Published online Mar 9, 2024. doi: 10.5409/wjcp.v13.i1.87713
Peer-review started: August 23, 2023
First decision: September 19, 2023
Revised: November 10, 2023
Accepted: December 28, 2023
Article in press: December 28, 2023
Published online: March 9, 2024
Processing time: 196 Days and 4.9 Hours
Maintenance rates of exclusive breastfeeding (EBF) worldwide are low, thus, one of the objectives of the summary of policies on breastfeeding (BF) in world nutrition goals for 2025 are that at least 50% of infants under six months of age receive EBF that year. The Objective of this study is to document the rates of EBF in children born in San Ignacio University Hospital (HUSI) and identify factors associated with maintenance.
To document the percentages of EBF in those that were born at HUSI and identify factors associated to their maintenance.
This is a study of cases and controls in an analytic, retrospective cohort that took children born alive between January 2016 and January 2019 at HUSI located in the city of Bogotá, Colombia.
Receiving information about BF at HUSI was able to maintain EBF up until 4 mo (OR = 1.65; 95%CI: 1.02-2.66). The presence of gynecologic and obstetric comorbidities (OR = 0.32; 95%CI: 0.12-0.83), having mastitis (OR = 0.56; 95%CI: 0.33-0.94), and receiving information from mass media (OR = 0.52; 95%CI: 0.31-0.84) are factors associated with not maintaining EBF.
Receiving education at a Women- and Child-Friendly Institution was the only significant factor to achieve EBF until 4 mo, with a frequency greater than the one reported in the country, which matches multiple studies where counseling and individualized support on BF achieve this purpose. Knowledge about BF and early detection of obstetric/gynecologic complications must be strengthened among the healthcare staff in charge of mothers during post-partum. Additionally, strategies must be promoted to continue BF such as creating milk banks with the objective of increasing BF rates even when mothers return to work.
Core Tip: Globally, exclusive breastfeeding (EBF) maintenance rates are low; therefore, one goal of the breastfeeding policy brief is to improve it. In the present study, we document that receiving information about BF in our hospital managed to maintain EBF up to 4 mo and that the presence of gyneco-obstetric comorbidities, having mastitis and receiving information from mass media were factors associated with non-maintenance of EBF.
- Citation: Murillo Galvis M, Ortegon Ochoa S, Plata García CE, Valderrama Junca MP, Inga Ceballos DA, Mora Gómez DM, Granados CM, Rondón M. Exclusive breastfeeding greater than 50%, success of education in a university hospital in Bogotá: Case-control study. World J Clin Pediatr 2024; 13(1): 87713
- URL: https://www.wjgnet.com/2219-2808/full/v13/i1/87713.htm
- DOI: https://dx.doi.org/10.5409/wjcp.v13.i1.87713
The international community recognizes breastfeeding (BF) as the healthiest, most economic, and safe way of feeding a newborn and infant. The World Health Organization (WHO) defines exclusive BF (EBF) as the single intake of breastmilk without any other food or beverage, including water, during the first six months of life[1]. As for the European positions, European Society for Paediatric Gastroenterology, Hepatology and Nutrition (ESPGHAN) considers that 6 mo of EBF is the desirable objective, however, according to the nutritional needs of each child, complementary feeding, as defined by the WHO as the period in which BF is given together with other foods and beverages (including dairy formulas and breast milk substitutes), can be initiated earlier, but never in children younger than 17 wk of life[2].
Despite these positions, low rates of onset and maintenance of BF persist globally which becomes a public health problem[2]. Because of this, in 1990 international associations met with support of the WHO and UNICEF and created the Innocenti Declaration; a declaration intended to promote, protect, and support BF. This declaration established a series of criteria that each government must comply with to increase BF rates, which include the creation of a national BF committee, compliance to the “ten steps for healthy breast feeding,” regulation of breast milk substitutes, and infant formulas, and the protection and BF rights for working women[3]. In addition, the WHO suggests that 50% of children under 6 mo must receive EBF by the decade ending on 2025[4].
The “2015 National Nutritional Situation in Colombia” (ENSIN) documented that in our country, EBF has presented a progressive reduction since 2005, where 46.9% of children under 6 mo received EBF while in 2015 only 36.1% did so, a level very inferior to the global average of 43%[4]. The 2010-2020 Ten-Year Plan from the Ministry of Health Promotes Institutions that apply the Women- and Child-Friendly Institution model (WCFI), adopted by San Ignacio University Hospital (HUSI) in 2013 which looks to promote BF and quality care for mothers and children through different political, family, educational, and other actions[5]. HUSI applies the WCFI strategy educating both the parents of newborns that are by the mother during postpartum as those that are hospitalized in the newborn unit about to be discharged. Taking this context into account, the objective of the study is to document the percentages of EBF in those that were born at HUSI and identify factors associated to their maintenance.
Case study and controls in a retrospective, analytical cohort. The two definitions of the WHO and ESPGHAN were included. This was conducted between January 2016 and January 2019 through calls to mothers of newborns at HUSI in Bogotá, Colombia. The Research Ethics Committee at HUSI and the Faculty of Medicine of the Javeriana Pontifical University approved the study on June 28, 2018.
All newborns at HUSI between the dates mentioned were included in the study. 10 exclusion criteria were considered: mother with human immunodeficiency virus; documented type 1 herpes virus on the nipple; mother with severe diagnosed disease during the prenatal period that avoided feeding with breast milk; mothers that received medications contraindicated in BF such as anticoagulants, cardiovascular (amiodarone, ergotamine), antineoplastic, psychologic drugs, iodides, amphetamines, cocaine, lysergic acid diethylamide, marihuana; patients with mothers that have received radioactive iodine-131 or that have received iodine or topical iodophors given the prolonged time of bioavailability; patients with galactosemia; maple syrup urine disease, phenylketonuria or newborn patients with weight below 1500 g, or less than 32 wk that require additional feeding (substitutes).
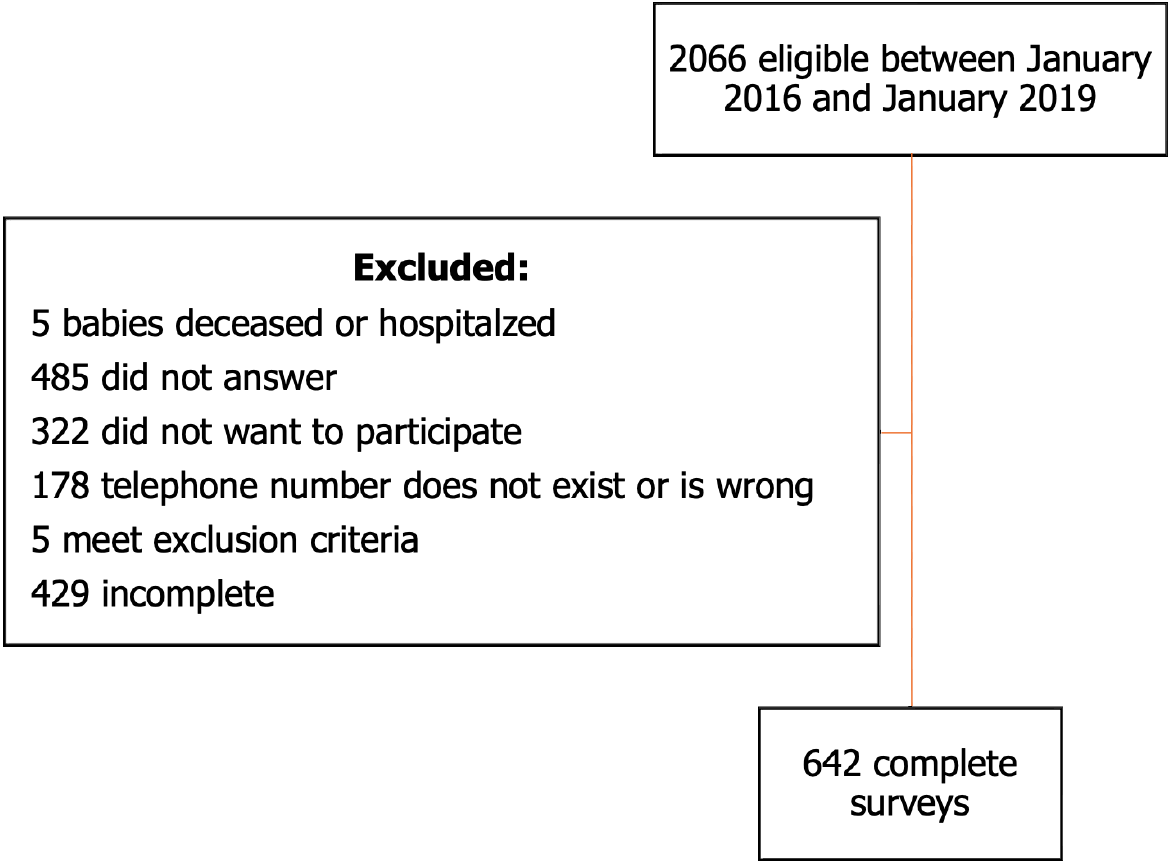
Size determination of the sample considered the prevalence of EBF documented in the 2015 ENSIN, the inclusion of the maximum association model of 20 parameters, and the possibility of 10 positive outcomes for every parameter with which a total of 583 surveys was calculated as 10% failed responses is added to the above (wrong telephone numbers, no response by the mother, incomplete information) for a total of 642 complete surveys to collect (Figure 1).
A 25-question telephone survey was conducted, divided into 5 sections: the first includes social-demographic factors (maternal age, minor’s age, place of residence, education level, parity, cigarette consumption, and monthly income). The second section was centered on the age of suspension of BF and the reasons why it was discontinued. Knowledge about BF and its benefits were part of the third section. The fourth section documented diseases during pregnancy and BF, and the last section gathered information received both before and after delivery about BF and places where that information was received.
Telephone calls where the interviewer indicated the purpose of the study in a clear language in order to obtain more consistent answers; guaranteed patient confidentiality, responses, and requested verbal consent from the mothers to conduct the survey.
The data were analyzed on STATA after correcting digitalization and inconsistencies. Quantitative variables were presented in percentages while qualitative variables were presented through standard deviations. A bivariate logistic regression model was conducted between EBF and each one of the possible factors that influence, reporting and OR with a 95%CI. Then, a multiple logistic regression model was conducted including significant variables (P < 0.15) and those considered clinically important. The presence of possible confounding variables was assessed.
The majority of mothers surveyed were between 19 and 35 years old (75.4%), followed by mothers older than 36 (13.1%) and the rest corresponded to those under 18 (1.1%). With regards to their homes, the majority lived in the urban area (86.9%), in comparison with 13.1% that liven the rural zone. In relation to their level of education, the majority of mothers had completed high school (27.9%), 3.6% had only attended Elementary school, 33.2% had technical or technologic studies, 24.6% had a professional degree, 10.6% had some type of graduate or post graduate degree, and only 0.2% didn’t have any type of education. Regarding parity, almost half of those interviewed had only one child (49.7%), followed by 38% who had two children, and the remaining 12.3% referred having three or more children. With regards to the mother´s harmful habits during pregnancy, only 18 (2.8%) of the mothers were found to have consumed tobacco (Table 1).
| Variable | n | % |
| Maternal age (yr) | ||
| ≤ 18 | 7 | 1.1 |
| 19-35 | 484 | 75.4 |
| ≥ 36 | 151 | 23.5 |
| Place of residence | ||
| Urban | 558 | 86.9 |
| Rural | 84 | 13.1 |
| Level of education | ||
| Elementary | 23 | 3.6 |
| High school | 179 | 27.9 |
| Technical | 147 | 22.9 |
| Technologic | 66 | 10.3 |
| Professional | 158 | 24.6 |
| Postgraduate/specialization | 68 | 10.6 |
| None | 1 | 0.2 |
| Multiparity | ||
| One | 319 | 49.7 |
| Two | 244 | 38.0 |
| Three or more | 79 | 12.3 |
| Tobacco consumption | ||
| Yes | 18 | 2.8 |
| No | 624 | 97.2 |
The report of EBF until 4 mo of age was 72% and until 6 mo 59% (Table 2). Amongst the questions asked there was one about the knowledge about the age recommended for EBF, 412 mothers (64.2%) affirmed to know about that age. Considering the definitions of the WHO and ESPGHAN, 53.7% of them affirmed that the age was up to 6 mo of life, compared to 1.2% who mentioned that was for those younger than 6 mo (Table 3).
| Duration | n | % |
| Up until 4 mo | ||
| EBF | 461 | 72 |
| Non-EBF | 179 | 28 |
| Up until 6 mo | ||
| EBF | 377 | 59 |
| Non-EBF | 263 | 41 |
| Duration | n | % |
| Younger than 6 mo | 8 | 1.2 |
| 6 mo | 345 | 53.7 |
| 7 to 12 mo | 37 | 5.8 |
| 13 to 24 mo | 17 | 2.6 |
| 36 mo | 1 | 0.2 |
| More than 36 mo | 4 | 0.6 |
| Variable | EBF for 6 mo | EBF for 4 mo | ||||
| n | % | OR (95%CI) | n | % | OR (95%CI) | |
| Univariate analysis | ||||||
| Maternal age | ||||||
| ≤ 18 yr | 16 | 4.2 | 2.2 (0.76-6.5) | 18 | 3.9 | 2.5 (0.69-9.15) |
| 19 to 35 yr | 299 | 79.3 | 0.96 (0.63-1.48) | 369 | 80 | 1.1 (0.67-1.69) |
| ≥ 36 yr | 72 | 19 | 74 | 16 | ||
| Multiparity | ||||||
| 1 child | 180 | 47.7 | 222 | 48.1 | ||
| 2 child or more | 197 | 52.2 | 1.2 (0.9-1.7) | 239 | 51.8 | 1.27 (0.9-1.8) |
| Cigarette consumption | ||||||
| Yes | 11 | 2.9 | 1.1 (0.4-2.9) | 12 | 2.6 | 0.77 (0.28-2.09) |
| No | 366 | 97 | 449 | 97.3 | ||
| Income | ||||||
| Less than 1 million | 91 | 24.1 | 101 | 21.9 | ||
| 1 to 3 million | 136 | 36 | 0.69 (0.4-1.1) | 172 | 37.3 | 0.93 (0.59-1.47) |
| More than 3 million | 116 | 30.7 | 0.77 (0.49-1.2) | 143 | 31 | 1.01 (0.63-1.63) |
| No information | 34 | 9 | 45 | 9.7 | ||
| Received help | ||||||
| Yes | 316 | 83.8 | 394 | 85.4 | ||
| No | 61 | 21.4 | 0.87 (0.56-1.36) | 67 | 14.5 | 1.28 (0.81-2.03) |
The variables analyzed were adjusted by groups of maternal age and controlled by the following confounding factors: infant assisting to day care, maternal civil status, and mother’s parity without documenting confounding effects.
A univariate and multivariate analysis was conducted finding that the presence of obstetric/ gynecologic comorbidities (OR = 0.32; 95%CI: 0.12-0.83), having mastitis (OR = 0.56; 95%CI: 0.33-0.94) and receiving information from mass communication media (OR = 0.52; 95%CI: 0.31-0.84) are factors that were associated to not achieving EBF until 4 mo of age (Tables 3-5).
| Variable | EBF for 4 mo | |
| OR | 95%CI | |
| Pathologies during pregnancy | ||
| Mastitis | 0.56 | (0.33-0.94) |
| Obstetric/gynecologic comorbidities | 0.57 | (0.3-1) |
| Medical comorbidities | 0.43 | (0.08-2.27) |
| Surgeries | 1.40 | (0.5-3.9) |
| Pathologies during BF | ||
| Mastitis | 1.17 | (0.43-3.17) |
| Obstetric/gynecologic comorbidities | 0.32 | (0.12-0.83) |
| Medical comorbidities | 1.74 | (0.64-4.65) |
| Surgeries or accidents | 0.40 | (0.07-2.32) |
| Information | ||
| Receive information at HUSI | 1.65 | (1.02-2.66) |
| Communication media | 0.52 | (0.31-0.84) |
A systematic review published in the Lancet journal in 2016 identified that WCFI institutions in which counseling was provided on BF and support about it after delivery increased adherence to EBF by 49%[6]. Maintenance of EBF until 4 mo was the main finding of the study considering that HUSI is a WCFI institution since 2013. Having received information about BF during immediate postpartum increases its maintenance by the mother since it links feeding and attachment patterns which favors their learning[7]. In this study we effectively saw how the majority of mothers (53.7%) affirmed knowing which was the age recommended by the WHO.
Another aspect to consider is the duration of the maternity leave agreed on 18 wk for Colombia (approximately 4 mo), time that matches the duration of EBF documented in the study. This coincides with one the findings of Castrillón-García et al[8] who documented that one of the main factors for abandonment of EBF is mother’s return to work.
Likewise, another finding that influences abandonment of EBF is the presence of obstetric/gynecologic complications and mastitis. This was evidenced in the study conducted in 2017 in Milan, Italy, where they documented that two factors associated to abandonment of EBF were the presence of mastitis and cracked nipples[9].
Communication media are a controverted factor since there are studies such as the one mentioned in the review of the Lancet in which these are associated with an early start of BF vs a crosscutting study conducted in Laos in 2014 that found a negative association between the promotion of dairy formulas in the local media and BF, being congruent with the findings documented in this study[6,10,11].
According to all of the above, you can see that not only factors related to the mother, but also environmental factors and society influence the duration of EBF, that is why it is important to document them in order to create strategies and improvement plans that help its maintenance.
The study showed that receiving education in a WCFI institution was the most influencing factor so that EBF was maintained until four months with a frequency higher than that reported in Colombia, and additionally, EBF was increased by 59% until 6 mo. What was found within the limitations was that when the interviewer was identified as working for the institution, the affirmative response of mothers could be induced from the information received previously. However, it is clear that when comparing the answers of mothers that reported having received information vs those that didn´t, the first group had greater adherence to the recommendation. Another limitation is that this study represents our hospital population but might not be representative of the global population since BF practices and associated factors can significantly vary between regions, cultures, and healthcare environments. Existing knowledge on the duration of EBF by mothers interviewed in the study coincides with what is presented in the 2010-2020 Ten-Year Plan assessment in which mothers from Quibdó, Leticia, Yopal, Tunja and Sincelejo were interviewed, which indicates that the information they have is clear and equivalent[5].
This study underscores the importance of the WCFI strategy for EBF maintenance. For that reason and considering that in Colombia there is a large population in rural areas, it is important to educate health professionals and staff in delivery rooms that work in the most remote areas about this strategy in order to increase adherence to and early recognition of gynecologic and obstetric complications. Additionally, this finding is useful as it opens up the possibility to conduct national studies to assess the impact of this strategy regionally, and with that, suggest applying it internationally.
The international community recognizes breastfeeding (BF) as the healthiest, most economic, and safe way of feeding a newborn and infant. Exclusive BF (EBF) of 6 mo is the desirable objective, however, supplementary feeding can be initiated earlier, depending on the nutritional needs of each child, but never in children younger than 17 wk.
Taking this context into account, the objective of the study is to document the percentages of EBF in those that were born at San Ignacio University Hospital (HUSI) and identify factors associated to their maintenance.
The Objective of this study is to document the rates of EBF in children born in HUSI (acronym in Spanish) and identify factors associated with maintenance.
Case studies and controls in a retrospective, analytical cohort were analyzed between January 2016 and January 2019 through calls to mothers of newborns at HUSI in Bogotá, Colombia.
The study showed that receiving education in a WCFI institution was the most influencing factor so that EBF was maintained until four months with a frequency higher than that reported in Colombia, and additionally, EBF was increased by 59% until 6 mo.
This study underscores the importance of WCFI strategies for EBF maintenance. Additionally, this finding is useful as it opens up the possibility of conduct national studies to assess the impact of the strategy in the region, and therefore recommends its application internationally.
Additionally, this finding is useful as it opens up the possibility to conduct national studies to assess the impact of this strategy regionally, and with that, suggest applying it internationally.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Pediatrics
Country/Territory of origin: Colombia
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Choudhary RK, India S-Editor: Zhang H L-Editor: A P-Editor: Zhang XD
| 1. | Agostoni C, Decsi T, Fewtrell M, Goulet O, Kolacek S, Koletzko B, Michaelsen KF, Moreno L, Puntis J, Rigo J, Shamir R, Szajewska H, Turck D, van Goudoever J; ESPGHAN Committee on Nutrition. Complementary feeding: a commentary by the ESPGHAN Committee on Nutrition. J Pediatr Gastroenterol Nutr. 2008;46:99-110. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 654] [Cited by in RCA: 577] [Article Influence: 33.9] [Reference Citation Analysis (0)] |
| 2. | Seghnp-Aep S. Protocolos diagnóstico-terapéuticos de Gastroenterología, Hepatología y Nutrición Pediátrica. 2nd ed. España: Ergón S.A, 2010. |
| 3. | Eglash A, Montgomery A, Wood J. Breastfeeding. Dis Mon. 2008;54:343-411. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 23] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 4. | Ministerio de Salud y Protección Social. Encuesta Nacional de la Situación Nutricional ENSIN 2015. 1st ed. Colombia, 2015. |
| 5. | Ministerio de Salud de Colombia. Evaluación de Proceso Plan Decenal de Lactancia Materna 2010-2020 Convenio 519 de 2015. Colombia, 2016: 128-132. |
| 6. | Rollins NC, Bhandari N, Hajeebhoy N, Horton S, Lutter CK, Martines JC, Piwoz EG, Richter LM, Victora CG; Lancet Breastfeeding Series Group. Why invest, and what it will take to improve breastfeeding practices? Lancet. 2016;387:491-504. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1135] [Cited by in RCA: 1344] [Article Influence: 149.3] [Reference Citation Analysis (0)] |
| 7. | Shifraw T, Worku A, Berhane Y. Factors associated exclusive breastfeeding practices of urban women in Addis Ababa public health centers, Ethiopia: a cross sectional study. Int Breastfeed J. 2015;10:22. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 49] [Cited by in RCA: 49] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 8. | Castrillón JJC, Cardona AAG, Corrales SV, Meneses JDV. Razones de abandono de la lactancia materna en madres de niños de jardines infantiles. Arch Med. 2015;17:369-378. [DOI] [Full Text] |
| 9. | Colombo L, Crippa BL, Consonni D, Bettinelli ME, Agosti V, Mangino G, Bezze EN, Mauri PA, Zanotta L, Roggero P, Plevani L, Bertoli D, Giannì ML, Mosca F. Breastfeeding Determinants in Healthy Term Newborns. Nutrients. 2018;10. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 65] [Cited by in RCA: 95] [Article Influence: 13.6] [Reference Citation Analysis (0)] |
| 10. | Phoutthakeo P, Otsuka K, Ito C, Sayamoungkhoun P, Kounnavong S, Jimba M. Cross-border promotion of formula milk in Lao People's Democratic Republic. J Paediatr Child Health. 2014;50:51-56. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 13] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 11. | Haiden N, Ziegler EE. Human Milk Banking. Ann Nutr Metab. 2016;69 Suppl 2:8-15. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 76] [Article Influence: 9.5] [Reference Citation Analysis (0)] |