Published online Jun 9, 2024. doi: 10.5409/wjcp.v13.i2.91255
Revised: March 1, 2024
Accepted: April 8, 2024
Published online: June 9, 2024
Processing time: 164 Days and 16.7 Hours
Childhood obesity is a growing global concern with far-reaching health implications. This study focuses on evaluating the knowledge and practices of physi
To assess the awareness and practices of physicians in Morocco concerning the connection between maternal obesity and childhood obesity.
The research encompasses a comprehensive survey of practicing physicians, revealing significant gaps in awareness and practices related to maternal obesity.
Notably, a significant portion of doctors do not provide adequate guidance to overweight pregnant women, highlighting the urgency for targeted educational programs.
In conclusion, this research illuminates critical areas for improvement in tackling childhood obesity in Morocco. By addressing these gaps, fostering awareness, and enhancing medical practices, the healthcare system can contribute significantly to preventing childhood obesity and improving the overall health of future generations.
Core Tip: In this groundbreaking first study, we focused on an in-depth assessment of the knowledge and practices of physicians in Morocco regarding the link between maternal and childhood obesity, comprehensively investigating from the first months of life through childhood. The growing global scale of childhood obesity makes this research an essential milestone, highlighting significant gaps in medical awareness and practice in Morocco. Our findings highlight the urgency of targeted educational programs, underscoring that this study offers unique insights and crucial implications for the prevention of childhood obesity.
- Citation: Douiyeh I, Khamlich J, Nabih N, Saih A, Boumendil I, Regragui A, Kettani A, Safi A. Assessing Moroccan physician knowledge and practices regarding maternal obesity's impact on childhood obesity: Implications for prevention and intervention. World J Clin Pediatr 2024; 13(2): 91255
- URL: https://www.wjgnet.com/2219-2808/full/v13/i2/91255.htm
- DOI: https://dx.doi.org/10.5409/wjcp.v13.i2.91255
The World Health Organization (WHO) has defined obesity as excess body fat with adverse health consequences. In accordance with the International Classification of Diseases, overweight and obesity are assessed using the body mass index (BMI), which represents the ratio between weight (in kilograms) and the square of height (in meters)[1].
The WHO has established thresholds for adults to define corpulence in terms of BMI, irrespective of gender. However, this approach proves tricky when it comes to assessing corpulence in children.
Indeed, it is impractical to refer to a single BMI value, whatever the age and sex of the child, due to the physiological variations in corpulence during growth and development. In practice, doctors use child-specific BMI reference curves, as well as weight and height reference curves. This more adapted approach takes account of physiological differences linked to age and gender, offering a more accurate assessment of children's corpulence throughout their growth[2].
Certainly, childhood obesity emerges as a critical public health issue with far-reaching implications. The WHO underscores the global scale of this concern, revealing that in 2020, over 39 million children under the age of 5 were identified as overweight or obese[2]. Projections derived from predictive models paint a concerning picture, suggesting that the prevalence of this metabolic disorder is poised to affect more than 70 million children worldwide by 2025[1].
Turning attention to Africa, the WHO's data for 2016 indicated a substantial challenge, with approximately 38.2 million children under the age of 5 being reported as overweight or obese in the continent[2].
Childhood obesity is recognized as an important precursor to adult obesity. The interconnection between obesity in childhood and adulthood is clear, as around 80% of obese children are likely to retain this condition into adulthood[3]. The persistence of obesity from childhood to adulthood can be attributed to the expansion of adipose tissue, intensified during childhood by adipocyte hyperplasia and hypertrophy[4].
The global prevalence of obesity represents a significant issue with far-reaching implications, particularly concerning the health of mothers, fetuses, and children. The escalation of obesity during pregnancy is a parallel concern accompanying the global surge in obesity across various populations. Children born to obese mothers face potential disturbances in their growth trajectories, manifesting as either growth restriction or overgrowth. Elevated fetal weight and adiposity at birth contribute to the heightened risks of macrosomia, complicating the delivery process for larger infants. Furthermore, the ramifications extend beyond birth, impacting the long-term health outcomes of newborns, infants, and eventually, adults. The investigation by Whitaker and his team indicated that maternal obesity during the first trimester of pregnancy is associated with an increased risk. This risk is estimated at 2.0 (95%CI: 1.7 to 2.3%) at age 2, 2.3 (95%CI: 2.0 to 2.6%) at age 3, and 2.3 (95%CI: 2.0 to 2.6%) at age 4[5].
Given the potential and psychological health problems associated with childhood obesity[6,7], addressing this issue becomes paramount through education, prevention, and intervention strategies.
Treatment of childhood obesity involves a combination of lifestyle modifications, behavior therapy, and, in some cases, medication or surgery. Physicians play a pivotal role in both preventing and treating childhood obesity. As primary healthcare providers, they can identify children who are at risk of becoming overweight or obese and intervene early to prevent the development of obesity-related health problems. By providing education and guidance on healthy habits, physical activity, and reducing sedentary behavior, physicians can also refer patients to other healthcare professionals for additional support.
The primary objective of this survey is to pinpoint the challenges and facilitators in primary care as perceived by physicians, proposing strategies to enhance overall practice. In the broader context, the aim is to enhance the likelihood of formulating national guidelines for childhood obesity care, ultimately elevating the quality of healthcare in this domain.
In order to collect the necessary data for assessing the current state of childhood and maternal obesity care in Morocco, we collaborated through a partnership with the Ain CHock ASsociation of Moroccan doctors (ACHAS).
In the initial phase, we dispatched explanatory emails to practitioners engaged in the fields of maternal and childhood obesity, encompassing generalists, gynecologists, diabetologists, and pediatricians. These emails detailed the survey's objectives and acknowledged the main collaborators contributing to the study, namely the ACHAS Association and Hassan II University. The questionnaire was made accessible through a free survey website, and responses were gathered online from September 2021 to July 2022. Additionally, we endeavored to inform select physicians about the study through telephone outreach and during conferences. Unfortunately, the utilization of the free survey website yielded suboptimal results, potentially attributed to practitioners' skepticism regarding the link, as they exhibited a preference for printed questionnaires. Consequently, in alignment with Moroccan cultural preferences, we adopted an alternative strategy employing printed questionnaires and direct engagement with practitioners across various settings, including private clinics, private practices, public hospitals, universities, and military hospitals. This revised approach, however, demonstrated more favorable outcomes.
Survey participation was restricted, with a significant number of approached doctors declining due to time constraints and the questionnaire's length. Only 93 doctors ultimately consented to partake in the study. The questionnaire, comprising 30 distinct questions, necessitated approximately 30 minutes for completion. Respondents were queried on demographic characteristics, maternal obesity care, macrosomia, predictive maternal risk factors for childhood obesity, childhood obesity management, and training in the subject. All collected data were treated as confidential, with the identities of the participants omitted and preserved anonymously.
Upon scrutinizing the data, a discernible gender disparity emerged, with 21% female and 78% male participants. This divergence primarily stems from discrepancies in questionnaire engagement and completion rates between the genders. Notably, male participation exhibited a more pronounced presence, marked by a higher rate of questionnaire completion. Conversely, among female participants, a relatively diminished level of interest was observed, with the majority of those who initially consented to participate failing to complete the questionnaire.
The preponderance of participants received their medical education in Casablanca (56.52%) and Rabat (21.73%). Concerning specialization, 52.17% of participants identified as generalists, while 41.93% were specialists, comprising 19.35% gynecologists and 8.7% pediatricians.
The survey revealed a significant disparity in professional activity between Casablanca and other centers. A notable proportion of survey participants practice in Casablanca (51.61%), the principal metropolitan area in Morocco.
Regarding professional experience, 52.78% of respondents have practiced their specialty for over ten years, whereas 47.12% have practiced for less than ten years. The distribution of respondents across practice settings is as follows: Private practice (46.7%), public hospital (42.2%), university teaching (3.3%), retired (1.1%), and military hospital (1.1%; Table 1).
| Parameter | Effective, n | Percentage (%) |
| Gender | ||
| Women | 20 | 21.5 |
| Men | 73 | 78.5 |
| Age range | ||
| 30 yr or less | 32 | 34.4 |
| 31-40 yr | 29 | 31.2 |
| 41-50 yr | 18 | 19.4 |
| 51-65 yr | 32 | 34.4 |
| 66-75 yr | 2 | 12.9 |
| City of education medicine | ||
| Rabat | 20 | 21.73 |
| Casablanca | 52 | 56.52 |
| Fès | 4 | 4.34 |
| Marrakech | 2 | 2.17 |
| Oujda | 1 | 1.08 |
| Other | 13 | 14.13 |
| Status of participant | ||
| Resident/internal | 4 | 4.30 |
| Generalist | 48 | 51.6 |
| Specialist | 39 | 41.93 |
| Researcher/teacher | 2 | 2 |
| City of medical practice | ||
| Casablanca | 49 | 51.61 |
| Rabat | 6 | 6.45 |
| Other | 38 | 40.86 |
| Current specialty of participants | ||
| Generalist | 48 | 52.17 |
| Gynecology | 18 | 19.35 |
| Pediatrics | 8 | 8.7 |
| Labour doctor | 7 | 7.60 |
| Endocrinologist | 2 | 2.15 |
| Diabetology | 1 | 1.07 |
| Sports medicine | 2 | 2.15 |
| Resident | 2 | 2.15 |
| Nutritionist | 2 | 2.15 |
| Surgery | 1 | 1.07 |
| Length of practice | ||
| Less than 5 yr | 28 | 30.10 |
| 5-10 yr | 13 | 13.97 |
| 11-15 yr | 9 | 9.67 |
| 16-20 yr | 10 | 10.75 |
| 21-30 yr | 23 | 24.73 |
| 31-40 yr | 3 | 3.22 |
| Over 40 yr | 1 | 1075 |
| Type of practice | ||
| University teaching | 3 | 3.3 |
| Private practice | 42 | 46.7 |
| Public hospital | 38 | 42.2 |
| Military hospital | 1 | 1.1 |
| Retired | 1 | 1.1 |
| Other | 6 | 6.45 |
The second section of the inquiry primarily focused on maternal obesity. According to participant responses, 77.9% of the interviewed doctors attend to less than ten overweight pregnant women per week, while 14% manage 11 to 20 cases, and 5.9% handle more than 21 overweight pregnant women weekly. A notable 76.8% of doctors recommend that overweight pregnant women undergo follow-up with a dietitian, while 19% do not. Additionally, 93.1% of doctors educate women about the diverse risks associated with excessive weight gain during pregnancy.
The findings indicate that 24.4% of overweight pregnant women are unaware of the health risks posed by their condition, both for themselves and their child. Furthermore, the results highlight that 52.3% of doctors lack sufficient information about the specific care required for overweight pregnant women (Table 2).
| Parameter | n | Percentage (%) |
| Number of pregnant women consulting overweight | ||
| Less than 10 per week | 67 | 77.9 |
| 11 to 20 per week | 14 | 16.3 |
| 21 to 50 per week | 4 | 4.7 |
| Over 50 per week | 1 | 1.2 |
| Do you suggest overweight pregnant women see a dietitian | ||
| Yes | 63 | 76.8 |
| No | 19 | 23.2 |
| Do you educate women about the risks of excessive weight gain during pregnancy | ||
| Yes | 81 | 93.1 |
| No | 6 | 6.9 |
| Are overweight women aware of the risks of overweight in their health and the health of their child | ||
| Yes | 65 | 75.6 |
| No | 21 | 24.4 |
| Are you sufficiently aware of the care of obese pregnant women | ||
| Yes | 46 | 47.7 |
| No | 42 | 52.3 |
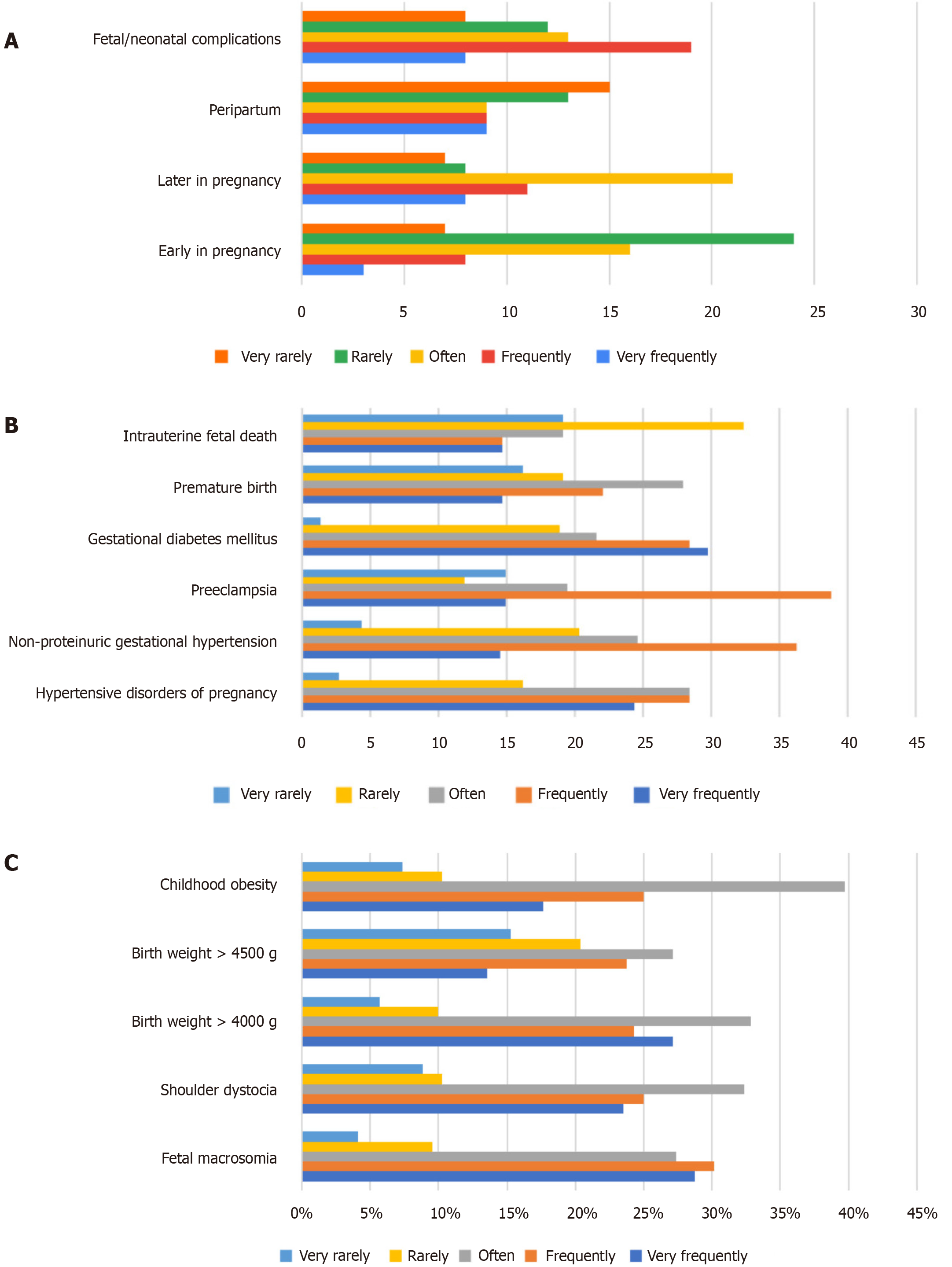
Concerning the incidence of obstetric complications in pregnant women, participating doctors in our survey observed that complications are infrequently noted in early pregnancy and during the peripartum period. However, they are more prevalent and frequent in later stages of pregnancy and during the fetal/neonatal period (Figure 1A).
Complications commonly observed in late pregnancy encompass pre-eclampsia, hypertension, and gestational diabetes, as illustrated in Figure 1B. On the other hand, regarding complications observed in the fetal and neonatal stages, doctors predominantly reported cases of infantile obesity, closely followed by macrosomia and shoulder dystocia, as depicted in Figure 1C.
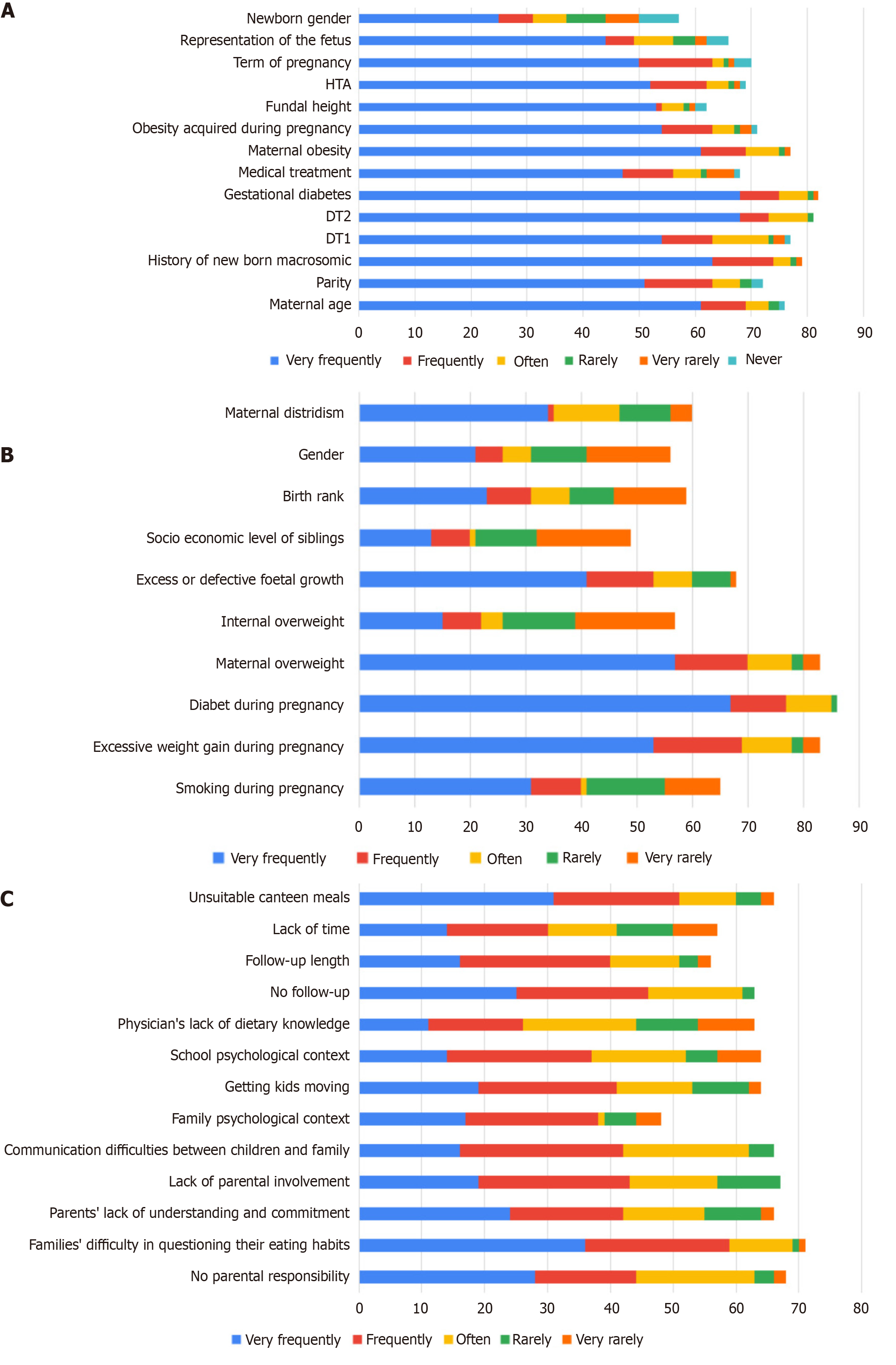
The third section of the survey, dedicated to macrosomia, reveals that 81.2% of the interviewed doctors encounter fewer than ten macrosomic newborns per week, with 16.5% managing 11 to 20 macrosomic newborns and 2.4% handling more than 21 macrosomic newborns weekly. Participants identified five high-risk factors scientifically associated with macrosomia. The majority noted gestational diabetes (71.7%), followed by type 2 diabetes (57.6%), maternal obesity (51.1%), a history of macrosomic newborns (51.1%), and obesity acquired during pregnancy (40.2%; Table 3 and Figure 2A).
| Parameter | n | Percentage (%) |
| On average in a normal week, how many babies are born with macrosomia | ||
| Less than 10 per week | 69 | 81.2 |
| 11 to 20 per week | 14 | 16.5 |
| 21 to 50 per week | 1 | 1.2 |
| Over 50 per week | 1 | 1.2 |
| Select the risks factors that you think are scientifically associated with a risk of macrosomia | ||
| Maternal age | 32 | 34.8 |
| Parity | 18 | 19.6 |
| History of new born macrosomic | 47 | 51,1 |
| DT1 | 33 | 35.9 |
| DT2 | 53 | 57.6 |
| Gestational diabetes | 66 | 71.7 |
| Medical treatment | 12 | 13 |
| Maternal obesity | 47 | 51.1 |
| Obesity acquired during pregnancy | 37 | 40.2 |
| Fundal height | 24 | 26.1 |
| HTA | 13 | 14.1 |
| Term of pregnancy | 15 | 16.3 |
| Representation of the fetus | 4 | 4.3 |
| Newborn gender | 4 | 4.3 |
An analysis of the participants' responses reveals that 76.7% of them consider diabetes during pregnancy to be closely linked to an increased risk of obesity in children, followed by excessive weight gain during pregnancy and maternal overweight at 56.7% each (Table 4).
| Parameter | n | Percentage (%) |
| Which of the following risk factors do you think are scientifically associated with a risk of childhood obesity for the unborn child | ||
| Smoking during pregnancy | 8 | 8.9 |
| Excessive weight gain during pregnancy | 51 | 56.7 |
| Diabetes during pregnancy | 69 | 76.7 |
| Maternal overweight | 51 | 56.7 |
| Excess or defective foetal growth | 20 | 22.2 |
| Socio economic level of siblings | 7 | 7.8 |
| Birth rank | 3 | 3.3 |
| Gender | 4 | 4.4 |
| Maternal depression | 28 | 31.1 |
| Do you feel sufficiently aware of the management of pediatric obesity | ||
| Yes | 54 | 62.8 |
| No | 32 | 37.2 |
| Do you feel sufficiently aware of the effect of maternal overweight on pediatric obesity | ||
| Yes | 43 | 48.3 |
| No | 46 | 51.7 |
Figure 2B, presented in our results, clearly shows participants' lack of interest in maternal weight during consultations. On the other hand, 51.7% of participants stated that they did not feel sufficiently informed about the impact of maternal overweight on paediatric obesity.
The final segment of the survey focused on the area of childhood obesity. Participants' responses indicate that 93.6% of surveyed physicians reported encountering fewer than ten obese children weekly. In contrast, 6.4% of surveyed physicians grapple with 11 to 20 cases, while 12.9%contend with more than 50 cases of childhood obesity per week.
Regarding the tools and criteria employed by healthcare professionals to identify childhood obesity, participants underscored several critical approaches. The most prevalent methods included the utilization of weight and height curves, favored by 49.4% of respondents, closely followed by the use of a BMI over 30, selected by 48.1% of participants. Moreover, an equal percentage of 48.1% emphasized the importance of traditional weight and height measurements as crucial tools for detecting childhood obesity.
An examination of participants' responses highlights that the most pivotal areas for addressing childhood obesity include nutrition and parental education, garnering a significant 61.5%. Additionally, children's lifestyle was identified as a crucial element, receiving a response of 60.3%. The significance of children's diet was also underscored, with a percentage of 51.3%.
Furthermore, participants accentuated the value of collaboration in managing childhood obesity, particularly with nutritionists (58.8%) and dietitians (53.8%). This underscores the acknowledgment among participants of the importance of involving specialized professionals in the interdisciplinary approach to addressing the multifaceted aspects of childhood obesity (Table 5).
| Parameter | n | Percentage (%) |
| On an average week, how many obese children come to you | ||
| Less than 10 per week | 73 | 93.6 |
| 11 to 20 per week | 5 | 6.4 |
| 21 to 50 per week | 0 | 0 |
| Over 50 per week | 2 | 12.9 |
| What criteria and tools do you use to detect obesity in children | ||
| Clinical examination | 37 | 45.7 |
| Physical appearance | 26 | 32.1 |
| Weight and height | 39 | 48.1 |
| Balance | 24 | 29.6 |
| BMI > 30 | 39 | 48.1 |
| Study of growth curve/chart | 31 | 38.3 |
| Weight and height curves | 40 | 49.4 |
| Weight/height ratio | 22 | 27.2 |
| What areas in the overall management of this child’s obesity seem essential to you | ||
| Nutrition and parenting | 48 | 61.5 |
| Family history, environment | 23 | 29.5 |
| Parent’s motivations | 29 | 37.2 |
| Child education | 38 | 48.7 |
| Children’s diet | 40 | 51.3 |
| Children’s physical activity | 33 | 42.3 |
| Psychological evaluation of | 28 | 35.9 |
| Child’s lifestyle | 47 | 60.3 |
| Children’s habits | 25 | 32.1 |
| History of childhood obesity | 23 | 29.5 |
| Child’s motivation | 25 | 32.1 |
| What network of partners would you be likely to mobilize in this care | ||
| Dietician | 43 | 53.8 |
| Nutritionist | 47 | 58.8 |
| Psychiatrist | 21 | 26.3 |
| Pediatrician | 33 | 41.3 |
| Endocrinologist | 33 | 41.3 |
| Sport educator | 24 | 24 |
| Physical education teacher | 14 | 17.4 |
| Multidisciplinary team | 1 | 1.3 |
| Parents and child | 1 | 1.3 |
| Prent first | 1 | 1.3 |
| Child psychiatrist | 1 | 1.3 |
| Have you received training in childhood obesity | ||
| Yes | 7 | 9.1 |
| No | 67 | 87 |
| If you were offered training in the management of childhood obesity, what topics would you like to see covered | ||
| Behavioral approaches/therapies | 29 | 38.7 |
| Psychotherapy | 15 | 20 |
| Psychological approach | 16 | 16 |
| Low calories diets | 20 | 26.7 |
| Nutrition | 42 | 56 |
| Ways to motivate children and parents | 23 | 30.7 |
| Preventive and educational methods | 21 | 28 |
| Request for treatment in specialized centers | 9 | 12 |
| Follow-up of childhood obesity in clinical cases | 26 | 34.7 |
| Clinical and metabolic consequences of obesity | 17 | 22.7 |
| Complications in obese children | 19 | 25.3 |
Ensuring the well-being of these children presents significant challenges, with primary impediments encountered by healthcare professionals arising from families displaying reluctance to scrutinize their eating habits, inadequately adapted meals in the canteen, inconsistent monitoring practices, communication barriers between children and their families, and a lack of parental responsibility (Figure 2C). Approximately 87% of the surveyed physicians disclosed a lack of specific training in childhood obesity, indicating a substantial deficiency in their professional preparation to address this urgent health concern. This underscores a critical gap in the healthcare system's capacity to adeptly navigate the intricacies associated with pediatric obesity. Additionally, it is noteworthy that 56% of participants expressed a keen interest in receiving training specifically focused on nutrition.
The study identifies critical findings and offers recommendations to address childhood obesity effectively. It underscores a lack of systematic risk assessment and awareness among healthcare providers regarding childhood obesity, emphasizing the need for standardized protocols and enhanced training programs. Additionally, the study emphasizes the importance of multifaceted approaches, including nutrition education, lifestyle modifications, and early screening initiatives, to combat childhood obesity. It also advocates for the establishment of pediatric obesity medicine centers to provide resources and research opportunities. Furthermore, integrating maternal health into obesity prevention strategies is proposed for a holistic approach to family health. The study aims to fill existing gaps in understanding how healthcare professionals in Morocco approach maternal obesity, providing insights that can inform targeted interventions and contribute to the broader goal of mitigating the childhood obesity epidemic. The implications of this study extend to improved healthcare practices, enhanced medical education, and the overall well-being of future generations.
According to United Nations International Children's Emergency Fund, Asia and Africa collectively harbor 42 million children under the age of five who are overweight or obese[8]. Despite the escalating prevalence of childhood obesity on a global scale, Morocco has not fully grasped the magnitude and repercussions of this phenomenon.
Ien terms of study limitations, data collection was a major challenge. Physicians' demanding workloads made it difficult to obtain respondents available to complete the questionnaire.
A 2011 survey conducted on the population and health of the Moroccan family revealed that 12.5% of children under the age of 5 are overweight, of whom 2.6% suffer from obesity. In 2003-2004, this proportion of affected children was 10.4%. Adolescents aged 13 to 15 are also affected, with overweight and obesity rates of 14.6% and 2.8%, respectively, according to the 2010 Moroccan School Student Health Survey[9].
Recent research indicates that the first three years of a child's life can predict the development of obesity. During this initial phase, there is a critical involvement in molding eating habits and lifestyle, exerting a substantial impact on the child's subsequent weight trajectory. Family environments and behaviors during these early years are crucial factors associated with predisposition to obesity in children. These findings highlight the importance of implementing preventive interventions and health promotion programs from the earliest years of life to reduce the risk of childhood obesity[10].
The WHO recognizes that the battle against the epidemic of childhood obesity cannot rely solely on isolated interventions. Indeed, it is crucial to consider the three critical stages of life: preconception and pregnancy, infancy, and childhood and adolescence[11].
Concerning preconception and pregnancy, the WHO strongly advocates for screening and management of hyperglycemia and gestational hypertension. It is also essential to ensure appropriate follow-up and management to control weight gain during pregnancy. Additionally, guidance and counseling for future parents before conception and during pregnancy must emphasize the importance of suitable nutrition[11,12].
Various studies have investigated the implications of fetal macrosomia, highlighting its significant association with overweight and obesity[13,14]. A systematic review, incorporating the results of 20 separate studies, corroborated this relationship, demonstrating that macrosomia is a significant risk factor for obesity in both children and adults[15].
In particular, the development of macrosomia is intimately linked to several factors, including maternal obesity and gestational diabetes. The mechanisms underlying this complex relationship highlight the impact of maternal health conditions on the child's birth weight and, by extension, on his or her subsequent risk of developing obesity problems[16].
From the results of the responses obtained from physicians (Figure 2A), it is clear that the search for risk factors associated with macrosomia is not a systematic practice within the medical community. This finding suggests variability in clinical approach, underlining the need for greater awareness of macrosomia risk assessment during medical consultations.
On the other hand, according to our findings, 19% of doctors do not recommend that overweight pregnant women consult a dietician, and 6.9% do not even educate women about the risks associated with excessive weight gain during pregnancy. Worryingly, 24.4% of overweight pregnant women are unaware of the repercussions of excess weight on their health and that of their child. In addition, more than half of doctors (52.3%) do not feel sufficiently informed about the care of obese pregnant women, which could explain the lack of advice given to their patients (Table 2).
WHO guidelines encompass all manifestations of malnutrition, whether nutritional deficiency or nutritional excess[11,12], the latter being of particular concern in Morocco. Cultural influence, in particular the misconception widespread among Moroccan mothers and society, encourages pregnant women to adopt the erroneous idea that they need to eat for two, leading to maternal overweight. This misperception contributes to nutrition-related health problems, and underlines the importance of increased education and awareness to promote healthy eating practices during pregnancy. In addition, a study carried out at the maternity hospital in Morocco revealed that maternal overweight and obesity are a problem in the population studied, with prevalence of 34.9% and 41% respectively[17].
These data underline the urgent need for training programs to raise awareness and encourage doctors to provide appropriate advice to overweight pregnant women. Filling these knowledge gaps is essential to ensure proper management. Previous studies have clearly demonstrated that dietary advice can have very positive effects, not only on gestational weight gain, but also on glucose metabolism, underlining the importance of strengthening the training of healthcare professionals in this specific area[18,19].
According to our study, 76.7% of participants consider diabetes during pregnancy to be a risk factor for childhood obesity, followed closely by maternal weight gain and maternal obesity (56.7%; Table 4). These findings align with doctors' observations, which are in complete accordance with the extensive scientific research in this field. Various studies have conclusively established that gestational diabetes is a significant risk factor for the subsequent development of obesity in young children[20,21]. In addition, a review by Adriana Mannino and colleagues concluded that the impact of maternal overweight on childhood obesity is no longer open to dispute, underlining the need for targeted interventions to prevent this growing scourge[22].
However, it is interesting to note that, in practice, little attention is given to maternal weight during medical consultations (Figure 2B). This neglect may stem from the fact that 51.7% of participants did not feel sufficiently informed about the impact of maternal obesity on pediatric obesity. This finding raises further important questions about the awareness and importance given to this specific aspect of maternal health during medical interactions. This underscores the need for increased awareness and also highlights potential gaps in participants' knowledge and understanding of the crucial link between maternal weight and its impact on pediatric health. These observations further emphasize the imperative of targeted educational initiatives and reinforced communication strategies to bridge this awareness gap among individuals participating in medical consultations[11].
It is crucial to provide clear guidance and support to promote good nutrition, healthy diets, physical activity and to discourage the use of, and exposure to, tobacco, alcohol, drugs and other toxins[11].
As far as early childhood is concerned, the WHO has drawn up a number of guidelines to promote healthy eating, adequate sleep and physical activity, with the aim of instilling good habits in children from an early age. Among these guidelines, some are of particular importance. Firstly, it is crucial to raise parents' awareness of the benefits of breastfeeding for both mother and child, through appropriate training. It is also essential to actively encourage mothers to opt for breastfeeding. In addition, clear guidance needs to be provided on recommended sleep duration and the management of time spent on sedentary activities, helping to foster healthy development in children and prevent potential health problems[11].
A recent study in Norway, involving 170 children, has deepened our understanding of the links between childhood obesity and sleep patterns. The results of this research highlight an important nuance beyond simple sleep duration, emphasizing that the precise timing of sleep may represent a risk factor of more substantial concern than total sleep duration. In particular, the study significantly observed that overweight children have later sleep schedules compared with their normal-weight peers. This finding suggests a correlation between late sleep schedules and the risk of obesity in children. These findings could inform health recommendations to promote healthy sleep habits from childhood onwards, aiding in averting childhood obesity and enhancing the general well-being of young people[23].
According to the conclusions drawn from our study, a significant proportion - 61.5% of participants - consider nutrition and parental education to be crucial areas in the management of childhood obesity. In a more immediate context, the child's lifestyle was also considered essential by 60.3% of participants, closely followed by diet-related concerns, mentioned by 51.3% (Table 4).
With regard to obesity screening, there is no comprehensive guide to optimal screening for childhood obesity. This is in line with the results of our survey: participants used different strategies to identify childhood obesity (Table 4).
Early detection of childhood obesity represents a crucial issue in promoting children's health, but it proves to be a delicate task due to the various factors involved. Identifying the early signs of this condition in its initial stages is, of course, complex. Indeed, it's becoming imperative for doctors to systematically incorporate the calculation of BMI into every pediatric consultation.
Regular monitoring of BMI and its recording on weight curves creates a visual history of a child's weight growth over time. According to the latest research, doctors should systematically examine weight/length curves for children under two and BMI for children over 2, in addition to standard weight and length curves. As BMI increases with age, percentiles specific to age and sex are used rather than BMI[24].
This procedure provides health practitioners with crucial data for assessing a child's physical evolution and detecting any propensity towards obesity in the early stages. It is also relevant to note that 60% of children who are overweight at the age of one will not maintain this condition into adulthood. These curves are particularly useful around the age of 6, when physiological variations in weight can make clinical assessment misleading. At this age, children of normal build who may appear slim could be masking overweight in those whose BMI is around the 97th percentile, which may not be clinically evident[25].
Emphasizing the importance of this approach highlights the need for constant vigilance on the part of practitioners to anticipate and treat any risk of obesity in children at an early stage. This proactive approach not only contributes to preventive health management, but also offers the opportunity to initiate early interventions, thus promoting more positive outcomes for children's long-term well-being.
Participants also recognized the importance of collaboration with nutritionists and dietitians in the management of childhood obesity. Participants acknowledged several obstacles in the management of obesity (Figure 2C), arising from families reluctant to examine their eating habits, insufficiently adapted meals in the canteen, inconsistent monitoring practices, communication barriers between children and their families, and a lack of parental responsibility (Figure 2C). These challenges collectively underscore the complex nature of effectively monitoring the health of these children. Tackling these obstacles requires a comprehensive, multidimensional approach, encompassing not only dietary and lifestyle considerations but also a nuanced understanding of the interpersonal dynamics within families. Effective monitoring demands a holistic approach to these issues, recognizing the interdependence of the various elements that contribute to the overall health and well-being of these children.
A significant portion of participants indicated that they had never received training in childhood obesity and expressed an interest in undergoing nutrition training to enhance their ability in dealing with obesity cases (Figure 2C). This desire for additional training underscores the recognition among healthcare professionals of the central role nutrition plays in the management of childhood obesity. The call for nutrition training reflects a proactive stance on the part of these professionals, signaling a commitment to enhancing their expertise and, ultimately, improving the quality of care provided to children facing obesity problems.
These findings collectively underscore the imperative of targeted educational programs and initiatives within the medical community. Bridging the knowledge gap through comprehensive training not only meets the immediate needs of healthcare professionals, but also contributes to the broader goal of fostering a more informed and competent healthcare system in the face of the growing concern about childhood obesity.
In 2014, a collaborative team of researchers from Tunisia, Morocco, France and England formulated a strategy to mitigate the escalation of obesity as part of the Cooperation in university and scientific research obe-Maghreb research project. This initiative, active from 2013 to 2017, comprises five distinct strands: encouraging the production of health-promoting foods, shaping the environment to encourage healthy physical activity, educating the population on the adoption of good eating behaviors, improving obesity screening and management services, and implementing an information, communication and education plan to prevent and combat obesity. The fourth component is dedicated to strengthening the basic training program for medical and paramedical students in the detection and management of obesity. This involves developing teaching modules, integrating and implementing training in screening and management, and establishing systematic screening for excess weight before and during the university career. In addition, this component aims to reinforce the basic training program for students in the medical and paramedical fields by systematically screening for obesity in pre-school, school, professional (public and private) and health environments[26].
Morocco's commitment to tackling childhood obesity and aligning itself with the recommendations of WHO and the guidelines of the 2011-2019 national nutrition strategy cannot be overlooked. Indeed, Morocco launched a promising strategy in 2016 to develop a plan to prevent and control obesity and overweight among children. This strategy is structured around several stages: first, a literature review of international recommendations and other countries' experiences in preventing and controlling childhood obesity. Next, a summary of the current nutritional and epidemiological situation of children, identifying the gains to be consolidated and the opportunities to be seized. In addition, a review of programs and interventions carried out by the Ministry of Health and its partners, aimed at contributing to the prevention and control of overweight and obesity, identifying strengths and areas for improvement. Secondly, the establishment of an operational plan adopting a logical framework approach, followed by the presentation and discussion of the operational plan. Finally, the facilitation of national consensus workshops and the final validation of the above-mentioned plan. This approach demonstrates Morocco's commitment to the fight against childhood obesity by adopting a strategic and coordinated approach in line with international best practices[9]. However, to date, there has been no feedback on the implementation of the above-mentioned steps. This observation underlines the importance of implementing transparent and regular monitoring to assess the effectiveness of the measures undertaken and guarantee the success of this national strategy.
Establishing dedicated pediatric obesity medicine centers would be highly advantageous in addressing this significant health concern. Such centers are pivotal in the comprehensive management of childhood obesity, offering essential resources and infrastructure to foster new knowledge generation and innovation in the field. Additionally, these centers hold the potential to provide multidisciplinary training, equipping the next generation of scientists with the skills necessary to effectively address this intricate issue.
Specialized training programs conducted by these centers can play a crucial role in increasing awareness and educating healthcare professionals, researchers, and practitioners involved in childhood obesity management. By disseminating in-depth knowledge and promoting a collaborative approach, these centers contribute to the development of expertise in the field.
Moreover, these specialized centers possess the capability to actively contribute to the formulation of guidelines and treatment protocols aimed at enhancing childhood obesity management. Through collaboration with multidisciplinary experts, they can develop evidence-based guidelines that incorporate the latest scientific advancements, guiding practitioners toward effective and appropriate interventions.
Furthermore, it would be pertinent to integrate the monitoring of overweight pregnant women into initiatives aimed at preventing obesity associated with maternal obesity. In particular, centers dedicated to pediatric obesity medicine could expand their focus to encompass the monitoring and management of pregnant women's weight.
This integrated approach, addressing both maternal and child health, holds significant preventive potential in the battle against obesity from the earliest life stages. It underscores the importance of a holistic strategy, wherein the management of childhood obesity is intricately linked to the monitoring and management of maternal weight, fostering more positive outcomes for the overall health of the family.
Finally, nations should implement or establish effective mechanisms for disseminating research findings to both the general public and relevant healthcare professionals. This dissemination can be achieved through existing national, regional, and international journals, as well as through websites and databases that may have regional relevance.
In Morocco, there is a deficiency in scientific publications, newspapers, and magazines dedicated to the subject of obesity. The accessibility of scientific information plays a crucial role in keeping knowledge up-to-date and conveying new expertise and treatments to physicians. Nevertheless, there is a genuine necessity to facilitate the transmission of information to physicians by establishing Moroccan publications specifically focused on obesity.
If the primary objective of medicine is to prioritize the preservation of life, it becomes essential to articulate the conditions of survival and define the quality of that survival. Through adequate education and comprehensive training, we can collaboratively enhance the quality of life for our patients. Empowering local doctors with the necessary expertise to deliver specialized care for childhood and maternal obesity is the only sustainable approach to expanding access to such care. However, achieving this goal requires the establishment of a robust infrastructure, backed by local authorities, and collaboration with countries where the management of childhood and maternal obesity is a common practice. If the primary objective of medicine is to prioritize the preservation of life, it becomes essential to articulate the conditions of survival and define the quality of that survival. Through adequate education and comprehensive training, we can collaboratively enhance the quality of life for our patients. Empowering local doctors with the necessary expertise to deliver specialized care for childhood and maternal obesity is the only sustainable approach to expanding access to such care. However, achieving this goal requires the establishment of a robust infrastructure, backed by local authorities, and collaboration with countries where the management of childhood and maternal obesity is a common practice.
| 1. | The World Health Organization. Obesity. 2017. [cited 2 April 2024]. Available from: https://www.who.int/health-topics/obesity. |
| 2. | The World Health Organization. Key facts about obesity and overweight. 2021. [cited 2 April 2024]. Available from: https://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight. |
| 3. | Lee JM, Pilli S, Gebremariam A, Keirns CC, Davis MM, Vijan S, Freed GL, Herman WH, Gurney JG. Getting heavier, younger: trajectories of obesity over the life course. Int J Obes (Lond). 2010;34:614-623. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 129] [Cited by in RCA: 139] [Article Influence: 8.7] [Reference Citation Analysis (0)] |
| 4. | Freedman DS, Sherry B. The validity of BMI as an indicator of body fatness and risk among children. Pediatrics. 2009;124:S23-S34. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 323] [Cited by in RCA: 332] [Article Influence: 20.8] [Reference Citation Analysis (0)] |
| 5. | Leddy MA, Power ML, Schulkin J. The impact of maternal obesity on maternal and fetal health. Rev Obstet Gynecol. 2008;1:170-178. [PubMed] |
| 6. | Nader N, Singhal V, Javed A, Weaver A, Kumar S. Temporal trends in the diagnosis and management of childhood obesity/overweight in primary care. J Prim Care Community Health. 2014;5:44-49. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 7. | Liang L, Meyerhoefer C, Wang J. Obesity counseling by pediatric health professionals: an assessment using nationally representative data. Pediatrics. 2012;130:67-77. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 28] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 8. | Moumen H. UNICEF-WHO-The World Bank: Joint Child Malnutrition Estimates (JME) - Levels and Trends - 2023 edition. UNICEF DATA. May 18, 2023. [cited 2 April 2024]. Available from: https://data.unicef.org/resources/jme-report-2023/. |
| 9. | Royaume du Maroc, Ministère de la Santé, Direction de la Population. Stratégie Nationale de Nutrition Elaboration d'un plan de prévention et du contrôle de l'Obésité et du surpoids chez les enfants. 2016. Available from: https://www.sante.gov.ma/Documents/2016/04/TDR%20ob%C3%A9sit%C3%A9%20infantile%202016%20finalfinalfinal.pdf. |
| 10. | Geserick M, Vogel M, Gausche R, Lipek T, Spielau U, Keller E, Pfäffle R, Kiess W, Körner A. Acceleration of BMI in Early Childhood and Risk of Sustained Obesity. N Engl J Med. 2018;379:1303-1312. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 413] [Cited by in RCA: 526] [Article Influence: 75.1] [Reference Citation Analysis (0)] |
| 11. | Organisation mondiale de la Santé. Rapport de la Commission pour mettre fin à l'obésité de l'enfant. Mar 24, 2016. [cited 3 April 2024]. Available from: https://apps.who.int/gb/ebwha/pdf_files/WHA69/A69_8-fr.pdf. |
| 12. | Organisation mondiale de la Santé. Rapport de la Commission pour mettre fin à l'obésité de l'enfant : plan de mise en œuvre. Mar 27, 2017. [cited 3 April 2024]. Available from: https://apps.who.int/gb/ebwha/pdf_files/WHA70/A70_31-fr.pdf. |
| 13. | Rugholm S, Baker JL, Olsen LW, Schack-Nielsen L, Bua J, Sørensen TI. Stability of the association between birth weight and childhood overweight during the development of the obesity epidemic. Obes Res. 2005;13:2187-2194. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 93] [Cited by in RCA: 96] [Article Influence: 7.4] [Reference Citation Analysis (0)] |
| 14. | Pan XF, Tang L, Lee AH, Binns C, Yang CX, Xu ZP, Zhang JL, Yang Y, Wang H, Sun X. Association between fetal macrosomia and risk of obesity in children under 3 years in Western China: a cohort study. World J Pediatr. 2019;15:153-160. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 24] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 15. | Yu ZB, Han SP, Zhu GZ, Zhu C, Wang XJ, Cao XG, Guo XR. Birth weight and subsequent risk of obesity: a systematic review and meta-analysis. Obes Rev. 2011;12:525-542. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 414] [Cited by in RCA: 374] [Article Influence: 26.7] [Reference Citation Analysis (0)] |
| 16. | Mohammadbeigi A, Farhadifar F, Soufi Zadeh N, Mohammadsalehi N, Rezaiee M, Aghaei M. Fetal macrosomia: risk factors, maternal, and perinatal outcome. Ann Med Health Sci Res. 2013;3:546-550. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 45] [Cited by in RCA: 60] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 17. | Taoudi F, Laamiri FZ, Barich F, Hasswane N, Aguenaou H, Barkat A. Study of the Prevalence of Obesity and Its Association with Maternal and Neonatal Characteristics and Morbidity Profile in a Population of Moroccan Pregnant Women. J Nutr Metab. 2021;2021:6188847. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 7] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 18. | Wolff S, Legarth J, Vangsgaard K, Toubro S, Astrup A. A randomized trial of the effects of dietary counseling on gestational weight gain and glucose metabolism in obese pregnant women. Int J Obes (Lond). 2008;32:495-501. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 263] [Cited by in RCA: 267] [Article Influence: 15.7] [Reference Citation Analysis (0)] |
| 19. | Artal R, Catanzaro RB, Gavard JA, Mostello DJ, Friganza JC. A lifestyle intervention of weight-gain restriction: diet and exercise in obese women with gestational diabetes mellitus. Appl Physiol Nutr Metab. 2007;32:596-601. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 143] [Cited by in RCA: 128] [Article Influence: 7.1] [Reference Citation Analysis (0)] |
| 20. | Ardıç C, Çolak S, Uzun K, Salı G, Aydemir T, Telatar G. Maternal Gestational Diabetes and Early Childhood Obesity: A Retrospective Cohort Study. Child Obes. 2020;16:579-585. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 21. | Mantzorou M, Papandreou D, Pavlidou E, Papadopoulou SK, Tolia M, Mentzelou M, Poutsidi A, Antasouras G, Vasios GK, Giaginis C. Maternal Gestational Diabetes Is Associated with High Risk of Childhood Overweight and Obesity: A Cross-Sectional Study in Pre-School Children Aged 2-5 Years. Medicina (Kaunas). 2023;59. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 6] [Reference Citation Analysis (0)] |
| 22. | Mannino A, Sarapis K, Moschonis G. The Effect of Maternal Overweight and Obesity Pre-Pregnancy and During Childhood in the Development of Obesity in Children and Adolescents: A Systematic Literature Review. Nutrients. 2022;14. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 21] [Reference Citation Analysis (0)] |
| 23. | Skjåkødegård HF, Danielsen YS, Frisk B, Hystad SW, Roelants M, Pallesen S, Conlon RPK, Wilfley DE, Juliusson PB. Beyond sleep duration: Sleep timing as a risk factor for childhood obesity. Pediatr Obes. 2021;16:e12698. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 32] [Cited by in RCA: 41] [Article Influence: 10.3] [Reference Citation Analysis (0)] |
| 24. | Barlow SE; Expert Committee. Expert committee recommendations regarding the prevention, assessment, and treatment of child and adolescent overweight and obesity: summary report. Pediatrics. 2007;120:S164-S192. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3035] [Cited by in RCA: 3062] [Article Influence: 170.1] [Reference Citation Analysis (0)] |
| 25. | Thibault H, Rolland-Cachera MF. [Prevention strategies of childhood obesity]. Arch Pediatr. 2003;10:1100-1108. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 22] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 26. | El Ati J, Traissac P, Delpeuch F, Aounallah-Skhiri H, Béji C, Eymard-Duvernay S, Bougatef S, Kolsteren P, Maire B, Ben Romdhane H. Gender obesity inequities are huge but differ greatly according to environment and socio-economics in a North African setting: a national cross-sectional study in Tunisia. PLoS One. 2012;7:e48153. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 34] [Cited by in RCA: 41] [Article Influence: 3.2] [Reference Citation Analysis (0)] |