Published online Dec 9, 2023. doi: 10.5409/wjcp.v12.i5.331
Peer-review started: June 25, 2023
First decision: August 17, 2023
Revised: September 4, 2023
Accepted: October 30, 2023
Article in press: October 30, 2023
Published online: December 9, 2023
Processing time: 165 Days and 17.9 Hours
Intra-gastric migration of the distal ventriculoperitoneal shunt (VPS) catheter clinically presenting with or without trans-oral extrusion is one of the rare complications of VPS catheter insertion.
To identify the demographics, clinical presentation, clinical findings, and results of surgical therapy offered for the treatment of intra-gastric migration of the distal VPS catheter, clinically presented with or without trans-oral extrusion.
An online search was performed for the extraction/retrieval of the published/ available literature pertaining to the above-mentioned VPS complication. Manuscripts were searched from PubMed, PMC (PubMed Central), ResearchGate, and Google Scholar databases using various terminology relating to the VPS complications. The first case of migration of a VPS catheter into the stomach was reported in the year 1980, and the data were retrieved from 1980 to December 2022. Cases were categorized into two groups; Group A: Cases who had migration of the distal VPS catheter into the stomach and clinically presented with trans-oral extrusion of the same, and Group B: Cases who had migration of the distal VPS catheter into the stomach, but presented without trans-oral extrusion.
A total of n = 46 cases (n = 27; 58.69% male, and n = 19; 41.3% females) were recruited for the systematic review. Group A included n = 32, and Group B n = 14 cases. Congenital hydrocephalus was the indication for the primary VPS insertion for approximately half of the (n = 22) cases. Approximately sixty percent (n = 27) of them were children ≤ 5 years of age at the time of the diagnosis of the complication mentioned above. In seventy-two percent (n = 33) cases, this complication was detected within 24 mo after the VPS insertion/last shunt revision. Clinical diagnosis was evident for the entire group A cases. Various diagnostic modalities were used to confirm the diagnosis for Group B cases. Various surgical procedures were offered for the management of the complication in n = 43 cases of both Groups. In two instances, intra-gastric migration of the distal VPS catheter was detected during the autopsy. This review documented four deaths.
Intra-gastric migration of the peritoneal end of a VPS catheter is one of the rare complications of VPS catheter implantation done for the treatment of hydrocephalus across all age groups. It was more frequently reported in children, although also reported in adults and older people. A very high degree of clinical suspicion is required for the diagnosis of a case of an intra-gastric migration of the distal VPS catheter clinically presenting without trans-oral extrusion.
Core Tip: This systematic review included n = 46 cases of intra-gastric migration of the peritoneal end of a ventriculoperitoneal shunt (VPS) catheter. Thirty-two cases clinically presented with the peroral extrusion of the distal VPS catheter. The remaining n = 14 cases clinically presented with other symptoms but without peroral extrusion of the distal VPS catheter. Sixty percent were children ≤ 5 years of age at the time of diagnosis of VPS complication mentioned above. In more than two-thirds of cases, the VPS complication was evident within 24 mo after the primary VPS insertion/last VPS revision. The demographics, indications for the primary/initial VPS insertion, age distribution at the time of VPS insertion and diagnosis of the VPS complication, the interval, and the surgical procedures carried out by the various authors for the above-described VPS complication are described in the manuscript.
- Citation: Ghritlaharey RK. Migration of the distal ventriculoperitoneal shunt catheter into the stomach with or without trans-oral extrusion: A systematic literature review and meta-analysis. World J Clin Pediatr 2023; 12(5): 331-349
- URL: https://www.wjgnet.com/2219-2808/full/v12/i5/331.htm
- DOI: https://dx.doi.org/10.5409/wjcp.v12.i5.331
The treatment of hydrocephalus has evolved over centuries, but progress has occurred during the past few decades[1,2]. The ventriculoperitoneal shunt insertion is the commonly performed surgical procedure for treating hydrocephalus caused by various etiologies and is performed across all age groups[3-7]. Various complications occur in approximately one-fifth to four-fifths of the cases following the VPS insertion, and many of them require shunt revisions[5-9]. VPS revisions are needed more during the first 12 mo following the initial VPS placement[5,6,8]. VPS complications and shunt revisions are more frequently documented and required in children than adults[5,8]. Perforation of the hollow viscus viz gastrointestinal tract, urinary bladder, and uterus (female genital tract) by the peritoneal end of a VPS catheter is known, and it may occur with or without extrusion of the distal VPS catheter through the natural orifices[10-14]. Perforation of the large bowel by the peritoneal end of a VPS catheter and protrusion/extrusion of the same via the anal canal is commonly reported[10,11]. Migration of the distal VPS catheter into the stomach is a rare clinical entity[14]. The preferred reporting items for systematic reviews and metaanalyses (PRISMA) guidelines are followed for reporting this manuscript[15,16]. This manuscript is a systematic literature review of the n = 46 cases published (1980 to December 2022) on the management of the intra-gastric migration of the distal VPS catheter clinically presented with or without trans-oral extrusion[17-62]. Thirty-two cases had intra-gastric migration of the distal VPS catheter and clinically presented with trans-oral extrusion of the same[17-48]. Remaining n = 14 cases had intra-gastric migration of the distal VPS catheter but clinically presented without trans-oral extrusion of the distal VPS catheter[49-62].
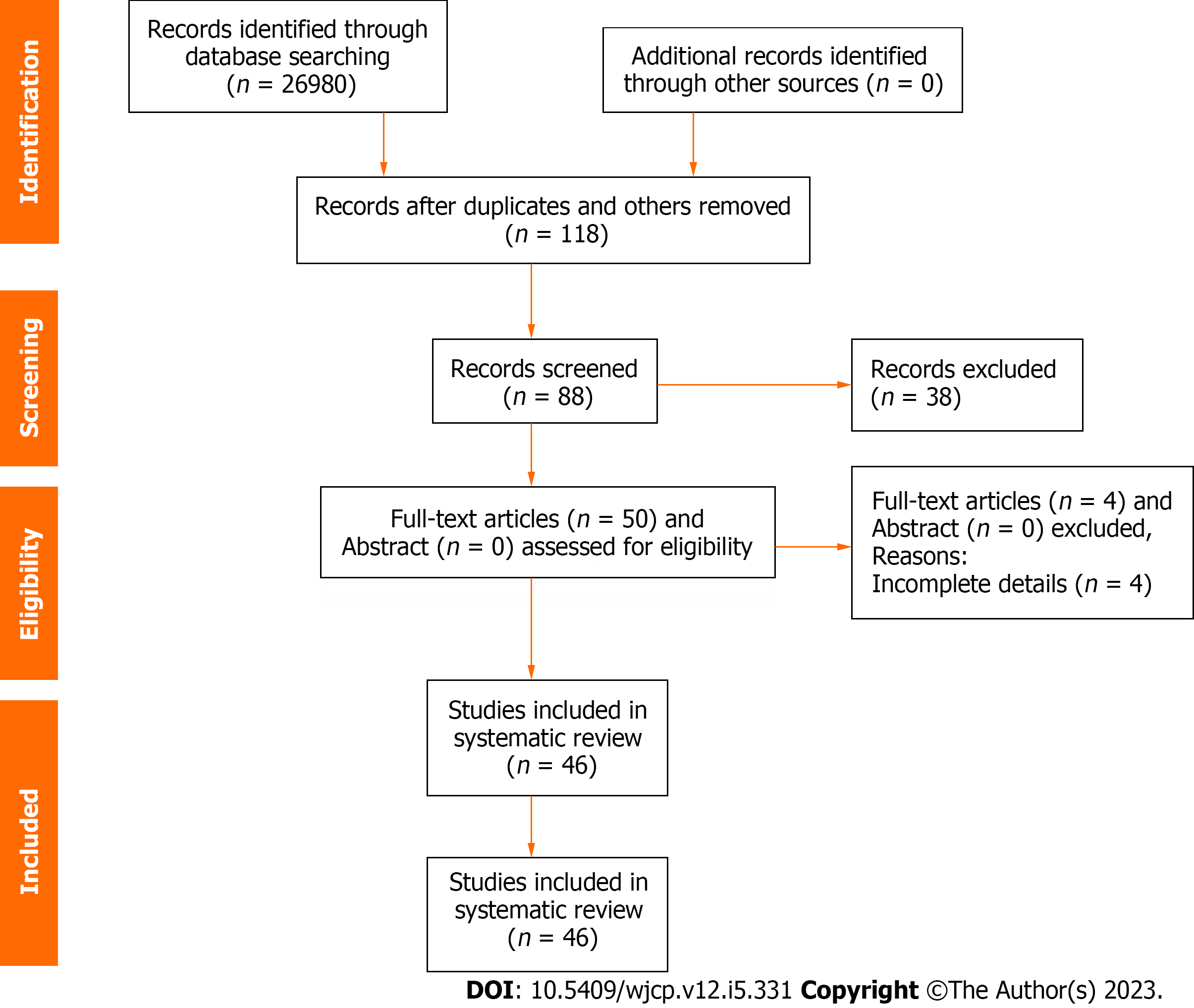
PubMed, PMC, ResearchGate, and Google Scholar databases were searched for retrieval of the published/available literature pertaining to the migration of the distal VPS catheter into the stomach with or without trans-oral extrusion. Various terminology relating to VPS complications were utilized during the online search. Some of the keywords employed during the online search were “trans-oral extrusion of distal VPS catheter”, “per-oral/oral extrusion of distal VPS catheter”, “intra-gastric migration of distal VPS catheter”, “protrusion/extrusion of VPS catheter”, “bowel perforation by distal VPS catheter”, and “rare complication of VPS catheter”. The maiden case of migration of a VPS catheter into the stomach was reported by Nishijima et al[49] in 1980, and related literature/manuscripts were retrieved from 1980 to December 2022, and those were preferably available in the English language. Four cases (n = 2 duodenal and n = 2 jejunal) of bowel perforation (not gastric perforation) by the distal VPS catheter, clinically presented with trans-oral extrusion were also included in the present review. Cases/case reports retrieved during online search with incomplete details were excluded from the review. Cases are categorized into two groups, Groups A and Group B. Group A: Cases who had migration of the distal VPS catheter into the stomach and clinically presented with trans-oral extrusion of the same, and Group B: Cases who had migration of the distal VPS catheter into the stomach but clinically presented without trans-oral extrusion. The “Preferred Reporting Items for Systematic Reviews and MetaAnalyses” (PRISMA) guidelines are followed for reporting this systematic review. The selection of articles for systematic review was done by assessing the titles, abstracts, and full texts of the manuscripts. Literature selection and extraction of the desired information from the manuscripts were independently carried out by the author alone, as this is a single-author manuscript. The desired information retrieved from the published literature/case reports were the patient’s age, sex, indication for the VPS insertion, interval from VPS insertion to the diagnosis of the complication, clinical characteristics, diagnostic modalities used, surgical procedures offered/performed, postoperative complications, and the outcome of surgical therapy. This manuscript is a systematic review of the published cases, and institutional ethical committee approval is not required.
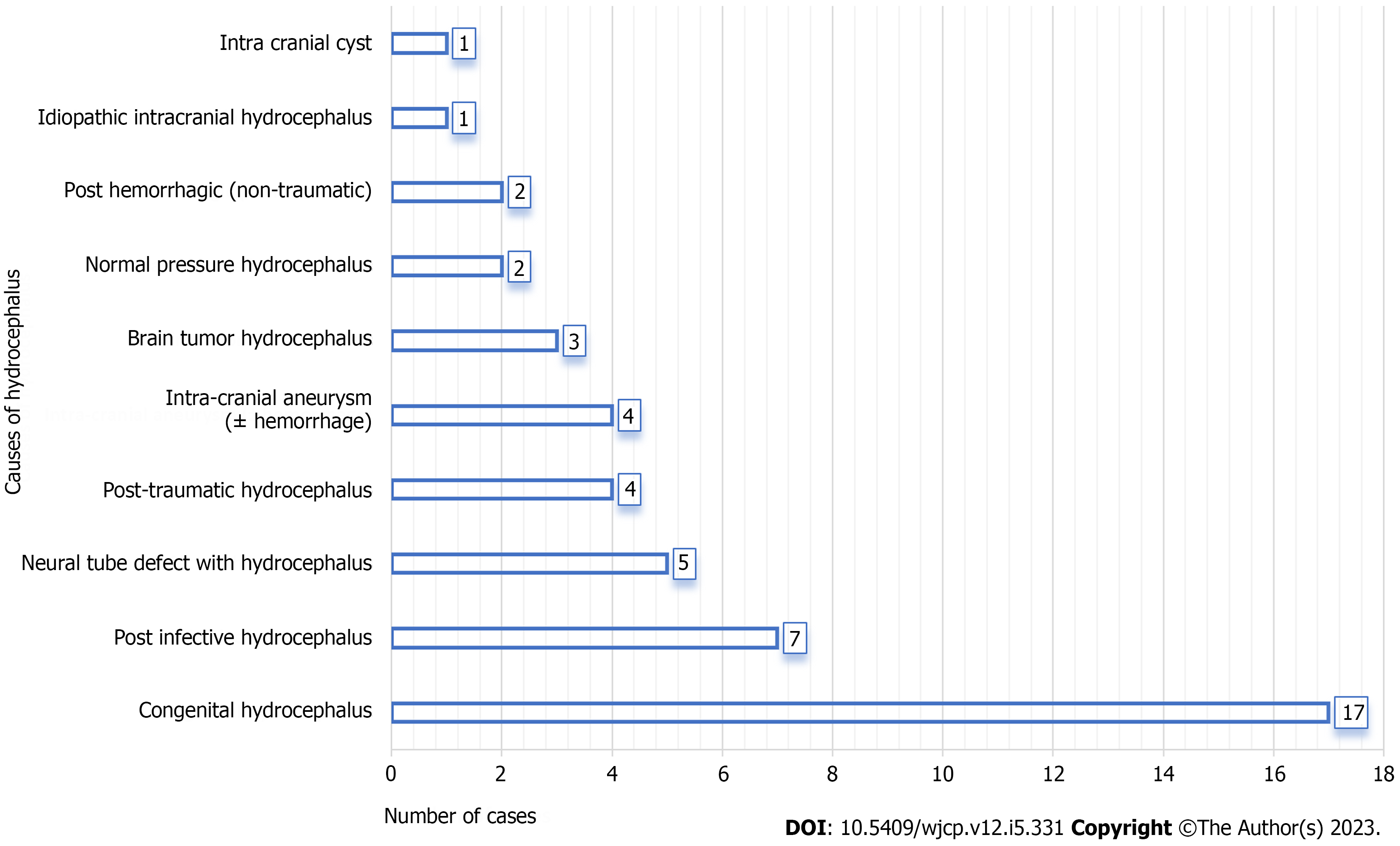
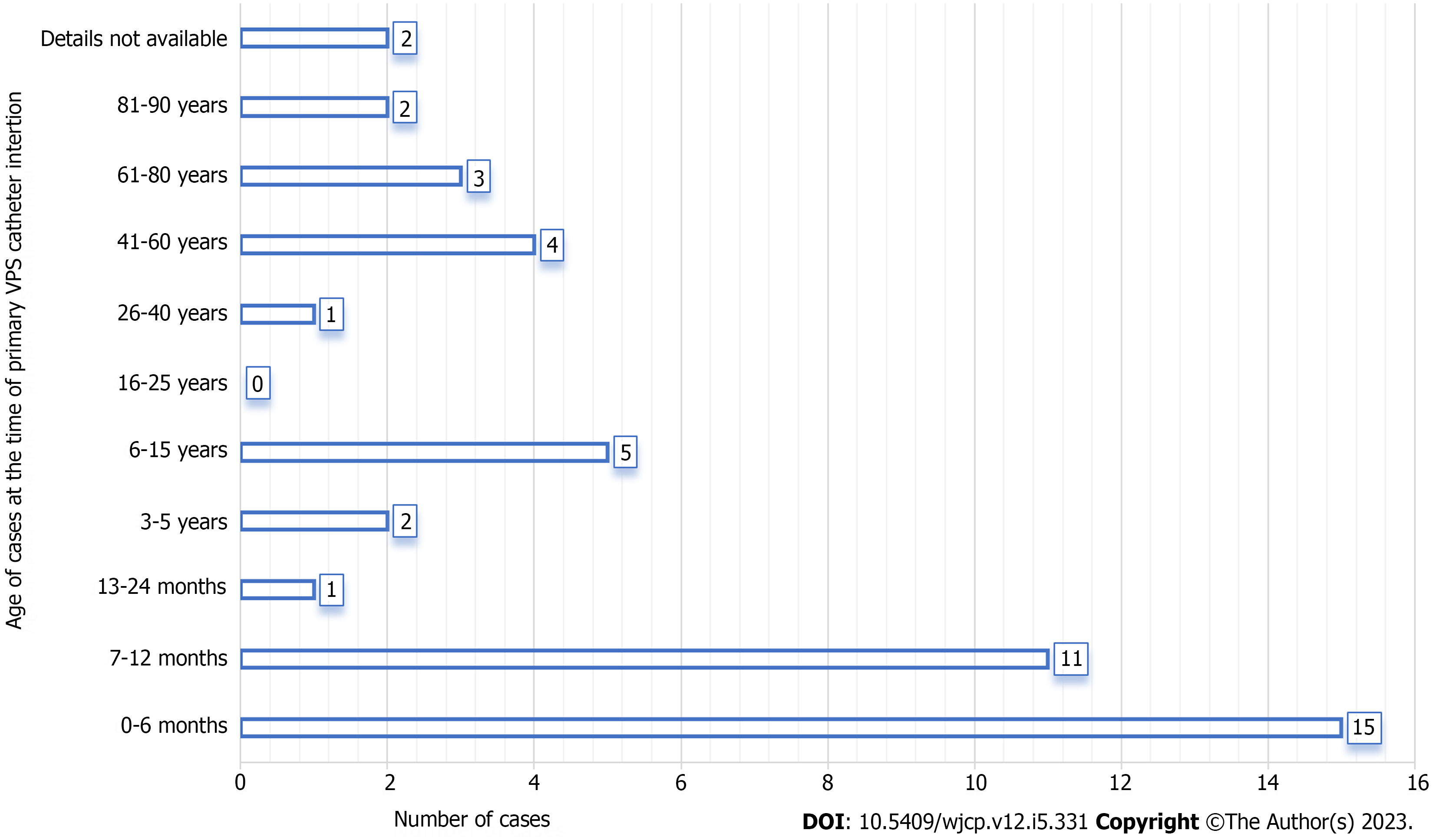
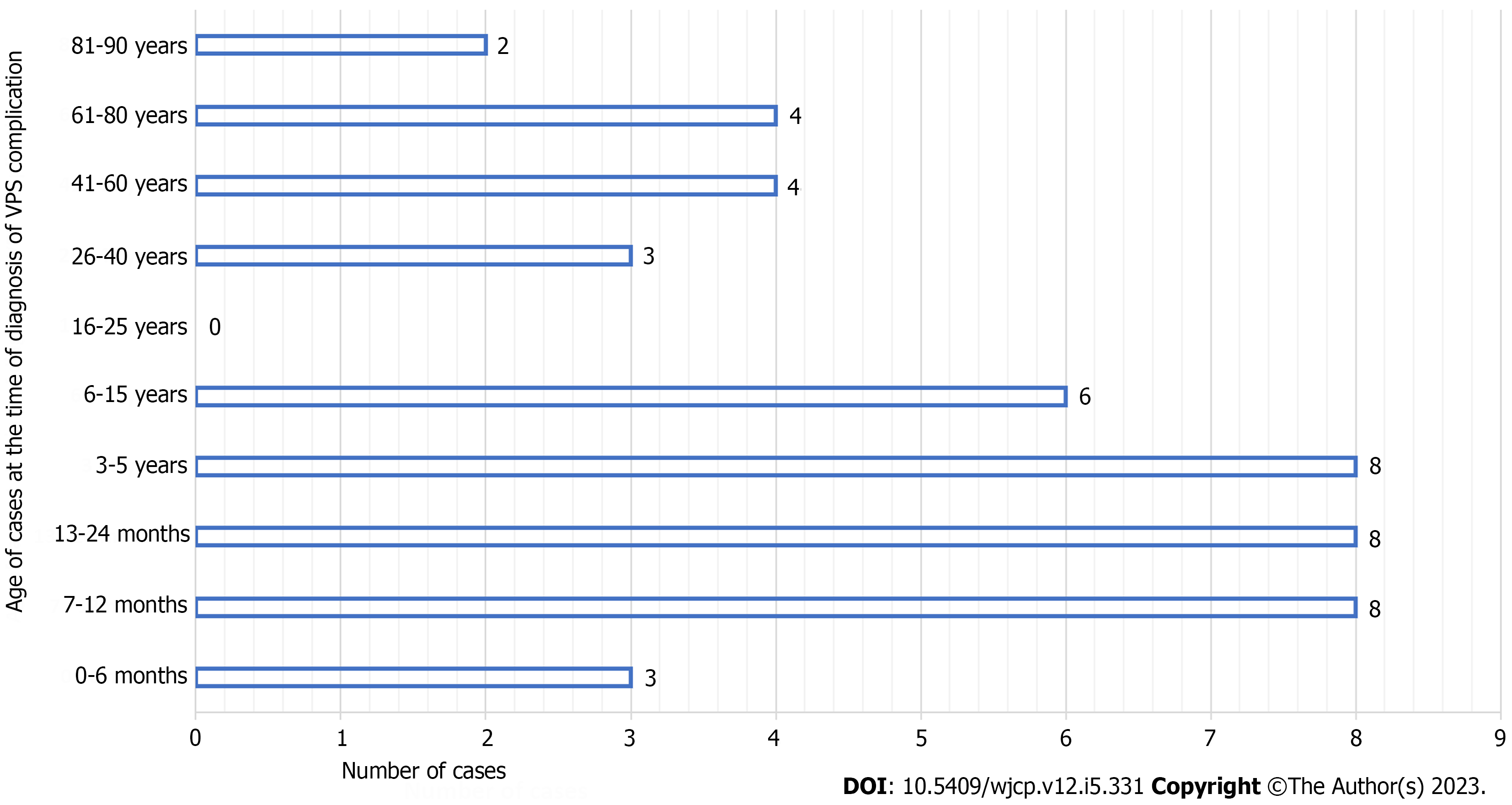
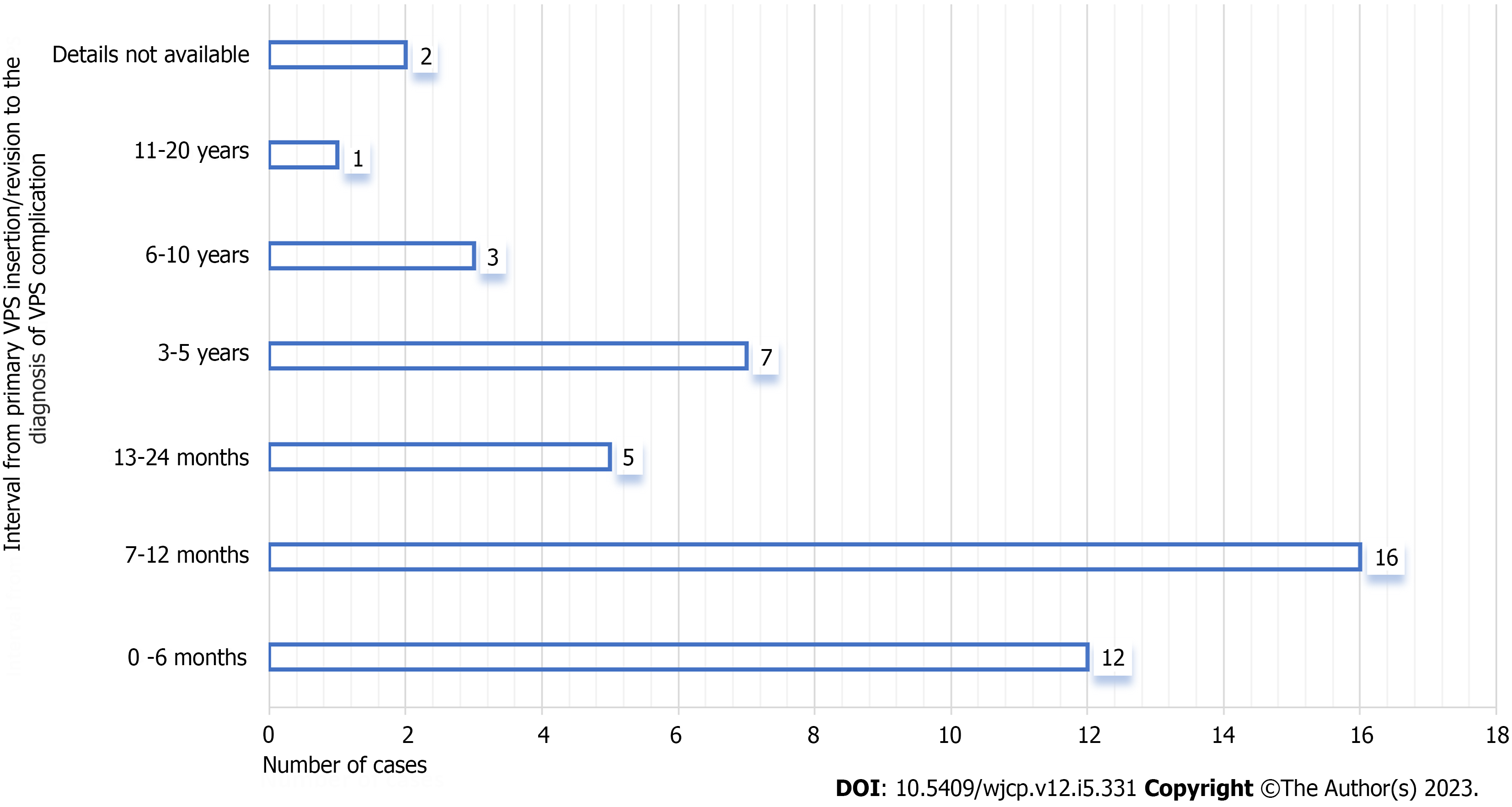
A total of n = 46 cases of intra-gastric migration of the peritoneal end of a VPS catheter clinically presented with or without peroral extrusion were included for the systematic review and retrieved from the n = 46 manuscripts. The process of database search, screening, and selection of the manuscripts for the present systematic review is presented in a PRISMA flow diagram in Figure 1. Group A included n = 32 cases and details are provided in Table 1. Group B included n = 14 cases and details are provided in Table 2. The causes of hydrocephalus and indications for the primary VPS insertion for the entire case are detailed in Figure 2. Congenital hydrocephalus was the indication for the primary VPS insertion for approximately half of the (n = 22) cases. Figure 3 detailed the distribution of the age of the entire cases at the time of primary VPS insertion. The initial VPS catheter placement was done during infancy in two-thirds (n = 22) of Group A cases. The initial VPS catheter placement was done during infancy only in one-fourth (n = 4) of Group B cases. Figure 4 details the distribution of the age of the entire cases at the time of diagnosis of the above-mentioned VPS complication. Approximately sixty percent (n = 27) of them were children ≤ 5 years of age at the time of diagnosis of the complication mentioned above. Figure 5 details the interval from the primary/initial VPS insertion/last VPS revision to the diagnosis of the VPS complication mentioned above. In seventy-two percent (n = 33) cases, this complication was detected within 24 mo after the VPS insertion/last shunt revision.
| Ref. | Indication for VPS insertion | Age VPS insertion sex | Age trans-oral extrusion | Interval (mo) | VPS (R) | History GI Surg | Shunt tract infection | Peritonitis meningitis | CSF infection | Operative procedures executed | 1Site repaired (Yes/No) | Complication | Outcome |
| Griffith et al[17], 1987 | Hydrocephalus (Post infective) | 9.6 yr Female | 9.9 yr | 3 | Yes | Yes | No | No | No | Part of distal VPS catheter cut by child, proximal VPS catheter as EVD, delayed ventriculo-atrial shunt done | Stomach (No) | Yes | Death |
| Danismend et al[18], 1988 | Hydrocephalus (Congenital?) | 8 mo Female | 18 mo | 10 | No | No | No | No | No | Removal of distal VPS catheter and Immediate ventriculo-atrial shunt done | Stomach (Yes) | Nil | R |
| Park et al[19], 2000 | Hydrocephalus | 12 mo female | 5 yr | 48 | No | No | Yes | No | No | Removal of part of distal VPS catheter, Proximal VPS catheter as EVD, Delayed re-VPS/VPS (R) done | Stomach (No) | Nil | R |
| (Post-haemorrhagic) | |||||||||||||
| Jiménez Moya et al[20], 2001 | Hydrocephalus (Brain tumor) | 9.11 yr female | 11.2 yr | 2 | Yes | Yes | No | No | No | Removal of entire VPS catheter, Delayed re-VPS insertion done | Stomach (NA) | Nil | R |
| Kothari et al[21], 2006 | Hydrocephalus (Congenital) | 1 mo male | 18 mo | 17 | No | No | No | No | Yes | Removal of entire VPS catheter, Delayed re-VPS insertion done | Stomach? (No) | Nil | R |
| Odebode et al[22], 2007 | Hydrocephalus (Congenital?) | 9 mo female | 15 mo | 6 | No | No | Yes | No | No | Removal of entire VPS catheter, Delayed re-VPS insertion done | Jejunum (Yes) | Nil | R |
| Berhouma et al[23], 2008 | Hydrocephalus with NTD (Congenital) | 9 mo male | 2 yr | 15 | No | No | No | No | Yes | Removal of part of distal VPS catheter, Proximal VPS catheter as EVD | NA (No) | Yes | Death |
| Murali et al[24], 2008 | Hydrocephalus (Congenital) | 6 mo male | 6 yr | 66 | No | No | No | No | No | Removal of part of distal VPS catheter, Proximal VPS catheter as EVD, Removal of cranial catheter failed | Stomach (No) | Nil | R |
| Sridhar et al[25], 2009 | Hydrocephalus (Post infective) | 2 mo female | 8 mo | 6 | No | No | No | No | No | Removal of entire VPS catheter (re-VPS catheter insertion not required) | Stomach? (No) | Nil | R |
| Sinnadurai et al[26], 2009 | Hydrocephalus (Cyst) | 12 yr female | 27 yr | 2 wk | Yes | No | No | No | No | Removal of part of distal VPS catheter, Proximal VPS catheter as EVD, Delayed VPS (R) done | Stomach (No) | Nil | R |
| Low et al[27], 2010 | Hydrocephalus (Post infective) | 6 mo male | 12 mo | 6 | No | Yes | No | No | No | Removal of entire VPS catheter, Insertion of EVD, Delayed re-VPS insertion done | Stomach (No) | Nil | R |
| Dua et al[28], 2011 | Hydrocephalus with NTD (Congenital) | 20 d male | 8 mo | 7 | No | No | No | No | No | Removal of part of distal VPS catheter, Proximal VPS catheter as EVD, Delayed re-VPS insertion done | Stomach (No) | Nil | R |
| Agarwal et al[29], 2011 | Hydrocephalus (Congenital) | 4 mo male | 12 mo | 8 | No | No | No | No | No | Removal of entire VPS catheter, Delayed re-VPS insertion done | NA (No) | Nil | R |
| Gupta et al[30], 2012 | Hydrocephalus (Congenital) | 6 mo male | 4 yr | 42 | No | No | No | No | No | Removal of entire VPS catheter (re-VPS insertion not required) | Stomach (No) | Nil | R |
| Kundal et al[31], 2012 | Hydrocephalus (Post infective) | 6 yr male | 7 yr | 12 | No | No | No | No | No | Removal of entire VPS catheter, Delayed re-VPS insertion done | NA (No) | Nil | R |
| Yilmaz et al[32], 2013 | Hydrocephalus (Pseudotumor) | 37 yr female | 47 yr | 120 | No | Yes | No | No | No | Removal of entire VPS catheter (re-VPS insertion not required) | Stomach (Yes) | Nil | R |
| Gupta et al[33], 2014 | Hydrocephalus (Congenital) | 12 mo male | 11 yr | 7 | Yes | No | No | No | No | Removal of entire VPS catheter (Previous VPS functioning well) | Stomach (No) | Nil | R |
| Mandhan et al[34], 2015 | Hydrocephalus with NTD (Congenital) | Infant female | 11 yr | 53 | No | Yes | No | No | No | Removal of entire VPS catheter (re-VPS insertion not done/required?) | Stomach (No) | Nil | R |
| Thiong’o et al[35], 2015 | Hydrocephalus (Congenital) | 10 d female | 3 mo | 2 | No | No | No | No | No | Removal of entire VPS catheter, Insertion of EVD, Delayed re-VPS insertion done | Stomach? (No) | Nil | R |
| Sohal et al[36], 2015 | Hydrocephalus (Congenital?) | NA male | 11 mo | 10 d | Yes | Yes | No | No | No | Removal of part of distal VPS catheter, Proximal VPS catheter as EVD, Delayed ventriculo-atrial shunt done | Stomach (No) | Nil | R |
| Ghritlaharey et al[37], 2015 | Hydrocephalus (Post infective/Congenital) | 12 mo female | 24 mo | 9 | Yes | No | No | No | No | Removal of part of distal VPS catheter, Proximal VPS catheter as EVD, Delayed VPS (R) done | Stomach? (No) | Yes | R |
| Shahet al[38], 2016 | Hydrocephalus (Congenital) | 12 mo male | 4 yr | 12 | Yes | No | No | No | No | Removal of entire VPS catheter (re-VPS insertion not required) | Stomach (No) | Nil | R |
| Sharmaet al[39], 2017 | Hydrocephalus (Congenital) | Neonate male | 8 mo | 7 | No | No | No | No | No | Removal and re-positioning of distal VPS catheter into the peritoneal cavity | Stomach (No) | Nil | R |
| Al Fauzi Aet al[40], 2017 | Hydrocephalus (Brain tumor) | 4 yr male | 5 yr | 12 | No | No | No | No | No | Removal of entire VPS catheter (re-VPS insertion not required) | Stomach (No) | Nil | R |
| Reyeset al[41], 2017 | Hydrocephalus (Post-haemorrhagic) | 2 mo male | 16 mo | 8 | Yes | No | No | No | No | Removal of entire VPS catheter, Immediate re-VPS insertion done | Stomach (No) | Nil | R |
| Badriet al[42], 2018 | Hydrocephalus (Congenital) | 4 yr male | 4 yr | 1 | No | No | No | No | No | Removal of distal VPS catheter, Immediate VPS (R) done | Duodenum (Yes) | Nil | R |
| Romualdet al[43], 2018 | Hydrocephalus (Congenital) | 24 mo male | 34 mo | 10 | No | No | No | No | Yes | Removal of entire VPS catheter, Insertion of EVD, Delayed re-VPS insertion done | Duodenum (Yes) | Nil | R |
| Ezzatet al[44], 2018 | Hydrocephalus (Congenital) | 2 mo male | 22 mo | 20 | No | No | No | No | No | Removal of entire VPS catheter, Cranial catheter as EVD? Delayed re-VPS insertion done | Stomach? (No) | Nil | R |
| Bemoraet al[45], 2019 | Hydrocephalus (Post infective) | 7 mo female | 16 mo | 9 | No | No | No | No | NA | Removal of entire VPS catheter, Immediate re-VPS insertion done | Stomach (No?) | Nil | R |
| Feeneyet al[46], 2020 | Hydrocephalus (Post trauma) | 57 yr male | 58 yr | 11 | No | No | No | No | Yes | Removal of distal VPS catheter, Proximal VPS catheter as EVD, Removal of proximal VPS catheter (re-VPS insertion not required) | Jejunum (No) | Nil | R |
| Calgaroet al[47], 2020 | Hydrocephalus (Congenital) | 2 mo male | 7 mo | 5 | No | No | No | No | NA | Removal of entire VPS catheter, Immediate re-VPS insertion done | Stomach? (No) | Nil | R? |
| Najibet al[48], 2022 | Hydrocephalus with NTD (Congenital) | Neonate male | 8 mo | 7 | No | No | No | No | No | Removal of part of distal VPS catheter and re-positioning of remaining distal catheter into the peritoneal cavity | Stomach (Yes) | Nil | R |
| Ref. | Indication for VPS insertion | Age VPS insertion sex | Age gastric migration | Interval (mo) | VPS (R) | History GI Surg | Shunt tract infection | Peritonitis meningitis | CSF infection | Operative procedures executed | 1Site repaired (Yes/No) | Complication | Outcome |
| Nishijima et al[49], 1980 | Hydrocephalus (NPH) | 69 yr female | 71 yr | 27 | No | No | No | Meningitis | Yes | Distal VPS catheter found within the gastric lumen (Autopsy finding) | Stomach (Autopsy) | - | Death |
| Oi et al[50], 1987 | Hydrocephalus (posttraumatic) | 12 mo male | 3 yr | 24 | Yes | No | Yes | Meningitis | Yes | Removal of part of distal VPS catheter, Proximal VPS catheter as EVD, Delayed VPS revision done | Stomach (Glue) | Nil | R |
| Oshio et al[51], 1991 | Hydrocephalus (Posttraumatic) | 12 mo male | 3 yr | 24 | No | No | Yes | Meningitis | Yes | Removal of part of distal VPS catheter, Proximal VPS catheter as EVD?, Delayed VPS revision done | Stomach (Glue) | Yes | R |
| Ho et al[52], 1992 | Hydrocephalus (NPH) | 68 yr male | 72 yr | 42 | No | No | No | Meningitis | Yes | Distal VPS catheter found within the gastric lumen (Autopsy finding) | Stomach (Autopsy) | - | Death |
| Alonso-Vanegas et al[53], 1994 | Hydrocephalus with NTD (Congenital) | Neonate female | 4 mo | 4 | No | No | No | No | No | Removal of entire VPS catheter, Immediate ventriculo-atrial shunt | Stomach (Yes) | Nil | R |
| Christoph et al[54], 1995 | Hydrocephalus (Congenital) | 5 mo female | 5 mo | 1 d | No | Yes | No | No | No | Removal of distal VPS catheter from gastric lumen and converted as EVD, Delayed ventriculo-atrial shunt done | Stomach (NA) | Nil | R |
| Hart et al[55], 2001 | Hydrocephalus (Congenital) | NA female | 33 yr | NA | NA | No | No | No | No | Removal of distal VPS catheter from gastric lumen and relocation of distal catheter within the peritoneal cavity | Stomach (NA) | Nil | R |
| Masuoka et al[56], 2005 | Hydrocephalus (Intracranial aneurysm) | 47 yr male | 51 yr | 42 | No | No | No | No | Yes | Removal of entire VPS catheter (re-VPS insertion not required) | Stomach (No) | Nil | R |
| Cheng et al[57], 2007 | Hydrocephalus (Posttraumatic) | 87 yr male | 88 yr | 8 | No | No | No | No | Yes | Removal of entire VPS catheter (re-VPS insertion not done/required) | Stomach (Yes) | Nil | R |
| Cohen-Added et al[58], 2018 | Hydrocephalus (Intracranial aneurysm) | 65 yr male | 72 yr | 7 yr? | No | No | No | No | No | Surgical therapy not executed for intra-gastric migration of distal VPS catheter | Stomach (No) | -- | R |
| Sidhu et al[59], 2019 | Hydrocephalus (Intracranial aneurysm) | 83 yr? male | 84 yr | 12? | No | Yes | No | No | No | Removal of entire VPS catheter (re-VPS insertion not required) | Stomach (NA) | Nil | R |
| Yala et al[60], 2019 | Hydrocephalus (Intracranial aneurysm) | 41 yr female | 65 yr | 36? | Yes | No | No | No | No | Removal of distal VPS catheter from gastric lumen and relocation of distal catheter within the peritoneal cavity | Stomach (Yes) | Nil | R |
| Chen et al[61], 2020 | Hydrocephalus (Post infective) | 44 yr female | 54 yr | NA | Yes | No | No | No | Yes | Removal of entire VPS catheter, Placement of EVD, Delayed re-VPS insertion done | Stomach (Yes) | Nil | R |
| Scarascia et al[62], 2022 | Hydrocephalus (IIH) | 15 yr female | 31 yr | 16 yr? | No | No | No | No | No | Removal of entire VPS catheter (re-VPS insertion not done) | Stomach (Yes) | Yes | R? |
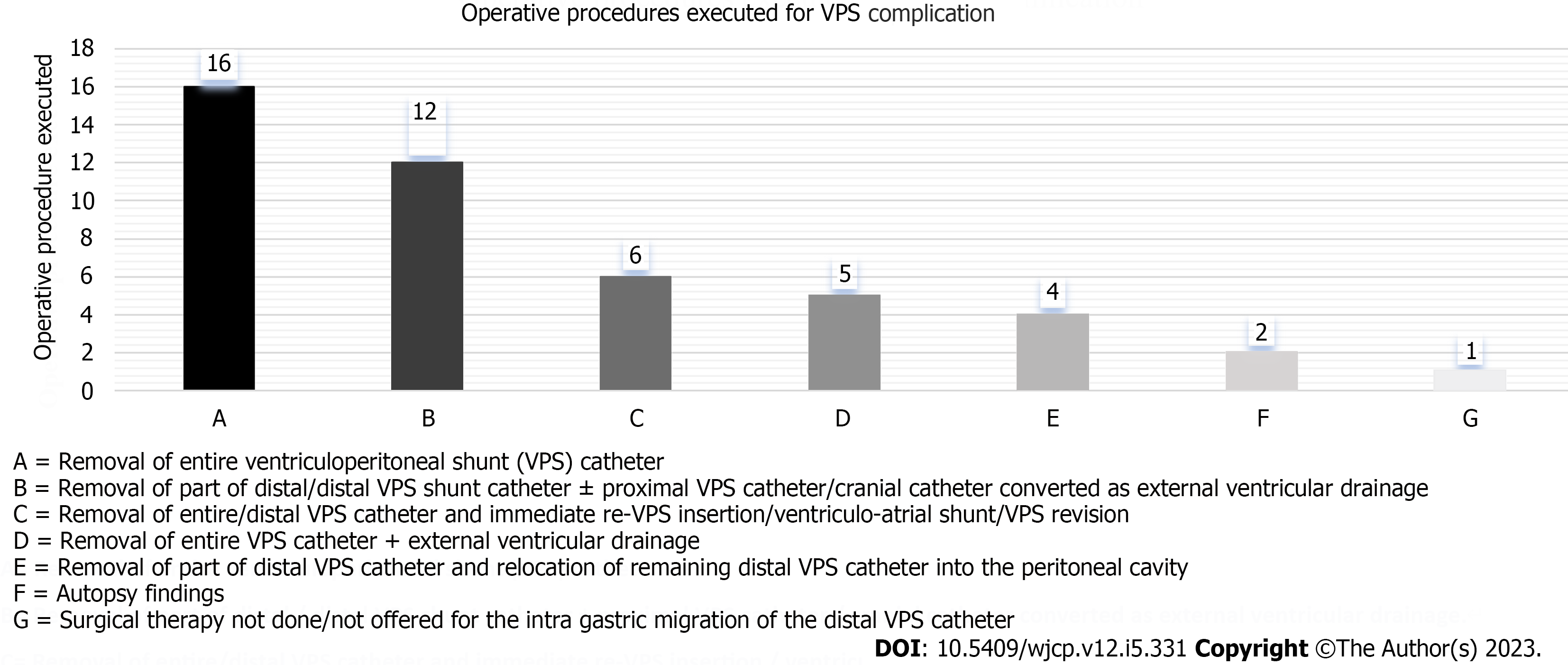
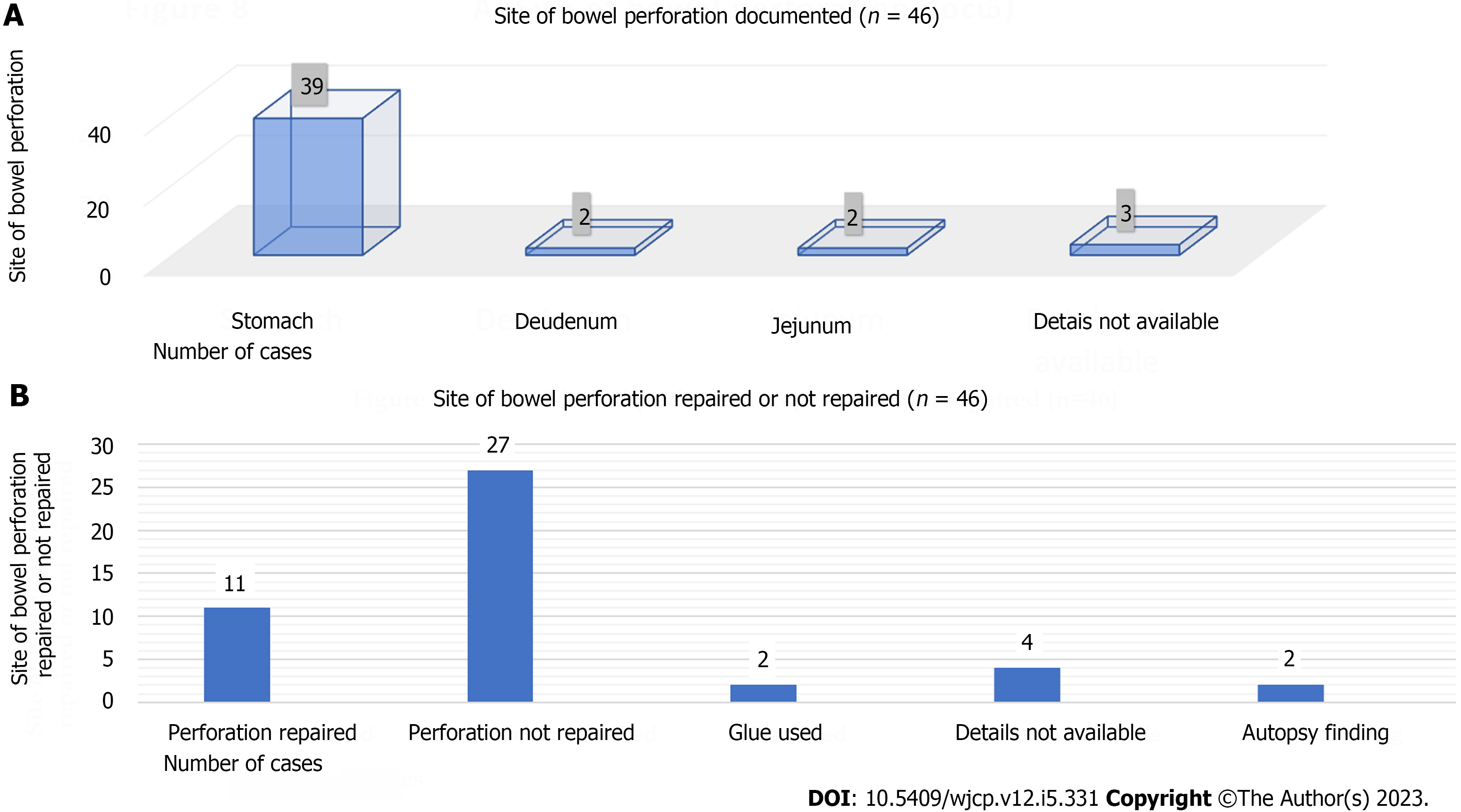
The chief complaint and clinical finding for Group A cases was the trans-oral extrusion of the distal VPS catheter (Figure 6). In most cases, it was associated with a bout of vomiting of short duration. Mild abdominal pain/discomfort relating to the upper gastrointestinal (GI) tract was also documented in some cases. Clinical presentation in Group B cases was vague and not specific to the distal VPS catheter complication. Group B cases mostly had symptoms relating to the central nervous system (CNS) or upper GI tract. Clinical diagnosis was evident in the entire Group A cases due to the clinical finding of the presence of trans-oral extrusion/protrusion of the distal VPS catheter. Various diagnostic modalities (radiological and endoscopic) were used to confirm the diagnosis in Group B cases. Different surgical procedures were offered for the management of the above-mentioned VPS complication and are detailed in Figure 7. Removal of the entire VPS catheter/removal of part of the peritoneal /peritoneal catheter with or without external ventricular drainage (EVD) was preferred by the authors. In n = 2 Group B cases, an intra-gastric migration of the distal VPS catheter was detected during the autopsy. For one Group B case, the surgical therapy was not carried out, as his VPS catheter was not causing any problems. Percutaneous surgical removal of the entire or the distal VPS catheter with or without an EVD was a procedure of choice and was opted for n = 27 (n = 24 Group A and n = 3 Group B) cases. For the management of VPS complications mentioned above, formal laparotomy was carried out only in n = 11 (n = 7 Group A and n = 4 Group B) cases. The site of bowel perforation caused by the distal VPS catheter is detailed in (Figure 8A). In eighty-five percent of cases, the site of bowel perforation was the stomach. The site of bowel perforation was repaired only in n = 11 cases and is detailed in (Figure 8B). The review revealed n = 4 (8.69%) deaths, two from each group.
Perforation of the gastrointestinal tract, urinary bladder, and uterus by the distal VPS catheter is a known complication of the VPS placement carried out for the treatment of hydrocephalus, and most of them clinically present with the extrusion of the peritoneal part of a VPS catheter through the natural orifices[10-14]. Perforation of the large bowel by the peritoneal end of a VPS catheter and extrusion of the same via the anal canal is most common and is reported to occur in 0.1% to 2.5% of the cases[10,11]. Migration of the distal VPS catheter into the stomach is a rare clinical entity, and two-thirds of them presented with the trans-oral extrusion of the distal part of peritoneal catheter[17-62].
A total of n = 46 manuscripts including n = 46 cases of the above-mentioned VPS complication were reviewed for systematic review[17-62]. Forty-four manuscripts are published in the English language[17-19,21-40,42-62]. Only n = 2 manuscripts published and available in languages other than English are also included in the review. For the above two manuscripts, the desired details are obtained by translating them into the English language using Google Translate[20,41]. All the n = 46 manuscripts included in the review are already published, and none are conference proceedings or unpublished. All the n = 46 manuscripts included for systematic review are full-text articles[17-62]. Thirty-five manuscripts described/detailed the isolated case[17,19,23-30,32,33,37-43,45,46,48-54,56-62]. Two of the manuscripts included in the review are original articles[35,44]. For one case, the details were extracted from a manuscript published as a case series[31]. Eight manuscripts are published and available under the headings of medical images, letters to the editor, correspondence, and technical notes[18,20-22,34,36,47,55]. Four manuscripts included n = 5 cases of the above-mentioned VPS complications were excluded from review due to the incomplete desired information[63-66].
This review included n = 46 cases (n = 27; 58.69% were males and n = 19; 41.3% were females). It was evident more in males, with a male-to-female ratio of 1.42:1. Group A included n=32 cases (n = 20; 62.5% male, and n = 12; 37.5% females) while Group B included n=14 cases (n = 7; 50% male, and n = 7; 50% females).
The indication for the primary VPS insertion was congenital hydrocephalus for approximately half of the entire cases (n = 22) cases and approximately sixty percent (n = 19) of the Group A cases. Post-infective hydrocephalus was also one of the indications for VPS insertion in approximately one-fifth (n = 6) of the Group A cases. Normal pressure hydrocephalus (NPH), idiopathic intracranial hypertension, and intracranial aneurysm with or without hemorrhage were the indications for the primary VPS catheter insertion for fifty percent of the Group B cases.
Group A cases were much younger than the Group B cases at the time of initial VPS placement. Two-thirds (n = 22) of Group A and one-fourth (n = 4) of Group B cases were infants, at the time of initial VPS placement. Three-fourths (n = 9) of Group B cases were > 40 years of age, at the time of initial VPS placement. Group A cases were much younger at the time of the diagnosis of VPS complications as well. More than half (n=17) of Group A cases were children ≤ 2 years of age at the time of diagnosis of the VPS complication mentioned above. One-fourths (n = 4) of Group B cases were children ≤ 5 years of age at the time of diagnosis of the VPS complication mentioned above. Seventy-two percent (n = 23) of Group A cases were ≤ 5 years of age, while more than half (n = 8) of Group B cases were > 40 years of age. Age was not a bar for the intra-gastric migration of the distal VPS catheter. A trans-oral extrusion of the distal VPS catheter was infrequently reported after 15 years, and only three cases were reported after the age of 15 years. Probably one of the reasons may be the age difference at the time of primary VPS insertion for both the Group cases and the second reason may be the difference in the indication for the initial VPS catheter insertion. The probable reason for a greater number of intra-gastric migrations clinically presented as trans-oral extrusion of the distal VPS catheter in children than in adult/older population may be because the number of VPS placements carried out in infants and children are many folds more than done in adults and older age. Like the present findings, a recent review included n = 210 cases of the management of extrusion of the distal part of peritoneal catheter through the anal canal, also evidenced that in 73% of the cases, the age of the cases was ≤ 5 years of age[11]. For n = 19 of the Group A and n = 9 of the Group B cases, the details of the shunt type/which type of the VPS catheter implanted during the initial procedure was not available/not mentioned by the authors in the manuscripts[20,21,23-27,29-32,34,36,38,42,43,45,47,48,52,54,55,57-62]. “Chhabra slit n spring hydrocephalus VPS catheter” (Shahjahanpur, India) was used during the VPS implantation in n = 8 of the Group A cases[22,28,33,35,37,39,40,44]. For the remaining n = 4 Group A and n = 5 Group B cases, the shunt catheter used during VPS insertion were: (1) Raimondi peritoneal catheter (n = 3); (2) Codman Hakim VPS system (n = 5); and (3) VPS catheter (Biomed valve, slit valve, silicon catheter, not spring type) (n = 1), respectively[17-19,41,46,49-51,53,56]. As in this review, in sixty percent (n = 28) cases, which type of VPS catheter implanted was not available, and therefore it is not clear whether any particular shunt catheter was responsible for the increased risk of gastric perforation.
For the entire Group A and Group B cases, the interval from the initial VPS insertion/VPS revision to the diagnosis of the VPS complication described above ranged from one day to 11 years. For the cases that had a history of VPS revision, for them, the interval was calculated from the date of the last VPS revision done. In seventy-two percent (n = 33) of the entire case, this complication was detected within 24 mo after the VPS insertion/shunt revision. In 60% (n = 28) of the entire case, it occurred within 12 mo of VPS insertion/last shunt revision. In one-fourths (n = 12) of the entire cases, it was detected within 6-months of VPS insertion/shunt revision. For Group A cases, the said complication was detected within a month to 24 mo in more than four-fifths (n = 27) of cases. For Group B cases, the complication was detected within a month to 24 mo in forty-three percent (n = 6) cases. In n = 5 of Group B cases, the interval from VPS insertion to the detection of the said VPS complication was 3 to 10 years. A recent systematic review (2022) of the n = 210 cases on the management of trans-anal extrusion of the distal VPS catheter also revealed that in 70% of the cases, it occurred within 12 mo after the VPS insertions[11]. Like the above finding, the present review also revealed that 60% of the entire cases and four-fifths of Group A cases were also diagnosed within 12 mo of the VPS insertion. In a recent systematic review (2022) of the n = 37 instances of the management of the perforation and intra-vesical (urinary bladder) migration of the distal part of the peritoneal catheter clinically presented with or without per-urethral extrusion identified that only onethird of the cases presented within 12 mo after the VPS insertion[12]. It means that urinary bladder perforation by the distal VPS catheter is a late complication than colonic or gastric perforation by the distal VPS catheter.
Peroral extrusion of the distal part of a VPS catheter was the chief complaint and clinical finding for Group A cases and it was evident in all the n = 32 cases reviewed. In the majority of the cases, the trans-oral extrusion of the distal VPS catheter was associated with a bout of vomiting of short duration. Mild abdominal pain/discomfort relating to the upper GI tract was also documented in some cases. A few Group A cases also had associated headaches and fever. Clinical presentation in Group B cases was vague, and not specific to the distal VPS catheter complication. The Group B cases mostly had symptoms relating to the CNS or gastrointestinal tract (GIT). Five cases presented with symptoms related to the CNS. Six cases presented predominantly with symptoms related to the upper GIT. Eight cases also had associated general symptoms like fever, weakness, and others.
In a 5-mo-old girl, an iatrogenic gastric perforation occurred during the initial/primary VPS insertion, but it was unnoticed. On the first postoperative day, the presence of a distal VPS catheter within the lumen of the stomach was detected, and it was treated successfully[54]. An 87-year-old man underwent investigation for upper GI bleeding/coffee-ground vomiting and the intra-gastric presence of his distal VPS catheter was detected during the upper GI endoscopy[57]. A 65-year-old woman was under investigation for iron deficiency anemia and the intra-gastric presence of her distal VPS catheter was detected during the upper GI endoscopic evaluation[60].
VPS catheter tract infection was not a frequent clinical finding. During the clinical examination, n = 4 (two from each Group) cases had features suggestive of shunt tract infection. Clinical features of peritonitis were not documented in any of the cases reviewed. The occurrence of peritonitis after the bowel/colon perforation by a distal VPS catheter is not a rule, and it was not reported in most cases. In a systematic review of trans-anal extrusion of the distal VPS catheter, peritonitis was documented only in 3.8% of the cases[11]. Possibly for similar reasons like colon perforation clinically presented with per-rectal extrusion of VPS catheter, there was no peritonitis even though there was perforation and migration of distal VPS into the stomach in a present review. Clinical signs of meningitis were evident in n = 4 of Group B and none of the Group A cases. Cerebrospinal fluid (CSF) infection was documented in n = 11 cases. CSF infection was more frequently documented in Group B cases, as half of them had CSF infection. CSF infection was less frequent in Group A cases, as only n = 4 had CSF infection at the time of diagnosis of the VPS complication mentioned above.
The clinical diagnosis of peroral extrusion of the distal part of a VPS catheter was evident for the entire Group A cases. Various investigations were required for the diagnosis of Group B cases. Varieties of investigations were needed and carried out to confirm or exclude the continuity of the VPS catheter, the presence or absence of gas under the diaphragm, peritoneal fluid collections, and evaluation of the ventricular system. A skiagram of the head, abdomen, and chest was one of the commonly advised investigations. Cranial computed tomography (CT) scan was ordered in n = 15 cases (n = 10 for Group A and n = 5 for Group B) for the confirmation of the position of the ventricular catheter within the ventricle and the understanding of the hydrocephalus/ventricles[23,24,28,32,37,38,40,42,43,46,51,58,59,61,62]. CT scan of the abdomen was ordered for n = 9 cases[26,46,55,56,58,59,60-62]. It was only ordered for n = 2 of the Group A cases[26,46]. CT scan of the abdomen was ordered for n = 7 of the Group B cases for the confirmation of the intra-gastric position of the distal VPS catheter[55,56,58,59,60-62]. Shuntogram (n = 3) and dye studies (n = 3) were performed/done during the investigations[33,34,50,51,53]. Upper gastrointestinal endoscopic evaluation was carried out in n = 12 cases[19,32,34,38,55-62]. Eight of the Group B cases were evaluated by the upper GI endoscopy, which was helpful in the confirmation of the intra-gastric location of the distal VPS catheter[55-62].
Much progress has taken place not only in the field of better understanding of the etiopathogenesis of the hydrocephalus, but also in the field of physiology of CSF circulation, development of shunt devices/shunt systems, use of newer technology, perioperative and postoperative care, and management of the shunt related complications[67-69]. VPS catheter implantation is among the most frequently performed surgical procedures in the management of hydrocephalus, caused by various etiology, and performed across the globe for all ages. Many VPS-related complications also require shunt revisions[70-74]. The insertion of the peritoneal/distal VPS catheter within the peritoneal cavity for primary VPS insertion or shunt revision surgery can be done via mini-laparotomy, using a trocar or laparoscopic technique with the advantages and disadvantages of each of the surgical techniques[75-77]. A recent international survey carried out for the preference of the distal VPS catheter insertion within the peritoneal cavity found that most of the responded neurosurgeons preferred doing so via/through a mini-laparotomy, and it was frequently preferred by the surgeons over the laparoscopic methods[78].
Management of the intra-gastric migration of the distal VPS catheter with or without trans-oral extrusion is three-fold: (1) The removal of intra-gastric migrated distal VPS catheter; (2) treatment of the gastric perforation caused by the distal VPS catheter; and (3) shunt revision, if required. It differs from case to case, depending upon the presence or absence of shunt or shunt tract infection, CSF infection/meningitis, peritonitis, and the general condition of the patient. Various surgical procedures were offered for the management of the above-described complication in n = 43 cases of both Groups. One-third (n = 16) of the entire case was treated by the removal of the entire VPS catheter. One-fourth (n = 12) of the entire case was treated by the removal of the part of the peritoneal/distal VPS catheter with or without conversion to EVD. In six cases (n = 5 Group A and n = 1 Group B), the entire/distal VPS catheter was removed and shunt revision was carried out during the same operative procedure. In five cases (n = 4 Group A and n = 1 Group B), the entire VPS catheter was removed and an EVD was inserted. Four cases (n = 2 Group A and n = 2 Group B) were managed by the relocation of the distal/remaining distal VPS catheter within the peritoneal cavity. In two instances/cases, the intra-gastric presence of the distal VPS catheter was detected during the autopsy[49,52]. In one of the cases, the surgical therapy was deferred as he was clinically stable and did not have symptoms related to the intra-gastric migration of the distal VPS catheter[58]. Percutaneous surgical removal of the entire/distal VPS catheter with or without an EVD was the procedure of choice and was preferred in n = 27 (n = 24 Group A and n = 3 Group B) cases. Exploratory laparotomy was carried out for the management of the above-described distal VPS catheter complication in n = 11 (n = 7 of Group A and n = 4 of Group B) cases[18,22,32,39,41,42,43,53,54,59,61]. The laparoscopic technique was applied in n = 5 cases and was carried out in n = 4 Group B cases[34,55,57,60,62].
The functional status of the VPS catheter was not mentioned/not provided in the literature reviewed for n = 22 of Group A and n = 11 of Group B cases[17,19-23,26,27,30-32,34-36,41-49,51-54,57-62]. The distal end of the VPS catheter was draining CSF, confirming that the VPS catheter was functioning well in n = 6 of Group A and n = 2 of Group B cases, respectively[18,24,25,29,37,39,50,55]. The authors also documented that the VPS catheter was not functional, and it was not draining CSF at the distal end in n = 4 of Group A and n = 1 of Group B cases, respectively[28,33,38,40,56].
Crust formation at the tip of the distal VPS catheter was not detected/documented in any of the Group A cases managed for the transoral extrusion of the distal VPS catheter[17-48]. Crust formation at the tip of the distal VPS catheter was not detected/documented during the radiological/endoscopic evaluation and operative procedures executed for the management of intragastric migration of the distal peritoneal catheter/distal VPS catheter n = 11 of the Group B cases[50,51,53-57,59-62]. Only in one of the Group B cases, during the autopsy, a white stone-like structure was detected at the tip of the distal VPS catheter, although the other drainage holes/perforations of the distal VPS catheter were patent. The intragastric part of the distal VPS catheter was like a rigid coiled spring catheter[52]. In this case, the stone/crust formation at the tip of the distal VPS catheter that happened either before the intragastric migration or afterward was also not explained/not clear[52].
The literature review documented/revealed the use of the stomach as the site for the insertion of the distal VPS catheter for CSF diversion in the treatment of hydrocephalus[79-82]. In 1965, Alther described a direct insertion of the distal VPS catheter into the stomach through a Witzel-type fistula[79,80]. In 1972, Lamesch reported/published the use of a gastric tube for the insertion of a distal CSF shunt catheter in seven mongrel dogs. He experimented and performed ventriculogastrostomy by means of the creation of the pedunculated gastric pouch and insertion of the distal shunt catheter within the gastric pouch. In the same paper, he also reported the first successful result of a ventriculogastrostomy that was performed by him on a 3-year-old boy. The operation was performed by him on April 22, 1970. He further reported that the boy was doing well at the follow-up done 10 mo after the operation[80]. In 1975, Weiss et al[81] also reported ventriculogastrostomy as an alternative means for CSF diversion as a preliminary study. They experimented with the technique in eight of the mongrel dogs. They also performed ventriculogastrostomy on a 3-wk-old child for the treatment of hydrocephalus. In 1977, Duff et al[82] reported their experience with ventriculo-gastric shunts and the role of gastroscopy in shunt evaluation and revision. They reported their experience of ventriculo-gastric shunts, that was performed on six patients, and their age ranged from three weeks to nine years. Two of their cases developed distal shunt obstruction and were evaluated and successfully treated by means of gastroscopy.
The stomach was the site of perforation by the distal VPS catheter n = 25 of the Group A and all (n = 14) the Group B cases. The duodenum was perforated by the distal VPS catheter in two of the Group A cases[42,43]. The jejunum was perforated by the distal VPS catheter in two of the Group A cases[22,46]. The site of perforation by the distal VPS catheter was not mentioned/not provided in the manuscripts for three cases. Repair of the bowel perforation caused by the distal VPS catheter is not always required. A systematic review of n = 210 cases of bowel perforation by the distal part of the VPS catheter clinically presented with the extrusion of the same via the anal canal revealed that colon/bowel perforation was repaired only in onefourth of the cases. In the remaining, threefourths cases, the colon/bowel perforation healed spontaneously, after the removal of the migrated/extruded VPS catheter[11]. In the present systematic review of n = 46 cases of gastric perforation by the distal VPS catheter only one-fourth (n = 11; n = 6 Group A and n = 5 Group B) of the cases, the perforation site was surgically repaired. In two cases, the perforation site was sealed by the fibrin glue application. In more than half (n = 27) cases, the gastric perforation caused by the distal VPS catheter was not repaired and healed spontaneously.
Shunt revision was also an integral part of the management of the intra-gastric migration of a distal VPS catheter clinically presented with or without peroral extrusion of the distal end of VPS catheter. In the present review of n = 46 cases of the trans-gastric migration of the distal VPS catheter, the details for n = 25 (n = 20 Group A and n = 5 Group B) cases are available regarding the shunt revision procedures. Delayed re-VPS insertion/VPS revision or VA shunt placement was preferred over the immediate shunt revision. The advantages of delayed reVPS insertion/VPS revisions or VA shunt insertion were that the optimal treatment was provided for meningitis/CSF infection, if present, and it was also possible to evaluate the cases for the requirement of shunt revision. Delayed re-VPS insertion/VPS revision or conversion to a VA shunt was carried out in n = 19 (n = 15 Group A and n = 4 Group B) cases. For the Group A cases; delayed re-VPS insertion in n = 11, VPS revision in n = 2, and VA shunt placement in n = 2, were preferred by the authors. In six (n = 5 Group A and n = 1 Group B) cases, the shunt revision procedure was executed immediately after removing the entire/distal VPS catheter. The authors performed an immediate re-VPS insertion in n = 3, VPS revision in n = 1, and an immediate VA shunt insertion in n = 2 cases. In the present review, authors also documented that re-VPS insertion/VPS revision or VA shunt insertion was not required in n = 10 (n = 7 Group A and n = 3 Group B) cases, neither during the immediate postoperative nor during the followup period.
The exact cause and mechanism of why and how the distal VPS catheter perforates the stomach, migrated within the stomach, and in some of them extruded trans-orally and not extruded in other cases. Possible factors that were responsible for the above in the present review were; the younger age of cases (infants and children younger than 5 years), redundant intra-peritoneal distal VPS catheter in children, history of VPS revisions, and history of abdominal/GI surgery. One-fourth (n = 11) underwent VPS revision in the past, and n = 8 of the cases had a history of abdominal/GI surgery in the past and were also the possible factors responsible for the migration of the distal VPS catheter into the stomach. The presence of meningitis (n = 4) and CSF infection (n = 11) in the present study was most probably the result of ascending infection, and may not be the factor responsible for the VPS complication discussed. The perforation of the gastric wall by the distal VPS catheter may be a result of the continuous friction effect. Once there is a small perforation, it is sealed off without producing clinical peritonitis. The distal VPS catheter is forced within the stomach due to the variation in the size of the stomach, the force of abdominal wall movements, and changes in the intra-abdominal pressure. Once it is within the stomach, why some of them extruded trans-orally is not very clear. Most probably, the presence of redundant extra length of the distal VPS catheter within the peritoneal cavity/stomach (especially in children) is responsible for the peroral extrusion of the distal part of a VPS catheter. The intra-gastric distal VPS catheter acts as a foreign body and is expelled per-orally by forceful regurgitation/vomiting. The combination of forceful upward movement of the stomach, increased intra-peritoneal pressure, and forceful abdominal wall movement during nausea/vomiting are responsible for the trans-oral extrusion/protrusion of the distal VPS catheter. The length of the distal VPS/peritoneal catheter is not much extra or redundant in adults and older people and may be the reason for the migration of the distal VPS catheter within the stomach only, and clinically not presenting as trans-oral extrusion of the same.
In the present review, a total of five cases documented complications that were detected during the immediate and late postoperative period. The complications revealed were brain stem herniation (n = 1), CSF infection (n = 2), meningitis (n = 1), and VPS catheter extrusion from the abdominal wound (n=1). During the management of the cases of the intra-gastric migration of the distal VPS catheter, this study revealed a total of four (8.69%) deaths, two from each Group[17,23,49,52]. In a 9.3-year-old girl, a VPS catheter was inserted for post-infective hydrocephalus. She also required a feeding gastrostomy for inadequate oral nutritional intake. Three months after VPS insertion, she presented with trans-oral extrusion of her distal VPS catheter, without the clinical features of peritonitis or meningitis, and her CSF also did not detect any organisms. Her VPS complication was treated with EVD and placement of a VA shunt. One month after the VA shunt insertion, she developed acute brain stem herniation and died of the same[17]. A two-year-old boy was diagnosed with congenital hydrocephalus and associated neural tube defect (NTD). His NTD was repaired and a VPS catheter was also placed at the age of 9 mo. Fifteen months after the VPS insertion at the age of two years, he presented with trans-oral extrusion of his distal VPS catheter, without the clinical features of meningitis and peritonitis. His VPS complication was treated with the removal of part of the peritoneal/distal VPS catheter and conversion of the proximal VPS catheter as an EVD. He had a CSF infection and developed ventriculitis that failed to respond well to the antibiotics, and finally died of the same during the treatment[23]. Two of the Group B cases died due to the intra-gastric migration of the distal VPS catheter and the related complication[49,52]. A 69 years-old female developed meningitis 7 mo after VPS insertion that was done for normal pressure hydrocephalus. She was treated conservatively and finally, she died of pneumonia 27 mo after the VPS insertion[49]. A 68-year-old man was diagnosed with NPH and a VPS catheter was implanted. His CNS condition deteriorated further. He was also detected with CSF infection and was treated with antibiotics and other supportive measures, but died of the same[52]. In the above two cases, the intra-gastric migration of the distal VPS catheter was detected during the autopsy[49,52].
This systematic review revealed/obtained a limited number of published literature/manuscripts, and it is one of the limitations of this review. Four manuscripts that included five cases were excluded from review for various reasons[63-66]. There was no uniformity in the treatment of the cases, treated by surgical techniques ranging from simple per-cutaneous removal of the entire/distal VPS catheter to exploratory laparotomy. For n = 4 (8.69%) cases, the entry site in the bowel by the distal VPS catheter is also not known/not available. The exact cause and the mechanism for the perforation of the stomach and intra-gastric migration of the distal VPS catheter is also not known.
Intra-gastric migration of the peritoneal end of a VPS catheter is one of the rare complications of VPS catheter implantation done for the treatment of hydrocephalus across all age groups. Intra-gastric migration with trans-oral extrusion of the distal VPS catheter was twice more commonly reported than the intra-gastric migration of the distal VPS catheter without trans-oral extrusion. It was more frequently reported in children, although also reported in adults and older people. Intra-gastric migration of the distal VPS catheter without transoral extrusion was more frequent in adults and older age groups. Formal exploration of the abdomen for the management of the VPS complication described above was neither done nor required in 70% of cases. In two-thirds of cases, the repair of the stomach/bowel perforation caused by the distal VPS catheter was not done and it healed after the removal of the distal shunt catheter from the stomach/bowel. A very high degree of clinical suspicion is required for the diagnosis of the intra-gastric migration of the distal VPS catheter, clinically presenting without trans-oral extrusion.
Intra-gastric migration of the distal ventriculoperitoneal shunt (VPS) catheter clinically presenting with or without trans-oral extrusion is one of the rare complications of VPS catheter insertion.
To know more about the intra-gastric migration of the distal VPS catheter.
This systematic review of the literature aims to highlight the demographics, clinical characteristics, and outcome of the surgical procedures performed for the intra-gastric migration of the distal VPS catheter, clinically presented with or without trans-oral extrusion of the distal end of peritoneal/VPS catheter.
An online search was carried out for extraction/retrieval of published literature about the intra-gastric migration of the distal VPS catheter. PubMed, PubMed Central, ResearchGate, Google Scholar, and Google Images databases were searched using various terminology relating to the VPS complications. Manuscripts were retrieved from 1980 to December 2022. The selection of literature for the present review was done by assessing the titles, abstracts, and full texts of the manuscripts.
A total of n = 46 cases of intra-gastric migration of the distal VPS catheter clinically presented with or without peroral extrusion were recruited for the systematic review and were retrieved from the n = 46 manuscripts. Approximately sixty percent of them were children ≤ 5 years of age at the time of diagnosis of the complication mentioned above. In seventy-two percent of cases, this complication was detected within 24 mo after the VPS insertion/last shunt revision. Removal of the entire VPS catheter/removal of part of the distal/distal VPS catheter with or without external ventricular drainage was preferred by the authors. Percutaneous surgical removal of the entire or the distal VPS catheter with or without external ventricular drainage was a procedure of choice and was opted for n = 27 cases. For the management of VPS complications mentioned above, formal laparotomy was carried out only in n = 11 cases. In eighty-five percent of cases, the site of bowel perforation was the stomach. The site of bowel perforation was repaired only in n = 11 cases.
Intra-gastric migration of the peritoneal end of a VPS catheter is one of the rare complications of VPS catheter implantation done for the treatment of hydrocephalus across all age groups. It was more frequently reported in children, although also reported in adults and older people. Formal exploration of the abdomen for the management of the VPS complication described above was neither done nor required in 70% of cases. In two-thirds of cases, the repair of the stomach/bowel perforation caused by the distal VPS catheter was not done and it healed after the removal of the distal shunt catheter from the stomach/bowel.
This systematic review revealed that the intra-gastric migration of the peritoneal end of a VPS catheter was more commonly reported in children than adults and older people. Intra-gastric migration with peroral extrusion of the distal VPS catheter was twice as commonly reported than the intra-gastric migration of the distal VPS catheter clinically presented without peroral extrusion. A high degree of clinical suspicion is required for the diagnosis of cases of an intra-gastric migration of the distal VPS catheter clinically presenting without trans-oral extrusion. The exact mechanism for the intra-gastric migration of the peritoneal end of the VPS catheter is not known and requires some specific experimental studies.
Provenance and peer review: Invited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Neurosciences
Country/Territory of origin: India
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Rajderkar DA, United States S-Editor: Liu JH L-Editor: A P-Editor: Cai YX
| 1. | Hochstetler A, Raskin J, Blazer-Yost BL. Hydrocephalus: historical analysis and considerations for treatment. Eur J Med Res. 2022;27:168. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 62] [Cited by in RCA: 81] [Article Influence: 27.0] [Reference Citation Analysis (0)] |
| 2. | Srinivas D, Tyagi G, Singh GJ. Shunt Implants - Past, Present and Future. Neurol India. 2021;69:S463-S470. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 3. | Pande A, Lamba N, Mammi M, Gebrehiwet P, Trenary A, Doucette J, Papatheodorou S, Bunevicius A, Smith TR, Mekary RA. Endoscopic third ventriculostomy versus ventriculoperitoneal shunt in pediatric and adult population: a systematic review and meta-analysis. Neurosurg Rev. 2021;44:1227-1241. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 16] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 4. | Chalasani R, Goonathilake MR, Waqar S, George S, Jean-Baptiste W, Yusuf Ali A, Inyang B, Koshy FS, George K, Poudel P, Mohammed L. The Outcome of Surgical Intervention (Ventriculoperitoneal Shunt and Endoscopic Third Ventriculostomy) in Patients With Hydrocephalus Secondary to Tuberculous Meningitis: A Systematic Review. Cureus. 2022;14:e25317. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Reference Citation Analysis (0)] |
| 5. | Reddy GK, Bollam P, Caldito G. Long-term outcomes of ventriculoperitoneal shunt surgery in patients with hydrocephalus. World Neurosurg. 2014;81:404-410. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 186] [Cited by in RCA: 249] [Article Influence: 20.8] [Reference Citation Analysis (0)] |
| 6. | Merkler AE, Ch'ang J, Parker WE, Murthy SB, Kamel H. The Rate of Complications after Ventriculoperitoneal Shunt Surgery. World Neurosurg. 2017;98:654-658. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 92] [Cited by in RCA: 144] [Article Influence: 16.0] [Reference Citation Analysis (0)] |
| 7. | Desai VR, Sadrameli SS, Jenson AV, Asante SK, Daniels B, Trask TW, Britz G. Ventriculoperitoneal shunt complications in an adult population: A comparison of various shunt designs to prevent overdrainage. Surg Neurol Int. 2020;11:269. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 17] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 8. | Paff M, Alexandru-Abrams D, Muhonen M, Loudon W. Ventriculoperitoneal shunt complications: a review. Interdisciplinary Neurosurgery. 2018;13:66-70. [RCA] [DOI] [Full Text] [Cited by in Crossref: 82] [Cited by in RCA: 139] [Article Influence: 19.9] [Reference Citation Analysis (0)] |
| 9. | Harischandra LS, Sharma A, Chatterjee S. Shunt migration in ventriculoperitoneal shunting: A comprehensive review of literature. Neurol India. 2019;67:85-99. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 41] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 10. | Morosanu CO, Nicolae L. Gastrointestinal complications following ventriculoperitoneal shunt insertion for pediatric hydrocephalus. J Pediatr Neurosci. [Epub ahead of print] [cited 2023 June 10]. [RCA] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 11. | Ghritlaharey RK. Systematic literature review of the management of transanal extrusion of distal ventriculoperitoneal shunt catheter: 1966–2020. Med J DY Patil Vidyapeeth. 2022;15:629-659. [RCA] [DOI] [Full Text] [Cited by in Crossref: 1] [Reference Citation Analysis (3)] |
| 12. | Ghritlaharey RK. Systematic review of migration of distal ventriculoperitoneal shunt catheter into the urinary bladder with or without per-urethral extrusion. Med J DY Patil Vidyapeeth. 2022;15:840-853. [RCA] [DOI] [Full Text] [Cited by in Crossref: 1] [Reference Citation Analysis (0)] |
| 13. | Ghritlaharey RK. Management of trans-vaginal extrusion of the distal ventriculoperitoneal shunt catheter: a systematic literature review from 1973 to 2021. Int J Res Med Sci. 2021;9:3416-3423. [RCA] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.3] [Reference Citation Analysis (1)] |
| 14. | Ghritlaharey RK. Review of the Management of Peroral Extrusion of Ventriculoperitoneal Shunt Catheter. J Clin Diagn Res. 2016;10:PE01-PE06. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 6] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 15. | Moher D, Liberati A, Tetzlaff J, Altman DG; PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. J Clin Epidemiol. 2009;62:1006-1012. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9247] [Cited by in RCA: 8877] [Article Influence: 554.8] [Reference Citation Analysis (0)] |
| 16. | Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. Syst Rev. 2021;10:89. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2603] [Cited by in RCA: 4474] [Article Influence: 1118.5] [Reference Citation Analysis (33)] |
| 17. | Griffith JA, DeFeo D. Peroral extrusion of a ventriculoperitoneal shunt catheter. Neurosurgery. 1987;21:259-261. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 31] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 18. | Danismend N, Kuday C. Unusual complication of ventriculoperitoneal shunt. Neurosurgery. 1988;22:798. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 15] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 19. | Park CK, Wang KC, Seo JK, Cho BK. Transoral protrusion of a peritoneal catheter: a case report and literature review. Childs Nerv Syst. 2000;16:184-189. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 53] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 20. | Jiménez Moya A, Penela Vélez De Guevara T, Gracia Remiro R, Romero Escós D, Santana Rodríguez C, Reig Del Moral C, Martín MH. Extrusion of a ventriculoperitoneal shunt catheter through the mouth. An Esp Pediatr. 2001;54:609-610 (Spanish). [RCA] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 21. | Kothari PR, Shankar G, Kulkarni B. Extruded ventriculo-peritoneal shunt: An unusual complication. J Indian Assoc Pediatr Surg. 2006;11:255-256. [RCA] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 22. | Odebode TO. Jejunal perforation and peroral extrusion of a peritoneal shunt catheter. Br J Neurosurg. 2007;21:235-236. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 14] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 23. | Berhouma M, Messerer M, Houissa S, Khaldi M. Transoral protrusion of a peritoneal catheter: a rare complication of ventriculoperitoneal shunt. Pediatr Neurosurg. 2008;44:169-171. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 25] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 24. | Murali R, Ravikumar V. Transoral migration of peritoneal end of ventriculoperitoneal shunt: A case report of a rare complication and review of literature. J Pediatr Neurosci. 2008;3:166-168. [RCA] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 25. | Sridhar K, Karmarkar V. Peroral extrusion of ventriculoperitoneal shunt: case report and review of literature. Neurol India. 2009;57:334-336. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 14] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 26. | Sinnadurai M, Winder MJ. Silicone spaghetti. J Clin Neurosci. 2009;16:1348-1350. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 6] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 27. | Low SW, Sein L, Yeo TT, Chou N. Migration of the abdominal catheter of a ventriculoperitoneal shunt into the mouth: a rare presentation. Malays J Med Sci. 2010;17:64-67. [PubMed] |
| 28. | Dua R, Jain R. Peroral extrusion of ventriculoperitoneal shunt: a case report and review of the literature. Cent Eur Neurosurg. 2011;72:107-108. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 5] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 29. | Agarwal M, Adhana R, Namdev H, Yadav YR, Agrawal T. Transoral extrusion of the ventriculo-peritoneal shunt: A case report and review of literature. J Pediatr Neurosci. 2011;6:149-151. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 5] [Reference Citation Analysis (0)] |
| 30. | Gupta M, Digra NC, Sharma N, Goyal S, Agrawal A. Peroral extrusion of the peritoneal catheter in an infant. N Am J Med Sci. 2012;4:290-292. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 6] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 31. | Kundal VK, Gajdhar M, Sharma C, Agrawal D, Kundal R. Wandering distal end of ventriculo-peritoneal shunt: Our experience with five cases and review of literature. J Nepal Paediatr Soc. 2012;32:266-269. [RCA] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 32. | Yilmaz MB, Egemen E, Tonge M, Kaymaz M. Transoral protrusion of a peritoneal catheter due to gastric perforation 10 years after a ventriculoperitoneal shunting: case report and review of the literature. Turk Neurosurg. 2013;23:285-288. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 4] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 33. | Gupta R, Mala TA, Gupta A, Paul R, Malla SA, Gupta AK. Transoral migration of peritoneal end of ventriculoperitoneal shunt with perforation of gastro-esophageal junction: a case report of a rare complication. Bangladesh J Med Sci. 2014;13:492-495. [RCA] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 34. | Mandhan P, Wong M, Samarakkody U. Laparoendoscopic removal of peroral extrusion of a ventriculoperitoneal shunt. Asian J Endosc Surg. 2015;8:95-97. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 7] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 35. | Thiong'o GM, Luzzio C, Albright AL. Ventriculoperitoneal shunt perforations of the gastrointestinal tract. J Neurosurg Pediatr. 2015;16:36-41. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 20] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 36. | Sohal AP, Whittle V, Nicholson C, Kisler J. Where did the oral tube originate from? J Paediatr Child Health. 2015;51:738, 740. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 37. | Ghritlaharey RK. Extrusion of ventriculoperitoneal shunt catheter through mouth in a two-year-old girl: A case report. Int J Clin Pediatr Surg. 2015;1:1-4. [DOI] [Full Text] |
| 38. | Shah AS, Singh D, Loomba P, Singh H, Mittal A, Srivastava S. Peroral extrusion of ventriculoperitoneal shunt: An unusual complication and review of literature. Indian J Neurosurg. 2016;5:196-201. [RCA] [DOI] [Full Text] [Cited by in Crossref: 1] [Reference Citation Analysis (0)] |
| 39. | Sharma DD, Meena A, Shukla AK, Sharma P, Raipuria G. Trans-oral migration of VP shunt tube through gastric perforation with review of literature. Int J Med Res Prof. 2017;3:303-305. [DOI] [Full Text] |
| 40. | Al Fauzi A, Suryaningtyas W, Wahyuhadi J, Parenrengi MA, Turchan A, Wijaya MC, Jonatan M, Mahyudanil, Setyono H. Upward migration and peroral extrusion of a peritoneal shunt catheter: Case report and review of the literature. Surg Neurol Int. 2017;8:178. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 6] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 41. | Reyes MJ, Díaz KA, Prada CA. Migración del catéter de derivación ventriculoperitoneal con protrusión por cavidad oral: Reporte de un caso y revisión de la literatura. Neurociencias Journal. 2017;24:153-160. |
| 42. | Badri M, Gader G, Belkahla G, Kallel J, Zammel I. Transoral migration of the inferior end of a ventriculoperitoneal shunt: A case report with literature review. Neurochirurgie. 2018;64:203-205. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 43. | Romuald K, Dominique NO, Guy V. Transoral migration of the inferior end of a peritoneal catheter: A rare complication of ventriculoperitoneal shunt. Int J Sci Res. 2018;7:1629-1632. |
| 44. | Ezzat AAM, Soliman MAR, Hasanain AA, Thabit MA, Elshitany H, Kandel H, Abdel-Bari SH, Ghoul AMF, Abdullah A, Alsawy MFM, Ghaleb AA, Al Menabbawy A, Marei AA, El Razik BA, Schroeder HWS, Marx S, Zohdi A, El Refaee E. Migration of the Distal Catheter of Ventriculoperitoneal Shunts in Pediatric Age Group: Case Series. World Neurosurg. 2018;119:e131-e137. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 25] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 45. | Bemora JS, Yu Song MT, Rakotondraibe WF, Ratovondrainy W, Rabarijaona M, Andriamamonjy C. A rare complication of ventriculoperitoneal shunt: gastric perforation. Journal of Advance Research in Medical & Health Science. 2019;5:744. [DOI] [Full Text] |
| 46. | Feeney V, Ansar N, Donaldson-Hugh B, Alalade AF. Transoral Protrusion of a Ventriculoperitoneal Catheter Caused by Jejunal Perforation in an Adult: Rare Case Report and Review of the Literature. World Neurosurg. 2020;137:200-205. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 47. | Calgaro S, Colangelo AC, Otchirov S, Pizzol D, Antunes M. Failed ventriculoperitoneal shunt as treatment of infantile hydrocephalus. World J Pediatr Surg. 2020;3:e000123. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 48. | Najib C, Abdellaoui H, Othmane A, Abdelhalim M, Khalid K, Youssef B. Transoral protrusion of a ventriculo-peritoneal shunt catheter in an 8-month-Old. J Pediatr Surg Case Rep. 2022;76:102112. [RCA] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 49. | Nishijima M, Ohyama H, Higuchi H. [Gastric perforation in ventriculo-peritoneal shunt--a case report (author's transl)]. No Shinkei Geka. 1980;8:679-683. [PubMed] |
| 50. | Oi SZ, Shose Y, Asano N, Oshio T, Matsumoto S. Intragastric migration of a ventriculoperitoneal shunt catheter. Neurosurgery. 1987;21:255-257. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 20] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 51. | Oshio T, Matsumura C, Kirino A, Go M, Bando Y, Manabe Y, Nakagawa Y. Recurrent perforations of viscus due to ventriculoperitoneal shunt in a hydrocephalic child. J Pediatr Surg. 1991;26:1404-1405. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 15] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 52. | Ho KJ. Recurrent meningitis associated with intragastric migration of a ventriculoperitoneal shunt catheter in a patient with normal-pressure hydrocephalus. South Med J. 1992;85:1145-1148. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 9] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 53. | Alonso-Vanegas M, Alvarez JL, Delgado L, Mendizabal R, Jiménez JL, Sanchez-Cabrera JM. Gastric perforation due to ventriculo-peritoneal shunt. Pediatr Neurosurg. 1994;21:192-194. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 28] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 54. | Christoph CL, Poole CA, Kochan PS. Operative gastric perforation: a rare complication of ventriculoperitoneal shunt. Pediatr Radiol. 1995;25 Suppl 1:S173-S174. [PubMed] |
| 55. | Hart AL, Hollanders D. 98 unusual cases and technical notes. Endoscopy. 2001;33:98. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (1)] |
| 56. | Masuoka J, Mineta T, Kohata T, Tabuchi K. Peritoneal shunt tube migration into the stomach--case report--. Neurol Med Chir (Tokyo). 2005;45:543-546. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 18] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 57. | Cheng JY, Lo WC, Liang HH, Kun IH. Migration of ventriculoperitoneal shunt into the stomach, presenting with gastric bleeding. Acta Neurochir (Wien). 2007;149:1269-1270. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 9] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 58. | Cohen-Addad DI, Hewitt K, Bell D. A ventriculoperitoneal shunt incidentally found in the stomach. Radiol Case Rep. 2018;13:1159-1162. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 6] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 59. | Sidhu JS, Mandal A, Kafle P, Chaulagai B, Gayam V. Ventriculoperitoneal shunt migration inside the gastric lumen: A rare case report. Cureus. 2019;11:e4453.. [RCA] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 5] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 60. | Yala KR, Shilpa L, Nazneen A. Peritoneal shunt catheter migration into the stomach: Case report and review of literature. Adv Res Gastroenterol Hepatol. 2019;12:75-76 (555844). [DOI] [Full Text] |
| 61. | Chen YH, Hsieh CT, Sun JM, Chang SI. Gastric perforation by a ventriculoperitoneal shunt in an adult. Neurosciences (Riyadh). 2020;25:144-147. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 62. | Scarascia A, Atallah E, Pineda MA, Rosenwasser R, Judy K. Gastric perforation from a migrating ventriculoperitoneal shunt: A case report and review of literature. Radiol Case Rep. 2022;17:4899-4902. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 63. | Fermin S, Fernández-Guerra RA, Sureda PJ. Extrusion of peritoneal catheter through the mouth. Childs Nerv Syst. 1996;12:553-555. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 12] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 64. | Tamlikha A, Shukri F, Zahari Z. Transoral migration of ventriculoperitoneal shunt: A rare presentation. GMJ. 2021;32:131-134. [RCA] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 65. | Faheem M, Jaiswal M, Prajapati HP, Kumar R, Saba Nu, Ojha BK. Unusual complications of ventriculoperitoneal shunt surgery: Tertiary care experience. J Pediatr Neurosci. [Epub Ahead of print] [Cited 2023 June 11]. [DOI] [Full Text] |
| 66. | Pant N, Singh S, Singh G, Kumar A, Rai RK, Rawat J, Wakhlu A. The wandering ventriculoperitoneal shunt and the scope of its salvage. Childs Nerv Syst. 2021;37:2613-2618. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 67. | Symss NP, Oi S. Is there an ideal shunt? A panoramic view of 110 years in CSF diversions and shunt systems used for the treatment of hydrocephalus: from historical events to current trends. Childs Nerv Syst. 2015;31:191-202. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 29] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 68. | Miyake H. Shunt Devices for the Treatment of Adult Hydrocephalus: Recent Progress and Characteristics. Neurol Med Chir (Tokyo). 2016;56:274-283. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 35] [Cited by in RCA: 45] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 69. | Texakalidis P, Tora MS, Wetzel JS, Chern JJ. Endoscopic third ventriculostomy versus shunt for pediatric hydrocephalus: a systematic literature review and meta-analysis. Childs Nerv Syst. 2019;35:1283-1293. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 18] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 70. | Frassanito P, Tamburrini G, Di Rocco C. Surgical treatment of hydrocephalus based on CSF shunt devices. In: Di Rocco C, Pang D, Rutka J (eds) Textbook of Pediatric Neurosurgery. Springer, Cham 2018. [DOI] [Full Text] |
| 71. | Sobana M, Halim D, Aviani JK, Gamayani U, Achmad TH. Neurodevelopmental outcomes after ventriculoperitoneal shunt placement in children with non-infectious hydrocephalus: a meta-analysis. Childs Nerv Syst. 2021;37:1055-1065. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 15] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 72. | Hasanain AA, Abdullah A, Alsawy MFM, Soliman MAR, Ghaleb AA, Elwy R, Ezzat AAM, Al Menabbawy A, Marei AA, Abd El Razik B, El Hamaky MI, Schroeder HWS, Fleck S, El Damaty A, Marx S, Nowak S, Baldauf J, Zohdi A, El Refaee EA. Incidence of and Causes for Ventriculoperitoneal Shunt Failure in Children Younger Than 2 Years: A Systematic Review. J Neurol Surg A Cent Eur Neurosurg. 2019;80:26-33. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 5] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 73. | Rizvi I, Garg RK, Malhotra HS, Kumar N, Sharma E, Srivastava C, Uniyal R. Ventriculo-peritoneal shunt surgery for tuberculous meningitis: A systematic review. J Neurol Sci. 2017;375:255-263. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 27] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 74. | Muram S, Isaacs AM, Sader N, Holubkov R, Fong A, Conly J, Hamilton MG. A standardized infection prevention bundle for reduction of CSF shunt infections in adult ventriculoperitoneal shunt surgery performed without antibiotic-impregnated catheters. J Neurosurg. 2023;138:494-502. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 7] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 75. | He M, Ouyang L, Wang S, Zheng M, Liu A. Laparoscopy versus mini-laparotomy peritoneal catheter insertion of ventriculoperitoneal shunts: a systematic review and meta-analysis. Neurosurg Focus. 2016;41:E7. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 26] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 76. | Ding Q, Wang J, Fan H, Jiang W, Guo H, Ji H, Song T, Xu S, Liu B. Introduction and comparision of three different fixation methods in the suprahepatic space in laparoscopy-assisted ventriculoperitoneal shunt for hydrocephalus. Sci Rep. 2023;13:6231. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 77. | Greuter L, Ruf L, Guzman R, Soleman J. Open versus laparoscopic ventriculoperitoneal shunt placement in children: a systematic review and meta-analysis. Childs Nerv Syst. 2023;39:1895-1902. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 3] [Article Influence: 1.5] [Reference Citation Analysis (1)] |
| 78. | Ruf L, Greuter L, Guzman R, Soleman J. Distal shunt placement in pediatric ventriculoperitoneal shunt surgery: an international survey of practice. Childs Nerv Syst. 2023;39:1555-1563. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 79. | Alther E. [The gastric valve. A new surgical technic for the treatment of infantile hydrocephalus]. Schweiz Med Wochenschr. 1965;95:234-236. [PubMed] |
| 80. | Lamesch AJ. Ventriculogastrostomy by means of a gastric tube for the treatment of hydrocephalus: a preliminary report. J Pediatr Surg. 1972;7:55-59. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 81. | Weiss MH, Jane JA, Apuzzo ML, Heiden JS, Kurze T. Ventriculogastrostomy, an alternative means for CSF diversion: a preliminary study. Bull Los Angeles Neurol Soc. 1975;40:140-144. [PubMed] |
| 82. | Duff TA, Rosenthal J, Jane JA. Evaluation and revision of ventriculo-gastric shunts by gastroscopy. Neurochirurgia (Stuttg). 1977;20:28-31. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |