Published online Sep 9, 2025. doi: 10.5409/wjcp.v14.i3.107858
Revised: April 7, 2025
Accepted: May 8, 2025
Published online: September 9, 2025
Processing time: 79 Days and 1.3 Hours
Point-of-care ultrasound (POCUS) is the use of portable ultrasound devices by trained healthcare professionals to diagnose and monitor medical conditions directly at the patient's bedside, such as in emergency settings. We described a case where POCUS use, in Pediatric Emergency Department, allowed an early diagnosis and timely management in the surgical department, with a favorable outcome for child. Therefore we write this case because it is desirable to po
A 13-year-old girl with acute gastrointestinal symptoms, such as vomit and abdominal and lumbar pains. Upon physical examination, the patient had lo
It is desirable to spread POCUS in emergency settings where it allows a sig
Core Tip: The use of point-of-care ultrasound in the Emergency Department enable early diagnosis and timely intervention, in a 13-year-old girl with ovarian torsion, presented with acute gastrointestinal symptoms, leading to a favorable outcome. This case supports the integration of bedside ultrasound as a fifth pillar of clinical examination, especially in the Emergency Department.
- Citation: Cucuzza ME, Sciacca TV, Cucuzza C, Di Stefano VA. Combining point-of-care ultrasound with physical examination in a pediatric emergency department of ovarian torsion: A case report. World J Clin Pediatr 2025; 14(3): 107858
- URL: https://www.wjgnet.com/2219-2808/full/v14/i3/107858.htm
- DOI: https://dx.doi.org/10.5409/wjcp.v14.i3.107858
Point-of-care ultrasound (POCUS) is the use of portable ultrasound devices by trained healthcare professionals to diagnose and monitor medical conditions directly at a patient's bedside, such as in an emergency setting. POCUS can be used in various settings like hospitals, Emergency Departments, and ambulances. It provides real-time imaging, it helps healthcare professionals to make informed clinical decisions, and it guides treatment interventions quickly and effectively[1]. In critically ill patients, combining POCUS with physical examination is highly beneficial. It enables clinicians to perform quick, real-time assessments that are tailored to a patient's urgent clinical needs, integrating both visual and tactile information for more accurate diagnosis and treatment. In the Emergency Department, POCUS is a game-changer, enabling clinicians to make quicker decisions in urgent situations by providing immediate, real-time imaging at the bedside. In pediatric care, POCUS is especially valuable because it is non invasive, well tolerated by children, and avoids exposure to ionizing radiation, making it a safe and effective diagnostic tool. Pediatricians in Emergency Departments can use POCUS for various conditions, including abdominal pain, to detect appendicitis, intestinal obstruction, and intussusception, as well as respiratory issues like pneumonia or foreign body aspiration. Its use in pediatrics allows for more accurate and efficient diagnoses, especially in children who may be harder to assess due to their smaller body size, rapidly changing clinical conditions, and challenges with traditional imaging techniques[2]. In this case, the use of POCUS in the Pediatric Emergency Department enabled early diagnosis and timely management in the surgical department, resulting in a positive outcome for the child. This case underscores the importance of promoting ultrasound as the 'fifth pillar' of clinical examination, even in pediatric emergency settings, to enhance the care of pediatric patients
This case presents a 13-year-old girl, with normal height and weight, caucasian race.
She came to our Pediatric Emergency Department with acute gastrointestinal symptoms, such as vomiting and abdominal and lumbar pains.
She had a history of menarche at 10 years, with regular, painless menstrual cycles, which were ongoing at the time of presentation.
Past personal and family medical history was unremarkable. She reported no drug allergies and she was up to date with her vaccinations.
Upon physical examination, the patient had localized abdominal pain in the left lower quadrant, but her vital signs were normal.
Laboratory (routine blood tests, routine urine tests and urinary sediment examination) results were normal.
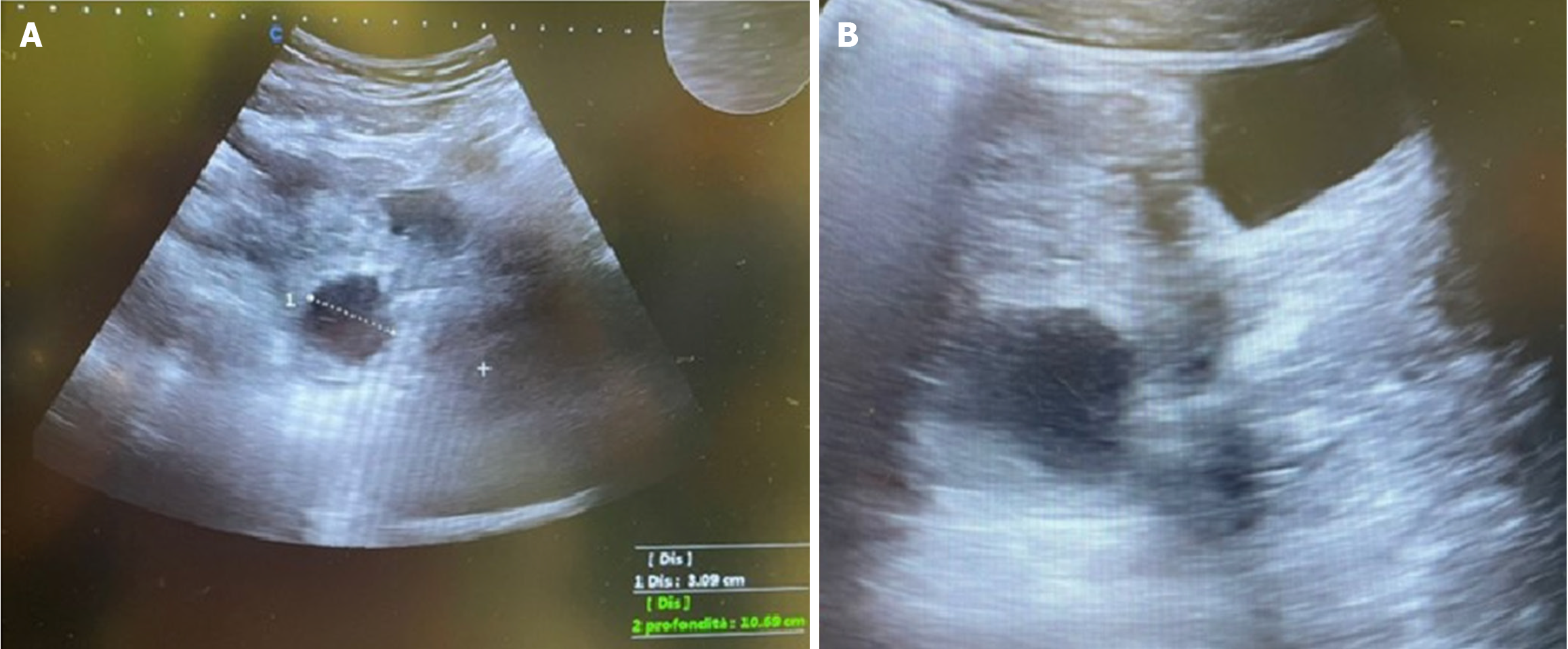
Ultrasonography performed at the bedside revealed anechoic fluid collection in the pelvic cavity, which appeared on both sides, along with an enlarged left ovary with an irregular structure containing a 3-cm cyst (Figure 1). These findings raised the suspicion of ovarian torsion, a gynecological emergency, due to the presence of an ovarian cyst and anechoic fluid.
Given the concern of ovarian torsion, the patient was transferred to the Gynecology Surgery Unit for further evaluation.
A Gynecology expert confirmed ovarian torsion diagnosis.
She underwent emergency surgery, where the affected ovary was detorsed and part of it was removed.
The postoperative recovery was smooth, and the patient had no complications. She had no complications at the 3-month clinical and ultrasound follow-up.
Ovarian torsion is a gynecological emergency, primarily affecting patients under 20 years of age, and accounts for 2%–7% of Acute Abdomens. Although it can occur at any age in the pediatric population, ovarian torsion has two peaks of incidence: Up to 52% of cases occur between ages 9–14, and up to 16% of cases occur in the first year of life[3]. In fact, these age groups have a higher incidence of cysts of various types (dermoid cysts, hemorrhagic or follicular ovarian cysts, paratubular or paraovarian cysts, cystadenomas, and polycystic ovaries), which can act as a focal point, predisposing to ovarian torsion, especially when they are larger than 3 cm[4].
The transabdominal ultrasound, associated with the study of blood flow using color Doppler, is the method of choice for diagnosis. However, to date, there are no clinical or imaging criteria sufficient to confirm the preoperative diagnosis of ovarian torsion[5]. In fact, the presence of blood flow on color Doppler does not completely exclude the possibility of ovarian torsion, and a definitive diagnosis can only be made through surgical exploration[6]. Surgical treatment options include ovarian detorsion, ovarian detorsion with oophoropexy (surgical fixation of the ovary to the lateral pelvic wall to prevent future recurrence), and surgical removal (oophorectomy)[7]. In the past, the management of a twisted ovary with an ischemic and hemorrhagic appearance was traditionally ovariectomy. However, several studies have suggested that ovarian preservation in the pediatric age group is preferable despite its appearance, due to the well-established reparative ability of the ovary itself[8]. Although the exact duration of the vascular interruption required to cause irreversible damage to the ovary is still unknown, and the ovary's double blood supply (uterine-ovarian vessels and infundibulo-pelvic vessels) makes it resistant to vascular injuries, the vitality of the ovary decreases over time, from the onset of pain to surgical detorsion. Therefore, the black or bluish macroscopic appearance of the ovary (black-bluish ovary) and presumed ovarian necrosis at the time of detorsion are not reliable indicators of the organ's vitality, and are not correlated or correlatable with the current or future ability of the ovary to develop follicles[9]. However, an early diagnosis, compared to the onset of symptoms, increases the likelihood of saving the adnexa. Timely intervention is key, as early surgical treatment can prevent more complicated procedures such as total resection of the ovary[9,10]. In this case, the attending physician's use of POCUS helped to establish an early diagnosis, which facilitated prompt intervention and a favorable outcome for the patient. In this diagnostic challenge, the strength of POCUS is its ability to provide real-time, immediate visual confirmation of suspected conditions, complementing physical examinations by offering and enabling quick decision-making.
The integration of POCUS with clinical examinations offers a more comprehensive and efficient diagnostic approach, enabling physicians to make timely decisions without the delays associated with traditional imaging methods. In this case, ovarian torsion was suspected due to the combination of abdominal pain, ultrasound findings, and the presence of a cyst. Early diagnosis and surgical intervention were crucial for preserving the patient’s ovarian function and preventing further complications. To our knowledge, there are few cases that have emphasized the utility of POCUS in pediatric emergency settings, highlighting the uniqueness of the described case. It is desirable to encourage learning periods for the POCUS technique among pediatric emergency physicians.
Our case illustrates that, in emergency settings, POCUS can save valuable time in patient management, leading to better outcomes. Therefore, it is essential to promote ultrasound as the "fifth pillar" of clinical examination at the bedside. Expanding POCUS use not only improves pediatric training but also has the potential to enhance patient outcomes, particularly in emergency settings.
We thank our colleagues from the Gynecology Unit of “Cannizzaro” hospitals for their contribution. Who endorse the data and conclusions.
| 1. | Vieira RL, Hsu D, Nagler J, Chen L, Gallagher R, Levy JA; American Academy of Pediatrics. Pediatric emergency medicine fellow training in ultrasound: consensus educational guidelines. Acad Emerg Med. 2013;20:300-306. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 70] [Cited by in RCA: 78] [Article Influence: 6.5] [Reference Citation Analysis (0)] |
| 2. | Singh Y, Tissot C, Fraga MV, Yousef N, Cortes RG, Lopez J, Sanchez-de-Toledo J, Brierley J, Colunga JM, Raffaj D, Da Cruz E, Durand P, Kenderessy P, Lang HJ, Nishisaki A, Kneyber MC, Tissieres P, Conlon TW, De Luca D. International evidence-based guidelines on Point of Care Ultrasound (POCUS) for critically ill neonates and children issued by the POCUS Working Group of the European Society of Paediatric and Neonatal Intensive Care (ESPNIC). Crit Care. 2020;24:65. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 314] [Cited by in RCA: 360] [Article Influence: 72.0] [Reference Citation Analysis (1)] |
| 3. | Baron SL, Mathai JK. Ovarian Torsion. 2023 Jul 17. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing, 2025. [PubMed] |
| 4. | Poonai N, Poonai C, Lim R, Lynch T. Pediatric ovarian torsion: case series and review of the literature. Can J Surg. 2013;56:103-108. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 41] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 5. | Kives S, Gascon S, Dubuc É, Van Eyk N. No. 341-Diagnosis and Management of Adnexal Torsion in Children, Adolescents, and Adults. J Obstet Gynaecol Can. 2017;39:82-90. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 43] [Article Influence: 7.2] [Reference Citation Analysis (0)] |
| 6. | Peña JE, Ufberg D, Cooney N, Denis AL. Usefulness of Doppler sonography in the diagnosis of ovarian torsion. Fertil Steril. 2000;73:1047-1050. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 198] [Cited by in RCA: 157] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 7. | Sriram R, Zameer MM, Vinay C, Giridhar BS. Black Ovary: Our Experience with Oophoropexy in All Cases of Pediatric Ovarian Torsion and Review of Relevant Literature. J Indian Assoc Pediatr Surg. 2022;27:558-560. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 8. | Huerta CT, Rodriguez C, Parreco J, Thorson CM, Sola JE, Perez EA. Contemporary Trends in Laparoscopy and Ovarian Sparing Surgery for Ovarian Torsion in the Pediatric Population. J Pediatr Surg. 2024;59:393-399. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 9. | Avila A, Motta M, Schechter D, Samuels S, Jaramillo I, Whitehouse J, Neville HL, Levene T. Ovarian Salvage With Prompt Surgical Intervention for Adnexal Torsion: Does Timing Matter? Am Surg. 2024;90:1508-1513. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 10. | Lorenzo GD, Mirenda G, Gentile RM, Pozzolo CD, De Santo D, Romano F, Ricci G. Use of Indocyanine Green to Evaluate Ovarian Perfusion After Laparoscopic Detorsion. A Step-By-Step Demonstration Video. J Minim Invasive Gynecol. 2024;31:269-270. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |