 to 0.35) (Figure 3). Long-term neurodevelopmental outcome was not reported. Authors concluded that there was insufficient evidence to support routine use of corticosteroids as first line treatment of hypotension in preterm infants.
There was one high-level evidence paper comparing different inotropes: A systematic review by Dempsey et al[29] in 2007. One of the aims of the article was to compare the effectiveness of different inotropes. Pubmed search was performed looking for studies comparing 2 interventions, and seeking important clinical outcomes (survival, brain or lung injury, long-term neurodevelopmental outcome). Only randomised control trials in hypotensive preterm infants were included. This systematic review compared dopamine with other inotropes. In the comparison with dobutamine, only articles already included in Subhedar’s Cochrane review were found, and concluded the same as above: Dopamine is more likely to increase BP than dobutamine. Four further studies were identified comparing dopamine to other inotropes regarding blood flow, which was irrelevant to our question, but showed that dopamine decreased LVO. Some studies were identified reporting a comparison of dopamine and adrenaline, but there was little evidence to support the use of this drug according to this review (2 studies). The authors concluded that there are many small studies addressing short-term effects of various catecholamines on physiological variables, but that there is no evidence regarding clinically important outcomes.
Even though various inotropes are used, Dopamine still seems to be the one which is most commonly prescribed in hypotension in all infants, including VLBW infants[15]. We looked at the evidence supporting the usage of dopamine and summarized this in Table 2. In this review, we wanted to determine whether dopamine could be used as a first line therapy. By definition, a first line therapy should be effective, safe to use with minimal side effects and easily available. Having a standardised approach to hypotension would make practice more homogeneous; this has its advantages and inconveniences. A universal initial approach allows one to start treatment and then consider other options according to the underlying pathology. In treatment of hypotension, there is no evidence to support the use of volume expansion, whether saline, or albumin[30,31]. Dopamine has been shown overall to be statistically more effective in increasing BP and with less treatment failure than dobutamine[16], There is no statistical evidence of dopamine being more effective than adrenaline or corticosteroids. There were no papers of high evidence looking at treatment of hypotension with noradrenaline. Nevertheless, adrenaline has been shown to have more side effects than dopamine by increasing lactate, blood sugars, and lowering base excess[23]. There is not enough evidence regarding mid and long term outcomes to support the usage of hydrocortisone as a first line drug[27]. The meta-analysis by Higgins et al[32] showed that hydrocortisone successfully increases BP. This article was not included in our review, as it did not compare steroids to other inotropes. Antenatal steroids are believed to have a positive effect on low BP in the preterm infant[33].
| Ref. | Title of study | Study group | Study type (evidence) | Outcome | Key result | Comment |
| All inotropes | ||||||
| Dempsey et al[29] | Treating hypotension in the preterm infant: When and with what: a critical and systematic review | Preterm infant | Critical systematic review | Which preterm may benefit from treatment and with what intervention | 17 studies reviewed. No threshold BP that was predictive of a poor outcome. None of the interventions (volume expansion, catecholamines or steroids) for hypotensive infants improved the outcome | Not able to comment which inotropes were beneficial |
| Dopamine | ||||||
| Sassano-Higgins et al[13] | A meta-analysis of dopamine use in hypotensive preterm infants: Blood pressure and cerebral hemodynamics | Preterm infants | Meta analysis | Dopamine effect on Hypotension CNS injury | Dopamine increases mean arterial blood pressure (12 studies; n = 163; r = 0.88, 95%CI: 0.76 to 0.94) and systolic blood pressure (8 studies; n = 142; r = 0.81, 95%CI: 0.42 to 0.94). Dopamine administration was associated with a significantly greater overall efficacy for increase in BP than dobutamine (7 studies; n = 251; r = 0.26; 95%CI: 0.20 to 0.32), colloid (2 studies; n = 67; r = 0.60; 95%CI: 0.41 to 0.74) and hydrocortisone (1 study; n = 28; r = 0.40; 95%CI: 0.034 to 0.67); There were no statistically significant differences in adverse neurological outcomes between dopamine and dobutamine | Dopamine is more effective than dobutamine, colloid or hydrocortisone alone. No increased incidence of adverse effects compared to other therapies |
| Dopamine and dobutamine | ||||||
| Subhedar et al[16] | Dopamine vs dobutamine for hypotensive preterm infants | Preterm infant | Cochrane review | Effectiveness and safety of dopamine and dobutamine in the treatment of systemic hypotension | 5 trials = 209 infants. Fewer infants having treatment failure of hypotension with dopamine than dobutamine (RD -0.23, 95%CI: -0.34 to -0.13; NNT = 4.4, 95%CI: 2.9 to 7.7). No evidence of a significant difference in neonatal mortality between dopamine and dobutamine (RD 0.02, 95%CI: -0.12 to 0.16), incidence of periventricular leukomalacia (RD -0.08, 95%CI: -0.19 to 0.04), or severe periventricular haemorrhage (RD -0.02, 95%CI: -0.13 to 0.09), or incidence of tachycardia (RD -0.06, 95%CI: -0.25 to 0.14) | Dopamine is more effective than dobutamine in the short term treatment, none of the studies reported the incidence of adverse long term neurodevelopmental outcomes |
| Filippi et al[19] | Dopamine vs dobutamine in very low birthweight infants: Endocrine effects | VLBW | Prospective RCT (non-blinded) | Endocrine effects of dopamine and dobutamine in hypotensive VLBW | Suppression of TSH, T(4) and PRL was observed in dopamine-treated newborns from 12 h of treatment onwards, whereas levels of growth hormone reduced significantly only at 12 h and 36 h of treatment (P < 0.01). TSH, T(4) and PRL rebound was observed from the first day onwards after stopping dopamine. Dobutamine administration did not alter the profile of any of the hormones and no rebound was observed after stopping treatment | Dopamine induced a transient pituitary suppression, comparing to dobutamine. But this is totally reversible |
| Dopamine and adrenaline | ||||||
| Pellicer et al[25] | Cardiovascular support for low birth weight infants and cerebral hemodynamics: A randomized, blinded, clinical trial | LBW | RCT double blinded | Quantitative changes in cerebral concentrations of oxyhemoglobin and deoxyhemoglobin, cerebral intravascular oxygenation (HbD), and cerebral blood volume | Among hypotensive LBW infants, cardiovascular support with low/moderate-DP or low-dose EP increased cerebral perfusion. Low-dose EP was as effective as low/moderate-dose DP in increasing MBP among LBW infants. Heart rate was higher in the EP group than in the DP group (respectively 167 vs 159 when optimal BP was obtained) | Low-dose EP was as effective as low/moderate-dose DP in increasing MBP among LBW infants. EP led to a higher heart rate than DP |
| Valverde et al[23] | Dopamine vs epinephrine for cardiovascular support in low birth weight infants: Analysis of systemic effects and neonatal clinical outcomes | LBW | RCT | Short-term changes in heart rate, mean BP, acid-base status, lactate, glycemia, urine output, and fluid-carbohydrate Debit. Medium-term morbidity, enteral nutrition tolerance, gastrointestinal complications, severity of lung disease, patent ductus arteriosus, cerebral ultrasound diagnoses, retinopathy of prematurity, and mortality | Mean blood pressure showed a significant increase from baseline throughout the first 96 h with no differences between groups (dopamine: 36%; epinephrine: 37%). However, epinephrine produced a greater increase in heart rate than dopamine. After treatment began, epinephrine patients showed higher plasma lactate (first 36 h) and lower bicarbonate and base excess (first 6 h) and received more bicarbonate, and had higher blood glucose levels (P < 0.05). For medium-term morbidity, there were no differences in neonatal clinical outcomes in responders | Transitory adverse effects of epinephrine on carbohydrate and lactate metabolism could undermine the use of epinephrine as a first-line inotrope in preterm infants who are prone to such metabolic disturbances |
| Paradisis et al[24] (2004, reviewed in 2009) | Adrenaline for prevention of morbidity and mortality in preterm infants with cardiovascular compromise | Preterm infant | Cochrane review | Effectiveness and safety of adrenaline compared to no treatment or other inotropes in reducing mortality and morbidity in preterm infants with cardiovascular compromise | One trial comparing adrenaline with dopamine infusion was included. It enrolled hypotensive, predominantly preterm infants in the first 24 h. Only infants > 1750 g are included in this review. Both adrenaline and dopamine significantly increased heart rate and mean BP, with no statistically significant effect on left or right ventricular outputs. No significant difference was reported between the 2 inotropes | The study was reported as being randomised and double blinded, but methods were not reported. Published abstract, side effects and safety were not reported |
| Dopamine and steroids | ||||||
| Ibrahim et al[27] | Corticosteroids for treating hypotension in preterm infants | Preterm infant | Cochrane review | Effectiveness and safety of corticosteroids used either as primary treatment of hypotension or for the treatment of refractory hypotension | 4 studies were included in this review enrolling a total of 123 babies. In one study, persistent hypotension was more common in hydrocortisone treated infants as compared to those who received dopamine as primary treatment for hypotension (RR 8.2, 95%CI: 0.47 to 142.6; RD 0.19, 95%CI: 0.01 to 0.37). There were no statistically significant effects on any other short or long-term outcome | Long term benefit or safety data is lacking with steroids |
Dopamine is more effective than dobutamine in increasing BP, but there was no statistical significance in the differences of other outcomes (mortality, periventricular flare, intraventricular haemorrhage grade 3-4, tachycardia)[16]. In the articles analysed, doses of dopamine used were not specified, but this drug was administered at a treatment dose for hypotension. This is important as low doses of dopamine (0.5-2 micrograms/kg per minute) act on dopaminergic receptors which usually increases renal perfusion. Medium doses (2-6 micrograms/kg per minute) act on beta-receptors causing vasodilatation and a positive inotropic and chronotropic effect (increasing output and heart rate). At high doses (> 6-10 micrograms/kg per minute), dopamine acts on alpha-receptors leading mainly to peripheral vasoconstriction[8]. In preterm infants there are differences in receptor maturation depending on the gestation. Hence there is a vasoconstrictive effect in preterms even if dopamine is used at medium doses[34].
On a short term scale, dopamine induces transient and reversible pituitary suppression, however despite this endocrine effect, there is no clinical implication on the infant: Comparing to dobutamine there were no changes with regards to the heart rate, oxygen requirement, fluid intake and mean urine output[19]. However, even though there was significantly decreased, but reversible levels of TSH, T4, and PRL, the long term outcome of this transient suppression remain unknown[19]. In the Cochrane review by Subhedar et al[16], the effects of dopamine and dobutamine on the left ventricular outflow could not be compared in view of unpublished raw data, yet in a non statistical approach, it seems that dobutamine had more effect on increasing left ventricular outflow.
It is also important to remember the physiological effect of these drugs: Dopamine has a vasoconstrictive effect when acting on the alpha-receptors[6]. Peripheral vasoconstriction by definition will increase systemic BP, but it will also reduce the flow and oxygenation, potentially leading to hypoperfusion in organs such as the brain, the kidneys and the skin[35]. The underlying cause and pathophysiology of decreased BP is essential to take into consideration when treating. Thus it is important to consider different agents in specific situations such as volume deficiency, cardiac failure, sepsis or adrenal insufficiency.
This review was initially aimed at all infants admitted to the neonatal unit, however all evidence points towards the use of inotropes in the preterm infants, therefore the recommendations from this article are aimed at preterm infants with initial hypotension. Therefore, individual treatment for specific conditions was not addressed in this review. Another limitation is that only papers published with high levels of scientific evidence, in the top of the evidence pyramid, have been analysed. Additionally, the literature collected did not focus on direct long-term side effects of the drugs (such as direct effects on brain perfusion and development), independently from their effects on BP.
Other than the above-mentioned inotropes, there are some new drugs such as Milrinone, which is an inotrope/vasodilator and phosphodiesterase inhibitor, and mainly used post cardiac surgery to improve cardiac output. It inhibits an enzyme, which results in an accumulation in cyclic adenosine monophosphate increasing cardiac muscle contractility, and relaxation of the smooth vascular muscle allowing treatment of pulmonary hypertension. Side effects include arrhythmias[36]. Other drugs like levosimendran and terlipressin, have inotropic effects, but there is not enough evidence in the preterm to promote their usage.
The current practice of treating hypotension concentrates on improving the number of the BP, but one may argue it is important to consider the blood flow as well. This idea emerged in 1928 from Jarisch “It is a source of regret that measurement of flow is much more difficult than measurement of pressure. This has led to an undue interest in BP measurements. Most organs however, require flow rather than pressure[37]”. There are current studies looking at the flow, and the effect in the management of low BP by inotropes: Neocirculation is looking at the effect of dobutamine on the superior vena cava flow[38], and the TOHOP study looking at NIRS for objective end organ perfusion as an adjunct to management of hypotension[39]. Controversially, other trials are looking at whether hypotension needs to be treated in the initial period of life of a preterm infant; the concept of permissive hypotension is becoming more common. Even though it is known that low BP in a preterm infant is associated with adverse outcomes, it remains unknown whether treatment of hypotension improves the outcome. The on-going HIP trial is aiming to determine whether there is a difference in short and long-term outcome in preterm infants in managing hypotension with volume and dopamine vs a permissive placebo approach[11].
In this review, we are only able to comment on preterm infants. Term infants usually have multiple aetiologies for hypotension like hypovolaemia, cardiogenic shock, septic shock, endocrine causes like congenital adrenal hyperplasia, sedation drugs[40], and there have been no studies with high levels of evidence which have compared various inotropes in a term infant.
In preterm infants, dopamine is the most studied drug, is more effective in increasing BP than dobutamine. There was no difference in morbidity and mortality outcomes when dopamine was compared to hydrocortisone or adrenaline. In preterm infants, dopamine is effective, and in general safer than others to use. All evidence points towards the fact that dopamine can be considered as a first line inotrope in preterm neonatal hypotension.
Different inotropes are used in the treatment of neonatal hypotension. Clinicians have their own preferences in using particular inotropes as a first line, depending on the unit policy and their previous personal experience.
Controversies exist on the best initial approach of what inotrope to use in the management of neonatal hypotension. There are new studies investigating the necessity of inotropic support and increasing blood pressure.
This study reviewed current evidence on different inotropes commonly used, and concluded that dopamine is a safe and effective option for the treatment of neonatal hypotension.
Hypotension in the neonatal population, specially in preterm infants, is a common problem faced daily by clinicians. Having an evidence-based approach is in the best clinical interest of the patients.
Cerebral autoregulation: Process which aims to maintain adequate and stable cerebral blood flow; Periventricular leucomalacia: White brain matter injury characterized by necrosis of white matter near the lateral ventricles; Preterm: Birth of a baby at less than 37 wk of gestation.
This is a nice systematic review providing good insight into commonly used inotropic agents in neonatal care, focusing on preterm infants.
P- Reviewer: Classen CF, Sangkhathat S, Watanabe T S- Editor: Song XX L- Editor: A E- Editor: Wang CH b
| 1. | Al-Aweel I, Pursley DM, Rubin LP, Shah B, Weisberger S, Richardson DK. Variations in prevalence of hypotension, hypertension, and vasopressor use in NICUs. J Perinatol. 2001;21:272-278. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 146] [Cited by in RCA: 137] [Article Influence: 5.7] [Reference Citation Analysis (0)] |
| 2. | O’Brien F, Walker IA. Fluid homeostasis in the neonate. Paediatr Anaesth. 2014;24:49-59. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 28] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 3. | Miall-Allen VM, de Vries LS, Whitelaw AG. Mean arterial blood pressure and neonatal cerebral lesions. Arch Dis Child. 1987;62:1068-1069. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 272] [Cited by in RCA: 250] [Article Influence: 6.6] [Reference Citation Analysis (0)] |
| 4. | Watkins AM, West CR, Cooke RW. Blood pressure and cerebral haemorrhage and ischaemia in very low birthweight infants. Early Hum Dev. 1989;19:103-110. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 248] [Cited by in RCA: 228] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 5. | Goldstein RF, Thompson RJ, Oehler JM, Brazy JE. Influence of acidosis, hypoxemia, and hypotension on neurodevelopmental outcome in very low birth weight infants. Pediatrics. 1995;95:238-243. [PubMed] |
| 6. | Gupta S, Donn SM. Neonatal hypotension: dopamine or dobutamine? Semin Fetal Neonatal Med. 2014;19:54-59. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 25] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 7. | Evans N. Which inotrope for which baby? Arch Dis Child Fetal Neonatal Ed. 2006;91:F213-F220. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 66] [Cited by in RCA: 55] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 8. | Ibrahim CP. Hypotension in preterm infants. Indian Pediatr. 2008;45:285-294. [PubMed] |
| 9. | Seri I, Evans J. Controversies in the diagnosis and management of hypotension in the newborn infant. Curr Opin Pediatr. 2001;13:116-123. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 106] [Cited by in RCA: 83] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 10. | Cunningham S, Symon AG, Elton RA, Zhu C, McIntosh N. Intra-arterial blood pressure reference ranges, death and morbidity in very low birthweight infants during the first seven days of life. Early Hum Dev. 1999;56:151-165. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 112] [Cited by in RCA: 100] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 11. | Dempsey EM, Barrington KJ, Marlow N, O’Donnell CP, Miletin J, Naulaers G, Cheung PY, Corcoran D, Pons G, Stranak Z. Management of hypotension in preterm infants (The HIP Trial): a randomised controlled trial of hypotension management in extremely low gestational age newborns. Neonatology. 2014;105:275-281. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 50] [Cited by in RCA: 48] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 12. | Seri I. Cardiovascular, renal, and endocrine actions of dopamine in neonates and children. J Pediatr. 1995;126:333-344. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 139] [Cited by in RCA: 96] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 13. | Sassano-Higgins S, Friedlich P, Seri I. A meta-analysis of dopamine use in hypotensive preterm infants: blood pressure and cerebral hemodynamics. J Perinatol. 2011;31:647-655. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 39] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 14. | Keeley SR, Bohn DJ. The use of inotropic and afterload-reducing agents in neonates. Clin Perinatol. 1988;15:467-489. [PubMed] |
| 15. | Rios DR, Moffett BS, Kaiser JR. Trends in pharmacotherapy for neonatal hypotension. J Pediatr. 2014;165:697-701.e1. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 46] [Article Influence: 4.2] [Reference Citation Analysis (1)] |
| 16. | Subhedar NV, Shaw NJ. Dopamine versus dobutamine for hypotensive preterm infants. Cochrane Database Syst Rev. 2003;CD001242. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 66] [Cited by in RCA: 63] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 17. | Rozé JC, Tohier C, Maingueneau C, Lefèvre M, Mouzard A. Response to dobutamine and dopamine in the hypotensive very preterm infant. Arch Dis Child. 1993;69:59-63. [PubMed] |
| 18. | Miall-Allen VM, Whitelaw AG. Response to dopamine and dobutamine in the preterm infant less than 30 weeks gestation. Crit Care Med. 1989;17:1166-1169. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 26] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 19. | Filippi L, Pezzati M, Poggi C, Rossi S, Cecchi A, Santoro C. Dopamine versus dobutamine in very low birthweight infants: endocrine effects. Arch Dis Child Fetal Neonatal Ed. 2007;92:F367-F371. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 45] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 20. | Wood DF, Johnston JM, Johnston DG. Dopamine, the dopamine D2 receptor and pituitary tumours. Clin Endocrinol (Oxf). 1991;35:455-466. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53] [Cited by in RCA: 60] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 21. | Seri I, Tulassay T, Kiszel J, Ruppert F, Sulyok E, Ertl T, Bódis J, Csömör S. Effect of low-dose dopamine infusion on prolactin and thyrotropin secretion in preterm infants with hyaline membrane disease. Biol Neonate. 1985;47:317-322. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 22] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 22. | Barrington K, Chan W. The circulatory effects of epinephrine infusion in the anesthesized piglet. Pediatr Res. 1993;33:190-194. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 20] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 23. | Valverde E, Pellicer A, Madero R, Elorza D, Quero J, Cabañas F. Dopamine versus epinephrine for cardiovascular support in low birth weight infants: analysis of systemic effects and neonatal clinical outcomes. Pediatrics. 2006;117:e1213-e1222. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 85] [Cited by in RCA: 84] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 24. | Paradisis M, Osborn DA. Adrenaline for prevention of morbidity and mortality in preterm infants with cardiovascular compromise. Cochrane Database Syst Rev. 2004;CD003958. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 17] [Cited by in RCA: 13] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 25. | Pellicer A, Valverde E, Elorza MD, Madero R, Gayá F, Quero J, Cabañas F. Cardiovascular support for low birth weight infants and cerebral hemodynamics: a randomized, blinded, clinical trial. Pediatrics. 2005;115:1501-1512. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 125] [Cited by in RCA: 118] [Article Influence: 5.9] [Reference Citation Analysis (0)] |
| 26. | Watterberg KL. Adrenal insufficiency and cardiac dysfunction in the preterm infant. Pediatr Res. 2002;51:422-424. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 26] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 27. | Ibrahim H, Sinha IP, Subhedar NV. Corticosteroids for treating hypotension in preterm infants. Cochrane Database Syst Rev. 2011;CD003662. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 31] [Cited by in RCA: 40] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 28. | Bourchier D, Weston PJ. Randomised trial of dopamine compared with hydrocortisone for the treatment of hypotensive very low birthweight infants. Arch Dis Child Fetal Neonatal Ed. 1997;76:F174-F178. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 93] [Cited by in RCA: 83] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 29. | Dempsey EM, Barrington KJ. Treating hypotension in the preterm infant: when and with what: a critical and systematic review. J Perinatol. 2007;27:469-478. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 30. | Osborn DA, Evans N. Early volume expansion versus inotrope for prevention of morbidity and mortality in very preterm infants. Cochrane Database Syst Rev. 2001;CD002056. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 16] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 31. | Osborn DA, Evans N. Early volume expansion for prevention of morbidity and mortality in very preterm infants. Cochrane Database Syst Rev. 2004;CD002055. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 58] [Cited by in RCA: 50] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 32. | Higgins S, Friedlich P, Seri I. Hydrocortisone for hypotension and vasopressor dependence in preterm neonates: a meta-analysis. J Perinatol. 2010;30:373-378. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 34] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 33. | Moïse AA, Wearden ME, Kozinetz CA, Gest AL, Welty SE, Hansen TN. Antenatal steroids are associated with less need for blood pressure support in extremely premature infants. Pediatrics. 1995;95:845-850. [PubMed] |
| 34. | Noori S, Seri I. Neonatal blood pressure support: the use of inotropes, lusitropes, and other vasopressor agents. Clin Perinatol. 2012;39:221-238. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 74] [Cited by in RCA: 71] [Article Influence: 5.5] [Reference Citation Analysis (1)] |
| 35. | Vincent JL, De Backer D. Circulatory shock. N Engl J Med. 2014;370:583. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 27] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 36. | Chang AC, Atz AM, Wernovsky G, Burke RP, Wessel DL. Milrinone: systemic and pulmonary hemodynamic effects in neonates after cardiac surgery. Crit Care Med. 1995;23:1907-1914. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 205] [Cited by in RCA: 147] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 37. | Geerts BF, Aarts LP, Jansen JR. Methods in pharmacology: measurement of cardiac output. Br J Clin Pharmacol. 2011;71:316-330. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 31] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 38. | Geerts BF; Neocirculation. [accessed 2015 Jul 26]. Available from: http://neocirculation.eu/index.php. |
| 39. | UMC Utrecht. Treatment of Hypotension of Prematurity (TOHOP). gov [Internet]. Bethesda (MD): National Library of Medicine (US). [accessed 2015; https://clinicaltrials.gov/ct2/show/NCT01434251. |
| 40. | Fanaroff JM, Fanaroff AA. Blood pressure disorders in the neonate: hypotension and hypertension. Semin Fetal Neonatal Med. 2006;11:174-181. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 56] [Cited by in RCA: 58] [Article Influence: 3.1] [Reference Citation Analysis (1)] |